Periprosthetic Fractures
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > I – General Considerations > 6 – Periprosthetic Fractures
6
Periprosthetic Fractures
TOTAL HIP ARTHROPLASTY
Femoral Shaft Fractures
Epidemiology
-
Intraoperative: There is a 0.8% to 2.3% incidence overall, including cemented and uncemented components.
-
Postoperative: There is a 0.1% incidence.
-
They occur more frequently with
noncemented components, with an incidence of 2.6% to 4% to as high as
17.6% for noncemented revisions.
Risk Factors
-
Osteopenia: Osteoporosis or bone loss secondary to osteolysis.
-
Stress risers secondary to cortical defects.
-
Revision surgery.
-
Inadequate implant site preparation: Large implant with inadequate reaming or broaching may be responsible.
-
Pericapsular pathology: A scarred capsule with inadequate release may result in intraoperative fracture.
-
Loose components: Loose femoral components are responsible for up to 33% of periprosthetic femur fractures.
Surgical Considerations (to Avoid Periprosthetic Fracture during Revision Surgery)
-
Use longer-stem prosthesis, spanning twice the bone diameter beyond the defect.
-
Consider bone grafting the defect.
-
Place cortical windows in an anterolateral location on the femur in line with the neutral bending axis.
-
Leave cortical windows <30% of the bone diameter.
-
Choose the correct starting point for reaming and broaching.
Classification
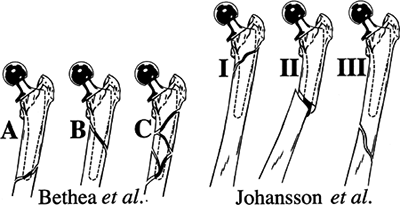
JOHANSSON (FIG. 6.1)
| Type I: | Fracture proximal to the prosthetic tip with the stem remaining in the medullary canal |
| Type II: | Fracture extending beyond the distal stem with dislodgement of the stem from the distal canal |
| Type III: | Fracture entirely distal to the tip of the prosthesis |
COOKE AND NEWMAN (MODIFICATION OF BETHEA)
| Type I: | Explosion type with comminution around the stem; prosthesis always loose and fracture inherently unstable |
| Type II: | Oblique fracture around the stem; fracture pattern stable, but prosthetic loosening usually present |
| Type III: | Transverse fracture at the distal tip of the stem; fracture unstable, but prosthetic fixation usually unaffected |
| Type IV: | Fracture entirely distal to the prosthesis; fracture unstable, but prosthetic fixation usually unaffected |
 |
|
Figure 6.1. Classification scheme proposed by Johansson.
|
P.42
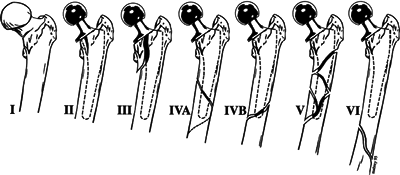
AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS CLASSIFICATION
This divides the femur into three separate regions:
| Level I: | Proximal femur distally to the lower extent of the lesser trochanter |
| Level II: | 10 cm of the femur distal to level I |
| Level III: | Covers remainder of femur distal to level II |
| Type I: | Fracture proximal to the intertrochanteric line that usually occurs during dislocation of the hip |
| Type II: | Vertical or spiral split that does not extend past the lower extent of the lesser trochanter |
| Type III: | Vertical or spiral split that extends past the lower extent of the lesser trochanter but not beyond level II, usually at the junction of the middle and distal thirds of the femoral stem |
| Type IV: | Fractures that traverse or lie within the area of the femoral stem in level III, with type IVA being a spiral fracture around the tip and type IVB being a simple transverse or short oblique fracture |
| Type V: | Severely comminuted fractures around the stem in level III |
| Type VI: | Fractures distal to the stem tip, also in level III |
 |
|
Figure 6.2. American Academy of Orthopaedic Surgeons classification of fractures associated with hip arthroplasty.
