Physical Examination of the Spine
evaluation of spinal disorders. Despite great advances in imaging, such
as computed tomography and magnetic resonance imaging, these modalities
provide instantaneous images of continuously dynamic tissues. Clinical
correlation of imaging findings with the physical examination provides
the basis for treatment decision making. The development of a
systematic physical examination is a fundamental skill for the spine
surgeon. A routine approach improves the identification of subtle
clinical findings and helps improve diagnostic accuracy.
diagnosis that may have origins from spinal cord, root, or
musculoskeletal pathology. Conversely, it can implicate disorders that
mimic spinal pathology, such as lower extremity arterial insufficiency,
which can feign neurogenic claudication. Only after a complete exam are
diagnostic tests ordered to confirm a specific diagnosis. Ordering an
array of diagnostic tests without a complete physical exam often adds
costs unnecessarily and leads to confusion concerning the significance
of incidental positive findings.
Patients may present to the emergency or trauma department with an
acute spinal injury. This can range from spinal cord injury from a
cervical fracture-dislocation after a diving injury to sudden-onset
back and leg pain from lifting a heavy box. Initial examination is
crucial to guide additional diagnostic evaluation and possible surgical
intervention, with goals of preventing additional injury and restoring
function.
of chronic and subacute problems. A thorough examination in the clinic
is no less important than in the emergency setting. A greater emphasis
is placed, however, on performing specific provocative tests in
consideration of the patient’s signs and symptoms.
systematic spine examination. The patient’s presentation in each of the
two aforementioned settings results in emphasis on different aspects of
physical examination. The fundamentals of examination remain the same,
however.
the coordinated efforts of the spine surgeon, general trauma surgeon,
and ancillary staff. Information regarding the accident scene can help
estimate the mechanism of injury, severity, and approximate amount of
energy that was imparted. This information can lead to a higher index
of suspicion for some patients who present with minimal complaints in
relation to the energy of the trauma. For example, significant
front-end automobile damage may heighten the awareness of possible
blunt intraabdominal injury, major vessel injury, or distracting
ligamentous spinal injury from a sudden deceleration mechanism.
helps to remember the components: Airway, Breathing, and Circulation
are mandatory in the initial evaluation of the patient. Proper
oxygenation and perfusion of tissues helps to reduce further injury at
the cellular level. This includes the possible prevention of further
hypoxic injury after spinal cord injury. As the patient is
hemodynamically stabilized, specific life-threatening injuries are
addressed. After this, any Deficits are noted after proper Exposure of
the patient; this can show posterior injuries or injuries concealed by
clothing.
patient, it is imperative to perform a thorough and efficient
examination of the spine. Full spine precautions are followed until
injury is ruled out. The full exam must be completed despite detection
of one spinal injury. The incidence of noncontiguous spinal injuries
has been found in 15% of cases.
bony or ligamentous spinal injury. The determination of the type of
spinal cord injury is important. An incomplete injury may have a good
prognosis for some functional motor recovery, whereas complete injuries
have a much poorer prognosis. An incomplete spinal cord injury
is defined as the presence of some motor or sensory function more than
three segments below the level of injury (American Spinal Injury
Association definition). A complete spinal cord injury is defined as the absence of motor or sensory function more than three segments below the level of injury.
-
Inspect the patient. Inspection requires
adequate exposure of the entire patient and is mandatory to avoid
missing injuries obscured by clothing or positioning. -
Assess the overall appearance and status
of the patient. Unusual posturing, such as decerebrate or decorticate
posturing, may signify a traumatic brain injury, which may limit
detailed neurologic examination. -
Determine the need for mechanical
ventilation. Patients with spinal cord injuries above the C4-5 level
typically are unable to breathe independently because of denervation of
the diaphragm and may require mechanical ventilation. -
Examine the head and skull to look for
contusions, lacerations, or ecchymosis that can suggest a pattern or
directional mechanism of cervical spine injury. -
Assess the chest wall and pelvis.
-
Note any spontaneous movement of the
extremities because in the intubated or obtunded patient this may
represent the extent of the motor exam. The lack of spontaneous
movement in uninjured extremities may signify a neurologic deficit. -
Look for subtle findings, such as shoulder or lap belt markings, which can raise the suspicion of thoracolumbar spinal injury.
