Elbow Fractures and Dislocations
virtue of the complex articular structure, complex capsuloligamentous
and musculotendinous arrangements, and the proximity of neurovascular
structures. An increasing understanding of elbow injuries has led to a
rapid evolution in treatment concepts.90
Awareness of the patterns of injury and the pitfalls of each can lead
to restoration of a functional elbow in most patients. The majority of
complications can be addressed with secondary surgery, but certain key
structures—such as the ulnotrochlear relationship—must be reconstructed
and protected by the initial treatment or salvage measures will become
necessary.
180-degree capture of the trochlea in the trochlear notch is tilted
somewhat posterior, thereby increasing the anterior buttress of the
coronoid process (Fig. 32-1A). The trochlea is wide and has a central groove that interdigitates with a ridge in the center of the trochlear notch (Fig. 32-1B).
The contacts between (i) the anteromedial coronoid facet and the medial
lip of the trochlea and (ii) the radial head and capitellum represent
the most important stabilizing columns of the elbow. In the absence of
a radial head or capitellum, the contact between the lateral lip of the
trochlea and the lateral portion of the coronoid becomes more important.
The importance of the MCL may also have been overstated because of the
fact that its contribution to elbow stability is much easier to isolate
in cadavers.16,83
Injury to the lateral collateral ligament (LCL) is a consistent feature
of traumatic elbow instability and inadequate treatment of the LCL is
the source of a large proportion of the cases of posttraumatic elbow
instability.86,89,92
The LCL and MCL are often referred to as complexes to emphasize that
their contributions to elbow stability are enhanced by adjacent
capsuloligamentous, fascial, and musculotendinous structures.16 The anterior capsule also makes a substantial contribution to elbow stability.83
joint provide an important element of stability when other stabilizing
structures have been injured.24,26
 |
|
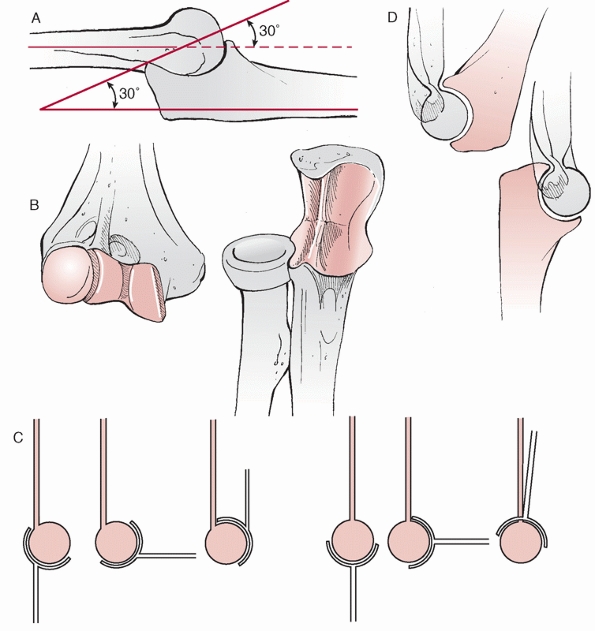
FIGURE 32-1 The elbow is an inherently stable joint. A.
The trochlear notch of the ulna provides a nearly 180-degree capture of the trochlea, which tilts posteriorly approximately 30 degrees. B. The ridge in the center of the trochlear notch interdigitates with a groove on the trochlea, further enhancing stability. C. Flexion of the elbow is enhanced by the anterior translation of the trochlea with respect to the humeral shaft as well as the coronoid and radial fossae on the anterior surface of the humerus that accept the coronoid process and radial head respectively. D. Posteriorly, the olecranon fossa enhances extension by accommodating the olecranon process. |
translation of the trochlea with respect to the humeral shaft and the
coronoid and radial fossae above the trochlea on the anterior surface
of the distal humerus62 (Fig. 32-1C). Extension of the elbow is enhanced by the olecranon fossa above the trochlea posteriorly (Fig. 32-1D).
The elbow has a predilection for stiffness after trauma as a result of
capsular scarring and formation of fibrous tissue in the fossae and
heterotopic ossification. Loss of the anterior translation of the
trochlea and articular malalignment, incongruity, and arthrosis will
also limit motion.
of these patterns can help the surgeon anticipate associated fractures
and ligament injuries, better predict the prognosis of the injury, and
plan and execute operative treatment.106,109,111,112
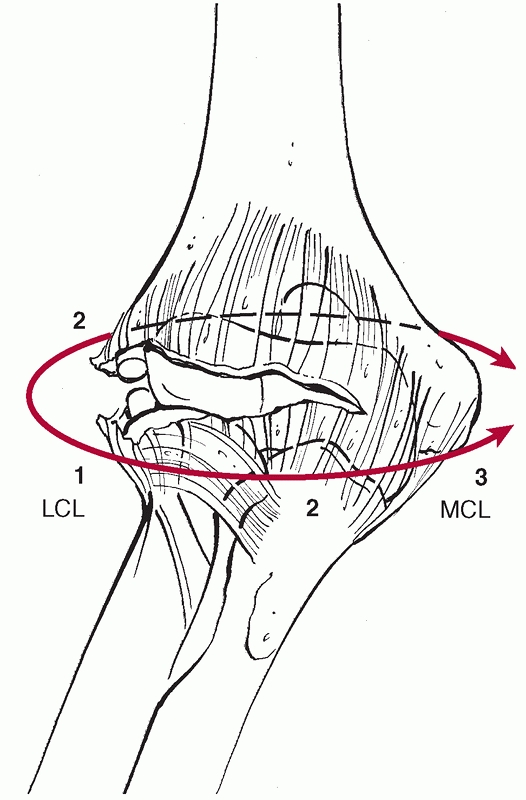
For example, the capsuloligamentous injury in an elbow dislocation
progresses from lateral to medial with a posterolateral rotatory
mechanism.91 As the elbow dislocates
posteriorly, the radial head and/or the coronoid process can fracture
as they collide with the distal humerus. The last structure to be
injured is the anterior band of the MCL91 (Fig. 32-3). On the other hand, the elbow can be destabilized by a distinct injury pattern that involves
a varus posteromedial rotational injury force.90
This is characterized by a fracture of the anteromedial facet of the
coronoid process with either a LCL injury, a fracture of the olecranon,
or both. The anatomy of specific injury patterns is described in
greater detail for each specific injury later.
 |
|
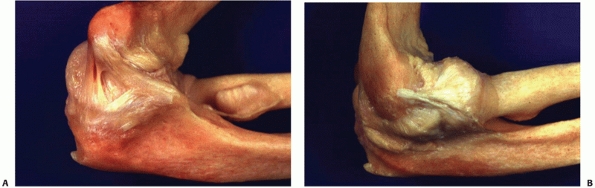
FIGURE 32-2 The medial and lateral collateral ligament complexes of the elbow. A.
The medial collateral ligament is described as having anterior, posterior, and transverse bundles, but the most important part is the anterior bundle, which originates on the undersurface of the medial epicondyle and inserts at the base of the coronoid process. B. The lateral collateral ligament originates from the inferior point of a small tubercle in the center of the lateral epicondyle, converges with the annular ligament and inserts onto the lateral aspect of the ulna at the crista supinatoris. (Courtesy of David Ruch, MD.) |
origins from the epicondyles along with a variable amount of the common
extensor or flexor musculature.73
This facilitates identification and repair of the injury. The MCL
originates from the anteroinferior portion of the medial epicondyle (Fig. 32-2A).
The LCL originates at the inferior portion of a small tubercle on the
lateral epicondyle, which represents the center of rotation of the
elbow (Fig. 32-2B).
 |
|
FIGURE 32-3
The capsuloligamentous structures of the elbow are injured in a lateral to medial progression during a dislocation of the elbow. The elbow can dislocate with the anterior band of the medial collateral ligament (MCL) remaining intact. |
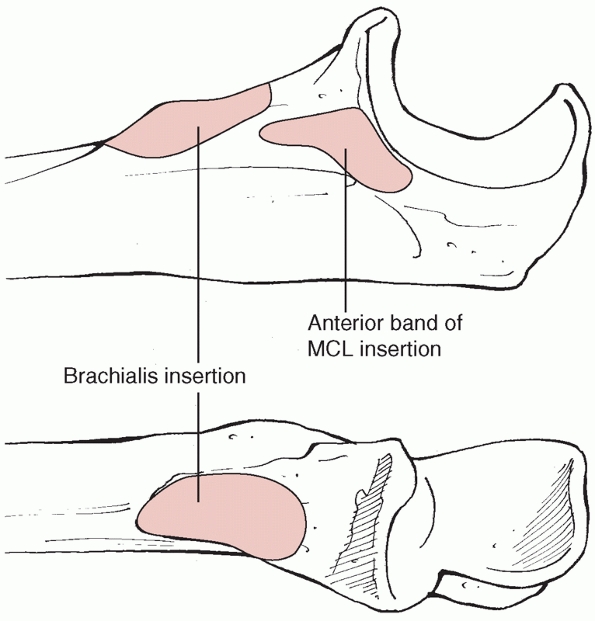
Consequently, the anterior band of the MCL is likely to be intact in
complex fractures associated with large fractures of the coronoid base
or anteromedial coronoid
fractures,
with its function disrupted by the bony injury and restored with stable
internal fixation. The brachialis has a broad insertion that extends
distal to the coronoid process8 (Fig. 32-4).
Even with large coronoid fractures, a substantial portion of the
brachialis insertion usually remains on the ulnar shaft. The anterior
capsule inserts a few millimeters below the tip of the olecranon
process.8 This has been interpreted
to mean that a very small coronoid fracture involving the very tip of
the coronoid process (type 1 according to Regan and Morrey) may
represent intra-articular free fragments; however, operative treatment
of small coronoid fractures discloses that coronoid tip fractures are
much larger on exposure than might be guessed based on the radiographs
and that they always include the capsular insertion.101,109,110,112,117
 |
|
FIGURE 32-4
The soft tissue attachments to the coronoid process. The anterior band of the medial collateral ligament (MCL) inserts at the base of the coronoid process. Consequently, if there is a large coronoid fracture, or a coronoid fracture that involves the anteromedial facet of the coronoid, the medial collateral ligament usually remains intact, the failure having occurred through bone rather than ligament. Although the anterior capsule inserts several millimeters below the tip of the coronoid process, tip fractures nearly always include the capsular insertion. The brachialis insertion is broad and extends distally and its function is rarely disrupted by a fracture of the coronoid. |
ulnar metaphysis occurs at the transverse groove of the olecranon,
which is a nonarticular area with consequently less subchondral bone,
and it is also a relatively narrow area in the sagittal plane (Fig. 32-1B). These factors may increase the susceptibility to fracture at this site.77
The robust blood supply of the skin of the upper extremity increases
the safety of elevating skin flaps even in the face of posttraumatic
swelling, blistering, and contusion. As a result, elbow surgeons often
prefer to make a single, long posterior skin incision, through which
all aspects of the elbow can be exposed, including the anterior
structures.94 Separate medial and
lateral incisions can also be used, although care must be taken to
protect the medial antebrachial cutaneous nerve on the medial side of
the elbow as it is prone to develop a painful neuroma when injured.23
constrictive cubital tunnel at the medial epicondyle and is held
tightly by Osbourne fascia for several centimeters distal to the elbow.
Consequently, it is no surprise that ulnar nerve dysfunction is common
after elbow injury in either the acute, subacute, or chronic setting.
In many cases, mobilization and transposition of the ulnar nerve
facilitate internal fixation of the medial epicondyle or the coronoid
process. An in situ release may be considered for any major elbow
trauma, particularly those associated with elbow instability, in an
attempt to help limit ulnar nerve-related sequelae.
with careful dissection and retractor placement. The radial nerve is
most often injured by retraction. The safety of retraction is improved
by a more extensive release of the common extensor and radial wrist
extensor muscles from the lateral condyle. One must also take care to
protect the posterior interosseous nerve when implants are applied to
the neck of the radius. The brachialis muscle usually provides
protection for the median nerve and brachial artery.
medial and lateral aspects of the elbow. These are not necessarily
internervous intervals, but since they are developed for only a few
centimeters, the nerve supply to the muscles is usually safe. On the
medial aspect, the flexor pronator mass can be split in half,49 the split of the flexor carpi ulnaris where the ulnar nerve runs can be developed,90,112 the entire flexor pronator mass can be elevated off of the ulna from posterior to anterior,94,127 or the flexor pronator mass can be detached and reflected distally (Fig. 32-5).
On the lateral aspect of the elbow, essentially any interval can be
developed. The most commonly used intervals are between the extensor
carpi radialis longus and brevis (or between the extensor carpi
radialis brevis and the extensor digitorum communis)48,81; between the anconeus and extensor carpi ulnaris (the Kocher approach)63; or reflecting the entire common extensor mass with the ruptured LCL origin or lateral epicondyle fracture fragment33,43,44,106 (Fig. 32-6).
 |
|
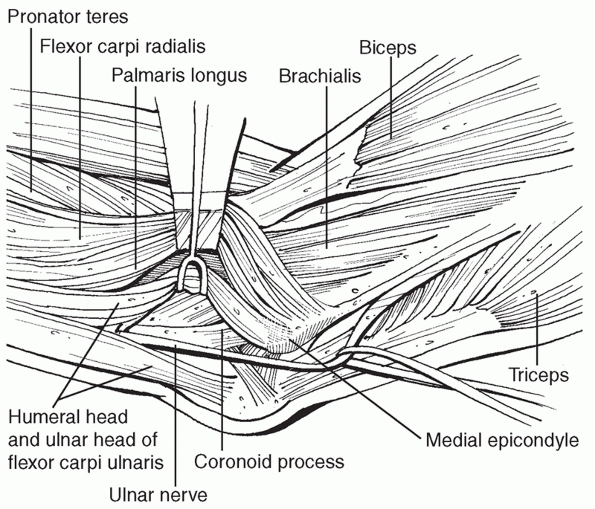
FIGURE 32-5
Medial exposures of the coronoid and elbow joint. From posterior to anterior, the intervals that can be used are elevation of the entire flexor pronator mass off of the medial ulna, development of the split in the flexor carpi ulnaris where the ulnar nerve runs, or splitting the flexor pronator mass anteriorly. |
 |
|
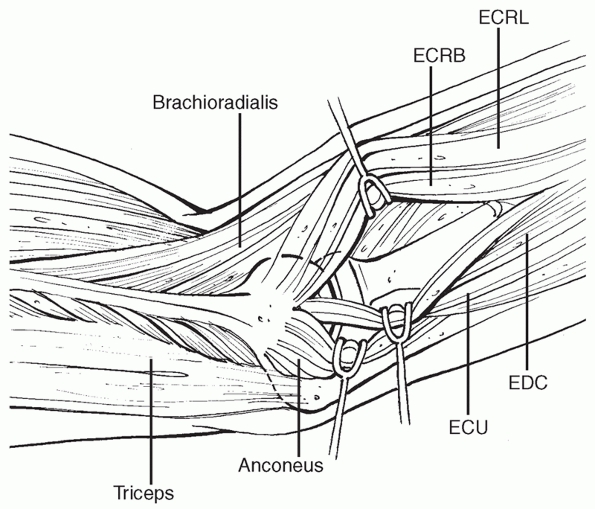
FIGURE 32-6
Lateral exposures of the elbow joint. The Kocher exposure (between the anconeus and extensor carpi ulnaris) is a commonly used exposure, but a more anterior exposure (splitting the common extensor muscles) can help protect the lateral collateral ligament complex and provide better access to the coronoid. |
and neurovascular structures. The posterior interosseous nerve crosses
over the radial neck and may be in direct contact with the bone.
Pronation helps to protect the nerve during a lateral approach to the
radial head19 and supination helps to protect it during an anterior approach.45
the placement of implants. The nonarticular area can be determined as a
roughly 90-degree arc with its midpoint directly laterally with the
forearm in neutral rotation, with a slightly greater margin anteriorly.124
It can be more straightforward to define a safe area intraoperatively
by applying a plate as posteriorly as possible with the forearm in full
supination125 or as the area on the
proximal radius that corresponds to the area between Lister’s tubercle
and the radial styloid on the distal radius9 (Fig. 32-7).
