Stress Fractures
overuse injuries seen in athletes. Stress fractures account for 10% of
the visits made to a sports medicine specialist. They were first
described by the Prussian military physician Breithaupt in 1885. He
called stress fractures of the metatarsal shaft, “march fractures.”
Stress fractures develop when excessive, repetitive loads are placed on
the bone without adequate periods of rest. This causes an increase in
osteoclast activity, which creates an imbalance between bone resorption
and bone formation. The osteoclasts resorb bone, and the osteoblasts
form new bone. This metabolic imbalance with greater osteoclast than
osteoblast activity is called a fatigue fracture. Stress fractures are
more common in weight-bearing activities, especially running and
jumping activities. More than 90% of stress fractures occur in the
lower extremities. In nature, only three types of animals get stress
fractures: race horses, racing greyhounds, and humans.
stress. Wolf’s law states that bone develops the structure and form
that is most suited to resist the forces acting on it. Thus, the
mechanical strain and forces on the affected bone influence bone
remodeling. Both cancellous and cortical bone remodel throughout their
life cycle. A bone’s response to stress is a function of multiple
factors: number of loading cycles, cycle frequency, amount of strain,
strain rate, and strain duration/cycle. How effectively bone responds
to stress depends on the subject’s metabolic state, nutritional status,
age, sex, ethnicity, and level of fitness. Tensile forces create a
positive electrical charge and stimulate osteoclasts and bone
resorption. Compressive forces create a negative electrical charge and
stimulate osteoblasts and new bone formation.
literature as to whether or not women sustain a higher number of stress
fractures than men. Military studies show that male recruits sustain a
stress fracture rate of 0.9% to 4.7%. Female recruits sustain stress
fracture rates between 1.1% and 13.9%. However, studies comparing
stress fracture rates between male and female athletes do not support
any gender difference. These studies showed male athletes with a rate
of 0.54 stress fractures per 1,000 training hours, and females at 0.86
per 1,000 training hours. There was no significant statistical
difference between these rates.
person’s body type or characteristics, whereas an extrinsic risk factor
is any outside environmental variable. Some extrinsic risk factors are
training regimen, footwear, and training surface. Athletes who maintain
a high training volume are at increased risk for stress fractures.
Also, athletes who have abrupt increases in the duration, frequency, or
intensity of training are at greater risk of developing a stress
fracture. Sports medicine physicians often see this when athletes make
the jump from junior varsity to varsity or from high school to
college-level sports participation. Improper program design and
training errors are the most frequently encountered cause of stress
fractures. One study showed that training errors were responsible for
22.4% of all stress fractures. Another extrinsic risk factor is poor
footwear. Athletic shoes older than 6 months increase the risk of an
athlete developing a stress fracture; however, the more shock-absorbing
ability a pair of running shoes has, the greater the decrease in an
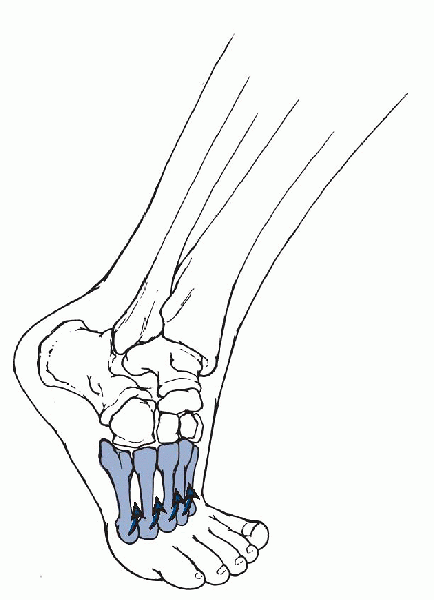
athlete’s risk of getting a stress fracture (Fig. 9-1).
Often, the higher the price of the shoe, the more powerful is the
shoe’s ability as a shock reducer on the user. Just as more cushioning
in the footwear can reduce the force on the runner, so can the type of
training surface. Harder, less compliant surfaces—like cement,
pavement, and asphalt—increase the risk of stress fracture when
compared with rubberized tracks, grass, and sand. Uneven terrain also
increases one’s risk for developing a stress fracture.
 |
|
Figure 9-1
The loads on the metatarsal heads during gait produce bending moments in the metatarsal bones that may contribute to stress fractures. (From Oatis CA. Kinesiology: The Mechanics and Pathomechanics of Human Movement. Baltimore: Lippincott Williams & Wilkins, 2004.) |
one’s risk for developing a stress fracture, there are even more
intrinsic factors. Some examples of intrinsic risk factors are gender,
age, race, foot structure, nutrition status, and many more. Women are
at greater risk than men for developing femoral, metatarsal, or pelvic
stress fractures. Data from the military show that white individuals
are at greater risk than black individuals for stress fractures.