Four people are required for the standard logroll maneuver used to
examine the spine. One person stays at the head of the bed and
coordinates the movements. Three people are positioned on the side of
the patient to stabilize and turn the chest, pelvis, and limbs as a
unit. As the head and neck are manually stabilized, the posterior
portion of the cervical collar can be removed. Palpation begins at the
base of the skull and proceeds caudally. No attempts at manipulation or
range of motion testing of the cervical spine should be performed at
this time.
|
TABLE 1-1 GUIDELINES FOR SPINE PRECAUTIONS
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
represents the posterior base of the skull and marks the junction of
the head with the cervical spine. Crepitus or ecchymosis can signify a
basilar skull fracture. Palpation of the midline is performed next. The
spinous processes of the upper cervical spine are difficult to palpate,
but the overall sagittal and coronal alignment of the cervical spine
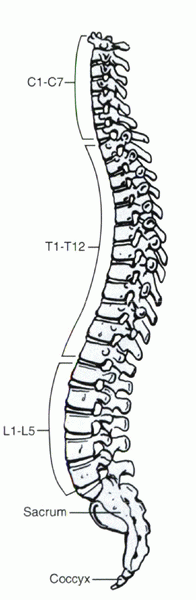
can be assessed (Fig. 1-1). Any abnormal
position of a spinous process, tenderness to direct palpation,
associated paraspinal muscle spasm, torticollis, or neck malposition
can signify an underlying injury. Common injuries encountered in the
upper cervical spine are difficult to assess solely by physical
examination. These injuries include dens fractures, atlantoaxial
instability, and C 1 ring fractures.
The spinous processes here are easier to palpate, and sagittal and
coronal alignment can be assessed more easily. Common injuries
encountered in this region include fractures, subluxations,
dislocations, and fracture-dislocations. The first large spinous
process, or vertebra prominens, encountered is usually that of C7 or T1. This is a landmark for the cervicothoracic junction.
 |
|
Figure 1-1
The axial alignment of the adult human spine as seen in the lateral view. Note the normal lordosis of the cervical and lumbar areas. |
palpated easily. The ribs and associated costovertebral joints provide
increased stability to the thoracic spine so that small amounts of
displacement or step-off suggest high-energy injuries with a high rate
of spinal cord injury. Systematic palpation along the thoracic spine is
performed to note any point tenderness, malalignment, or interspinous
widening. Rib fractures can be detected with tenderness to palpation.
thoracic spine. The spinous processes are easily palpable. Alignment is
noted along with tenderness or interspinous gaps. The tops of the iliac
crests are usually at the level of the L4-5 interspace, which can be a
useful surface landmark. Taking both hands on either side of the iliac
crests and placing the thumbs toward the midline directs the examiner
to the space between the L4 and L5 spinous processes.
is performed. This part of the exam is important because fractures of
the sacrum frequently are missed initially. Missed, untreated sacral
fractures can lead to persistent neurologic deficits, such as bowel,
bladder, and sexual dysfunction from distal sacral root injuries. After
palpation, the cervical collar is replaced, and the patient is gently
and uniformly logrolled back to the supine position.
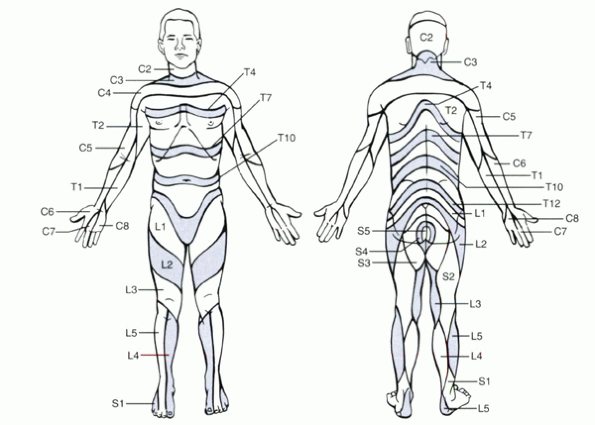
respective nerve roots. The sensory dermatomes can overlap one another
by one third of their width. Thoracic and lumbar nerve roots exit below
the corresponding numbered vertebral body. Cervical roots exit above
their corresponding numbered vertebrae, as there are eight cervical
roots for seven cervical vertebrae. The C8 root exits below the C7
vertebral body (Fig. 1-2).