It has a slightly elliptical cross section and interdigitates precisely
with both the lesser sigmoid notch and the lateral lip of the trochlea,
as well as the capitellar articular surface.62
The slight angulation of the proximal radius with respect to the shaft
further complicates attempts to reconstruct or replace the radius.
 |
|
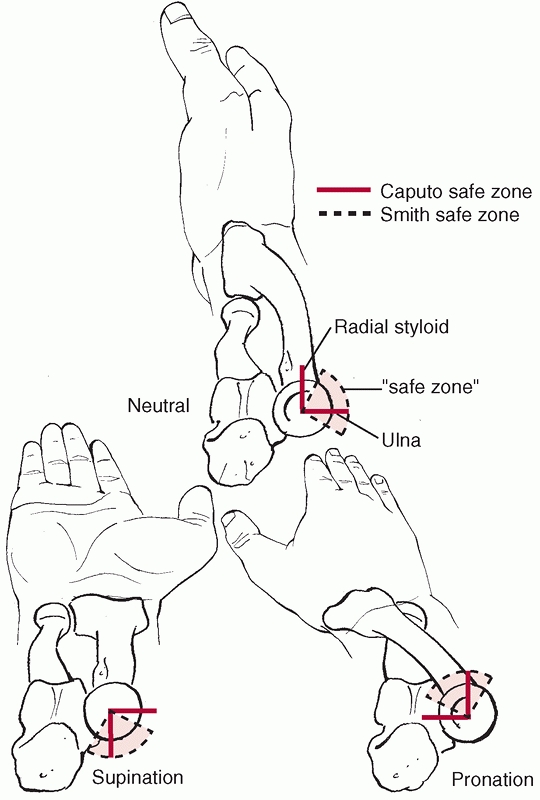
FIGURE 32-7
The nonarticular area of the radial head—or the so-called safe zone for the application of internal fixation devices—has been defined in various ways. Smith and Hotchkiss defined it based on lines bisecting the radial head made in full supination, full pronation, and neutral. Implants can be placed as far as halfway between the middle and posterior lines and a few millimeters beyond halfway between the middle and anterior lines. Caputo and colleagues recommend using the radial styloid and Lister’s tubercle as intraoperative guides to this safe zone, but this describes a slightly different zone. |
the posterior and proximal aspects of the olecranon. This is notable
during the application of a plate that contours around this portion of
the bone—if the center of the triceps insertion is not split and
elevated from the bone, the proximal aspect of the plate will rest well
off the bone. For complex olecranon fractures, this compromise may
sometimes be preferable to additional dissection of the soft tissue
attachments.
different injury types and are best considered in general before
reviewing the specific injury types.
determined by the injury forces or mechanism, the energy of the injury,
and the quality of the underlying bone. Recognition of the injury
pattern helps with management of the injury and counseling of the
patient.
present with varying degrees of pain, swelling, and ecchymosis. In many
cases, there is also instability, crepitation, and deformity.
open wounds or acute neurovascular injury. Most elbow injuries occur in
isolation with ipsilateral skeletal injuries and polytrauma being much
less common.
restoration of a congruent articular reduction. Malaligned articular
surfaces or instability will restrict motion and cause arthrosis that
is difficult to salvage.111,119
In contrast, a stiff but congruent elbow joint can often be restored to
good function with secondary surgeries even when there is extensive
heterotopic bone, an ununited fracture, or ulnar neuropathy.15,60,66,108
While the majority of elbow injuries benefit from early active use and
exercise, with complex articular fractures and very unstable elbows it
can be better to err on the side of achieving a healed and congruent
but stiff elbow by delaying mobilization or even—in rare instances—by
cross-pinning the joint.
understanding of the injury components. Appropriate treatment of each
injury component will help avoid pitfalls and provide the best
opportunity for recovery.
elbow injury and can become permanently stiff if confident active
exercises are not encouraged.
for daily activities are usually initiated within a few days, most
often the morning after surgery. The patient is encouraged to use the
other hand, gravity, and pushing against other objects to help assist
with elbow mobilization.
discouraged. There is a long-standing belief that this will contribute
to heterotopic bone formation. It may also be more likely to loosen
implants or impede healing. Finally, the patient must learn how to
mobilize his or her own upper extremity if the exercise program is to
be effective.
sagging or subluxation of an otherwise concentrically reduced joint
noted radiographically can usually be addressed by encouraging
confident active motion of the elbow.26,55
This adds a dynamic muscular component of stability, which overcomes
what is likely a form of pseudosubluxation of the joint. More
substantial subluxations should be treated operatively as they risk
damage to the articular surface. Given the useful dynamic component of
stability, combined with the fact that the elbow can dislocated in a
cast when unstable, the value of casts or braces for enhancing elbow
stability must be questioned—I personally do not use them. The idea of
an extension block brace is also common but probably not usually
necessary because patients then usually struggle to regain extension.
fracture is repaired, it is useful to avoid shoulder abduction for a
few weeks—“varus stress precautions.”26
various devices) with or without continuous anesthesia via a brachial
plexus catheter is gaining in popularity despite the lack of evidence
that it improves elbow motion. It is not clear that the additional risk
and cost are justified. I believe that active elbow motion is the key
and that motivated patients will do better—I therefore shy away from
passive treatments.
Some permanent loss of elbow motion is to be expected for all but the
simplest injuries; usually it is a loss of extension. Severe loss of
motion is often associated with heterotopic ossification, joint
incongruity, ulnar neuropathy, or arthrosis. In the absence of these
associated problems, a program of active-assisted exercises
supplemented by static progressive or dynamic elbow splints can improve
motion to a functional range in a large percentage of patients.34,37
With complex or unresponsive stiffness, operative release of the
contracted capsule, the constricted ulnar nerve, heterotopic bone, and
osteophytes can often improve motion.49
Passive manipulation of the elbow in an attempt to regain motion is
generally discouraged for fear of causing heterotopic ossification,
inhibiting healing, or fracturing the arm.
Both of these interventions may also inhibit fracture healing.
Radiation also has a potential cancer risk that must be respected. It
is still recommended that these prophylactic measures be used
selectively. Patients with head injuries, high-energy
fracture-dislocations, and repeat surgery during the first few weeks
are at the highest risk for substantial heterotopic ossification.
runs beneath the cubital tunnel fascia and Osbourne fascia. Cubital
tunnel syndrome—a gradually developing, chronic ulnar neuropathy—is
quite common after elbow trauma.72
It is likely because of the swelling, bleeding, tissue injury and
distortion, scar formation and tissue contracture, heterotopic
ossification, and arthrosis that develop after injury. Consideration
has been given to routine in situ decompression of the ulnar nerve for
some fractures that seem to be particularly at risk, such as
fracture-dislocations of the elbow.
injury can contribute to stiffness and pain in addition to affecting
hand function.29 It is important to
be aware of the importance of the ulnar nerve and always evaluate the
patient for symptoms and signs of ulnar nerve dysfunction, being
particularly suspicious when stiffness or pain is greater than might
otherwise be expected.
(caused by either the injury or handling of the nerve during surgery)
usually, but not always, recovers. It can take a very long time, in
some cases more than 1 year or longer, to recover. Serial clinical
examination and nerve conduction studies and electromyography can help
determine if surgical intervention is worthwhile. Operative treatment
is considered if serial neurophysiological testing does not demonstrate
improvement or if there is obvious worsening of the deficit on exam.
This will lead to arthrosis and must be addressed as soon as possible.
Even a few weeks of elbow motion and use in a malaligned position can
permanently damage the articular surfaces. At that point, only a
interpositional arthroplasty or total joint arthroplasty can be
considered—neither are great options in young, active individuals.
operative treatment, additional surgery is necessary as soon as
possible, even though early reoperation increases the risk of extensive
heterotopic ossification. Operative treatment of persistent elbow
malalignment consists of restoration of the stabilizing anatomy of the
elbow (radial head, coronoid, collateral ligaments) and hinged external
fixation to maintain a concentric reduction during the initial
treatment period.107,111,119
While this is fortunately uncommon, it is my impression that patients
in whom the trochlear notch is relatively spared do better than those
with instability associated with large and complex coronoid fractures.
vascularized and nonunions are relatively uncommon overall; however,
several specific injuries are more prone to nonunions than others and
require specific attention in treatment.
have been more problematic.93,113
Much of this seems to relate to inadequate fixation of the proximal,
metaphyseal fragment, particularly with osteoporotic bone. In the
treatment of both fresh fractures and nonunions, it seems better to
apply a long plate on the dorsal surface of the ulna that wraps around
the olecranon process, thereby providing additional screw fixation.113,116,119
It is also important not to remove the muscular and periosteal
attachments to the comminuted fragments in the metaphysis but rather to
bridge this area with a long plate and use the fragments as
vascularized bone grafts, rather than depending on them for stability.
In the setting of nonunion, debriding the fracture site of sclerotic,
inflammatory, and devitalized tissues and applying a nonstructural
cancellous bone graft has been very successful in our experience.115,116
We do not know the true incidence of nonunion because it rarely causes
symptoms; we do not usually reevaluate the elbow radiographically; and
ununited fractures of the radial head may eventually heal without
additional intervention if followed for longer than 2 years.14,120
In this case, usually the reconstructed radial head has served well as
a stabilizer of the elbow and, with the ligaments now healed, it can
safely be resected without replacing it.
operative treatment of elbow fractures. They are usually related to
complex open injuries, devitalized fracture fragments, and
immunocompromised patients. These infections are usually treated with
serial débridement, retention of implants, and parenteral antibiotics,
particularly when the fracture is complex. Healing of the fractures can
usually be achieved with this regimen. Eventually, complete eradication
of the infection usually requires implant removal. Elbow mobility is
typically allowed during treatment of infection. It can be assisted
with external fixation or hinged external fixation when there is
associated elbow instability or an unsupported fracture or nonunion.
excellent blood supply. Most patients with wound edge necrosis or
slight wound separation can be treated with dressing changes, but
patients with exposed implants or an underlying total elbow
arthroplasty should be treated operatively to obtain better skin cover.
This can often be accomplished with local rotational flaps, pedicled
flaps (such as a radial forearm flap), or, on occasion, a free
microvascular tissue transfer.122,126 I follow the so-called reconstructive stepladder (see Chapter 14), using the simplest procedure that will address the problem.
supplement and pharmaceutical companies, there is no cure for
posttraumatic arthrosis. Patients must adapt to and live with the
arthrosis or consider reconstructive procedures, none of which are
perfect. Débridement of osteophytes and loose bodies and capsulectomy
can be useful in the short term and may be best used in conjunction
with ulnar nerve release because ulnar neuropathy is a commonly
associated problem.1
Total elbow arthroplasty has a finite life span (with each revision
becoming increasingly more difficult), is more prone to infection and
major complications than knee or hip arthroplasty, requires strict
activity limitations (a 5-kg lifting limit), and is only suitable for
older, low-demand patients. Fascial interpositional arthroplasty is
better suited for younger, more active patients. The material used for
interposition has traditionally been the cutis layer of skin or the
fascia lata, but more recently allograft Achilles tendon has been used.
Interpositional arthroplasty does not eliminate elbow pain and leaves
the elbow somewhat unstable. Thus, it is best suited for patients with
severe stiffness related to arthrosis.12,30
capitellum. This can occur with a pure axial load (the most extreme
example of which is the Essex-Lopresti injury28),
with a posterolateral rotatory (elbow dislocation) type of load, or as
the radial head dislocates posteriorly as part of a posterior Monteggia
injury or posterior olecranon fracture-dislocation. The vast majority
of these injuries are the result of a fall onto the outstretched hand,
with the higher energy injuries representing falls from a height or
during sports.
(radiographically occult fractures, for instance) can be quite painful
because the elbow joint is usually distended with blood. There is a
variable amount of swelling and ecchymosis, which may correspond with
the degree of associated ligament injury. The distal radioulnar joint,
the interosseous space, and the medial side of the elbow should be
examined for signs of associated ligament injury. There is often
crepitation of the radial head with forearm rotation, and occasionally
a fracture fragment will block forearm rotation.
treat. One of the keys to successful management is to identify and
address associated injuries. This is particularly important for very
displaced fractures and fractures that involve the entire head of the
radius. In the study by Davidson and colleagues, all 11 patients with a
fracture involving the entire radial head had an associated injury to
the elbow or forearm.17 In my
experience, complex fractures of the entire head do occur without
associated ligament damage on occasion—particularly in older
patients—but I believe that one should assume there is an associated
injury until it has been proved otherwise. In fact, a markedly
displaced partial radial head fracture should raise similar concerns.
can help guide treatment. These patterns include (i) fracture of the
radial head associated with rupture of the MCL, (ii) concomitant
fractures of the radial head and capitellum, (iii) posterior
dislocation of the elbow with fracture of the radial head, (iv)
posterior dislocation of the elbow with fracture of the radial head and
the coronoid process (the so-called terrible triad of the elbow), (v)
posterior Monteggia fractures including posterior olecranon
fracture-dislocations, and (vi) Essex-Lopresti lesions and variants.
associated ligament injury. In particular, intraoperative examination
after removal of the radial head is important to avoid missing injury
to the interosseous ligament of the forearm. After removing the radial
head fragments, the surgeon should push and pull on the radius. If the
radial neck is very mobile and collides with the capitellum, the
surgeon should assume that the interosseous ligament of the forearm is
injured.123
include (i) correction of any hindrance of forearm rotation by the
fracture, (ii) restoration of elbow and forearm motion by early
initiation of an adequate exercise program, (iii) achieving stability
of the forearm and elbow, (iv) limitation of the potential for
ulnohumeral and radiocapitellar arthrosis, although the latter seems to
be an uncommon problem, and (v) avoidance of injury-related
complications and complications related to operative intervention,
including nonunion, avascular necrosis, an expanded or incongruous
radial head that restricts motion, restriction of motion by plates and
screws, radioulnar synostosis, posterolateral rotatory instability, and
a prominent radial head prosthesis leading to capitellar wear.
symptoms described earlier, radiographs of the elbow and wrist will
disclose most associated injuries. For isolated partial fractures of
the radial head, the ability of the patient to fully pronate and
supinate the forearm will influence treatment. Pain can make this very
difficult to evaluate during the first few days after injury. If the
radiographs reveal a fracture that may restrict forearm rotation and
operative treatment is being considered, it may be useful to aspirate
some of the blood from the elbow joint and instill some local
anesthetic (usually lidocaine). This can be done at the anatomic
soft-spot (roughly at the center of a triangle formed by the dorsal
point of the olecranon, the radial head, and the lateral epicondyle) on
the lateral side of the elbow. Alternatively, if the patient returns to
the office a few days to a week after injury, he or she is likely to
feel much better and be capable of demonstrating forearm rotation. A
true block to forearm rotation is uncommon, so either injection or
delayed serial examination or both are important steps in decision
making.
radial head typically reveals a more complex fracture than was apparent
on radiographs. While two-dimensional and three-dimensional computed
tomography scans will depict these aspects in greater detail and
thereby facilitate planning of the operation, it is not necessary to
obtain these studies provided that the surgeon is prepared for all
possible treatment options including repair with plates and/or screws
or excision of the fractured radial head with insertion of a metal
prosthesis if there is an associated forearm or elbow injury.
fractures of the radial head at a time when they were either excised or
treated nonoperatively. He distinguished nondisplaced fractures that
did well with nonoperative treatment (type 1), comminuted fractures of
the entire head of the radius (type 3) that were best treated by
excision, and displaced fractures involving part of the radial head
(type 2), which presented a treatment dilemma in that the majority of
the head was intact, but some of these fractures had poor results. His
classification did not include radial neck fractures, did not account
for associated injuries, and did not quantify displacement.
