Staying Out of Trouble with Orthopaedic Infections
– Special Maladies and Concerns > 16 – Staying Out of Trouble with
Orthopaedic Infections
|
|
trouble for our orthopaedic ancestors—and their patients. Today, with
vastly superior imaging and antibiotics, most orthopaedic infections
can be located, identified, and treated in a timely fashion with rare
residual sequelae. To stay out of trouble, it is important to recognize
several trends over the last couple of decades. First, it is much more
likely that the orthopaedist will see a child very early after the
start of a bone or joint infection. This can make diagnosis very
difficult, because inflammatory markers such as C-reactive protein
(CRP) or erythrocyte sedimentation rate (ESR) may initially be normal
or only slightly elevated.
is subacute osteomyelitis. Likewise, knee-jerk antibiotic
administration may blunt the initial picture.
normal initially. An aspiration may not yield any pus early after
infection, and radiographs may well be normal also.
in the management of infants and younger children so that you don’t
miss other site infections that may be disastrous (such as meningitis).
there is often a trauma history. This may lead the orthopaedist down
the path of looking for occult fractures, sprains, etc., delaying
diagnosis. To stay out of trouble, recognize that if it is an injury,
with each passing day the area looks and feels better; in an infection,
with each passing day it looks and feels worse.
especially spina bifida but also cerebral palsy and others, can present
with a fracture and have a picture that mimics infection (Fig. 16-1).
complain of pain. Instead, they may limp or not walk or not move the
body part. Don’t forget about referred pain: pain from the back and the
psoas area can refer to the hip, and pain that
originates
in the hip can refer to the distal thigh or knee region. Be sure to get
a history of recent infections. A particularly important example is
chicken pox: the virus lowers immunity and the skin lesions can be
infected. In these cases, the bacterial pathogen is usually
streptococcus, but can be staphylococcus.1
 |
|
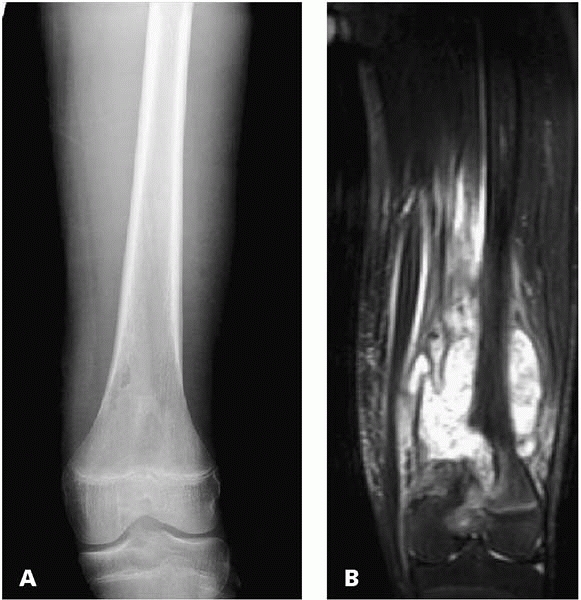
▪ FIGURE 16-1 Fractures in children with spina bifida can be hard to distinguish from infection. This baby (A) presented with erythema and swelling. A knee radiograph (B) demonstrated a subtle fracture of the distal femoral physis. (Case courtesy of R. Davidson, MD.)
|
WBC is often normal, although a left shift may be a clue that there is
an infection. It is also essential to keep in mind that leukemia may be
in the differential diagnosis. If this is a possibility, you will want
your primary care doctors or infection consultants to look at a manual
differential/smear to rule out leukemia. ESR rises slowly and is
unreliable in the early presentation of bone and joint infections. It
is also unreliable in the neonate or children with sickle cell disease.
C-reactive protein can rise after trauma, giving you a false positive.
It is also usually elevated in otitis media and other childhood
infections, so like other markers, specificity is poor. Blood cultures
are good, but the best way to isolate an organism is by aspirating the
suspected site of osteomyelitis.
under conscious sedation with careful localization. Most osteomyelitis
is in the metaphysis very near the physis.
pediatric orthopaedic infections, radiographs can fool you by lagging
behind the actual clinical activity. You may encounter imaging that is
normal after the disease has started or imaging that looks worse
despite rapid clinical resolution. It is well known that changes in the
bone take more than a week to show up on plain radiographs after the
start of Acute hematogenous osteomyelitis (AHO). To stay out of
trouble, look for soft-tissue swelling as an early radiographic sign.
