Posterior and Multidirectional Instability of the Shoulder
difficulties in making the appropriate diagnosis. Anterior instability
due to a macrotraumatic event is simple to diagnose and treat. With
more subtle events, in which the direction of instability is not
readily obvious, treatment is significantly more complex. The problem
is usually created by the existence of multidirectional instability
(MDI) in an individual. The balance of stability versus mobility in the
glenohumeral joint is what allows a wide range of motion and
performance of overhead activities. Finding this balance, however, is
especially difficult in cases of posterior and MDI. The axiom of
exhausting conservative management is critically important in this
population, especially as it applies to those whose instability is
proportional to their leisure activity level. The disability associated
with posterior subluxation is variable. Typically, activities of daily
living and work functions are not limited by recurrent posterior
subluxation. Participation in sports is generally more troublesome,
often requiring modification or complete elimination of the activity.
Even though it is not appropriate to terminate someone’s hobbies as
they affect instability, it certainly should be taken into
consideration in situations where there is a significant vulnerability
to further injury.
surgery, as well as genetics, should be practiced in these cases.
Problems with posterior and MDI may be attributable not only to
activity level but also to inherited anatomy and laxity. In Neer and
Foster’s original 1980 study describing the capsular shift procedure,
all 40 shoulders had inferior instability, with generalized ligamentous
laxity noted in 17 patients.
straightforward and easily solved by addressing the posterior
structures only. This chapter will discuss MDI as a separate entity in
most sections.
underestimated historically, likely because of difficulties in
diagnosis. The incidence of posterior instability has been estimated at
5% of all instability, with the majority being anterior. Recently, with
increasing use of shoulder arthroscopy, the
incidence has risen. The understanding of the condition has also increased significantly.
infrequent basis. This form of instability results from some
combination of excessive tissue compliance, muscular dyscoordination,
and occasionally inadequacy of the glenoid concavity. With increasing
understanding of the pathophysiology of instability—and especially
understanding problems about the rotator interval—the incidence has
increased in proportion to other instabilities, with many surgical
failures being attributed to a lack of recognition of an additional
direction of instability.
instability is difficult to ascertain. Several studies are available
that summarize the impact of selective cutting of various sections of
the glenohumeral joint capsule and its intrinsic ligaments. The
influence of passive and active stabilizers of the shoulder in the most
clinically relevant position of 90 degrees of forward flexion and
varying degrees of rotation has been studied. Of the muscles tested,
the subscapularis contributed the most to resisting a subluxation
force. The coracohumeral ligament was an effective contributor in
neutral humeral rotation, and the posterior-inferior glenohumeral
ligament was an effective contributor in internal humeral rotation. The
long head of the biceps was found to reduce the subluxation force in
neutral rotation and internal rotation but became less important with
external rotation.
rotated and adducted shoulder, the superior glenohumeral ligament
(SGHL) is the most important stabilizer. At 45-degree abduction, the
anterior band of the inferior glenohumeral ligament is the primary
restraint to inferior translation in neutral or internal rotation,
whereas the posterior band of the inferior glenohumeral ligament is the
primary restraint in external rotation.
1.5 Nm was applied while selective sectioning was performed. With
regard to the posterior structures, the infraspinatus and teres minor
were the primary stabilizers to internal rotation for the first 45
degrees of abduction, with the lower half of the posterior capsule
active from 45 to 90 degrees. In addition, no cases of posterior
subluxation occurred with intact anterior structures, thus giving
credence to the circle concept of instability.
be a contributory factor in the etiology of the instability pattern. In
addition, the concept of static posterior subluxation with the possible
contribution to later degenerative arthritis has also been espoused.
Patients with this diagnosis who have been followed for the longest
period of time appear to progress from subluxation to degenerative
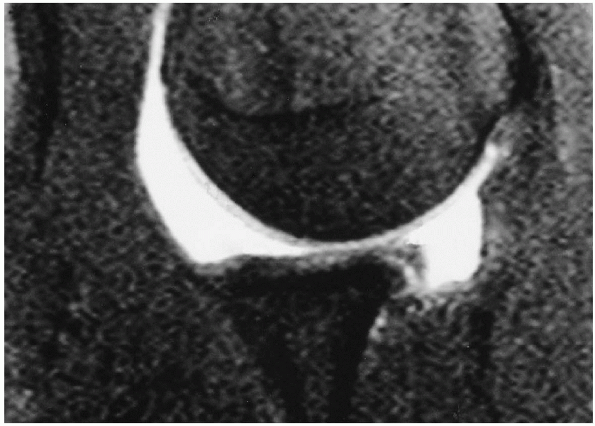
joint disease at a relatively young age (Fig. 18-1).
 |
|
Figure 18-1 MRI with gadolinium arthrogram depicting static posterior subluxation in a 30-year-old patient.
|
abnormalities, whether from instability, labral lesions, or arthrosis.
The musculature most susceptible to this includes the serratus anterior
and trapezius. Scapular instability has been found in as many as 100%
of instability problems. The abnormalities in muscle function are
thought to occur as a result of a decreased ability of the musculature
to exert torque and stabilize the scapula, as well as a disorganization
of the normal muscle firing patterns.
understanding of shoulder instability, especially MDI, has been the
delineation of the pathophysiology associated with lesions of the
rotator interval. This area is a triangular space, with its apex
centered at the transverse humeral ligament over the biceps sulcus,
having its greatest dimension at the base of the coracoid process. The
interval is a section of the glenohumeral joint capsule that is
bordered superiorly by the anterior margin of the supraspinatus tendon
and inferiorly by the superior border of the subscapularis tendon. The
coracohumeral ligament (CHL) strengthens the interval, as does the
SGHL, which courses from the anterosuperior labrum deep to the
substance of the rotator interval capsule and the CHL to insert near
the lesser tuber osity (Fig. 18-2).