(Modified from Petty W, ed. Total Joint Replacement. Philadelphia: WB Saunders, 1991:291–314.)
|
P.43
VANCOUVER CLASSIFICATION
| Type A: | Fracture in the trochanteric region |
| AG: | Greater trochanter region |
| AL: | Lesser trochanteric region |
| Type B: | Around or just distal to the stem |
| B1: | Stable prosthesis |
| B2: | Unstable prosthesis |
| B3: | Unstable prosthesis plus inadequate bone stock |
| Type C: | Well below the stem |
 |
|
Figure 6.3. Vancouver classification scheme for periprosthetic fractures about total hip arthroplasties.
(Modified from Duncan CP, Masri BA. Fractures of the femur after hip replacement. In: Jackson D, ed. Instructional Course Lectures 44. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1995:293–304.)
|
Treatment Principles
-
Treatment depends on
-
Location of the fracture.
-
Stability of the prosthesis.
-
A loose stem should be revised.
-
-
Bone stock.
-
Age and medical condition of the patient.
-
Accurate reduction and secure fixation.
-
-
Options include:
-
Nonoperative treatment: limited weight bearing, brace, cast, or traction.
-
Open reduction and internal fixation (ORIF) (with plate and screws or cable and/or strut allograft).
-
Revision plus ORIF.
-
P.44
VANCOUVER TYPE A FRACTURES
-
These are usually stable and minimally displaced.
-
ORIF is used to maintain abductor function with wide displacement.
-
Revision of acetabular component is indicated with severe polyethylene wear.
VANCOUVER TYPE B1 FRACTURES
-
These are usually treated with internal fixation.
-
Options for fixation include:
-
Wires or cables.
-
Plate and screws and/or cables.
-
Cortical onlay allograft.
-
Combination.
-
-
Long-term results depend on:
-
Implant alignment.
-
Preservation of the periosteal blood supply.
-
Adequacy of stress riser augmentation.
-
-
Routine bone graft is used with ORIF.
VANCOUVER TYPE B2 FRACTURES
-
Revision arthroplasty and ORIF are used.
-
Choice of implant includes:
-
Uncemented prosthesis:
-
Extensive coated long-stem curved prosthesis.
-
Fluted long-stem prosthesis.
-
-
Cemented prosthesis.
-
VANCOUVER TYPE B3 FRACTURES
-
No sufficient bone stock supports the revision prosthesis.
-
Options include:
-
Proximal femoral reconstruction.
-
Composite allograft.
-
-
Proximal femoral replacement.
-
-
Treatment depends on:
-
The age of the patient.
-
The severity of the bone defect.
-
The functional class of the patient.
-
VANCOUVER TYPE C FRACTURES
-
Treat independently of the arthroplasty.
-
Use a plate and screws and/or cables with or without a strut allograft.
-
Do not make any new stress riser.
Acetabular Fractures
-
Nondisplaced fractures should be observed
and treated with crutches and limited weight bearing. There is a high
incidence of late loosening of the acetabular component, requiring
revision. -
Displaced fractures should be treated by ORIF, and the component should be revised.
P.45
TOTAL KNEE ARTHROPLASTY
Supracondylar Femur Fractures
Epidemiology
-
The postoperative incidence is 0.6% to 2.5%.
-
They generally occur within 10 years after surgery, usually secondary to relatively minor trauma.
-
Fracture of the patella after total knee arthroplasty may occur, with a prevalence of 0.1% to 8.5%.
Risk Factors
Supracondylar fractures after total knee replacement are multifactorial in origin, and risk factors include:
-
Osteoporosis.
-
Preexisting neurologic disease.
-
Notching of the anterior cortex:
-
Biomechanical analysis: 3 mm of anterior notching reduces torsional strength by 29%.
-
There is a high correlation between
notching and supracondylar fractures in patients with rheumatoid
arthritis and significant osteopenia. -
In the absence of significant osteopenia, there is no correlation between notching and supracondylar fractures.