For comparison, position both limbs symmetrically, and ask for a
soft-tissue technique. Bone scan with pinhole views have been used in
the past, but have been largely replaced by MRI (Fig. 16-2).
significant source of trouble. Look for signs of clinical improvement
before switching to oral antibiotics.
 |
|
▪ FIGURE 16-2
This 13-year-old boy presented for a consultation for limb sparing surgery because the initial treating orthopaedist thought it was osteosarcoma based on the plain radiographs and MRI (A,B). Fortunately, a gram stain and culture was performed at the time of biopsy. Intraoperative culture grew MRSA. The lesson: culture every biopsy (and biopsy every infection). (Case courtesy of J. Dormans, MD.) |
have infectious disease specialists on staff. Ask these experts, or the
child’s primary care doctor, to help you define the best antibiotic and
antibiotic course. Remember that some antibiotics can cause side
effects, such as neutropenia. You or one of the primary doctors should
be following a WBC.
potential site of osteomyelitis are not absolute. Many orthopaedists
use the failure to show clinical improvement after 24 to 36 hours of
antibiotics as the main reason to do an irrigation and debridement.
Others recommend doing an irrigation and debridement every time pus is
aspirated, or there are disruptive changes on radiographs. Extended
follow-up may be warranted for young children with osteomyelitis.
Because the infection in infants and young children occurs so close to
the growth plate, there is a risk for growth arrest.
especially in the hip, where it is a surgical emergency. Surgical
irrigation and debridement is also recommended for most other joints,
although there is some literature to support the efficacy of repeat
aspirations and antibiotics for joints other than the hip.
of a swollen joint in your head. You should consider Lyme arthritis in
endemic areas as well as various rheumatologic conditions. The
experienced examiner will note that in both Lyme arthritis and
nonbacterial arthritis, there may be a large effusion but no
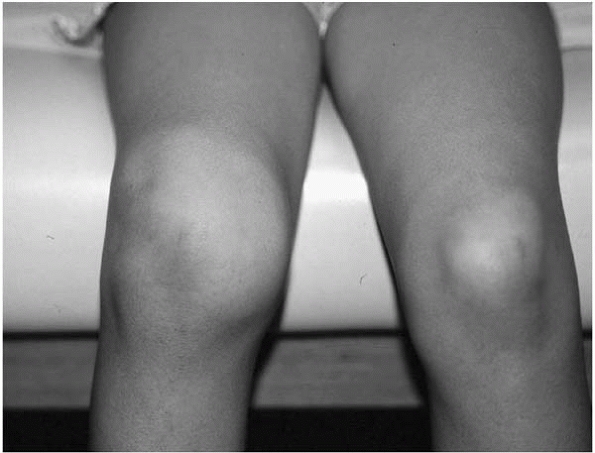
significant short arc tenderness3 (Fig. 16-3).
 |
|
▪ FIGURE 16-3
The classic finding in Lyme arthritis of the knee: huge swelling, little pain with motion. No need to rush this one to the OR for irrigation and debridement. |
-
Leukemia
-
Metastatic neuroblastoma
-
Langerhans cell histiocytosis
-
Ewing sarcoma
-
Sickle cell disease
-
Infarct
-
Gaucher disease
children with JRA or Lyme arthritis will have a synovial WBC greater
than 100,000. Keep gonococcal arthritis in your differential. You won’t
see gonococcal arthritis exclusively in sexually active teens; sadly,
you may encounter the infection in a younger child who has been
sexually abused. As the organism responsible for gonococcal arthritis
is notoriously difficult to grow in culture, be sure to obtain proper
cultures for the differential diagnosis. Recognize that septic
arthritis usually makes bigger and faster rises to CRP and ESR than
osteomyelitis.
septic arthritis. Widening of a hip joint space is a very unreliable
sign of septic arthritis of the hip. Such
widening
may be affected by positioning, and is more common in infants. If you
do see a true widened hip joint space, it means that there is
substantial pressure on the joint. This is not usually present early in
the process. Also keep in mind that ultrasonography itself cannot
absolutely distinguish transient synovitis from septic arthritis of the
hip4.