contribute to humeral head translations, as well as play a significant
role in posterior stability of the joint. In one cadaveric study, a
radio frequency probe was used to perform a thermal capsuloplasty of
the rotator interval. An electromagnetic tracking device was used to
measure anterior and posterior glenohumeral translations. Anterior
translation was decreased by 31.5%, whereas posterior translation was
decreased by 43.1% while applying a 10 N load. Clinical studies have
also documented the beneficial effect of rotator interval closure in
supplementing open stabilizations, as well as in selected cases of MDI.
 |
|
Figure 18-2 Wide rotator interval in an active overhead athlete with signs of MDI.
|
associated with electrical shocks and seizure disorders. The effect of
an excessive electrical charge and a tonic seizure is to predominantly
activate the posterior rotator cuff musculature. This can cause a
posterior dislocation, which is missed by physicians and other health
care providers upon first presentation in up to 50% of cases.
expanded to include other mechanisms. A common mode involves a
posterior force applied to the arm while it is in a forward flexed,
adducted, and internally rotated position. Most commonly, this problem
is noted in football players who block with their arms in such a
position. For that reason, offensive linemen appear to have the largest
incidence of this problem relative to other positions.
gradual phenomenon that is a spectrum of pathologies. Most commonly,
patients have evidence of subtle laxity in both shoulders. This subtle
congenital laxity, superimposed on the performance of repetitive
overhead activities, leads to a gradual stretching of the restraining
structures and symptomatic instability. A critical distinction is the
separation of laxity from instability. In many situations, the
contralateral, asymptomatic shoulder exhibits significant laxity but
not symptomatic instability. This needs to be carefully considered in
the treatment.
instability patterns; however, in MDI patients, this preexisting laxity
may be more significant. Samples of shoulder capsule and skin from 25
patients with anterior instability, MDI, failed MDI surgery, as well as
patients with no history of instability were analyzed for collagen
characteristics and elastin density. Patients in the anterior
instability and MDI groups were not statistically different; however,
patients who failed MDI surgery had smaller fibrils and decreased
density of collagen, as well as an increase in elastin density. This
lends credence to a genetic predisposition to shoulder laxity in this
subgroup.
of the patients, there are variations in the anatomic findings that may
impact the degree and type of instability. In a study of 10 adult
glenohumeral cadaveric joints sectioned in the abducted, externally
rotated position, 80% had a capsular origin from the labrum, whereas in
20% it originated solely from the glenoid neck. This correlated closely
to an embryological study in which 77% of the glenohumeral ligaments
originated from the labrum and 23% from the glenoid neck. These
variables are important to note because they may impact not only laxity
and/or instability but also surgical repair. Repair of a normal
anatomic variant would regrettably result in an equivocal surgical
outcome.
-
A thorough history and physical examination are imperative in patients with recurrent instability.
-
The report of the initial episode of instability is key to determining the direction(s) of pathology.
-
Factors that determine the direction and
type of instability are: the position of the arm when symptoms occur,
the intensity of the force leading to the episode, and the number and
types of recurrences. -
In addition, radiographs from any of the earlier events are helpful to confirm the direction of instability.
-
The type and mechanism of the inciting event in the patient’s instability are critical to the diagnosis.
-
The less traumatic the episode, the more
likely there is generalized ligamentous laxity and perhaps bony glenoid
deficiency or malposition. -
In many cases, the initial trauma
associated with posterior instability occurs with the arm held in
forward flexion, adduction, and internal rotation. -
In most studies, evaluating the presentation of posterior instability pain appears to be a prominent factor.
-
Although the pathologic cause of
subluxation can be capsular laxity and/or a labral tear, the majority
of patients present with either posterior or diffuse pain in their
shoulder. -
Commonly, the athletes suffering from
this problem are weight lifters, throwers, racquet sport athletes,
swimmers, and football players.-
Football players deserve special
attention because their specific position appears to play an important
role in the diagnosis. Most commonly, offensive lineman are affected. -
With the current blocking techniques
allowing for the players to “punch out” with their arms in a forward
flexed position, the capsule sustains intense posterior stress.
-
-
The additional cumulative trauma associated with weight lifting may contribute to the problem.
-
The usual presentation of MDI is that of vague shoulder pain, often global in nature, and occasionally severe and debilitating.
-
This is in contradistinction to most
cases of anterior instability, in which the instability itself is
typically the reason for the patient’s initial office visit.
-
-
In patients with MDI, the most obvious diagnosis is often scapular dyskinesia.
-
Patients with atraumatic instability may
have a family history of similar findings and a history of other joint
problems, most notably recurrent patellofemoral instability.
-
Both shoulders are carefully examined so that the symptomatic and asymptomatic sides can be compared.
-
It is helpful to begin on the normal side to assess for general laxity and strength and to gain the patient’s confidence.
-
Regardless of the type of instability, a thorough evaluation includes assessment of motion, laxity, and stability.
-
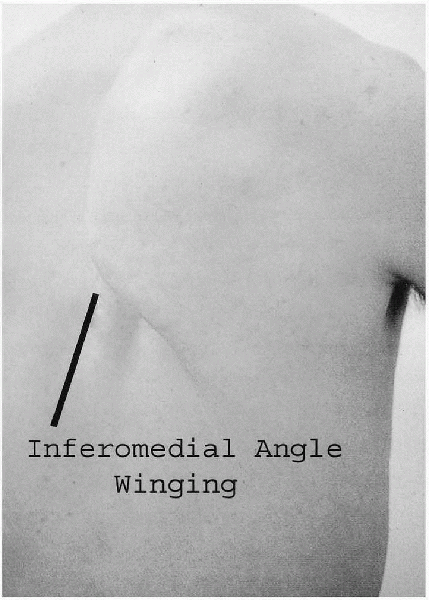
Often, the presenting complaint from patients with either symptom complex is scapular winging.