-
Classification
NEER, WITH MODIFICATION BY MERKEL
| Type I: | Minimally displaced supracondylar fracture |
| Type II: | Displaced supracondylar fracture |
| Type III: | Comminuted supracondylar fracture |
| Type IV: | Fracture at the tip of the prosthetic femoral stem of fracture of the diaphysis above the prosthesis |
| Type V: | Any fracture of the tibia |
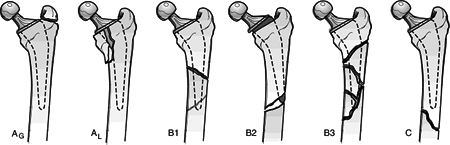
PERIPROSTHETIC FEMUR FRACTURES ABOUT TOTAL KNEES (LEWIS AND RORABECK)
This classification takes into account both fracture displacement and prosthesis stability (Fig. 6.4).
| Type I: | The fracture is nondisplaced, and the bone-prosthesis interface remains intact. |
| Type II: | The interface remains intact, but the fracture is displaced. |
| Type III: | The patient has a loose or failing prosthesis in the presence of either a displaced or a nondisplaced fracture. |
Treatment
PRINCIPLES
-
Anatomic and mechanical alignment are critical.
-
Nondisplaced fractures may be treated nonoperatively.
-
ORIF is indicated if the alignment is unacceptable by closed means and if bone stock is adequate for fixational devices.
-
If bone quality is poor, the fracture
should be treated nonoperatively, despite poor alignment, with clinical
and radiographic reevaluation after healing. -
Immediate prosthetic revision is indicated in selected cases.
P.46
NONOPERATIVE TREATMENT
 |
|
Figure 6.4. Classification scheme for periprosthetic fracture of the knee.
(Modified from Lewis PL, Rorabeck CH. Periprosthetic fractures. In: Engh GA, Rorabeck CH, eds. Revision Total Knee Arthroplasty. Baltimore: Williams & Wilkins, 1997:275–295.)
|
-
Long leg casting or cast bracing for 4 to 8 weeks may be used to treat minimally displaced fractures.
OPERATIVE TREATMENT
-
Displaced periprosthetic fractures around
a total knee replacement are almost always managed with ORIF because of
the difficulties in maintaining acceptable alignment after displacement.-
A blade plate, dynamic condylar screw,
dynamic compression plate, condylar buttress plate, locked plate, or
retrograde intramedullary nailing may be used for operative
stabilization. -
Primary revision with a stemmed component may be considered if there is involvement of the bone-implant interface.
-
Bone loss may be addressed with autologous grafting.
-
Cases of severe bone loss, especially in
the metaphyseal region, may be addressed with distal femoral
replacement with a specialized prosthesis designed for oncology
management.
-
-
Fractures around the diaphysis or the tip
of a femoral component may be treated with cortical strut grafts and
cerclage wiring, dynamic compression plate, locked plate, or a
combination of techniques. -
Acceptable alignment guidelines
-
Angulation <5 to 10° in either plane
-
<5 mm translation
-
<10-degree rotation
-
<1 cm shortening
-
Tibial Fractures
Risk Factors
-
Significant trauma (shaft fractures)
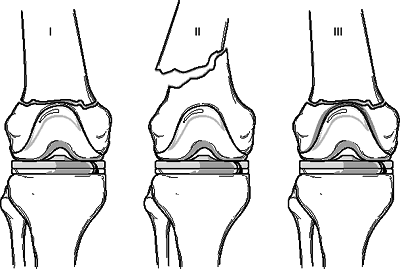
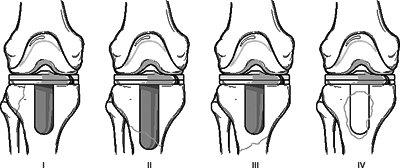 Figure 6.5. Classification of periprosthetic tibial fractures.(Modified from Felix NA, Stuart MJ, Hansen AD. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop 1997;345:113–124.)
