TENDON TRANSFERS IN COMBINED NERVE PALSIES OF THE FOREARM AND HAND
III – THE HAND > Conditions of Nerves > CHAPTER 58 – TENDON
TRANSFERS IN COMBINED NERVE PALSIES OF THE FOREARM AND HAND
Department of Orthopaedics and Rehabilitation, The University of New
Mexico Health Sciences Center, Albuquerque, New Mexico, 87131-5296.
severe functional loss. Multiple nerve palsies usually result from
extensive trauma. There may be skeletal instability with loss of normal
motion. Circulation is usually impaired, and the result is ischemic
pain and increased fibrosis. Muscle–tendon units are often lacerated
and sometimes avulsed; consequently, neuromotor function is impaired,
and the resulting fibrotic infiltration complicates normal muscle
function.
weakness and diminished sensibility but also poor proprioception on the
forearm and hand, with a loss of position sense and other normal
feedback mechanisms. As joints stiffen and muscles atrophy, maintaining
a mobile extremity without deforming contracture demands persistent
rehabilitation and meticulous splinting. The most important aspect of a
rehabilitation program is the patient’s acceptance of the
responsibility and initiative for recovery. Reconstructive surgical
procedures should not be undertaken until appropriate joint motion
returns and skeletal alignment is stable (18,25,29,31,33).
Sensibility loss is more profound in combined nerve palsies, and motor
return rarely passes two major joints distal to the injury (19).
Make nerve repairs as soon as clinically appropriate, but delay
surgical reconstruction to restore sensibility until all indicated
tendon transfers have been performed and the patient has supple tissues
with an established range of motion. Precise sensibility first requires precise motion (24,26,29),
which may be obtained through surgical reconstruction and focused
rehabilitation. The motion expected after tendon transfer cannot exceed
the passive motion present preoperatively.
should be synergistic with the anticipated postoperative action, or at
least retrainable by conscious control. Electromyographic studies
indicate that a new activity pattern can be developed to correspond
with a new mechanical function, but the old activity pattern is not
lost (42). Furthermore, the longer the surgeon waits for clinical nerve recovery, the more difficult it is to prevent gradual deformity.
those with neurapraxic lesions, may not regain normal strength for
elective transfer procedures (15). Previously repaired tendons may be used for transfer only under optimal conditions (7).
Reconstruction for combined nerve palsies is made more difficult by the
smaller number of motor tendons that are available to stabilize
residual function (9) or to provide additional function while awaiting potential nerve recovery following neurorrhaphy (5).
It is usually inappropriate, therefore, to use intact muscle–tendon
units as internal splints to enhance patterns of motion in combined
nerve palsies (20). Use as few transfers as
necessary. The objective of reconstructive surgery in the extremity
with combined nerve injuries is limited. Strive for a balanced,
functional hand, because tendon transfers redistribute existing assets
rather than create new ones (43). The motor muscle for transfer is selected on the basis of its current clinical function.
complicated than those in isolated nerve palsy for a number of reasons:
Extremity injuries are often complex; the patient has poor
proprioception and distorted sensibility; fewer muscles are available
for transfer and the ones that are available for potential transfer are
weak. In addition, combined palsies require multiple operations, and
longer follow-up time is required to make valid outcome-based decisions
regarding tissue or tendon transfer than in isolated palsies (24,26). (Principles for tendon transfers are presented in Chapter 54.)
of injury. Return of good muscle power across two joints distal to the
nerve injury is rare (24). Ongoing assessment
requires multiple quantitative tests that are repeated at regular
intervals of 3 to 4 weeks. They include the following:
-
A voluntary muscle test with recorded range of motion
-
A test for light-touch two-point discrimination distance over autonomous zones for pertinent peripheral nerves
-
A wrinkle test for sudomotor function
-
Gross grip and finger-pinch strength tests
-
Timed pick-up test for median or ulnar nerve lesions (24,33)
must have developed the cerebral imprint for the proposed neuromuscular
function to be reconstructed, and he must comprehend what is to be done
and accept the postoperative discipline for rehabilitation. If the
patient is an adult, it is relevant to determine whether he desires an
increase in functional performance or only cosmetic improvement.
either high or low injuries, can present at mixed levels, as in, for
example, a low ulnar and high radial palsy. A combined nerve palsy that
presents at mixed levels requires a systematic but individualized
approach. These unusual combinations are not discussed in this chapter.
Surgeons reconstructing extremities with multiple nerve injuries should
be experienced enough to select the appropriate procedures for each
individual case.
maintain the desired result. After either median or ulnar palsy, the
thumb–index web must be maintained to prevent thumb adduction and
supination contracture. Wrist extension is a priority in radial palsy (23).
Maintaining a mobile extremity without deforming contracture demands a
vigorous rehabilitation program. Use progressive static splints or
dynamic splints when full passive range of motion is not present. As
stated, the functional range of motion achievable after tendon transfer
depends on passive movement present before surgery.
homeostasis and equilibrium are present. Chronic wounds are
contraindications to elective surgery. Soft tissues should be free of
scar contracture. The timing of tendon transfers varies with the level
of the nerve injuries, as well as with the severity of the extremity
injury.
-
Position the patient supine with the involved extremity on an arm table.
-
Mobilize the motor muscle to protect its
neurovascular bundle, which usually enters the proximal third of the
muscle. The selected muscle–tendon unit should have amplitude adequate
for the anticipated motion (2). Reevaluate the texture, vascularity, and excursion of the selected muscle under direct vision at the operating table (28). -
Do not cross bare bone with the
transferred tendon. Muscle–tendon units that must move through fascial
planes, such as an interosseous membrane, must have as large an opening
in the fascia as practical. Place the muscle in the fascial window, as
the exterior muscle fibers will adhere to the edges of the window while
the interior muscle fibers will retain motion. If the tendon is placed
in the fascial window, it will bind fast and motion will be lost (17).
The motor muscle selected must be strong enough for its new task,
because it will have to pull itself free of the healing fibrosis after
surgery and will usually lose one grade of strength on Lovett’s
clinical scale (17). -
Select an appropriate moment arm for the direction of muscle–tendon action (8).
Most muscles are parallel to bone, and the angle of approach between
the transferred tendon and its insertion should be small. The greater
the angle of approach that the tendon takes to its insertion point, the
greater the force the muscle can exert, but the result is a
“bowstring.” When a pulley is required to increase the approach angle
to more than 45°, a loss of force secondary to friction occurs.
