Terminal Nerve Blocks
II – Single-Injection Peripheral Blocks > A – Upper Extremity > 8
– Terminal Nerve Blocks
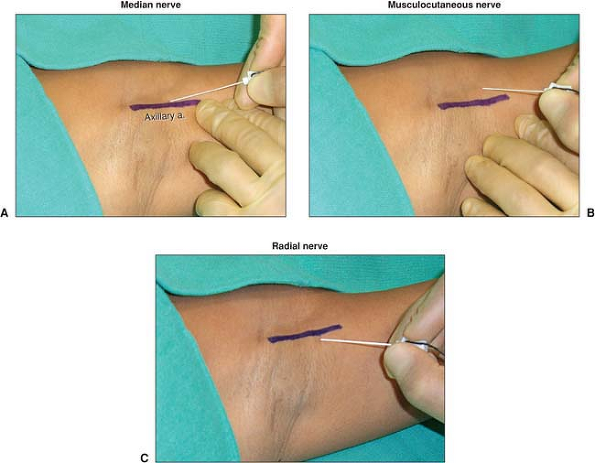
The axillary artery pulse is palpated and marked in the middle of the
axilla. After disinfection, sterile draping, and local infiltration
with 1% lidocaine, a 50-mm insulated needle connected to a nerve
stimulator (1.5 mA, 2 Hz, 0.1 ms) is inserted above the artery,
pointing in a proximal direction almost parallel to the artery at a 30°
to 45° angle to the skin (Fig. 8-1A).
After identification of a median nerve response (flexion of the fingers
and the wrist) at a current below 0.5 mA, 15 mL of local anesthetic is
injected slowly (10 mL/min) and in 5-mL increments. The 50-mm insulated
needle is then withdrawn from the skin and redirected toward the
coracobrachialis muscle (Fig. 8-1B).
After identifying a musculocutaneous nerve response (biceps
contraction, flexion of the elbow) at a current below 0.5 mA, 10 mL of
local anesthetic is injected slowly (10 mL/min) and in 5-mL increments.
The 50-mm insulated needle is then completely withdrawn and reinserted
below the artery 45° to the skin and to the artery (Fig. 8-1C).
After identification of a radial nerve response (extension of the
fingers and the wrist) at a current below 0.5 mA, 15 mL of local
anesthetic is injected in the same fashion as for the two other nerves.
The
axillary
block is completed by a subcutaneous infiltration at the medial aspect
of the upper arm at a high humeral level to block intercostobrachial
nerve fibers.
 |
|
Figure 8-1. A. Indicating an Axillary artery response, B. Indicating a Musculocutaneous nerve response and C. Indicating a Radial nerve response.
|
-
A separate stimulation and injection of
the ulnar nerve has been shown to be unnecessary for a complete
axillary block. if an ulnar nerve response (adduction of the thumb and
the little finger) is encountered during the performance of an axillary
block, 5 to 10 mL of local anesthetic can be injected after the
response is maintained below 0.5 mA. -
If one of the nerves is not completely
blocked with this approach, the block can be easily completed by an
injection at the midhumeral or elbow level after stimulating the nerve
in question. -
The radial nerve is probably the most
difficult nerve to stimulate and block when performing an axillary
block. Injecting after eliciting a distal twitch (wrist or finger
extension) has been demonstrated to yield a higher success rate than
accepting a proximal twitch (forearm extension). -
Distal digital pressure has been shown not to promote proximal local anesthetic spread and is therefore not necessary.
-
Axillary blocks significantly reduce the
incidence of complex regional pain syndrome after Dupuytren’s
contracture surgery, when compared with general anesthesia or
intravenous regional anesthesia with lidocaine.
ZJ, Rotboll Nielsen P, Sorenson T, et al. Low dose axillary block by
targeted injections of the terminal nerves. Can J Anaesth 1999;46:658–664.
SS, Pristas R, Dixon D, et al. The incidence of complex regional pain
syndrome after fasciectomy for Dupuytren’s contracture: a prospective
observational study of four anesthetic techniques. Anesth Analg 2006;102:499–503.
S, Bartoli M. Selective ulnar nerve stimulation is not essential for
axillary plexus block using a multiple stimulation technique. Reg Anesth Pain Med 2001;26:12–16.
S, Lepri A, Magherini M, et al. A comparison of proximal and distal
radial nerve motor responses in axillary block using triple
stimulation. Reg Anesth Pain Med 2005;30:458–463.
S, Lepri A, Ponzecchi P. Axillary brachial plexus block using
peripheral nerve stimulator: a comparison between double- and
triple-injection techniques. Reg Anesth Pain Med 2001;26:499–503.