Mason’s classification to (i) include fractures of the radial neck,
(ii) provide a quantitative definition of displacement (a fragment
involving 30% or more of the articular surface that is displaced more
than 2 mm), and (iii) incorporate fracture-dislocations of the elbow as
suggested by Johnston54 as a Mason
type 4 fracture. The inclusion of radial neck fractures is not useful
because these fractures have different management issues and should be
considered separately. The inclusion of dislocations is also not useful
because fractures of the radial head are associated with a variety of
complex injury patterns and, regardless of which injury pattern is
present, it is still important to characterize the fracture of the
radial head. Finally, there are little data to support the quantitative
definition of displacement that is offered in this system.
directly reflects current treatment options: type 1 fractures are
minimally displaced fractures that do well with nonoperative treatment;
type 2 fractures are displaced partial head fractures that block
forearm rotation and fractures involving the entire head that are
repairable; and type 3 fractures are irreparable fractures that require
excision with or without prosthetic replacement.48
This classification is useful conceptually, but the means for
distinguishing repairable from unrepairable fractures are incompletely
defined.
mixes fractures of the proximal radius and ulna in a way that is not
useful for patient management; however, one useful aspect of this
system is a modifier that distinguished fractures with greater than
three fragments from those with two or three major fragments. The
presence of greater than three fragments has been associated with a
much higher risk of early failure of internal fixation, nonunion, and
loss of forearm rotation.120
treatment, but are not well accounted for in current classification
systems, include (i) lost fragments—a very common occurrence with
displaced fractures, (ii) fragments that are too small to be repaired
and must be discarded, (iii) fragments with little or no subchondral
bone, (iv) fragments with osteoporotic bone, (v) impaction and
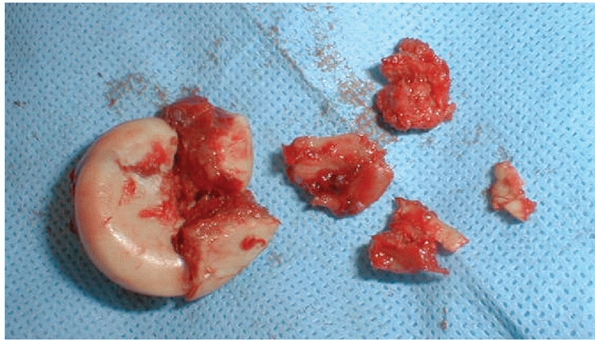
deformation of the fracture fragments, and (vi) metaphyseal bone loss (Fig. 32-8). Partial resection of the radial head has long been associated with inferior results11 and was one factor associated with problems in our study of operative treatment.106
Therefore, when fragments are lost, are too small to fix, or have
inadequate or poor quality bone and must be discarded, the surgeon
probably ought to err toward resection of the radial head with or
without prosthetic replacement depending on the presence or absence of
associated injuries. Impacted
fractures
may be less suitable for operative fixation because enlargement and
deformation of the radial head have been observed in long-term
follow-up and seem to hinder forearm rotation. Metaphyseal bone loss
and impaction are observed even with partial radial head fractures and
plate fixation may be superior to screws alone in this circumstance (Fig. 32-9).
 |
|
FIGURE 32-8 These fracture fragments demonstrate impaction and deformation of the head in the largest fragment (left), metaphyseal fragmentation and small unrepairable articular fragments (right).
|
head are treated nonoperatively. The major problem that patients
encounter after an isolated fracture of the radial head is elbow
stiffness. Only one study has noted fracture displacement with
immediate active motion,102 and it seems to be a very unusual problem. Nonunion occurs on occasion but is usually asymptomatic.14,104
 |
|
FIGURE 32-9 Substantially displaced partial head fractures (Mason 2) may benefit from plate fixation. A. This fracture is part of a posterior Monteggia injury. B. Fixation with screws was complicated by delayed union and settling of the fracture. The metaphyseal bone loss is evident.
|
The only absolute indication for internal fixation of an isolated
displaced Mason type 2 fracture is restriction of forearm rotation
because of the fracture fragment. In one recent study from Malmo,
Sweden, at least 74% of patients with a fracture involving greater than
30% of the head and displaced greater than 2 mm had good or excellent
results decades after the fracture using a very strict rating system.46
fracture-dislocations of the elbow. Two series have documented good
results in terms of stability, but this approach is associated with a
high rate of reoperation to address problems related to the fractured
radial head.6,56
Extreme caution is advised in the presence of an associated fracture of
the coronoid as these so-called terrible triad injuries can be very
unstable.56,117
replacement is still a very good treatment option in select
patients—usually older patients with complex isolated fractures, but
also for the occasional fracture-dislocation without a fracture of the
coronoid. The surgeon, however, should always be prepared to place a
prosthesis in case a careful intraoperative evaluation discloses
forearm instability or an associated coronoid fracture.
indication for operative treatment of a displaced partial radial head
fracture (Mason type 2) is a block to motion. A relative indication is
displacement of greater than 2 mm without a block to motion.
exposure is developed, taking care to protect the uninjured LCL
complex. The anterolateral aspect of the radial head is usually
involved and is readily exposed through these intervals. The fracture
is usually only slightly displaced. In fact, it is usually impacted
into a stable position. The periosteum is usually intact over the
metaphyseal fracture line. An attempt should be made to preserve this
inherent stability by using a bone tamp to reposition the fragment.
After the fragment has been realigned, one or two small screws are used
to secure it (Fig. 32-10).
Injury. The treatment of partial radial head fractures that are part of
a complex injury pattern must also consider the important role of the
radial head in elbow stability. Even a relatively small fracture can
make an important contribution to the stability of the elbow and
forearm. Partial head fragments that are part of a complex injury are
often displaced and unstable with little or no soft tissue attachments.
Occasionally some fragments are lost in the soft tissues.
candidates for open reduction and internal fixation (ORIF), widely
displaced fractures associated with complex injuries can be very
challenging to treat because of fragmentation, the small size of the
fragments, lost fragments, poor bone quality, limited subchondral bone
on the fracture fragments, and metaphyseal comminution and bone loss (Fig. 32-9).
achieved. Discarding the unrepairable fragments (partial radial head
resection) has been documented to have poor results in older series,11
but a recent report on the operative treatment of terrible triad
injuries reported partial head resection in several patients with no
apparent problems related to it.101
 |
|
FIGURE 32-10 The majority of isolated partial head fractures (Mason type 2) are impacted but not widely displaced. A. This fragment blocked forearm rotation. B. A bone tamp was used to realign the fragment and it was secured with two screws.
|
for a very unstable elbow or forearm injury, it may be preferable to
resect the remaining intact radial head and replace it with a metal
prosthesis, to enhance stability.
treating a fracture-dislocation of the forearm or elbow with an
associated fracture involving the entire head of the radius, ORIF
should only be considered a viable option if stable, reliable fixation
can be achieved. There is a risk of early failure that can contribute
to recurrent instability.120 Many
patients who develop a chronic Essex-Lopresti lesion (longitudinal
instability of the forearm) had failed internal fixation of a radial
head fracture. Other factors, such as loss offragments, metaphyseal
bone loss, impaction and deformity of fragments,17
and the size and quality of the fracture fragments, may make ORIF a
less predictable choice. In particular, if there are more than three
articular fragments, the rates of early failure, nonunion, and poor
forearm rotation may be unacceptable120 (Fig. 32-11).
articular fragments without impaction or deformity. Each should be of
sufficient size and bone quality to accept screw fixation, and there
should be little or no metaphyseal bone loss. Excellent exposure is
required, and the surgeon should not hesitate to release the origin of
the LCL complex to improve exposure in the unusual situation where it
is not injured (Fig. 32-12). In many cases, it
will prove useful to remove the fracture fragments from the wound and
reassemble them outside the body (on the “back table”). Sacrificing any
small residual capsular attachments to do this seems to be an
acceptable tradeoff to achieve the goal of stable, anatomic fixation.
The reconstructed radial head is then secured to the radial neck with a
plate. Consideration should be given to applying bone graft to
metaphyseal
defects—sufficient bone can often be obtained from the lateral epicondyle or proximal ulna.
 |
|
FIGURE 32-11
Early failure and nonunion are common after open reduction an internal fixation of fractures that involve the entire radial head (Mason type 3), particularly those fractures that create more than three articular fragments. A. This displaced fracture was part of a fracture-dislocation. B. Stable internal fixation was achieved initially. C. Six months later, the plate was broken and the radial neck remained unhealed. |
the past three decades of the twentieth century did not provide much
stability and often caused a destructive synovitis.10,36,130 Metal prostheses, which have been used for years in some centers,21,38,39,76
are now more widely available. Some prostheses have intentionally
smooth stems that lie somewhat loose in the radial neck, serving as a
spacer rather than a fixed prosthesis.21,38,39,76 Others are either press fit or cemented. Some designs have a mobile head.58
A radial head prosthesis that lies more than 1 mm proximal to the
lateral edge of the coronoid process (unpublished computed
tomography-based measurements from our research group) may hinge the
elbow open on the lateral side and lead to capitellar wear, arthrosis,
and synovitis (Fig. 32-13).
displaced partial head fractures nonoperatively, preferring to use no
more than a sling for comfort if possible, with immediate initiation of
active motion.
head fractures that are displaced more than 2 mm, and repairable
fractures associated with fracture-dislocations of the forearm and
elbow are treated with ORIF.
(leading to a tenuous repair) are excised. A metal prosthesis is
inserted when there is elbow or forearm instability, and in most young,
active patients (Table 32-1).
(Kocher exposure)63,81 (Fig. 32-6).
This interval is fairly easy to define intraoperatively. It represents
the most posterior interval and provides good access to fragments of
the radial head that displace posteriorly. It also provides greater
protection for the posterior interosseous nerve. On the other hand,
attention must be paid to protecting the LCL complex. The anconeus
should not be elevated posteriorly and the elbow capsule and annular
ligament should be incised diagonally, in line with the posterior
margin of the extensor carpi ulnaris.16
 |
|
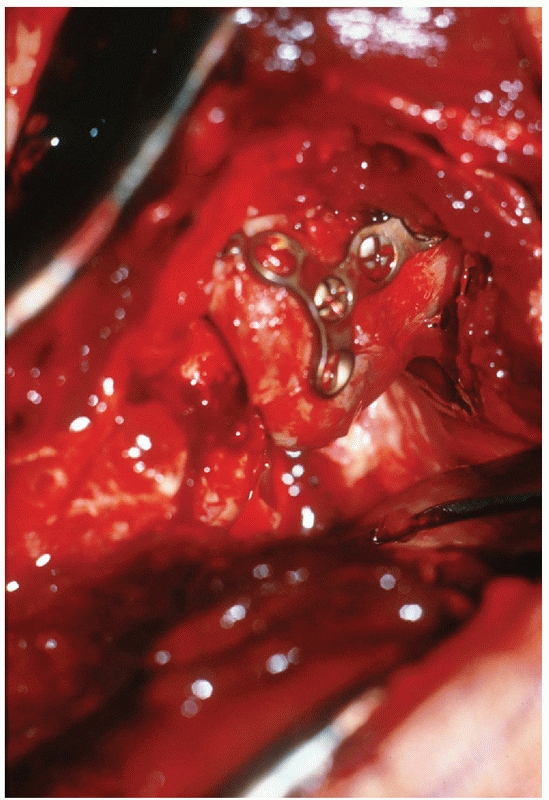
FIGURE 32-12
In this patient with lateral collateral ligament avulsion from the lateral epicondyle, excellent exposure of the radial head has been obtained to facilitate plate application. |
|
TABLE 32-1 Pitfalls and Pearls for Fractures of the Radial Head
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
FIGURE 32-13
The major pitfall with a metallic radial head prosthesis is implantation of a prosthesis that is too long. This radiograph shows gaping open on the lateral side of the ulnohumeral joint and a large cyst in the capitellum. |
recommends going directly through the extensor digitorum communis
muscle. I find these intervals difficult to define precisely based on
intraoperative observations. A useful technique for choosing a good
interval and protecting the LCL complex was described by Hotchkiss48:
starting at the supracondylar ridge of the distal humerus, if one
incises the origin of the extensor carpi radialis, elevates it, and
incises the underlying elbow capsule, it is then possible to see the
capitellum and radial head. The interval for more distal dissection
should be just anterior to a line bisecting the radial head in the
anteroposterior plane.
radial head that merit operative treatment are associated with
fracture-dislocations of the elbow. In this context, exposure is
greatly facilitated by the associated capsuloligamentous and muscle
injury.73,109,120 When the elbow has dislocated, the LCL has ruptured and the injury always occurs (or nearly always according to some authors73) as an avulsion from the lateral epicondyle. Along with a variable amount of muscle avulsion from the lateral epicondyle,27,55,57,73,112
these injuries leave a relatively bare epicondyle. There is often a
split in the common extensor muscle that can be developed more distally.
fracture-dislocation or posterior Monteggia fracture, the radial head
often displaces posteriorly through capsule and muscle. Accentuation of
the injury deformity usually brings the radial head up into the wound (Fig. 32-14).
In some cases, the surgeon will extend the posterior muscle injury to
mobilize the olecranon fracture proximally to expose and manipulate the
coronoid fracture through the elbow articulation. Slight additional
dissection between the radius and the ulna is acceptable given the
usually extensive injury in this region, but extensive new dissection
in this area has been implicated in an increased risk of proximal
radioulnar synostosis.2,131
the LCL complex intact (for instance, an Essex-Lopresti injury), it may
be difficult to gain adequate exposure without releasing the LCL
complex from the lateral epicondyle. This can be done either by
directly incising the origin of the LCL complex from bone or by
performing an osteotomy of the lateral epidcondyle.32,33,43,44,94 In either case, a secure repair and avoidance of varus stress in the early postoperative period are important.
 |
|
FIGURE 32-14
When treating a posterior olecranon fracture-dislocation or posterior Monteggia injury, the radial head can often be addressed through the posterior traumatic interval. |
the setting of an olecranon fracture-dislocation or posterior Monteggia
injury, it may be useful to seal the end of the radius with bone wax.
The LCL complex should be reattached to the lateral epicondyle if
avulsed.
paralleled the development of small screws (2.7, 2.0, and 1.5 mm) and
the techniques for using them.44 At
the same time, small, headless, variable pitch compression screws (such
as the Herbert screw) were developed, allowing for fixation of entirely
articular fragments.7,69,96
Standard screws can be used in this way as well, countersinking the
head below the articular surface, although they are prone to backing
out into the joint with the slightest amount of settling at the
fracture site.
Kirschner wires. Threaded wires are usually used because of the
tendency for smooth wires to migrate and travel to various parts of the
body.65 Absorbable pins and screws are being developed for similar uses47,97 but are still somewhat brittle and sometimes associated with an inflammatory response.
the entire head. Plate types include T- and L-shaped plates with
standard screws, small (condylar) blade plates, and new plates designed
specifically for the radial head (many of which incorporate angular
stable screws—screws that thread directly into the plate). The use of
plates that are placed within the radial head or countersunk into the
articular surface has also been described.32
the radial head is still attached to the neck, it is separated at the
point on the radial neck where the flare of the head begins. I prefer
to use a prosthesis with a smooth stem that serves as a loose spacer.21,38
The laxity in the neck facilitates insertion and removal of the
prosthesis and accommodates some of the nonanatomic features of the
prosthesis compared to the native radial head. I use a neck diameter
one size less than the reamer that can be passed with slight effort. I
use a head size slightly smaller in diameter than the native head. I
almost never add more length through the head. It is important to
realize that the prosthesis will sit on the most prominent portion of
the radial neck; therefore, one should be careful to choose a head
thickness based
upon
the thinnest portion of the radial head. I smooth off but do not evenly
plane the remaining radial neck. It is important to check the level of
the radial head with respect to the lateral edge of the coronoid
process—it should be no more than 1 mm more proximal.
into the neck, a prosthetic head of greater thickness can be used. In
cases of extreme neck comminution, the prosthesis can be cemented in
the neck.
interosseous nerve during ORIF of a radial head fracture is unusual.
Most commonly, this complication is experienced as a palsy related to
retraction or exposure that resolves over weeks to months. To limit the
potential for this complication, retractors should not be placed around
the radial neck, the forearm should be pronated during exposure of the
radial neck, and consideration should be given to identifying and
protecting the nerve when more distal dissection and internal fixation
are needed, particularly when a more anterior muscle interval is used
for exposure.
infrequent, particularly after ORIF of complex fractures involving the
entire head. In a recent series, 3 of 14 fractures involving the entire
radial head and creating greater than three articular fragments had
failure of fixation within the first month.120
Because this situation can contribute to instability of the forearm or
elbow, unstable or unpredictable fixation is undesirable and such
fractures should probably be treated with prosthetic replacement. Among
fractures of the entire radial head, 6 of 11 fractures in one series43 and 8 of 26 fractures in another series120
(including 2 of 12 fractures with three or fewer fragments and 6 of 14
fractures with greater than three articular fragments) had nonunion.
performed to improved forearm rotation, and not for painful arthrosis
of the radiocapitellar joint.5,35
Incongruity of the proximal radioulnar joint presents as stiffness
rather than pain or arthrosis and incongruity of the radiocapitellar
joint inconsistently and unpredictably leads to radiocapitellar
arthrosis, which seems to be an uncommon problem.
malalignment of the elbow, capitellar wear, and synovitis and usually
needs to be removed. Removal of a metal radial head prosthesis can be
very difficult. Given the alternative of releasing the origin of the
LCL complex to subluxate the elbow, in most patients, I prefer to
excise a portion of the radial neck so that I can pry out the
prosthesis. The difficulty encountered in removing these prostheses is
one reason I prefer to use one with a slightly loose-fitting stem.
with screws that lock to the plate. Prostheses also continue to evolve.
It remains unclear how appropriately sized prostheses will function
over the long term. If they continue to perform as well as they have in
published studies, surgeons will likely gradually become more confident
with prosthetic replacement and less accepting of tenuous internal
fixation.
posterolateral rotatory instability (elbow dislocations with or without
associated fractures), varus posteromedial rotational instability
(anteromedial coronoid facet fractures), and olecranon
fracture-dislocations. Identification of the specific pattern of
traumatic elbow instability will indicate which structures are likely
to be injured, the morphology of the injuries, and the prognosis, all
of which will help to guide management.
dislocation of the elbow with or without fractures of the radial head
and coronoid. Posterolateral rotatory injuries occur during a fall on
to the outstretched arm that create a valgus, axial, and posterolateral
rotatory force. The ulna and the forearm supinate away from the humerus
and dislocate posteriorly. Sometimes this results in injury to the
radial head or coronoid. The soft tissue injury proceeds from lateral
to medial, with the anterior band of the MCL being the last structure
injured91 (Fig. 32-3). It is possible to dislocate the elbow with the anterior band of the MCL remaining intact.
a fall onto the outstretched arm that creates a varus stress, axial
load, and posteromedial rotational force to the elbow.90
This results in fracture of the anteromedial facet of the coronoid
process and either (i) injury to the LCL, (ii) fracture of the
olecranon, or (iii) an additional fracture of the coronoid at its base.20,22,105
When the fracture of the anteromedial facet is very small (more or less
a capsular avulsion) and the elbow completely dislocates, this may
represent an alternative mechanism for elbow dislocation in contrast to
the posterolateral rotatory mechanism. I suspect that dislocations that
occur via a varus, posteromedial rotational mechanism may be less
stable and more likely to require operative treatment.25
of a direct blow to the flexed elbow, but the mechanism of posterior
olecranon fracture-dislocations is more speculative with some authors
suggesting they may result from the same mechanism that usually creates
elbow dislocations, particularly in older osteopenic individuals.95,98
instability, the problem is evident. In some patients the dislocation
has reduced, either spontaneously or with assistance. Pain, ecchymosis,
and swelling are present along with deformity if the elbow is still
dislocated. The point of the olecranon process and the medial and
lateral epicondyles should form a triangle in the coronal plane with
the elbow flexed 90 degrees. If the point of the olecranon is well
posterior to the epicondyles, the elbow is likely dislocated.
and median nerves are most commonly involved. The brachial artery may
also be injured, particularly with an open dislocation, which is also
unusual.
intended to restore the inherent bony stability of the elbow that
allows treatment of the most simple elbow dislocations with immediate
active motion with a high degree of success. Critical to achieving this
is restoration of the trochlear notch of the ulna, particularly the
coronoid process. Anatomic alignment of anteromedial and basal coronoid
fractures is necessary for elbow stability and function.
