NEUROLOGIC CONDITIONS ABOUT THE SHOULDER
III – THE HAND > Conditions of Nerves > CHAPTER 59 – NEUROLOGIC
CONDITIONS ABOUT THE SHOULDER
Departments of Orthopaedic Surgery, and Hand and Upper Extremity
Service, University of California, Davis, School of Medicine,
Sacramento, California, 95817.
include pain, weakness, or both. Obtain a complete history and perform
a thorough physical examination; pay particular attention to testing
and grading each muscle about the shoulder girdle and examining for
specific local areas of tenderness. Then decide to what extent the pain
is related to organic pathology. This decision making takes into
consideration the patient’s credibility, whether worker’s compensation
is a factor, and whether litigation is pending.
to evaluating the source of low back pain. Most often, pathology
resides in the rotator cuff or with intraarticular problems; take care
not to fall into the trap of missing some of the less common diagnostic
entities. The shoulder often is implicated in pain arising from the
neck (1,8). This
chapter does not discuss the qualities of cervical radiculopathy and
arthritic changes about the neck, but I mention them here to remind you
not to have tunnel vision when evaluating the shoulder.
thoracic outlet syndrome, suprascapular nerve compression syndrome, and
quadrilateral space syndrome. See Chapter 61 for a complete discussion of thoracic outlet syndrome.
about the shoulder, due to palsies of the suprascapular, axillary, long
thoracic, and spinal accessory nerves, as well as palsy of the upper
brachial plexus. Vague shoulder pain and weakness of the involved
muscle groups are the main symptoms of isolated nerve injuries about
the shoulder (44).
and treatment of specific nerve entrapments or palsies about the
shoulder that result in pain, weakness, or both. Systemic conditions,
such as arthrogryposis, muscular dystrophies, polio, and stroke, will
not be discussed; instead, see the works of Saha (58) and Scholtstaedt et al. (60). Also see Chapter 67, Chapter 68, and Chapter 178.
to an isolated nerve insult, one must be aware of a syndrome comprising
pain and flaccid paralysis of the muscles about the shoulder girdle.
Parsonage and Turner first described it in 1948 (50), calling it neuralgic amyotrophy. The syndrome today is more often referred to by their names.
simple: Without any constitutional disturbance, pain starts suddenly
across the top of the shoulder blade and may radiate down the outer
side of the upper arm or into the neck. This pain lasts from a few
hours to a fortnight or more, and then a flaccid paralysis, of some of
the muscles of the shoulder girdle and often of the arm, develops, and
in some cases there is a patch of numbness over the outer side of the
upper arm. When the paralysis appears, the severe pain usually stops,
but a dull ache may persist considerably longer. This clinical picture
is subject to modifications. (50)
were able to identify a precipitating cause in 66 patients. Some of the
causes cited were infection, trauma, or previous vaccination. They
noted that local pain was almost always the presenting symptom,
generally a constant severe ache that lasted for a few hours to a week
or two and then stopped fairly suddenly as muscle paralysis appeared.
Involvement of the long thoracic nerve leading to paralysis of the
serratus anterior was the most common finding. The authors also
reported cases in which the suprascapular nerve, the axillary nerve,
and C-5 and C-6 nerve root were involved. The prognosis for recovery
was related to the amount of initial paralysis. Muscles not completely
paralyzed or those showing some return during the first few weeks
usually recovered completely in 6 months or less. With severe wasting
occurring early and rapidly, the prognosis for useful return of
function was poor. Recovery of voluntary power in completely paralyzed
muscles was found 9 to 12 months after the onset, and recovery
continued up to 2 years or longer. The only treatment recommended was
to move the shoulder joint through its full range of motion on a
regular basis to prevent stiffness.
understood today than it was by Parsonage and Turner in 1948. It is
important to keep this fact in mind when evaluating any nerve palsy
about the shoulder, because early surgical treatment is not indicated (17).
A history of severe pain preceding muscle paralysis or the close timing
of a vaccination forms the basis for this diagnosis. Other than
symptomatic therapy, no specific treatment is available.
suprascapular notch, resulting in little more than pain about the
medial aspect of the scapula. The pain is usually diffuse, deep aching
and may be localized to the posterior aspect of the shoulder. Adduction
of the forward-flexed arm across the body produces traction on the
nerve and may increase this pain (53). Deep
palpation over the suprascapular notch may show marked tenderness. With
further compression or traction on this nerve, atrophy and loss of
external rotator function will ensue (Fig. 59.1).
The external rotation deficit limits the patient’s ability to perform
activities with the arm in an overhead position. With prolonged
compression and loss of all external rotator function, posterior
shoulder instability may also result.
 |
|
Figure 59.1. A 27-year-old body-builder noticed asymmetry of his shoulder muscles. The arrow
points to atrophy of the infraspinatus muscle. Some decrease in supraspinatus muscle mass is evident but is masked by the well-developed trapezius muscle. Electrodiagnostic studies confirmed suprascapular nerve palsy. |
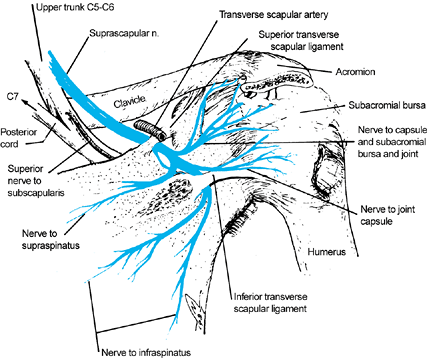
It courses laterally, deep to the trapezius and omohyoid muscles, and
enters the supraspinous fossa passing under the transverse
suprascapular ligament. The suprascapular artery and vein course with
the nerve, but they pass above the transverse suprascapular ligament.