Eventually, a bowstrung tendon will shift to a straight line and then
become too slack for effective action. The more distal to the joint’s
axis of motion the transfer is anchored, the more force the muscle can
exert on the joint, but also the more excursion is required of the
tendon to provide a normal range of motion in the joint. If the
insertion of a transferred tendon is split, the motor will act
primarily on the slip under greater tension. -
A tendon transfer is more effective when
it crosses only one joint. If the tendon bowstrings across a proximal
joint, its mechanical advantage at that joint will be so great that it
may force that joint into unwanted movement or use up all its amplitude
so that it cannot move the distal joint. An example is the transfer of
the brachioradialis (BR) into the flexor pollicis longus (FPL): When
the elbow and wrist are extended, the patient can hold an object
tightly, but when the elbow is fully flexed, the muscle–tendon power is
dissipated at the elbow, and the patient drops the object. A second
example is an unstable bony nonunion where tendon transfers fail
because the telescoping skeleton prevents the development of adequate
amplitude for functional power. -
Use synthetic sutures for tendon fixation
to minimize tissue reaction. The suture can be relatively large, such
as 2-0 for forearm transfers. Some tendon ischemia is prevented by
inserting the suture through the center of the tendon and then circling
only half the tendon; when suturing along the length of the tendon,
protect circulation further by alternating these half-tendon circles
from side to side. Avoid “lacing” a transferred tendon into a group of
paralyzed muscle–tendon units; lacing creates bulk, with twist and
scar, and increases friction. Select a precise insertion point, and at
that point, suture a short length of the mobile paralyzed tendons and
the transferred tendons side to side to prevent a shifting moment-arm,
or “whipsawing,” of the tendons. Alternatively, leave the paralyzed
tendon in its bed and pass the transferred tendon across it, as can be
done with the flexor carpi ulnaris (FCU) to the extensor digitorum
communis (EDC). This is an oblique transfer, and there should be a
double line of nonabsorbable sutures to prevent shifting of the four
slips of the EDC. You can disconnect the paralyzed tendon from its
fibrotic muscle and connect it directly to the transferred muscle.
Complete excision of the paralyzed muscle mass, however, may bring
unwelcome hemorrhage and should not be done unless the paralyzed muscle
belly is causing deformity. -
Deflate the tourniquet when final tension
is set for the transfer so that muscle ischemia does not contract the
muscle to such a degree that the tension is set too loose. The tension
of a tendon transfer is best judged when the hand is in the position it
will assume when the transferred tendon contracts. For extensor
transfers, resting tension should be strong enough to passively hold
the extremity in functional position against gravity; at the same time,
be sure that the wrist has the potential for a normal arc of flexion.
Flexor tendons often cross more than one joint and should be fixed at
somewhat greater than normal tension against gravity. Appropriate
tension brings perception of the new muscle more readily into
consciousness, because stretch reflexes and other feedback mechanisms
are stimulated when opposing muscles work to restore the neutral
position of the extremity (4).
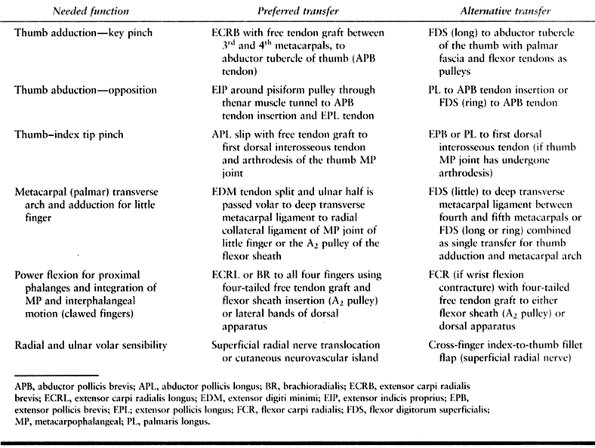
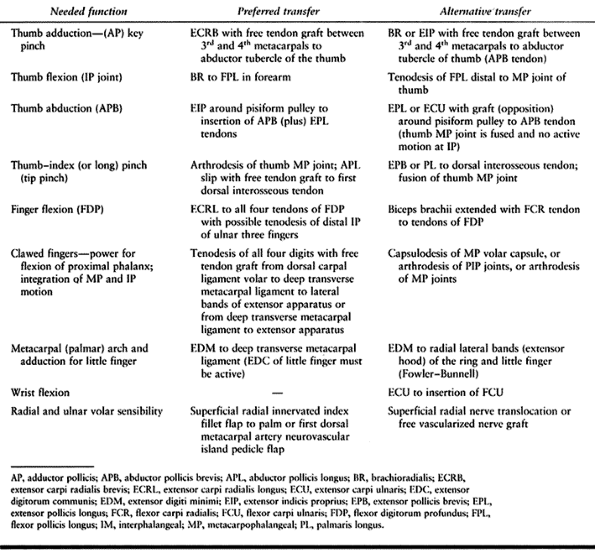
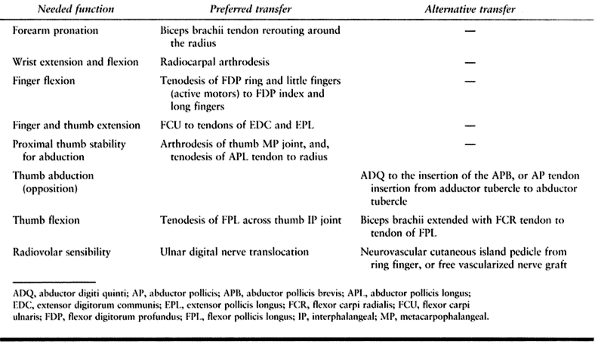
combined nerve palsy. The complete loss of palmar sensibility and
intrinsic motor muscles produce an almost useless claw hand (Table 58.1).
Examination demonstrates a flat transverse palmar or metacarpal arch,
with hyperextension at the metacarpophalangeal (MP) joints and
hyperflexion
at
the proximal interphalangeal (PIP) joints. An abducted little finger
may be associated with the flat transverse metacarpal arch. The patient
flexes the wrist to obtain greater finger extension, a functional
tenodesis, but with prolonged use the result is often a fixed flexion
contracture of the wrist. Do not attempt tendon transfers until
contractures have been corrected and the hand is mobile.
 |
|
Table 58.1. Combined Low (Distal) Median and Ulnar Palsy
|
immobilizing it in radiopalmar abduction. If possible, abduct the thumb
on a swivel splint (C-bar), which will add rotation to abduction and
prevent carpometacarpal joint contracture (27).
-
An inadvertent contracture can be
relieved by a Z-plasty of the skin web. A local dorsal free skin flap
may be necessary. If Z-plasty release is necessary, identify the
superficial radial nerve and preserve it for possible sensory
reconstruction. -
Excise tightened fascia over the thenar
intrinsic muscles. It may be necessary to strip the adductor pollicis
from the third metacarpal in fixed contractures. -
Additional strength in a palsied power
train requires a new muscle–tendon unit, and in median–ulnar palsy,
additional strength must be added by radial-innervated muscle–tendon
units (18,21,24,33). This is most important for the thumb. -
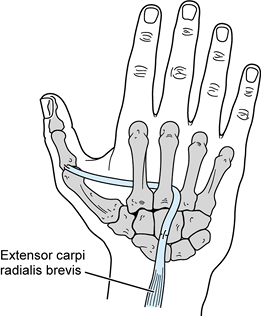
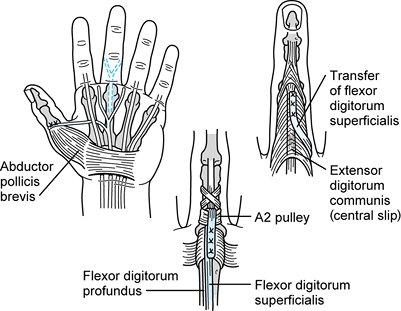
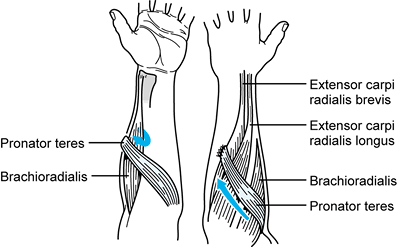
Use the extensor carpi radialis brevis (ECRB) to enhance thumb adduction for key pinch (Fig. 58.1) (38).