Radiocapitellar contact is also very important to the stability of the
injured elbow. The LCL is far more important than the MCL in the
setting of most cases of traumatic elbow instability. The trochlear
notch (coronoid and olecranon), radial head, and LCL are repaired or
reconstructed, but the MCL rarely needs to be repaired. Some surgeons
are still becoming comfortable with the idea that MCL repair is not
necessary for most fracture-dislocations.118
If the elbow is stable, or can be made stable with surgery on the
lateral side, the MCL will heal properly with active motion and its
repair is not necessary to achieve stability.101
fracture-dislocations result in injury to all of the capsuloligamentous
stabilizers of the elbow joint.27,56,57,91
The exceptions include fracture-dislocations of the olecranon and other
injuries with fractures of the coronoid involving nearly the entire
coronoid process.90,109,115,116
medial and the elbow can completely dislocate with the anterior band of
the MCL remaining intact.91 There is also a variable degree of injury to the common flexor and extensor musculature.27,55,57,71
avulsion from the lateral epicondyle in over 75% of patients with elbow
dislocations.73 In my personal
observations treating over 60 fracture-dislocations of the elbow, I
have found that the LCL is always avulsed from the lateral epicondyle.
In many patients, there are small pieces of the ligament or other long
strands of musculotendinous tissue, which may lead the surgeon to
misinterpret the situation (Fig. 32-15). Defined practically, reattachment of the soft tissue sleeve to the lateral epicondyle is nearly always sufficient.
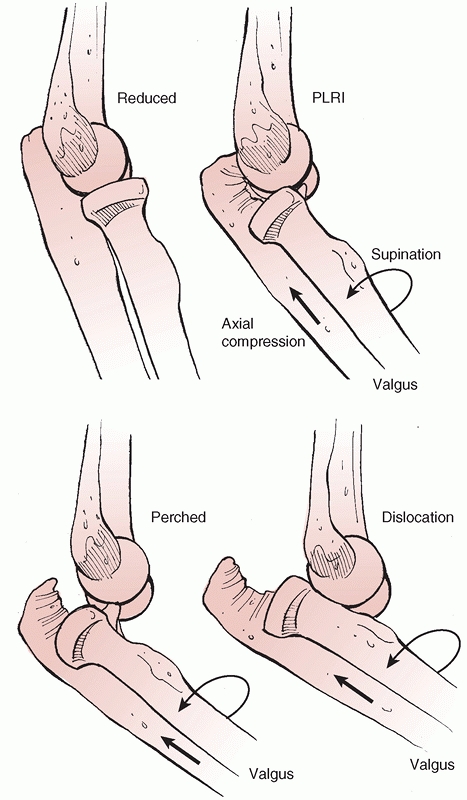
Stage 1 involves partial or complete disruption of the LCL, which may
result in slight posterior subluxation of the radial head with respect
to the capitellum. Stage 2 involves an incomplete posterior dislocation
with disruption of the lateral ligamentous complex and further injury
to the osseous or ligamentous supporting structures anteriorly and/or
posteriorly. The medial edge of the ulna may be found to rest on the
trochlea. This gives the appearance of the
coronoid being perched on the trochlea on a lateral radiograph.91
Stage 3 is divided into three subgroups (A, B, and C). Stage 3A
involves injury to all the soft tissue support except the anterior band
of the MCL. The elbow dislocates in a posterolateral direction,
rotating about the intact anterior MCL. Stage 3B involves injury to the
entire medial ligamentous complex, resulting in varus, valgus, and
rotary instability. Stage 3C injuries are very unstable because of
complete soft tissue disruption from the distal humerus, with the elbow
having the ability to dislocate even when immobilized in a cast.90
 |
|
FIGURE 32-15
The lateral collateral ligament nearly always fails via avulsion of its lateral epicondylar origin. The remaining tissue attached to the epicondyle is the remnant of the common extensor musculature, much of which has been torn more distally. |
 |
|
FIGURE 32-16 Posterolateral rotatory instability (PLRI) occurs in several stages. Elbow dislocation is the final stage.
|
intra-articular fractures are at greater risk for recurrent or chronic
instability.41,56,109
Fracture-dislocations of the elbow usually occur in one of several
distinct, recognizable injury patterns: (i) posterior dislocation with
fracture of the radial head, (ii) posterior dislocation with fractures
of the radial head and coronoid process—the so-called terrible triad
injury (Fig. 32-17), (iii) varus posteromedial rotational instability pattern injuries (Fig. 32-18), (iv) anterior olecranon fracture-dislocations (Fig. 32-19), and (v) posterior olecranon fracture-dislocations (Fig. 32-20).
Each of these patterns is associated with characteristic injury
components and fracture morphologies, the knowledge of which can help
guide effective management.
injuries and olecranon fracture-dislocations are not true dislocations
in that apposition of the articular surfaces is not lost (Figs. 32-18, 32-19 and 32-20). Rather, they are usually fracture-subluxation injuries where the major problem is disruption of the trochlear notch.
 |
|
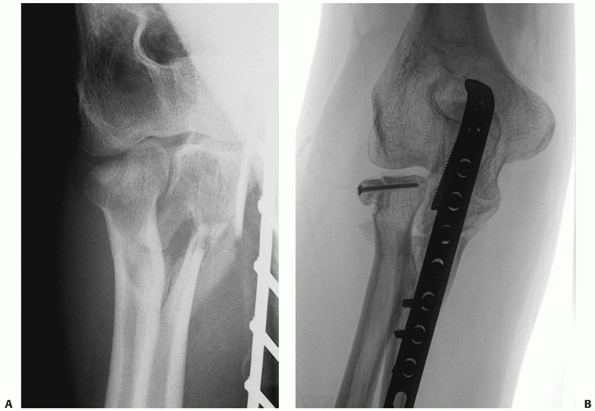
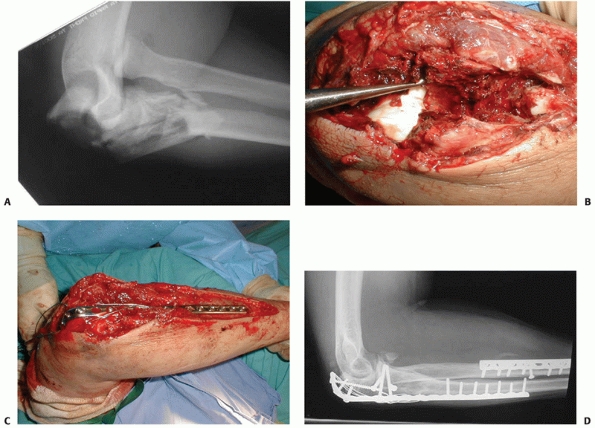
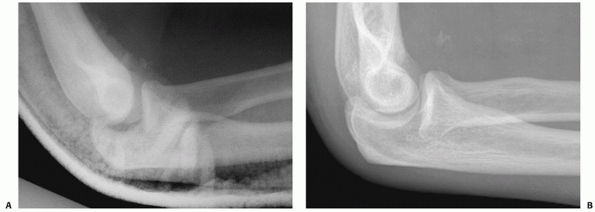
FIGURE 32-17 The so-called terrible triad of the elbow consists of dislocation of the elbow with fractures of the coronoid and radial head. A.
The coronoid fragment is the triangular fragment anterior to the trochlea. After manipulative reduction, this elbow could not be kept reduced despite cast immobilization. B. The coronoid fracture is a transverse fracture of the tip as seen on this three-dimensional computed tomography reconstruction. C. Operative fixation of the coronoid, replacement of the radial head, and reattachment of the lateral collateral ligament complex to the lateral epicondyle restored good elbow function. |
The injuries that give surgeons the most trouble are the terrible
triad, varus posteromedial, and olecranon fracture-dislocations with
associated coronoid fractures.90 In each case, the fracture of the coronoid is the most important and challenging part of the injury.
classified coronoid fractures based on the size of the fragment: type
I, avulsion of the tip of the coronoid process; type II, a single or
comminuted fragment involving 50% of the process or less; and type III,
a single or comminuted fragment involving more than 50% of the process.103
They also included a modifier to indicate the presence (type B) or
absence (type A) of an elbow dislocation. However, it has become clear
that the pattern of the overall injury and morphology of the fracture
may be equally or more important than the size of the fragment and the
presence or absence of dislocation.
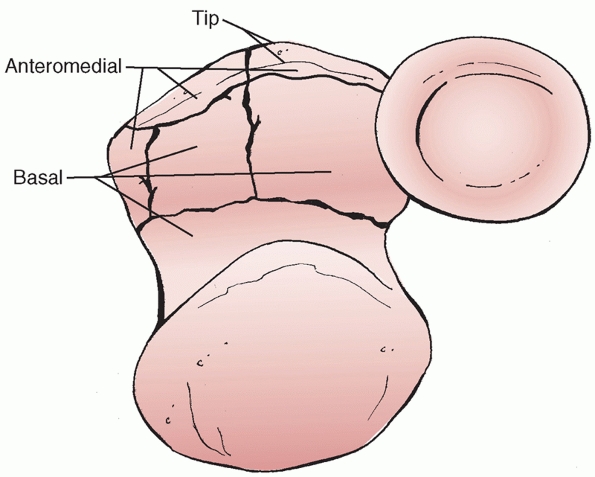
a new classification system for coronoid fractures based on the
anatomic location of the fracture. Fractures may involve the tip, the
anteromedial facet, or the basal aspect of the coronoid. The three
groups are further divided into subtypes based on the severity of
coronoid involvement.
His
system considers the mechanism of injury along with the associated
fractures and soft tissue injuries and helps to dictate treatment (Fig. 32-21).
 |
|
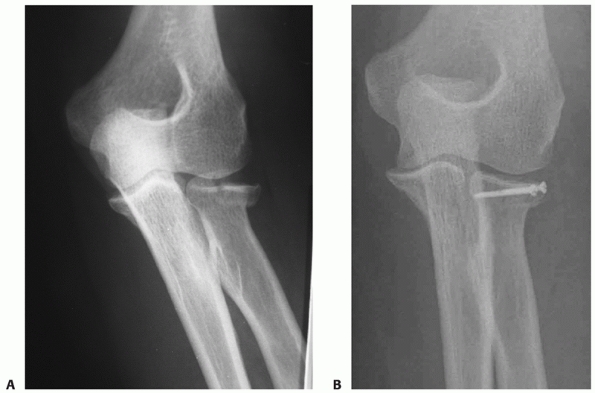
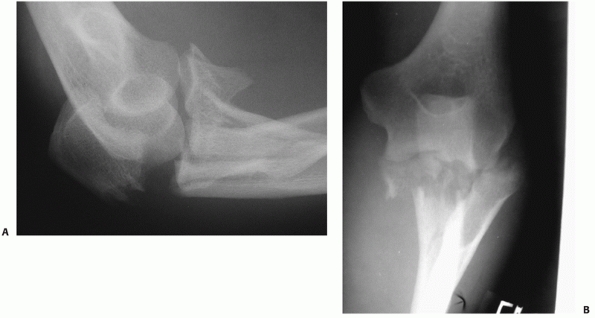
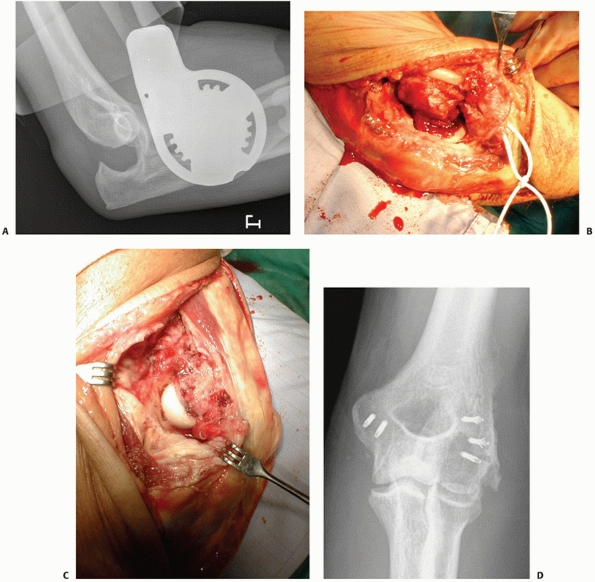
FIGURE 32-18 Small coronoid fractures are often problematic. A. This appears to be a small isolated fracture of the coronoid. B.
On the anteroposterior view, it is clear that the anteromedial facet of the coronoid process is fractured. There is varus subluxation and opening of the joint on the lateral side betraying the associated lateral collateral ligament injury. C. Three-dimensional computed tomography depicts external rotation of the distal humerus with respect to the forearm as the trochlea rotates forward into the coronoid defect. D. There are separate coronoid tip and anteromedial facet fracture fragments. (continues) |
 |
|
FIGURE 32-18 (Continued) E.
Exposure is obtained by transposing the ulnar nerve anteriorly and elevating the anterior portion of the flexor-pronator muscles off of the medial collateral ligament and the coronoid process. F. The coronoid fractures were secured with a buttress plate and the lateral collateral ligament origin was reattached to the lateral epicondyle with a suture anchor. G. A concentric reduction and good elbow function resulted. |
but does not extend medially past the sublime tubercle or into the
body. Tip, subtype 1 fractures involve less than 2 mm of the coronoid
and may be found in isolation or with a fracture-dislocation. Tip,
subtype 2 fractures involve greater than 2 mm and are largely
associated with terrible triad injuries. In my experience, all of these
fracture fragments contain the insertion of the anterior capsule and
the 2-mm distinction between subtypes 1 and 2 is arbitrary and does not
influence treatment.
anteromedial aspect of the coronoid. Anteromedial subtype 1 fractures
extend from just medial to the tip of the coronoid to the anterior half
of the sublime tubercle (the insertion of the anterior band of the
MCL). Anteromedial subtype 2 fractures are subtype 1 injuries with
extension of the fracture line into the tip. Anteromedial subtype 3
fractures involve the anteromedial rim and the entire sublime tubercle
with or without involvement of the tip of the coronoid. The mechanism
of injury is usually a varus/posteromedial rotation injury with axial
loading. The LCL complex is generally disrupted unless the olecranon is
also fractured. Radial head fractures may be seen in higher-energy,
subtype 3 injuries. Anteromedial coronoid fractures cause incongruent
articulation of the ulnohumeral joint, which may lead to an earlier
onset of posttraumatic arthritis.
involve at least 50% of the height of the coronoid. Basal subtype 1
fractures involve the coronoid alone, while subtype 2 fractures are
associated with fractures of the olecranon. In general, these fractures
have less soft tissue disruption than those that involve only the tip
of the coronoid.
treatment: (i) Terrible triad injuries nearly always have a small
transverse fracture of the tip of the coronoid including the anterior
capsular attachment (Fig. 32-17B). Much less
commonly, the coronoid fracture is either very large or involves the
anteromedial facet of the coronoid preferentially. (ii) Varus
posteromedial rotational instability pattern injuries are defined by a
fracture of the anteromedial facet of the coronoid process (Fig. 32-18).
(iii) In the setting of an olecranon fracture-dislocation, the coronoid
fracture can be one simple large fragment; it can be fragmented into
two or three large pieces (anteromedial facet, central, and lesser
sigmoid notch) with or without a tip fragment as well, or it can be
more comminuted.
Substantial subluxation or redislocation of the elbow is challenging to
treat and the elbow can be unstable despite cast immobilization.
