Pediatric Elbow
-
Elbow fractures represent 8% to 9% of all upper extremity fractures in children.
-
Of all elbow fractures, 86% occur at the distal humerus; 55% to 75% of these are supracondylar.
-
Most occur in patients 5 to 10 years of age, more commonly in boys.
-
There is a seasonal distribution for
elbow fractures in children, with the most occurring during the summer
and the fewest during the winter.
-
The elbow consists of three joints: the ulnohumeral, radiocapitellar, and proximal radioulnar.
-
The vascularity to the elbow is a broad anastomotic network that forms the intraosseous and extraosseous blood supplies.
-
The capitellum is supplied by a posterior branch of the brachial artery that enters the lateral crista.
-
The trochlea is supplied by a medial
branch that enters along the nonarticular medial crista and a lateral
branch that crosses the physis. -
There is no anastomotic connection between these two vessels.
-
-
The articulating surface of the
capitellum and trochlea projects distally and anteriorly at an angle of
approximately 30 to 45 degrees. The center of rotation of the articular
surface of each condyle lies on the same horizontal axis; thus,
malalignment of the relationships of the condyles to each other changes
their arcs of rotation, limiting flexion and extension. -
The carrying angle is influenced by the
obliquity of the distal humeral physis; this averages 6 degrees in
girls and 5 degrees in boys and is important in the assessment of
angular growth disturbances. -
In addition to anterior distal humeral
angulation, there is horizontal rotation of the humeral condyles in
relation to the diaphysis, with the lateral condyle rotated 5 degrees
medially. This medial rotation is often significantly increased with
displaced supracondylar fractures. -
The elbow accounts for only 20% of the longitudinal growth of the upper extremity.
-
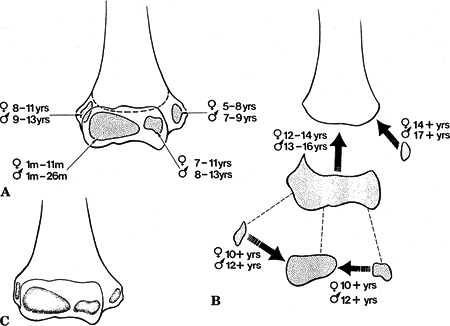
Ossification: With the exception of the
capitellum, ossification centers appear approximately 2 years earlier
in girls compared with boys -
CRMTOL: The following is a mnemonic for the appearance of the ossification centers around the elbow (Fig. 44.1):
| Capitellum: | 6 months to 2 years; includes the lateral crista of the trochlea |
| Radial head: | 4 years |
| Medial epicondyle: | 6 to 7 years |
| Trochlea: | 8 years |
| Olecranon: | 8 to 10 years; often multiple centers, which ultimately fuse |
| Lateral epicondyle: | 12 years |
 |
|
Figure
44.1. Ossification and fusion of the secondary centers of the distal humerus. (A) The average ages of the onset of ossification of the various ossification centers are shown for both boys and girls. (B) The ages at which these centers fuse with each other are shown for both boys and girls. (C) The contribution of each secondary center to the overall architecture of the distal humerus is represented by the stippled areas. (From Rockwood CA, Wilkins KE, Beaty JH. Fractures and Dislocations in Children. Philadelphia: Lippincott-Raven, 1999:662.)
|
-
Indirect: This is most commonly a result of a fall onto an outstretched upper extremity.
-
Direct: Direct trauma to the elbow may
occur from a fall onto a flexed elbow or from an object striking the
elbow (e.g., baseball bat, automobile).
-
Patients typically present with varying
degrees of gross deformity, usually accompanied by pain, swelling,
tenderness, irritability, and refusal to use the injured extremity. -
The ipsilateral shoulder, humeral shaft, forearm, wrist, and hand should be examined for associated injuries.
-
A careful neurovascular examination
should be performed, with documentation of the integrity of the median,
radial, and ulnar nerves, as well as distal pulses and capillary
refill. Massive swelling in the antecubital fossa should alert the
examiner to evaluate for compartment syndrome of the forearm. Flexion
of
P.502
the
elbow in the presence of antecubital swelling may cause neurovascular
embarrassment; repeat evaluation of neurovascular integrity is
essential following any manipulation or treatment. -
All aspects of the elbow should be
examined for possible open lesions; clinical suspicion may be followed
with intraarticular injection of saline into the elbow to evaluate
possible intraarticular communication of a laceration.
-
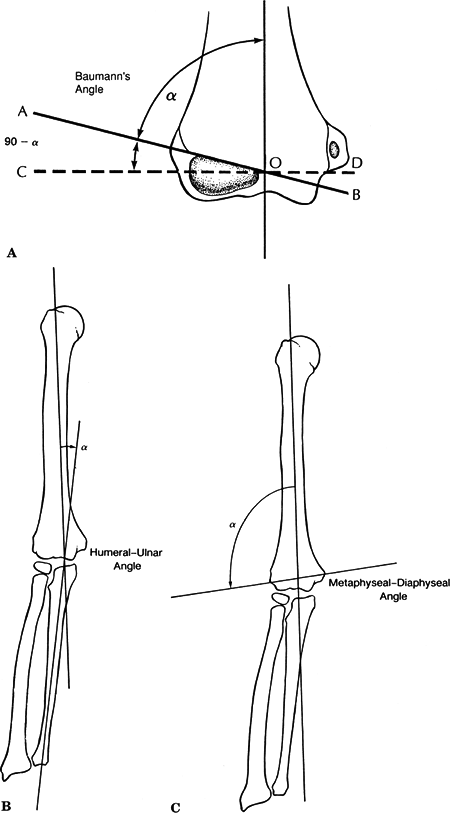
Standard anteroposterior (AP) and lateral
views of the elbow should be obtained. On the AP view, the following
angular relationships may be determined (Fig. 44.2):-
Baumann angle: This is the angulation of
the lateral condylar physeal line with respect to the long axis of the
humerus; normal is 15 to 20 degrees and equal to the opposite side. -
Humeral-ulnar angle: This angle is
subtended by the intersection of the diaphyseal bisectors of the
humerus and ulna; this best reflects the true carrying angle. -
Metaphyseal-diaphyseal angle: This angle
is formed by a bisector of the humeral shaft with respect to a line
delineated by the widest points of the distal humeral metaphysic.
-
-
On a true lateral radiograph of the elbow flexed to 90 degrees, the following landmarks should be observed (Fig. 44.3):
-
Teardrop: This radiographic shadow is
formed by the posterior margin of the coronoid fossa anteriorly, the
anterior margin of the olecranon fossa posteriorly, and the superior
margin of the capitellar ossification center inferiorly. -
Diaphyseal-condylar angle: This projects
30 to 45 degrees anteriorly; the posterior capitellar physis is
typically wider than the anterior physis. -
Anterior humeral line: When extended
distally, this line should intersect the middle third of the capitellar
ossification center. -
Coronoid line: A proximally directed line
along the anterior border of the coronoid process should be tangent to
the anterior aspect of the lateral condyle.
-
-
Special views
-
Jones view: Pain may limit an AP
radiograph of the elbow in extension; in these cases, a radiograph may
be taken with the elbow hyperflexed and the beam directed at the elbow
through the overlying forearm with the arm flat on the cassette in
neutral rotation. -
Internal and external rotation views may
be obtained in cases in which a fracture is suspected but not clearly
demonstrated on routine views. These may be particularly useful in the
identification of coronoid process or radial head fractures.
![]() Figure
Figure
44.2. Anteroposterior x-ray angles for the elbow. (A) The Baumann angle
(α). (B) The humeral-ulnar angle. (C) The metaphyseal-diaphyseal angle.(From O’Brien
WR, Eilert RE, Chang FM, et al. The metaphyseal-diaphyseal angle as a
guide to treating supracondylar fractures of the humerus in children,
1999, unpublished data.)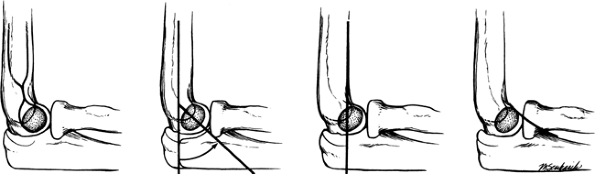 Figure
Figure
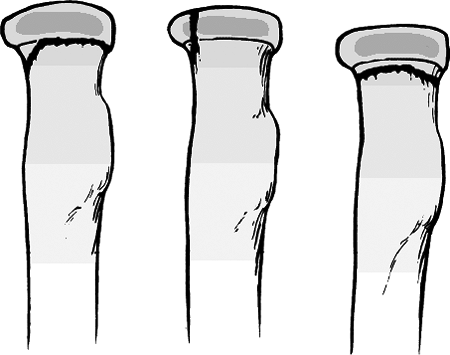
44.3. Intraosseous blood supply of the distal humerus. (A) The vessels
supplying the lateral condylar epiphysis enter on the posterior aspect
and course for a considerable distance before reaching the ossific
nucleus. (B) Two definite vessels supply the ossification center of the
medial crista of the trochlea. The lateral one enters by crossing the
physis. The medial one enters by way of the nonarticular edge of the
medial crista.(From Rockwood CA, Wilkins KE, Beaty JH. Fractures and Dislocations in Children. Philadelphia: Lippincott-Raven, 1999:663.) -
-
The contralateral elbow should be obtained for comparison as well as identification of ossification centers. A pseudofracture
of an ossification center may exist, in which apparent fragmentation of
an ossification center may represent a developmental variant rather
than a true fracture. This may be clarified with comparison views of
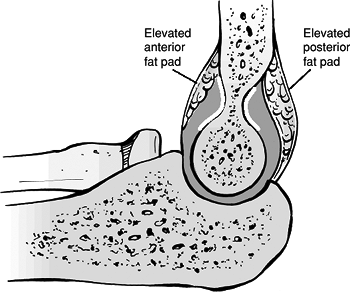
the uninjured contralateral elbow.![]() Figure 44.4. Elevated anterior and posterior fat pads.(Adapted from The Journal of Bone and Joint Surgery, in Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 44.4. Elevated anterior and posterior fat pads.(Adapted from The Journal of Bone and Joint Surgery, in Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Fat pad signs: Three fat pads overlie the major structures of the elbow (Fig. 44.4):
-
Anterior (coronoid) fat pad: This
triangular lucency seen anterior to the distal humerus may represent
displacement of the fat pad owing to underlying joint effusion. The
coronoid fossa is shallow; therefore, anterior displacement of the fat
pad is sensitive to small effusions. However, an exuberant fat pad may
be seen without associated trauma, diminishing the specificity of the
anterior fat pad sign. -
Posterior (olecranon) fat pad: The deep
olecranon fossa normally completely contains the posterior fat pad.