The sensory component supplies the posterior capsule of the shoulder
joint and has no cutaneous distribution (57).
The suprascapular nerve courses deep to the supraspinatus muscle,
innervating this muscle with two branches. The nerve continues to the
lateral edge of the spine of the scapula, curving around it medially
into the infraspinous fossa, deep to the infraspinatus muscle. As the
nerve courses under the edge of the spine of the scapula, it commonly
passes through an inferior transverse scapula ligament (the
spinoglenoid ligament) that inserts at the lateral border of the
scapular spine and the scapular neck.
 |
|
Figure 59.2.
The course and distribution of the suprascapular nerve originating from the upper trunk, passing under the superior transverse scapular ligament and innervating the supraspinatus, then passing under the inferior transverse scapular ligament and innervating the infraspinatus. (From Narakas A. Compression Syndromes about the Shoulder Including Brachial Plexus. In: Szabo RM, ed. Nerve Compression Syndromes—Diagnosis and Treatment. Thorofare, NJ: Slack, 1989, with permission.) |
underneath the transverse suprascapular ligament; isolated atrophy and
weakness of the infraspinatus muscle, however, have been attributed to
compressions underneath the inferior transverse scapular ligament (63,65). Dermirhan et al. studied the anatomy and morphology
in cadavers to determine the role of entrapment in the suprascapular
nerve. They found the spinoglenoid ligament to be present in 60.8% of
shoulders, and that it was wider at the superior entrance of the tunnel
and fanned and twisted toward the inferior aspect (9).
In all their specimens, the fibers inserted into the posterior shoulder
capsule. During cross-body adduction and internal rotation of the
glenohumeral joint, the suprascapular nerve moved laterally and
stretched underneath the spinoglenoid ligament. In this position, the
interaction of the spinoglenoid ligament and the posterior capsule
resulted in stretching of the nerve (9).
compression of the suprascapular nerve. Diagnostic are denervation
potentials in the supraspinatus and infraspinatus muscles and prolonged
conduction time from Erb’s point to the supraspinatus and infraspinatus
muscles in the absence of involvement of other peripheral nerves (37).
Root compression at the C-5 level can mimic suprascapular nerve
entrapment syndrome; if C-5 root compression is the cause, however,
electrodiagnostic studies of the deltoid and rhomboids will demonstrate
abnormalities in these muscles. Magnetic resonance imaging is also
useful not only for the detection of ganglion cysts but also for
assessing the stage of paralysis (26).
Rengachary et al. studied the anatomy of the suprascapular notch in
cadavers and concluded that certain configurations might contribute to
nerve entrapment (56). Ticker et al. found the ligament to be partially ossified in 18% of cadavers (66).
It is debatable whether this entity is an actual nerve entrapment
syndrome or a situation in which the nerve is fixed at a given point
and the dysfunction is actually caused by traction.
and in 12 found isolated paralysis of the infraspinatus on the dominant
side (16). They attributed this denervation to
the athlete’s repeated stressing and stretching of the nerve when
serving (with the arm cocked) and following through. Sandow and Ilic
proposed that the infraspinatus branch of the suprascapular nerve can
be directly compressed between the lateral border of the scapular spine
and the medial margin of the rotator cuff during the extremes of
shoulder motion during sports such as volleyball and baseball; they
treat these athletes with a “notchplasty” in addition to release of
both the superior and inferior suprascapular ligaments (59).
suprascapular nerve for severe pain or atrophy. Martin et al., however,
reviewed their experience with nonsurgical treatment and concluded that
“in the absence of a well-defined lesion producing mechanical
compression of the suprascapular nerve, suprascapular neuropathy should
be treated non-operatively” (43). Twenty
percent of the patients in their study failed conservative treatment,
however, and no predictors were found that would indicate the need for
operative versus nonoperative care. For exposure of the nerve,
posterior, anterior, and superior approaches have all been described (45,48,53,64).
Most authors have abandoned the anterior approach because it is a more
difficult dissection and has a higher risk of complications.
-
Place the patient either prone or in the lateral decubitus position, with the involved side uppermost.
-
Make the skin incision parallel to and 1 inch superior to the scapular spine, along its entire length.
-
Elevate the trapezius muscle from the
spine and reflect it superiorly, exposing the supraspinatus muscle.
Palpate the suprascapular ligament overlying the suprascapular notch. -
Clean the suprascapular ligament with a
blunt elevator. Protect the suprascapular artery and vein, which are
superficial to the ligament. Protect the suprascapular nerve and
sharply excise (not just release) the transverse suprascapular ligament. -
Enlarge the suprascapular notch only if
you find that the nerve is not completely free of impingement or
traction. Inspect and palpate the surrounding region for any abnormal
masses. -
Reattach the trapezius muscle to the spine of the scapula using nonabsorbable sutures placed through drill holes in the bone.
-
Close the wound in routine fashion.
-
Following surgery, immobilize the patient
in a sling for 10 days. Then remove the sutures and initiate gradual
progressive range-of-motion and shoulder-strengthening exercises.
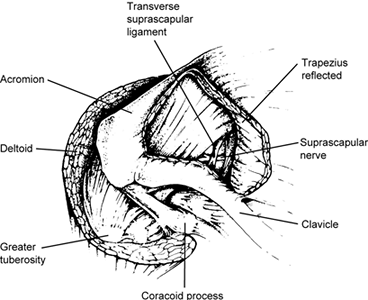
offers ease of access to the suprascapular ligament while avoiding
detachment of the trapezius muscle (Fig. 59.3) (45).