Therefore, it is very important not to leave the operating room until
adequate stability has been achieved. Morrey78
recommended that the elbow should not redislocate before reaching 45
degrees of flexion from a fully flexed position, and Jupiter109
and I recommended that the elbow should be able to go to 30 degrees
before substantial subluxation or dislocation occurs. These are
relatively arbitrary numbers.
 |
|
FIGURE 32-19
Anterior (or trans olecranon) olecranon fracture-dislocations are relatively uncommon injuries that are characterized by anterior translation of the forearm, an intact radial head, and fracture of the proximal ulna. A. This very complex proximal ulna fracture involves the coronoid process. B. The coronoid is split in the sagittal plane and can be repaired with interfragmentary compression screws. C. The metaphyseal and diaphyseal fragmentation is bridged with a long plate, contoured to wrap around the dorsal surface of the ulna. Tension wires are used to enhance fixation of the small proximal fragments. D. Six months later, the fracture is healed and good elbow function has been restored. |
 |
|
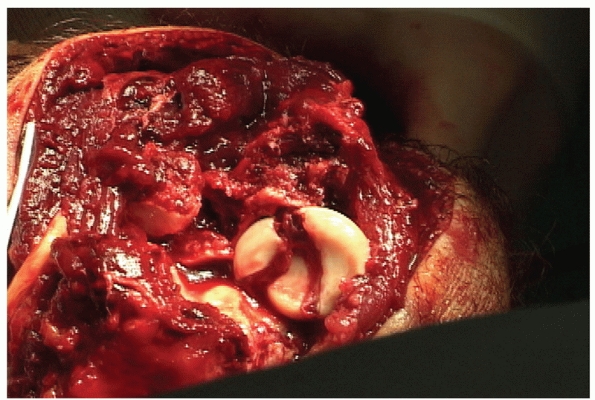
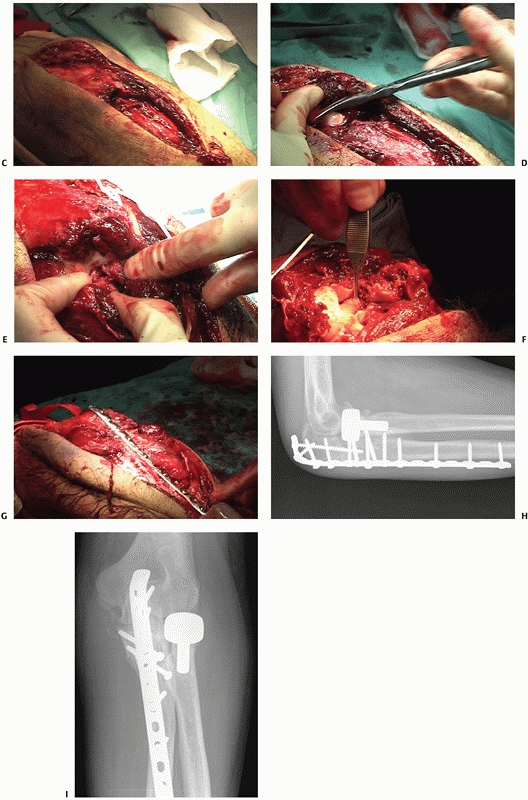
FIGURE 32-20 Posterior olecranon fracture-dislocations can be very complex injuries. A. In this patient, the coronoid and radial head are fractured. B. The coronoid is split into three fragments. (continues)
|
 |
|
FIGURE 32-20 (Continued) C. A posterior skin incision discloses muscle injury. D.
If the muscle injury is opened up and extended somewhat, the olecranon fragment can be translated proximally like an olecranon osteotomy, exposing the elbow articulation. E. An additional medial exposure with transposition of the ulnar nerve helps with manipulation of the anteromedial fracture fragment. F. The coronoid is split into three large fragments: anteromedial, central, and lesser sigmoid notch. G. A long dorsal plate is applied, bridging the comminution and securing the coronoid. H. The radial head is replaced. I. The anteromedial portion of the coronoid is secured with screws. Healing occured and good elbow function was restored. |
 |
|
FIGURE 32-21
O’Driscoll has described the common fracture fragments seen with coronoid fractures. The tip fragment is seen most often with varus posteromedial injuries and terrible triad injuries, but can also be seen in comminuted basal injuries. The anteromedial facet fracture is seen in varus posteromedial rotatory instability as well as with posterior olecranon fracture-dislocations. Basal fractures are usually associated with olecranon fracture-dislocations. |
In other words, I support the upper arm or humerus, straighten the
elbow, and let gravity apply a stress to the extended elbow. I then
gently flex the elbow and feel for any clunk or crepitation. I repeat
the maneuver under image intensification. In most cases, the elbow is
stable with this maneuver and no more than slight subluxation is seen
radiographically. If greater subluxation occurs, I consider additional
treatment such as the use of hinged external fixation.
 |
|
FIGURE 32-22
A useful method for intraoperative testing of elbow stability is to place the arm in gravity extension with the forearm in neutral. After this maneuver is performed, the elbow is gently flexed and palpated for recurrence of any subluxation or dislocation. It is also useful to monitor this maneuver on an image intensifier. |
manipulative reduction. Acute redislocations and chronic recurrent
dislocations are uncommon.25 Mobilization of the elbow within 2 weeks results in less stiffness and pain.74,100
Simple elbow dislocations that redislocate after manipulative reduction
seem to be related to a greater degree of soft tissue avulsion from the
distal humerus and are typically observed in frail older patients and
younger patients with very high-energy dislocations.25,71
reduction will help to ensure there are no associated fractures. Even
very small fractures of the coronoid and radial head can be important
and potentially problematic.117 These can be better characterized with two- and three-dimensional computed tomography scans.
fractures are exceedingly uncommon. Medial and lateral dislocations are
likely to be incompletely reduced posterior dislocations. Consequently,
classification of simple elbow dislocations into anterior, medial,
lateral, and posterior is not very useful.
posterolateral position may be more likely than a posteromedial
dislocation to have torn the anterior band of the MCL.87,91
conscious sedation. The basic technique for manipulative reduction is
to line up the olecranon and the distal humerus in the mediallateral
plane, apply traction across the elbow with the elbow flexed at 90
degrees, and lever the olecranon over the distal humerus with direct
pressure. It can sometimes be helpful to supinate the forearm.
Reduction is usually easy, but it can take some force if the anterior
band of the MCL is intact. Successful reduction can be confirmed by
checking for a smooth, unrestricted arc of elbow motion and realignment
of the relationship between the point of the olecranon and the medial
and lateral epicondyles in the same plane.
patient move the elbow through as complete an arc of motion as pain
will allow. In the unusual elbow that redislocates with this maneuver,
some authors have suggested attempting range of motion with the forearm
pronated and, if successful, applying a cast brace that allows elbow
motion with the forearm held in this position. It is interesting to
check varus and valgus stability to note that in some patients valgus
stability is preserved, but this examination does not usually alter
treatment.
of flexion and the forearm in neutral rotation is applied for comfort
and discarded within 2 weeks of injury. Active elbow motion is
encouraged as soon as the patient can tolerate it. Specific exercises
to regain terminal elbow extension and flexion are often helpful and
can be taught by the physician or a therapist.
alternative is to forego the brace or cast and encourage confident active motion of the elbow.26
Patients with persistent subluxation of the elbow resemble patients
with so-called pseudosubluxation of the shoulder from pain-related
inhibition of the shoulder muscles. Active elbow mobilization provides
additional dynamic muscular contribution to elbow stability. This
should only be attempted in patients with slight subluxation or opening
of the joint and not in patients with “perched” dislocations in which
the trochlea is resting on and scraping against the coronoid process (Fig. 32-23).
 |
|
FIGURE 32-23
Residual subluxation of the elbow after a simple elbow dislocation can be effectively treated with active elbow exercises in most patients. A. This is attempted when the subluxation is more of a pseudosubluxation, as seen here, and not when the trochlea is perched on the coronoid. B. A radiograph taken after confident active mobilization of the elbow shows a concentric reduction. |
reduced position, redislocates before a postreduction radiograph is
obtained, or dislocates later on despite splint immobilization the
dislocation is deemed unstable and operative treatment is required.
There are three general approaches to this problem: (i) open relocation
and repair of soft tissues back to the distal humerus (Fig. 32-24), (ii) hinged external fixation and (iii) cross-pinning of the joint.
splint if possible and start immediate active mobilization of the
elbow. I do not immobilize the elbow longer than 1 week. Slight
subluxations nearly always recover with confident elbow exercises, and
I have used this technique following reduction as late as 6 weeks after
a simple elbow dislocation (Table 32-2).
unstable elbow dislocations benefit from cast immobilization.
Persistent subluxation may be exacerbated by additional weight on a
relaxed elbow and the elbow also becomes very stiff. Unstable elbows
can dislocate despite cast or brace immobilization and the patient may
not be aware of it.117
the elbow after manipulative reduction and active elbow exercises
requires operative treatment. In older patients, it is often sufficient
to repair the lateral soft tissues back to the lateral epicondyle. In
younger patients with high-energy injuries, I have found that repair of
both the medial and lateral soft tissue structures back to the distal
humerus may not completely stabilize the elbow, and stability may be
enhanced by reattachment of the anterior capsule to the coronoid
process. I try to limit operative dissection using either cross-pinning
alone or LCL repair combined with hinged external fixation. I have
performed hinged external fixation without ligament repair and found it
did not provide adequate stability to initiate elbow motion. In older,
infirm patients, cross-pinning of the ulnohumeral joint is adequate and
can be accomplished with sedation and local anesthesia. The pins are
protected in an above elbow cast and removed 3 weeks after surgery.
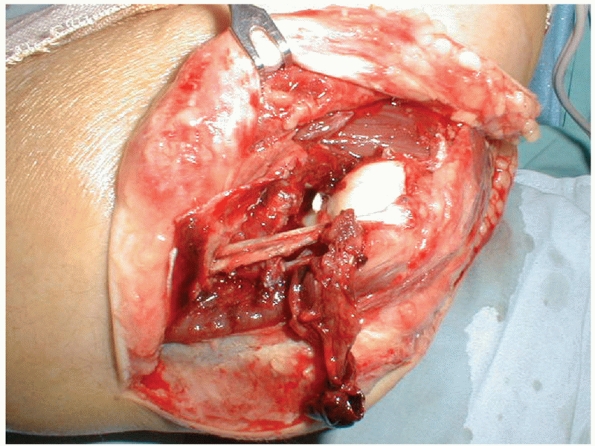
skin flap elevated. The extent of the soft tissue injury may not be
apparent until the overlying fascia is incised. The avulsed LCL origin
and common extensor musculature are reattached to the lateral
epicondyle with suture anchors or sutures passed through drill holes in
bone. I place one anchor or drill hole at the origin of the LCL and one
more proximally if necessary for repair of the avulsed or detached
radial wrist extensor muscle origins (Fig. 32-25).
This lateral soft tissue repair is often sufficient in older patients,
but a medial sided repair will be necessary in most young patients with
high-energy injuries (Fig. 32-24).
medial flap is elevated and the ulnar nerve is released from where it
passes through the medial intermuscular septum proximally through
Osbourne’s fascia distally and transposed into the subcutaneous tissues
anteriorly. The anterior capsule is reattached to the coronoid using
sutures passed through drill holes in the coronoid (entering from the
dorsal surface of the ulna) and the MCL and common
flexor
origins are then repaired back to the medial epicondyle using suture
anchors or sutures passed through drill holes in bone. If the elbow
dislocates in gravity extension, hinged external fixation or
cross-pinning of the elbow should be considered. If stability is
restored with soft tissue repair alone, the elbow can be mobilized
within a few days of surgery, but I usually splint the elbow until
suture removal about 10 days later and then initiate active elbow
exercises.
 |
|
FIGURE 32-24 A 35-year-old man who fell from four stories had an unstable simple elbow dislocation. A. Despite a hinged brace, the trochlea is perched on the coronoid process. B. The medial collateral ligament and common flexor muscles were avulsed from the medial epicondyle. C. The lateral collateral ligament and common extensor muscles were stripped off of the lateral epicondyle. D. Anteroposterior radiograph after reattachment of the soft tissues to the epicondyles shows concentric reduction.
|
Steinmann pins and a hinged external fixator is applied. There are
several varieties of hinged external fixators including unilateral
(lateral) fixators, fixators with transfixation pins, and fixators
based on an Ilizarov-type frame—the specific instructions for
application should be followed (Fig. 32-26).
surgery. Some fixators include a mechanism for applying a static
progressive stretch to the elbow, and this can be instituted
immediately. The fixator is removed 4 weeks after surgery and the
exercises are continued.
Kirschner wires are drilled across the ulnohumeral joint. Usually one
axially directed wire and one obliquely directed wire (starting lateral
to avoid the ulnar nerve) are adequate (Fig. 32-27).
The wires are aimed somewhat posteriorly to account for the anterior
translation of the trochlea with respect to the humeral shaft. The
adequacy of the reduction is confirmed radiographically, the wires are
trimmed and bent above the skin and a wellpadded cast is applied. The
cast and pins are removed 3 or 4 weeks later and active exercises are
initiated. Some surgeons who use cross-pinning prefer to use screws
because they are worried about breakage of the pins, but I have not
found this desirable or necessary.
|
TABLE 32-2 Pitfalls and Pearls for Simple Elbow Dislocations
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
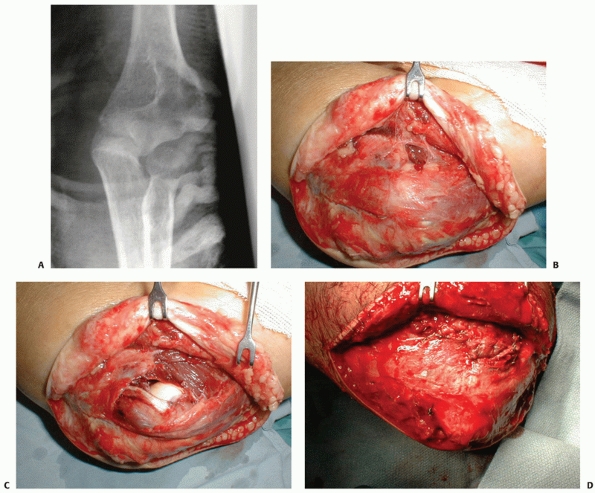 |
|
FIGURE 32-25 A 65-year-old woman had an unstable simple elbow dislocation. A. The elbow seems to be hinging open on some intact medial soft tissues. B. After elevating a lateral skin flap, there is very little damage evident. C.
After incision of the overlying fascia, the injury to the lateral collateral ligament and common extensors is apparent. The remaining tissue on the lateral epicondyle is tendon and not ligament. D. Repair of the lateral sided soft tissue injury restored stability. |
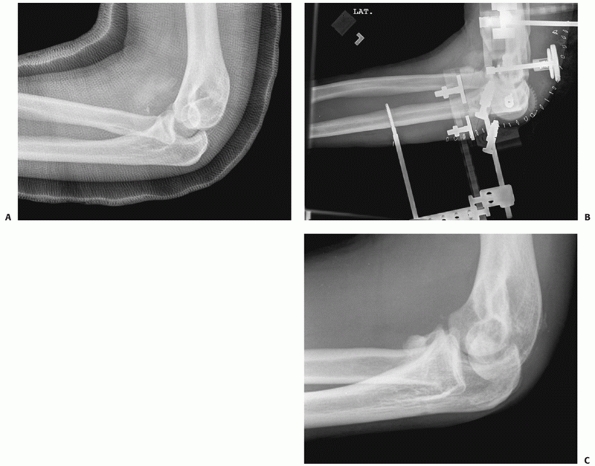 |
|
FIGURE 32-26 A 30-year-old man injured in a fall from a height had an unstable simple elbow dislocation. A. The trochlea remains perched on the coronoid process despite cast immobilization. B.
An open reduction, reattachment of the lateral collateral ligament to the lateral epicondyle and application of hinged external fixation were performed. C. A second procedure to remove anterior heterotopic bone was performed and a stable elbow with near normal elbow motion was obtained. |
is very uncommon after elbow dislocation. Persistent subluxation and
dislocation can destroy the ulnohumeral articulation if not promptly
identified and treated as the joint surfaces scrape against one
another. Slight subluxation with relative congruence of the articular
surfaces can be treated with active exercises as described earlier.
Wide dislocation is actually preferred over subluxation with abnormal
contact of the articular surfaces, because the articular surfaces are
less likely to be damaged. We have had success treating a chronic
simple elbow dislocation with relocation and 6 weeks of hinged external
fixation without ligament repair or reconstruction, likely because the
articular surfaces have been relatively well preserved.61
posterior dislocation of the elbow with fracture of the radial head.
This injury is identical to a simple elbow dislocation with the
addition of a fracture of the radial head as it collides with the
capitellum during dislocation.
as a result of fracture of the radial head creates an additional
measure of instability, but this injury pattern is not as problematic
as when the coronoid process is fractured as well. Broberg and Morrey6 and Josefson and colleagues56 documented good results
treating these injuries with or without radial head resection and 1
month of cast immobilization with two caveats: (i) patients with
associated coronoid fractures redislocated in the cast and (ii)
patients treated nonoperatively often needed secondary procedures to
address restriction of forearm rotation because of the fracture of the
radial head. While the radial head may not be necessary to keep the
elbow concentrically reduced in this injury pattern, some authors have
suggested that preservation of the stabilizing influence of
radiocapitellar contact may delay the onset of ulnohumeral arthrosis.121
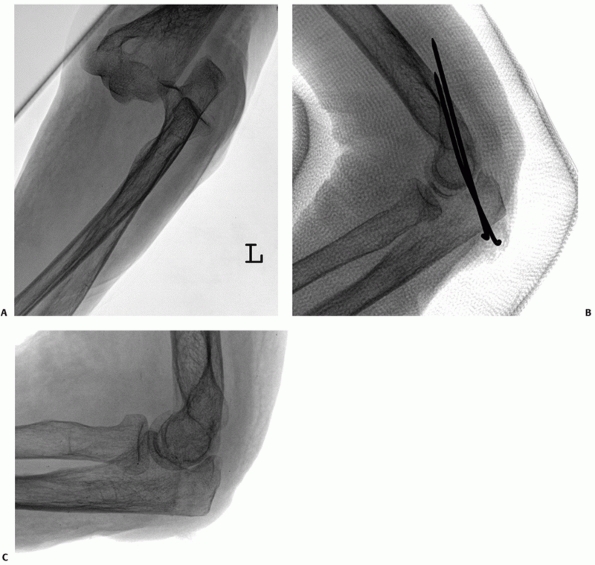 |
|
FIGURE 32-27 An 80-year-old woman had an unstable simple elbow dislocation after a fall. A. The radiograph of the initial injury. B.