-
Light touch
-
Pinprick
-
Vibration
-
Proprioception
-
Temperature
-
Pain response
usually are feasible. Simple testing of light touch can entail the use
of the examiner’s fingertips or a cotton-tipped applicator against the
skin. Testing is performed bilaterally to detect asymmetric
innervation. This can delineate the general areas of sensory deficiency.
demarcate specific dermatomes where sensory function may be diminished
or absent. To perform pinprick testing, a cotton-tipped applicator or
tongue depressor can be snapped in half and the pointed end used for
testing. Alternatively, a manufactured device can be used if readily
available. The affected areas or spinal cord level can be outlined with
a skin marker for subsequent serial evaluations.
 |
|
Figure 1-2
The relationship of the spinal nerve roots to the vertebral bodies. The eighth cervical root exits below the C7 vertebra because there are eight cervical roots but only seven cervical bodies. |
The C5 dermatome innervates the skin overlying lateral shoulder and
deltoid muscle. C6 usually innervates the radial aspect of the forearm
and the thumb. C7 usually innervates the middle finger distal to the
metacarpophalangeal joint. C8 usually innervates the ulnar aspect of
the forearm, including the ring and small fingers. T1 usually
innervates the medial arm.
Three regions can be used as landmarks, however, as follows:
 |
|
Figure 1-3
Anterior and posterior sensory dermatomes. (From Browner BD, Jupiter JB, Levine AM, Trafton PG. Skeletal trauma, 2nd ed. Philadelphia: WB Saunders, 1998.) |
-
T4 dermatome usually innervates the chest wall at the level of the nipples.
-
T7 usually innervates the chest wall at the level of the xiphoid process and the inferior border of the sternum.
-
T10 usually innervates the skin along the abdominal wall at the level of the umbilicus.
be supplied by distal cervical nerve roots, the so-called cervical
cape. Sensation in this region should not be misinterpreted as thoracic
level function because this can lead to inaccurate determination of the
level or type of spinal cord injury.
levels correlate with skin patches that are oriented obliquely along
the thighs and legs (see Fig. 1-3). The L2
dermatome corresponds to the anterior thigh. The L3 dermatome usually
involves the anterior knee. The L4 to S1 dermatomes are tested in the
foot. L4 innervates the medial foot; L5, the dorsal foot; and S1, the
lateral foot.
the perineal region. They form concentric rings around the anus with S5
in the center (Fig. 1-4). Although the reflex
examination is discussed in detail later, evaluation of rectal tone and
the bulbocavernosus reflex is performed best in conjunction with
perianal sensory testing. The “anal wink” is described as the
contraction of the anal sphincter when the skin around the anus is
stimulated. The anal wink is a normal
response, and its absence can indicate spinal cord injury. Rectal tone
is assessed and should be characterized as normal, decreased, or
absent. The presence of rectal tone and perianal sensation can indicate
sacral sparing and continued function of the sacral roots and their
connections through the cord to the cerebral cortex. Sacral sparing may
be the only indication of an incomplete cord injury during the initial
trauma evaluation. Four common incomplete cord injury patterns are the
central cord syndrome, anterior cord syndrome, posterior cord syndrome,
and Brown-Séquard syndrome. These are described in further detail in Table 1-2.
is tested. This is elicited most easily by a gentle tug on a Foley
catheter. During the digital rectal exam, this maneuver elicits a
normal reflexive contraction of the anal sphincter. If a catheter has
not been placed, the reflex can be elicited by a gentle squeeze of the
glans penis in men or the clitoris in women. The absence of the
bulbocavernosus reflex indicates spinal shock. Spinal shock
is a state of flaccid paralysis, hypotonia, and areflexia that can
occur immediately after a severe spinal cord injury. The reflex returns
in most people after 24 hours, signifying the end of spinal shock. If
there is no evidence of sacral sparing or spinal
cord
function distal to the level of injury after the period of spinal shock
is over, this is a complete cord injury and there is little chance for
further recovery of function. No determination of the completeness of
spinal cord injury can be made while the patient is in spinal shock.
 |
|
Figure 1-4
The concentric rings of the dermatomes around the perineal area. (From Browner BD, Jupiter JB, Levine AM, Trafton PG. Skeletal trauma, 2nd ed. Philadelphia: WB Saunders, 1998.) |
of motor strength testing. Extremity injuries and associated pain
should be noted in documenting strength testing. Motor strength is
graded by a 0-to-5 scale (Table 1-3). It is
important to clarify a standard grading scale to optimize interexaminer
and intraexaminer repeatability. Although some use a + or – to note
slightly more or slightly less strength, this practice may create
confusion. For example, subsequent examiners may not be able to
differentiate between strength graded as 5 – versus 4 +.
|
TABLE 1-2 COMMON SPINAL CORD INJURY SYNDROMES
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||
-
Grade 5: Signifies full strength with the ability to move the joint against full resistance.
-
Grade 4: Signifies the ability of the muscle to move the joint against some, but not full, resistance.