Thus, only moderate to large effusions cause posterior displacement,
resulting in a high specificity of the posterior fat pad sign for
intraarticular disorders (a fracture is present >70% of the time
when the posterior fat pad is seen). -
Supinator fat pad: This represents a
layer of fat on the anterior aspect of the supinator muscle as it wraps
around the proximal radius. Anterior displacement of this fat pad may
represent a fracture of the radial neck; however, this sign has been
reported to be positive in only 50% of cases. -
Anterior and posterior fat pads may not
be seen following elbow dislocation owing to disruption of the joint
capsule, which decompresses the joint effusion.
-
-
These comprise 55% to 75% of all elbow fractures.
-
The male-to-female ratio is 3:2.
-
The peak incidence is from 5 to 8 years, after which dislocations become more frequent.
-
The left, or nondominant side, is most frequently injured.
-
Remodeling of bone in the 5- to 8-year
old causes a decreased anteroposterior diameter in the supracondylar
region, making this area susceptible to injury. -
Ligamentous laxity in this age range increases the likelihood of hyperextension injury.
-
The anterior capsule is thickened and
stronger than the posterior capsule. In extension, the fibers of the
anterior capsule are taut, serving as a fulcrum by which the olecranon
becomes firmly engaged in the olecranon fossa. With extreme force,
hyperextension may cause the olecranon process to impinge on the
superior olecranon fossa and supracondylar region. -
The periosteal hinge remains intact on the side of the displacement.
-
Extension type: Hyperextension occurs
during fall onto an outstretched hand with or without varus/valgus
force. If the hand is pronated, posteromedial displacement occurs. If
the hand is supinated posterolateral displacement occurs. Posteromedial
displacement is more common. -
Flexion type: The cause is direct trauma or a fall onto a flexed elbow.
-
Patients typically present with a swollen, tender elbow with painful range of motion.
-
S-shaped angulation at the elbow: a complete (Type III) fracture results in two points of angulation to give it an S shape.
-
Pucker sign: This is dimpling of the skin
anteriorly secondary to penetration of the proximal fragment into the
brachialis muscle; it should alert the examiner that reduction of the
fracture may be difficult with simple manipulation. -
Neurovascular examination: A careful
neurovascular examination should be performed with documentation of the
integrity of the median, radial, and ulnar nerves as well as their
terminal branches. Capillary refill and distal pulses should be
documented. The examination should be repeated following splinting or
manipulation.
| Type I: | Immobilization in a long arm cast or splint at 60 to 90 degrees of flexion is indicated for 2 to 3 weeks. |
| Type II: | This is usually reducible by closed methods followed by casting; it may require pinning if unstable (crossed pins versus two lateral pins) or if reduction cannot be maintained without excessive flexion that may place neurovascular structures at risk. |
| Type III: | Attempt closed reduction and pinning; traction (olecranon skeletal traction) may be needed for comminuted fractures with marked soft tissue swelling or damage. Open reduction and internal fixation may be necessary for rotationally unstable fractures, open fractures, and those with neurovascular injury (crossed pins versus two lateral pins). |
-
Concepts involved in reduction
-
Displacement is corrected in the coronal and horizontal planes before the sagittal plane.
-
Hyperextension of the elbow with longitudinal traction is used to obtain apposition.
-
Flexion of the elbow is done while applying a posterior force to the distal fragment.
-
Stabilization with control of displacement in the coronal, sagittal, and horizontal planes is recommended.
-
Lateral pins are placed first to obtain
provisional stabilization, and if a medial pin is needed, the elbow can
be extended before pin placement to help protect the ulnar nerve.
-
| Type I: | Immobilization in a long arm cast in near extension is indicated for 2 to 3 weeks. |
| Type II: | Closed reduction is followed by percutaneous pinning with two lateral pins or crossed pins. |
| Type III: | Reduction is often difficult; most require open reduction and internal fixation with crossed pins. |
-
Immobilization in a long arm cast (or
posterior splint if swelling is an issue) with the elbow flexed to 90
degrees and the forearm in neutral should be undertaken for 2 to 3
weeks postoperatively, at which time the cast may be discontinued and
the pins
P.508
removed.
The patient should then be maintained in a sling with range-of-motion
exercises and restricted activity for an additional 4 to 6 weeks.
-
Neurologic injury (7% to 10%): This may
be caused by a traction injury during reduction owing to tenting or
entrapment at the fracture site. It also may occur as a result of
Volkmann ischemic contracture, angular deformity, or incorporation into
the callus or scar. Most are neurapraxias requiring no treatment.-
Median nerve/anterior interosseous nerve (most common)
-
Radial nerve
-
Ulnar nerve: This is most common in
flexion-type supracondylar fractures; early injury may result from
tenting over the medial spike of the proximal fragment; late injury may
represent progressive valgus deformity of the elbow. It is frequently
iatrogenic in extension-type supracondylar fractures following medial
pinning.
-
-
Vascular injury (0.5%): This may
represent direct injury to the brachial artery or may be secondary to
antecubital swelling. This emphasizes the need for a careful
neurovascular examination both on initial presentation and following
manipulation or splinting, especially after elbow flexion is performed.
Observation may be warranted if the pulse is absent, yet the hand is
still well perfused. -
Loss of motion: A >5-degree loss of elbow motion occurs in 5% secondary to poor reduction or soft tissue contracture.
-
Myositis ossificans: Rare and is seen after vigorous manipulation.
-
Angular deformity (varus more frequently
than valgus): Significant in 10% to 20%; the occurrence is decreased
with percutaneous pinning (3%) compared with reduction and casting
alone (14%). -
Compartment syndrome (<1%): This rare
complication can be exacerbated by elbow hyperflexion when excessive
swelling is present in the cubital fossa.
-
These comprise 17% of all distal humerus fractures.
-
Peak age is 6 years.
-
Often result in less satisfactory outcomes than supracondylar fractures because:
-
Diagnosis less obvious and may be missed in subtle cases.
-
Loss of motion is more severe due to intraarticular nature.
-
The incidence of growth disturbance is higher.
-
-
The ossification center of the lateral condyle extends to the lateral crista of the trochlea.
-
Lateral condylar physeal fractures are
typically accompanied by a soft tissue disruption between the origins
of the extensor carpi radialis longus and the brachioradialis muscles;
these origins remain attached to the free distal fragment, accounting
for initial and late displacement of the fracture. -
Disruption of the lateral crista of the
trochlea (Milch Type II fractures) results in posterolateral
subluxation of the proximal radius and ulna with consequent cubitus
valgus; severe posterolateral translocation may lead to the erroneous
diagnosis of primary elbow dislocation.
-
“Pull-off” theory: Avulsion injury occurs by the common extensor origin owing to a varus stress exerted on the extended elbow.
-
“Push-off” theory: A fall onto an
extended upper extremity results in axial load transmitted through the
forearm, causing the radial head to impinge on the lateral condyle.
-
Unlike the patient with a supracondylar
fracture of the elbow, patients with lateral condylar fractures
typically present with little gross distortion of the elbow, other than
mild swelling from fracture hematoma most prominent over the lateral
aspect of the distal humerus. -
Crepitus may be elicited associated with supination-pronation motions of the elbow.
-
Pain, swelling, tenderness to palpation, painful range of motion, and pain on resisted wrist extension may be observed.
-
AP, lateral, and oblique views of the elbow should be obtained.
-
Varus stress views may accentuate displacement of the fracture.
-
In a young child whose lateral condyle is
not ossified, it may be difficult to distinguish between a lateral
condylar physeal fracture and a complete distal humeral physeal
fracture. In such cases, an arthrogram may be helpful, and the
relationship of the lateral condyle to the proximal radius is critical:-
Lateral condyle physeal fracture: This
disrupts the normal relationship with displacement of the proximal
radius laterally owing to loss of stability provided by the lateral
crista of the distal humerus. -
Fracture of the entire distal humeral
physis: The relationship of the lateral condyle to the proximal radius
is intact, often accompanied by posteromedial displacement of the
proximal radius and ulna.
-
-
Magnetic resonance imaging (MRI) may help to appreciate the direction of the fracture line and the pattern of fracture.
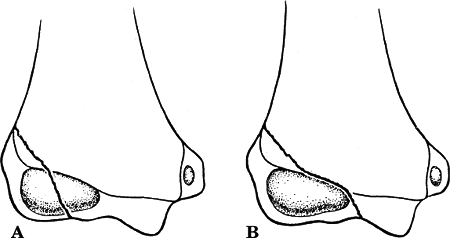
| Type I: | The fracture line courses lateral to the trochlea and into the capitulotrochlear groove. It represents a Salter-Harris Type IV fracture: the elbow is stable because the trochlea is intact; this is less common. |
| Type II: | The fracture line extends into the apex of the trochlea. It represents a Salter-Harris Type II fracture: the elbow is unstable because the trochlea is disrupted; this is more common (Fig. 44.5). |
 |
|
Figure
44.5. Physeal fractures of the lateral condyle. (A) Salter-Harris Type IV physeal injury (Milch Type I). (B) Salter-Harris Type II physeal injury (Milch Type II). (From Rockwood CA, Wilkins KE, Beaty JH. Fractures and Dislocations in Children. Philadelphia: Lippincott-Raven, 1999:753.)
|
| Stage I: | Fracture nondisplaced with an intact articular surface |
| Stage II: | Fracture with moderate displacement |
| Stage III: | Complete displacement and rotation with elbow instability |
-
Nondisplaced or minimally displaced
fractures (Jakob stage I; <2 mm) (40% of fractures) may be treated
with simple immobilization in a posterior splint or long arm cast with
the forearm in neutral position and the elbow flexed to 90 degrees.