Through a dorsal longitudinal zigzag incision (1.5 cm) that extends
from the base of the third metacarpal to the dorsal retinaculum,
identify the ECRB and transect it at its insertion.![]() Figure 58.1.
Figure 58.1.
Transfer of the extensor carpi radialis brevis extended with a free
tendon graft to add power to key pinch, as well as to align and provide
power to wrist extension. -
Through a longitudinal incision between
the distal thirds of the third and fourth metacarpals, expose the
dorsal interosseous fascia and make a small window between the
paralyzed interosseous muscles. -
Harvest a tendon graft (palmaris longus
or plantaris). Attach this graft to the distal end of the ECRB and pass
it volarly between the third and fourth metacarpals into the palmar
space. A short incision in the palmar crease will identify the free
graft and the adductor pollicis muscle. Then tunnel the tendon graft
radialward just superficial (volar) to the adductor pollicis and deep
(dorsal) to the flexor tendons and neurovascular structures. Make a
short incision over the abductor tubercle of the first metacarpal.
Attach the graft to the fascia over the abductor tubercle of the first
metacarpal, and to the tendon of the abductor pollicis brevis, which
improves pronation. -
Test the length of the transfer graft.
With the wrist in dorsiflexion, the thumb should be against the palm;
with the wrist in palmar flexion, the thumb should fall into abduction. -
Postoperatively, immobilize the hand with the thumb in neutral position (not adducted) and the wrist in 40° of dorsiflexion (38). The average strength of key pinch is doubled by this operation (11,38).
-
Use the extensor indicis proprius (EIP) to increase thumb abduction and opposition (Fig. 58.2) (6,22).
Identify the EIP through a short dorsal longitudinal or small zigzag
incision over the MP joint of the index finger. If identified, preserve
the superficial radial nerve for sensory reconstruction.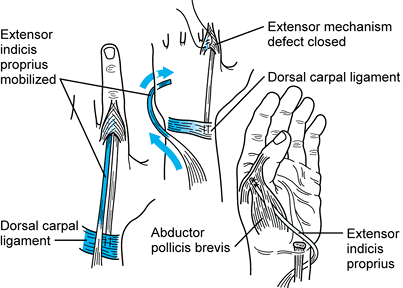 Figure 58.2. Transfer of the extensor indicis proprius to add power for abduction of the thumb.
Figure 58.2. Transfer of the extensor indicis proprius to add power for abduction of the thumb. -
Extend the EIP tendon by removing a slice
of the extensor apparatus in line with the tendon, and then
meticulously repair the extensor apparatus with nonabsorbable sutures. -
Make a short incision over the dorsum of
the hand distal to the dorsal retinaculum in line with the EIP tendon.
Free the EIP from the EDC to the index and deliver it into the forearm
longitudinal incision. Free the muscle bluntly from surrounding soft
tissues. -
Make a short transverse incision just
distal to the pisiform. Use a tendon passer to tunnel the EIP tendon
subcutaneously around the ulnar border of the forearm, using the
pisiform and its ligaments as a pulley. Apply intermittent tension on
the EIP tendon to assess the range of functional motion. -
Make a short incision along the radial
border of the thumb MP joint, and identify the tendon of the abductor
pollicis brevis (APB). Use a tendon passer to develop a subcutaneous
tunnel across the palm from the pisiform to the thumb MP joint. For the
patient anticipating considerable palmar pressure in daily activities,
make a short incision over the thenar muscle area and create an
intramuscular tunnel for the EIP tendon. The tunnel results in less
bowstringing across the base of the palm (17,21,22,27).
Attach the transfer to the APB tendon, the joint capsule, and the
extensor pollicis longus (EPL) over the proximal phalanx of the thumb.
Set the tension with the wrist in neutral flexion–extension and the
thumb in maximal abduction. -
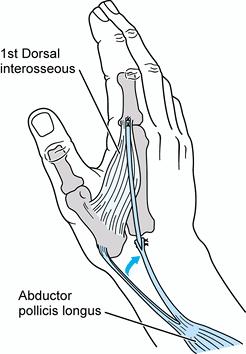
The abductor pollicis longus (APL) can provide additional second-MP-joint stability for thumb–index tip pinch (Fig. 58.3) (16,20).
Identify the slips of the APL at the radial styloid of the radius
through a short incision. Identify and protect the sensory branches of
the radial nerve. Distal to the dorsal retinaculum, identify the
extensor pollicis brevis (EPB). Then apply traction to each abductor
tendon to determine which one inserts on the metacarpal. Preserve this
slip and detach one of the remaining slips at its insertion. Obtain a
tendon graft
P.1674
from
the palmaris longus or plantaris. Make a short incision over the
insertion of the first dorsal interosseous tendon at the level of the
second MP joint. Suture the graft to the tendon of the first dorsal
interosseous muscle and pass it subcutaneously to the radial styloid
and suture it to the previously selected slip of the APL tendon.
Tension is proper when the index finger and the wrist are in neutral
position (16).
Follow-up studies indicate that tendon transfers to the first dorsal
interosseous muscle tendon do not add significant strength to pinch (31).![]() Figure 58.3. Transfer of the abductor pollicis longus extended with a free tendon graft to improve stability for thumb–index tip pinch.
Figure 58.3. Transfer of the abductor pollicis longus extended with a free tendon graft to improve stability for thumb–index tip pinch. -
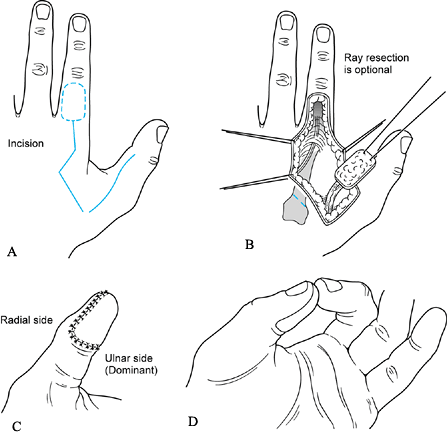
Arthrodesis of the MP joint of the thumb will strengthen both key and tip pinch (13). The chevron arthrodesis is the most effective procedure for fusion of the MP and PIP joints (Fig. 58.4) (17,35).
Through a dorsal longitudinal incision, widely expose the joint. Point
the apex of the chevron proximally. The apex of the distal bone is
perpendicular to the coronal plane of the bone. Angle the cuts of the
apex of the proximal bone to the desired degree of flexion at the
arthrodesis site. An appropriate position is 15° of flexion, 5° of
abduction, and some pronation so that the pulp of the thumb faces the
pulp of the index finger. Immobilize for approximately 8 weeks (35).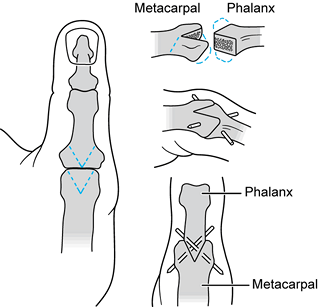 Figure 58.4. Arthrodesis of the metacarpophalangeal joint of the thumb utilizing a chevron-shaped mortise cut.
