Rotator Cuff Tears: Mini-Open and Open Surgical Treatment
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 39 – Rotator Cuff Tears: Mini-Open and Open
Surgical Treatment
subacromial bursa and rotator cuff) constitutes the most common cause
of shoulder pain. This pathology encompasses a spectrum of disease
ranging from acute bursitis and tendinitis to chronic tendinitis and
finally to tears of the rotator cuff, either partial thickness or full
thickness. Considerable debate continues concerning the underlying
cause of rotator cuff tears and also concerning their management.
Treatment options for full-thickness rotator cuff tears include
nonoperative treatment with exercises, subacromial decompression with
debridement of the tear, and rotator cuff repair, either through
arthroscopic, arthroscopically assisted (mini-open), or open surgical
techniques. In addition, some massive rotator cuff tears are treated
with tendon transfers, involving the use of latissimus dorsi, teres
major, and/or pectoralis major tendons. This chapter will focus on
mini-open and open repair of full-thickness rotator cuff tears.
both intrinsic tendon factors as well as the extratendinous anatomy of
the subacromial space. Histologic studies of tendons have demonstrated
degenerative changes in older specimens. Moreover, the tendon fibers
undergo differential strains, with the articular-side fibers undergoing
significantly greater tensile strain with the arm in abduction. This
perhaps explains why tear initiation usually occurs on the undersurface
or articular side of the tendon. Others have pointed to the relative
avascularity of the “critical zone” of the supraspinatus as another
intrinsic factor predisposing this region of the tendon to tear.
structures of the subacromial space, specifically, the coracoacromial
arch in the pathogenesis of rotator cuff tears. Neer postulated that
the overwhelming majority of rotator cuff tears were the result of
attritional wear from excrescences on the undersurface of the anterior
third of the acromion and to a lesser extent, the undersurface of the
distal clavicle. Narrowing of the supraspinatus outlet by excrescences
or spurs on the acromial undersurface resulted in frictional wear on
the region of the supraspinatus, where most tears initiate. Several
biomechanical studies have demonstrated that contact pressures between
the acromial undersurface and the rotator cuff are maximal in this
region of the supraspinatus with the shoulder abducted between 60 and
120 degrees. Moreover, cadaver studies have correlated acromial
morphology with the incidence of rotator cuff tears and found that
those with a type III or hooked morphology had the highest incidence of
tears.
of rotator cuff tears. A hard fall can certainly result in tearing of
the rotator cuff. An anterior dislocation in a patient older than 40
years of age can be associated with a rotator cuff tear. In younger
patients, such dislocations result in stretching of the glenohumeral
ligaments, avulsion of the anteroinferior labrum, or rarely, a fracture
of the anteroinferior glenoid rim, but almost never in a full-thickness
rotator cuff tear. A traumatic episode may also result in the
progression of a previously existing rotator cuff tear, causing an
acute onset of shoulder weakness. Such an acute extension of a chronic
tear may turn an asymptomatic shoulder into one with acute pain and
weakness. This is not infrequently seen in elderly patients.
Full-thickness tears are rarely seen in those younger than 40 years of
age and are likely caused by repetitive microtrauma involved with work
and recreational sports activities. The incidence of full-thickness
rotator cuff tears rises in those older than 40 years of age, and they
occur more commonly in the dominant shoulder, supporting the notion
that attrition is an important etiologic factor.
basis of a thorough history and physical examination of the shoulder. A
subacromial injection of lidocaine can be used to confirm the
diagnosis, and radiographs can provide supportive evidence and rule out
other diagnoses. Staging of disease in the rotator cuff, ranging from
tendinitis to partial tears to full-thickness tears can be precisely
achieved through magnetic resonance imaging or ultrasonography.
with pain in the anterosuperior aspect of the shoulder. The pain
usually radiates to the deltoid region, but not distally past the
elbow. Pain, which is located predominantly in the posterior shoulder
or trapezius region or which radiates into the forearm or hand or which
is accompanied by paresthesias is more likely due to cervical
radiculopathy than to subacromial pathology. In rotator cuff disease,
the pain is usually increased with overhead use of the arm and with
active abduction and reaching behind the body. Often the pain is
increased at night with the supine position, perhaps because this
increases compression of the inflamed tendon and bursa beneath the
acromion. Patients may complain of a catching sensation and of shoulder
weakness, particularly with activities performed above shoulder height.