Athlete data are more limited, but the results suggest the same
conclusion. One study showed two times increased risk of stress
fractures in whites. There has been conflicting evidence about the role
the age of an athlete plays with regard to stress fractures. One
retrospective study looked at 20,422 military recruits and found a
positive association between increasing age (17 to 34 years) and the
incidence of stress fractures in both men and women. This meant that as
the age of a military recruit rises, so does the risk that he or she
will develop a stress fracture. However, a later study showed that for
each year of age increase between ages 17 and 26, the risk for all
stress fractures decreased by 28% per year.
affect an athlete’s risk for stress fractures: bone mineral density
(BMD), bone geometry, and foot structure. BMD relates to the quality of
the bone present in an athlete. Low BMD has been clearly shown to be
associated with an increased risk of stress fracture. Studies have
found that lower BMD in the lumber spine, femoral neck, total hip, and
foot were significant predictors of stress fracture development in both
male and female track and field athletes. Bone geometry refers to the
amount of force a bone can withstand based on its cross-sectional area
and cross-sectional moment of inertia. The wider a bone’s
cross-sectional area and cross-sectional moment of inertia, the more
force the bone can handle. One study of military recruits revealed that
31% of recruits with femoral, tibial, or foot stress fractures had
narrower medial to lateral tibial widths than the recruits who did not
sustain a stress fracture under identical training conditions. Tibial
moment of inertia as measured on x-rays correctly predicted 92% of
stress fractures during the first year of military training in male
recruits. This concept is presently being studied in the athletic
population. No clear relationship has been found between an
individual’s specific foot structure and his or her risk for developing
stress fractures. Foot type does have an effect on what type of stress
fracture an individual is at greater risk for developing. A pes cavus,
or high-arched, foot absorbs less stress and transmits greater force to
the tibia and femur. A pes planus, or lowarched, foot absorbs more
stress in the foot itself, placing those bones at greater risk for a
stress fracture. This is a correlation between pronated feet and tibial
stress fractures and cavus feet with metatarsal and femoral stress
fractures.
had a lower intake of calcium compared with those without stress
fractures. The Recommended Daily Allowance for calcium is 1,000 mg/day;
but, for athletes, there is much debate about whether or not this
amount is too low. Athletes should aim for 1,200 to 1,500 mg of
calcium/day, as well as for 400
to 800 IU of vitamin D/day. Vitamin D increases calcium transport, stimulates osteoblasts, and decreases parathyroid hormone.
disorders, and stress fractures. Female runners with a history of
stress fractures are more likely to have a history of oligomenorrhea or
amenorrhea. Menarche is the age at which a female first begins
menstruating. The long-term effects of delayed menarche are unknown.
One study of female college distance runners revealed that 50% had
irregular menstrual cycles. Some of the potential complications are
osteopenia, stress fractures, and scoliosis. Estrogen deficiency at any
age lowers bone mass. Lower fat intake per kilogram of body weight was
more likely to sustain a stress fracture. There is still a lack of
large prospective longitudinal studies on the effect of hormone
replacement or birth control therapy pills on BMD in young female
athletes.
that is important for the maintenance and/or improvement of bone
health. Physical inactivity is associated with bone loss, osteopenia,
and osteoporosis. Resistance training has a more profound site-specific
effect than aerobic exercise. Cross-sectional studies performed on
female athletes show that resistance training is positively correlated
with bone density. Females who combined aerobic and strength training
had a higher lumbar spine BMD when compared with control subjects who
participated in aerobics without resistance training. One study showed
that children who engage in modest physical activity had a higher BMD
than their sedentary peers.
-
Taking a proper history and physical examination is vital for early diagnosis of a stress fracture.
-
No matter the site of the stress
fracture, there are some common threads that are found in both the
history and the physical examination. -
There is usually an insidious onset of pain over a 2- to 3-week period or even longer.