The elbow was stabilized with two smooth Kirschner wires under sedation and local anesthesia and a long arm cast was applied. The pins and cast were removed 4 weeks later. C. A stable concentric reduction with near normal motion was obtained. |
operative treatment. Whereas avoidance of operative treatment might be
unwise when the elbow dislocation is associated with both coronoid and
radial head fractures, it is a reasonable treatment option in patients
with dislocation and fracture of the radial head only. A computed
tomography scan may be necessary to be certain that the coronoid is not
fractured. Patients who elect nonoperative treatment need to be aware
of the slight potential for instability and the substantial potential
for restriction of motion or arthrosis from the radial head fracture.
The literature documents the results after one month of cast
immobilization,6,56
but under close supervision, it is reasonable to remove the splint and
begin active motion at the patient’s first visit to the office,
typically about 1 week after injury.
Replacement and Lateral Collateral Ligament Repair. When the fracture
of the radial head cannot be repaired with confidence,
it
is reasonable to resect it (without prosthetic replacement). Good
results with this treatment have been reported, provided that there is
no coronoid fracture.6,56
The experience reported in the literature does not include collateral
ligament repair. We now understand the importance of the LCL to elbow
stability, and it is helpful to reattach this ligament to the lateral
epicondyle.101
native anatomy and contributes to the immediate and long-term stability
of the elbow. The injured LCL facilitates exposure of the radial head.
replacement with a metal prosthesis will enhance immediate and
long-term stability but also expose the patient to its potential
complications.
usually possible (particularly if radiocapitellar contact has also been
restored), but up to 10 days of immobilization is reasonable.101
treated a few very motivated and informed patients nonoperatively and
have been delightfully surprised with the results (Fig. 32-28).
Most patients will benefit from treatment of the radial head fracture.
I repair the radial head only when all the fragments are present, the
bone quality is adequate, and secure fixation can be accomplished.
Otherwise, I resect the radial head and replace it with a metal
prosthesis. I have treated a few lower-demand patients who did not want
a prosthesis (again, well informed and motivated) with resection and
LCL repair alone, also with good results. Operative treatment of the
radial head fracture and collateral ligament injury are described
earlier.
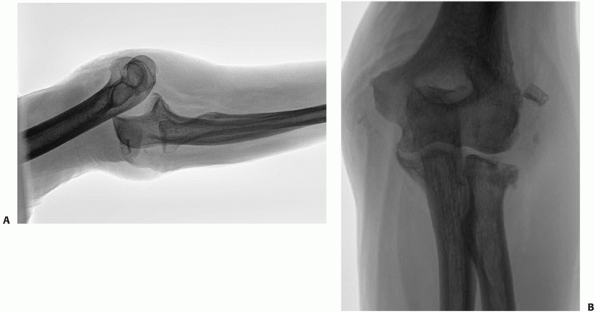 |
|
FIGURE 32-28 A fracture-dislocation of the elbow without a coronoid fracture can be treated nonoperatively in some patients. A. A 55-year-old patient with an elbow dislocation and radial head fracture had manipulative reduction and splinting. B.
Despite a complex fracture of the radial head, the patient declined operative treatment. Concentric reduction was maintained and his eventual functional result was excellent. |
instability are very uncommon with this injury pattern. Untreated or
inadequately treated fractures of the radial head can contribute to
loss of forearm motion and arthrosis and are treated with a second
operation to excise the radial head. An oversized radial head
prosthesis can cause painful radiocapitellar wear and arthrosis.
delays the progression of ulnohumeral arthrosis is unproved, but a
patient without a radial head probably could not be a baseball pitcher.
The potential enhancement of stability that a radial head prosthesis
can provide in a young athlete or laborer must be balanced with the
potential short- and long-term risks of a metal prosthesis, which
remain incompletely defined.
small, to a dislocation of the elbow and fracture of the radial head,
dramatically increases the instability and the potential for problems.56,101,117 As a result, the term “terrible triad of the elbow” has been coined by Hotchkiss50
to refer to this injury pattern. Not all terrible triad injuries will
be unstable, but it can be difficult to predict which injuries will be
unstable. Recurrent subluxation or dislocation can destroy the elbow
articulation, particularly if it is not recognized and abnormal contact
of the articular surface persists.
fragments come from the radial head or coronoid. The coronoid fracture
is usually quite easily distinguished as a small triangular fragment
anterior to the trochlea in a dislocated position and in the coronoid
fossa after reduction (Fig. 32-17A). The coronoid process
should be evaluated for a defect. Given the important influence of an
associated coronoid fracture, a computed tomography scan should be
obtained if there is any doubt. The coronoid fracture is nearly always
a small transverse fracture of the tip with the capsule attached (Fig. 32-17B). On rare occasions, the fracture will involve the anteromedial facet.
dislocate in a cast, unknown to the patient. Radial head resection
without prosthetic replacement is unwise as recurrent dislocation of
the elbow is common.117 Good results
have been documented with repair of the coronoid or anterior capsule,
repair or replacement of the radial head, and LCL repair.101
Doing so restores stability in most cases, but in some patients MCL
repair or hinged external fixation is also necessary. The use of
cross-pinning of the ulnohumeral joint has been presented at a national
meeting (K. Cramer and colleagues, presented at the 1999 annual meeting
of the Orthopaedic Trauma Association, Charlotte, NC) with reasonably
good results but has not yet been published in a peer-reviewed journal.
With specific treatment of each of the injury components, this step
should rarely be necessary.101
have used it in very motivated patients with concentric reductions who
were capable of confident active motion of the elbow. In particular,
when a patient presents more than 1 week after injury with a
comfortable and stable 80- to 100-degree arc of ulnohumeral motion,
unrestricted forearm motion, and a concentric reduction on radiographs,
it is difficult to justify operative treatment.
head repair or replacement and LCL repair only in many patients;
however, if doing so results in inadequate stability, these repairs
must be taken down to restore access to the coronoid. Respecting that
these injuries are infamously problematic, I prefer to repair the
coronoid fracture, the radial head and the LCL working from inside out.
This nearly always restores good stability in gravity extension of the
elbow without the need for MCL repair, hinged external fixation, or
cross-pinning of the joint.
of the small transverse fractures of the coronoid that are usually
associated with a terrible triad injury pattern can be accomplished
through a lateral exposure. The unusual anteromedial coronoid fracture
will require a separate medial exposure.
incision, elevating a lateral skin flap. This provides access to the
dorsal ulna for passing the coronoid sutures and to the medial side of
the elbow in case the ulnar nerve or MCL needs to be addressed or a
hinged external fixator will be applied.
but usually the overlying fascia is intact. In such cases, I identify
the supracondylar ridge of the humerus and incise and elevate the
radial wrist extensors off of the ridge anteriorly. As one works
distally, it will become apparent that the LCL and some or all of the
common extensor musculature has been avulsed from the lateral
epicondyle. An interval in the common extensors is selected based upon
what is injured and it is developed distally. This interval should be
anterior to the midline of the radial head and neck. The supinator is
spread bluntly over the radial neck, but it is rarely necessary to
dissect very far distally where the posterior interosseous nerve would
be placed at risk.
elevation of the radial wrist extensors from the supracondylar ridge,
slight splitting of the supinator distally, and subluxation of the
elbow all help to expose the coronoid fracture in the depths of the
wound.
drill holes in the ulna. Creation of the drill holes can be facilitated
with a drill guide such as that used to assist with repair of the
anterior cruciate ligament of the knee or they can be made free hand.
Two drill holes, one medial and one lateral, are created in the bed of
the coronoid fracture. A simple method for passing the sutures is to
put a suture loop on a Keith needle, pass the needle and loop into the
drill holes and pull the suture loop from the coronoid base out into
the wound. A suture can then be easily passed through the loop and
pulled through the ulna. Suture passers can also be used, but they
require passing the suture deep in the confined space of the wound. The
suture is passed through drill holes in the coronoid fragment for
larger fragments (Fig. 32-29B) and around the
fragment and through the anterior capsular attachment in small or
comminuted coronoid fragments. It is then passed through the other hole
in the ulna. Precise anatomic alignment is not crucial—the goal is to
restore the anterior capsular insertion and create an anterior bony
buttress (Fig. 32-29C). This suture is not tied
until the radial head has been treated as subluxation of the joint
facilitates treatment of the radial head.
described in the section on radial head fractures. The LCL is repaired
as described earlier (Fig. 32-29D). The
coronoid suture is then tensioned and tied followed by tying of the LCL
repair sutures. Stability in gravity extension is tested. If there is
substantial subluxation or dislocation of the elbow in gravity
extension, consideration is given to repairing the MCL. Alternatively,
a hinged external fixator is applied. If the elbow remains unstable
after the surgeon has done everything within their skill and resources
to stabilize it, it is reasonable to cross-pin the elbow.
ulnar neuropathy are all relatively more frequent after terrible triad
injuries than simple dislocations and dislocation with fracture of the
radial head.101,117
always necessary for these injuries. We have data showing that
nonoperative treatment and radial head resection without prosthetic
replacement risks redislocation117 and data that fixation of the coronoid can restore stability in most cases,101 but we do not have data regarding the efficacy of treatment of the radial head and collateral ligaments alone.
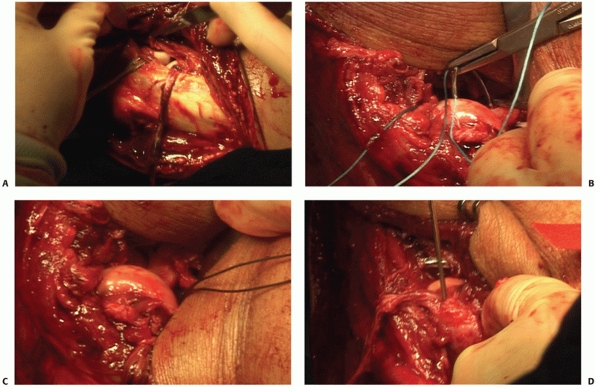 |
|
FIGURE 32-29 Operative treatment of a terrible triad elbow fracture-dislocation. A.
A traumatic rent in the common extensors was developed distally. The strand of tissue still attached to the lateral epicondyle is musculoteninous, not ligament. B. Sutures passed through drill holes in the ulna are passed through drill holes in the large coronoid fragment. C. The coronoid is reduced, restoring an anterior buttress and the function of the anterior capsule. D. The lateral collateral ligament complex is reattached to the lateral epicondyle using a suture anchor. The radial head has been replaced with a prosthesis. |
that it is rarely necessary when all of the lateral structures and the
coronoid have been repaired.101 In
fact, it is my impression that in the rare patient in whom treatment of
the coronoid, radial head, and LCL do not restore stability, then
repair of the MCL will not add much and one should be prepared to
proceed to hinged external fixation or cross-pinning of the joint.
controversial. I would point out that a stiff elbow with preserved
articular surface is easier to treat than an elbow with a damaged
articular surface because of chronic subluxation and abnormal wear.
Recognizing the expense, skill, and resources needed to apply a hinged
fixator successfully, I think cross-pinning has a useful role for the
very unstable elbow.
expected, but the patient is often capable of substantial active
motion. In fact, given the small size of the associated coronoid
fracture in most cases, the surgeon may be tempted to treat the injury
with early active motion to avoid instability (Table 32-3). Patients will often report clunking or giving way of the elbow when this is attempted—evidence of the underlying instability.
subluxation and arthrosis of the elbow. It has only recently been
recognized and it is relatively uncommon, so our knowledge of the
results of nonoperative treatment is limited. Early experience would
suggest that these injuries benefit from operative treatment.90
injury is a displaced fracture of the anteromedial facet of the
coronoid process (Fig. 32-30A), reflecting the varus injury mechanism. Associated injuries include one of the following: (i) injury to the LCL (Fig. 32-30B), (ii) fracture of the olecranon (Fig. 32-30C), or (iii) an additional fracture of the coronoid at its base (Fig. 32-30D-F). It is rare to have more than one of these associated injuries.
reconstructions, is useful to plan treatment of the coronoid fracture.
The coronoid fracture usually involves anteromedial facet and tip
fragments and occasionally extends to the base of the coronoid process.
|
TABLE 32-3 Pitfalls and Pearls for Elbow Fracture-Dislocations and Coronoid Fractures
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
injured structures. The LCL and/or olecranon fracture is repaired, and
the coronoid is repaired through a medial exposure using some
combination of wires, plates, and screws. A buttress plate is
particularly useful.
Fracture. A medial skin flap is elevated with care taken to protect the
medial antebrachial cutaneous nerve and the ulnar nerve. We prefer to
mobilize the ulnar nerve from the cubital tunnel, allowing it to remain
anteriorly transposed in the subcutaneous tissues at the end of the
procedure (Fig. 32-18E). From the medial side,
the coronoid can be exposed directly medially—between the heads of the
flexor carpi ulnaris where the ulnar nerve usually lies—or superiorly
through the over-the-top approach described by Hotchkiss49 for contracture release (Fig. 32-5). Taylor and Scram127
described elevation of the entire flexor-pronator mass, but this
requires far more dissection than elevation from within the split in
the flexor carpi ulnaris. It is useful for very large fragments.
superficial to the anterior band of the MCL. In addition, capsular
attachments to the tip of the coronoid should be preserved. Through
this exposure a small T-plate or a plate designed specifically for
internal fixation of the coronoid can be applied.
of the ulnar nerve is needed to perform a medial repair and ulnar nerve
palsies sometimes occur. Large tapes and tapes with hemostats should
not be used for retraction as they may lead to excessive traction on
the nerve. A means for providing adequate retraction of the nerve
without prolonged pressure needs to be devised. I have sutured the skin
to the forearm fascia to hold the transposed nerve anteriorly as I work
on the coronoid.
Improved exposure and plating techniques for the medial coronoid will
most likely be developed with increasing experience with this injury
pattern.
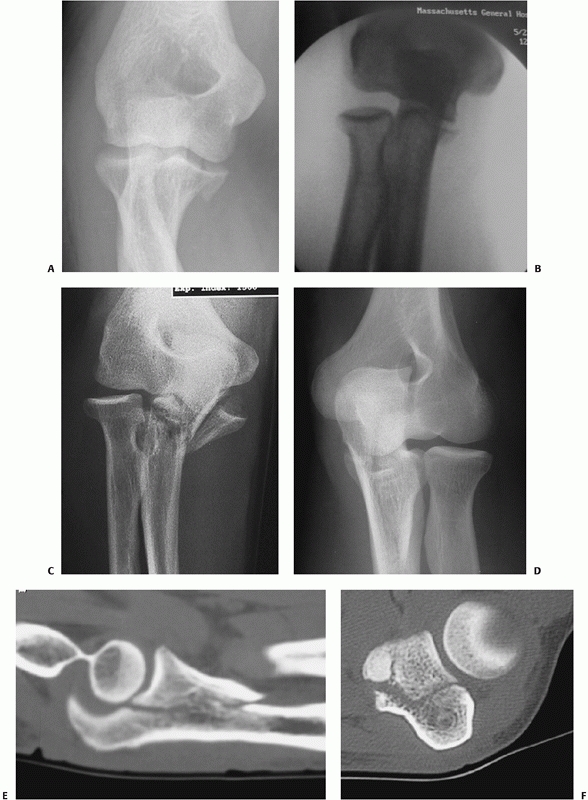 |
|
FIGURE 32-30 Varus posteromedial rotational instability injuries occur in several forms. A. Some patients present with small isolated anteromedial facet coronoid fractures. B. Stress radiographs reveal injury to the lateral collateral ligament. C.
Alternatively, there may be a fracture of the olecranon, in which case there is usually not a lateral collateral ligament injury. D-F. Finally, some patients with anteromedial coronoid facet fractures may have a fracture of the coronoid at its base. |
proximal ulna, no matter how complex, is to restore the contour and
dimensions of the trochlear notch of the ulna. Small articular
incongruities and comminution in the relatively nonarticular transverse
groove will be of little consequence provided that stable realignment
of the coronoid and olecranon facets is achieved.90,115,116 These fractures often occur in patients with poor bone quality.116
Careful technique and an understanding of how to achieve reliable
internal fixation are important. Restoration of the trochlear notch is
the key to restoring elbow stability. Also important are repair or
replacement of the radial head and repair of the LCL complex when they
are injured. Stable fixation will allow immediate mobilization, thereby
diminishing the risk of stiffness and heterotopic ossification (Table 32-4).
often of limited quality because of the deformity and pain in the limb.