I prefer this approach, as long as access to the spinoglenoid ligament
is not required. It leaves a very cosmetically acceptable scar. This
approach is, however, too limited to excise ganglions that originate
from the glenohumeral joint. It may be combined with the posterior
approach if a more extensile exposure is needed.
 |
|
Figure 59.3.
Superior surgical approach to the transverse suprascapular ligament. The trapezius is reflected medially to expose the suprascapular ligament and nerve. (Illustration courtesy of J. Menon.) |
-
Place the patient in a semi-sitting beach chair or a lateral position held by a vacuum bean bag.
-
Start the incision over the distal third
of the clavicle, extending it over the acromioclavicular joint to the
lateral border of the spine of the scapula. -
Incise the subcutaneous tissue along the line of the incision.
-
Detach the trapezius muscle from the distal third of the clavicle and the acromion process and reflect it medially.
-
Palpate the superior border of the
scapula, directing a finger toward the coracoid process. Move the fat
pad underneath the trapezius to one side to expose the superior border
of the scapula. -
Pass a right-angle clamp beneath the ligament and through the foramen, and then transect the ligament.
-
Remove the ends of the ligament with a rongeur.
-
Reattach the trapezius muscle to the
lateral end of the acromion and the clavicle by passing sutures through
drill holes; then close the skin.
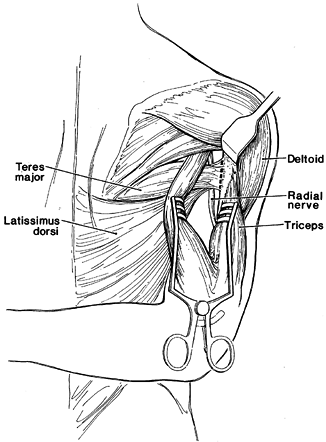
damage of the supraspinatus and infraspinatus muscles, consider
reconstructive substitution for the external rotators. The operation
that I have found works best is the one described by Zachary and Leeds (73) [a modification of L’Episcopo’s (34) procedure], which is a transfer of the teres major and the latissimus dorsi to the lateral aspect of the humerus (Fig. 59.4).
 |
|
Figure 59.4.
Posterior view right shoulder. Transplantation of the teres major and latissimus dorsi muscles for restoration of external rotation at the shoulder. Retraction of the deltoid muscle superiorly and separation of the long and lateral heads of the triceps muscle expose the insertion of the teres major and latissimus dorsi. The tendons of the teres major and latissimus dorsi are passed through slots in the lateral head of the triceps muscle and fixed to the posterolateral aspect of the humerus through drill holes in the bone. (Adapted from Zachary RB, Leeds MB. Transplantation of Teres Major and Latissimus Dorsi for Loss of External Rotation at the Shoulder. Lancet 1947;253:758, with permission.) |
-
Place the patient prone with the arm in full internal rotation.
-
Make a curvilinear incision over the posterior aspect of the upper third of the arm.
-
Expose the insertion of the teres major
and latissimus dorsi muscles by retracting the posterior border of the
deltoid muscle superiorly; separate the long and lateral heads of the
triceps muscle. -
Identify the radial nerve at the lower
border of the teres major muscle. Detach the teres major and latissimus
dorsi muscles together from their insertion on the humerus. -
Fully externally rotate the arm and pass
the tendinous insertions of the teres major and latissimus dorsi
muscles through a slit in the upper part of the lateral head of the
triceps. -
Attach the latissimus dorsi and teres
major muscles to the posterior lateral aspect of the humerus with
mattress sutures passed through drill holes in the bone. -
Close the wound, and use a shoulder abduction splint to immobilize the patient in 90° of forward flexion and external rotation.
-
Continue immobilization for 4 weeks, and then begin range-of-motion exercises.
is a terminal branch of the posterior cord. It lies on the
subscapularis muscle behind the axillary artery and dips posteriorly
just inferior to the glenohumeral joint before emerging in the
quadrilateral space (Fig. 59.5). It innervates
the teres minor and the deltoid muscles. The axillary nerve enters the
quadrilateral space together with the posterior humeral circumflex
artery.
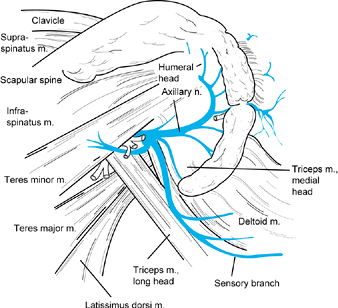 |
|
Figure 59.5.
Posterior view of the axillary nerve and posterior circumflex humeral vessels as they course through the quadrilateral space. (From Narakas A. Compression Syndromes about the Shoulder Including Brachial Plexus. In: Szabo RM, ed. Nerve Compression Syndromes—Diagnosis and Treatment. Thorofare, NJ: Slack, 1989, with permission.) |
subscapularis fascia, superiorly by the teres minor, inferiorly by the
teres major, laterally by the humerus and joint capsule, and medially
by the long head of the triceps (49). The
axillary nerve is tethered in this space by muscular fascia, joint
capsule, and periosteum. At the time of surgery, normally this space
will admit an index finger along the neurovascular pedicle; the arm is
in a relaxed position at the side. In abduction, this space is narrowed
by the scissorlike effect of the triceps and the teres major, and the
nerve is placed under tension by its distal site of innervation. Full
forward flexion of the arm puts the subscapularis, teres major, and
triceps muscles under tension, and it causes the humeral head to
impinge on the axillary nerve. Abduction and external rotation further
narrow the tunnel (49).
space syndrome) is a rare condition, and the diagnosis is often delayed
(7). One case caused by a ganglion has been reported (27).