-
At first, the athlete recalls the pain
only appearing at the end of a contest or practice, and the pain
quickly resolves with rest. -
As time passes, the onset of pain is
earlier and earlier in the practice or game, and it needs more and more
rest before it goes away. -
The pain finally becomes so severe that
the athlete needs to modify his or her activity or else he or she will
be unable to compete. -
Eventually, minimal activity causes pain even with the athlete having stopped sports participation.
-
-
Often, the onset of pain correlates with a recent change in training habits or equipment.
-
An athlete may have dramatically
increased his or her mileage, may have changed his or her running
shoes, or may have started running on asphalt instead of the school
track.
-
-
The pain is localized to the area of the body receiving the repetitive stress.
-
There is no history of an acute or traumatic event.
-
Careful nutrition and menstrual history should be obtained for all female athletes.
-
The hallmark of the physical examination is tenderness over the affected bone.
-
There may or may not be localized edema around the stress fracture site, but rarely is a deformity seen at the site.
-
One study of stress fractures showed that
66% of the patients had localized tenderness over the fracture site,
whereas only 25% had soft-tissue swelling.
-
-
Percussion of the bone at a site away from the actual stress fracture may produce pain.
-
Functional testing, such as hopping on one foot, may elicit pain.
-
Three of the most common imaging studies
to use in the diagnosis of a possible stress fracture are plain films,
triple-phase bone scan, and magnetic resonance imaging (MRI).
-
Plain radiographs are normal during the
initial 2 or 3 weeks that an athlete develops symptoms. In fact, they
may not reveal any abnormal findings for several months. -
Seventy percent of plain films are normal in patients who are ultimately diagnosed with a stress fracture.
-
Abnormal findings on a plain film are
usually a thin incomplete radiolucent fracture line, a fluffy
periosteal reaction, or a thin linear area of sclerosis that is
perpendicular to the major trabecular lines. -
A positive plain radiographic finding is usually cortical bone, periosteal reaction, cortical lucency, or a fracture line.
-
In cancellous bone, the findings are more subtle and consist of a bandlike area of focal sclerosis without periosteal reaction.
-
Triple-phase bone scans are highly
sensitive but lack specificity. They can detect increased uptake in a
bone as soon as 2 or 3 days after the onset of clinical symptoms. -
In contrast to stress fractures, shin splints are positive only in the delayed phase.
-
Acute stress fractures reveal clear, localized areas of increased uptake on all three phases.
-
As healing occurs, the flow phase returns to normal first, and then the pool phase reverts to normal.
-
Lagging behind clinical resolution,
activity on the delayed phase decreases over 3 to 18 months as the bone
remodels. For this reason, bone scans should not be used to monitor
healing and return to activity.
-
MRI has several advantages over the other imaging methods:
-
It has a sensitivity on par with bone scans but a much greater specificity.
-
It does not expose the patient to any ionizing radiation.
-
It takes a shorter imaging time than a triple-phase bone scan.
-
It gives a more precise anatomic location to the stress fracture site.
-
It allows for the determination of both the extent and the orientation of the stress fracture.
-
-
There are two stress fracture patterns seen on MRI—a bandlike fracture line and no clearcut fracture line.
-
The bandlike fracture line, which is more
common, is a low signal on all imaging sequences and is surrounded by a
larger, more poorly defined area of bony edema. The fracture line is
continuous with the cortex and extends into the medullary space.-
The high signal intensity of the surrounding edema decreases the longer an athlete has the symptoms.
-
-
The fracture pattern without the fracture line is called a stress response and represents an earlier stage in the evolution of the stress injury.
-
-
The MRI is a sensitive test for early detection of periosteal and marrow edema along a fracture line.
-
A stress reaction reveals only grade I or
II marrow edema and periosteal reaction, whereas a grade III or IV
means a stress fracture is present.
-
distance runners. Femoral neck stress fractures account for 5% to 10%
of all stress fractures. Femoral shaft stress fractures account for
slightly less than 5%. There are two distinct types of femoral neck
stress fractures: tension and compression. Compression stress fractures
occur on the inferior and medial cortex of the femoral neck.
Compression stress fractures are low-risk fractures and rarely
displace. Young, healthy patients are more likely to develop
compression fractures. As muscles tire, they lose their ability to
absorb stress, increasing the forces across the femoral neck and, over
time, creating the stress fracture. Tension stress fractures occur on
the superior cortex of the femoral neck. Tension stress fractures are
high-risk fractures because they have a tendency to displace.
-
Early diagnosis is extremely important in treating tension stress fractures because of this risk.