Nevertheless, it is usually possible to discern the overall pattern of
the injury, which in turn leads one to suspect other injury components
that may not be immediately obvious. For example, a posterior olecranon
fracture-dislocation is often associated with fractures of the radial
head and coronoid process as well as injury to the LCL complex,116 whereas an anterior fracture-dislocation rarely involves injury to the radial head or collateral ligaments.115
|
TABLE 32-4 Pitfalls and Pearls for Olecranon and Proximal Ulna Fractures
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
splint immobilization of the limb (when appropriate) may provide better
views of the elbow and additional information about the injury. When
additional information about fractures of the radial head or coronoid
may influence decision making, computed tomography is useful. In
particular, three-dimensional reconstructions with the distal humerus
removed can provide a very accurate characterization of the injury.
Using such images, preoperative planning will be more accurate.
injury can be obtained by viewing the elbow under the image intensifier
once the patient is anesthetized. For some complex injuries, complete
characterization of the injury pattern—and therefore a final treatment
plan—can only be made based on operative exposure. Thus, the surgeon
must be comfortable with extensile exposures providing adequate access
to the injury components.
been recognized as a distinct injury that is usually associated with
fracture of the radial head and often occurs in the setting of
osteoporosis59,95,98 (see Chapter 31).
There is a spectrum of posterior Monteggia injuries with similar
features that vary according to the location of the ulnar fracture.59
These have been subclassified as type A when the fracture is at the
level of the trochlear notch (involving the olecranon and often the
coronoid processes); type B, in the metaphysis just distal to the
trochlear
notch; and type C, in the diaphysis. Type D fractures are multifragmented fractures that involve more than one region.59
These fractures are inherently unstable by virtue of the associated
capsuloligamentous damage, fracture and dislocation of the radial head,
and the morphology of the ulnar fracture, which often involves a
triangular or quadrangular fragment of the ulna that includes the
anterior ulnar cortex and sometimes the coronoid process.
distinguishes three factors that have a direct influence on treatment:
(i) fracture displacement, (ii) comminution, and (iii) ulnohumeral
instability79 (Fig. 32-31).
Type 1 fractures that are nondisplaced or minimally displaced are
either noncomminuted (type 1A) or comminuted (type 1B) and are treated
nonoperatively. Type II fractures feature displacement of the proximal
fragment without elbow instability—these fractures require operative
treatment. Type IIA fractures, which are noncomminuted, are well
treated by tension band wire fixation. When the fracture is oblique, an
ancillary interfragmentary compression screw can be added. Type IIB
fractures are comminuted and require plate fixation. Type III fractures
feature instability of the ulnohumeral joint and require surgical
treatment.
complex, and identification of basic injury patterns can facilitate
management. Even a simple fracture pattern of the olecranon can have
associated injuries, which the surgeon must be careful not to miss.
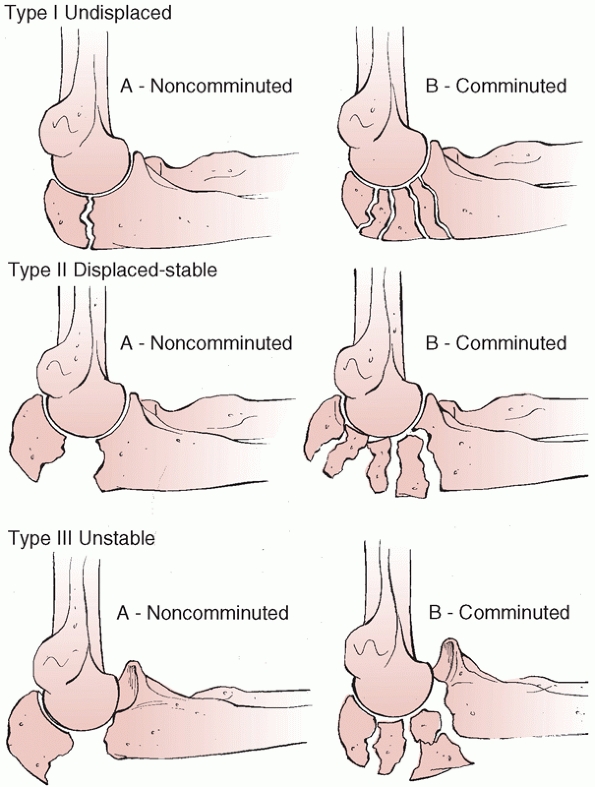 |
|
FIGURE 32-31
The Mayo classification of olecranon fractures divides fractures according to displacement, comminution, and subluxation/dislocation. |
injuries have only recently been recognized and described. The central
element of this injury is a fracture of the anteromedial facet of the
coronoid process, resulting in varus instability.112
There is an associated injury, either an avulsion of the LCL complex
from the lateral epicondyle or a fracture of the olecranon—but rarely
both. The radial head is rarely fractured.
Anterior olecranon fracture-dislocations have been described as
transolecranon fracture dislocations because the trochlea of the distal
humerus implodes through the trochlear notch of the ulna as the forearm
translates anteriorly4,115 (Fig. 32-19). This pattern can be confused with posterior fracture-dislocations with a similar appearance, so the term anterior olecranon fracture-dislocation
may be preferable. Anterior fracture-dislocations are injuries to the
ulnohumeral articulation with the radioulnar relationship being
relatively preserved and the radial head rarely injured. The fracture
of the proximal ulna can be a simple oblique fracture, but it is often
very complex, including fragmentation of the olecranon, fragmentation
extending into the ulnar diaphysis, and fracture of the coronoid.
Associated collateral ligament injury is unusual.4,115
of the olecranon as the most proximal type of a posterior Monteggia
injury.59 Common factors of
posterior Monteggia injuries include an apex posterior fracture of the
ulna, posterior translation of the radial head with respect to the
capitellum, fracture of the radial head, and frequent injury to the LCL
complex. With posterior olecranon fracture-dislocations (or type A
posterior Monteggia fractures, according to Jupiter and colleagues59),
the fracture of the ulna occurs at the level of the olecranon and is
nearly always associated with a fracture of the coronoid process. When
a complex olecranon fracture-dislocation is identified as being
posterior in direction, fractures of the radial head and coronoid and
injury to the LCL should be suspected (Fig. 32-20).
specific type of olecranon fracture-dislocation. Those associated with
a varus posteromedial mechanism will involve the anteromedial facet and
the tip and the radial head will not be fractured. The fracture of the
coronoid that occurs with an anterior olecranon fracture-dislocation is
usually a single, large fragment involving nearly the entire coronoid,
but it is occasionally split once or twice in the sagittal plane. The
fractures of the coronoid associated with posterior olecranon
fracture-dislocations are more variable including the occasional
fracture of the tip, a single large fragment, comminution into three
fragments (anteromedial, central, and sigmoid notch), and more
extensive comminution (Fig. 32-19).
displaced and does not displace further with the arm placed in 90
degrees of flexion can be treated nonoperatively. The elbow is splinted
for 3 to 4 weeks in 90 degrees of flexion, and then gentle active
motion is started gradually progressing to active assisted motion.
cannot be repaired. Tension band wiring techniques can gain fixation of
the soft tissue attachments until healing occurs. As a result, excision
of the olecranon and triceps advancement are used sparingly for primary
treatment of fractures of the olecranon and occasionally for treatment
of secondary complications. As primary treatment, excision of the
olecranon is best suited to infirmed older patients with limited
functional demands.18,31 The surgeon must be certain that the collateral ligaments, radial head, and coronoid process are intact.
fractures at the level of the transverse groove of the trochlear notch,
without associated ligament injuries or fracture of the coronoid or
radial head (Fig. 32-32). Tension band wire techniques have been described using screws or Kirschner wires.
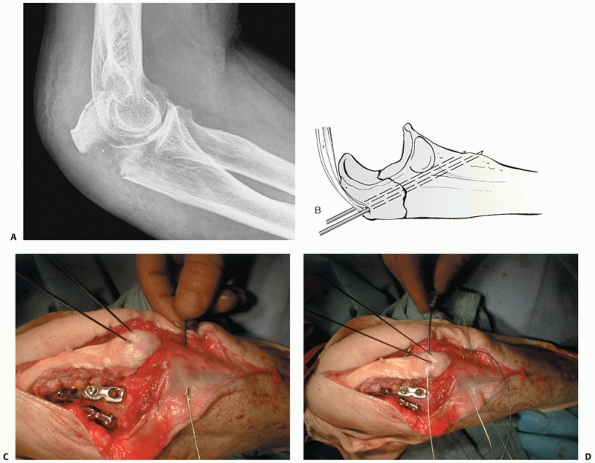 |
|
FIGURE 32-32 Tension band wiring is useful for simple isolated fractures of the olecranon. A. Lateral radiograph demonstrates a transverse fracture of the olecranon. B.
The fracture is realigned and secured with two 0.045-inch Kirschner wires drilled obliquely so that they engage the anterior ulnar cortex distal to the coronoid. C. Two 22-gauge stainless steel wires are passed through drill holes in the ulna distal to the fracture. D. The wires are passed underneath the triceps insertion adjacent to the Kirschner wires. (continues) |
nondisplaced fracture of the olecranon but prefer to repair the
majority of these fractures to start confident active motion exercises
and functional use of the limb.
ligament injuries, I use tension band wiring with Kirschner wires
rather than a screw. For comminuted fractures and fracture
dislocations, I use a dorsal plate and screws contoured to wrap around
the proximal ulna.109,115,116
For some complex fractures, I place the proximal aspect of the plate
over the triceps insertion. Otherwise, I elevate the triceps insertion
and place the plate directly on bone. When the proximal olecranon
fragment is small, fragmented, or osteopenic, I also use a tension band
wire that engages the triceps insertion (Fig. 32-33).
anteromedial facet, I use a medial plate unless the fragments are large
enough to be reliably repaired with screws.112
For unreconstructable or very complex fractures of the coronoid, I use
4 to 8 weeks of hinged external fixation to maintain a concentric
ulnohumeral reduction and protect the healing coronoid.
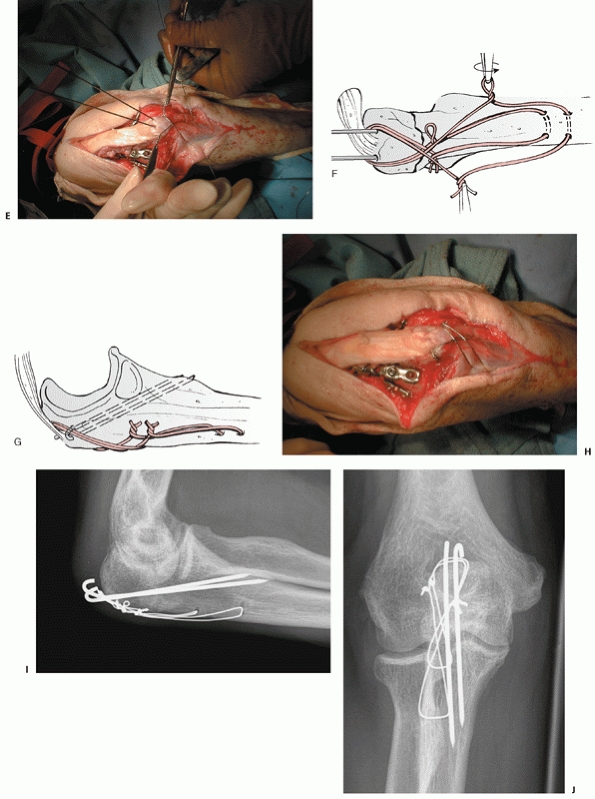 |
|
FIGURE 32-32 (Continued) E,F. The wires are then tensioned both medially and laterally. G. The Kirschner wires are then bent 180 degrees and impacted into the olecranon beneath the triceps insertion. H. The wires are bent into the adjacent soft tissues so that the entire construct has a very low profile. I. Postoperative lateral radiograph. J. Postoperative anteroposterior radiograph.
|
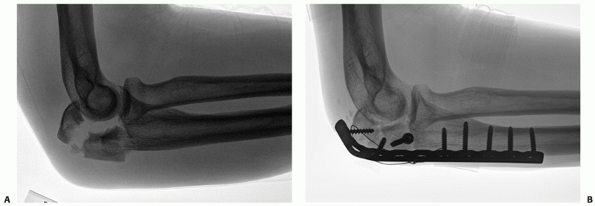 |
|
FIGURE 32-33 Comminuted olecranon fractures require plate and screw fixation. A. This injury created a small olecranon fragment. B.
In addition to the plate and screws used to maintain alignment of the trochlear notch, a tension band wire is used to gain hold of the small proximal fragment. |
for all complex fractures of the proximal ulna. Traumatic wounds are
incorporated. Some surgeons prefer that the incision not pass directly
over the olecranon, and curve it slightly.81 A direct midline incision may cut fewer cutaneous nerves.23
The fragments of the olecranon are excised. Drill holes are made
starting from immediately adjacent to the articular margin of the
remaining olecranon and exiting the dorsal surface of the ulna. Stout
sutures are placed in the triceps using one of a variety of techniques
designed to gain hold over a broad portion of the tendon. These are
then passed through the drill holes in the ulna, tensioned and tied.
The elbow is immobilized for 4 weeks and active motion is allowed
thereafter. In low-demand individuals, formal therapy is not necessary.
fracture is opened and the hematoma removed to be sure that comminution
and articular involvement are limited. Periosteum and muscular
attachments are elevated minimally—just enough to ensure accurate
reduction of the fragments. A large tenaculum clamp can be used to
maintain reduction of the olecranon. A drill hole made in the dorsal
surface of the ulna can provide a good anchor point for the distal tine
of the clamp.
Two parallel Kirschner wires are drilled across the osteotomy site. The
majority of surgeons use 0.062-inch wires, but we use 0.045-inch wires
with few problems. The wires are often drilled parallel to the ulnar
diaphysis, but we and others favor drilling the wires obliquely so that
they pass through the anterior ulnar cortex, just distal to the
coronoid process.13,99
This is intended to limit the potential for wire migration. After
exiting the anterior cortex, the wires are retracted between 5 and 10
mm, anticipating subsequent impaction of the wires into the olecranon
process proximally.
muscles are partly elevated from the apex of the ulna distal to the
fracture site to expose the cortex. The appropriate distance between
the fracture and the transverse ulnar drill hole(s) has been commented
on based on mechanical calculations, but the location is determined
more practically by the transition from the flat proximal ulna to the
apex posterior triangular shape of the diaphysis. Likewise, the
placement of the drill holes in the anteroposterior plane is not
critical except that they should not be so dorsal as to risk breaking
out of the ulna. Large drill holes (2.5 mm) facilitate wire passage.
for the tension wire, but we prefer to use two 22-gauge stainless steel
wires, each passed through its own drill hole distally (Fig. 32-32). The smaller wires are less prominent.
configuration over the dorsal ulna. The proximal end of each wire is
passed deep to the Kirschner wires, through the insertion of the
triceps using a large-gauge needle. The tension band wires are then
tensioned on both the medial and lateral sides of the ulna until they
rest flush with the ulna. Some surgeons prefer to twist the wires until
they are very tight, but this cannot be done with smaller gauge
wires—they will break. The wire does not need to be tight; it is only
important to take up all of the slack in the wires. This is done by
twisting each wire until it starts to bend over itself. The twisted
ends are trimmed and bent into the adjacent soft tissues to limit
prominence.
degrees and trimmed. The triceps insertion is then incised, and these
bent ends are impacted into the proximal olecranon using a bone tamp
and mallet. The strength of the fixation can be tested by completely
flexing the elbow—the fracture should not separate.
Some surgeons prefer to use screws instead of Kirschner wires. Some
recommend using a very long screw that engages the medullary canal of
the ulnar diaphysis distally.51
Others recommend aiming the screw anteriorly to engage the anterior
ulnar cortex. An oblique screw is particularly well suited to an
oblique fracture. The remaining portion of the technique is as
described for the Kirschner wire technique.
A straight plate will only have two or three screws in metaphyseal bone
proximal to the fracture. Many patients with complex proximal ulna
fractures have osteopenic bone, which further compromises the strength
of plate and screw fixation. Bending the plate around the proximal
aspect of the olecranon provides for additional screws to be placed in
the proximal fragment. In addition, the most proximal screws are
oriented orthogonal to the more distal screws. Finally, the most
proximal screws can be very long, crossing the fracture line into the
distal fragment. In some cases, these screws can be directed to engage
one of the cortices of the distal fragment, such as the anterior ulnar
cortex.
ulna also has several advantages over plates applied to the medial or
lateral aspects of the ulna. Placing the plate along the flat dorsal
surface can assist in obtaining and monitoring reduction. The dorsal
surface is in the plane of the forces generated by active elbow motion
so that the plate functions to a certain extent as a tension band.