This is maintained for 3 to 4 weeks, after which range-of-motion
exercises are instituted. -
Closed reduction of fractures (Jakob
stage II) may be performed with the elbow extended and the forearm
supinated. Further room for manipulation may be provided by exerting
varus stress on the elbow. If the reduction is unable to be held,
percutaneous pins may be placed. Closed reduction is unsuccessful in
50% owing to rotation. Late displacement is a frequent complication.
-
Open reduction is required for unstable Jakobs stage II and stage III fractures (60%).
-
The fragment may be secured with two crossed, smooth Kirschner wires that diverge in the metaphysis.
-
The passage of smooth pins through the physis does not typically result in growth disturbance.
-
Care must be taken when dissecting near
the posterior aspect of the lateral condylar fragment because the sole
vascular supply is provided through soft tissues in this region. -
Postoperatively, the elbow is maintained
in a long arm cast at 60 to 90 degrees of flexion with the forearm in
neutral rotation. The cast is discontinued 3 to 4 weeks postoperatively
with pin removal. Active range-of-motion exercises are instituted.
-
-
If treatment is delayed (>3 weeks),
closed treatment should be strongly considered, regardless of
displacement, owing to the high incidence of osteonecrosis of the
condylar fragment with late open reduction.
-
Lateral condylar overgrowth with spur
formation: This usually results from an ossified periosteal flap raised
from the distal fragment at the time of injury or surgery. It may
represent a cosmetic problem (cubitus pseudovarus) as the elbow gains
the appearance of varus owing to a lateral prominence but is generally
not a functional problem. -
Delayed union or nonunion (>12 weeks):
This is caused by pull of extensors and poor metaphyseal circulation of
the lateral condylar fragment, most commonly in patients treated
nonoperatively. It may result in cubitus valgus necessitating ulnar
nerve transposition for tardy ulnar nerve palsy. Treatment ranges from
benign neglect to osteotomy and compressive fixation late or at
skeletal maturity. -
Angular deformity: Cubitus valgus occurs
more frequently than varus owing to lateral physeal arrest. Tardy ulnar
nerve palsy may develop necessitating transposition. -
Neurologic compromise: This is rare in the acute setting. Tardy ulnar nerve palsy may develop as a result of cubitus valgus.
-
Osteonecrosis: This is usually
iatrogenic, especially when surgical intervention was delayed. It may
result in a “fishtail” deformity with a persistent gap between the
lateral physeal ossification center and the medial ossification of the
trochlea.
-
Represent <1% of distal humerus fractures.
-
Typical age range is 8 to 14 years.
-
Medial condylar fractures are
Salter-Harris Type IV fractures with an intraarticular component
involving the trochlea and an extraarticular component involving the
medial metaphysis and the medial epicondyle (common flexor origin). -
Only the medial crista is ossified by the secondary ossification centers of the medial condylar epiphysis.
-
The vascular supply to the medial
epicondyle and metaphysis is derived from the flexor muscle group. The
vascular supply to the lateral aspect of the medial crista of the
trochlea traverses the surface of the medial condylar physis, rendering
it vulnerable in medial physeal disruptions with possible avascular
complications and “fishtail” deformity.
-
Direct: Trauma to the point of the elbow,
such as a fall onto a flexed elbow, results in the semilunar notch of
the olecranon traumatically impinging on the trochlea, splitting it
with the fracture line extending proximally to metaphyseal region. -
Indirect: A fall onto an outstretched
hand with valgus strain on the elbow results in an avulsion injury with
the fracture line starting in the metaphysis and propagating distally
through the articular surface. -
These are considered the mirror image of lateral condylar physeal fractures.
-
Once dissociated from the elbow, the powerful forearm flexor muscles produce sagittal anterior rotation of the fragment.
-
Patients typically present with pain,
swelling, and tenderness to palpation over the medial aspect of the
distal humerus. Range of motion is painful, especially with resisted
flexion of the wrist. -
A careful neurovascular examination is important, because ulnar nerve symptoms may be present.
-
A common mistake is to diagnose a medial
condylar physeal fracture erroneously as an isolated medial epicondylar
fracture. This occurs based on tenderness and swelling medially in
conjunction with radiographs demonstrating a medial epicondylar
fracture only resulting from the absence of a medial condylar
ossification center in younger patients. -
Medial epicondylar fractures are often
associated with elbow dislocations, usually posterolateral; elbow
dislocations are extremely rare before ossification of the medial
condylar epiphysis begins. With medial condylar physeal fractures,
subluxation of the elbow posteromedially is often observed. A positive
fat pad sign indicates an intraarticular fracture, whereas a medial
epicondyle fracture is typically extraarticular with no fat pad sign
seen on radiographs.
-
AP, lateral, and oblique views of the elbow should be obtained.
-
In young children whose medial condylar
ossification center is not yet present, radiographs may demonstrate a
fracture in the epicondylar region; in such cases, an arthrogram may
delineate the course of the fracture through the articular surface,
indicating a medial condylar physeal fracture. -
Stress views may help to distinguish
epicondylar fractures (valgus laxity) from condylar fractures (both
varus and valgus laxity). -
MRI may help to appreciate the direction of the fracture line and the pattern of fracture.
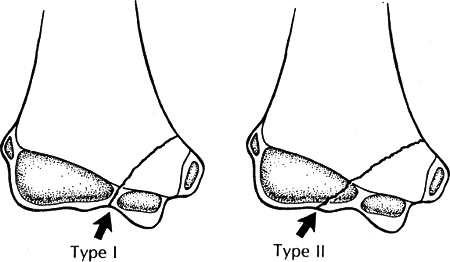
| Type I: | Fracture line traversing through the apex of the trochlea: Salter-Harris Type II; more common presentation |
| Type II: | Fracture line through capitulotrochlear groove: Salter-Harris Type IV; infrequent presentation |
 |
|
Figure 44.6. Fracture patterns. Left: In the Milch Type I injury, the fracture line terminates in the trochlea notch (arrow). Right: In the Milch Type II injury, the fracture line terminates in the capitulotrochlear groove (arrow).
(From Rockwood CA, Wilkins KE, Beaty JH. Fractures and Dislocations in Children. Philadelphia: Lippincott-Raven, 1999:786.)
|
-
Closed reduction may be performed with
the elbow extended and the forearm pronated to relieve tension on the
flexor origin, with placement of a posterior splint or long arm cast.
Unstable reductions may require percutaneous pinning with two parallel
metaphyseal pins. -
Closed reduction is often difficult
because of medial soft tissue swelling, and open reduction is usually
required for stage II and III fractures.
-
Unreducible or unstable Kilfoyle stage II
or stage III fractures of the medial condylar physis may require open
reduction and internal fixation. Rotation of the condylar fragment may
preclude successful closed treatment.-
A medial approach may be used with identification and protection of the ulnar nerve.
-
The posterior surface of the condylar
fragment and the medial aspect of the medial crista of the trochlea
should be avoided in the dissection because these provide the vascular
supply to the trochlea. -
Smooth Kirschner wires placed in a
parallel configuration extending to the metaphysis may be used for
fixation, or cancellous screw fixation may be used in adolescents near
skeletal maturity. -
Postoperative immobilization consists of
long arm casting with the forearm in neutral rotation and the elbow
flexed to 90 degrees for 3 to 4 weeks, at which time the pins and the
cast may be discontinued and active range-of-motion exercises
instituted.
-
-
If treatment is delayed (>3 weeks),
closed treatment should be strongly considered, regardless of
displacement, owing to the high incidence of osteonecrosis of the
trochlea and lateral condylar fragment from extensive dissection with
late open reduction.
-
Missed diagnosis: The most common is a
medial epicondylar fracture owing to the absence of ossification of the
medial condylar ossification center. Late diagnosis of medial condylar
physeal fracture should be treated nonoperatively. -
Nonunion: Uncommon and usually represent
untreated, displaced medial condylar physeal fractures secondary to
pull of flexors with rotation. They tend to demonstrate varus
deformity. After ossification, the lateral edge of the fragment may be
observed to extend to the capitulotrochlear groove. -
Angular deformity: Untreated or treated
medial condylar physeal fractures may demonstrate angular deformity,
usually varus, either secondary to angular displacement or from medial
physeal arrest. Cubitus valgus may result from overgrowth of the medial
condyle. -
Osteonecrosis: This may result after open reduction and internal fixation, especially when extensive dissection is undertaken.
-
Ulnar neuropathy: This may be early,
related to trauma, or more commonly, late, related to the development
of angular deformities or scarring. Recalcitrant symptoms may be
addressed with ulnar nerve transposition.
-
Most occur in patients younger than age 6 to 7 years.
-
These were originally thought to be
extremely rare injuries. It now appears that with advanced imaging
(e.g., MRI), they occur fairly frequently, although the exact incidence
is not known owing to misdiagnoses.