bacterial pathogens responsible for septic arthritis in children. H flu
is now nearly eliminated as a common pathogen, but the incidence of
positive Kingella kingae cultures is rising.5
It may be that kingella has been present for a long time, but is so
difficult to isolate by culture that we are just isolating it more
frequently now. To culture Kingella, use a blood culture bottle to help
with your bacterial isolation.6
-
Hip
-
Proximal humerus
-
Proximal radius
-
Distal lateral tibia
in school-age children, while septic arthritis of the hip is a rare but
potentially crippling disaster if unrecognized. Rapidly telling the
difference between transient synovitis and septic arthritis is an
essential skill to stay out of trouble in pediatric orthopaedics.7
In septic arthritis, children are usually sick with a fever and are
getting worse by the hour. In septic arthritis they usually won’t bear
weight on the affected hip. You will usually find pain with simple log
rolling of the hip. The CRP may be elevated but the ESR may not in the
first 24 hours after the infection.8
irrigation and debridement on any hip with bacteria on gram stain (or
if there are greater than 50,000 WBCs in the aspiration fluid but a
negative gram stain if the clinical picture is worrisome for septic
arthritis).
your most important pediatric orthopaedic emergencies. The timeliness
of treatment is just as important as compartment syndrome, and probably
more important than a rapid irrigation and debridement of an open
fracture.
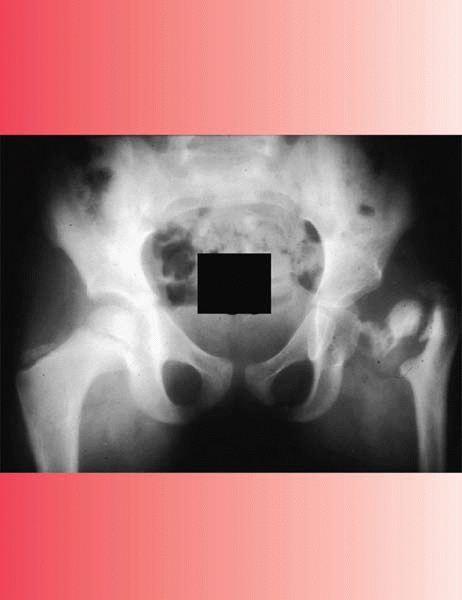
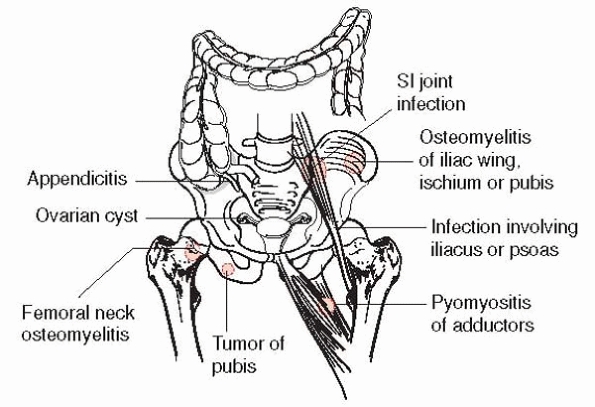
Osteomyelitis of the pelvis and septic arthritis of the sacroiliac (SI)
joint certainly fall into this category. Such patients are usually
older children and
teens,
whereas septic arthritis of the hip is usually seen in younger
children. Pelvic osteomyelitis and SI joint infections usually have
protean manifestations much like spinal infections. The flexion
abduction external rotation test (FABER) can be very helpful to stress
the SI joint and localize the problem to this area. Palpation over the
SI joint or compression of the iliac wings can also be provocative for
pain in the SI region. A psoas abscess can also present looking just
like septic arthritis of the hip.11
Depending on the duration and how extensive, these hips are usually not
so painful with general rotation at 90 degrees but are worse with
extension. After the pus has been dissected around the hip capsule,
these children present much more like classic septic arthritis of the
hips. Sometimes you can find tenderness over the brim of the pelvis. A
quick way to distinguish psoas abscess from a septic hip is an
ultrasound, which can often detect swelling of the psoas. An MRI may be
also helpful to distinguish these two conditions.12
Also, don’t forget non-orthopaedic conditions like appendicitis,
gynecologic conditions, or even hernias that can mimic some of the
signs and symptoms of hip joint septic arthritis.
 |
|
▪ FIGURE 16-4 The various conditions that can mimic classic pediatric hip septic arthritis.
|
arthritis and not transient synovitis, it is important to adhere to
certain surgical principles and techniques to stay out of trouble.