Frequently affected tasks include work activities that require lifting
or repetitive overhead use and sports activities, such as tennis, golf,
and swimming.
shoulder may present with symptoms similar to those of rotator cuff
disease and should be considered in the differential diagnosis.
Cervical radiculopathy, specifically a herniated cervical disc at the
C5–C6 level, can present with pain in the deltoid and biceps regions.
Acromioclavicular arthritis causes pain in the superior aspect of the
shoulder and trapezial region and may coexist with rotator cuff
disease. Adhesive capsulitis, particularly in its early prestiffness
phase, may be mistaken for rotator cuff disease, as pain in the deltoid
region is often the earliest symptom. Subtle glenohumeral instability
may present as anterosuperior shoulder pain without frank episodes of
subluxation or sensation of instability, particularly in young overhead
athletes. These patients may have both an underlying instability
problem and a secondary subacromial bursitis or tendinitis and may be
difficult to diagnose precisely. Finally, calcific tendinitis can mimic
a rotator cuff tear, as the anatomic distribution of pain is similar,
and the intensity of pain may cause a pseudoparalysis, which can
resemble the weakness seen with large rotator cuff tears. The history
of an acute atraumatic onset and the presence of a calcific deposit on
plain radiographs serve to differentiate these diagnoses.
diagnosis of rotator cuff disease. In cases of chronic large or massive
tears, simple inspection of the shoulder may suggest the diagnosis, as
there is usually atrophy of the supraspinatus and infraspinatus
muscles, and sometimes a visible rupture of the tendon of the long head
of the biceps. There may be a diffuse swelling around the shoulder—a
so-called fluid sign or a localized fluid collection at the
acromioclavicular joint. Occasionally, with an acute traumatic tear,
ecchymosis may be present. However, with smaller tears or more acute
tears, the appearance of the shoulder is usually normal.
tenderness over the subacromial bursa and greater tuberosity.
Approximately 10% to 15% of patients with a rotator cuff tear will also
have symptomatic acromioclavicular arthritis, which is diagnosed
clinically by tenderness directly over the acromioclavicular joint and
by painful adduction of the shoulder. With full-thickness rotator cuff
tears, subacromial crepitation can often be appreciated with passive
range of motion of the shoulder. Usually, passive range of motion is
preserved with rotator cuff tears, although a small percentage of
shoulders with tears will develop stiffness. Active range of motion is
often normal with smaller tears, but loss of active motion can occur
with larger tears.
testing, may be normal with partial-thickness tears and even with
smaller full-thickness tears. However, larger tears usually produce
shoulder weakness, which can be detected by resistance testing or in
more severe cases, by lag signs or “drop-arm” signs. Thus, the patients
may not be able to actively elevate or externally rotate the shoulder
fully, producing a lag between their active and passive motion. In a
similar manner, loss of infraspinatus function will cause a shoulder
that is placed into an externally rotated position to fall into
internal rotation, producing a drop-arm sign. Subscapularis deficiency
results in an inability to lift the arm off the lumbar spine when it is
placed into internal rotation, producing a positive “lift-off” sign, as
described by Gerber.
diagnosing rotator cuff problems. The Neer impingement sign, which is
tested by stabilizing the patient’s scapula while fully passively
elevating the arm, is nearly always positive in patients with
subacromial pathology. The Hawkins sign, tested by fully internally
rotating the shoulder at 90 degrees of flexion, is also quite useful in
detecting subacromial problems. Resisted testing of the supraspinatus,
as popularized by Jobe, can further suggest rotator cuff pathology.