-
The epiphysis includes the medial
epicondyle until age 6 to 7 years in girls and 8 to 9 years in boys, at
which time ossification occurs. Fractures before this time thus include
medial epicondyle. -
The younger the child, the greater the
volume of the distal humerus that is occupied by the distal epiphysis;
as the child matures, the physeal line progresses distally, with a
V-shaped cleft forming between the medial and lateral condylar
physes—this cleft protects the distal humeral epiphysis from fracture
in the mature child, because fracture lines tend to exit through the
cleft. -
The joint surface is not involved in this injury, and the relationship between the radius and capitellum is maintained.
-
The anteroposterior diameter of the bone
in this region is wider than in the supracondylar region, and
consequently there is not as much tilting or rotation. -
The vascular supply to the medial crista
of the trochlea courses directly through the physis; in cases of
fracture, this may lead to avascular changes. -
The physeal line is in a more proximal
location in younger patients, therefore, hyperextension injuries to the
elbow tend to result in physeal separations instead of supracondylar
fractures through bone.
-
Birth injuries: Rotatory forces coupled
with hyperextension injury to the elbow during delivery may result in
traumatic distal humeral physeal separation. -
Child abuse: Bright demonstrated that the
physis fails most often in shear rather than pure bending or tension.
Therefore, in young infants or children, child abuse must be suspected,
because a high incidence of transphyseal fracture is associated with
abuse. -
Trauma: This may result from hyperextension injuries with posterior displacement, coupled with a rotation moment.
-
Young infants or newborns may present
with pseudoparalysis of the affected extremity, minimal swelling, and
“muffled crepitus,” because the fracture involves softer cartilage
rather than firm, osseous tissue. -
Older children may present with
pronounced swelling, refusal to use the affected extremity, and pain
that precludes a useful clinical examination or palpation of bony
landmarks. In general, because of the large, wide fracture surface
there is less tendency for tilting or rotation of the distal fragment,
resulting in less deformity than seen in supracondylar fractures. The
bony relationship between the humeral epicondyles and the olecranon is
maintained. -
A careful neurovascular examination
should be performed, because swelling in the cubital fossa may result
in neurovascular compromise.
-
AP, lateral, oblique radiographs should be obtained.
-
The proximal radius and ulna maintain
normal, anatomic relationships to each other, but they are displaced
posteromedially with respect to the distal humerus. This is considered
diagnostic of transphyseal fracture. -
Comparison views of the contralateral elbow may be used to identify posteromedial displacement.
-
In the child whose lateral condylar
epiphysis is ossified, the diagnosis is much more obvious. There is
maintenance of the lateral condylar epiphysis to radial head
relationship and posteromedial displacement of the distal humeral
epiphysis with respect to the humeral shaft. -
Transphyseal fractures with large metaphyseal components may be mistaken for a low supracondylar fracture or a fracture
P.516
of the lateral condylar physis. These may be differentiated by the
presence of a smooth outline of the distal metaphysis in fractures
involving the entire distal physis as compared with the irregular
border of the distal aspect of the distal fragment seen in
supracondylar fractures. -
Elbow dislocations in children are rare,
but they may be differentiated from transphyseal fractures by primarily
posterolateral displacement and a disrupted relationship between the
lateral condylar epiphysis and the proximal radius. -
An arthrogram may be useful for clarification of the fracture pattern and differentiation from an intraarticular fracture.
-
MRI may be helpful in appreciating the direction of the fracture line and the pattern of fracture.
-
Ultrasound may be useful in evaluating neonates and infants in whom ossification has not yet begun.
| Group A: | Infant, before the appearance of the lateral condylar ossification center (birth to 7 months); diagnosis easily missed; Salter-Harris type I |
| Group B: | Lateral condyle ossified (7 months to 3 years); Salter-Harris type I or II (fleck of metaphysis) |
| Group C: | Large metaphyseal fragment, usually exiting laterally (age 3 to 7 years) |
represent child abuse injuries, it is not uncommon for parents to delay
seeking treatment.
-
Closed reduction with immobilization is
performed with the forearm pronated and the elbow in 90 degrees of
flexion if the injury is recognized early (within 4 to 5 days). This is
maintained for 3 weeks, at which time the patient is allowed to resume
active range of motion. -
Severe swelling of the elbow may necessitate Dunlop-type sidearm traction. Skeletal traction is typically not necessary.
-
When treatment is delayed beyond 6 to 7
days of injury, the fracture should not be manipulated regardless of
displacement, because the epiphyseal fragment is no longer mobile and
other injuries may be precipitated; rather, splinting for comfort
should be undertaken. Most fractures eventually completely remodel by
maturity.
-
DeLee Type C fracture patterns or
unstable injuries may necessitate percutaneous pinning for fixation. An
arthrogram is usually performed to determine the adequacy of reduction. -
Angulation and rotational deformities
that cannot be reduced by closed methods may require open reduction and
internal fixation with pinning for fixation.
-
Malunion: Cubitus varus is most common,
although the incidence is lower than with supracondylar fractures of
the humerus because of the wider fracture surface of transphyseal
fractures that do not allow as much angulation compared with
supracondylar fractures. -
Neurovascular injury: Extremely rare
because the fracture surfaces are covered with cartilage. Closed
reduction and immobilization should be followed by repeat neurovascular
assessment, given that swelling in the antecubital fossa may result in
neurovascular compromise. -
Nonunion: Extremely rare because the vascular supply to this region is good.
-
Osteonecrosis: May be related to severe
displacement of the distal fragment or iatrogenic injury, especially
with late exploration.
-
Comprise 14% of distal humerus fractures.
-
50% are associated with elbow dislocations.
-
The peak age is 11 to 12 years.
-
The male-to-female ratio is 4:1.
-
The medial epicondyle is a traction
apophysis for the medial collateral ligament and wrist flexors. It does
not contribute to humeral length. The forces across this physis are
tensile rather than compressive. -
Ossification begins at 4 to 6 years of
age; it is the last ossification center to fuse with the metaphysis (15
years) and does so independently of the other ossification centers. -
The fragment is usually displaced distally and may be incarcerated in the joint 15% to 18% of the time.
-
It is often associated with fractures of the proximal radius, olecranon and coronoid.
-
In younger children, a medial epicondylar
apophyseal fracture may have an intracapsular component, because the
elbow capsule may attach as proximally as the physeal line of the
epicondyle. In the older child, these fractures are generally
extracapsular given that the capsular attachment is more distal, to the
medial crista of the trochlea.
-
Direct: Trauma to the posterior or
posteromedial aspect of the medial epicondyle may result in fracture,
although these are rare and tend to produce fragmentation of the medial
epicondylar fragment. -
Indirect:
-
Secondary to elbow dislocation: The ulnar collateral ligament provides avulsion force.
-
Avulsion injury by flexor muscles results
from valgus and extension force during a fall onto an outstretched hand
or secondary to an isolated muscle avulsion from throwing a ball or arm
wrestling, for example.
P.518 -
-
Chronic: Related to overuse injuries from repetitive throwing, as seen in skeletally immature baseball pitchers.
-
Patients typically present with pain, tenderness, and swelling medially.
-
Symptoms may be exacerbated by resisted wrist flexion.
-
A careful neurovascular examination is
essential, because the injury occurs in proximity to the ulnar nerve,
which can be injured during the index trauma or from swelling about the
elbow. -
Decreased range of motion is usually
elicited and may be secondary to pain. Occasionally, a mechanical block
to range of motion may result from incarceration of the epicondylar
fragment within the elbow joint. -
Valgus instability can be appreciated on
stress testing with the elbow flexed to 15 degrees to eliminate the
stabilizing effect of the olecranon.
-
AP, lateral, and oblique radiographs of the elbow should be obtained.
-
Because of the posteromedial location of
the medial epicondylar apophysis, the ossification center may be
difficult to visualize on the AP radiograph if it is even slightly
oblique. -
The medial epicondylar apophysis is
frequently confused with fracture because of the occasionally
fragmented appearance of the ossification center as well as the
superimposition on the distal medial metaphysis. Better visualization
may be obtained by a slight oblique of the lateral radiograph, which
demonstrates the posteromedial location of the apophysis. -
A gravity stress test may be performed, demonstrating medial opening on stress radiographs.
-
Complete absence of the apophysis on
standard elbow views should prompt a search for the displaced fragment
after comparison views of the contralateral, normal elbow are obtained.
Specifically, incarceration within the joint must be sought, because
the epicondylar fragment may be obscured by the distal humerus. -
Fat pad signs are unreliable, given that
epicondylar fractures are extracapsular in older children and capsular
rupture associated with elbow dislocation may compromise its ability to
confine the hemarthrosis. -
It is important to differentiate this
fracture from a medial condylar physeal fracture; MRI or arthrogram may
delineate the fracture pattern, especially when the medial condylar
ossification center is not yet present.
-
Acute
-
Chronic
-
Tension stress injuries (“Little League elbow”)
-
-
Most medial epicondylar fractures may be
managed nonoperatively with immobilization. Studies demonstrate that
although 60% may establish only fibrous union, 96% have good or
excellent functional results. -
Nonoperative treatment is indicated for
nondisplaced or minimally displaced fractures and for significantly
displaced fractures in older or low-demand patients. -
The patient is initially placed in a
posterior splint with the elbow flexed to 90 degrees with the forearm
in neutral or pronation. -
The splint is discontinued 3 to 4 days after injury and early active range of motion is instituted. A sling is worn for comfort.
-
Aggressive physical therapy is generally not necessary unless the patient is unable to perform active range-of-motion exercises.
