Proximal Humerus Fractures
-
Proximal humerus fractures comprise 4% to 5% of all fractures and represent the most common humerus fracture (45%).
-
The increased incidence in the older population is thought to be related to osteoporosis.
-
The 2:1 female-to-male ratio is likely related to issues of bone density.
-
The shoulder has the greatest range of
motion of any articulation in the body; this is due to the shallow
glenoid fossa that is only 25% the size of the humeral head and the
fact that the major contributor to stability is not bone, but a soft
tissue envelope composed of muscle, capsule, and ligaments. -
The proximal humerus is retroverted 35 to 40 degrees relative to the epicondylar axis.
-
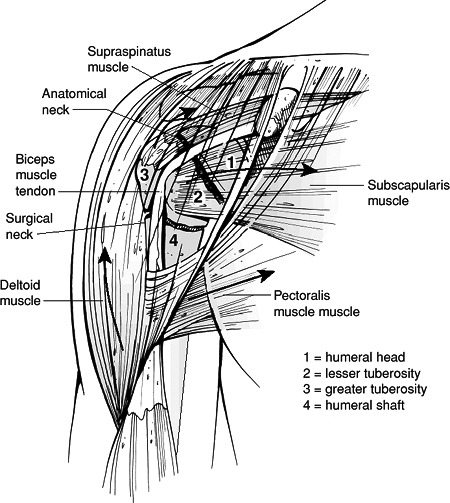
The four osseous segments (Neer) (Fig. 15.1) are:
-
The humeral head.
-
The lesser tuberosity.
-
The greater tuberosity.
-
The humeral shaft.
-
-
Deforming muscular forces on the osseous segments (Fig. 15.1):
-
The greater tuberosity is displaced superiorly and posteriorly by the supraspinatus and external rotators.
-
The lesser tuberosity is displaced medially by the subscapularis.
-
The humeral shaft is displaced medially by the pectoralis major.
-
The deltoid insertion causes abduction of the proximal fragment.
-
-
Neurovascular supply:
-
The major blood supply is from the anterior and posterior humeral circumflex arteries.
-
The arcuate artery is a continuation of
the ascending branch of the anterior humeral circumflex. It enters the
bicipital groove and supplies most of the humeral head. Small
contributions to the humeral head blood supply arise from the posterior
humeral circumflex, reaching the humeral head via tendo-osseous
anastomoses through the rotator cuff. Fractures of the anatomic neck
are uncommon, but they have a poor prognosis because of the precarious
vascular supply to the humeral head. -
The axillary nerve courses just
anteroinferior to the glenohumeral joint, traversing the quadrangular
space. It is at particular risk for traction injury owing to its
relative rigid fixation at the posterior cord and deltoid, as well as
its
P.166
proximity
to the inferior capsule where it is susceptible to injury during
anterior dislocation and anterior fracture-dislocation.
-
 |
|
Figure
15.1. Displacement of the fracture fragments depends on the pull of the muscles of the rotator cuff and the pectoralis major. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Most common is a fall onto an outstretched upper extremity from a standing height, typically in an older, osteoporotic woman.
-
Younger patients typically present with
proximal humeral fractures following high-energy trauma, such as a
motor vehicle accident. These usually represent more severe fractures
and dislocations, with significant associated soft tissue disruption
and multiple injuries. -
Less common mechanisms include:
-
Excessive shoulder abduction in an individual with osteoporosis, in which the greater tuberosity prevents further rotation.
-
Direct trauma, usually associated with greater tuberosity fractures.
-
Electrical shock or seizure.
-
Pathologic processes: malignant or benign processes in the proximal humerus.
P.167 -
-
Patients typically present with the upper
extremity held closely to the chest by the contralateral hand, with
pain, swelling, tenderness, painful range of motion, and variable
crepitus. -
Chest wall and flank ecchymosis may be present and should be differentiated from thoracic injury.
-
A careful neurovascular examination is
essential, with particular attention to axillary nerve function. This
may be assessed by the presence of sensation on the lateral aspect of
the proximal arm overlying the deltoid. Motor testing is usually not
possible at this stage because of pain. Inferior translation of the
distal fragment may result from deltoid atony; this usually resolves by
4 weeks after fracture, but if it persists, it must be differentiated
from a true axillary nerve injury.
-
Trauma series, consisting of AP and lateral (“Y”) views in the scapular plane as well as an axillary view.