-
Scapular dyskinesis or loss of control of
scapular motion during arm elevation is seen by observing the patient
from behind and by asking him or her to slowly elevate and lower the
arms. -
The motion of the scapulae on the chest wall is then observed for asymmetry.
-
Several repetitions may be necessary before this is observed.
-
Winging can also be better demonstr ated by asking the patient to push against a wall to accentuate the problem.
-
-
In most cases of dyskinesia associated
with posterior or MDI, the static observation of the scapulothoracic
joint is normal, whereas the active evaluation reveals marked
scapulothoracic motion asymmetry (Fig. 18-3).
-
Posterior instability is best evaluated
with the jerk test, which involves placing the patient’s arm in 90
degrees of elevation and 90 degrees of internal rotation. -
The maneuver can be performed with the patient in the seated or supine position.
-
The supine position is simpler and
preferred because it puts the patient at ease and gives the examiner
some mechanical advantage.
-
-
In either position, the arm is then moved
from the coronal to the sagittal plane and back, whereas an axial load
is applied to the humerus. -
If posterior instability is present, the humeral head subluxes over the glenoid rim and reproduces the patient’s symptoms.
-
Reduction of the humeral head when the arm returns to the coronal plane is often accompanied by a palpable and audible clunk.
-
The competence of the glenoid concavity
and the integrity of the soft-tissue structures about the shoulder
should also be assessed with the load and shift test. -
The supine patient’s arm is positioned in 20 degrees of abduction and 20 degrees of forward flexion with neutral rotation.
-
The humeral head is loaded axially into the glenoid fossa and translated both posteriorly and anteriorly.
-
An assessment with respect to the degree of translation is made.
-
The extent of translation is described relative to the ability to translate the humeral head out of the glenoid fossa (Table 18-1).
-
In addition to the aforementioned signs
of excessive translation, using signs of labral pathology (such as the
crank, O’Brien’s, and Kibler maneuvers) can help assess the integrity
of the labral structures. -
These tests are delineated in other sections of this chapter, or in review articles on the topic.
 |
|
Figure 18-3 Scapulothoracic dyskinesia with winging in an active thrower with MDI.
|
-
The assessment of MDI includes the
examination maneuvers described earlier, as well as all of the
maneuvers that apply to anterior instability. These are described in
greater detail in other parts of this textbook. -
Specific maneuvers that delineate MDI
further include the assessment of a sulcus sign, an indicator of
inferior shoulder translation, as well as determination of generalized
signs of ligamentous laxity—including elbow and knee hyperextension,
the ability to place the thumb to the forearm, and metacarpophalangeal
joint hyperextension. -
The sulcus test is performed with the patient in the seated position.
-
A distraction force is applied to the arm
at the side of the body with the shoulder in neutral rotation. The
degree of separation between the acromion and humeral head is then
determined. -
Grading is shown in Table 18-2 and Figure 18-4.
-
-
Inferior laxity should always be assessed
in both shoulders because a large number of asymptomatic shoulders will
have a positive sulcus sign. -
Additionally, the degree of inferior
instability should be assessed with the arm in an externally rotated
position while maintaining neutral abduction. -
An obliteration of the sulcus sign in this position indicates competence of the rotator interval or the SGHL complex.
-
The importance of this factor cannot be
underestimated because simple rotator interval closure is often enough
to stabilize a shoulder with MDI.
-
|
TABLE 18-1 GRADING OF TRANSLATION OF THE HUMERAL HEAD OUT OF THE GLENOID FOSSA IN POSTERIOR INSTABILITY
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||
-
Although the diagnosis of instability can
be made without any further imaging studies, a number of imaging
modalities may be helpful in delineating the anatomical factors
involved, as well as associated pathological entities, especially in
older individuals whose incidence of rotator cuff pathology is
increased with instability. -
The use of routine radiographic imaging, especially in patients who will require surgical intervention, should be used.
-
In some cases, simple soft-tissue reconstructions may not suffice to stabilize a joint.
-
Surgical discussion with the patient
should include the possibility of bony reconstruction, as described
later in this chapter and in otherareas of this text.
-
-
The standard radiographs that should be
obtained include an anteroposterior view (made perpendicular to the
scapular plane), an axillary view, and a lateral or Y view. -
It is important to detect lesions such as
glenoid deficiencies, glenoid retroversion, erosion of the posterior
glenoid, and extra-articular ossifications of the posterior glenoid
margin (Bennet lesions). -
In cases in which a significant bony
deficit is either seen or suspected, more specialized views can be
obtained, such as the Stryker notch view or the Bernageau view. -
In continued questions of bony deficiency, the use of computed tomography scanning is certainly useful and indicated.
-
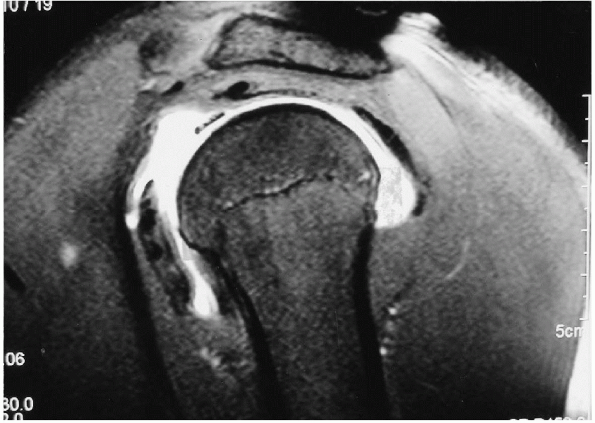
The use of routine magnetic resonance imaging (MRI) studies is not advocated in most situations.