Finally, the injection of 10 mL of 1% lidocaine into the subacromial
space will reliably reduce or eliminate pain that is caused by
subacromial pathology and can be helpful in confirming the diagnosis of
a rotator cuff disorder.
the diagnosis of a rotator cuff disorder. Excrescences on the acromion,
greater tuberosity, and undersurface of the distal clavicle can be seen
on an anteroposterior radiograph in a shoulder with rotator cuff
pathology. Moreover, a diminished acromiohumeral interval is suggestive
of a rotator cuff tear, and some would suggest that an acromiohumeral
interval of <6 mm is indicative of an irreparable tear. In the
supraspinatus outlet view, a lateral radiograph with a 10-degree caudal
tilt, the morphology of the acromion, and
any
associated spurring can be clearly visualized. This information can be
helpful in surgical planning, concerning the extent of the subacromial
decompression that will be required in a particular shoulder. An
axillary radiograph will reveal the presence of an unfused acromial
epiphysis or os acromiale. Finally, plain radiographs are useful in
ruling out other painful shoulder conditions, such as glenohumeral
arthritis and calcific tendinitis.
supplemented by plain radiographs can allow the diagnosis of a rotator
cuff or subacromial disorder, magnetic resonance imaging or
ultrasonography can help to stage the problem accurately. These imaging
techniques can differentiate between tendinitis, partial-thickness
tears, and full-thickness tears of the rotator cuff. When a tear is
present, these studies indicate which tendon or tendons are involved,
the size of the tear, and the degree of tendon retraction. Magnetic
resonance imaging is also quite useful in providing data about the
rotator cuff muscles, such as information about the degree of muscle
atrophy or fatty infiltration. Such structural information can help the
surgeon choose an appropriate surgical technique for rotator cuff
repair and provide insight about the reparability of a tear. In the
United States, magnetic resonance imaging has replaced the arthrogram
as the test of choice in most centers for staging rotator cuff disease.
Ultrasonography, while relatively inexpensive and allowing bilateral
examination in a cost-effective way, is less familiar to most North
American surgeons and requires greater expertise to perform and
interpret accurately.
include nonoperative treatment with exercises and various surgical
techniques of repair. Nonoperative treatment has been shown to result
in pain relief and functional improvement, but these results are less
predictable than those of surgical repair and may deteriorate over time
with tear extension. Older, more sedentary patients, who put less
demand on the shoulder for overhead work or sports activities, appear
to benefit more consistently from nonoperative treatment than younger,
more active patients. Patients in their 70s and 80s are also more
likely to present with chronic large or massive tears with a
significant degree of muscle atrophy and fatty degeneration on magnetic
resonance imaging. Such patients are less likely to achieve functional
improvement after rotator cuff repair and are probably best managed
with nonoperative treatment.
seventh decades with a symptomatic full-thickness rotator cuff tear are
best served by early rotator cuff repair. Numerous studies on the
results of rotator cuff repair have reported a satisfactory outcome in
85% to 95% with predictable pain relief and functional improvement in
most patients. Although complete healing of the tendons did not appear
necessary to achieve satisfactory pain relief, the best functional
results were seen in patients in whom the repair was intact at
follow-up in studies by Harryman et al. and Gerber et al. Moreover,
work by Yamaguchi et al. has suggested that the natural history of
rotator cuff tears is extension of the tear in a considerable
percentage of these tears. This information, combined with other recent
data that demonstrate that muscle atrophy is only partially reversible
and fatty infiltration of the muscles appears to be irreversible, would
suggest that early repair of a symptomatic rotator cuff tear is the
optimal treatment for an active, healthy patient.
to evolve. Since Neer’s description of anterior acromioplasty in 1972,
most of those techniques have combined subacromial decompression with
tendon repair, although a few authors have recently questioned the use
of acromioplasty. In addition to the traditional method of open rotator
cuff repair, newer techniques combining arthroscopic acromioplasty with
mini-open rotator cuff repair and completely arthroscopic repair have
become more popular. For dealing with some of the massive irreparable
tears, tendon transfer techniques and the use of synthetic grafts have
been used. The remainder of this chapter will focus on the techniques
of mini-open and open rotator cuff repair.
decompression with open tendon repair through a small deltoid split.