-
Patients with a femoral stress fracture
usually present with an insidious onset of pain in the groin, which
gets worse with impact loading. -
Athletes also have a painful hip range of motion on the affected side.
-
Femoral shaft stress fractures cause athletes to complain of mild deep thigh pain with weight-bearing.
-
Both the “hop” test and the “fulcrum” test are helpful in making the diagnosis of a femoral shaft stress fracture.
-
The most common site for a femoral shaft
stress fracture is the medial compression side of the femur at the
junction of the proximal and middle thirds of the shaft. -
The differential diagnosis for femoral
stress fractures should include muscle strains, bursitis, synovitis,
infection, neoplasm, slipped capital femoral epiphysis (SCFE), Perthes
disease, development dysplasia of the hip (DDH), and osteoid osteoma.
-
Patellar stress fractures are extremely rare.
-
The differential diagnosis should include patellofemoral pain syndrome and patellar tendonitis.
are distance running, soccer, and basketball. The athlete usually
presents with a pain that progressively worsens in both intensity and
frequency. The pain is also aggravated by impact loading. Often, the
sports medicine physician may elicit a history of the athlete changing
his or her footwear, running surface, or increasing the training
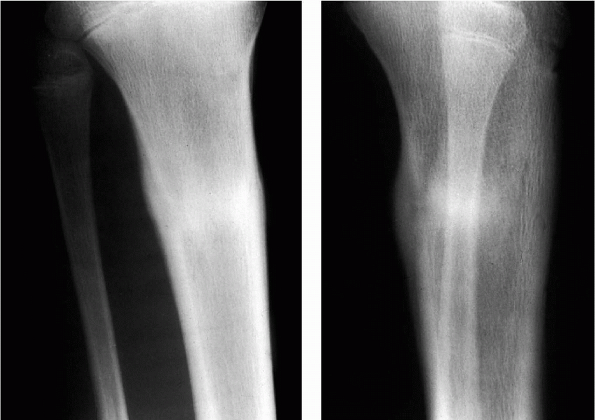
intensity, mileage, or frequency. The most common location for a tibial
stress fracture is at the junction of the middle and distal thirds of
the tibia in the posteromedial cortex, the compression side of the
tibia (Fig. 9-2). Less common, but more
concerning, areas for stress fractures of the tibia are the anterior
cortex of the midtibia and the medial malleolus.
-
The sports medicine physician should evaluate the athlete’s gait for pronated feet.
-
The differential diagnosis for tibial
stress fractures should include nerve entrapment, muscle strains,
popliteal artery compression syndrome, shin splints (medial tibial
stress syndrome), and exertional compartment syndrome.
distance runners. In particular, distance runners who train on hard
surfaces are at increased risk. The most common site on the fibula is
the distal third just proximal to the inferior
tibiofibular ligaments at the junction of cortical and cancellous bone.
 |
|
Figure 9-2
A stress fracture in a young male athlete. Note the sclerosis and widened cortices associated with bone healing. (From Bucholz RW, Heckman JD. Rockwood and Green’s Fractures in Adults, 5th ed. Lippincott Williams & Wilkins, 2002.) |
stress fractures are young men and middle-aged women. The young men
develop a stress fracture that is 5 to 6 cm proximal to the distal tip
of the lateral malleolus. In middle-aged women, the common site is 3 to
4 cm proximal to the malleolar tip. Fibular stress fractures that
develop in middle-aged women are usually because of metabolic problems
such as osteoporosis or osteopenia. Athletes who have a valgus hindfoot
have an increased risk of developing distal fibular stress fractures.
-
Surgery is seldom needed to treat a fibular stress fracture.
-
In most cases, immobilization in a short leg cast or boot for 6 to 8 weeks is sufficient.
majority of athletes who present with heel pain have a soft-tissue
injury and not a stress fracture. Calcaneal stress fractures are most
common in long-distance runners, military recruits, and older,
osteoporotic patients.
-
Patients present with tenderness and pain at the posterosuperior calcaneus just anterior to the apophyseal plate.
-
On physical examination, an athlete has
pain both dorsal and anterior on the calcaneal tubercle, as well as on
the medial and lateral sides of the heel anterior to the Achilles
tendon. -
Calcaneal stress fractures are usually
incomplete and show up as a vertical condensation within the cancellous
bone of the calcaneal tubercle. -
Radiographs taken 2 weeks or more after
the onset of symptoms usually reveal a sclerotic line perpendicular to
the trabecular stress lines in the posterosuperior aspect of the
calcaneus.-
This is the most common site for a calcaneal stress fracture.