-
The clinical indications for MRI include suspected rotatorcuff pathology.
-
In cases of MDI, the arthrogram portion of an MRI may shed light on the capsular volume.
-
The posterior-inferior glenoid labrum is
difficult to visualize in many MRI studies and as such is not useful in
determining the treatment algorithm in many cases. -
In repetitive overhead athletes, an MRI
study with gadolinium enhancement should be considered because superior
labrum anterior-posterior (SLAP) lesions frequently occur and may
impact the surgical approach. -
In addition, the evaluation of capsular volume and labral injury is made more definitive with the use of MRI (Fig. 18-5).
|
TABLE 18-2 GRADING OF THE SULCUS SIGN IN MULTIDIRECTIONAL INSTABILITY
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 18-4 Sulcus sign in a patient with failed anterior instability repair.
|
 |
|
Figure 18-5 MRI with gadolinium arthrogram depicting a posterior labral tear in a patient with significant posterior capsular redundancy.
|
-
The initial treatment of any instability
remains nonsurgical, with the emphasis on supervised strengthening of
the rotator cuff muscles and special attention to the infraspinatus and
teres minor, deltoid strengthening, and scapulothoracic stabilization
in posterior instability. -
This treatment regimen has proven
particularly successful in atraumatic instability and has allowed 80%
of patients to function effectively as opposed to 16% of those with the
traumatic variants of instability. -
It is paramount to separate those patients with voluntary instability from this group of patients.
-
It is important to differentiate between
patients who are able to sublux their shoulders by positioning and
muscular activation and those who do so for secondary gain.-
Patients who actively attempt to either
sublux or dislocate their shoulders, most commonly in a posterior
direction, are clearly poor candidates for surgical reconstruction of
any kind. -
One way to separate these individuals is
to assess their instability (or its reproducibility by the patient)
with the arm both at the side and at 90 degrees of flexion. -
In those whose humeral head subluxes
posteriorly with flexion and cross body adduction, a better response is
seen with surgical intervention. -
With that said, there is substantial
evidence to support surgical intervention in patients who can
voluntarily sublux their shoulders, fail conservative management, and
cannot participate in activities at their desired level.
-
-
In summary, patients who have posterior
instability of the shoulder should not be condemned to nonoperative
management solely because they are able to subluxate the shoulder
voluntarily. -
The judicious use of psychiatric evaluations for determination of confounding variables is suggested.
-
This is probably the most complex patient population seen in instability problems.
-
The basic idea is to maintain mobility while limiting excessive translation.
-
Surgical stabilization is considered for
recurrent posterior traumatic instability and for persistent atraumatic
posterior instability. -
The indications for stabilization of a
shoulder with MDI are continuing instability that persists despite
concerted rehabilitation and activity modification.-
The caveat here is that this is feasible for the patient.
-
-
The determination of which surgical procedure to opt for can be a challenge.
-
A particular technique is chosen on the
basis of the quality of the soft tissues and the bony anatomy and, most
importantly, by the experience of the surgeon. -
Unfortunately, these procedures are performed on an infrequent basis by most surgeons.
-
This can lead to insecurity by the
surgeon, and occasionally to poor decision making as a result of
inexperience with the nuances of posterior and MDI.
-
-
The most important decision regarding the
surgical intervention of a shoulder with any form of instability is the
examination of the shoulder under anesthesia. The importance of this
single maneuver cannot be overstated. -
The final decision with respect to the
order of repair, the direction of repair, and the type of repair should
be predicated on simple anatomical principles. -
Translation under anesthesia can be significantly different than that while the patient is conscious.
-
In a study of 50 patients, using the load
and shift test before and after the induction of anesthesia, 92% were
found to have anterior translation at least one grade higher during
anesthesia than while awake.
-
-
The typical findings associated with a specific injury to any given anatomical structure within the shoulder are well defined.
-
A simple and thorough examination
covering all of the known stabilizing elements should delineate the
consequent steps to be taken in a surgical procedure. -
Table 18-3 demonstrates the common areas involved in instability and the subsequent findings noted on physical examination.
-
This table can be used to determine the
necessity of repair of each specific anatomical structure at the time
of surgical intervention.
-
-
Finally, the contralateral shoulder should also be examined to assess for signs of generalized laxity.
-
There is no consensus with regard to the
procedure of choice for the patient with posterior instability who
fails a conservative course of treatment. -
Open surgical stabilization techniques
for the treatment of recurrent posterior instability include
soft-tissue and bony procedures. -
A variety of arthroscopic techniques have also been described.
-
The bony procedures include posterior
bone block, posterior glenoid osteotomy, and humeral rotational
osteotomy; bony pathology, however, is rare.-
In most situations, the use of soft-tissue procedures is sufficient.
-
The indications for posterior bone block
procedures are reserved for those situations in which a softtissue
procedure has failed. -
In the case of glenoid osteotomy, the
indications for the procedure are excessive posterior glenoid version
greater than 10 degrees.-
In one study, the average glenoid version
angle was altered from 9.35 to 4.62 degrees. However, 25 % of the
patients showed postoperative degenerative changes in the glenohumeral
joint at 5 years.
-
-
The use of humeral osteotomy for the treatment of recurrent instability does not have strong support in the literature.
-
In general, the outcome of bony
procedures has been inconsistent and difficult to justify in shoulders
without definite bony deformity.
-
-
Soft-tissue procedures that have been
well described include those that address the capsule either from a
posterior approach or from an anterior approach.-
Labral pathology is also addressed, if present.
-
The success rates for these repairs have been as high as 96% in primary repairs.