Since the anterior acromioplasty is performed arthroscopically, this
technique allows preservation of the deltoid origin during the repair
of the torn rotator cuff. Other advantages for this procedure compared
with traditional open rotator cuff repair include lower perioperative
morbidity and shorter hospital stays, superior cosmesis with smaller
incisions, easier rehabilitation, and the ability to treat associated
intra-articular pathology, such as labral tears or biceps lesions,
during the arthroscopic portion of the procedure. In comparison with
wholly arthroscopic repair, the mini-open procedure is technically
easier to perform and has a lower learning curve.
appropriate for small to medium-sized tears (i.e., <3 cm) without
significant retraction. These tears usually involve the supraspinatus
tendon alone or the supraspinatus and upper portion of the
infraspinatus. Larger tears or those with extensive retraction can be
treated with this technique, but are more easily treated with
traditional open techniques, as these tears require more extensive
tissue mobilization and transposition, which can be difficult to
achieve through the limited exposure afforded by the small deltoid
split. Subscapularis tears are also difficult to access through the
mini-open approach and are usually treated using an open approach.
beach-chair position under interscalene block regional anesthesia.
Arthroscopic examination of the glenohumeral joint is carried out
through a standard posterior portal. This allows for inspection of the
intra-articular structures and treatment of associated pathology of the
labrum or biceps tendon, as well as debridement of the undersurface of
the rotator cuff, using arthroscopic instruments introduced
through
a standard anterior portal. The arthroscope is then removed from the
glenohumeral joint and is introduced into the subacromial space. An
arthroscopic acromioplasty is performed to create a smooth undersurface
of the anterior third of the acromion. As this technique has been
extensively reviewed elsewhere in this text, we will focus on the
details of the mini-open tendon repair.
 |
|
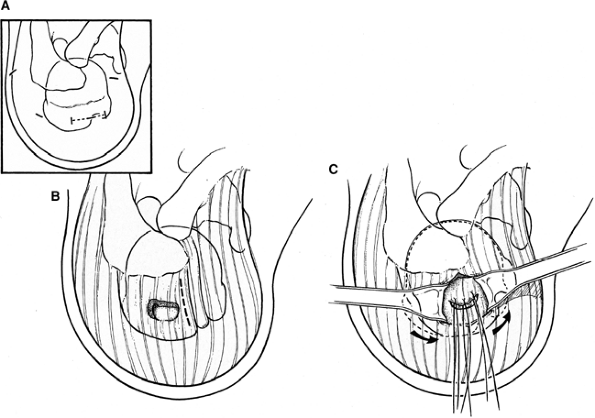
Figure 39-1 A: Limited 3- to 4-cm skin incision, which includes the anterolateral portal and is directed along the skin lines for cosmesis. B: Deltoid split (dotted line), starting from the anterolateral acromion and extending 4 cm distally. C: Arm rotation allows the tear to be positioned below the deltoid split. (From
Post M, Bigliani LU, Flatow EL, et al. Rotator cuff repair. In: Post M, Bigliani LU, Flatow EL, et al., eds. The Shoulder: Operative Technique. Lippincott Williams & Wilkins; 1998
, with permission.) |
the arthroscope and burr are removed from the subacromial space. The
anterolateral portal incision is extended to a total length of 3 to 4
cm and is directed horizontally along the skin lines (approximately
parallel to the lateral border of the acromion) (Fig. 39-1A).
This yields a more cosmetically pleasing scar than vertically oriented
incisions. The subcutaneous tissue is incised and undermined to expose
the deltoid fascia. The deltoid is then split from the anterolateral
corner of the acromion to a point 4 to 5 cm distally, incorporating the
previous puncture site through the deltoid in the split (Fig. 39-1B).
Care is taken proximally not to release or avulse the deltoid from the
anterior acromion and distally not to exceed 4 to 5 cm and thereby
jeopardize the axillary nerve. Further bursectomy is then performed to
allow better visualization of the torn rotator cuff. The torn portion
of the rotator cuff can be delivered directly below the deltoid split
by varying the rotation of the arm (Fig. 39-1C).
are placed into the tendon along the perimeter of the tear to assist
with mobilization of the torn rotator cuff. A blunt periosteal elevator
is used to release adhesions on both the articular and bursal surfaces
of the cuff. The tendon is mobilized until it easily reaches its
insertion on the greater tuberosity without significant tension.