-
Grade 3: Signifies movement against gravity alone without any added resistance.
-
Grade 2:
Signifies the ability to move the extremity or joint through a full
range after gravity has been eliminated. Grade 2 biceps function means
that the elbow can be flexed fully when the arc of motion is in a
horizontal plane (e.g., the arm lying flat on the bed), but not when
the arc of motion is in a vertical plane (Fig. 1-5). -
Grade 1: Signifies visible contraction of the muscle without the ability to move joint.
-
Grade 0: Signifies no visible muscle contraction.
|
TABLE 1-3 MANUAL MOTOR TESTING GRADING SCALE
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
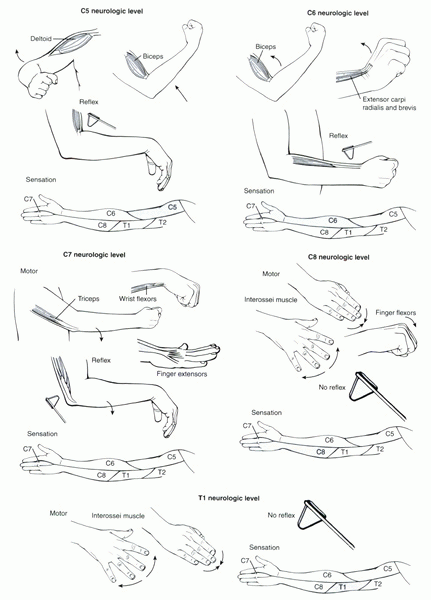
innervated by more than one root. Five major roots are evaluated in the
upper extremity for cervical evaluation, C5 to T1, as follows:
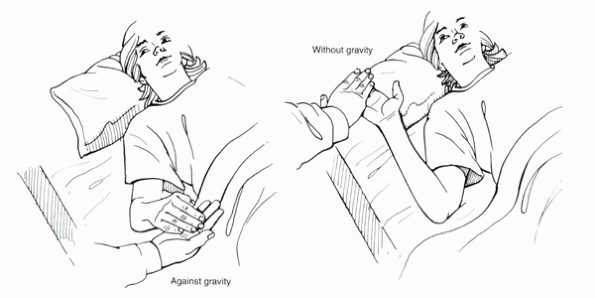 |
|
Figure 1-5
An example illustrating the difference between grade 2 versus grade 3 motor function of the biceps. If the elbow is able to be flexed without gravity, but unable to be flexed with gravity, the biceps is graded as having grade 2 strength. |
-
C5—evaluated by testing the deltoid with shoulder abduction
-
C6—evaluated by testing the biceps and wrist extensors
-
C7—evaluated by testing the triceps, wrist flexors, and finger extensors
-
C8—evaluated by testing the finger flexors
-
T1—evaluated by testing the intrinsic muscles of the hand through finger abduction and adduction
to myotomal root level testing of thoracic spinal cord function.
Although assessment of regional contraction in the thorax and abdomen
can be performed, sensory testing of the dermatomes is used more
accurately to determine the level of function.
-
L1 and L2—evaluated by testing hip flexion
-
L3—tested by knee extension, understanding that significant contributions to quadriceps innervation are made by L2 and L4
-
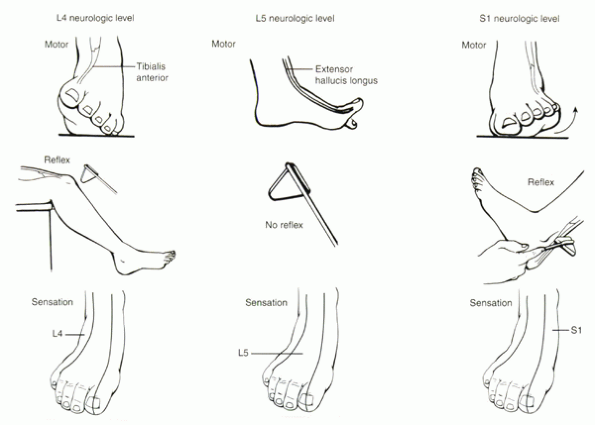
L4—evaluated better alone by testing ankle dorsiflexion through the tibialis anterior
-
L5—evaluated by testing great toe dorsiflexion through the extensor hallucis longus
-
S1—evaluated by testing ankle plantar flexion through gastrocnemius complex
be systematic and consistent to improve interexaminer and intraexaminer repeatability and reliability.