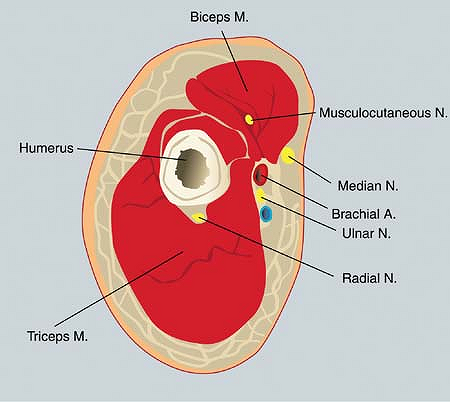
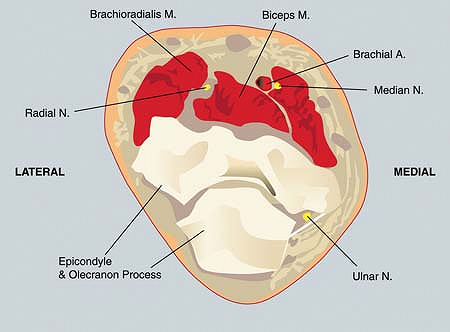
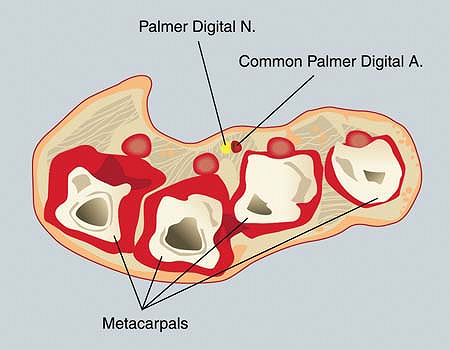
Upper one-third of arm and the brachial artery. At the level of the
brachial canal, the median, ulnar, radial, and musculocutaneous nerves
are dispersed around the brachial artery (Fig. 8-2).
The median nerve usually runs anterior and superior to the brachial
artery, while the musculocutaneous nerve runs posterior and superior to
the median nerve in a groove between the biceps and coracobrachialis
muscle. The ulnar nerve runs medial to the brachial artery, and the
radial nerve runs medial and posterior, between the triceps muscle and
the medial border of the humerus. The closer to the elbow, the more
separated are the nerves.
 |
|
Figure 8-2.
At the level of the brachial canal, the median, ulnar, radial, and musculocutaneous nerves are dispersed around the brachial artery. |
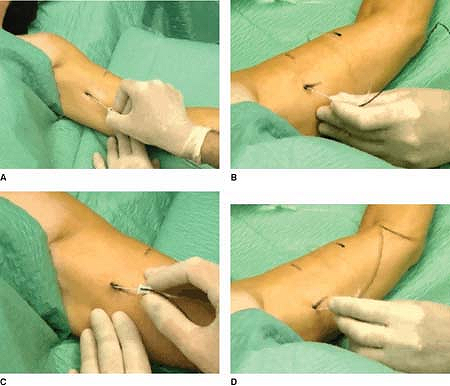
First, a line is drawn over the brachial artery. Then, a 22-gauge,
50-mm insulated needle connected to a nerve stimulator (2 mA, 2 Hz, 0.1
ms) is introduced almost tangentially to the skin, between the brachial
artery and the palpating finger of the anesthesiologist, in the
direction of the axilla in search of the median nerve. The stimulation
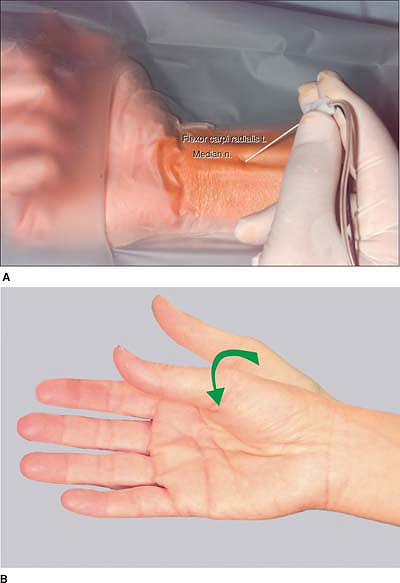
of the median nerve (Fig. 8-3A)
induces a contraction of the flexor carpi radialis and flexor digitorum
superficialis of the fingers (flexion of the fingers). Once this
response is obtained, the position of the needle is adjusted to
maintain the same motor response with a current of 0.3 to 0.5 mA. Then,
8 mL of local anesthetic is injected slowly. Next, the needle is
withdrawn to the skin, the current
is increased to 5 mA, and the needle is redirected in search of the ulnar nerve (Fig. 8-3B).