Figure 58.4. Arthrodesis of the metacarpophalangeal joint of the thumb utilizing a chevron-shaped mortise cut.
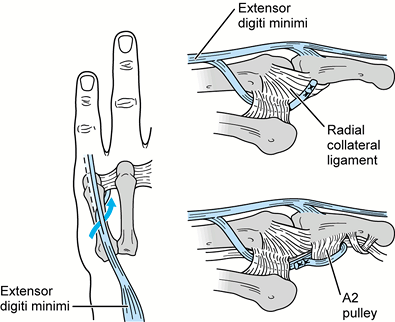
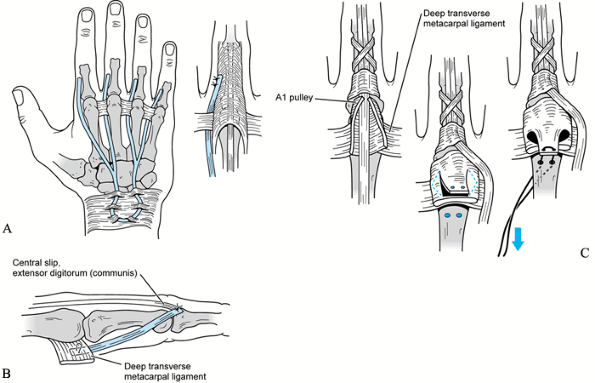
usually have a flat transverse (palmar) arch. The extensor digiti
minimi (EDM) has the potential to abduct the little finger through its
indirect insertion into the abductor tubercle on the proximal phalanx (Fig. 58.5) (1). The EDM, however, should not be transferred unless there is an active EDC to the little finger.
 |
|
Figure 58.5. Transfer of the ulnar half of the extensor digiti minimi to correct abduction of the little finger.
|
-
Make a longitudinal incision over the
dorsal aspect of the MP joint of the little finger. Detach the ulnar
half of the EDM from the dorsal apparatus and dissect proximally to the
distal edge of the extensor retinaculum (the dorsal carpal ligament).
Make a palmar incision obliquely from the distal palmar crease to the
proximal digital crease to expose the deep transverse metacarpal
ligament and the flexor sheath of the little finger. Pass the ulnar
half of the EDM between the fourth and fifth metacarpals into the
palmar wound. If the little finger is clawed as well as abducted,
insert the tendon slip into the radial aspect of the A1 pulley, or a radially based
P.1675
flap of the flexor tendon sheath just distal to the proximal pulley. -
If the little finger is not clawed, pass
the tendon slip beneath the deep transverse metacarpal ligament and
suture it into the phalangeal attachment of the radial collateral
ligament of the MP joint of the little finger. Set the tension with the
wrist in neutral flexion–extension and the MP joint in 20° of flexion.
Splint the ring and little fingers for 4 weeks with the wrist extended
and the MP joint flexed; leave the interphalangeal joints free to
prevent adhesions of the flexor tendons. -
The most reliable method for increasing
power for gross grasp is to add an extra muscle–tendon unit to the
power train for flexion of the proximal phalanges. Prolong the extensor
carpi radialis longus (ECRL) or the brachioradialis (BR) with palmaris
longus, plantaris, or toe extensor tendon slips (29,31) (Fig. 58.6) (see Chapter 58).
The junction between the ECRL and the tendon slip must be proximal
enough so that the suture site will not bind on the metacarpal shafts.
Pass the tendon slips superficial to the dorsal carpal ligament,
through the lumbrical space, and radial to the fifth, fourth, and third
metacarpal, but ulnar to the second metacarpal. Tunnel the free tendon
slips volar to the deep transverse metacarpal ligament (intervolar
plate ligament). If not passed correctly, the transfer will act only as
a radial deviator and will not control the hyperextension of the MP
joint. The slip insertion should be into the A2 pulley of the flexor sheath (Fig. 58.6D) or into the bone of the proximal phalanx (Fig. 58.6C)
for power flexion. If coordination of finger extension and flexion is
more important than flexion power, the insertion can be the lateral
band of the dorsal apparatus (Fig. 58.6B) (24). Identify the lateral bands of the dorsal apparatus or the A2
pulley of the flexor sheath with short longitudinal incisions. Suture
the tendons with the wrist dorsiflexed 45° and the MP joints flexed 60°
to 80°.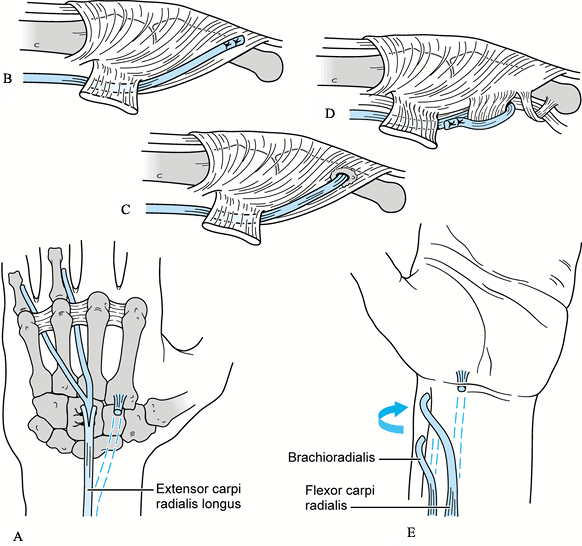 Figure 58.6.
Figure 58.6.
Transfer of the extensor carpi radialis longus with free tendon grafts
for power flexion of the proximal phalanx. Additional free tendon
grafts for the index and long finger (A)
should be added between the second and third metacarpals to achieve
full power of the transfer. (This addition is not illustrated.)
sensation. Motor reconstruction is concentrated on the thumb, but few
patients gain enough precise motor function to have good sensibility.
Methods for restoration of sensation include free nerve grafts, free
vascularized nerve grafts, digital nerve translocation, neurocutaneous
flaps,
neurovascular
cutaneous island pedicles, and free neurovascular cutaneous islands. We
prefer microsurgical digital nerve translocation and creation of a
neurovascular cutaneous island pedicle (10,28,31,40,41).
-
The brachioradialis (BR) also may be used to motor thumb adduction.
-
The most practical procedure in
median–ulnar palsy is translocation of the superficial radial nerve.
Expose the superficial radial nerve through a longitudinal zigzag
incision over the radial dorsal aspect of the index phalanx and dorsum
of the hand. Expose the nerve to the base of the thumb–index web, if a
Z-plasty of the web has not been done. Expose the ulnar proper volar
digital nerve of the thumb through a longitudinal incision. Translocate
the superficial radial nerve to the ulnar proper volar digital nerve of
the thumb using microsurgical techniques. A major advantage is that the
nerve translocation procedure may be done at the same time as the
tendon transfers for median–ulnar palsy. -
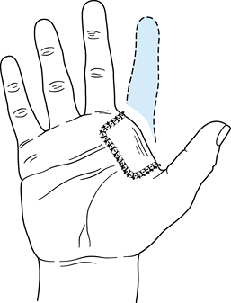
An alternative procedure to a nerve
translocation is to create a neurovascular cutaneous island pedicle.