-
An absolute indication for operative
intervention is an irreducible, incarcerated fragment within the elbow
joint. Closed manipulation may be used to attempt to extract the
incarcerated fragment from the joint as described by Roberts. The
forearm is supinated, and valgus stress is applied to the elbow,
followed by dorsiflexion of the wrist and fingers to put the flexors on
stretch. This maneuver is successful approximately 40% of the time. -
Relative indications for surgery include
ulnar nerve dysfunction owing to scar or callus formation, valgus
instability in an athlete, or significantly displaced fractures in
younger or high-demand patients. -
Acute fractures of the medial epicondyle
may be approached through a longitudinal incision just anterior to the
medial epicondyle. Ulnar nerve identification is important, but
extensive dissection or transposition is generally unnecessary. After
reduction and provisional fixation with Kirschner wires, fixation may
be achieved with a lag-screw technique. A washer may be used in cases
of poor bone stock or fragmentation. -
Postoperatively, the patient is placed in
a posterior splint or long arm cast with the elbow flexed to 90 degrees
and the forearm pronated. This may be converted to a removable
posterior splint or sling at 7 to 10 days postoperatively, at which
time active range-of-motion exercises are instituted. Formal physical
therapy is generally unnecessary if the patient is able to perform
active exercises.
-
Unrecognized intraarticular
incarceration: An incarcerated fragment tends to adhere and form a
fibrous union to the coronoid process, resulting in significant loss of
elbow range of motion. Although earlier recommendations were to manage
this nonoperatively, recent recommendations are to explore the joint
with excision of the fragment. -
Ulnar nerve dysfunction: The incidence is
10% to 16%, although cases associated with fragment incarceration may
have up to a 50% incidence of ulnar nerve dysfunction. Tardy ulnar
neuritis may develop in cases involving reduction of the elbow or
manipulation in which scar tissue may be exuberant. Surgical
exploration and release may be warranted for symptomatic relief. -
Nonunion: May occur in up to 60% of cases
with significant displacement treated nonoperatively, although it
rarely represents a functional problem. -
Loss of extension: A 5% to 10% loss of
extension is seen in up to 20% of cases, although this rarely
represents a functional problem. This emphasizes the need for early
active range-of-motion exercises. -
Myositis ossificans: Rare, related to
repeated and vigorous manipulation of the fracture. It may result in
functional block to motion and must be differentiated from ectopic
calcification of the collateral ligaments related to microtrauma, which
does not result in functional limitation.
-
Extremely rare in children.
-
The lateral epicondylar ossification
center appears at 10 to 11 years of age; however, ossification is not
completed until the second decade of life. -
The lateral epicondyle represents the
origin of many of the wrist and forearm extensors; therefore, avulsion
injuries account for a proportion of the fractures, as well as
displacement once the fracture has occurred.
-
Direct trauma to the lateral epicondyle may result in fracture; these may be comminuted.
-
Indirect trauma may occur with forced
volarflexion of an extended wrist, causing avulsion of the extensor
origin, often with significant displacement as the fragment is pulled
distally by the extensor musculature.
-
Patients typically present with lateral
swelling and painful range of motion of the elbow and wrist, with
tenderness to palpation of the lateral epicondyle. -
Loss of extensor strength may be appreciated.
-
The diagnosis is typically made on the AP
radiograph, although a lateral view should be obtained to rule out
associated injuries. -
The lateral epicondylar physis represents
a linear radiolucency on the lateral aspect of the distal humerus and
is commonly mistaken for a fracture. Overlying soft tissue swelling,
cortical discontinuity, and clinical examination should assist the
examiner in the diagnosis of lateral epicondylar apophyseal injury.
-
Avulsion
-
Comminution
-
Displacement
-
With the exception of an incarcerated
fragment within the joint, almost all lateral epicondylar apophyseal
fractures may be treated with immobilization with the elbow in the
flexed, supinated position until comfortable, usually by 2 to 3 weeks.
-
Incarcerated fragments within the elbow
joint may be simply excised. Large fragments with associated tendinous
origins may be reattached with screws or Kirschner wire fixation and
postoperative immobilization for 2 to 3 weeks until comfortable.
-
Nonunion: Commonly occurs with
established fibrous union of the lateral epicondylar fragment, although
it rarely represents a functional or symptomatic problem. -
Incarcerated fragments: May result in
limited range of motion, most commonly in the radiocapitellar
articulation, although free fragments may migrate to the olecranon
fossa and limit terminal extension.
-
Of these fractures, 31% are associated with injuries to the proximal radius.
-
Rare in children, representing 1:2,000 fractures about the elbow.
-
No verified, isolated fractures of the capitellum have ever been described in children younger than 12 years of age.
-
The fracture fragment is composed mainly
of pure articular surface from the capitellum and essentially
nonossified cartilage from the secondary ossification center of the
lateral condyle.
-
Indirect force from axial load
transmission from the hand through the radial head causes the radial
head to strike the capitellum. -
The presence of recurvatum or cubitus valgus predisposes the elbow to this fracture pattern.
-
Patients typically present with minimal swelling with painful range of motion. Flexion is often limited by the fragment.
-
Valgus stress tends to reproduce the pain over the lateral aspect of the elbow.
-
Supination and pronation may accentuate the pain.
-
AP and lateral views of the elbow should be obtained.
-
Radiographs of the normal, contralateral elbow may be obtained for comparison.
-
If the fragment is large and encompasses
ossified portions of the capitellum, it is most readily appreciated on
the lateral radiograph. -
Oblique views of the elbow may be
obtained if radiographic abnormality is not appreciated on standard AP
and lateral views, especially because a small fragment may be obscured
by the density of the overlying distal metaphysis on the AP view. -
Arthrography or MRI may be helpful when a
fracture is not apparent but is suspected to involve purely
cartilaginous portions of the capitellum.
| Type I: | Hahn-Steinthal fragment: large osseous component of capitellum, often involving the lateral crista of the trochlea |
| Type II: | Kocher-Lorenz fragment: articular cartilage with minimal subchondral bone attached; “uncapping of the condyle” |
-
Adequate reduction of displaced fractures
is difficult with closed manipulation. Modified closed reduction
involving placement of a Steinmann pin into the fracture fragment with
manipulation into the reduced position may be undertaken, with
postoperative immobilization consisting of casting with the elbow in
hyperflexion. -
Excision of the fragment is indicated for
fractures in which the fragment is small, comminuted, old (>2
weeks), or not amenable to anatomic reduction without significant
dissection of the elbow. -
Open reduction and internal fixation may
be achieved by the use of two lag screws, headless screws, or Kirschner
wires placed posterior to anterior or anterior to posterior. The heads
of the screws must be countersunk to avoid intraarticular impingement. -
Postoperative immobilization should
consist of casting with the elbow in hyperflexion for 2 to 4 weeks
depending on stability, with serial radiographic evaluation.
-
Osteonecrosis of the capitellar fragment:
This is uncommon; synovial fluid can typically sustain the fragment
until healing occurs. -
Posttraumatic osteoarthritis: This may
occur with secondary incongruity from malunion or particularly after a
large fragment is excised. -
Stiffness: Loss of extension is most
common, especially with healing of the fragment in a flexed position.
This is typically not significant, because it usually represents the
terminal few degrees of extension.
-
Rare, especially in young children,
although this rarity may represent misdiagnosis because purely
cartilaginous fractures would not be demonstrated on routine
radiographs. -
Peak incidence is in patients 12 to 13 years of age.
-
Because of the muscular origin of the
flexor and extensor muscles of the forearm, fragment displacement is
related not only to the inciting trauma but also to the tendinous
attachments. Displacement therefore includes rotational deformities in
both the sagittal and coronal planes. -
Fractures in the young child may have a
relatively intact distal humeral articular surface despite osseous
displacement of the overlying condylar fragments because of the
elasticity of the cartilage in the skeletally immature patient.
-
Flexion: Most represent wedge-type
fractures as the anterior margin of the semilunar notch is driven into
the trochlea by a fall onto the posterior aspect of the elbow in >90
degrees of flexion. The condylar fragments are usually anteriorly
displaced with respect to the humeral shaft. -
Extension: In this uncommon mechanism, a
fall onto an outstretched upper extremity results in a wedge-type
fracture as the coronoid process of the ulna is driven into the
trochlea. The condylar fragments are typically posteriorly displaced
with respect to the humeral shaft.
-
The diagnosis is most often confused with
extension-type supracondylar fractures because the patient typically
presents with the elbow extended, with pain, limited range of motion,
variable gross deformity, and massive swelling about the elbow. -
The ipsilateral shoulder, humeral shaft, forearm, wrist, and hand should be examined for associated injuries.
-
A careful neurovascular examination is
essential, with documentation of the integrity of the median, radial,
and ulnar nerves, as well as distal pulses and capillary refill.
Massive swelling in the antecubital fossa should alert the examiner to
evaluate for compartment syndrome of the forearm. Flexion of the elbow
in the presence of antecubital swelling may cause neurovascular
embarrassment; repeat evaluation of neurovascular integrity is thus
essential following any manipulation or treatment. -
All aspects of the elbow should be
examined for possible open lesions; clinical suspicion may be followed
with intraarticular injection of saline into the elbow to evaluate
possible intraarticular communication of a laceration.
-
Standard AP and lateral views of the injured elbow should be obtained.
-
Comparison views of the normal,
contralateral elbow may be obtained in which the diagnosis is not
readily apparent. Oblique views may aid in further fracture definition. -
In younger patients, the vertical,
intercondylar component may involve only cartilaginous elements of the
distal humerus; the fracture may thus appear to be purely
supracondylar, although differentiation of the two fracture patterns is
important because of the potential for articular disruption and
incongruency with T-type fractures. An arthrogram should be obtained
when intraarticular extension is suspected. -
Computed tomography and MRI are of
limited value and are not typically used in the acute diagnosis of
T-type fractures. In younger patients, these modalities often require
heavy sedation or anesthesia outside of the operating room, in which
case an arthrogram is preferred because it allows for evaluation of the
articular involvement as well as treatment in the operating room
setting.
| Type I: | Nondisplaced or minimally displaced |
| Type II: | Displaced, with no metaphyseal comminution |
| Type III: | Displaced, with metaphyseal comminution |
-
This is reserved only for truly
nondisplaced Type I fractures. Thick periosteum may provide sufficient
intrinsic stability such that the elbow may be immobilized in flexion
with a posterior splint. Mobilization is continued for 1 to 4 weeks
after injury. -
Skeletal olecranon traction with the
elbow flexed to 90 degrees may be used for patients with extreme
swelling, soft tissue compromise, or delayed cases with extensive skin
injury that precludes immediate operative intervention. If used as
definitive treatment, skeletal traction is usually continued for 2 to 3
weeks, at which time sufficient stability exists for the patient to be
converted to a hinged brace for an additional 2 to 3 weeks.