Occasionally, this may require a sharp release of the coracohumeral
ligament at the base of the coracoid if this structure is tethering the
retracted tendon. However, with most of the smaller tears selected for
repair through this approach, mobilization is usually easily achieved
without the need for sharp releases.
the repaired rotator cuff is then prepared using a rongeur to remove
any bony excrescences or fibrous tissue and to yield a bleeding bony
base. Either suture anchor devices or sutures passed through bone
tunnels in the greater tuberosity can be used to repair the cuff. It is
this author’s preference to use sutures passed through bone tunnels, as
this technique allows more uniform compression of the tendon to the
surface of the tuberosity than the suture anchor method, which provides
more of a point contact type of fixation between the tendon and bone.
One to three bone tunnels are then created, depending on the size of
the tear to be repaired. The technique used by the author to create
these tunnels in the greater tuberosity involves the use of a curved
awl to start the tunnel proximally and then the use of a sharp
trocar-tipped needle to pierce the lateral cortex of the tuberosity
distally. Through each tunnel, two no. 1 or no. 2 braided nonabsorbable
sutures are passed, thus doubling the number of sutures available for
the repair. Each of the sutures is then passed through the torn tendon.
The sutures are usually placed in simple fashion, although the modified
Mason-Allen stitch is used for repairs of tissue of lesser quality. The
sutures are tied with the arm at the side in neutral to slight internal
rotation. After the tendon has been repaired, the deltoid split is
repaired, and the skin is closed with a subcuticular repair.
begun immediately to maintain the range of motion. Extension is
deferred early on to avoid unduly stressing the tendon repair. A sling
is used to prevent active use of the arm for approximately 6 weeks to
protect the tendon repair. Active use for activities of daily living is
allowed after 6 weeks, and
resistive
exercises are begun at 10 to 12 weeks postoperatively. Although the
rehabilitation may proceed more easily and less painfully than after
open repair (especially during the first few weeks), the rate of tendon
healing to bone is not affected by the technique of repair. The biology
of tendon healing still requires a period during which stresses across
the repair must be minimized to avoid rerupture of the repaired tendon.
in 1911, open repair has been the standard method. During the first
half of the twentieth century, the results of rotator cuff repair were
unpredictable, probably largely owing to the acromionectomy procedures
and transacromial approaches that were used. These procedures produced
damage to the deltoid and alteration of its normal fulcrum, resulting
in poor function and even inconsistent pain relief. Since the
introduction of anterior acromioplasty by Neer and the abandonment of
earlier acromionectomy techniques, the results of rotator cuff surgery
have improved significantly, yielding satisfactory outcomes in 85% to
90% of patients.
it affords wide exposure for access to even massive tears of the
rotator cuff. Such exposure is necessary when attempting to mobilize
the chronically contracted tendons in a large or massive tear. The
major disadvantage of this technique is that it involves incision of
the anterior deltoid to gain exposure and to perform the anterior
acromioplasty. This has the potential risk of deltoid dehiscence,
though this complication is uncommon when the deltoid is repaired and
protected properly in the early postoperative period. Greater
perioperative morbidity, as measured by the need for narcotic
analgesics and by longer hospital stays, is also cited as a relative
disadvantage of open repair. There has been a shift to arthroscopically
assisted rotator cuff repair for treating smaller tears and even more
recently to arthroscopic repair of many tears. Although patient
satisfaction and pain relief appear to be comparable for the results of
open repair and those of arthroscopic repair, the structural results
(i.e., anatomic healing of the repaired tendons to bone) of
arthroscopic repair appear to be inferior to those of open repair for
large and massive tears.