-
The amount of pathologic laxity present
in any given patient has been difficult to quantify. In most studies,
however, the posterior inferior margin of the capsule appears to be the
critical area that needs to be addressed with the repair.
-
-
The CHL and SGHL complexes play a significant role in posterior instability.
-
Several authors have adopted an anterior surgical approach to correct posterior instability. Nobuhara and Ikeda (1987)
reported 96% good and excellent results with rotator interval
reconstructions in 78 patients with posteroinferior instability.
Recurrent instability occurred in only 4%.
-
-
Other soft-tissue procedures seek to
excessively tighten internal rotation by buttressing the capsular
imbrication with muscle tissue.P.238-
A posterior capsular plication and
overlapping of the infraspinatus tendon (reverse Putti-Platt repair)
has been reported but has shown a large percentage of unsatisfactory
results.
-
-
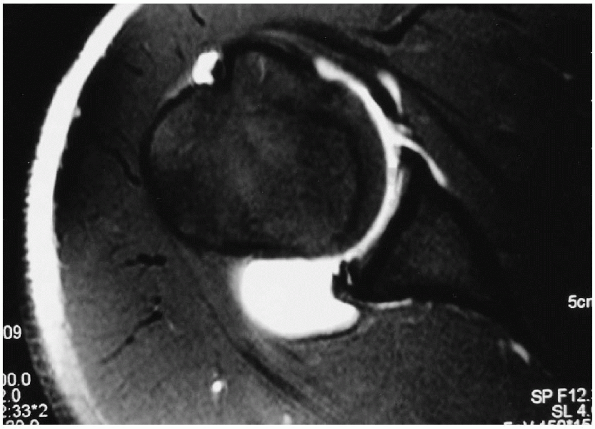
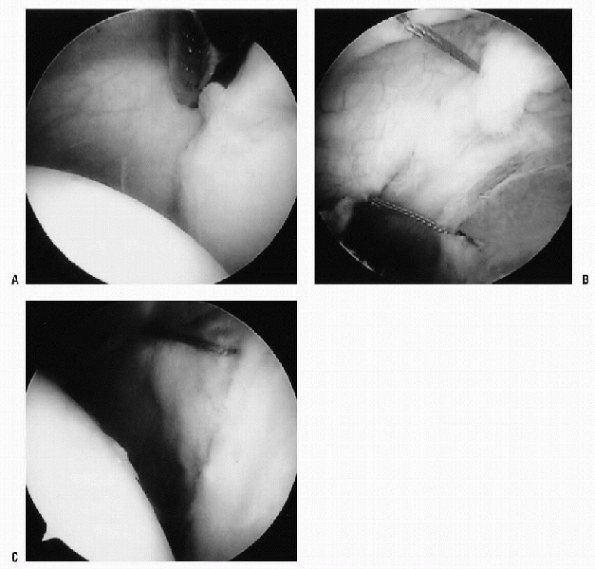
Arthroscopic techniques for the treatment of posterior instability are well described in the literature (Fig. 18-6).
-
Many studies, however, are limited in usefulness as a result of the limited sample sizes.
-
In one study, the capsule was prepared by
gentle abrasion of the synovial surface of the posterior capsule then
advanced by about 1 cm to the posterior glenoid labrum and sutured in
place using three to eight nonabsorbable sutures (Fig. 18-5).
At a minimum 2-year follow-up, 12 of 14 patients treated with
arthroscopic posterior capsular plication had 12 excellent results, and
2 had fair results. -
Another study delineated the pathologic
findings in 41 patients with posterior instability and noted that there
were four types of labral lesions: a labral split or flap tear (32%),
synovial and capsular stripping (22%), chondral or labral erosion
(17%), and Bankart-type detachment (12%).
-
-
A study assessing the outcomes of
traumatic posterior instability shed light on the fact that posterior
disruptions occur more frequently than previously thought and can be
managed arthroscopically in a straightforward fashion.-
It was concluded that arthroscopic repair of the posterior capsulolabral complex was an effective means of management.
-
-
In a study that used a variety of
techniques designed to address the multiple factors responsible for
instability, it was shown that a 90% success rate with 1- to 7-year
follow-up in the maintenance of stability can be achieved.-
Sixty-one patients were treated with six failures, two of which responded to rehabilitation and did not require further surgery.
-
The treatment algorithm included the use
of absorbable tacks for posterior labral repairs in conjunction with
arthroscopic rotator interval plication. In cases with more extensive
capsular laxity, a suture punch capsulorrhaphy with an extensive
vertical shift was also used. A mini-open capsulorrhaphy was used in
P.239cases
of diffuse posterior capsular damage, whereas thermal capsulorrhaphy
was used in simple diffuse stretching of the entire capsular complex.
-
-
Laser and radio frequency-induced
capsular shrinkage (thermal capsulorrhaphy) has also been used in an
attempt to imbricate the capsule.-
The lack of basic science to validate the
use of these devices, along with the lack of long-term clinical
outcomes, makes it difficult to recommend these treatment modalities. -
The basic science studies available
indicate that with the use of an yttrium-aluminum-garnet laser the
amount of glenohumeral joint translation may be decreased. A decrease
in posterior translation from 7.2 to 4.4 mm was noted with a 15-N load,
whereas a 20-N load allowed translation of 10.4 mm before and 6.5 mm
after ablation. In addition, the response to heat-induced shrinkage is
proportional to the collagen density of the area. -
Areas with high collagen density, such as
the middle and inferior glenohumeral ligaments, will respond more
dramatically than the posterior capsule and rotator interval. -
There is a paucity of peer-reviewed
literature to justify the use of heat capsulorraphy. A limited number
of non-peer-reviewed articles show promising results thus far, but none
deal exclusively with posterior instability.