-
Axillary is the best view for evaluation
of glenoid articular fractures and dislocations, but it may be
difficult to obtain because of pain. -
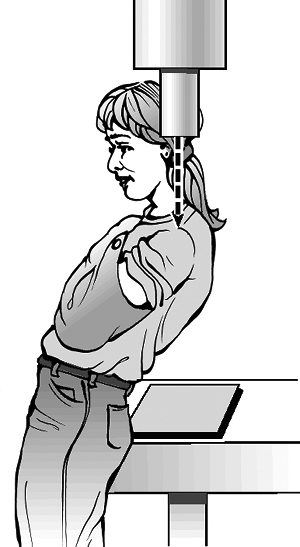
Velpeau axillary: If a standard axillary
cannot be obtained because of pain or fear of fracture displacement,
the patient may be left in the sling and leaned obliquely backward 45
degrees over the cassette. The beam is directed caudally, orthogonal to
the cassette, resulting in an axillary view with magnification (Fig. 15.2). -
Computed tomography is helpful in
evaluating articular involvement, degree of fracture displacement,
impression fractures, and glenoid rim fractures. -
Magnetic resonance imaging is generally
not indicated for fracture management, but it may be used to assess
rotator cuff integrity.
-
Four parts: These are the greater and lesser tuberosities, humeral shaft, and humeral head.
-
A part is defined as displaced if >1 cm of fracture displacement or >45 degrees of angulation.
-
Fracture types include:
-
One-part fractures: no displaced fragments regardless of number of fracture lines.
-
 |
|
Figure 15.2. A Velpeau axillary view can be obtained without abducting the shoulder.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Minimally displaced fractures
-
Up to 85% of proximal humerus fractures are minimally displaced or nondisplaced.
-
Sling immobilization or swathe for comfort.
-
Frequent radiographic follow-up is important to detect loss of fracture reduction.
-
Early shoulder motion may be instituted at 7 to 10 days if the patient has a stable or impacted fracture.
-
Pendulum exercises are instructed initially followed by passive range-of-motion exercises.
-
At 6 weeks, active range-of-motion exercises are started.
-
Resistive exercises are started at 12 weeks.
-
-
Two-part fractures
-
Anatomic neck fractures: These are rare
and difficult to treat by closed reduction. They require open reduction
and internal fixation (ORIF) (younger patients) or prosthesis (e.g.,
shoulder
P.169
hemiarthroplasty) and are associated with a high incidence of osteonecrosis.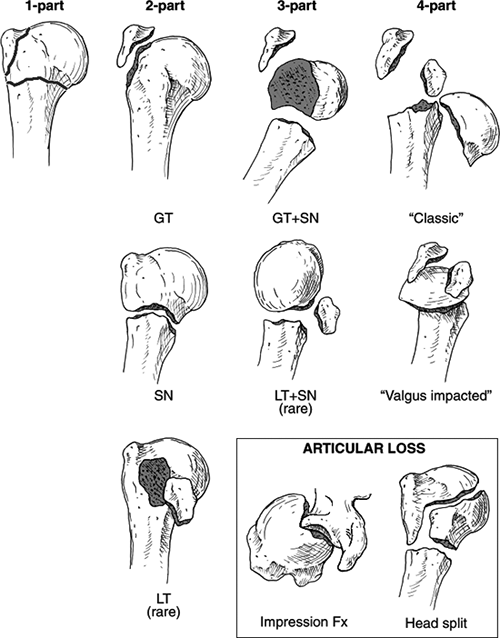 Figure 15.3. The Neer classification of proximal humerus fractures.(Reprinted with permission from Neer CS. Displaced proximal humeral fractures: I. Classification and evaluation. J Bone Joint Surg Am 1970;52:1077–1089.).)
Figure 15.3. The Neer classification of proximal humerus fractures.(Reprinted with permission from Neer CS. Displaced proximal humeral fractures: I. Classification and evaluation. J Bone Joint Surg Am 1970;52:1077–1089.).) -
Surgical neck fractures
-
If the fracture is reducible and the
patient has good-quality bone, one can consider fixation with
percutaneously inserted terminally threaded pins.-
Problems associated with multiple pin
fixation include nerve injury (axillary), pin loosening, pin migration,
and inability to move the arm.
-
-
Irreducible fractures (usually interposed
soft tissue) and fractures in osteopenic bone require ORIF with pins,
intramedullary nails with or without a supplemental tension band, or
plate and screws.