Finally, dorsal plate placement requires very limited soft tissue
stripping.
muscle attachments. A plate contoured to wrap around the proximal ulna
can be placed on top of the triceps insertion with few problems. This
is particularly useful when the olecranon fragment is small or
fragmented. Alternatively, the triceps insertion can be incised
longitudinally and partially elevated medially and laterally to allow
direct plate contact with bone.
of the ulnar diaphysis. This might seem unsettling to some surgeons,
but has not been a problem in our hands. One advantage of this
situation is that the muscle need only be split sufficiently to gain
access to this apex—there is no need to elevate the muscle or
periosteum off either the medial or lateral flat aspect of the ulna. No
attempt is made to precisely realign intervening fragmentation—once the
relationship of the coronoid and olecranon facets is restored and the
overall alignment is restored, the remaining fragments are bridged,
leaving their soft tissue attachments intact. Despite extensive
fragmentation, bone grafts52 are rarely necessary if the soft tissue attachments are preserved.115,116
evaluated and often definitively treated through the exposure provided
by the fracture of the olecranon process. With little additional
dissection, the olecranon fragment can be mobilized proximally,
providing exposure of the coronoid through the ulnohumeral joint. If
the exposure of the radial head through the posterior injury is
inadequate, a separate muscle interval (e.g., Kocher or Kaplan intervals81)—accessed by the elevation of a broad lateral skin flap can be used.
the straight dorsal skin incision, a separate medial or lateral
exposure can be developed. Posterior olecranon fracture-dislocations
often require a lateral exposure to address a fracture of the radial
head or coronoid, or to repair the LCL. When the LCL is injured it is
usually avulsed from the lateral epicondyle. This injury facilitates
both exposure and repair. The LCL origin and common extensor
musculature can be included in an anterior or a posterior flap, or
mobilized distally.
releasing the origins of the radial wrist extensors from the lateral
supracondylar ridge and elevating the brachialis from the anterior
humerus, and by excising the fractured radial head.110,112
A medial exposure, developed between the two heads of the flexor carpi
ulnaris, or by splitting the flexor-pronator mass more anteriorly, may
be needed to address a complex fracture of the coronoid, particularly
one that involves the anteromedial facet of the coronoid process.
directly through the elbow joint using the limited access provided by
the olecranon fracture.41,42,88
Provisional fixation can be obtained using Kirschner wires to attach
the fragments to either the metaphyseal or diaphyseal fragments of the
ulna or to the trochlea of the distal humerus when there is extensive
fragmentation of the proximal ulna.40,68
An alternative to keep in mind when there is extensive fragmentation of
the proximal ulna is the use of a skeletal distractor (a temporary
external fixator).68,115
External fixation applied between a wire driven through the olecranon
fragment and up into the trochlea and a second wire in the distal ulnar
diaphysis can often obtain reduction indirectly when distraction is
applied between the pins. Definitive fixation can usually be obtained
with screws applied under image intensifier guidance. The screws are
placed through the plate when there is extensive fragmentation of the
proximal ulna. If the coronoid fracture is very comminuted and cannot
be securely repaired, the ulnohumeral joint should be protected with
temporary hinged or static external fixation, or temporary pin fixation
of the ulnohumeral joint, depending on the equipment and expertise
available.
olecranon. A very long plate should be considered (between 12 or 16
holes), particularly when there is extensive fragmentation or the bone
quality is poor. When the olecranon is fragmented or osteoporotic, a
plate and screws alone may not provide reliable fixation. In this
situation, it has proved useful to use ancillary tension band wire
fixation to control the olecranon fragments through the triceps
insertion.
complex fractures or fracture-dislocations, but rarely fail when used
for simple fractures unless the patient returns to forceful activity
too soon. Plate loosening is most common in older patients with
fracture-dislocations when a noncontoured plate has been placed on
either the medial or lateral side of the proximal ulna (Fig. 32-34).
Failed internal fixation can be salvaged with realignment and repeat
internal fixation using a dorsal contoured plate and screws. If there
is a bone defect or delayed union, autogenous cancellous bone graft can
be applied to the fracture site.
Proximal ulnar nonunion usually occurs after a fracture-dislocation of
the proximal ulna. Union can usually be achieved with contoured dorsal
plate fixation and autogenous bone grafting.93,113
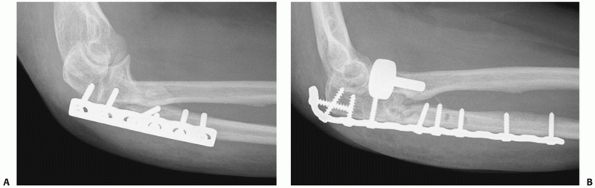 |
|
FIGURE 32-34 Medial and lateral plates seem prone to failure when treating posterior Monteggia injuries. A.
This plate only has two screws in the proximal, osteoporotic metaphyseal fragment and it is therefore not surprising that it loosened. B. A much more secure plate applied to the dorsal surface and contoured to wrap around the olecranon process has four screws in the proximal fragment with orthogonal interlocking of the most proximal screws. |
surgeon when treating a complex proximal ulna fracture. It is usually
the result of some combination of fixation of the proximal ulna with
apex dorsal deformity, as well as inadequate treatment of an injury to
the coronoid, radial head and for LCL complex. This instability can
often be salvaged by secondary surgery, often including the use of
hinged external fixation.71,107,111,119
these injuries, particularly posterior olecranon-fracture dislocations.
Proximal radioulnar synostosis occurs fairly frequently with these
injuries.
fixation for even relatively simple fractures of the olecranon. In some
ways, the tension band wire is a more reliable way to fix these
relatively small fracture fragments. Additional data are needed to
understand the relative advantages and disadvantages of each technique.
ulna and olecranon fracture-dislocations continues to evolve and
improve. In particular, the handling of a complex comminuted basal
coronoid fracture still represents a substantial challenge.
SA, Morrey BF, Adams RA, et al. Ulnohumeral arthroplasty for primary
degenerative arthritis of the elbow: long-term outcome and
complications. J Bone Joint Surg Am 2002;84A:2168-2173.
G, Worsdorfer O, Braun K. [Radio-ulnar bridge callus following
osteosynthesis of forearm fractures.] Aktuelle Traumatol
1990;20:194-198.
DM, Dunning CE, Beingessner CJ, et al. The effect of radial head
fracture size on radiocapitellar joint stability. Clin Biomech
2003;18:677-681.
AE, Mazzocca AD, Santoro VM. The nonarticulating portion of the radial
head: anatomic and clinical correlations for internal fixation. J Hand
Surg 1998;23A:1082-1090.
RM, Medige J, Curtain D, et al. Silicone rubber replacement of the
severely fractured radial head. Clin Orthop 1986;209:259-269.
SL, Morrey BF. Treatment of the mobile, painful arthritic elbow by
distraction interposition arthroplasty. J Bone Joint Surg Br
2000;82B:233-238.
MS, Hastings H. Posttraumatic contracture of the elbow: operative
release using a lateral collateral liagment sparing approach. J Bone
Joint Surg Br 1998;80B:805-812.
MS, Hastings H. Rotatory instability of the elbow: the anatomy and role
of the lateral stabilizers. J Bone Joint Surg Am 1997;79A:225-233.
ML, Fernandez JJ, Lim TH, et al. Partial olecranon excision: the
relationship between triceps insertion site and extension strength of
the elbow. J Hand Surg Am 2003;28A:117-122.
T, Botte MJ, Abrams RA. Anatomical considerations regarding the
posterior interosseous nerve during posterolateral approaches to the
proximal part of the radius. J Bone Joint Surg Am 2000;82A:809-813.
JN, de Jong IM, Lindenhovius AL, et al. The anteromedial facet of the
coronoid process of the ulna. J Shoulder Elbow Surg 2007;16:667-670.
JN, Parisien R, van Duijn PJ, et al. Radial head arthroplasty with a
modular metal spacer to treat acute traumatic elbow instability. J Bone
Joint Surg Am 2007;89:1075-1080.
AD, Kulijdian A, McKee MD, et al. Residual subluxation of the elbow
after dislocation or fracture-dislocation: treatment with active elbow
exercises and avoidance of varus stress. J Shoulder Elbow Surg 2007;Dec
24.
CE, Zarzour ZD, Patterson SD, et al. Muscle forces and pronation
stabilize the lateral ligament deficient elbow. Clin Orthop
2001;388:118-124.
M, Müller W, Rüedi TP, et al. The operative treatment of elbow
dislocation in the adult. J Bone Joint Surg Am 1979;61A:239-244.
E, Wang J, Jupiter JB. Secondary ulnar nerve palsy in adults after
elbow trauma: a report of two cases. J Hand Surg 2001;26A:675-678.
C. Fractures of the radial head. In: McQueen MM, Jupiter JB, eds.
Radius and Ulna. Oxford: Butterworth-Heinemann, 1999:159-168.
JJ, Faber KJ, Patterson SD, et al. The effectiveness of turnbuckle
splinting for elbow contractures. J Bone Joint Surg Br 2000;82B:74-78.
I, Peylan J, Yosipovitch Z, et al. Late results of excision of the
radial head for an isolated closed fracture. J Bone Joint Surg Am
1986;68A:675-679.
M, Bullough PG. Synovial and osseous inflammation in failed
silicone-rubber prosthesis. J Bone Joint Surg Am 1982;64A:574-580.
DP, McCoy H. Turnbuckle orthotic correction of elbow-flexion
contractures after acute injuries. J Bone Joint Surg Am
1979;61A:1092-1095.
R, MacDermid JC, Faber KJ, et al. Comminuted radial head fractures
treated with a modular metallic radial head arthroplasty. Study of
outcomes. J Bone Joint Surg Am 2006;88A:2192-2200.
H, Engles DR. Fixation of complex elbow fractures, part II: proximal
ulna and radius fractures. Hand Clin 1997;13:721-735.
U. Combined fractures of the upper end of the ulna and the radius in
adults: a series of 120 cases. Rev Chir Orthop 1998;84:142-153.
P, Josefsson PO, Hasserius R, et al. Uncomplicated Mason type II and
III fractures of the radial head and neck in adults. A long-term
follow-up study. J Bone Joint Surg Am 2004;86A:569-574.
E, Böstman O, Rokkanen P. Absorbable polyglycolide pins in fixation of
displaced fractures of the radial head. Arch Orthop Trauma Surg
1990;109:258-261.
RN. Elbow contracture. In: Green DP, Hotchkiss RN, Pederson WC, eds.
Green’s Operative Hand Surgery. Philadelphia: Churchill-Livingstone,
1999:667-682.
RN. Fractures and dislocations of the elbow. In: Rockwood CA, Green DP,
Bucholz RW, et al, eds. Rockwood and Green’s Fractures in Adults. 4th
ed. Philadelphia: Lippincott-Raven, 1996:929-1024.
DT, Horowitz DS, Ha G, et al. Cyclic loading of olecranon fracture
fixation constructs. J Bone Joint Surg Am 2003;85A:831-837.
FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral
ligament in athletes. J Bone Joint Surg Am 1986;68A:1158-1163.
PO, Gentz CF, Johnell O, et al. Surgical versus nonsurgical treatment
of ligamentous injuries following dislocation of the elbow joint. J
Bone Joint Surg Am 1987;69A:605-608.
T, Garreaue de Loubresse C, Piriou P, et al. A floating prosthesis for
radial head fractures. J Bone Joint Surg Br 1996;78B:244-249.
JB, Ring D. Treatment of unreduced elbow dislocations with hinged
external fixation. J Bone Joint Surg Am 2002;84A:1630-1635.
RL, O’Driscoll SW. Elbow dislocations. In: Morrey BF, ed. The elbow and
Its Disorders. 2nd ed. Philadelphia: WB Saunders, 1993:441-452.
P, Morrey BF. The column procedure: a limited lateral approach for
extrinsic contracture of the elbow. J Bone Joint Surg Am
1998;80A:1603-1615.
JA, Wolfson AH. Early excision of heterotopic ossification about the
elbow followed by radiation therapy. J Bone Joint Surg Am
1997;79A:749-755.
MD, Bowden SH, King GJ, et al. Management of recurrent, complex
instability of the elbow with a hinged external fixator. J Bone Joint
Surg Br 1998;80B:1031-1036.
MD, Jupiter JB, Bosse G, et al. The results of ulnar neurolysis for
ulnar neuropathy during post-traumatic elbow reconstruction. Orthop
Trans 1995;19:162-163.
MD, Schemitsch EH, Sala MJ, et al. The pathoanatomy of lateral
ligamentous disruption in complex elbow instability. J Shoulder Elbow
Surg 2003;12:391-396.
TL, Noble PC, Bennet JB, et al. Simple dislocation of the elbow in the
adult: results after closed treatment. J Bone Joint Surg Am
1988;70A:244-249.
GK, Drennan DB, Maylahn DJ. Treatment of displaced segmental radial
head fractures: long-term follow-up. J Bone Joint Surg Am
1981;63A:712-717.
JK, Werier J, MacDermid JC, et al. Arthroplasty with a metal radial
head for unreconstructable fractures of the radial head. J Bone Joint
Surg Am 2001;83A:1201-1211.
BF. Anatomy of the elbow joint. In: Morrey BF, ed. The Elbow and Its
Disorders. 2nd ed. Philadelphia: WB Saunders, 1995:16-52.
BF. Current concepts in the treatment of fractures of the radial head,
the olecranon, and the coronoid. J Bone Joint Surg Am 1995;77A:316-327.
BF. Surgical exposures of the elbow. In: Morrey BF, ed. The Elbow and
Its Disorders. 2nd ed. Philadelphia: WB Saunders, 1993:139-166.
BF, Adams RA, Bryan RS. Total elbow replacement for posttraumatic
arthritis of the elbow. J Bone Joint Surg Br 1991;73B:607-612.
BF, Tanaka S, An KN. Valgus stability of the elbow. A definition of
primary and secondary constraints. Clin Orthop 1991;265:187-195.
ME, Nazarian S, Koch P, et al. The Comprehensive Classification of
Fractures of Long Bones. Berlin: Springer-Verlag, 1990.
BJ, O’Driscoll SW, Morrey BF. Ligamentous reconstruction for
posterolateral rotatory instability of the elbow. J Bone Joint Surg Am
1992;74A:1235-1241.
SW. Classification and spectrum of elbow instability: recurrent
instability. In: Morrey BF, ed. The Elbow and Its Disorders. 2nd ed.
Philadelphia: WB Saunders, 1993:453-463.
SW, Morrey BF, Korinek S, et al. Elbow subluxation and dislocation. A
spectrum of instability. Clin Orthop 1992;280:186-197.
K, Hirvensalo E, Bostman O, et al. Treatment of radial head fractures
with absorbable polyglycolide pins: a study on the security of fixation
in 38 cases. J Orthop Trauma 1994;8:94-98.
MJ, Williams JL, Marshall MP, et al. Biomechanical comparison of
fixation methods in transverse olecranon fractures: a cadaveric study.
J Orthop Trauma 1997;11:565-572.
DM, Wild LM, Schemitsch EH, et al. Standard surgical protocol to treat
elbow dislocations with radial head and coronoid fractures. J Bone
Joint Surg Am 2004;86A:1122-1130.
D, Doornberg JN. Fracture of the anteromedial facet of the coronoid
process. Surgical technique. J Bone Joint Surg Am 2007;89A(suppl 2 Pt
2):267-283.
D, Hannouche D, Jupiter JB. Surgical treatment of persistent
dislocation or subluxation of the ulnohumeral joint after
fracture-dislocation of the elbow. J Hand Surg [Am] 2004(29A):470-480.
D, Jupiter J. The operative release of complete ankylosis of the elbow
due to heterotopic bone in patients without severe injury of the
central nervous system. J Bone Joint Surg Am 2003;85A:849-857.
D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with
fractures of the coronoid and radial head. J Bone Joint Surg Am
2002;84A:547-551.
D, Jupiter JB, Zilberfarb J. Roles of the medial collateral ligament
and the coronoid in elbow stability. Reply to letter to the editor. J
Bone Joint Surg Am 2003;85A:568-569.
D, Kloen P, Tavakolian J, et al. Loss of alignment after operative
treatment of posterior Monteggia fractures: salvage with dorsal
contoured plate fixation. J Hand Surg [Am] 2004;29:694-702.
D, Quintero J, Jupiter JB. Open reduction and internal fixation of
fractures of the radial head. J Bone Joint Surg Am 2002;84A:1811-1815.
J, Romanillos O, et al. Results of acute excision of the radial head in
elbow radial head fracture-dislocations. J Orthop Trauma
2000;14:354-358.
AM, Urbanosky LR, Castle JA, et al. Radius pull test: predictor of
longitudinal forearm instability. J Bone Joint Surg Am
2002;84A:1970-1976.
GR, Hotchkiss RN. Radial head and neck fractures: anatomic guidelines
for proper placement of internal fixation. J Shoulder Elbow Surg
1996;5:113-117.
AD, Nowotarski PJ, Kelso TB, et al. Optimal position for plate fixation
of complex fractures of the proximal radius: a cadaver study. J Orthop
Trauma 1998;12:291-293.
TKF, Scham SM. A posteromedial approach to the proximal end of the ulna
for the internal fixation of olecranon fractures. J Trauma
1969;9:594-602.
Riet RP, Glabbeek FV, Verborgt O, et al. Capitellar erosion caused by a
metal radial head prosthesis. A case report. J Bone Joint Surg Am
2004;86A:1061-1064.
RS, Morrey BF, Melberg MW, et al. Inflammatory arthritis after failure
of silicone rubber replacement of the radial head. J Bone Joint Surg Br
1994;76B:78-81.
RW, Hanel DP. Early “simple” release of posttraumatic elbow contracture
associated with heterotopic ossification. J Hand Surg 1999;24:370-380.