-
|
TABLE 18-3 ANATOMICAL STRUCTURES RESPONSIBLE FOR SPECIFIC AREAS OF STABILITY
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||
|
TABLE 18-4 SUGGESTED TREATMENT FOR POSTERIOR INSTABILITY
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||
 |
|
Figure 18-6 Arthroscopic posterior capsular imbrication (all views from the anterior portal in a right shoulder). A: Posterior capsular redundancy with no evident labral pathology. B: Nonabsorbable sutures in place before closure. C: Capsular volume reduced after suture tying.
|
-
The basic principle of MDI surgery is to
reduce the volume of the capsule and therefore provide some restraint
to the humeral head, reducing the load on the shoulder musculature. -
This can be accomplished with a variety
of procedures, including the traditional open inferior capsular shift
through arthroscopic means or by thermal shrinkage. -
Neer and Foster introduced the concept of MDI and its treatment in 1980.
-
The inferior capsular shift was described
as a procedure for the symptomatic patient who had been unresponsive to
nonoperative therapy. -
In their study, 36 patients (40
shoulders) with involuntary inferior and multidirectional subluxation
and dislocation and who had failed standard operations underwent an
open inferior capsular shift, in which a flap of the capsule was
shifted to reduce capsular and ligamentous redundancy on all three
sides. -
Their results revealed that one shoulder
began subluxing again within 7 months after operation, but no other
unsatisfactory results were noted for at least 2 years.
-
-
A subsequent study by Cooper and Brems (1992) using the identical surgical procedure corroborated Neer and Foster’s findings.
-
The postoperative range of motion in this
population was well maintained with a mean forward elevation of 172
degrees; external rotation was 77 degrees, and internal rotation was to
the level of the eighth thoracic vertebra. Ninety-one percent of the
patients continued to function well without evidence of recurrence,
whereas four had disabling, recurrent instability. -
In a study analyzing the results in a
contact athlete population after surgical intervention, the overall
recurrence rate for a traditional open inferior capsular shift was 8%,
with successful return to sports occurring in 82% of the patients.
-
-
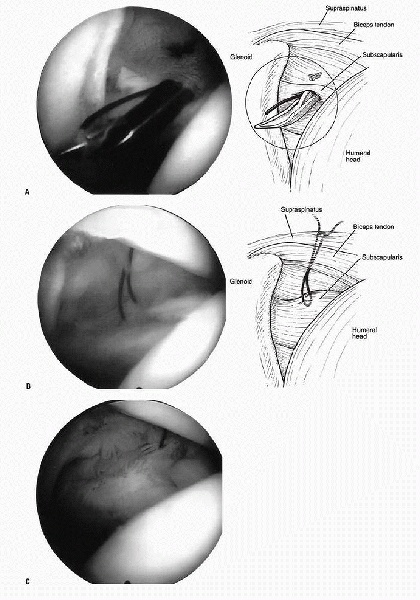
In addition to the traditional shift
procedure, further refinements in the technique have been made as a
result of increasing understanding of the rotator interval capsule (Fig. 18-7).-
A study of 10 shoulders using closure of
the interval—as well as imbrication of the anterior, inferior, and
posteroinferior aspects of the capsule through an anterior
approach—produced good or excellent results in 90% of patients.
-
-
In the more recent literature, arthroscopic-only techniques have attempted to imbricate the capsule in a variety of ways.
-
In a study by Treacy et al. (1999),
25 patients were treated with an arthroscopic transglenoid capsular
shift. At an average 5-year follow-up, 88% had satisfactory results,
with no patient experiencing loss of external rotation and 7 of 11
returning to sports at their preinjury level. -
In the 2001 prospective study by Gartsman et al.,
of 47 patients, 94% rated their results as good to excellent according
to the Rowe scale at 35-month average follow-up. One patient was
considered a failure of the index operation as a result of persistent
instability and underwent a second operative procedure, whereas two
others had persistent pain. In essence, 44 of 47 patients were treated
successfully.
-
-
In addition to the previously described
techniques, attempts to treat this problem with heat capsulorrhaphy
have been made, but heat therapies have thus far shown poor results,
compared not only with traditional open methods but also with the newer
arthroscopic procedures.
|
TABLE 18-5 SUGGESTED TREATMENT FOR MULTIDIRECTIONAL INSTABILITYa
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||
 |
|
Figure 18-7 Rotator interval closure. A:
Wide rotator interval closed with the use of BirdBeak (Arthrex, Inc, Naples, FL) suture-passing devices. The first suture is being delivered into the joint. B: A suture has been passed from the inferior edge of the supraspinatus to the superior edge of the subscapularis. C: Final closure obtained after knot-tying in the subacromial space. |
-
The most critical aspect of surgical treatment for posterior and MDI appears to be the rehabilitation.
-
These patients often have long-standing instability that has not been addressed with adequate rehabilitation.
-
The scapulothoracic articulation is frequently dysfunctional and needs to be addressed.
-
It is important to develop a stable platform for the shoulder positioners (rotator cuff) to be effective.
-
Although the specific rehabilitation
program varies on the basis of the procedure performed, some general
recommendations can be made. -
Any surgery for posterior instability seeks to reduce excessive laxity in the posterior capsule.
-
These patients should avoid stress to this area in the early phases of recovery.
-
As with any other surgical procedure,
early passive range of motion is highly beneficial to enhance
circulation within the joint to promote healing. -
The overall goals of the surgical
procedure and rehabilitation are to control pain and inflammation and
to regain normal upper extremity strength, endurance, and normal motion
while maintaining the desired level of function. -
In most cases, the patient should be placed in a splint/sling that protects the individual from excessive internal rotation.