-
Grade 3: Hyperreflexia
-
Grade 2: “Normal” response
-
Grade 1: Hyporeflexia
-
Grade 0: Absence of a reflex response
-
C5 is tested by the biceps; C6, the
brachioradialis; and C7, the triceps reflex. The reflexes are elicited
at the musculotendinous junction near their insertion sites (Fig. 1-6). -
T7 to L1 levels can be tested by
eliciting a superficial abdominal reflex. A light stroke of the skin
along four quadrants centered on the umbilicus should result in
contraction of the muscles to pull the umbilicus to that quadrant.
T7-T10 is tested above the umbilicus, and T10-L1 is tested below the
umbilicus. The bulbocavernosus and superficial anal reflexes were
discussed earlier.
-
L4 is tested by the patellar tendon reflex.
-
S1 is tested by the Achilles tendon reflex.
-
There is no reflex that can assess the L5 nerve root.
is checked by quickly dorsiflexing the relaxed ankle joint. Greater
than four beats of clonus is considered abnormal, with normal
individuals usually exhibiting one to two beats. Babinski’s sign (or plantar reflex)
is checked by stroking the sole of the foot from the heel toward the
toes with the handle end of a reflex hammer. It is considered positive
with an up-going great toe. A normal response is flexion of the toes.
shock. This can last 24 to 48 hours. After spinal shock has ended,
hyperreflexia, spasticity, and sustained clonus may be appreciated.
-
Level of spinal cord injury
-
Complete versus incomplete spinal cord injury
-
Status of spinal shock and sacral sparing
focused on areas pertaining to patient’s complaints. A systematic exam
is crucial, however, to avoid missing pathology and to make an accurate
assessment. Principles of the examination are the same as that of the
trauma exam, with more emphasis placed on the areas of symptoms and the
use of provocative maneuvers. The goal of the exam is to determine if
the patient’s complaints arise from axial mechanical pathology,
radiculopathy, myelopathy, or other pathology.
paralysis with little atrophy, Babinski’s sign, clonus, and other
pathologic reflexes suggests myelopathy and spinal cord compression.
Other complaints related to an upper motor neuron lesion include the
insidious onset of clumsiness in the hands and lower limbs, with
increasing difficulty in maintaining balance.
dysfunction corresponding to a specific root level, usually in a
unilateral distribution. Other signs of these lower motor neuron
lesions include flaccid weakness of innervated muscles, marked muscle
atrophy, and diminished or absent reflexes (Table 1-4).
-
Observe the overall patient, including affect, posture, and gait.
-
Evaluate the patient’s gait as he or she
walks into the room or down the examination hallway. This aspect of the
examination is often underappreciated and overlooked, but it can
provide significant information. Although a comprehensive discussion of
gait analysis is beyond the scope of this chapter, specific gait
patterns should be noted that might be related to neural pathology:-
Wide-based gait can signify instability related to myelopathy.
-
Locked knee can signify quadriceps weakness from L2-4 pathology.
-
Footdrop or steppage can signify loss of ankle dorsiflexion from weakness of tibialis anterior or extensor hallucis from L4-5.
-
Flatfoot or loss of push-off can signify loss of calf plantar flexion from weakness of the gastrocnemius-soleus from S1-2.
-
Abductor lurch most often is associated
with hip pathology, but can be related to abductor weakness from L5
innervation of the gluteus medius.
-
-
Assess the patient’s posture, which can
highlight areas of localized pain, muscle spasm, or deformity. Areas of
splinting or awkward motion of the extremities can be appreciated. -
Evaluate the skin for any abnormalities and previous surgical scars.
-
Evaluate the extremities for any muscle
atrophy or cutaneous signs of diseases that may have spine-related
pathology, such as rheumatoid arthritis or neurofibromatosis. -
With the patient standing upright,
observe the coronal and sagittal alignment of the spine. Note
exaggerated kyphosis, lordosis, or scoliosis in the spine with its
orientation and location. Further curve analysis is done as the patient
bends forward, noting differences in rib hump or paraspinal muscle
prominence. Approximate rotation can be measured using a scoliometer at
this time. As the patient stands upright again, take care to note
subtle curves in the thoracic and the lumbar portions of the spine.