-
A less common location is adjacent to the medial tuberosity on the calcaneus.
-
-
A sports medicine physician must have a high index of suspicion for a calcaneal stress fracture to avoid misdiagnosis.
-
Because plain films are usually negative, MRI is the diagnostic tool of choice.
-
The differential diagnosis for calcaneal
stress fractures should include plantar fasciitis, Achilles tendonitis,
and retrocalcaneal bursitis. -
Treatment is immobilization with a short leg cast or boot for 8 to 12 weeks.
primarily in runners, military recruits, dancers, and jumping athletes.
The classic location is at the talar neck, but they can also be found
at the lateral, posteromedial, and posterolateral parts of the talus.
In ballet dancers, the number one type of stress fracture is a
posterolateral talar fracture. There is a disruption of the
synchondrosis between the os trigonum and the posterior body of the
talus. The posterior impingement of the os trigonum against the
posterior tibia causes pain. This posterior impingement often occurs in
ballet dancers when they go into the en pointe position, which involves
dancing on one’s toes in hyperplantar flexion on the tibiotalar joint.
-
Plain radiographs are usually negative, and MRI is needed for definitive diagnosis.
-
The healing time for these stress fractures is usually 3 to 4 months.
basketball players, football players, soccer players, and runners.
Athletes usually describe an insidious onset of vague midfoot pain,
tenderness over the dorsum of the foot medially, tenderness on the
medial aspect of the longitudinal arch, foot pain that is worse with
activity, and pain that is reproduced by standing on one’s toes. The
most common site for a navicular stress fracture is at the junction of
the medial two-thirds and the lateral one-third of the bone. Navicular
stress fractures are the most difficult stress fracture of the foot and
ankle to treat. This is because the location of the stress fracture
corresponds to the zone of avascularity of the bone. The blood supply
to the navicular bone is an interosseous blood supply, which enters the
medial and lateral poles of the bone but diminishes in the zone where
the stress fracture usually occurs.
-
Athletes with a navicular stress fracture tend to present much later than with other lower-extremity stress fractures.
-
Plain radiographs rarely show navicular stress fractures.
-
The telltale sign is sclerosis in the subchondral bone adjacent to the talonavicular joint.
-
A computed tomography (CT) scan (or MRI)
is the imaging test of choice, since it can show the vertical fracture
line in the sagittal plane.
 |
|
Figure 9-3
Stress fractures of the metatarsal bones. These two radiographs show the progression of fractures from medial to lateral along the metatarsals in an insensate individual. (From Bucholz RW, Heckman JD. Rockwood and Green’s Fractures in Adults, 5th ed. Lippincott Williams & Wilkins, 2002.) |
occur most often in distance runners. The predisposing factor for
developing a cuboid fracture is an overload on the lateral column of
the foot, such as subtalar ankylosis or a varus hindfoot position. The
middle and lateral cuneiforms are most likely to develop a stress
fracture instead of the medial cuneiform because of the forces on the
foot transmitted through the second and third metatarsals. Both of
these types of stress fractures heal well because they involve
cancellous bone.
-
Treatment of both of these stress fractures is conservative.
-
A soft-soled, supportive shoe that is
custom-molded and cushioned to correct for any stiffness or varus
deformities in the patient should be worn.
fracture,” is more common in military recruits than in athletes.
Athletes participating in ballet, football, gymnastics, and basketball
are most at risk. Metatarsal stress fractures are the most common
lower-extremity stress fractures. The most common site is usually the
shaft (diaphysis or neck) of the second or third metatarsals (Fig. 9-3). Both pes cavus and pes planus feet are associated with an increased incidence of metatarsal stress fractures.
a short first metatarsal, a long second metatarsal, and a hypermobile
first metatarsal ray. This condition predisposes
an
athlete to a second metatarsal stress fracture. One study showed that
six of eight ballet dancers with stress fractures of the second
metatarsal had a Morton’s foot. Forefoot pain may be exacerbated by
running, jumping, or dancing; a callus is often felt.
metatarsal: a Jones-type fracture and a “dancer’s fracture.” A
“dancer’s fracture” is an acute fracture at the base of the fifth
metatarsal. This fracture at the proximal metaphysis is not a stress
fracture. However, a Jones fracture, named after Sir Robert Jones, is a
stress fracture at the metaphyseal-diaphyseal junction of the fifth
metatarsal. Jones stress fractures are more common in basketball and
football players.
