Posttraumatic Conditions
– HIP > Part B – Evaluation and Treatment of Hip Disorders > 6 –
Posttraumatic Conditions
posttraumatic arthritis, osteonecrosis, malunion, and nonunion.
End-stage arthritis may develop quickly after the injury or it may
develop years later. In many patients, treatment involves removal of
the current hardware and conversion to total hip arthroplasty.
Osteoporosis, bone loss, and heterotopic bone formation complicate
total hip arthroplasty. Hip salvage via other procedures such as
refixation of the fracture, valgus osteotomy, or femoral head reshaping
may be considered for patients with a viable femoral head.
Hip dislocations may damage the blood supply to the femoral head,
leading to late osteonecrosis, a risk increased in direct proportion to
the length of time the hip remains dislocated. Cartilage damage from
the initial injury predisposes patients to later arthritis. Surgical
treatment of acetabular fractures may lead to iatrogenic arthritis from
intra-articular hardware or malreduction. Elderly patients are at risk
for osteoporotic fracture patterns that are difficult to reduce and
stabilize effectively.
femoral head, malunion, nonunion, and severe arthritis. In the older
patient, these conditions are treated with hip replacement, whereas in
the younger patient hip salvage may be possible. Hip salvage may be
achieved by revision fixation, bone grafting, or femoral head
reshaping. Intertrochanteric fractures typically are treated with a hip
screw and side plate or an intramedullary hip screw. In the young
patient, nonunion can occur, and revision internal fixation with bone
grafting may be indicated. In the elderly patient, a nonunion or
malunion is best treated with arthroplasty.
trauma to the acetabulum or proximal femur. Acetabular fractures are
thought to occur at a rate of 3 per 100,000 population per year. The
rate of posttraumatic arthritis for all acetabular fractures is 20% to
30%. Posterior wall fractures represent about 25% of all fractures and
are at high risk for late arthritis. The elderly patient and those with
more comminuted fractures have worse results from initial reduction and
fixation than younger patients with simple fracture patterns. Almost
10% of fractures have severe initial damage to the femoral head or
acetabulum, which is best treated with acute arthroplasty.
each year in the United States, approximately 40% involve the femoral
neck. Femoral neck fractures are especially common in the elderly
patient. Of those treated with open reduction and internal fixation,
15% develop osteonecrosis, 30% develop nonunion, and 20% to 35% require
revision surgery. Intertrochanteric fractures also are common in the
osteoporotic individual, and rates in elderly women are estimated at 63
per 100,000 population. Failure of fixation is related to fracture
stability and the amount of comminution. In one study, 43% of fractures
were classified as unstable and up to 50% of unstable intertrochanteric
fractures may develop nonunion after internal fixation.
acetabulum resulting from an acetabular fracture or a hip dislocation
can lead to arthritic changes in the hip. Cartilage damage occurs to
the area of the joint next to the fracture and is termed marginal
impaction. Impacted cartilage must be elevated and supported with bone
graft during fixation. Postfracture damage to the femoral head also can
occur secondary to nonconcentric reduction or intra-articular bodies
while the patient awaits surgical fixation. Damage to 40% or more of
the weight-bearing articular cartilage, the femoral head, or acetabular
surface is an indication for acute total hip replacement.
of the blood supply to the femoral head. Disruption can occur by
traumatic dislocation of the femoral head, by traumatic injury from hip
fracture displacement, from elevated
intracapsular
pressure, or by surgical injury to the blood supply. The lateral
epiphyseal artery (the end branch of the medial circumflex artery),
which supplies the femoral head, enters the femoral head through the
obturator externus muscle on the posterior aspect of the femoral neck.
The risk of femoral head osteonecrosis is directly proportional to both
the length of time that a hip is dislocated and the amount of
displacement of a femoral neck fracture. Increased pressure in the hip
joint by bleeding from an intracapsular femoral neck fracture
tamponades the blood supply to the femoral head and also may contribute
to the development of osteonecrosis.