Septic hips in young children are drained anteriorly to avoid
disrupting the posterior blood supply to the femoral epiphysis. It is
critical to do a definitive capsulotomy. Be sure that the joint is
aggressively irrigated and that there is no purulent collection left
behind. Some have recommended decompression of the femoral neck if
there is associated osteomyelitis that has not decompressed itself into
the joint. Most surgeons place a drain around the femoral neck, secure
the drain carefully, and rest the child in bed for at a day or so to
keep the drain in and to allow the hip to quiet down.
infectious disease colleagues recommend four weeks of intravenous
antibiotics, following the clinical course and CRP closely.13
Beware when the CRP does not rapidly normalize in the first week after
surgery! You must ask yourself whether there is another collection of
fluid, whether the fluid reaccumulated, or if you have the right
diagnosis. Is it possible that you may have missed osteomyelitis of the
femoral neck? (See Fig. 16-5.) In this clinical scenario, it is best to get an MRI to determine why the child has not
had the expected clinical improvement. Finally, follow these children
for a couple of years afterwards to be certain that there is not AVN or
any proximal femoral growth disturbance (Fig. 16-6).
 |
|
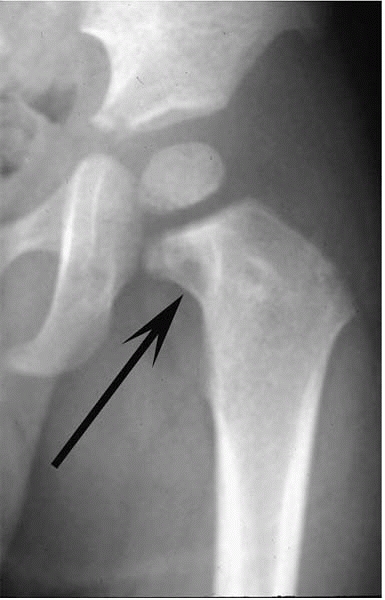
▪ FIGURE 16-5 An associated femoral neck osteomyelitis, as shown in this AP hip radiograph (arrow), delays improvement after an irrigation and debridement of the hip.
|
 |
|
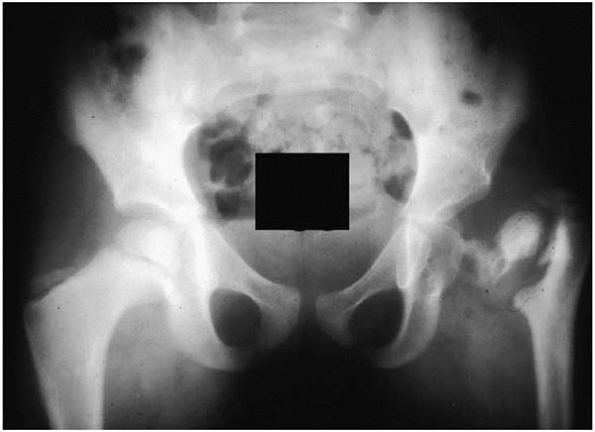
▪ FIGURE 16-6 The disastrous consequences of missing a septic arthritis of the hip.
|
infection, although the older literature called it inflammation and
questioned the role for antibiotics. The infection is believed to start
in the bone adjacent to the vertebral end plate. It often takes longer
to present and diagnose than other pediatric musculoskeletal
infections, so CRP and sedimentation rate are often quite high.
Cultures, obtained rarely, are usually negative. To stay out of
trouble, recognize that many children with such spinal infections will
not have back pain. Younger children may refuse to walk or just present
with lethargy. There may also be abdominal pain in the school-age
child, although teenagers typically have true low back pain.
bone scan may be negative in the first couple of weeks. An MRI is very
helpful in early spinal infections (Fig. 16-7).
Fight the urge to biopsy these children immediately. The cost and
morbidity of biopsy can be high and the yield is so low that empirical
treatment with antibiotics (be sure to cover staphylococcus) is the
standard of care. The indications for biopsy are soft, but include a
worsening clinical picture despite antibiotics.
antibiotics for a few days to be sure that there is no sign of an
epidural abscess. An epidural abscess is rare but is certainly an
emergency. An epidural abscess will present with worsening neurologic
signs and should be drained immediately.
considered in the first two months after birth, especially if the child
is premature. The clinical scenario is much different in this group. To
stay out of trouble, recognize that the lack of a mature immune system
means that all of the inflammatory responses we count on as indirect
evidence of infection will be absent. Routine lab tests are not even
helpful in many cases. Most important, to stay out of trouble, look for
more than one site of infection, especially in the NICU baby with
invasive monitoring.