-
Special care must be taken with the
proximal diaphyseal fifth metatarsal stress fractures because there is
a high incidence of nonunion due to poor blood supply. -
Plain radiographic films are usually negative so treat symptomatic patients conservatively.
-
Immobilize the patient to strict non-weight-bearing in a short leg cast for a minimum of 6 weeks.
-
If patient has persistent, unresolved
pain, is an elitelevel athlete, develops an established pseudarthrosis,
or fails conservative treatment, then operative intervention is
indicated. -
Differential diagnosis for metatarsal
stress fractures should include Morton’s neuroma, Freiberg’s
infraction, and metatarsal phalangeal joint instability.
They are seen in all active populations. In particular runners,
football players, golfers, and gymnasts are at increased risk. The
mechanism for injury is during weight transfer onto the medial column
of the forefoot. There is very little soft-tissue padding in this area.
The medial sesamoid bone is more likely to develop a stress fracture
because it is the larger of the two sesamoid bones.
-
An athlete usually presents with a story
of insidious onset of medial forefoot pain, which gets worse with
jumping, running, and toe-off activities. -
Usually, the patient presents with pain
on palpation of the sesamoid bones, as well as pain with dorsiflexion
of the metatarsophalangeal joint of the great toe. -
Plain radiographs using a metallic marker
over the area of pain using anteroposterior and sesamoid views may be
helpful in visualizing the stress fracture. Otherwise, an MRI is the
imaging method of choice. -
Conservative treatment is the primary method of choice.
-
The athlete uses off-loading orthoses, a protected weight-bearing cast, or a boot.
-
Surgery is needed only if conservative management fails.
-
Surgery consists of the excision of the
offending sesamoid bone and reconstruction of the flexor hallucis
brevis and intersesamoid ligaments.
occur more often in women than in men. The primary stress fracture site
is in the inferior pubic ramus adjacent to the symphysis pubis.
-
The athlete presents with groin pain that is exacerbated by activity.
-
The symptoms of a sacral stress fracture may mimic that of a herniated disc.
-
An athlete may complain of low back and sacral pain that radiates into the buttocks.
interarticularis is called a spondylolysis. Stress fractures of the
pars interarticularis are seen primarily in adolescents involved in
gymnastics or dancing. This is a fatigue-type injury that occurs
secondary to repetitive microtrauma. The mechanism is chronic and
repetitive loading of the lumbar facet joints due to hyperextension.
-
Athletes often present with low back pain made worse with hyperextension.
-
To confirm the diagnosis, an MRI or single-photon emission computed tomography (SPECT) scan is usually needed.
however, golfers and baseball players have also been found to be at
increased risk for rib stress fractures. In rowers, the ribs that are
usually affected are the fourth through the ninth. Rowing stress
fractures are usually associated with long-distance training. The
mechanism for a rib stress fracture is from the repetitive bending
forces on the ribs, especially in exhalation caused by the pull of the
serratus anterior and the external oblique muscles. During rowing, the
harmful position is believed to occur at the end of the drive phase,
with shoulder extension and scapular retraction. In golfers, it is the
posterolateral part of the rib in the leading side of the trunk that is
the most common site. As in rowers, the lower ribs are more at risk.
Electromyographic analysis of a golfer’s swing shows that the serratus
anterior is the primary force on the ribs during the swing. Golfers at
increased risk for developing a rib stress fracture are those with a
poor technique, those that take more strokes, and those who create
larger divots. First rib stress fractures have been reported in
baseball players.
-
Treatment of rib stress fractures is largely symptomatic.
-
Physical therapy focusing on strengthening and stretching of the serratus anterior is critical.
-
Also, addressing an athlete’s mechanics
of either his or her rowing form, golf swing, or baseball throwing or
hitting motion is vital.
-
Athletes report pain in the center of their chest.
-
Symptomatic treatment is all that is needed.
-
Treat athletes with rest, ice, anti-inflammatories, and avoid contact sports until pain-free.
-
Usually, it takes 6 to 12 weeks for an athlete to return to play.
throwing athletes. They may occur in the shaft of the humerus in adult
baseball players, especially pitchers. In skeletally immature throwing
athletes, stress fractures of the humerus may develop through the
proximal growth plate. The mechanism of injury is the creation of
opposing muscular contractions during throwing, which cause torsional
and tension forces on the growth plate. The muscles of the rotator cuff
are attached proximally to the physis, and the deltoid, pectoralis
major, and triceps all are attached distally to the growth plate.