Raise an island of skin over the distal third of the proximal phalanx
of the index finger (Fig. 58.7). The
superficial radial nerve and dorsal digital vessels form a
neurovascular bundle that is dissected proximally to the digital
artery. It may be necessary to ligate several anastomosing branches to
the volar digital artery (12,32).
Make an incision along the ulnar aspect of the thumb; elevate the
island with the neurovascular pedicle, and place it on the ulnar palmar
surface of the thumb. Many adult patients will perceive sensation as
coming from the donor site, but they will also make a cortical
adjustment and effectively use the miscued sensibility (29). Delay this procedure until tendon transfers have healed and initial rehabilitation is under way.![]() Figure 58.7. Neurovascular cutaneous island pedicle.
Figure 58.7. Neurovascular cutaneous island pedicle.
The most important clinical problem is the total loss of volar
sensibility, while atrophy of the finger pulps will discourage both
precision and power grip. If the other hand is normal, focus on
improving key pinch and simple grasp.
 |
|
Table 58.2. Combined High (Proximal) Median and Ulnar Palsy
|
and employ arthrodesis of the MP joint of the thumb to strengthen
thumb–index tip pinch. The surgical techniques are similar to those
used in low combined median and ulnar palsy.
-
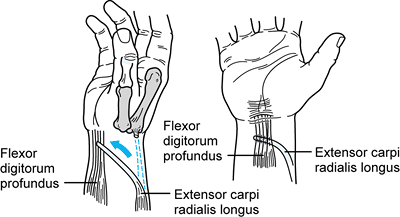
Use the ECRL for finger flexion (Fig. 58.8).
Make a midline longitudinal, slightly zigzag incision from a point
approximately 2.5 cm above the volar wrist crease to the proximal third
of the forearm. With traction, identify the tendon of the flexor carpi
radialis (FCR). On the radial aspect of this tendon is the radial
artery and the tendon of the BR. On the dorsal aspect of the FCR is the
flexor digitorum superficialis (FDS) and the flexor pollicis longus
(FPL). Tag the FPL, and displace the FDS ulnarward to reveal the flexor
digitorum profundus (FDP). Detach the ECRL at its insertion and release
it halfway or more up the forearm to obtain maximal muscle–tendon
motion. Tunnel the
P.1678
ECRL
around the radial side of the forearm across all four tendons of the
FDP, which is left in its usual position. Flex the fingers and align
them more transversely than obliquely to ensure equal tension for gross
grasp. The change in resting position is approximately 2 cm for the
index and long finger tendons. Suture the transfer well proximal to the
transverse carpal ligament to allow adequate and free excursion. Each
transfer junction has a proximal and distal suture to prevent
whipsawing under tension. Align tension so that there is functional
extension of the fingers with the wrist in 15° to 20° of flexion.![]() Figure 58.8. Transfer of the extensor carpi radialis longus to the flexor digitorum profundus for finger flexion.
Figure 58.8. Transfer of the extensor carpi radialis longus to the flexor digitorum profundus for finger flexion. -
Use the BR tendon to enhance thumb flexion (Fig. 58.9).
Identify the BR in the volar forearm incision and release it near its
insertion. Free it extensively from all tissue attachments so that it
has approximately 5 cm of passive mobility (28).
Also free the FPL so that it glides both proximally and distally to the
wrist. Weave the BR tendon into the tendon of the FPL, and secure it
with nonabsorbable sutures. Adjust tension so that there is full
extension of the thumb when the wrist is in 20° of flexion and the
thumb in full abduction (39). If thumb–index
tip pinch is unstable with MP joint extension and IP joint flexion (the
“crank-handle” effect), then thumb MP arthrodesis is indicated (3). As indicated previously, we routinely use arthrodesis of the MP joint of the thumb for the initial surgical reconstruction.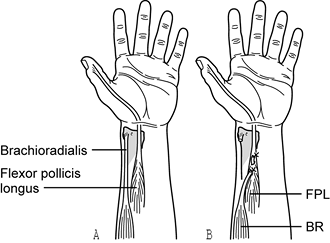 Figure 58.9. Transfer of the brachioradialis (BR) to the flexor pollicis longus (FPL) for thumb flexion. Both muscle–tendon units must glide freely before the anastomosis.
Figure 58.9. Transfer of the brachioradialis (BR) to the flexor pollicis longus (FPL) for thumb flexion. Both muscle–tendon units must glide freely before the anastomosis.
the intrinsic function will not be necessary, but when flexion is
restored to the IP joints, the fingers will gradually assume a clawed
position. Static techniques are used in most cases. Riordan (36)
credits Fowler for developing a tenodesis of all four fingers utilizing
free tendon grafts from the dorsal carpal ligament passed volar to the
deep transverse metacarpal ligament to the lateral bands of the
extensor apparatus (Fig. 58.10A). Wrist flexion increases the tension on the tenodesis so that the function is semiactive. Parkes (34)
placed a free tendon graft between the radial lateral band of the
dorsal apparatus of the finger and the deep transverse metacarpal
ligament (Fig. 58.10B). Riordan (37)
split the FDS of the long finger into four slips; one slip is passed
through the lumbrical canal of each finger and inserted into the
lateral band of the dorsal apparatus. Zancolli (44) opened the proximal (A1) pulley of the flexor sheath and excised a flap from the volar plate (Fig. 58.10C).
 |
|
Figure 58.10. A:
Dynamic dorsal tenodesis to control claw finger deformity. The free tendon to the index finger may be inserted on the ulnar side when increased index and long finger adduction for pinch is important. B: Static tenodesis to control claw finger can be obtained by using a free tendon graft or slip between the radial lateral band of the dorsal apparatus of the finger and the flexor retinaculum (deep transverse metacarpal ligament) in the palm. The grafts function independently in each finger. C: A Zancolli capsulodesis of the metacarpophalangeal (MP) joint to correct finger clawing. |
reconstruction of sensibility in this lesion. Two procedures to
transfer sensibility to the thumb are described in the section on low
median–ulnar nerve palsy. Sensibility can be transferred to the radial
volar aspect of the hand (Fig. 58.11). Careful
testing of the superficial radial nerve will demonstrate the distal
level of sensibility on the dorsum of the index finger.
 |
|
Figure 58.11. Fillet of index finger, with larger radial-innervated cutaneous island.
|
-
Remove the skeleton of the index finger
distal to the proximal third of the second metacarpal. Discard the
insensitive distal skin. Then fit the filleted index finger flap into
an additional volar defect created for it in the insensitive palmar
skin (29,31,32). This procedure will provide protective sensibility within the thumb–middle web space.
radius secondary to the concentration of extrinsic forces to the radial
side of the hand (26,29). A sequela of the carpal change is a decrease in the thumb–index web space, with loss of ability to grasp larger objects.
sensibility, and reconstruction is useful to improve function. Surgery
is often staged, however, and rehabilitation is difficult because
surgical procedures need to be performed
both for finger extension and flexion and for thumb adduction and abduction (Table 58.3).