Pain usually is described as being diffuse and anterior; extreme
movements of the shoulder involving abduction and external rotation,
however, exacerbate the symptoms. Typically, examination reveals
tenderness over the posterior aspect of the quadrilateral space. Rarely
is there any weakness of the deltoid or sensory deficit over the
distribution of the axillary nerve. Electromyographic examinations are
often normal and patients are often labeled neurotic.
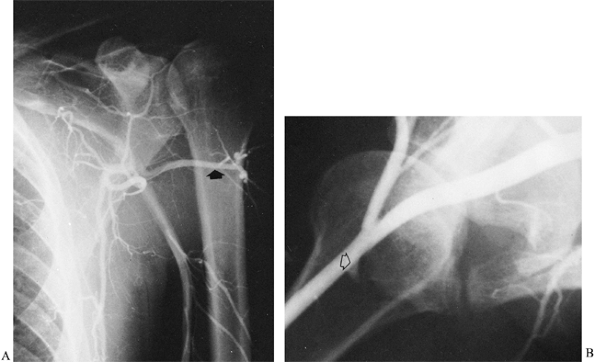
This invasive procedure should be performed to document this syndrome
only if surgery is contemplated. Perform a subclavian arteriogram by
using the Seldinger technique with the humerus at the side and in
abduction and external rotation (Fig. 59.6).
Follow the dye distally to visualize the posterior humeral circumflex
artery. In a positive arteriogram, the posterior humeral circumflex
artery is patent with the arm at the side and occludes with the arm in
external rotation and abduction. In normal extremities, the posterior
humeral artery does not occlude in this position.
 |
|
Figure 59.6. Subclavian arteriogram of a patient with quadrilateral space syndrome. A: With the arm at the side, the posterior humeral circumflex artery is patent (arrow). B: With the arm in abduction and external rotation, occlusion of the posterior humeral circumflex artery is seen near its origin (arrow).
|
unnecessary and make the diagnosis on the basis of tenderness over the
quadrilateral space, paresthesia over the lateral shoulder and upper
posterior arm, and deltoid weakness associated with decreased shoulder
abduction in the presence of a history of trauma (18).
In addition, I have found that a diagnostic nerve block is more
valuable in confirming the diagnosis than are any radiologic or
electrodiagnostic studies. I inject 10 ml of 1% plain lidocaine into
the quadrilateral space. If the injection produces numbness in the
distribution of the axillary nerve, and the shoulder pain resolves in
spite of provocative maneuvers, the diagnosis is more likely.
movements, administration of antiinflammatory medication, steroid
injections, and range-of-motion exercises. When this therapy has failed
and diagnosis is confirmed, surgical decompression is recommended.
-
Make a skin incision parallel to and one
fingerbreadth inferior to the scapular spine, and curve it along the
posterior border of the deltoid muscle (Fig. 59.7). Figure 59.7.
Figure 59.7.
Skin incision for decompression of the quadrilateral space. The
incision parallels and is just inferior to the spine of the scapula and
curves inferiorly over the posterior humerus. The x marks the location of the quadrilateral space. -
Dissect the fascia at the inferior border
of the deltoid muscle starting inferior and laterally and proceeding
superiorly and medially. Detach the deltoid muscle from the spine of
the scapula, leaving a musculotendinous border for reattachment (Fig. 59.8).![]() Figure 59.8.
Figure 59.8.
The deltoid muscle is dissected from the spine of the scapula and
reflected laterally. The axillary nerve exits the quadrilateral space
and is seen entering the deltoid (arrow). -
Elevate the teres minor muscle superiorly. Cahill (3,4) recommends detaching the teres minor muscle from the humerus at this point, but I have never found it necessary to do so.
-
Insert your index finger into the
quadrilateral space, directing it anteriorly, and palpate the posterior
humeral circumflex artery. -
Move the arm to extreme ranges of motion
and feel for any compressing structures. You may find a scarred
inferior glenohumeral ligament; tight teres minor, triceps, or teres
major tendons; or tight subscapularis fascia. I have been impressed by
the sharp scissorlike effect of the lateral head of the triceps tendon
on the axillary nerve and posterior humeral circumflex vessel;
therefore, I incise part of this tendinous insertion to create more
space in the tunnel. -
Reattach the deltoid muscle to the scapular spine with nonabsorbable sutures through drill holes in the bone.
-
Close the rest of the wound in the usual
fashion. After surgery, place the arm in a sling for 7 to 10 days, then
encourage gentle mobilization. -
Begin active deltoid muscle exercises at
6 weeks. Do not start resistive exercises requiring full abduction and
external rotation for 3 months.
-
Position the patient prone with the arm extended on an arm board.
-
With the patient standing before
induction of general anesthesia, determine the point of maximum
tenderness over the quadrilateral space. Make a vertical or an S-shaped
incision over this point. -
Raise skin flaps to expose the inferior border of the deltoid.
-
Incise the deltoid fascia along the
inferior border of the muscle and retract the deltoid superiorly to
expose the teres major and minor muscles. -
Dissect laterally and identify the tendon of the long head of the triceps.
-
Open the fascia between the teres muscle bellies and explore the quadrilateral space.
-
Identify the axillary nerve and the posterior circumflex humeral vascular bundle and tag them with rubber drains.