Figure 6.5. Classification of periprosthetic tibial fractures.(Modified from Felix NA, Stuart MJ, Hansen AD. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop 1997;345:113–124.) -
Tibial component malalignment associated with increased medial plateau stress fractures
-
Revision surgery with press-fit stems
P.47
Classification
PERIPROSTHETIC TIBIAL FRACTURES (FELIX et al)
-
Classification is based on three factors:
location of the fracture, stability of the implant, and whether the
fracture occurred intraoperatively or postoperatively (Fig. 6.5).Type I: Occur in the tibial plateau Type II: Adjacent to the stem Type III: Distal to the prosthesis Type IV: Involve the tubercle -
The stability of the implant is then used to classify the fractures further:
-
Subtype A is a well-fixed implant.
-
Subtype B is loose.
-
Subtype C fractures are intraoperative.
-
Treatment
NONOPERATIVE TREATMENT
-
Closed reduction and cast immobilization may be performed for most tibial shaft fractures after alignment is restored.
-
Early conversion to a cast brace to preserve knee range of motion is advised.
OPERATIVE TREATMENT
-
Periprosthetic tibial fractures not
involving the plateau require ORIF if closed reduction and cast
immobilization are unsuccessful. -
Type I fractures involving the tibial
plateau typically involve the bone-implant interface, necessitating
revision of the tibial component.
P.48
Patella Fractures
Epidemiology
-
The postoperative incidence is 0.3% to 5.4% (reported as high as 21%).
Risk Factors
-
Large, central peg component
-
Excessive resection of the patella during prosthetic implantation
-
Lateral release, with devascularization of the patella
-
Malalignment
-
Thermal necrosis (secondary to methylmethacrylate)
Classification
GOLDBERG
| Type I: | Fractures not involving cement/implant composite or quadriceps mechanism |
| Type II: | Fractures involving cement/implant composite and/or quadriceps mechanism |
| Type IIIA: | Inferior pole fractures with patellar ligament disruption |
| Type IIIB: | Inferior pole fractures without patellar ligament disruption |
| Type IV: | Fracture-dislocations |
Treatment
NONOPERATIVE TREATMENT
-
Fractures without component loosening,
extensor mechanism rupture, or malalignment of the implant (type I or
IIIB) may be treated nonoperatively. -
The patient may be placed in a knee immobilizer for 4 to 6 weeks, with partial weight bearing on crutches.
OPERATIVE TREATMENT
-
Indicated for patients with disruption of the extensor mechanism, patellar dislocation, or prosthetic loosening.
-
Treatment options include:
-
ORIF with revision of the prosthetic patella. This is indicated for type II, IIIA, and IV fractures.
-
Fragment excision: This may be undertaken for small fragments that do not compromise implant stability or patellar tracking.
-
Patellectomy: This may be necessary in cases of extensive comminution or devascularization with osteonecrosis.
-
Surgical considerations include adequate
medial arthrotomy, adequate lateral release, preservation of the
superior lateral geniculate artery, and preservation of the patellar
fat pad.
-
TOTAL SHOULDER ARTHROPLASTY
Epidemiology
-
Periprosthetic fractures of the shoulder complicate approximately 2% of cases.
P.49
Risk Factors
 |
|
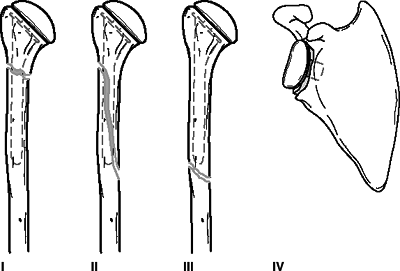
Figure
6.6. Classification of periprosthetic shoulder fractures. Type I: fractures occurring proximal to the tip of the prosthesis. Type II: fractures occurring in the proximal portion of the humerus with distal extension beyond the tip of the prosthesis. Type III: fractures occurring entirely distal to the tip of the prosthesis. Type IV: fractures occurring adjacent to the glenoid prosthesis. (From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002:587.)