in the semisitting or beach-chair position using regional interscalene
block anesthesia. The patient is positioned so that the shoulder
protrudes over the side of the operating table so that the arm can be
extended and rotated during the procedure, particularly to gain access
to retracted posterior cuff tendons. The shoulder is gently manipulated
through a full passive range of motion to break up any capsular
adhesions that occasionally may be present. An anterosuperior
deltoid-splitting approach is used for the repair of most tears,
although a deltopectoral approach is favored for isolated subscapularis
tears. The preferred incision for most open repairs is a 6- to 7-cm
incision, which starts over the lateral aspect of the acromion and
proceeds to a point just lateral to the coracoid process. This yields a
cosmetically acceptable scar, as the incision approximates the skin
lines. A needle-tip electrocautery is used to incise the subcutaneous
layer and to widely undermine this layer to expose the underlying
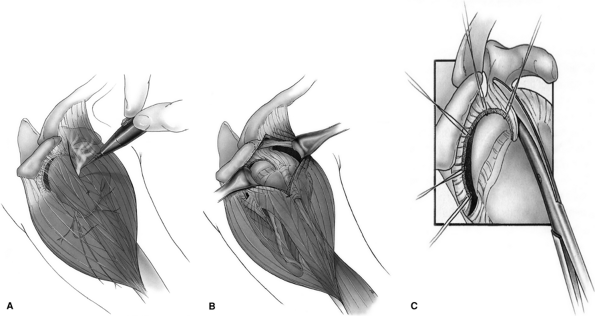
deltoid fascia. The deltoid split starts anterior to the
acromioclavicular joint and extends laterally 4 cm distal to the
anterolateral corner of the acromion (Fig. 39-2A).
A cuff of deltoid is left superiorly on the acromion to allow for a
secure deltoid repair. This split in the deltoid is centered over the
greater tuberosity to allow better exposure to the posterior cuff (Fig. 39-2B).
any spurs or excrescences from the acromial undersurface. The
coracoacromial ligament is released from the anterior aspect and
undersurface of the acromion. This ligament is typically partially
excised when there is a smaller tear but is preserved and later
repaired back to the acromion in massive tears, where there is concern
about the possibility of cuff failure and subsequent anterosuperior
instability. After the anterior acromion has been exposed and adherent
cuff and bursal tissue have been cleaned from its undersurface, a
beveled osteotome (with the bevel facing upward) is used to perform an
acromioplasty. The aim is to produce a smooth acromial undersurface,
and the amount of bone removal varies according to the anatomy. By
resecting only the downward projecting undersurface, effective
decompression can be achieved with minimal shortening of the acromion.
Osteophytes on the undersurface of the acromioclavicular joint are
removed with a rongeur. Excision of the distal clavicle is performed
only for preoperative acromioclavicular symptoms, and this is necessary
in only 10% to 15% of cases. When this is necessary, the author prefers
to resect the distal clavicle from below using a burr and rongeur so
that the superior ligamentous envelope can be preserved to avoid
microinstability of the acromioclavicular (AC) joint.
mobilization and repair of the torn tendons. At this point, the
characteristics of the tear are noted: size, shape, tendon involvement,
degree of retraction, and quality of the tissue available for repair.
The torn tendons are tagged with nonabsorbable sutures to assist with
mobilization. A blunt periosteal elevator is used to release bursal
adhesions, as well as to release adhesions between the tendons and
capsule on the articular side. With acute tears, where there are no
fixed contractures, mobilization proceeds quite easily. In large or
massive chronic tears, these blunt releases may not be sufficient to
restore mobile musculotendinous units to their insertion on the greater
tuberosity. The torn tendon may be tethered by the adjacent intact
tendon. Sharp release of the coracohumeral ligament at the base of the
coracoid may assist with mobilization of the supraspinatus tendon.
Additionally, as described by Bigliani, an “anterior interval slide” or
sharp release of the interval between the supraspinatus and
subscapularis tendons is performed when necessary (Fig. 39-2C). A similar release between the infraspinatus and supraspinatus is also occasionally needed.
excrescences and residual fibrous tissue down to a bleeding bony base.