-
-
Greater tuberosity fractures: If they are
displaced more than 5 to 10 mm (5 mm for superior translation), they
require ORIF with or without rotator cuff repair; otherwise, they may
develop nonunion and subacromial impingement. A greater tuberosity
fracture associated with anterior dislocation may reduce on reduction
of the glenohumeral joint and be treated nonoperatively. -
Lesser tuberosity fractures: They may be
treated closed unless displaced fragment blocks internal rotation; one
must rule out associated posterior dislocation.
P.170 -
-
Three-part fractures
-
These are unstable due to opposing muscle
forces; as a result, closed reduction and maintenance of reduction are
often difficult. -
Displaced fractures require operative fixation, except in severely debilitated patients or those who cannot tolerate surgery.
-
Younger individuals should have an
attempt at ORIF; preservation of the vascular supply is of paramount
importance with minimization of soft tissue devascularization. -
Older patients may benefit from primary prosthetic replacement (hemiarthroplasty).
-
-
Four-part fractures
-
Incidence of osteonecrosis ranges from 13% to 35%.
-
ORIF may be attempted in young patients
if the humeral head is located within the glenoid fossa and there
appears to be soft tissue continuity. Fixation may be achieved with
multiple Kirschner wire, screw fixation, suture or wire fixation, or
plate and screws. -
Primary prosthetic replacement of the humeral head (hemiarthroplasty) is the procedure of choice in the elderly.
-
Hemiarthroplasty is associated with unpredictable results from the standpoint of function.
-
-
Four-part valgus impacted proximal
humerus fractures represent variants that are associated with lower
rate of osteonecrosis and have had better reported results with ORIF (Fig. 15.4).
-
-
Fracture-dislocations
-
Two-part fracture-dislocations: may be treated closed after shoulder reduction unless the fracture fragments remain displaced.
-
Three- and four-part
fracture-dislocations: ORIF is used in younger individuals and
hemiarthroplasty in the elderly. The brachial plexus and axillary
artery are in proximity to the humeral head fragment with anterior
fracture-dislocations. -
Recurrent dislocation is rare following fracture union.
-
Hemiarthroplasty for anatomic neck fracture-dislocation is recommended because of the high incidence of osteonecrosis.
-
They may be associated with increased incidence of myositis ossificans with repeated attempts at closed reduction.
-
-
Articular surface fractures
-
These are most often associated with posterior dislocations.
-
Patients with >40% of humeral head
involvement may require hemiarthroplasty; ORIF should initially be
considered in patients <40 years of age, if possible.
-
 |
|
Figure 15.4. Drawing showing the anatomy of a valgus-impacted four-part fracture.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Vascular injury: This is infrequent (5%
to 6%); the axillary artery is the most common site (proximal to
anterior circumflex artery). The incidence is increased in older
individuals with atherosclerosis because of the loss of vessel wall
elasticity. -
Neural injury
-
Brachial plexus injury: This is infrequent (6%).
-
Axillary nerve injury: This is
particularly vulnerable with anterior fracture-dislocation because the
nerve courses on the inferior capsule and is prone to traction injury
or laceration. Complete axillary nerve injuries that do not improve
within 2 to 3 months may require electromyographic evaluation and
exploration.
-
-
Chest injury: Intrathoracic dislocation
may occur with surgical neck fracture-dislocations; pneumothorax and
hemothorax must be ruled out in the appropriate clinical setting. -
Myositis ossificans: This is uncommon and
is associated with chronic unreduced fracture-dislocations and repeated
attempts at closed reduction. -
Shoulder stiffness: It may be minimized
with an aggressive, supervised physical therapy regimen and may require
open lysis of adhesions for recalcitrant cases. -
Osteonecrosis: This may complicate 3% to
14% of three-part proximal humeral fractures, 13% to 34% of four-part
fractures, and a high rate of anatomic neck fractures. -
Nonunion: This occurs particularly in
displaced two-part surgical neck fractures with soft tissue
interposition. Other causes include excessive traction, severe fracture
displacement, systemic disease, poor bone quality, inadequate fixation,
and infection. It may be addressed with ORIF with or without bone graft
or prosthetic replacement. -
Malunion: This occurs after inadequate
closed reduction or failed ORIF and may result in impingement of the
greater tuberosity on the acromion, with subsequent restriction of
shoulder motion.