Normally the shoulders and pelvis should be level, and the head should
be well balanced over the midline of the body. Note any pelvic or
shoulder obliquity and trunk shift. The latter can be measured using a
plumb line dropped from the base of the skull to determine amount of
offset in centimeters from the center of the sacrum/coccyx. -
Perform an active range of motion test
for the cervical, thoracic, and lumbar spine. In the cervical spine,
the distance from the chin to the chest is a measure of flexion and can
be documented as the distance from the tip of the chin to the sternal
notch. Full neck extension normally allows the patient to look straight
up to the ceiling. Rotation and lateral bending are normally 70 and 40
degrees, respectively. The greatest amount of segmental flexion and
extension occurs between the occiput and C1. The greatest amount of
axial rotation (approximately 50%) occurs in the upper cervical spine,
facilitated by the nearly flat orientation of the C1-2 facets.
 |
|
Figure 1-6 Clinical testing of the C5-T1 nerve roots. (From Klein
JD, Garfin SR: History and physical examination. In Weinstein JN, Rydevik BL, Sonntag VKG, eds. Essentials of the spine. New York: Raven Press, 1995:71-95.) |
 |
|
Figure 1-7 Clinical testing of the L4-S1 nerve roots. (From Klein
JD, Garfin SR: History and physical examination. In Weinstein JN, Rydevik BL, Sonntag VKG, eds. Essentials of the spine. New York: Raven Press, 1995:71-95.) |
|
TABLE 1-4 COMPARISON OF CLINICAL FINDINGS IN MYELOPATHY VERSUS RADICULOPATHY
|
|||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||
the stability provided by the ribs. In the lumbar spine, motion testing
can be measured during the forward bending portion of inspection for
curve deformities. Flexion can be measured by the distance of the
fingertips to the toes. Extension is difficult to quantify accurately.
Rotation and lateral bending can be measured in degrees from the
orientation of the shoulders.
trauma exam remains the same for the clinical examination. The anatomic
landmarks can correlate areas of pain to specific vertebral levels. The
paraspinal areas are checked for tenderness, muscle spasm, and masses.
Lumbar strain is associated with paraspinal muscle spasm, tenderness to
palpation, and pain with motion over several lumbar levels without
radicular symptoms. Degenerative disc disease of a single level usually
can be limited, however, to central tenderness to palpation with less
paraspinal muscle spasm at a localized lumbar level, with or without
radicular symptoms. The sacroiliac (SI) joints and the coccyx are
evaluated for pain and tenderness.
Structures to evaluate include the sternocleidomastoid muscle, carotid
artery, and thyroid gland. If the patient reports mild difficulty
swallowing, this may be caused by cervical bony abnormalities,
osteophytes, or a mass that may be found by gentle palpation. The
supraclavicular fossa also is evaluated for masses or a cervical rib.
In the abdominal area, the umbilicus lies over the L3-4 levels near the
aortic bifurcation. Deep palpation near this area may detect an aortic
aneurysm, which can produce back pain.
extremities. Careful examination of pedal pulses is especially
necessary to assess for possible peripheral vascular disease in
patients with claudication symptoms.
for the trauma evaluation. Areas of pain or abnormal sensation are
noted for dermatomal, peripheral nerve, stocking-glove, or nonanatomic
distribution. Weakness of specific muscles or groups of muscles helps
distinguish root versus peripheral nerve dysfunction. Additional
attention should be paid to differentiating central nervous system from
peripheral nerve function. Careful physical examination with a high
index of suspicion can help differentiate between peripheral nerve
versus spinal cord and root pathology. Detailed understanding of the
brachial plexus and lumbosacral plexus is crucial.
Generally, hyperreflexia, including clonus and positive Babinski’s
sign, indicates myelopathy. Hyporeflexia or areflexia usually indicates
radiculopathy related to the specific root. Side-to-side differences
are noted.
the thighs. The examiner first can elicit the biceps reflex by
palpating the tendon at the elbow crease with the thumb, then lightly
tapping the reflex hammer against the thumb. Then the brachioradialis
reflex is tested. Finally, the examiner takes the patient’s relaxed arm
and supports it at the side so that the elbow is hanging free. The
triceps reflex is elicited at the tendinous portion of the triceps just
proximal to the olecranon.
subsequently) that indicate myelopathy in the cervical area should be
noted at this time. The scapulohumeral reflex suggests myelopathy of
the upper cervical spine above the C4 neurologic level. This reflex is
positive if the scapula elevates or the humerus abducts in response to
tapping on the spine of the scapula or tip of the acromion with the
patient seated. Myelopathy of the middle cervical levels is suggested
by Hoffman’s sign and inverted radial reflex. Hoffmann’s sign is
elicited by quickly flicking the middle finger into extension. A
positive sign is noted when the thumb and other fingers flex in
response to the maneuver. The inverted radial reflex also is noted when
the thumb and fingers flex during testing of the brachioradialis
reflex. Finally, myelopathy is suggested by two findings specific to
hand dysfunction known as “myelopathy hand.” The first is the
finger-escape sign, which is seen when the ulnar digits drift into
abduction and flexion when the patient is asked to extend the digits
fully with the palm facing down. The second is the inability to perform
a repeated grip and release maneuver rapidly with the fingers secondary
to weakness and spasticity of the hand.