infants with bone and joint infections should be followed for several
years after treatment.14
 |
|
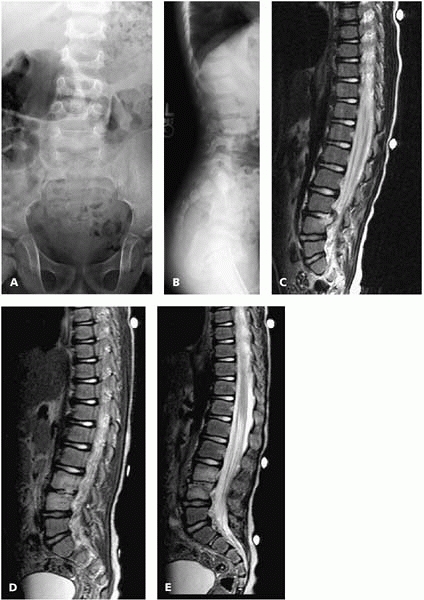
▪ FIGURE 16-7 Discitis. This 4-year-old boy presented with fever, back pain, and an elevated CRP. An AP (A) and lateral (B) radiograph showed narrowing of the L3-4 disc space. An MRI at presentation (C)
showed loss of normal fluid signal in the disc on T2 images and a small posterior collection. He was given the diagnosis of discitis/vertebral osteomyelitis, treated with IV antibiotics, and experienced rapid resolution of his symptoms. By 2 weeks after presentation, his CRP had normalized. One month later, the infectious disease team ordered a routine followup MRI, despite the fact that he was completely asymptomatic and had normal lab tests. They called Orthopaedics, alarmed that the MRI (D,E) had “dramatically worsened, with loss of disc space and involvement of the entire anterior L3 and L4 vertebral bodies.” They were wondering if a biopsy should be performed. Fortunately, the orthopaedist had treated many such cases, and recognized that this is the typical evolution of MRI appearance over time. The child was observed, and months later continued to have no symptoms or elevation in inflammatory markers. |
The biggest source of trouble here is separating an infarct from an
infection. In many ways these two problems can have a very similar
presentation. Both have pain and swelling, and the ESR may be falsely
low because of the hematologic nature of the tests and the abnormal red
blood cells. On the radiograph, you can see a periosteal reaction for
both and there can be edema on MRI in both conditions. If the picture
is suspicious for an infection, it is important to get blood cultures
and aspirate the site. Sequential radionuclide bone-marrow and bone
scans have also been shown to be helpful.15 It is important to cover both staph and salmonella until the cultures are positive.
 |
|
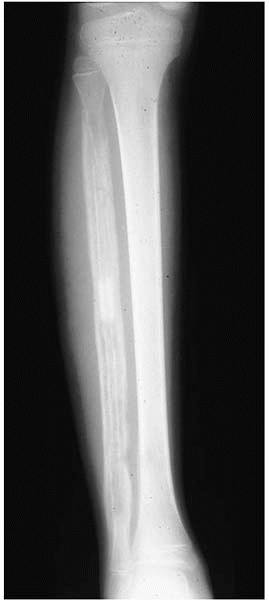
▪ FIGURE 16-8
This AP radiograph was taken several weeks after a child with sickle cell disease showed signs of osteomyelitis of the fibula. Note the extent of diaphyseal involvement. Biopsy of the diaphysis can be more difficult; general anesthesia with fluoroscopic image localization is helpful. (Case courtesy of J. Dormans, MD.) |
a difficult condition to manage. The cultures are almost always
negative, so a biopsy of the tissue is not recommended, unless
malignancy is in the differential diagnosis. It is important to follow
the patients to maturity, because deformities can develop.16 Growth arrest has also been described.17
Staphylococcus is the most common cause of the soft-tissue infection.
True osteomyelitis or foot septic arthritis develop in only a very
small percentage of puncture wound cases. Pseudomonas infection occurs
when the puncture goes through the sole of a shoe or when the child is
in dirty water, such as a lake. Pseudomonas loves cartilage, so
infections
in cartilage should be sought out. Initial care involves a tetanus
shot, limited superficial debridement, and anti-staphylococcal
antibiotics. If the infection develops in a bone or joint, you must
perform an irrigation and debridement in order to truly irrigate the
infection, especially if it is pseudomonas. Broadspectrum antibiotics
are needed. Getting help from your infectious disease team is valuable
in this scenario.