-
Closed reduction and percutaneous pinning
are used with increasing frequency for minimally displaced Type I
injuries, in accord with the current philosophy that the articular
damage, which cannot be appreciated on standard radiography, may be
worse than the apparent osseous involvement.-
Rotational displacement is corrected
using a percutaneous joystick in the fracture fragment, with placement
of multiple, oblique Kirschner wires for definitive fixation. -
The elbow is then protected in a posterior splint, with removal of pins at 3 to 4 weeks postoperatively.
-
-
Open reduction and internal fixation are
undertaken for Type II and Type III fractures using either a posterior,
triceps splitting approach, or the triceps-sparing approach as
described by Bryan and Morrey. Olecranon osteotomy is generally not
necessary for exposure and should be avoided.-
The articular surface is first
anatomically reduced and provisionally stabilized with Kirschner wires,
followed by metaphyseal reconstruction with definitive fixation using a
combination of Kirschner wires, compression screws, and plates. -
Semitubular plates are usually
inadequate; pelvic reconstruction plates and specifically designed
pediatric J-type plates have been used with success, often with two
plates placed 90 degrees offset from one another. -
Postoperatively, the elbow is placed in a
flexed position for 5 to 7 days, at which time active range of motion
is initiated and a removable cast brace is provided.
-
-
Loss of range of motion: T-type condylar
fractures are invariably associated with residual stiffness, especially
to elbow extension, owing to the often significant soft tissue injury
as well as articular disruption. This can be minimized by ensuring
anatomic reduction of the articular surface, employing arthrographic
visualization if necessary, as well as stable internal fixation to
decrease soft tissue scarring. -
Neurovascular injury: Rare but is related
to significant antecubital soft tissue swelling. Nerve injury to the
median, radial, or ulnar nerves may result from the initial fracture
displacement or intraoperative traction, although these typically
represent neurapraxias that resolve without intervention. -
Growth arrest: Partial or total growth
arrest may occur in the distal humeral physis, although it is rarely
clinically significant because T-type fractures tend to occur in older
children. Similarly, the degree of remodeling is limited, and anatomic
reduction should be obtained at the time of initial treatment. -
Osteonecrosis of the trochlea: This may
occur especially in association with comminuted fracture patterns in
which the vascular supply to the trochlea may be disrupted.
-
Of these fractures, 90% involve either physis or neck; the radial head is rarely involved because of the thick cartilage cap.
-
Represent 5% to 8.5% of elbow fractures.
-
The peak age of incidence is 9 to 10 years.
-
Commonly associated fractures include the olecranon, coronoid, and medial epicondyle.
-
Ossification of the proximal radial
epiphysis begins at 4 to 6 years of age as a small, flat nucleus. It
may be spheric or may present as a bipartite structure; these anatomic
variants may be appreciated by their smooth, rounded borders without
cortical discontinuity. -
Normal angulation of the radial head with
respect to the neck ranges between 0 and 15 degrees laterally, and from
10 degrees anterior to 5 degrees posterior angulation. -
Most of the radial neck is extracapsular;
therefore, fractures in this region may not result in a significant
effusion or a positive fat pad sign. -
No ligaments attach directly to the
radial head or neck; the radial collateral ligament attaches to the
orbicular ligament, which originates from the radial aspect of the ulna.
-
Acute:
-
Indirect: This is most common, usually
from a fall onto an outstretched hand with axial load transmission
through the proximal radius with trauma against the capitellum. -
Direct: This is uncommon because of the overlying soft tissue mass.
-
-
Chronic:
-
Repetitive stress injuries may occur,
most commonly from overhead throwing activities. Although most “Little
League elbow” injuries represent tension injuries to the medial
epicondyle, compressive injuries from valgus stress may result in an
osteochondrotic-type disorder of the radial head or an angular
deformity of the radial neck.
-
-
Patients typically present with lateral
swelling of the elbow, with pain exacerbated by range of motion,
especially supination and pronation. -
Crepitus may be elicited on supination and pronation.
-
In a young child, the primary complaint
may be wrist pain; pressure over the proximal radius may accentuate the
referred wrist pain.
 |
|
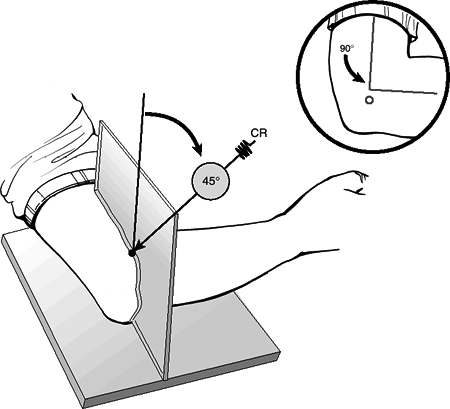
Figure
44.7. Radiocapitellar view. The center of the x-ray beam is directed at 45 degrees to separate the proximal radius and ulna on the x-ray. (From Long BW. Orthopaedic Radiography. Philadelphia: WB Saunders; 1995:152).
|
-
AP and lateral views of the elbow should be obtained. Oblique views may aid in further definition of the fracture line.
-
Special views
-
Perpendicular views: With an acutely
painful, flexed elbow, AP evaluation of the elbow may be obtained by
taking one radiograph perpendicular to the humeral shaft, and a second
view perpendicular to the proximal radius. -
Radiocapitellar (Greenspan) view: This
oblique lateral radiograph is obtained with the beam directed 45
degrees in a proximal direction, resulting in a projection of the
radial head anterior to the coronoid process of the anterior ulna (Fig. 44.7).
-
-
A positive supinator fat pad sign may be present, indicating injury to the proximal radius.
-
Comparison views of the contralateral elbow may help identify subtle abnormalities.
-
When a fracture is suspected through
nonossified regions of the radial head, an arthrogram may be performed
to determine displacement. -
MRI may be helpful in appreciating the direction of the fracture line and the pattern of fracture.
 |
|
Figure
44.8. Types of valgus injuries. Left: Type A: Salter-Harris type I or II physeal injury. Center: Type B: Salter-Harris type IV injury. Right: Type C: Total metaphyseal fracture pattern. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
This is based on the degree of angulation.
| Type I: | <30 degrees |
| Type II: | 30 to 60 degrees |
| Type III: | >60 degrees |
-
This is based on the mechanism of injury.
-
Valgus injuries are caused by a fall onto an outstretched hand (compression); angular deformity of the head is usually seen (Fig. 44.8).
Type A: Salter-Harris Type I or II physeal injury Type B: Salter-Harris Type III or IV intraarticular injury Type C: Fracture line completely within the metaphysis -
Fracture associated with elbow dislocation
-
Reduction injury
-
Dislocation injury
-
-
Simple immobilization is indicated for
O’Brien Type I fractures with <30-degree angulation. This can be
accomplished with the use of a collar and cuff, a posterior splint, or
a long arm cast for 7 to 10 days with early range of motion. -
Type II fractures with 30- to 60-degree angulation should be managed with manipulative closed reduction.
-
This may be accomplished by distal
traction with the elbow in extension and the forearm in supination;
varus stress is applied to overcome the ulnar deviation of the distal
fragment and open up the lateral aspect of the joint, allowing for
P.529
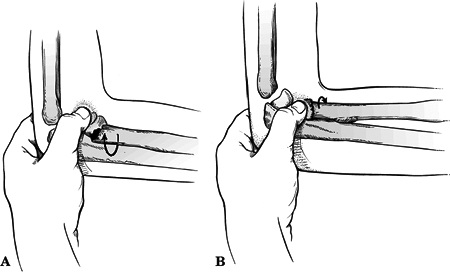
disengagement of the fragments for manipulation (Patterson) (Fig. 44.9).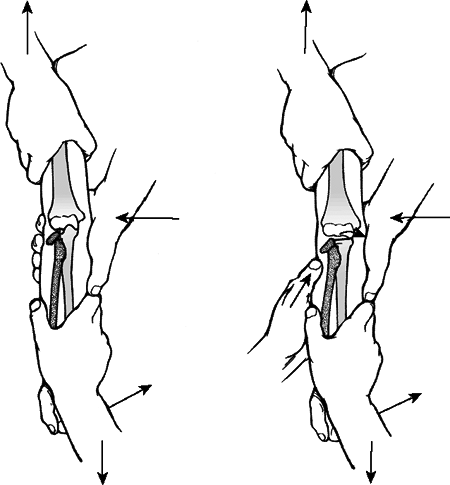 Figure
Figure
44.9. Patterson’s manipulative technique. Left: An assistant grabs the
patient’s arm proximally with one hand placed medially against the
distal humerus. The surgeon applies distal traction with the forearm
supinated and pulls the forearm into varus. Right: Digital pressure
applied directly over the tilted radial head completes the reduction.(Adapted from Patterson RF. Treatment of displaced transverse fractures of the neck of the radius in children. J Bone Joint Surg 1934;16:696×2013;698; in Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Israeli described a technique in which
the elbow is placed in flexion, and the surgeon’s thumb is used to
apply pressure over the radial head while the forearm is forced into a
pronated position (Fig. 44.10). -
Chambers reported another technique for
reduction in which an Esmarch wrap is applied distally to proximally,
and the radius is reduced by the circumferential pressure. -
Following reduction, the elbow should be
immobilized in a long arm cast in pronation with 90 degrees of flexion.