|
TABLE 6-1 Conditions After HIP Trauma
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
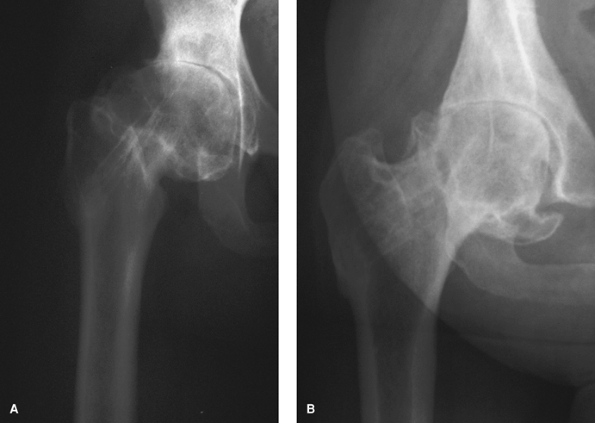
Figure 6-1 Patient with malunion of the femoral neck after pinning of a slipped capital femoral epiphysis. A: Anteroposterior radiograph showing the development of severe arthritis from femoroacetabular impingement. B: An oblique view gives a “true” view of the femoral neck and osteophytes and is helpful for preoperative templating.
|
including the superior and inferior gluteal, medial femoral circumflex,
obturator, fourth lumbar, and iliolumbar arteries. Disruption of the
entire blood supply requires stripping of the soft tissues from the
inner and outer tables of the acetabulum. Avoidance of excessive
stripping during extensile approaches is critical when stabilizing
complex acetabular fractures.
including posttraumatic arthritis, femoroacetabular impingement, and
limb-length discrepancy. Malreduction of an acetabular fracture causes
joint incongruity. Residual fracture step-off increases contact
pressure in the hip and leads to cartilage wear, arthritis, and poor
clinical outcomes. Malunion of a femoral neck or intertrochanteric
fracture leads to shortening of the hip with resultant limb-length
discrepancy and Trendelenburg gait. Shortening can occur when a
fracture is treated with parallel screw or sliding hip screw fixation.
Malunion of a femoral neck fracture results in an abnormal head/neck
angle, with retroversion and varus deformity of the femoral neck. The
abnormal neck/shaft angle causes the anterior aspect of the neck to
impinge on the acetabulum and is termed femoroacetabular impingement.
Impingement damages the superior anterior
acetabular labrum and leads to osteophyte formation and arthritis through a cam mechanism (Fig. 6-1).
are more common after unstable fractures. Factors related to the
nonunion include the stability and comminution of the initial fracture
and the quality of the reduction and fixation of the fracture.
Technical problems of initial fixation such as malreduction and
incorrect hardware selection or placement can lead to nonunion. The
role of bone mineral density is controversial.
posttraumatic conditions of the hip. Osteoarthritis is graded
radiographically by an evaluation of the minimal joint space or by the
system of Kellgren and Lawrence. Osteonecrosis is graded according to
the modified system of Ficat by its appearance on scans and plain
radiographs ranging from grade 1 (a lesion seen only on magnetic
resonance imaging) to grade 4 (severe degenerative joint disease on
radiographs). Nonunions are graded as atrophic or hypertrophic.
Individual fracture patterns can be classified using the
Arbeitsgemeinschaft fur Osteosyntheses/Orthopaedic Trauma Association
(AO/OTA) classification system, which numerically lists fractures by
site and pattern. Acetabular fractures are classified using the system
of Letournel and Judet into elementary and associated fracture
patterns. Femoral neck fractures are classified as stable or unstable
based on the amount of fracture displacement. Intertrochanteric
fractures are classified as stable or unstable depending on the number
of fracture fragments, the presence of an intact medial or lateral
buttress, and the direction of the fracture. Many fracture
classification systems lack interobserver and intraobserver reliability.
specifics about the energy (high or low) that caused the fracture,
patient age, comorbidities, and a determination of the presence of
osteoporosis. Any patient who fractured a bone after the age of 50
years is at high risk for osteoporosis and should be considered for
assessment with bone densitometry. Other evaluations should include the
patient’s gait to determine if a limp is present, measurement of limb
lengths for discrepancy, measurement of hip motion, and examination of
the patient and signs of infection. Patients should be questioned
carefully about severity and pattern of pain, the level of hip
dysfunction, and infection issues, including previous wound healing
problems.
evaluate the initial injury and to assess serial changes in the hip
over time. Up-to-date anteroposterior and lateral views of the hip and
an anteroposterior view of the pelvis are required. If substantial
rotational contracture of the hip exists, oblique views can be helpful (Fig. 6-1).