-
Sharply divide any fibrous bands to
decompress the space. (Although the authors do not mention this method,
I incise the part of the tendinous insertion of the lateral head of the
triceps if I find it compressing the axillary nerve and posterior
humeral circumflex vessel when the arm is placed in abduction and
external rotation.) -
Perform neurolysis if you find nerve fibrosis.
-
Close the wound in layers. No drain is usually necessary.
-
After surgery, place the arm in a sling
for 7 to 10 days, then encourage gentle mobilization and progress to
resistive exercises as tolerated.
joint makes it particularly susceptible to injury from trauma to the
shoulder joint. Coene and Narakas have reported that when diagnosed by
electromyography, the incidence of axillary nerve injury in
glenohumeral dislocations and humeral neck fractures is as high as 30% (6).
These lesions, which are often overlooked, frequently are neurapraxias
that resolve spontaneously. Persistent deltoid muscle palsy due to
lesions of the axillary nerve is rare, but when present it greatly
affects the function of the upper limb. Atrophy of the deltoid muscle
and loss of shoulder abduction strength are evident on examination.
Tinel’s sign may be positive in the infraclavicular region, but this
test is not reliable. Sensibility may be decreased over the lateral
aspect of the upper arm. Deltoid insufficiency may be masked by a
strong rotator cuff.
This test, which is based on the fact that no other muscle can
compensate for insufficiency of the posterior part of the deltoid, is
performed with the following steps (23):
-
Have the patient sit on an exam table, facing away from you.
-
Grasp both wrists and elevate the upper extremities into full passive shoulder extension.
-
Allow the shoulders to relax to submaximal extension to avoid elastic recoil in the shoulder.
-
Ask the patient to maintain this position as you let go.
-
The sign is positive when a lag or angular drop occurs when you let go. Changes may be subtle, with a lag drop as little as 5°.
reinnervation are absent by 6 months following injury, then surgical
exploration is indicated (6,52).
-
Place the patient in the lateral
position. Prepare and drape the shoulder widely to provide access both
anteriorly and posteriorly. -
Make a skin incision along the anterior
inferior border of the clavicle and extend it along the deltopectoral
groove. Open the deltopectoral interval while protecting the cephalic
vein. -
Detach the pectoralis minor muscle from
the coracoid process and expose the branches of the brachial plexus.
Leave a tendinous tag on the muscle for repair at closure. -
Isolate the posterior cord and identify the axillary nerve.
-
Abduct and externally rotate the arm, and
identify the inferior margin of the pectoralis major muscle insertion.
Totally or partially release the tendinous portion of the pectoralis
major muscle if necessary to better visualize the axillary nerve. -
The lesion usually cannot be addressed
with only an anterior approach. Therefore, at this point perform a
posterior approach, detaching the deltoid as previously described for
quadrilateral space syndrome. -
If a neuroma-in-continuity is found, resect the neuroma back to normal-appearing neural tissue.
-
Because repair of the nerve by direct
apposition is usually not technically possible, obtain a sural nerve
graft to bridge the gap. -
First, suture the sural nerve to the
distal stump of the axillary nerve, and pass the nerve graft through
the quadrilateral space and then suture to the proximal stump. -
Put the shoulder through a range of motion to demonstrate that there is no tension on the repair.
-
Reattach the pectoralis major (if detached), the pectoralis minor, and the deltoid muscles.
-
Close the subcutaneous tissues and skin in the usual fashion.
-
Postoperatively, immobilize the upper
extremity for 3–4 weeks in a shoulder immobilizer. Initiate physical
therapy as described for decompression of the quadrilateral space.
longstanding or with irreparable axillary nerve damage, consider a
tendon transfer. Deltoid muscle palsy is often associated with
paralyzed rotator cuff muscles, and shoulder arthrodesis becomes the
best option. If at least one of the rotator cuff muscles is active and
the usual prerequisites for tendon transfer are fulfilled (good passive
range of motion of the shoulder joint, normal articular surfaces, and a
strong muscle that is available for transfer), then consider restoring
deltoid function by tendon transfer. The trapezius transfer is most
commonly used (31). Recently, the latissimus
dorsi muscle, raised on its neurovascular pedicle and completely
rotated, has been used to replace the anterior part of the deltoid (28). Study the original description of the technique in detail if you plan to perform this operation (28).
iatrogenically during operations about the shoulder where it is either
detached from its origin or split. If the muscle is denervated, pain
and weakness result. The posterior deltoid muscle can be mobilized and
advanced to assume the function of the anterior portion (38).
to C-7. It passes posterior to the brachial plexus and lies on or
penetrates the anterior surfaces of the scalenus medius, then angulates
over the first or second ribs as it courses along the lateral thoracic
wall downward and branches to supply the digitations of the serratus
anterior muscle (30).
important to be aware that it courses obliquely in an anterosuperior to
posteroinferior direction as it progresses to the posterior angle of
the second rib (14). Traction on the nerve is
exerted when the shoulder is depressed or when the cervical spine is
bent in a contralateral direction. Kauppila’s autopsy study suggests
that the potential site for damage is anterior to the lower part of the
scapula, where the nerve may be exposed to both compression and
traction (32).
such as a direct blow to the shoulder or a sudden jerk of the arm
forward or backward (68). The nerve can be
injured between the coracoid process and the first or second ribs.
Injury to the nerve during surgery has been reported following axillary
approaches for thoracotomy, radical mastectomy, and axillary node
dissection (12,40,51). Repetitive trauma can also cause loss of serratus anterior
function, particularly in laborers who carry heavy objects on their
shoulders. Sustained compression has been described from the downward
strain on the shoulder produced by carrying heavy knapsacks. A sudden
forceful muscular exertion such as lifting a heavy box or pushing with
arms stretched overhead to support a ladder has also been reported as a
cause. The prognosis is favorable if the nerve injury is from chronic
minor trauma, but it seems to be less favorable if the nerve is injured
by a single major episode (67).