-
Athletes complain of pain made worse by hard throwing.
-
On examination, there is usually focal
tenderness and discomfort to manual resistance to shoulder abduction
and internal rotation. -
In younger throwers, widening of the
lateral portion of the physis (growth plate) may be present on external
rotation anteroposterior radiographs. -
The radiographs may also show lateral fragmentation, sclerosis, or cystic changes of the humerus.
common in throwing athletes. Usually, this type of stress fracture is
more common in adolescents and kids. Olecranon stress fractures are due
to repetitive extension overload.
-
Patients complain of pain on the lateral border of the ulna.
-
On examination, the athlete experiences pain over the olecranon with resisted extension.
-
If this stress fracture is not recognized early, displacement can occur.
-
Plain radiographs show fractures only
occasionally. A CT scan or MRI is the best imaging study for viewing an
olecranon stress fracture. -
Conservative treatment is preferred.
-
Once point tenderness over the olecranon
ceases, athletes can begin light strength training on their triceps and
biceps, as well as rotator cuff exercises. -
If symptoms persist and conservative treatment has failed, then surgical intervention is needed.
-
A single axial large cannulated screw is inserted through the distal triceps tendon.
in which their upper extremity serves in weight-bearing. In about
one-third of cases, a gymnast has bilateral stress fractures.
-
On examination, the athlete has pain along the distal radial physis, with extremes of wrist dorsiflexion and axial loading.
-
Once the initial diagnosis of a stress fracture is made, a treatment plan must be implemented as soon as possible.
-
The first goal of treatment is to control the athlete’s pain using nonsteroidal anti-inflammatory drugs, ice, and stretching.
-
The two basic principles are rest and immobilization of the stress fracture site.
-
It is important to break the athlete’s cycle of destructive, repetitive trauma through rest.
-
Rest allows the reparative phase to dominate over the resorption phase helping the fracture to heal.
-
In general, at least 6 to 8 weeks are needed for most stress fractures to heal, although some may take longer.
-
-
For immobilization of the stress fracture, we use prefabricated braces, orthoses, and walking boots.
-
The advantage of these over casts it that
they can be removed, enabling the athlete to perform active
range-of-motion exercises to try and maintain muscle tone and bulk and
to reduce joint stiffness.
-
-
-
Surgery should be considered for bones in which a complete fracture can lead to long-term disability.
-
These troublesome bones include stress fractures of the tibia, the navicular, the fifth metatarsal, and the femoral neck.
-
-
A close look must be taken at the athlete’s nutritional status.
-
The sports medicine physician should
evaluate the athlete’s intake of calcium and vitamin D and determine
whether or not an eating disorder exists.-
If an eating disorder is uncovered, a multidisciplinary approach should be used.
-
-
In a female athlete, if abnormal menstrual patterns are identified, estrogen supplementation should be considered.
-
The treating physician must make sure there are no medical conditions present that may affect bone integrity.
-
-
For athletes looking to return to play,
there is a definite progression to the activities to which they are
allowed to participate.P.113-
The first conditioning allowed should be swimming, which is a non-weight-bearing activity.
-
Nonimpact exercise such as biking comes
next, followed by weight-bearing nonimpact activities like the
elliptical machine, cross country skier machine, and stair climber. -
The final activities allowed should be
weight-bearing impact exercises such as walking, progressing to jogging
and finally running.
-
-
At each specific activity, the duration should progress from short to long, and the intensity level from low to high.
-
For each impact activity, an athlete
should have a pain-free progression from low intensity-short duration
to low intensity-long duration to high intensity-short duration to high
intensity-long duration before advancing to the next impact activity
level. -
Only after this complete, pain-free progression over at least 6 to 8 weeks can an athlete return to his or her sport.
-
In compression-type stress fractures of
the femoral neck, the patient should be made non-weight-bearing with
crutches until the patient is pain-free and has full range of motion.-
Usually, this is at least 4 to 6 weeks.
-
-
Athletes are allowed to return to sports
only when they are pain-free, have a full range of motion, and
radiographs show evidence of a healed fracture. -
If the fracture becomes complete or does not heal with non-weight-bearing and conservative management, pinning is recommended.
-
For tension-type stress fractures of the femoral neck, athletes should have surgical intervention.