In the case of an acetabular fracture, Judet views of the pelvis can
help assess the columns and walls of the acetabulum. A computed
tomography scan is used to assess for nonunion of the acetabulum or
hip, bone defects of the acetabulum, and heterotopic ossification. In
particular, a transverse nonunion of the acetabulum, termed a pelvic
discontinuity, requires refixation of the pelvis and must be evaluated
on the Judet views and computed tomography scan.
nonoperative modalities should be the first line of treatment.
Interventions include activity modification, weight reduction if the
patient is obese, ambulatory assistance devices (walker, wheelchair, or
motorized scooter, especially if the patient is elderly and infirm),
pain medications (such as acetaminophen, nonsteroidal anti-inflammatory
medications, and narcotic agents), and shoe lifts for limb-length
discrepancy. Patients with healing fractures require careful
radiographic follow-up until fracture union. In the event of a malunion
or nonunion, the younger patient may be at risk for early posttraumatic
arthritis and the older patient may be at risk for substantial bone
loss from screw cutout. In either case, earlier surgery may lead to a
better outcome.
should be assessed for infection. Infection may have caused the failure
of previous treatment, and if present, it will affect the management of
the patient. Erythrocyte sedimentation rate and C-reactive protein
serve as screening tools. Any patient with elevation of these values
should undergo hip aspiration under fluoroscopy. White blood
cell–tagged bone scans also may be used to evaluate for infection. In
all cases, intraoperative frozen sections should be sent to assess for
infection, and intraoperative cultures should be taken.
routine, and the treatment plan should be made well in advance of the
surgical date. Templating should be performed on the preoperative
radiographs ahead of time to help determine what implant systems will
be required. Operative reports from previous surgeries facilitate
ordering the correct tools for hardware removal. A broken-screw removal
set and a high-speed metal cutting burr should be available in case
screw heads are stripped.
and usually have been in poor health since their initial injury.
Contractures or bed sores may have developed from lack of activity. The
patient should be evaluated for systemic problems, may require
preoperative evaluation by a cardiologist, and may need an intensive
care unit bed postoperatively. It is
helpful
to plan for a geriatrician or hospitalist to follow the patient in the
postoperative period because postoperative medical complications such
as delirium are common. The patient and family should be prepared for a
lengthy recovery and the possibility of complications, including death.
 |
|
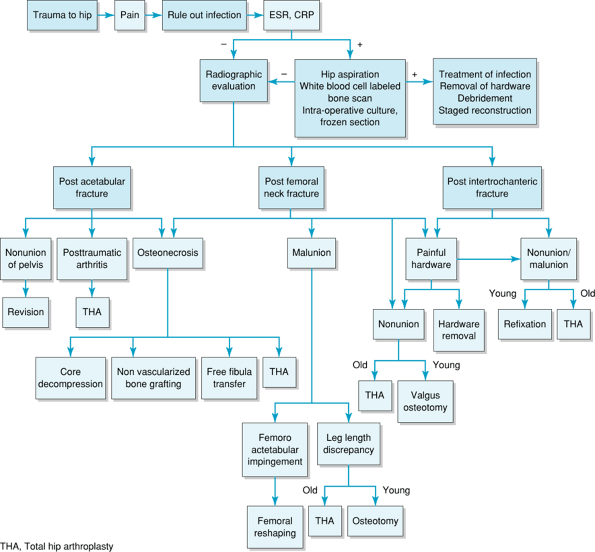
Figure 6-2 Diagnostic workup algorithm.
|
of the femoral head, malunion, or cartilage damage. Because total hip
replacement has been so successful, it is now the most commonly used
treatment option. Alternate options include hip resection or fusion,
but both lead to substantial leg-length discrepancy and hip dysfunction
and are not well accepted by patients.
and an uncemented acetabular component with additional screw fixation
should be used. Existing hardware from the previous fixation, including
posterior wall plates or column screws, should be removed only if they
impede reaming or cup insertion. The sciatic nerve is at great risk
when a posterior column plate is removed, and care must be taken with
retractor placement. Bone defects must be expected, depending on the
initial fracture pattern: The most common defects occur posteriorly
after posterior wall fractures or anteriorly and medially after
osteoporotic acetabular fractures. Bone graft from the arthritic
femoral head should be used first, and then cancellous allograft chips
as needed. Each patient should be examined intraoperatively for pelvic
dissociation; if present, the posterior
column
must be stabilized with a contoured reconstruction plate. The defect
then is packed with bone graft, and an uncemented cup is inserted with
multiple screws. For very large defects, an acetabular autograft
(protected by a cage) may be required.
nonunion, or malunion, generally are treated with hip arthroplasty.