Gozna and Harris studied cadavers and showed that, when the underside
of the scapula was coated with graphite and depressed forcefully
downward against the thorax, a graphite imprint was found on the long
thoracic nerve at the level of the second rib (19).
They concluded that this is the site of the nerve injury. Successful
repair of this nerve is hampered by its surgically inaccessible
location. Generally, one should wait for 1 or 2 years before
considering operative treatment, as most patients improve slowly with
time (17,19).
avulsion of the serratus anterior muscle, which also causes winging of
the scapula (21); the latter injury is rare. Electromyography and radiographs are diagnostic.
scapular instability with attempts to elevate the shoulder. The scapula
pulls away from the chest wall as the extremity moves into forward
flexion or abduction. Normally, to elevate the shoulder fully, the
scapula must remain stable and close to the chest wall; at the same
time, the medial angle must depress and the inferior angle must rotate
laterally and upward. Patients who have serratus anterior muscle palsy
may be able to attain full shoulder motion in a supine position where
the weight of the body supports and stabilizes the scapula; when they
are standing upright, however, they cannot complete full shoulder
flexion and abduction.
Statically, it stabilizes the scapula to the thorax so that
scapulohumeral muscles can work against a fixed point to achieve arm
elevation; dynamically, it actively rotates the scapula anteriorly and
dorsally to contribute to full arm elevation.
serratus anterior muscle paralysis, the medial rim of the scapula
protrudes from the thoracic wall, and the inferior border of the
scapula “wings.” The winging of the scapula is more distinct if the
patient lifts his arm into forward flexion and uses it for some sort of
exertion, such as in doing a pushup against a wall (Fig. 59.9).
 |
|
Figure 59.9.
This patient demonstrates inferior scapula winging while doing a pushup against the wall. She has a longstanding serratus anterior palsy from a traction injury. |
valuable in determining whether the lesion is partial or complete and
whether regeneration is occurring after Wallerian degeneration. The
rest of the upper brachial plexus requires electrodiagnostic study to
confirm the diagnosis of isolated long thoracic nerve palsy.
remaining muscles around the shoulder girdle and avoiding activities
that cause winging of the scapula. All exercises to strengthen the
muscles should be performed with the scapula stabilized. Have the
patient lie supine or stand upright with her back placed firmly against
a wall. Patients can be taught to substitute movements to stabilize the
scapula using a combination of trapezius and rhomboid muscle function.
In addition, a custom-fabricated shoulder brace can be used to
stabilize the scapula. Although these jacket-braces are usually not
well tolerated, they are often appreciated by self-employed laborers
who are highly motivated to use them in order to keep working.
patient is sufficiently handicapped, consider surgical stabilization.
There are two general approaches to scapular stabilization: static and
dynamic. Static procedures have been described using various ligaments,
fascia, or even bony scapulopexy with fixation of the scapula to the
ribs (11,20,33).
Although these procedures improve the winging of the scapula and allow
the humeroscapular muscles to function against a fixed point during
movement of the shoulder joint, they hinder motion of the scapular
thoracic joint and make it impossible to obtain a full range of motion.
Therefore, I prefer dynamic muscle stabilization if at all possible.
muscle include the pectoralis major, pectoralis minor, and teres major
muscles (5,25,39,42,55,67,74). The rhomboids and latissimus dorsi muscles have also been used, but few authors advocate transferring them to remediate
serratus anterior muscle palsy (24).
Pectoralis major transfer is probably the most common procedure, but it
takes away a very strong axiohumeral muscle and thereby limits forward
flexion, adduction, and internal rotation—functions already compromised
by the absence of the serratus anterior muscle. Moreover, the
pectoralis major tendon is too short to be directly sutured to the
inferior tip of the scapula unless you use fascia to elongate it.
be directly attached to the tip of the scapula without the addition of
fascia. Another reason not to choose the pectoralis minor muscle is
that it serves as an antagonist to the serratus anterior muscle; it
pulls the coracoid process down and forward and thus causes backward
rotation of the scapula. The pectoralis minor muscle is active in
downward movement of the arm, whereas the serratus anterior muscle acts
in lifting the arm. Furthermore, the pectoralis minor muscle is
relatively weak.
-
Its strength is equal to that of the serratus anterior.
-
Its function as a depressor and internal rotator of the humerus is taken over by the latissimus dorsi.
-
Its use does not further weaken the axioscapular muscle group.
-
The course of its fibers corresponds to that of the serratus anterior muscle.
-
It does not need to be elongated with fascia.
-
The surgical scars are inconspicuous (67).
 |
|
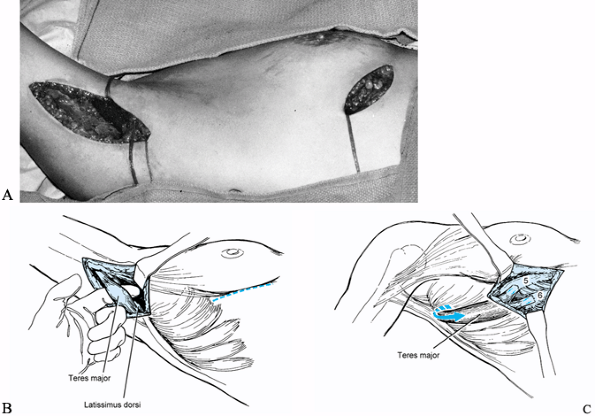
Figure 59.10. Surgical technique for teres major muscle transposition. A:
An incision is made in the axilla parallel to the posterior fold, and the insertion of the teres major tendon on the humerus is exposed. Then a curved incision is made in the inframammary crease. B: The teres major tendon is dissected off the humerus and fed subperiosteally from its humeral insertion and tagged with a suture. C: The teres major tendon is passed deep to the latissimus dorsi into the inframammary incision and attached subperiosteally to the fifth and sixth ribs (5,6). |
-
Place the patient in a lateral position.