the abdominal reflex. In the presence of myelopathy, this superficial
reflex often is diminished or absent. The superficial reflexes require
skin stimulation and are upper motor neuron reflexes. The two other
superficial reflexes that can be tested are the cremasteric reflex and
the anal reflex (anal wink).
the examination table so that the feet are free to move and not resting
on a step. The patellar tendon reflex is elicited easily with the
examiner standing to the patient’s side. The Achilles reflex is tested
with the ankle in gentle dorsiflexion to “preload” the
gastrocnemius-soleus. It is often difficult to obtain a good reflex
response because many patients cannot relax fully and often try to
“help” by keeping the ankle actively dorsiflexed. Pathologic reflexes
indicating myelopathy in the lower extremities include the presence of
clonus and Babinski’s sign, which have been described earlier. A
positive Oppenheim sign also is found in myelopathy when abnormal great
toe extension with splaying of the great toes is elicited when running
a finger firmly down the tibial crest.
exam lead to focused use of provocative maneuvers and special tests to
help discern pathology related to spinal versus nonspinal pathology. An
important consideration during provocative testing is to correlate the
findings with the patient’s reported symptoms. Pain can be produced
during testing, but it may not be clinically significant unless it is
concordant with the patient’s symptoms of radiculopathy.
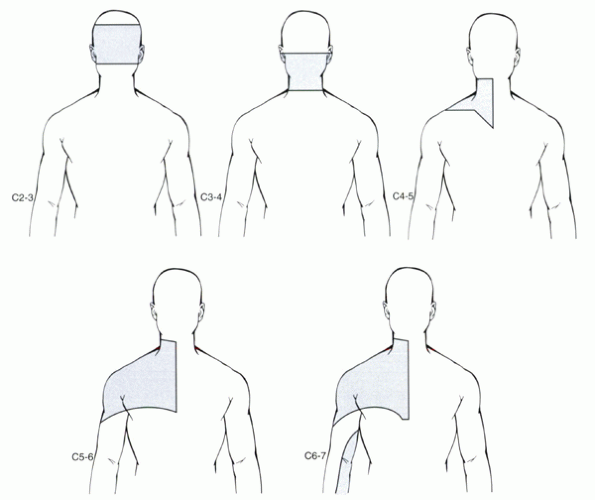
spine with the patient seated can reproduce and relieve symptoms
related to cervical root compression. Reported pain in the head and
neck areas should be noted because reliable patterns have been
correlated to specific cervical levels with discography (Fig. 1-8). Lhermitte’s sign
is a shocklike sensation in the trunk or extremities associated with
axial load combined with flexion or extension of the neck. The pain is
believed to occur from a reduction in foraminal or spinal canal space
during dynamic motion as a result of disc disease or herniation.
Performing a Valsalva maneuver also can be associated with a sharp or
shocklike pain in the neck or a dermatomal distribution from increased
intrathecal pressure irritating a nerve root. The Spurling maneuver
also can exacerbate symptoms of radiculopathy by the combination of
lateral flexion and rotation of the neck to the affected side. This can
help to differentiate radiculopathy from shoulder-related pain. Adson’s maneuver
can help distinguish pathology originating from compression of
neurovascular structures from thoracic outlet syndrome or a cervical
rib. This is suggested by noting a decreased radial pulse pressure at
the wrist when the patient takes a deep breath; holds the arm in an
abducted, extended, and externally rotated position; then rotates the
head toward the arm being examined. The decreased pulse from
compression of the subclavian artery can be associated with compression
of the adjacent brachial plexus and not the nerve roots. Because
shoulder problems often can mimic cervical radiculopathy (and vice
versa), careful assessment of the shoulder, including rotator cuff
testing, should be performed. Tests for peripheral nerve compression
syndromes, such as Tinel’s and Phalen’s signs, may be performed because
these syndromes can present with similar symptoms.
only way to test motor function of the thoracic roots. This is checked
during a partial situp with the patient supine on the exam table.
Normally the umbilicus should move proximally on the midline. Any
weakness of the rectus muscle, which is innervated broadly by T5-12,
would lead to deviation of the umbilicus away from the affected side. A
positive test can be related to thoracic radiculopathy.