Arthroplasty requires removal of the existing screws, but a standard
femoral stem usually can be inserted. Pain after hip fracture repair
may occur directly over hardware such as a sliding hip screw or
cannulated screw or it may be secondary to screws having backed out
substantially. However, before considering hardware removal, fracture
nonunion should be excluded by computed tomography scan.
 |
|
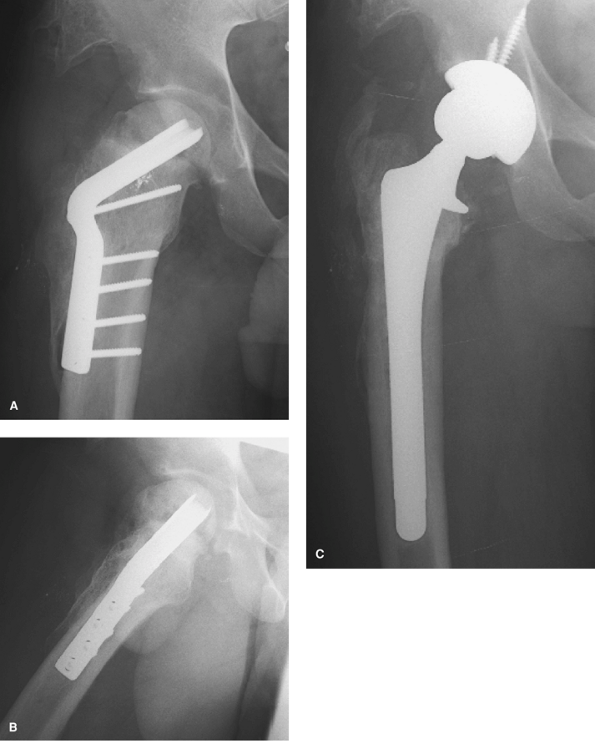
Figure 6-3 Young patient with femoral neck nonunion treated with valgus osteotomy and blade plate fixation. A: Anteroposterior view of the hip showing the blade plate. B: Lateral view of the hip reveals that the femoral head has collapsed from osteonecrosis. C: Anteroposterior view of the hip showing the uncemented total hip arthroplasty after blade plate removal.
|
should be considered for hip salvage surgery. For the young patient
with femoral neck nonunion, an intertrochanteric valgus producing
osteotomy converts shear forces into compression forces, allowing for
fracture healing (Fig. 6-3). The osteotomy is performed on a fracture table with fluoroscopy, and a 95-degree blade plate is used for fixation.
impingement. A femoral reshaping procedure can remove impinging
osteophytes to prevent additional arthritic
changes.
A trochanteric slide osteotomy approach to the hip avoids damage to the
femoral head’s blood supply. A burr is used to remove the impinging
osteophytes.
|
TABLE 6-2 Tips for Total HIP Replacement After Failed Treatment for Intertrochanteric Fracture
|
||||||
|---|---|---|---|---|---|---|
|
malunions should be treated with prosthetic replacement.
Hemiarthroplasty may be used in the elderly patient with intact
acetabular cartilage. Some technical difficulties of total hip
replacement should be recognized and are summarized in Table 6-2.
The previous scar from internal fixation may be too far anterior,
requiring a second incision. Care must be taken during exposure because
a hip contracture is usually present, making exposure difficult.
Fracture of the femur or ankle may occur by overzealous retraction. The
greater trochanter usually is widened and partially healed with callus
and heterotopic ossification. A modified direct lateral or posterior
approach can be used per surgeon preference. In some cases, the
trochanteric fragment has not healed to the femur, and a trochanteric
slide approach can be used. The hip should be exposed and dislocated
before hardware removal.
head, producing cartilage damage and a bony defect in the acetabulum.
In such a case, the remains of the femoral head should be used to graft
the defect, and an uncemented cup should be inserted. A bony defect of
the medial proximal femur often is present, leading to the need for a
calcar-replacing femoral prosthesis. A cemented or uncemented
prosthesis can be used, but the stem should extend past the final screw
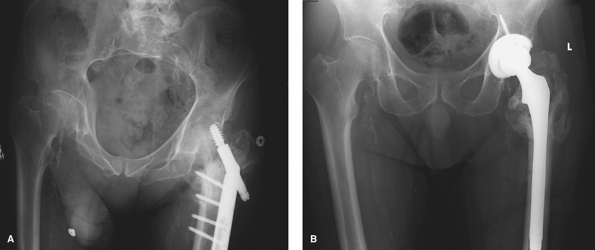
hole to avoid a stress riser (Fig. 6-4).