-
Many apply an abduction splint, but other
devices that allow 15 to 30 degrees of abduction and neutral internal
rotation are adequate in most situations. The UltraSling (DJ Ortho,
Vista, CA) device is one such apparatus.
-
-
Physical therapy should be initiated within the first week after surgery.
-
Supervised rehabilitation is to be
supplemented by a home fitness program in which the patient performs
the given exercises at home or at a gym facility. -
The first 1 to 3 weeks involve the
gradual return of motion, especially external rotation, which in many
cases is not addressed with a posterior reconstruction.-
Passive motion is instituted, with active-assisted motion in the scapular plane.
-
Motion should be limited in internal rotation to a maximum of 30 degrees, with external rotation on an as-tolerated basis.
-
Pendulum exercises are instituted.
-
Submaximal and pain-free isometrics in all planes can also be instituted.
-
-
Beginning at 3 weeks postoperatively, the
patient is advanced to unlimited internal rotation, while avoiding the
extremes of motion. -
Strengthening is instituted with neutral tubing and prone horizontal adduction exercises with a limit of 45 degrees.
-
Scapular stabilization is begun at this
time, as well as rhythmic stabilization in proprioceptive neuromuscular
facilitatory patterns. -
Immobilization is discontinued between 4
and 6 weeks, depending on the degree of capsular laxity and the extent
of the surgical procedure. -
At 6 weeks, posterior capsular stretching
is instituted and titrated, depending on the degree of original laxity
and the existing internal rotation contracture. -
Strengthening is increased with the use of an upper extremity ergometer.
-
Dynamic stabilization exercises are also
advanced such that, at the end of 12 weeks, the patient should have a
full, painless range of motion with normal arthrokinematics. -
Between 12 and 24 weeks, a light plyometric program is begun with a gradual return to sport-specific and functional drills.
-
An interval throwing program can also be instituted.
-
-
Return to activity requires both time and clinical evaluation.
-
To most safely and efficiently return to
normal or high-level functional activity, the patient requires adequate
strength, flexibility, and endurance. -
Functional evaluation, including strength
and range-of-motion testing, is one method of evaluating a patient’s
readiness to return to activity. -
Symptoms such as pain, swelling, or instability should be closely monitored both by the patient and physician.
-
In general, a return to contact sports is allowed at about 4 months and full unrestricted throwing at 6 months.
-
Historically, after surgery for MDI, 6
weeks of postoperative immobilization was recommended, followed by heat
and gentle assisted exercises.-
The goal was for range of motion to be 20 degrees less than the opposite shoulder.
-
Isometrics was advocated at 8 weeks and progressive resistive exercises beginning at 12 weeks.
-
Sports and lifting more than 20 lb were
restricted for 9 months, and certain swimming strokes (back and
butterfly), heavy overhead use of the arm, and contact sports were
advised against for 12 months after surgery. -
This protocol has fallen out of favor as
a result of the excessive tightness and severe muscle weakness that
followed the regime.
-
-
The current postoperative stabilization protocol for MDI involves about 6 weeks of immobilization.
-
The patient is able to perform elbow and hand range of motion only for at least 3 weeks and sometimes for the first 6 weeks.
-
After the initial immobilization, the
patient begins supine stretching exercises, followed by wand exercises
as tolerated. Flexion and internal rotation are increased beginning on
postoperative week 2. External rotation is mobilized to neutral, then
increased 10 degrees per week; abduction is allowed to 45 degrees, then
increased 10 degrees per week after 6 weeks. -
Isometrics are instituted as soon as possible to limit muscle atrophy.
-
Beginning at 6 weeks, strengthening is initiated, including the rotator cuff and scapulothoracic musculature.
-
Range of motion is returned to within normal limits with stretching and joint mobilization programs.
-
Eccentric exercise programs and
proprioceptive neuromuscular facilitation techniques are started at 12
weeks postoperatively. In addition, sports such as swimming can now be
resumed. An interval throwing program may also begin at this time, with
a gradual return to unrestricted activities at 4 to 6 months. -
The one muscle that deserves particular attention with respect to open procedures is the subscapularis.
-
In open surgery, that is typically the only muscle detached and subsequently repaired.
-
It is paramount to obtain a solid repair of that tendon.
-
Also important is the protection of that muscle in the physical therapy that follows.
-
-
To protect the repair, internal rotation strengthening should not be instituted until 6 weeks postoperatively.
-
The many reasons for failure in the
rehabilitation and reconstruction of patients with posterior or MDI can
be divided into incorrect diagnosis (direction), surgical error, and
rehabilitation error. -
The episode leading to recurrence is likely to offer some idea as to the etiology.
-
An atraumatic event leading to recurrence
in a patient may indicate failure to address some component of the
instability, whereas a more significant trauma may indicate simple
recurrence from a macrotraumatic event.
-
-
The patient should be questioned with regard to their postoperative satisfaction with the procedure.
-
If the patient indicates that functional
return had not occurred before a subluxation event, then he/she is
likely to have undergone inadequate rehabilitation or in more extreme
cases experienced a surgical failure.
-
-
The most common errors are incorrect
diagnosis and failure to address the primary (and often, secondary)
component of instability in cases of MDI.-
A reason for this is the vagueness of symptoms in most patients.
-
Commonly, the patient presents with only vague pain and inability to perform activities.
-
The variety of positions that cause the
instability vary from adduction to internal rotation and possibly
extension, further adding to the confusion.
-
-
The all-important examination under anesthesia may have been neglected or not performed at all.
-
This step should be the final determining factor with respect to the surgical intervention undertaken, as previously stated.
-
-
The patients themselves often dictate the appropriate course of action.
-
Frequently, in many cases of simple posterior or MDI, the best course of action is nonoperative.