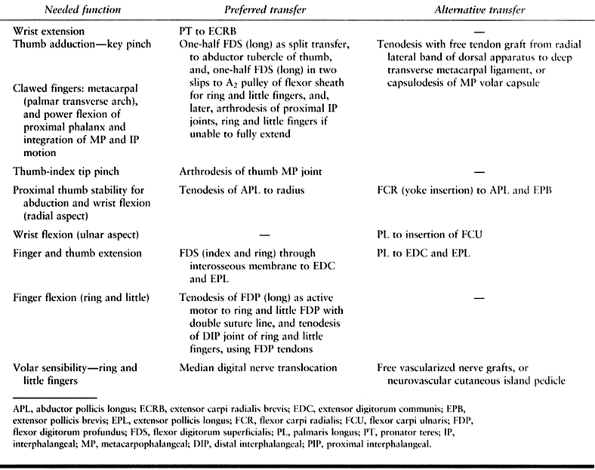 |
|
Table 58.3. Combined High (Proximal) Ulnar and Radial Palsy
|
A major function of the PT transfer to the ECRB is stabilization of the
wrist. Increasing dorsal extension power of the wrist by an increment
of one may increase power grip three to five times (5).
 |
|
Figure 58.12. Transfer of the pronator teres to the extensor carpi radialis brevis for wrist extension and stabilization.
|
-
Through a longitudinal incision on the
volar side of the radial aspect of the middle third of the forearm,
expose the tendons of the PT, ECRB, and ECRL. Free the PT with a
generous tongue of periosteum from the radius. Bluntly free the PT
muscle belly, avoiding neurovascular injury. Pronate the forearm, and
pass the PT subcutaneously and superficial to the BR and the ECRL
muscle for attachment to the tendon of the ECRB. The wrist should rest
in 30° of extension against gravity. -
Utilize the long FDS to improve the
integration of MP and interphalangeal joint flexion, key pinch for the
thumb, and the flattened metacarpal arch (Fig. 58.13) (22,24,30).
The ring finger FDS cannot be used when the ulnar-innervated portion of
the FDP is paralyzed. Expose the long finger FDS through a volar zigzag
incision
P.1680
that
extends from the PIP crease to the distal palmar crease. Release of the
long FDS may result in a residual hyperextension deformity of the PIP
joint. To prevent this problem, release the distal radial insertion of
the FDS proximal to the PIP joint and perform tenodesis to prevent
hyperextension of the joint after completion of the transfer. Release
the ulnar half of the FDS at its terminal insertion. Retain the flexor
sheath, especially the proximal A1 and A2 pulleys. The ulnar half of the long FDS tendon is split longitudinally again into two slips.![]() Figure 58.13. Transfer of the long flexor digitorum superficialis (FDS) for thumb adduction and opposition, and to prevent clawing of the ring and little fingers.
Figure 58.13. Transfer of the long flexor digitorum superficialis (FDS) for thumb adduction and opposition, and to prevent clawing of the ring and little fingers. -
When increased power for grip is desired
and the EDC will extend the PIP joint with the MP joint stabilized in
flexion, insert a long FDS ulnar slip into each A2 pulley of the ring and little fingers (Fig. 58.13). Make a longitudinal zigzag incision on the volar side of the little and ring fingers. Expose the proximal edges of
P.1681
the flexor sheaths and pass the FDS ulnar slips distally through the flexor sheaths and volarly around the distal edge of the A2 pulley and suture them in place. The A2 pulley insertion does not extend the PIP joint, while active flexion returns to the MP joint of the ring and little fingers. -
Extension of the fingers is usually weak,
however, or absent in high combined ulnar and radial palsy. If
preoperative testing indicates that the interphalangeal joints cannot
be actively extended by the EDC when the MP joint is flexed, then
insert the FDS slips into the dorsal apparatus (24,30).
Make short longitudinal incisions over the dorsal aspect of the PIP
joints of the right and little fingers. Direct the FDS ulnar slips
radial to the ring and little fingers and volar to the deep transverse
metacarpal ligament and then dorsally to be sutured at the insertion of
the central slip of the dorsal apparatus on the middle phalanx (Fig. 58.13). Traction on the transferred FDS slips should flex the MP joints and extend the PIP joints. -
Expose the abductor tubercle of the thumb
through either a short longitudinal incision over the tendon of the
APB, or a midline dorsal longitudinal incision for arthrodesis of the
MP joint. Arthrodesis of the thumb MP joint gives improved strength for
grip. Direct the radial half of the long FDS transversely over the
volar surface of the adductor pollicis, but dorsal to the flexor
tendons and neurovascular structures. Suture it into the insertion of
the pollicis brevis (PB) tendon. The functional mechanism of this
tendon transfer is similar to that of the Bunnell “tendon T” operation (20),
except that the pulley for this transfer is the distal edge of the
palmar fascia inserted into the third metacarpal rather than a free
tendon graft between the first and fifth metacarpals. Traction of the
transferred long FDS tendon should adduct and pronate the first
metacarpal, as well as increase the metacarpal (palmar) arch and
depress the clawed fingers (30). -
Use the index and ring FDS tendons to extend the fingers and the thumb (2,26) (Fig. 58.14).
Expose the FDS tendons through volar zigzag incisions that extend from
the PIP crease to the transverse palmar crease. Release the distal
radial insertion of the FDS tendon proximal to the PIP joint and
perform tenodesis to prevent hyperextension, or divide the FDS tendon
proximal to the chiasma tendinum and deliver it into the longitudinal
incision on the volar side of the radial aspect of the forearm.
Proximal to the pronator quadratus, excise two windows from the
interosseous membrane, one on each side of the anterior interosseous
artery. The windows should be as large as possible for the patient’s
anatomy. If there is any indication of injury to either the anterior or
posterior interosseous vessels, deflate the tourniquet and control
hemorrhage. It is very difficult to establish hemostasis after the two
FDS tendons are placed through the interosseous membrane.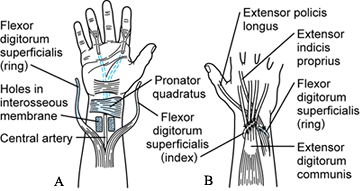 Figure 58.14.
Figure 58.14.
Transfer of the index and ring flexor digitorum superficialis tendons
through the interosseous membrane for finger and thumb extension. -
Make a J-shaped incision on the dorsum of
the forearm. The transverse arm passes from the radial styloid to the
ulnar styloid, with the longitudinal arm extending proximally on the
ulnar aspect of the dorsum of the forearm. Pass the two FDS tendons to
the dorsum of the forearm through the openings in the interosseous
membrane, with the index FDS to the radial side of the profundus muscle
group and the ring FDS to the ulnar side of the profundus group. Place
the muscle of both FDS units in the interosseous membrane windows,
because bare tendon will adhere with resulting loss of motion. If it is
not technically feasible to do so, route the FDS units subcutaneously
around both sides of the forearm. -
Attach the ring FDS to the EPL and the
EIP tendons. Suture the index FDS to the EDC tendons. Place the
junction well proximal to the dorsal retinaculum. If there is blocking
of the sutures against the dorsal retinaculum, narrow this fascial
band. Suture the index FDS obliquely across the tendons of the EDC
tendons with a double suture line to provide stability. The recipient
tendons are not divided proximal to the junction. Form a fist passively
with the wrist held in 45° of extension; then suture the tendons at
normal tension. With release of the fist, the digits should splay into
functional extension against gravity. The transfers must be tight
enough to provide extension, but not so tight that they limit
functional flexion of the fingers and wrist. Full flexion of the wrist
is uncommon.
by removing the FDS may ultimately result in either a flexion
contracture or a swan-neck deformity of these joints. Because it is not
possible to accurately predict which of these deformities will occur in
a given patient, we believe that it is preferable to wait for the onset
of deformity before treating it. The most predictable corrective
procedure may be arthrodesis of the PIP joint (13,25).