Previous screw holes should be plugged to prevent cement extravasation.
Careful trial reduction and intraoperative radiographs are recommended
to help ascertain whether the appropriately sized calcar buildup has
been used. If the calcar buildup is too small, the hip will remain
short and instability may result. Because instability is a larger
concern than wear in these elderly patients, a large femoral head
should be used. During closure, care should be taken with the greater
trochanter. If unstable fracture lines remain, the trochanter can be
stabilized with a claw and cables or wires.
 |
|
Figure 6-4 Elderly man with intertrochanteric fracture nonunion and sliding hip screw cutout. A: Anteroposterior view of the hip shows nonunion of the fracture and collapse. B:
Anteroposterior view of the hip showing a long-stemmed uncemented prosthesis used to bypass screw holes with calcar buildup for leg-length restoration. |
acetabulum, revision fixation with bone grafting is an option. A
95-degree fixed-angle blade-plate device can be inserted using the
intact inferior portion of the femoral head for fixation.
posttraumatic hip problems are case series. Little is known about
outcome measures in these patient groups, and no studies in the
literature are randomized or controlled. This lack of large,
investigative studies may reflect the fact that the numbers of patients
with these posttraumatic problems is small and that the spectrum of
failure mechanisms is wide.
treatment of acetabular fractures with total hip arthroplasty. In one
case series, 80% of patients had good or excellent results at
intermediate follow-up. Excessive medialization of the acetabular
component occurred in 10% of patients, and the difficulty of acute
arthroplasty was stressed. Several authors have reported the results of
late total hip arthroplasty for acetabular fractures: With modern
implants, 90% have good to excellent results at intermediate follow-up.
The procedures were noted to be more difficult with more blood loss
than with primary hip arthroplasty. Extended liners and additional bone
grafts often were required. Some reports have shown increased evidence
of component loosening that is thought to be related to the young age
and activity of patients at the time of hip replacement.
of femoral neck nonunion or osteonecrosis with total hip replacement.
Results are slightly inferior to those of primary total hip
arthroplasty, with higher rates of dislocation and trochanteric
complications. Valgus-producing osteotomies have been reported as
leading to healing of femoral neck nonunions in 80% of cases. However,
patients often continue to have a limp from abductor weakness.
Osteonecrosis may occur later after osteotomy, requiring subsequent hip
replacement. The results of femoral reshaping procedures for
femoroacetabular impingement from malunion of the femoral neck are
preliminary: One case series of the use of a trochanteric flip
osteotomy and femoral head reshaping showed excellent pain relief.
Long-term follow-up is needed to determine whether arthrosis is
prevented.
fractures with bone grafting and revision fixation are limited, but
available reports show 80% to 95% healing rate after the use of a
fixed-angle 95-degree blade-plate device in selected patients.
Arthroplasty for failed intertrochanteric fractures has been reported
to have 90% good to excellent results at intermediate follow-up. These
cases were technically difficult, and long-stemmed and calcar-replacing
implants commonly were used.
followed for 5 days. Postoperative radiographs should be scrutinized
carefully for iatrogenic fractures. Hip dislocation precautions
relative to the specific operative approach should be followed.
Weight-bearing restrictions depend on the stability of the components
achieved intraoperatively. If at all possible, weight bearing should be
allowed as tolerated because elderly patients often have difficulty
following weight-bearing restrictions. Radiographs should be obtained
and assessed during the postoperative year to document component
stability and bone in-growth.
restricted for 6 weeks after surgery and then may be advanced per the
patient’s tolerance. Radiographs must be assessed carefully to monitor
healing of the femoral neck and osteotomy and to monitor for the
development of osteonecrosis of the femoral head. If the fracture does
not heal or if substantial osteonecrosis develops, the patient is best
treated with hip replacement.
be started immediately. Active hip abduction exercises should be
restricted, and hip flexion >90 degrees should be restricted for 6
weeks to allow for osteotomy healing. Strengthening, stretching, and
full weight bearing begin thereafter. The hip should be followed
radiographically for trochanteric healing, osteonecrosis, and arthritic
changes.