The stimulation of the ulnar nerve induces a contraction of the flexor
carpi ulnaris (flexion of the little finger and opposition of the
little finger and thumb). Once this response is obtained, the position
of the needle is adjusted to maintain the same motor response with a
current of 0.3 to 0.5 mA. Then, 8 mL of local anesthetic is injected
slowly. Next, the needle is withdrawn to the skin, the current is
increased to 5 mA, and the needle is redirected in search of the radial
nerve (Fig. 8-3C).
The stimulation of the radial nerve induces a contraction of the
extensor muscles, including the extensor radialis (extension of the
fingers and especially the thumb). Once this response is obtained, the
position of the needle is adjusted to maintain the same motor response
with a current of 0.3 to 0.5 mA. Then, 8 mL of local anesthetic is
injected slowly. To block the musculocutaneous nerve, the needle is
withdrawn to the skin and reintroduced in a superior and posterior
direction toward the coracobrachialis muscle. The stimulation of the
musculocutaneous nerve (Fig. 8-3D)
induces contraction of the biceps muscle (flexion of the forearm). Once
this response is obtained, the position of the needle is adjusted to
maintain the same motor response with a current of 0.3 to 0.5 mA (Fig. 8-4).
Then, 5 mL of local anesthetic is injected slowly. After disconnection
of the nerve stimulator, 3 mL of local anesthetic is injected
subcutaneously medially and laterally to the brachial artery to block
the medial cutaneous nerve of the arm and the medial cutaneous nerve of
the forearm.
 |
|
Figure 8-3.
An insulated needle connected to a nerve stimulator is introduced almost tangentially to the skin between the brachial artery and the palpating finger of the anesthesiologist, in the direction of the axilla in search of the median nerve. |
 |
|
Figure 8-4.
Once the stimulation of the musculocutaneous nerve induces contraction of the biceps muscle, the position of the needle is adjusted to maintain the same motor response. |
-
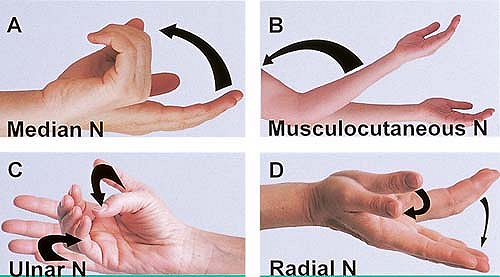
The intensity of the sensory block of the musculocutaneous nerve is tested on the lateral aspect of the forearm (Fig. 8-5B),
while that of the radial nerve is tested on the posterior aspect of the
forearm and hand, that of the ulnar nerve is tested on the medial
aspect of the hand (Fig. 8-5C) and little finger, and that of the median nerve is tested on the palmar side of the hand and of the second and third fingers (Fig. 8-5A). -
The onset of the block with ropivacaine occurs within 5 to 15 minutes.
-
This approach allows the different nerves to be blocked separately with only one cutaneous puncture point.
-
The high humeral block can be performed safely, effectively, and with a high success rate.
-
If the block is incomplete in one or more territories, it may be completed at the elbow or wrist.
-
The learning curve is steep. Speed and success increase quickly after only a few blocks.P.78
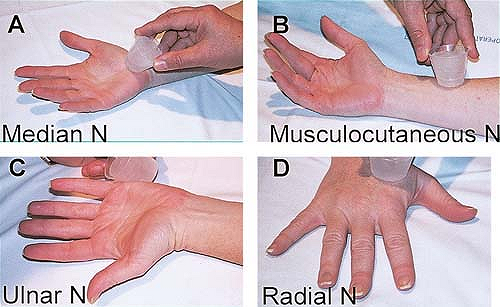 Figure 8-5.
Figure 8-5.
The intensity of the sensory block of the musculocutaneous nerve is
tested on the lateral aspect of the forearm, while that of the radial
nerve is tested on the posterior aspect of the forearm and hand, that
of the ulnar nerve is tested on the medial aspect of the hand and
little finger, and that of the median nerve is tested on the palmar
side of the hand and of the second and third fingers. -
The sequence in which the nerves are blocked is not important.
-
This approach also allows only the nerves
required to produce anesthesia in the surgical territory to be blocked
(hyperselective blocks). -
A block of different onset and duration
can be achieved by injecting at the level of each nerve a different
local anesthetic solution.
H, Narchi P, Mercier FJ, et al. Comparison between conventional
axillary block and a new approach at the midhumeral level. Anesth Analg 1997;84:1058–1067.