(L2-4) is performed by flexing the knee and passively hyperextending
the hip while the patient is prone. The straight-leg test (SLR) for
sciatica (L4-S1) can be performed while the patient is supine and while
the patient is sitting. A positive test recreates symptoms of
radiculopathy in the distribution of the affected nerve root (i.e.,
distal to the knee). Pain can be aggravated further with dorsiflexion
of the ankle (Lasègue’s sign). Kernig’s sign
is similar to the SLR test but with the addition of neck flexion during
the maneuver to re-create sciatica. Reproduction of pain when a
contralateral SLR is performed enhances specificity because it puts
tension on the involved lumbar root from the opposite side. Tightness
of the hamstring muscle is common in patients with associated
mechanical low back pain. This can mimic sciatica during SLR testing
but has the important distinction that pain usually does not extend
distal to the knee.
to evaluate for range of motion and pain at these joints. Internal
derangements in the knee or hip can mimic symptoms of spine pathology,
such as radiculopathy. Pain originating from the SI joints also needs
to be assessed. Manual compression of the iliac wings can elicit SI
symptoms. The FABER (flexion, abduction,
external rotation) figure-four position of the leg is performed to
assess for pain originating from SI instability or pain. The final test
for SI pathology is Gaenslen’s sign, when
the patient lies supine with both legs flexed to the chest similar to a
fetal position with one buttock and leg over the edge of the table.
Complaints of pain in the SI area when the leg is dropped and extended
over the edge of the table suggest pathology in that area.
inconsistent with objective findings during the physical exam, a series
of special tests may need to be performed to identify patients who may
be exaggerating or magnifying pain symptoms. Hoover’s sign
is performed to detect if a patient is giving full effort for motor
testing. In this test, both of the patient’s ankles are cupped under
the examiner’s hands simultaneously. The patient is asked to perform an
SLR with maximum effort. Usually the examiner feels downward pressure
on the other hand as the opposite leg provides increased leverage for
this strength test. If not, the patient simply is not attempting to
move the leg. Also commonly seen is “giving way,” or sudden lack of
resistance during manual strength testing. Motor testing is graded
against sustained resistance. Sudden giving way of the muscle group
being tested is not a reliable indicator of objective weakness.
to identify patients who may respond poorly to treatment, including
surgery or nonsurgical measures. These patients may be seeking
secondary gain, malingering, or exhibiting nonorganic causes of pain.
 |
|
Figure 1-8 Patterns of pain provoked by discography from the C2-3 to the C6-7 disc levels. (From Grubb SA, Kelly CK. Cervical discography: clinical implications from 12 years of experience. Spine 2000;25:1382-1389.)
|
-
Pain in nonanatomic distributions
-
Pain out of proportion to stimulus
-
Exaggerated pain behavior
maneuver can be performed. These tests are insufficient to produce an
organic pain response from spinal origin:
performed by gently rolling the loose skin over the lower back while
the patient is standing or prone and asking if radicular symptoms are
produced. Radicular symptoms should not occur.
by gently rotating the patient’s torso at the hips as the patient is
standing with the hands on the hips. This simulates spine motion, but
all the rotation occurs through the knees and should not generate back
pain.
performed by applying approximately 5 lb of axial load to the top of
the head. This small amount of load is not sufficient to cause
mechanical pain or instability. This is not to be confused with the
Spurling maneuver.
of the seated SLR test. Symptoms that are present during a supine SLR
but not present during seated SLR indicate a positive test. Normally,
if nerve root compression is present, radicular symptoms should be
aggravated during the seated SLR with associated complaints of sciatic
pain or physically leaning back to avoid the pain response.
signs. The presence of more than three positive signs predicts poor
treatment outcome, however.
the trauma patient and the clinic patient have some subtle differences
and emphases but share most aspects of the exam. Each exam can be
performed efficiently and reliably. The combination of patient history,
physical examination, and radiographic evaluation leads to proper
diagnosis and appropriate treatment plan.
JD, Garfin SR. History and physical examination. In: Weinstein JN,
Rydevik BL, Sonntag VKG, eds. Essentials of spine. New York: Raven
Press, 1995:71-95.
T, Shimada H. Shirakura K. Scapulohumeral reflex (Shimizu): its
clinical significance and testing maneuver. Spine 1993;18: 2182-2190.
PC, de Krom MC, Knottnerus JA. Consistency of history taking and
physical examination in patients with suspected lumbar nerve root
involvement. Spine 2000;25:91-97.