-
Tension-type stress fractures have a high likelihood of becoming displaced fractures.
-
Displaced fractures require open reduction and internal fixation.
-
Postoperative management consists of 6
weeks of non-weight-bearing, followed by gradual progression of
weight-bearing over the next 6 weeks.
-
-
The initial treatment for femoral shaft stress fractures is for the athlete to rest for 2 to 4 weeks.
-
During this period, the athlete progresses from toetouch weight-bearing to full weight-bearing.
-
-
If, after these initial 4 weeks, the
athlete is able to weight-bear pain-free, he or she is allowed to begin
low-impact activity. -
If low-impact activity is tolerated pain-free, the athlete is progressed slowly to higher-impact activities.
-
This process takes place over a course of 6 to 8 weeks.
-
-
If the stress fracture has delayed union, nonunion, or progresses to a complete fracture, intermedullary nailing is performed.
-
For athletes with a tibial stress
fracture, the first 6 weeks of treatment consist of complete rest while
using either crutches, a short leg cast, or a boot.-
Posteromedial cortex stress fractures respond well to rest.
-
-
After the pain has subsided, the athlete may begin some low-intensity, nonimpact aerobic activities such as swimming or biking.
-
Re-evaluate the athlete after 6 weeks.
-
If the athlete is pain-free, he or she may begin a gradual progression back in play.
-
Do not increase the athlete’s volume or intensity by more than 10% each week.
-
-
If at the 6-week mark the athlete still has pain, radiographs should be repeated.
-
If the radiographs have positive findings, complete rest should be continued for another 6 weeks.
-
If the radiographs are negative, the athlete can begin a slow return to activity.
-
-
If after 12 weeks the athlete still has pain, a CT scan or MRI should be obtained.
-
Surgical excision and bone grafting may be required if the fracture does not heal with rest and immobilization.
-
Navicular stress fractures are a difficult problem to treat.
-
Incomplete fractures are treated with
immobilization in a cast or boot, and athletes are made
non-weight-bearing for 6 to 8 weeks. -
A return to weight-bearing and activity is based on the clinical picture and evidence of radiographic healing.
-
For complete, nondisplaced fractures, attempt nonoperative treatment with cast and non-weight-bearing for 6 to 8 weeks.
-
The definitive initial treatment for
metatarsal stress fractures is rest, putting the patient in a boot or
on crutches for 6 weeks. -
The one exception is Jones-type stress
fractures of the fifth metatarsal, which require the athlete to be in a
short-leg cast or a boot for 12 weeks of non-weight-bearing. -
With these specific types of fractures,
many athletes choose operative management with an intramedullary
cancellous or cannulated screw and return to sports slowly after 6
weeks.
developing stress fractures, specific stress fractures, and the
diagnosing and treatment of stress fractures. In this final section, we
will discuss steps athletes, coaches, and team physicians can take to
prevent stress fractures. Nutrition plays a key role. The athlete must
be sure to take in enough calcium and vitamin D in his or her diet, as
well as to take in enough calories. The sports medicine
staff
should be looking for red flags pointing to possible eating disorders
in their athletes. Athletes (especially distance runners) should also
use proper footwear and try to train on softer, impact-absorbing
surfaces. An athlete’s training program should contain a cyclical
progression in terms of intensity and distance. Cross-training should
be encouraged. Training should place an emphasis on quality over
quantity. Most importantly, sports medicine physicians should educate
parents, coaches, and athletes about stress fractures.
GW, Saha H. Menstrual irregularity and stress fractures in collegiate
female distance runners. Am J Sports Med 1988;16:209-216.
KL, Malcolm SA, Thomas SA. The incidence and distribution of stress
fractures in competitive track and field athletes. Am J Sports Med
1996;24:211-217.
TJS, Grudger TD, Obermeyer L. Stress fractures in 295 trainees: a
one-year study on incidence as related to age, sex, and race. Mil Med
1983;148:666-667.
KM, Fuller PJ, Brukner PD, et al. Outcome of conservative and surgical
management of navicular stress fracture in athletes. Am J Sports Med
1992;20:657-666.
S, Caine D, Singer KM. Stress changes of the distal radial epiphysis in
young gymnasts. A report of twenty-one cases and a review of the
literature. Am J Sports Med 1985;13:301-308.
HR, Kaye JJ. Longitudinal stress fractures of the tibia: diagnosis by
magnetic resonance imaging. Skel Radiol 1996;25:319-324.