|
-
Excessive reaming of the proximal humerus
-
Overimpaction of the humeral component
-
Excessive torque placed on the humerus during implant insertion
Classification
University of Texas San Antonio Classification of Periprosthetic Shoulder Fractures (Fig. 6.6)
| Type I: | Fractures occurring proximal to the tip of the humeral prosthesis |
| Type II: | Fractures occurring in the proximal portion of the humerus with distal extension beyond the tip of the humeral prosthesis |
| Type III: | Fractures occurring entirely distal to the tip of the humeral prosthesis |
| Type IV: | Fractures occurring adjacent to the glenoid prosthesis |
Treatment
-
Controversial: Some advocate nonoperative
treatment with surgical intervention indicated for compromise of
prosthetic fixation and intraoperative fractures. Others advocate
aggressive operative stabilization of all periprosthetic fractures of
the shoulder.
Nonoperative Treatment
-
Closed treatment involves fracture brace,
isometric exercises, and early range-of-motion exercises until
radiographic evidence of healing.
P.50
Operative Treatment
-
Primary goals include fracture union, prosthesis stability, and maintenance of motion.
-
ORIF may be performed with cerclage wiring and possible bone grafting.
-
Revision to a long-stem prosthesis may be required for cases with gross implant loosening.
-
Options for postoperative immobilization
range from sling immobilization for comfort until range-of-motion
exercises can be instituted, to shoulder spica casting for 6 weeks in
cases of tenuous fixation.
TOTAL ELBOW ARTHROPLASTY
Epidemiology
-
The overall prevalence of periprosthetic fractures of the elbow is approximately 8%.
-
Most fractures are preceded by prosthetic
loosening and thinning of the cortices. These occur more commonly in
the humerus than in the ulna.
Risk Factors
-
Osteoporosis
-
Paucity of bone between the medial and lateral columns of the distal humerus
-
Abnormal humeral bowing in the sagittal plane
-
Size and angulation of the humeral and ulnar medullary canals
-
Excessive reaming to accommodate the prostheses
-
Revision elbow surgery
Classification (Fig. 6.7)
| Type I: | Fracture of the humerus proximal to the humeral component |
| Type II: | Fracture of the humerus or ulna in any location along the length of the prosthesis |
| Type III: | Fracture of the ulna distal to the ulnar component |
| Type IV: | Fracture of the implant |
Treatment
Nonoperative Treatment
-
Nondisplaced periprosthetic fractures
that do not compromise implant stability may be initially addressed
with splinting at 90 degrees and early isometric exercises. -
The splint may then be changed to a fracture brace for 3 to 6 weeks.
Operative Treatment
-
Displaced type I or type II fractures may
be managed with ORIF with cerclage wire fixation, or with plates and
screws. Alternatively, revision to a long-stem humeral component may be
performed, with the component extending at least two diameters proximal
to the tip of the implant. Supplemental bone grafting may be used as
necessary. -
Type III fractures are usually amenable to cerclage wiring.
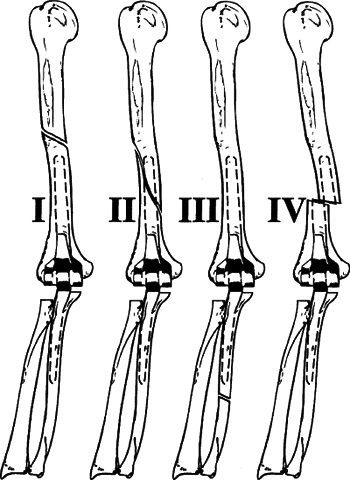 Figure
Figure
6.7. Classification of periprosthetic elbow fractures. Type I:
fractures of the humerus proximal to the humeral component. Type II:
fractures of the humerus or ulna in any location along the length of
the prosthesis (including those fractures that extend proximal and
distal to the humeral and ulnar components, respectively). Type III:
fracture of the ulna distal of the ulnar component. Type IV: fracture
of the implant.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002:601.) -
If stable fixation of implant components cannot be obtained, consideration should be given to more constrained prostheses.
-
Type IV fractures require component revision.
-
Displaced olecranon fractures should be fixed with a tension band and cement.
P.51