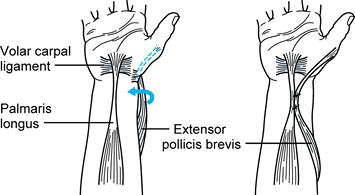
abduction of the first metacarpal may cause awkwardness and loss of
strong pinch. The FCR tendon can be split and inserted into the tendons
of the APL and the EPB and still retain wrist flexion (Fig. 58.15) (33).
We have seen this “yoke” insertion produce local irritation, however,
and we usually join the APL to the radius to provide a simple tether
for stability.
 |
|
Figure 58.15. Tenodesis of the palmaris longus and the extensor pollicis brevis to provide proximal stability of the thumb.
|
-
Increased flexion of the distal
interphalangeal (DIP) joints of the ring and little fingers may be
achieved by side-to-side tenodesis with the FDP of the long finger (Fig. 58.16).
Utilize a longitudinal incision on the radial volar aspect of the
forearm. Identify the tendons of the FDP; apply tension to the ring and
little finger tendons of the FDP until the finger pulps of all four
digits are in transverse alignment instead of the usual oblique
alignment. To maintain the transverse alignment, suture the tendons of
the inactive ring and little FDP tendons with nonabsorbable sutures to
the active long tendon of the FDP. The active index FDP is allowed
independent motion. A double line of sutures at the tendon junction
site is important to prevent whipsawing of the tendons during the power
grip. It may be appropriate to join the ring and little FDP tendons
across their DIP joints to eliminate one joint in the motion train.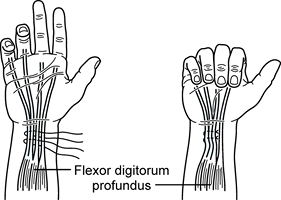 Figure 58.16. Tenodesis of the denervated long and little flexor digitorum profundus (FDP) tendons to the innervated index and long FDP tendons for active flexion of all four fingers.
Figure 58.16. Tenodesis of the denervated long and little flexor digitorum profundus (FDP) tendons to the innervated index and long FDP tendons for active flexion of all four fingers.
reconstruction. In high ulnar–radial palsy, patients have median
sensation and lack the precise ulnar motor function required for
precise sensibility. Delay any procedure until all tendon transfers
have healed and initial rehabilitation has been initiated.
and radial palsy will result in a hand that functions only slightly
more effectively than a prosthesis (24,25,31).
All wrist motors are lost except the FCU. Radiocarpal (wrist)
arthrodesis is indicated. When arthrodesis is performed on the wrist,
finger flexion is not enhanced by wrist extension, and the total range
of finger motion is limited (Table 58.4).
 |
|
Table 58.4. Combined High (Proximal) Median and Radial Palsy
|
-
The first priority in treatment is arthrodesis of the wrist, preferably using a low-profile plating technique.
-
Utilize the ulnar innervated portion of the FDP for flexion of the fingers and thumb (Fig. 58.17).
Approach the FDP through a longitudinal volar incision on the ulnar
aspect of the forearm. Because the radial portion of the FDP is
denervated, the FDP tendons to the index and long fingers must be under
greater tension than
P.1683
those
to the ring and little fingers. A double line of proximal and distal
sutures at the tendon junction is important to prevent shifting, or
whipsawing, of the tendons when a power grip is applied. After suture,
the finger pulps of all four digits are in transverse alignment instead
of the usual oblique alignment.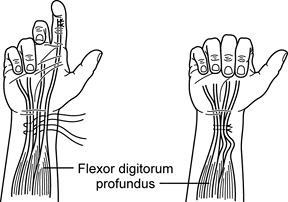 Figure 58.17. Tenodesis of the denervated index and long flexor digitorum profundus (FDP) tendons to the innervated ring and little FDP tendons for active flexion of all four fingers.
Figure 58.17. Tenodesis of the denervated index and long flexor digitorum profundus (FDP) tendons to the innervated ring and little FDP tendons for active flexion of all four fingers.
we have usually done the FDP “group suture” before tendon transfers for
finger extension. It is useful, however, to use dynamic finger
extension splits with intrinsic stops for appropriate positioning in
preparation for the surgical reconstruction of finger extension.
-
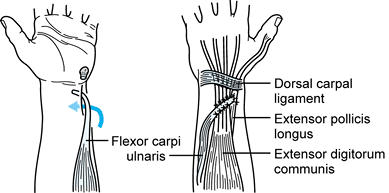
Utilize the FCU for finger and thumb extension (Fig. 58.18). The oldest surgical procedure for digital extension used the FCU (2). Through the incision described for the FDP modification, transect the FCU just proximal
P.1684
to the pisiform and free it up proximally to obtain appropriate passive
motion. A second longitudinal incision, 5–7 cm distal to the medial
epicondyle, will facilitate the release of the muscle. The limiting
factor in the dissection is the innervation of the FCU, which enters
the muscle in its proximal 5 cm.![]() Figure 58.18. Transfer of the flexor carpi ulnaris (FCU) to the extensor digitorum communis (EDC) and extensor pollicis longus (EPL) for finger and thumb extension.
Figure 58.18. Transfer of the flexor carpi ulnaris (FCU) to the extensor digitorum communis (EDC) and extensor pollicis longus (EPL) for finger and thumb extension. -
Make a dorsal longitudinal incision in
the midline of the forearm. Pass a tendon passer from the dorsal
incision subcutaneously around the ulnar border of the forearm, and
pull the tendon of the FCU into the dorsal incision. The FCU may need
to be passed back and forth, with careful observation and additional
dissection, plus release of subcutaneous tissues, to obtain a straight
pull from the medial epicondyle to the central portion of the dorsal
retinaculum. If there is excessive muscle bulk, the FCU muscle belly
can be trimmed distally; a bulky appearance, however, may be preferable
to excessive bleeding when the tourniquet is released. -
For finger and thumb extension, bring the
FCU well proximal to the dorsal retinaculum and suture it obliquely
across the tendons of the EDC and the EPL. Leave the extensor tendons
in their normal compartments, and place the FCU superficially across
each tendon with a double suture line for stability. When the EDC slip
to the little finger is absent, include the EDM in the tendon transfer.
The junction increases tension on the EDC tendon slips until the
fingers are held in a functional extension splay against gravity. -
After the tension is set for the EDC
tendon slips, add the EPL tendon as the final insertion of the FCU
transfer. Adjust tension against gravity so that the thumb fits into
the extension splay demonstrated by the digits. In high median–radial
palsy, however, finger flexion is inadequate, and the range of digit
extension should be more modest to fit the potential range of flexion.