M, Pulcini A, Macchi P, et al. An evaluation of the brachial plexus
block at the humeral canal using a neurostimulator (1417 patients): the
efficacy, safety, and predictive criteria of failure. Anesth Analg 2001;92:194–198.
E, Kern O, Mahoudeau G, et al. Block of the brachial plexus branches by
the humeral route: a prospective study in 503 ambulatory patients.
Proposal of a nerve blocking sequence. Acta Anesthesiol Scand 1999;43:609–613.
H, Guillaume F, Dixmerias F, et al. The enhancement of sensory blockade
by clonidine selectively added to mepivacaine after midhumeral block. Anesth Analg 2001;93;771–775.
Anesthesia and immediate postoperative analgesia for forearm, wrist,
and hand surgery. To complete the block of a nerve performed at the
axilla or with a high humeral approach.
The median nerve is just medial to the brachial artery. The radial
nerve is just lateral to the biceps tendon at the intercondylar fold.
It is important to recognize that the radial nerve divides into a
sensory and motor branch 2 to 3 cm before the elbow crease. At the
elbow, the ulnar nerve runs between the medial epicondyle of the
humerus and the olecranon process of the radius in the ulnar groove.
finger on the brachial artery pulse, the insulated needle connected to
a nerve stimulator (1.5 mA, 2 Hz, 0.1 ms) is introduced
immediately
medial to the brachial artery at a depth of 1.0 to 1.5 cm in search of
a stimulation of the median nerve (flexion of the first three fingers) (Fig. 8-7).
The position of the needle is adjusted to maintain the motor response
with a current less than 0.5 mA. After negative aspiration for blood,
the local anesthetic solution is injected slowly.
 |
|
Figure 8-6. Anatomic landmarks.
|
 |
|
Figure 8-7. Median nerve block.
|
and marked. The insulated needle connected to a nerve stimulator (1.5
mA, 2 Hz, 0.1 ms) is introduced 2.0 to 2.5 cm lateral to the biceps
tendon at least 3 cm cephalad from the elbow crease in search of a
stimulation of the radial nerve (extension of the thumb) (Fig. 8-8). The position of the needle is
adjusted to maintain the motor response with a current less than 0.5
mA. After negative aspiration for blood, the local anesthetic solution
is injected slowly.
 |
|
Figure 8-8. Radial nerve block.
|
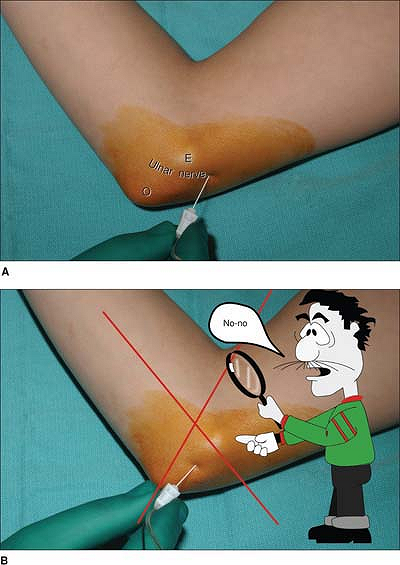
is flexed approximately 60°. The medial epicondyle of the humerus and
the olecranon process are identified along with the ulnar groove. A
25-mm insulated needle connected to a nerve stimulator (1.5 mA, 2 Hz,
0.1 ms) is introduced 2 to 3 cm cephalad to the middle between the
olecranon and medial epicondyle in search of a stimulation of the ulnar
nerve (Fig. 8-9A) (flexion of the fourth
and fifth fingers with opposition of the thumb). The position of the
needle is adjusted to maintain the same motor response with a current
less than 0.5 mA. After negative aspiration for blood, the local
anesthetic solution is injected slowly.
 |
|
Figure 8-9. Ulnar nerve block.
|
-
Injection of the local anesthetic
solution at the level of the ulnar groove should be avoided, because it
can cause compression of the nerve and postoperative paresthesia (Fig. 8-9B). -
Radial blocks performed at the level of
the elbow crease often produce an incomplete sensory block because at
this level the radial nerve is already divided into a sensory and motor
branch. -
Blocks at the elbow are easy to perform.
However, it is important to search for motor responses at the level of
the fingers and especially the thumb when blocking the radial nerve.