This should be maintained for 10 to 14 days, at which time
range-of-motion exercises should be initiated.
-
-
O’Brien Type II fractures (30- to
60-degree angulation) that are unstable following closed reduction may
require the use of percutaneous Kirschner wire fixation. This is best
accomplished
P.530
by
the use of a Steinmann pin placed in the fracture fragment under image
intensification for manipulation, followed by oblique Kirschner wire
fixation after reduction is achieved. The patient is then placed in a
long arm cast in pronation with 90-degree elbow flexion for 3 weeks, at
which time the pins and cast are discontinued and active range of
motion is initiated.![]() Figure
Figure
44.10. Flexion-pronation (Israeli) reduction technique. (A) With the
elbow in 90 degrees of flexion, the thumb stabilizes the displaced
radial head. Usually the distal radius is in a position of supination.
The forearm is pronated to swing the shaft up into alignment with the
neck (arrow). (B) Movement is continued to full pronation for reduction (arrow).(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Indications for open reduction and
internal fixation include fractures that are irreducible by closed
means, Type III fractures (>60-degree angulation), fractures with
>4 mm translation, and medial displacement fractures (these are
notoriously difficult to reduce by closed methods). Open reduction with
oblique Kirschner wire fixation is recommended; transcapitellar pins
are contraindicated because of a high rate of breakage, as well as
articular destruction from even slight postoperative motion. -
The results of open treatment are not
significantly different from those of closed treatment; therefore,
closed treatment should be performed when possible. -
Radial head excision gives poor results
in children owing to the high incidence of cubitus valgus and radial
deviation at the wrist due to the continued growth of the child.
-
Decreased range of motion occurs in (in
order of decreasing frequency) pronation, supination, extension,
flexion. The reason is loss of joint congruity and fibrous adhesions.
Additionally, enlargement of the radial head following fracture may
contribute to loss of motion. -
Radial head overgrowth: From 20% to 40%
of cases will experience posttraumatic overgrowth of the radial head,
owing to increased vascularity from the injury that stimulates
epiphyseal growth. -
Premature physeal closure: Rarely results in shortening >5 mm, although it may accentuate cubitus valgus.
-
Osteonecrosis of the radial head: Occurs
in 10% to 20%, related to amount of displacement; 70% of cases of
osteonecrosis are associated with open reduction. -
Neurologic: Usually posterior
interosseous nerve neurapraxia; during surgical exposure, pronating the
forearm causes the posterior interosseous nerve to move ulnarly, out of
the surgical field. -
Radioulnar synostosis: The most serious
complication, usually occurring following open reduction with extensive
dissection, but it has been reported with closed manipulations and is
associated with a delay in treatment of >5 days. It may require
exostectomy to improve function. -
Myositis ossificans: May complicate up to 32% of cases, mostly involving the supinator.
-
Referred to as “nursemaid’s elbow” or “pulled elbow.”
-
Male-to-female ratio is 1:2.
-
Occurs in the left elbow 70% of the time.
-
Occurs at ages 6 months to 6 years, with a peak at ages 2 to 3 years.
-
Recurrence rate is 5% to 30%.
-
Primary stability of the proximal
radioulnar joint is conferred by the annular ligament, which closely
apposes the radial head within the radial notch of the proximal ulna. -
The annular ligament becomes taut in supination of the forearm owing to the shape of the radial head.
-
The substance of the annular ligament is reinforced by the radial collateral ligament at the elbow joint.
-
After age 5 years, the distal attachment
of the annular ligament to the neck of the radius strengthens
significantly to prevent tearing or subsequent displacement.
-
Longitudinal traction force on extended
elbow is the cause, although it remains controversial whether the
lesion is produced in forearm supination or pronation (it is more
widely accepted that the forearm must be in pronation for the injury to
occur).
-
Patients typically present with an
appropriate history of sudden, longitudinal traction applied to the
extended upper extremity (such as a child “jerked” back from crossing
the street), often with an audible snap. The initial pain subsides
rapidly, and the patient allows the upper extremity to hang in the
dependent position with the forearm pronated and elbow slightly flexed
and refuses to use the ipsilateral hand (pseudoparalysis). -
A history of a longitudinal pull may be absent in 33% to 50% of cases.
-
Effusion is rare, although tenderness can usually be elicited over the anterior and lateral aspects of the elbow.
-
A neurovascular examination should be
performed, although the presence of neurovascular compromise should
alert the physician to consider other diagnostic possibilities because
neurovascular injury is not associated with simple radial head
subluxation.
-
Radiographs are not necessary if there is
a classic history, the child is 5 years old or younger, and the
clinical examination is strongly supportive. Otherwise, standard AP and
lateral views of the elbow should be obtained. -
Radiographic abnormalities are not
typically appreciated, although some authors have suggested that on the
AP radiograph >3 mm lateral displacement of the radial head with
respect to the capitellum is indicative of radial head subluxation.
However, disruption of the radiocapitellar axis is subtle and often
obscured by even slight rotation; therefore, even with a high index of
suspicion, appreciation of this sign is generally present in only 25%
of cases. -
Ultrasound is not routinely used in the
evaluation of radial head subluxation, but it may demonstrate an
increase in the echonegative area between the radial head and the
capitellum (radiocapitellar distance typically about 7.2 mm; a
difference of >3 mm between the normal and injured elbow suggests of
radial head subluxation).
-
A classification scheme for radial head subluxation does not exist.
-
It is important to rule out other
diagnostic possibilities, such as early septic arthritis or proximal
radius fracture, which may present in a similar fashion, especially if
a history of a longitudinal pull is absent.
-
Closed reduction
-
The forearm is supinated with thumb pressure on the radial head.
-
The elbow is then brought into maximum flexion with the forearm still in supination.
-
Hyperpronation may also be used to reduce the subluxation.
-
-
A palpable “click” may be felt on reduction.
-
The child typically experiences a brief
moment of pain with the reduction maneuver, followed by the absence of
pain and normal use of the upper extremity 5 to 10 minutes later. -
Postreduction films are generally
unnecessary. A child who remains irritable may require further workup
for other disorders or a repeat attempt at reduction. If the
subluxation injury occurred 12 to 24 hours before evaluation, reactive
synovitis may be present that may account for elbow tenderness and a
reluctance to move the joint. -
Sling immobilization is generally unnecessary if the child is able to use the upper extremity without complaint.
-
Chronically unreduced subluxation:
Unrecognized subluxation of the radial head generally reduces
spontaneously with relief of painful symptoms. In these cases, the
subluxation is realized retrospectively. -
Recurrence: Affects 5% to 39% of cases,
but generally ceases after 4 to 5 years when the annular ligament
strengthens, especially at its distal attachment to the radius. -
Irreducible subluxation: Rare owing to
interposition of the annular ligament. Open reduction may be necessary
with transection and repair of the annular ligament to obtain stable
reduction.
-
Represent 3% to 6% of all elbow injuries.
-
The peak age is 13 to 14 years, after physes are closed.
-
There is a high incidence of associated fractures: medial epicondyle, coronoid, and radial head and neck.
-
This is a “modified hinge” joint
(ginglymotrochoid) with a high degree of intrinsic stability owing to
joint congruity, opposing tension of triceps and flexors, and
ligamentous constraints. Of these, the anterior bundle of the medial
collateral ligament is the most important. -
Three separate articulations
-
Ulnohumeral (hinge)
-
Radiohumeral (rotation)
-
Proximal radioulnar (rotation)
-
-
Stability
-
AP: trochlea/olecranon fossa (extension); coronoid fossa, radiocapitellar joint, biceps/triceps/brachialis (flexion)
-
Valgus: Medial collateral ligament
complex (anterior bundle the primary stabilizer (flexion and
extension)) anterior capsule and radiocapitellar joint (extension) -
Varus: Ulnohumeral articulation, lateral ulnar collateral ligament (static); anconeus muscle (dynamic)
P.534 -
-
Range of motion is 0 to 150 degrees of flexion, 85 degrees of supination, and 80 degrees of pronation.
-
Functionally, range of motion requires 30 to 130 degrees of flexion, 50 degrees of supination, and 50 degrees of pronation.
-
Extension and pronation are the positions of relative instability.
-
Most commonly, the cause is a fall onto
an outstretched hand or elbow, resulting in a levering force to unlock
the olecranon from the trochlea combined with translation of the
articular surfaces to produce the dislocation. -
Posterior dislocation: This is a
combination of elbow hyperextension, valgus stress, arm abduction, and
forearm supination with resultant soft tissue injuries to the capsule,
collateral ligaments (especially medial), and musculature. -
Anterior dislocation: A direct force strikes the posterior aspect of the flexed elbow.
-
Patients typically present guarding the injured upper extremity with variable gross instability and massive swelling.
-
A careful neurovascular examination is
crucial and should be performed before radiographs or manipulation. At
significant risk of injury are the median, ulnar, radial, and anterior
interosseous nerves and the brachial artery. -
Serial neurovascular examinations should
be performed when massive antecubital swelling exists or the patient is
believed to be at risk for compartment syndrome. -
Following manipulation or reduction, repeat neurovascular examinations should be performed to monitor neurovascular status.
-
Angiography may be necessary to identify
vascular compromise. The radial pulse may be present with brachial
artery compromise as a result of collateral circulation.
-
Standard AP and lateral radiographs of the elbow should be obtained.
-
Radiographs should be scrutinized for
associated fractures about the elbow, most commonly disruption of the
apophysis of the medial epicondyle, or fractures involving the coronoid
process and radial neck.
-
Chronologic: Acute, chronic (unreduced), or recurrent.
-
Descriptive: Based on the relationship of the proximal radioulnar joint to the distal humerus.
-
Posterior
-
Posterolateral: >90% dislocations
-
Posteromedial
-
-
Anterior: Represents only 1% of pediatric elbow dislocations.