Over time, and with balanced flexor tension, the patient can usually
extend all fingers, or only the thumb. The occasional patient learns to
show individual digits in extension through selective flexion (26).
These FCU transfer functional activities are much more specific in
isolated radial palsy, with normal wrist mobility and individual FDP
flexor motion (23). The fused wrist, however,
prevents radial deviation of the wrist, which is the most common
long-term problem in isolated radial palsy with an FCU transfer.
indicated only in special circumstances of functional need. Transfer of
the abductor digiti quinti for thumb abduction (the Huber operation) (14)
results in inadequate excursion, and it is questionable that total hand
function is improved, inasmuch as the little finger, with sensation
intact, has lost its ability to oppose. Transfer of the insertion of
the adductor pollicis from the adductor tubercle of the first
metacarpal to the abductor tubercle is almost as effective (the de
Vecchi operation) (25,31).
neurovascular islands, are not usually indicated in high median–radial
palsy. Patients with high median–radial palsy do not regain precise
sensibility, because there are so few remaining precision muscle motors
and it is difficult to balance the advantages and disadvantages of
digital nerve translocations. Finally, many adult patients do not have
cortical reorientation following surgical procedures to restore
sensation.
determine how much function has been lost and how much retained.
Interview the patient to determine whether she desires an increase in
function or in cosmesis. Document passive range of motion and initiate
therapy before surgery if there are limitations in motion. Static and
dynamic splints are useful to maintain or increase joint range of
motion. For example, if the thumb–index web space is narrowed, a static
thumb web spacer may be fabricated and adjusted serially until full
range of motion is obtained with a web space equal to the contralateral
extremity. Sensibility evaluation is important because defects
influence how the patients uses her hand. Conduct a functional
assessment to document sensibility loss.
palsies. It is important that the patient comprehend what is to be done
and be ready to accept the postoperative discipline. Biofeedback is
effective, and if possible, the patient should be able to palpate the
major muscles to be transferred. The preoperative goals of
rehabilitation are to maintain or achieve a supple hand and to enhance
remaining hand function.
of the hand that has undergone tendon transfer procedures is
identification of the points at which the relocated musculotendinous
unit crosses the wrist and the digital joints. During the early
postoperative period, direct splinting toward protection of the
transfer, correction of stiffness secondary to postoperative
immobilization, and controlled tension on the musculotendinous
transfer. Brand (3) has recommended placing the
hand in a volar slab cast with a very light unpadded cylindrical wrap
to make a circular support that holds the fingers in the appropriate
position during the postoperative period. A soft bulky dressing may be
added.
transfers to improve intrinsic muscle function. All indicated surgery
can be done at the same time. Immobilize the forearm in a light,
compressive, bulky dressing with a volar plaster splint. Hold the wrist
in 45° of extension,
the MP joints (except the thumb) in full flexion, and the IP joints in full extension.
reapply a molded splint to hold the position of the joints. Initiate
light strengthening at 8 weeks postoperatively. The MP arthrodesis of
the thumb is immobilized for at least 8 weeks (35). Allow unrestricted use at 12–14 weeks postoperatively.
as more distal joints. Postoperatively, hold the hand and forearm in
light, well-padded splints within a bulky dressing, with the wrist in
10° to 15° of extension, the thumb in opposition, the fingers supported
in a “straight-line” position of full MP flexion, and the IP joints in
10° of flexion. Support the elbow in 90° of flexion (Munster level) (28).
Start gentle active motion under supervision at 6 weeks
postoperatively. Initiate strengthening at 8 weeks postoperatively.
Elastic splinting can be used to support finger flexion, and static
splints can be used to support thumb opposition. Gradually, change
emphasis to functional use of the hand.
reconstruction: First, do thumb and little-finger intrinsic procedures;
second, do finger and thumb flexion procedures; third, correct residual
claw fingers. These steps can be done at 3-month intervals, followed by
any elective procedure for sensibility.
is difficult to retrain flexion and extension simultaneously; consider
staging the surgery for these cases. The first stage might include
wrist and digit extension procedures, plus thumb abduction. The second
stage might include digit flexion and thumb adduction. Arthrodesis of
MP or IP joints can be done in either surgical stage, or the surgical
stages could be reversed in order.
surgical reconstructions. If done in the order just mentioned, the
first phase is a radial nerve correction, and the wrist is immobilized
in 45° of extension, the MP joints in 15° of flexion, and the thumb in
maximal extension and abduction. Immobilize the elbow in a Munster-type
above-elbow cast with 15° to 30° of pronation, leaving the PIP joints
free. Remove the sutures at 14 days, but do not remove the long-arm
cast until 6 weeks postoperatively. Use removable short-arm splints to
hold the wrist, fingers, and thumb in extension.
intrinsic balance for the thumb, 12 weeks after the first phase. Hold
the wrist in 45° of extension, the MP joints in full flexion, and the
IP joints in extension (10° of flexion if tenodesis is done). Adduct
the first metacarpal so that it is parallel with the plane of the
second metacarpal. Maintain this intrinsic-plus position by
immobilizing in plaster for 4 weeks before resuming active extension.
appropriate rehabilitation and can be done in two stages. The first
stage might include arthrodesis of the wrist and the MP joint of the
thumb, as well as tenodesis of the APL tendon to the radius. The second
stage could be limited to finger and thumb extension, plus any elbow
surgery. Finally, the flexors could undergo tenodesis. Tenodesis of the
finger FDP flexor and the thumb FPL flexor requires protective support
against a stronger FCU extensor.
extremity after combined nerve palsies have occurred should be
experienced enough to select appropriate procedures based on the
individual case. The appropriate donor muscles will change with the
combination of nerve palsies and tissue equilibrium. Perform surgical
procedures to restore motor function before doing procedures to improve
sensibility, because precise sensibility requires precise motion. To
add strength, a new muscle–tendon unit must be placed in the power
train. The anticipated result should be a balanced simplification of
functional performance, because surgery and rehabilitation will
redistribute the few remaining assets rather than create new ones.
Motivated patients create successful surgeons, and the key to success
for these surgical problems is simplicity. Complexity invites failure.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
T, Tsuyama N, Furusawa S. An Attempt to Regain Sensations in the Median
Nerve by Transferring the Superficial Radial Nerve to the Median Nerve.
Operation 1973;27:551.
GE Jr. Reconstruction of the Forearm and Hand after Peripheral Nerve
Injuries. In: Omer GE Jr, Spinner M, Van Beek AL, eds. Management of Peripheral Nerve Problems, 2nd ed. Philadelphia: Saunders, 1998:675.
GW, Cobb T, Lewis RC. Transfer of Sensibility in the Hand: A New Method
to Restore Sensibility in Ulnar Nerve Palsy with Use of Microsurgical
Digital Nerve Translocation. J Hand Surg 1991;16:219.
RL, Stark IZ, Gubernick I, et al. Electromyographic Analysis of
Brachioradialis to Flexor Pollicis Longus Tendon Transfer in
Quadriplegia. J Hand Surg [Am] 1990;15:335.