-
Make a skin incision parallel to the
posterior axillary fold to expose the insertion of the teres major and
the latissimus dorsi muscle. The insertion of the teres major tendon is
more distal than that of the latissimus dorsi. -
Identify the teres major tendon and detach it from the humerus while carefully retracting the neurovascular bundle laterally.
-
Insert two heavy nonabsorbable sutures
into the teres major tendon and bluntly dissect its muscle from the
latissimus dorsi tendon. -
Make an incision, concave side up, below the breast in the inframammary fold.
-
Create a blunt tunnel from the posterior
to the anterior incision, using a finger to dissect deep to the
latissimus dorsi muscle. -
Pass the sutures and the teres major
tendon deep to the latissimus dorsi muscle into the anterior wound.
Make sure that fascia is not binding the muscle and that the muscle is
neither kinked nor twisted in the axillary wound. -
Expose the fifth and sixth ribs subperiosteally through the inframammary incision.
-
Divide the teres major tendon into two
slips and insert the superior slip into the fifth rib and the inferior
slip into the sixth rib through drill holes in the bone. Determine
tension by placing the arm in abduction and forward flexion with
external rotation. In this position, the transferred teres major tendon
should feel snug and draw the inferior pole of the scapula toward the
chest wall. Secure this insertion with further nonabsorbable sutures
into the periosteum and the teres major tendon. -
Close the wounds in routine fashion.
-
After surgery, place the patient in a
shoulder abduction splint, maintaining the arm in abduction, forward
flexion, and external rotation for 6 weeks. -
Encourage motion of the elbow, wrist, and digits during the period of shoulder immobilization.
-
After 6 weeks, initiate physical therapy
to regain full range of motion in the shoulder along with gradual
strengthening exercises.
dysfunction. The trapezius muscle is important in stabilizing the
scapula during forward elevation of the arm, and paralysis of it
results in drooping, lateral displacement, and winging of the scapula,
with weakness of forward elevation and abduction. Patients complain of
pain in the shoulder and axilla. Pain and weakness increase with
exertion of the arm. The pain may result from traction on the brachial
plexus, causing a radiculitis; it has even been demonstrated that
traction on the suprascapular nerve alone can be the cause of pain in
trapezius palsy (46). The pain also may result from a neuroma (see Chapter 53), which is demonstrated by eliciting Tinel’s sign in the posterior cervical triangle.
foramen and passes inferior to the surface of the sternocleidomastoid
muscle, which it innervates. As it passes underneath or penetrates the
deep head of that muscle, it reappears under its posterior edge between
the upper and middle thirds. It then enters the posterior cervical
triangle, where it lies superficially. The nerve passes beneath the
trapezius and forms a plexus with fibers from the third and fourth
cervical nerves while innervating the trapezius muscle (72).
To delineate the safe limits for muscle-splitting incisions of the
trapezius, Jobe et al. dissected the shoulders of 25 cadavers and found
that the spinal accessory nerve runs a vertical course medial and
parallel to the vertebral border of the scapula (29).
They also found that three to six nerve branches also run a vertical
course lying 33% to 50% of the distance from the tips of the vertebral
spinous processes to the lateral tip of the acromion.
They concluded that muscle-splitting incisions are relatively safe in the lateral half of the muscle (29).
floor of the posterior cervical triangle renders it vulnerable to
injury. Most commonly, the injury occurs during a surgical procedure
such as surgical lymph node biopsy or removal of a benign tumor (13,71).
It used to be that the nerve was frequently excised during radical neck
dissection for malignant tumor, but more recently it is being spared
when this operation is performed. The nerve may also be injured by
penetrating or blunt trauma to the neck; I explored and grafted one
patient’s nerve that had been divided from a bite in the neck during a
lovers’ quarrel. Spontaneous palsy of the accessory nerve has been
reported, but all known cases were due to heavy, repetitive work or
were related to a particular incident of strenuous activity (41).
percuss to elicit Tinel’s sign in the posterior cervical triangle. The
patient may be unable to abduct the shoulder above 80°, and shrugging
of the shoulder produces winging of the superior border of the scapula.
An abduction test has been devised to further demonstrate the flaring
of the vertebral border of the scapula: Hold the patient’s wrist firmly
at his side and ask him to attempt abduction against resistance. The
test is considered positive if there is flaring of the entire vertebral
border of the scapula (69).
palsy, help localize the lesion, and rule out other forms of
neuropathy. Initially and up to 1 year, perform exploration of the
nerve with neurolysis, repair, or grafting as necessary. After 1 year,
consider reconstructive substitutions for the trapezius.
surgery, however, I give the patient a trial of shoulder immobilization
to see if removing the pull of the weight of the extremity on the
brachial plexus will decrease the pain. If Tinel’s sign is positive in
the posterior cervical triangle, I usually inject 3 or 4 ml of 1%
lidocaine at the site of Tinel’s sign to see if this injection
eliminates the pain. If the pain is diminished by a trial unweighing of
the arm, I find that trapezius muscle substitution reconstruction will
be predictably successful.
dynamic scapular stabilizations. Static stabilization procedures using
fascia tend to stretch in time and are more often used in patients who
have neuromuscular disorders and widespread weakness (10,22). The procedure of choice is an operation first described by Eden (15) in 1924, and later by Lange (35) in 1951. The Eden-Lange procedure is a lateral transfer of the levator scapulae and rhomboid major and minor muscles (36).