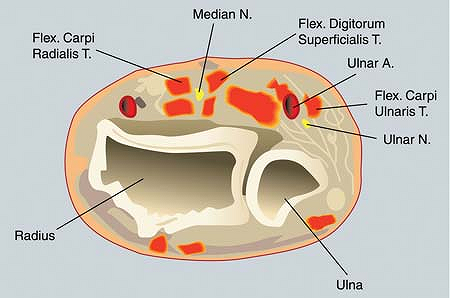
The ulnar nerve is located medially to the ulnar artery and posteriorly
to the flexor carpi ulnaris tendon. The median nerve is located
medially to the flexor carpi radialis tendon. The radial nerve is
located in the anatomic snuffbox.
25-mm insulated needle connected to a nerve stimulator (1.5 mA, 2 Hz,
0.1 ms) is introduced 0.8 to 1.5 cm immediately posterior to the tendon
in search of a stimulation of the ulnar nerve (Fig. 8-11).
The needle is positioned to maintain the motor response (flexion of the
fourth and fifth fingers with an opposition of the thumb)
with a current less than 0.5 mA. After negative aspiration for blood, the local anesthetic solution is slowly injected.
 |
|
Figure 8-10. Anatomic landmarks.
|
 |
|
Figure 8-11. Ulnar nerve block.
|
 |
|
Figure 8-12. Median nerve block.
|
sensory and therefore the block of the radial nerve is produced by
injecting the local anesthetic solution subcutaneously at the level of
the anatomic snuffbox using two injections (X shape) (Fig. 8-13).
 |
|
Figure 8-13. Radial nerve block.
|
-
Wrist blocks preserve most of the motor function of the fingers.
-
The use of a nerve stimulator is only helpful in performing an ulnar block.
-
The use of a nerve stimulator to block
the median nerve at the wrist is associated with a 20% to 30%
incomplete block because at this level the median nerve has already
divided into a motor and sensory branch (the motor branch running more
posteriorly).
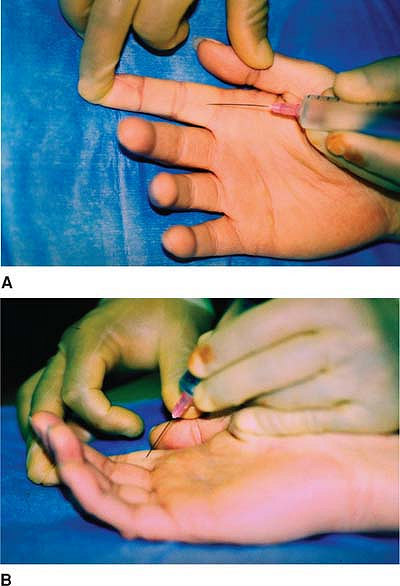
With the hand in full supination, the patient is asked to extend and
flex the fingers gently. The operator palpates the flexor tendon as it
glides over the protuberance of the metacarpal head and then marks it
with a skin pencil. The skin is penetrated at a 45° angle at the level
of the distal skin crease of the palm distal to the metacarpophalangeal
joint (Fig. 8-15A).
Resistance is felt as the needle penetrates the flexor tendon sheath.
The needle is then withdrawn slightly to sit above the tendon, at which
point the local anesthetic solution is injected with the operator’s
index finger pressing down on the flexor tendon proximal to the
metacarpophalangeal joint crease to prevent
proximal flow of the local anesthetic solution (Fig. 8-15B).
The bulging of the flexor tendon can be felt as the local anesthetic
solution flows freely. Pressure is applied at the injection site for 3
or 4 minutes.
 |
|
Figure 8-14. Anatomic landmarks.
|
 |
|
Figure 8-15. A: The skin is penetrated at a 45° angle at the level of the distal skin crease of the palm distal to the metacarpal joint. B:
The needle is withdrawn slightly to sit above the tendon, at which point the local anesthetic solution is injected with the operator’s index finger pressing down on the flexor tendon proximal to the metacarpophalangeal joint crease to prevent proximal flow of the local anesthetic solution. |
-
Lidocaine 1% is the local anesthetic of choice.
-
When anesthetic solution is injected, the patient may experience a feeling of finger expansion.
-
This block produces analgesia distal to
the palmar–digital crease that is more intense on the palmar side than
on the dorsal side. -
Considerable care must be taken to use
sterile techniques when performing this block to avoid contamination of
the flexor tendon sheath. In this regard, the hands of both the
operator and the patient should be disinfected with povidone-iodine,
then with alcohol. -
The onset of anesthesia is rapid, within 3 to 4 minutes of injection.
-
Compared with the conventional distal
nerve block technique, the risk for mechanical trauma to the
neurovascular bundle is minimal with this technique.
CK, Vartany A, Diao E. Comparison of transthecal and subcutaneous
single-injection digital block techniques in cadaver hands. J Hand Surg 1997;22:897–900.