-
Divergent: This is rare.
-
Medial and lateral dislocations: These are not described in the pediatric population.
-
Fracture dislocation: Most associated
osseous injuries involve the coronoid process of the olecranon, the
radial neck, or the medial epicondylar apophysis of the distal humerus.
Rarely, shear fractures of the capitellum or trochlea may occur.
-
Acute posterior elbow dislocations should
be initially managed with closed reduction using sedation and
analgesia. Alternatively, general or regional anesthesia may be used. -
Young children (0 to 8 years old): With
the patient prone and the affected forearm hanging off the edge of the
table, anteriorly directed pressure is applied to the olecranon tip,
effecting reduction. -
Older children (>8 years old): With
the patient supine, reduction should be performed with the forearm
supinated and the elbow flexed while providing distal traction
(Parvin). Reduction with the elbow hyperextended is associated with
median nerve entrapment and increased soft tissue trauma. -
Neurovascular status should be reassessed, followed by evaluation of stable range of motion.
-
Postreduction radiographs are essential.
-
Postreduction management should consist
of a posterior splint at 90 degrees with loose circumferential wraps
and elevation. Attention should be paid to antecubital and forearm
swelling. -
Early, gentle, active range of motion 5
to 7 days after reduction is associated with better long-term results.
Forced, passive range of motion should be avoided because redislocation
may occur. Prolonged immobilization is associated with unsatisfactory
results and greater flexion contractures. -
A hinged elbow brace through a stable arc of motion may be indicated in cases of instability without associated fractures.
-
Full recovery of motion and strength requires 3 to 6 months.
-
Indicated for cases of soft tissue and/or bony entrapment in which closed reduction is not possible.
-
A large, displaced coronoid fragment
requires open reduction and internal fixation to prevent recurrent
instability. Medial epicondylar apophyseal disruptions with entrapped
fragments must be addressed. -
Lateral ligamentous reconstruction in cases of recurrent instability and dislocation is usually unnecessary.
-
An external fixator for grossly unstable
dislocations (with disruption of the medial collateral ligament) may be
required as a salvage procedure.
-
Acute anterior dislocation of the elbow may be managed initially with closed reduction using sedation and analgesia.
-
Initial distal traction is applied to the
flexed forearm to relax the forearm musculature, followed by dorsally
directed pressure on the volar forearm coupled with anteriorly directed
pressure on the distal humerus. -
Triceps function should be assessed
following reduction, because stripping of the triceps tendon from its
olecranon insertion may occur. -
Associated olecranon fractures usually require open reduction and internal fixation.
-
This is a rare injury, with two types:
-
Anterior-posterior type (ulna
posteriorly, radial head anteriorly): This is more common; reduction is
achieved in the same manner as for a posterior dislocation concomitant
with posteriorly directed pressure over the anterior radial head
prominence. -
Mediolateral (transverse) type (distal
humerus wedged between radius laterally and ulna medially): This is
extremely rare; reduction is by direct distal traction on extended
elbow with pressure on the proximal radius and ulna, converging them.
-
-
Loss of motion (extension): This is
associated with prolonged immobilization with initially unstable
injuries. Some authors recommend posterior splint immobilization for 3
to 4 weeks, although recent trends have been to begin early (1 week),
supervised range of motion. Patients typically experience a loss of the
terminal 10 to 15 degrees of extension, which is usually not
functionally significant. -
Neurologic compromise: Neurologic
deficits occur in 10% of cases. Most complications occur with
entrapment of the median nerve. Ulnar nerve injuries are most commonly
associated with disruptions of the medial epicondylar apophysis. Radial
nerve injuries occur rarely.-
Spontaneous recovery is usually expected;
a decline in nerve function (especially after manipulation) or severe
pain in nerve distribution is an indication for exploration and
decompression. -
Exploration is recommended if no recovery is seen after 3 months following electromyography and serial clinical examinations.
-
-
Vascular injury (rare): The brachial artery is most commonly disrupted during injury.
-
Prompt recognition of vascular injury is essential, with closed reduction to reestablish perfusion.
-
If, after reduction, perfusion is not
reestablished, angiography is indicated to identify the lesion, with
arterial reconstruction with reverse saphenous vein graft when
indicated.
-
-
Compartment syndrome (Volkmann
contracture): May result from massive swelling from soft tissue injury.
Postreduction care must include aggressive elevation and avoidance of
hyperflexion of the elbow. Serial neurovascular examinations and
P.537
compartment pressure monitoring may be necessary, with forearm fasciotomy when indicated. -
Instability/redislocation: Rare (<1%)
after isolated, traumatic posterior elbow dislocation; the incidence is
increased in the presence of associated coronoid process and radial
head fracture (combined with elbow dislocation, this completes the terrible triad of the elbow).
It may necessitate hinged external fixation, capsuloligamentous
reconstruction, internal fixation, or prosthetic replacement of the
radial head. -
Heterotopic bone/myositis ossificans:
This occurs in 3% of pure dislocations, 18% when associated with
fractures, most commonly caused by vigorous attempts at reduction.-
Anteriorly, it forms between the
brachialis muscle and the capsule; posteriorly, it may form medially or
laterally between the triceps and the capsule. -
The risk is increased with a greater degree of soft tissue trauma or the presence of associated fractures.
-
It may result in significant loss of function.
-
Forcible manipulation or passive stretching increases soft tissue trauma and should be avoided.
-
Indomethacin or local radiation therapy
is recommended for prophylaxis postoperatively and in the presence of
significant soft tissue injury and/or associated fractures. Radiation
therapy is contraindicated in the presence of open physes.
-
-
Osteochondral fractures: Anterior shear
fractures of the capitellum or trochlea may occur with anterior
dislocations of the elbow. The presence of an unrecognized
osteochondral fragment in the joint may be the cause of an
unsatisfactory result of what initially appeared to be an uncomplicated
elbow dislocation. -
Radioulnar synostosis: The incidence is increased with an associated radial neck fracture.
-
Cubitus recurvatum: With significant
disruption of the anterior capsule, hyperextension of the elbow may
occur late, although this is rarely of any functional or symptomatic
significance.
-
These account for 5% of all elbow fractures.
-
The peak age is 5 to 10 years.
-
Twenty percent have an associated fracture or dislocation; the proximal radius is the most common.
-
The olecranon is metaphyseal and has a relatively thin cortex, which may predispose the area to greenstick-type fractures.
-
The periosteum is thick, which may prevent the degree of separation seen in adult olecranon fractures.
-
The larger amount of epiphyseal cartilage may also serve as a cushion to lessen the effects of a direct blow.
-
Extension injuries: With the arm
extended, the olecranon becomes locked in the olecranon fossa; if a
varus or valgus force is then applied, stress is concentrated in the
distal aspect of the olecranon; resultant fractures are typically
greenstick fractures that remain extraarticular and may extend proximal
to the coronoid process. -
Shear injuries: A direct force is applied
to the posterior olecranon, resulting in tension failure of the
anterior cortex; the distal fragment is displaced anteriorly by the
pull of the brachialis and biceps; this is differentiated from the
flexion-type injury by an intact posterior periosteum.
-
Soft tissue swelling is typically present over the olecranon.
-
An abrasion or contusion directly over the olecranon may indicate a flexion-type injury.
-
The patient may lack active extension,
although this is frequently difficult to evaluate in an anxious child
with a swollen elbow.
-
Standard AP and lateral x-rays of the elbow should be obtained.
-
Fracture lines associated with a flexion
injury are perpendicular to the long axis of the olecranon; these
differentiate the fracture from the residual physeal line, which is
oblique and directed proximal and anterior. -
The longitudinal fracture lines associated with extension injuries may be difficult to appreciate.
-
The radiographs should be scrutinized to detect associated fractures, especially proximal radius fractures.
-
Group A: Flexion injuries
-
Group B: Extension injuries
-
Valgus pattern
-
Varus pattern
-
-
Group C: Shear injuries
-
Nondisplaced flexion injuries are treated
with splint immobilization in 5 to 10 degrees of flexion for 3 weeks;
radiographs should be checked in 5 to 7 days to evaluate for early
displacement. -
Extension injuries generally need
correction of the varus or valgus deformity; this may be accomplished
by locking the olecranon in the olecranon fossa with extension and
applying a varus or valgus force to reverse the deformity;
overcorrection may help to prevent recurrence of the deformity. -
Shear injuries can be treated with immobilization in a hyperflexed position if the posterior periosteum remains intact,
P.539
with the posterior periosteum functioning as a tension band; operative
intervention should be considered if excessive swelling is present that
may result in neurovascular compromise in a hyperflexed position.
-
Displaced or comminuted fractures may require surgical stabilization.
-
Determining whether the posterior
periosteum is intact is key to determining the stability of a fracture;
if a palpable defect is present, or if the fragments separate with
flexion of the elbow, internal fixation may be needed. -
Fixation may be achieved with Kirschner
wires and a tension band, tension band alone, cancellous screws alone,
or cancellous screws and tension band. -
Removal of hardware is frequently
required and should be considered when deciding on a fixation technique
(i.e., tension band with wire versus tension band with suture). -
Postoperatively, the elbow is immobilized
in a cast at 70 to 80 degrees of flexion for 3 weeks, after which
active motion is initiated.
-
Delayed union: Rare (<1%) and is usually asymptomatic, even if it progresses to a nonunion.
-
Nerve injury: Rare at the time of injury;
ulnar neurapraxia has been reported after development of a
pseudarthrosis of the olecranon when inadequate fixation was used. -
Elongation: Elongation of the tip of the
olecranon may occur after fracture; the apophysis may elongate to the
point that it limits elbow extension. -
Loss of reduction: Associated with
fractures treated nonoperatively that subsequently displace; it may
result in significant loss of elbow function if it is not identified
early in the course of treatment.