The trapezius muscle has upper, middle, and lower components: The upper
portion rotates and elevates the scapula, the middle portion stabilizes
and adducts the scapula, and the lower portion downwardly rotates and
depresses the scapula. The lateral transfer of the levator scapulae and
rhomboid muscles allows them to approximate the function of the three
portions of the trapezius muscle by changing the direction of their
pull. The operation is well described by Bigliani et al., whose
technique follows (2).
-
Place the patient in a lateral decubitus position, and elevate the head of the table 15°.
-
Make an incision midway between the
spinous processes and the medial scapular border, parallel to and along
the length of the medial scapular border (Fig. 59.11). Figure 59.11. Incisions for the transfer of the rhomboids and levator scapulae in the treatment of trapezius paralysis.
Figure 59.11. Incisions for the transfer of the rhomboids and levator scapulae in the treatment of trapezius paralysis. -
Transect the trapezius muscle close to the scapula border.
-
Identify the levator scapulae and the rhomboid minor and major muscles, and carefully separate them from each other.
-
Use a narrow osteotome to detach the three muscles to be transferred from the medial border of the scapula (Fig. 59.12).
![]() Figure 59.12.
Figure 59.12.
The levator scapulae, rhomboid minor and rhomboid major tendon are
detached from their insertion on the medial border of the scapula and
then transferred laterally. -
Separate the three individual muscles and
dissect them proximally and medially, taking care to avoid injury to
the dorsal scapular nerve. Tag the ends of each muscle with
nonabsorbable sutures. -
Elevate the infraspinatus muscle from the inferior fossa of the scapula.
-
Place six drill holes in the scapula,
1.5–2 cm apart, starting 4–5 cm lateral to the medial border of the
scapula and 1 cm below its spine. -
Attach the rhomboid major and minor muscles to these drill holes with nonabsorbable heavy suture material.
-
Tie the sutures with the scapula in the
reduced position and the arm abducted 90°, and imbricate the
infraspinatus muscle over the repair. -
Make a 4 cm incision over the scapular spine, starting 3 cm medial to the acromion process and extending medially.
-
Dissect the trapezius, deltoid, and
supraspinatus muscles subperiosteally and drill three holes through the
spine of the scapula. Make a tunnel through the atrophied trapezius
muscle, connecting the medial and lateral wounds in the line of the
fibers of the upper trapezius. -
Pass the levator scapulae muscle through
the tunnel and secure it to the spine of the scapula using
nonabsorbable heavy suture material. -
Close the incisions in routine fashion and apply an abduction brace.
-
Keep the patient in an abduction brace for 6 weeks after surgery. Allow her to perform passive assistive exercises.
-
At 6 weeks, start her on a rehabilitation program to strengthen the shoulder.
a flail shoulder. In time, the weight of the shoulder will cause
inferior glenohumeral subluxation and pain. The pain may be secondary
to traction on the brachial plexus or joint incongruity. In general,
the treatment is reconstruction of the brachial plexus or a shoulder
arthrodesis (see Chapter 60 and Chapter 103).
flexion is also absent. While constructing elbow flexion with either
pectoralis major or latissimus dorsi tendon transfer, the shoulder may
be stabilized if the transfer is performed by rotating the muscle
completely on its neurovascular pedicle. Since the primary function of
these muscle transfers is elbow reconstruction, they will not be
described in this chapter (see Chapter 58 and Chapter 60).
scheme: *, classic article; #, review article; !, basic research
article; +, clinical results/outcome study
L, Narakas A. Surgical management of axillary nerve lesions, isolated
or combined with other infraclavicular nerve lesions. Periph Nerve Repair Regener 1986;3:47.
F, Harris M. Restoration of Function of the Shoulder following
Paralysis of the Trapezius by Fascial Sling Fixation and
Transplantation of the Levator Scapulae. Ann Surg 1950;132:1111.
M, Lotze M, Gerber L, Rosenbury S. Incidence, Recovery and Management
of Serratus Anterior Muscle Palsy after Axillary Node Dissection. Phys Ther 1983;63:1243.
L, Bechtol C. Paralysis of the Serratus Anterior Due to Electric Shock
Relieved by Transplantation of the Pectoralis Major Muscle: A Case
Report. J Bone Joint Surg Am 1963;45:156.
K, Muratso H, Kurosaka M, et al. Compression Neuropathy of the
Suprascapular Nerve as a Cause of Pain in Palsy of the Accessory Nerve:
A Case Report. J Bone Joint Surg Am 1990;72:938.
S, Burr D, Lucas S, et al. Suprascapular Entrapment Neuropathy: A
Clinical Anatomical and Comparative Study. Part 2: Anatomical Study. Neurosurgery 1979;5:447.
S, Nelt J, Singer P, Brackett C. Suprascapular Entrapment Neuropathy: A
Clinical Anatomical and Comparative Study. Part 1: Clincial Study. Neurosurgery 1979;5:441.
JB, Djurasovic M, Strauch RJ, et al. The Incidence of Ganglion Cysts
and Other Variations in Anatomy along the Course of the Suprascapular
Nerve. J Shoulder Elbow Surg 1998;7:472.