-
The concept of “conservative” therapy is easy to misuse.
-
In cases in which patients either can
modify their activities to reduce their instability or present with
congenital soft-tissue laxity, no surgery is the best therapy. -
Failure of repair in these patients can
lead to a cascade of events culminating in multiple failed procedures,
with a nonfunctional extremity and no obvious good salvage option.
-
-
Beyond misdiagnosis of the type of instability, failures are attributable to a lack of understanding of surgical principles.
-
In some situations, a labral detachment is properly addressed, but the remaining capsular redundancy is not.
-
In most cases, surgeons are more
comfortable with anterior approaches to the shoulder. Although in many
cases traditional open procedures work well, they are clearly
inadequate in others. -
Judicious use of the arthroscope and a
thorough examination under anesthesia go a long way toward preventing
those unfortunate decisions. -
In cases in which bony procedures are performed, the likelihood of complications increases.
-
Procedures redirecting the glenoid are
fraught with technical difficulty and carry with them the complications
of poor position of the osteotomy; nonunion, avascular necrosis; and
prominent hardware. -
All of these are devastating complications that may lead to salvage operations, including glenohumeral arthrodesis.
-
Overtightening of the joint and consequent degenerative changes are also fairly common problems.
-
The typical patient will spend 2 hours in the operating room but many days in the therapist’s office.
-
This fact is simply forgotten by many, not the least of which is the surgeon.
-
To that end, the most common
rehabilitation error is that of failure to complete the process (and in
some cases, not to institute it at all). -
A thorough rehabilitation focus,
beginning with scapulothoracic stabilization and strengthening with a
progression to proprioceptive neuromuscular facilitation, is integral
to returning patients to their preoperative activity level.
challenging clinical problem with more questions than answers.
Nonoperative treatment with concerted physical therapy remains the
cornerstone of treatment in most patients, with excellent results
obtained in most patients in the available literature.
important principles to apply with respect to operative intervention
are to adequately assess the patient for all possible directions of
instability and then to address these areas during the procedure. The
use of arthroscopy in these situations allows for a thorough diagnosis
and should be used in most cases.
case to case. Either traditional open means or newer arthroscopic
techniques appear to produce good to excellent results in the majority
of patients, when done properly.
surgical approach. In nearly all cases, the most important aspect is
the postoperative rehabilitation that takes into account not only the
glenohumeral joint but also the periscapular area.
RN, Soslowsky LJ, Malicky DM, et al. Posterior glenohumeral
subluxation: active and passive stabilization in a biomechanical model.
J Bone Joint Surg Am 1997;79:433-440.
SS, De Beer JF. Traumatic glenohumeral bone defects and their
relationship to failure of arthroscopic Bankart repairs: significance
of the inverted-pear glenoid and the humeral engaging Hill-Sachs
lesion. Arthroscopy 2000;16:677-694.
WZJ, Rockwood CAJ. Treatment of instability of the shoulder with an
exercise program. J Bone Joint Surg Am 1992;74: 890-896.
CH, Ogilvie-Harris DJ. Inferior capsular shift operation for
multidirectional instability of the shoulder in players of contact
sports. Br J Sports Med 2002;36:290-294.
RA, Brems JJ. The inferior capsular shift procedure for
multidirectional instability of the shoulder. J Bone Joint Surg Am
1992; 74:1516-1522.
LA, Warren RF. Glenohumeral joint stability: selective cutting studies
on the static capsular restraints. Clin Orthop 1996;330: 54-65.
VC, McMahon PJ, Lee TQ. Variation in the glenoid origin of the
anteroinferior glenohumeral capsulolabrum. Clin Orthop 2002; 400:26-31.
GM, Roddey TS, Hammerman SM. Arthroscopic treatment of multidirectional
glenohumeral instability: 2- to 5-year follow-up. Arthroscopy
2001;17:236-243.
DT, Sidles JA, Harris SL, et al. The role of the rotator interval
capsule in passive motion and stability of the shoulder. J Bone Joint
Surg Am 1992;74:53-66.
A, McBirnie J. Thermal capsular shrinkage for treatment of
multidirectional instability of the shoulder. J Bone Joint Surg Am
2003;85:2283-2287.
CS II, Foster CR. Inferior capsular shift for involuntary inferior and
multidirectional instability of the shoulder: a preliminary report. J
Bone Joint Surg Am 1980;62:897-908.
MW, Harner CJ, Fu FH. The role of the long head of the biceps muscle
and superior glenoid labrum in anterior instability of the shoulder. Am
J Sports Med 1994;22:121-126.
CR, Pierce DS, Clark JG. Voluntary dislocation of the shoulder: a
preliminary report on a clinical, electromyographic and psychiatric
study of twenty-six patients. J Bone Joint Surg Am 1973;55: 445-460.
SH, Savoie FH III, Field LD. Arthroscopic treatment of multidirectional
instability. J Shoulder Elbow Surg 1999;8:345-350.
HK, Piscopo M. Anterior capsular redundancy of the shoulder: congenital
or traumatic? An embryological study. J Bone Joint Surg Am
1985;67:363-366.
JJP, Micheli LJ, Arslenian LE, et al. Scapulothoracic motion in normal
shoulders and shoulders with glenohumeral instability and impingement
syndrome. A study using Moire topographic analysis. Clin Orthop
1992;285:191-199.
MA, Groh GI, Rockwood CA. Capsulorrhaphy through an anterior approach
for the treatment of atraumatic posterior glenohumeral instability with
multidirectional laxity of the shoulder. J Bone Joint Surg Am
1998;80:1570-1578.
SJ, Callaway GH, Cohen S, et al. Revision shoulder stabilization: 2- to
10-year results. J Shoulder Elbow Surg 1999;8:58-65.