 |
|
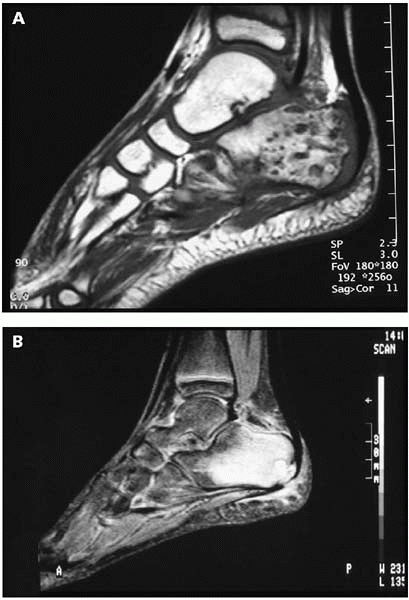
▪ FIGURE 16-9 T1 (A) and T2 (B) images of the foot of a child who stepped on a nail. There is osteomyelitis of the calcaneus.
|
-
Fever plus tenderness over a bone is acute hematogenous osteomyelitis until proven otherwise.
-
Be sure to get a
pediatrician to help in the management of infants and younger children
so that you don’t miss other site infections that may be disastrous
(such as meningitis). -
A common mistake in aspirating osteomyelitis is to be in the diaphyseal region, too far from the physis.
-
The premature switch to oral antibiotics is one of the biggest errors in judgment in managing osteomyelitis.
-
The hallmark of
differentiating Lyme arthritis or rheumatoid arthritis from septic
arthritis is noting that in the former there is a joint effusion that
is out of proportion to the symptoms. -
Remember: the patient doesn’t have to be a sexually active teen to have gonococcus arthritis.
-
Irrigation and debridement of the septic hip is more of an emergency than washing out an open fracture.
-
When draining a septic hip, take out a small sample of the capsule with its synovium.This ensures adequate decompression and gives tissue for culture.
-
Discitis: observe
the child on inpatient intravenous antibiotics for a few days to be
sure that there is no sign of an epidural abscess. -
Neonatal infection: look for more than one site of infection, especially in the NICU baby with invasive monitoring.
JE, Huang M, Dobbs M, et al. Causes of false-negative ultrasound scans
in the diagnosis of septic arthritis of the hip in children. J Pediatr Orthop. 2002;22(3):312-316.
A, Garcia-Garcia JJ, Sala P, et al. Enhanced culture detection of
Kingella kingae, a pathogen of increasing clinical importance in
pediatrics. Pediatr Infect Dis J. 2004;23(9):886-888.
F, Cohn L, Hashman N, et al. Recovery of Kingella kingae from blood and
synovial fluid of two pediatric patients by using the BacT/Alert
system. J Clin Microbiol. 1999;37(3):878.
MS, Mandiga R, Zurakowski D, et al. Validation of a clinical prediction
rule for the differentiation between septic arthritis and transient
synovitis of the hip in children. J Bone Joint Surg Am. 2004;86-A(8):1629-1635.
MJ, McGuire KJ, McGowan KL, et al. Assessment of the test
characteristics of C-reactive protein for septic arthritis in children.
J Pediatr Orthop. 2003;23(3):373-377.
MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis
and transient synovitis of the hip in children: an evidence-based
clinical prediction algorithm. J Bone Joint Surg Am. 1999;81(12):1662-1670.
J, Bagali M, Kaneker S. Physical signs in pyomyositis presenting as a
painful hip in children: a case report and review of the literature. J Pediatr Orthop B. 2004;13(3):211-213.
HK, Alman B, Cole WG. A shortened course of parenteral antibiotic
therapy in the management of acute septic arthritis of the hip. J Pediatr Orthop. 2000;20(1): 44-47.
DL, Kim SK, Greene NW, et al. Differentiation between bone infarction
and acute osteomyelitis in children with sickle-cell disease with use
of sequential radionuclide bone-marrow and bone scans. J Bone Joint Surg Am. 2001;83-A(12):1810-1813.
CM, Lam PY, Ditchfield M, et al. Chronic recurrent multifocal
osteomyelitis: review of orthopaedic complications at maturity. J Pediatr Orthop. 2002;22(4):501-505.
C, Reed MH, Black GB. Premature epiphyseal fusion and degenerative
arthritis in chronic recurrent multifocal osteomyelitis. Skeletal Radiol. 2000;29(2):94-96.
M, Bialik V, Miller Y, et al. Plantar puncture wounds in children:
analysis of 80 hospitalized patients and late sequelae. Isr Med Assoc J. 2003;5(4):268-271.