The lesser tuberosity is similarly prepared if the subscapularis tendon
is torn. Multiple bone tunnels are constructed, as previously
described, using a sharp curved awl and a trocar-tipped needle. The
location and number of tunnels varies according to the size of the
tear. Through each
of
the tunnels, two no. 1 or no. 2 braided nonabsorbable sutures are
passed to maximize the number of sutures available for tendon-to-bone
repair and to disperse the stresses in the repaired tendons. Simple
sutures are preferred if the tendon is of stout quality, but modified
Mason-Allen sutures may also be used if the tissue is of poorer
quality. The sutures are tied with the arm at the side in slight
flexion and neutral to slight internal rotation. Tendon-to-tendon
sutures are passed to repair the intervals that have been released. If
the biceps tendon is intact in its groove, it is left alone. If there
is significant fraying of the tendon (>50% of the tendon thickness)
or if it is subluxed, tenodesis is performed, and the intra-articular
portion is excised. Using the techniques described, complete repair can
usually be achieved. However, occasionally with three- and four-tendon
tears, this is not possible, and partial repair is performed. In these
rare cases, the emphasis is on restoring tissue both anteriorly and
posteriorly, and there may be a residual defect superiorly. When the
tendon repair has been completed, the split in the deltoid is repaired
with no. 1 nonabsorbable braided sutures. A subcuticular skin closure
is then performed.
 |
|
Figure 39-2 A:
The deltoid split starts anterior to the acromioclavicular joint and extends in an anterolateral raphe for 4 cm distal to the anterolateral corner of the acromion. B: This deltoid split is centered over the greater tuberosity and affords good access to the torn tendons (especially posteriorly). C: A sharp release of the rotator interval and coracohumeral ligament to the base of the coracoid or “interval slide” assists with mobilization of a chronically retracted supraspinatus tendon. (From Post M, Bigliani LU, Flatow EL, et al. Rotator cuff repair. In: Post M, Bigliani LU, Flatow EL, et al., eds. The Shoulder: Operative Technique. Lippincott Williams & Wilkins; 1998
, with permission.) |
begun on the first postoperative day. These consist of pendulum
exercises, as well as passive elevation in the scapular plane and
passive external rotation (with the arm at the side). The degree of
motion allowed depends on several factors, such as which tendons were
involved, the tension on the repair, and the quality of the repaired
tissue. With most tears, approximately 140 degrees of elevation and 40
degrees of external rotation are allowed in the early postoperative
period. With subscapularis involvement, external rotation is usually
limited to zero to 20 degrees. A sling is used for 6 weeks to prevent
active use of the shoulder. More advanced stretching exercises, as well
as light active use of the arm for activities of daily living, are
added after 6 weeks. Resistive exercises are deferred for 3 months and
are progressed gradually. Appropriate rehabilitation, which is
supervised and directed by the surgeon, plays a crucial role in
achieving a satisfactory outcome and avoiding complications, such as
deltoid dehiscence and cuff tendon failure, after rotator cuff repair.
FT, Warren RF, Cavo C, et al. Arthroscopic assisted rotator cuff
repair: Results using a mini-open deltoid splitting approach. Arthroscopy. 1996;12:50–59.
LM, Griggs S, Cameron BD, et al. Prospective longitudinal analysis of
postoperative shoulder function: a ten-year follow-up study of
full-thickness rotator cuff tears. J Bone Joint Surg. 2001;83A:1052–1056.
DT II, Mack LA, Wang KY, et al. Repairs of the rotator cuff.
Correlation of functional results with integrity of the cuff. J Bone Joint Surg. 1991;73A:982–989.
JP, Bernot MP, Kuhlman JR, et al. Postoperative assessment of shoulder
function: a prospective study of full-thickness rotator cuff tears. J Shoulder Elbow Surg. 1996;5:449–457.
SC, Schaefer R. “Mini-open” versus traditional open repair in the
management of small and moderate size tears of the rotator cuff. Arthroscopy. 1993;9:365–366.
LE, Tetro AM, Blam O, et al. Natural history of asymptomatic rotator
cuff tears: a longitudinal analysis of asymptomatic tears detected
sonographically. J Shoulder Elbow Surg. 2001;10: 199–203.
