MEDIAN NERVE PALSY
treatment of peripheral nerve disorders, surgical reconstruction for
paralysis of median innervated muscles remains a common procedure. This
chapter discusses the analysis of such problems and the concepts and
techniques of rehabilitation.
within the hand (intrinsic) and those whose origin is more proximal
(extrinsic). Table 56.1 lists these muscles
and their primary functions. The ulnar and radial nerve may activate
muscles usually innervated by the median nerve (21). These variations can lead to diagnostic confusion (11).
The pronator teres and quadratus both pronate the forearm. Because the
pronator teres is more effective if the elbow is extended, the
individual force of these two muscles can be determined by testing the
strength of pronation with the elbow in extension and then in flexion.
 |
|
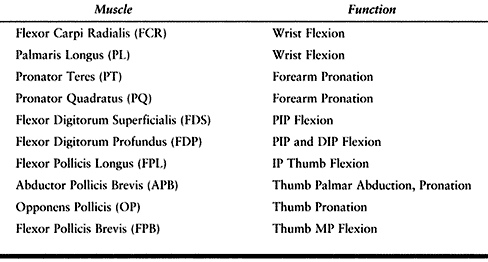
Table 56.1. Muscles Innervated by the Median Nerve
|
to flex the proximal interphalangeal joint of a finger is examined by
holding the other digits in extension, thereby inhibiting flexor
digitorum profundus function. Because the ring and small fingers often
share a common muscle belly, the power of proximal interphalangeal
joint flexion of these two digits should be tested both individually
and simultaneously. In testing the strength of distal joint flexion,
one evaluates the function of the flexor pollicis longus (FPL) and the
flexor digitorum profundus. Thumb opposition is a combined motion of
palmar abduction, pronation, and flexion (7).
This essential thumb motion brings the thumb pulp in contact with that
of one or more fingers. Although prehension is achieved by the three
thenar intrinsic muscles, the abductor pollicis brevis is the most
important (8,10).
as laceration, traction, fracture, gunshot wound, or chronic
compression neuropathy. Diabetic peripheral
neuropathy and viral and lepromatous infection are less common etiologies.
condition. Loss of active pronation adversely affects a person’s
ability to use a computer keyboard or a tool such as a screwdriver.
Weakness of the flexor carpi radialis is rarely a problem because the
flexor carpi ulnaris is innervated by the ulnar nerve and can
adequately perform wrist flexion. Of greater functional importance is
the loss of digital flexion of the thumb, index, and middle fingers.
The ring and small fingers are less affected because their profundi are
usually innervated by the ulnar nerve. Loss of opposition severely
affects one’s ability to grasp as well as engage in fine manipulation.
resolve, make efforts to maintain joint flexibility to prevent
contractures. Teach the patient to perform frequent range-of-motion
exercises primarily to prevent extension deformity of the finger joints
and fixed adduction of the thumb. Using Velcro loop straps to tie the
affected finger and a normal finger together preserves joint motion and
enhances hand function as well. An opposition splint maintains the
thumb–index web space and places the thumb in a more useful position.
If contractures have developed, a hand therapy program is required to
restore digital flexibility. Avoid dynamic traction on the thumb, which
can cause stretching of the ulnar collateral ligament rather than
improvement of the adduction contracture. A better method uses a static
thumb–index web space splint, which is modified as abduction is
obtained.
carpal tunnel syndrome that has caused thenar atrophy. In spite of
modern microsurgical techniques, recovery of motor function after
median nerve neurorrhaphy is frequently poor. Performing a tendon
transfer as an internal splint simultaneous with repair of proximal
median nerve injuries is useful, because permanent thenar palsy is
common. An opposition tendon transfer provides early functional
recovery, avoids adduction contracture, and eliminates the need for
splinting. Even if the intrinsic muscles are reinnervated, the
recovered strength is rarely normal.
splinting can be corrected by release of the deformity with skin
plasties or skin grafts and release of the adductor and the first
dorsal interosseous muscles and, if necessary, the trapeziometacarpal
joint capsule. Joint fusion places a digit in a more functional
position and is especially useful in treating palsy of the flexor
digitorum profundus (provided that the FDS is of normal strength) and
for weakness of the FPL. Although joint fusions are technically simple,
improve dexterity, and do not require postoperative rehabilitation,
they neither restore mobility nor improve weakness. Tendon transfers
require more surgical skill and patient cooperation than does joint
fusion, but they have the potential of providing active joint motion
and regaining strength.
that surgery must be individualized to meet the patient’s needs,
because “each hand is a problem in itself.” He wrote that candidates
for tendon transfer surgery must have adequate sensibility, the thumb
joints should be stable, and the skin and joints must be supple.
force of the tendon to be transferred, the direction of its pull, and
the axis of insertion into the thumb (6) (see Chapter 54).
Although it may not be possible to replace the function of several
weakened intrinsic muscles fully with one tendon transfer, the
replacement should match as closely as possible the normal force and
excursion of the paralyzed muscles. The force generated by a muscle is
proportional to its cross-sectional area, which is 6.0 cm2 for the median innervated thenar intrinsics (3).
are frequently used for tendon transfers, their potential force of
contraction is significantly less. Excursion, or the change in length
between full relaxation and contraction, depends on mean fiber length,
which averages 3.5 cm for the thenar muscles. This figure is surpassed
by all the commonly used transfers.
substitute one imbalance for another. Choosing a strong motor may
improve thumb function, but if a finger flexor is used, the improvement
occurs at the expense of power grip. To produce the motion of
opposition, the transfer must pull from the direction of the pisiform,
paralleling the fibers of the abductor pollicis brevis (7).
Transfers that use a pulley distal to the pisiform encourage metacarpal
flexion at the expense of palmar abduction. The reverse is true for
transfers that pull more proximal and radial to the pisiform. Unless
there exists a supple subcutaneous bed through which the transfer is to
be passed, the motor will not be able to transmit its force of
contraction. Therefore, skin resurfacing may be required before a
tendon transfer is performed. Although free skin grafts can be used in
some areas, flaps are frequently necessary to provide adequate
subcutaneous tissue to allow tendon excursion. Alternatively, a
Silastic tendon prosthesis can be used to form an adequate pathway for
eventual tendon transfer at a second stage.
Insertions into the ulnar base of the proximal phalanx do not produce
greater rotation during opposition, and these insertions may slip about
the metacarpophalangeal (MP) joint, causing unwanted extension or
flexion of the proximal phalanx. Insertions into the extensor mechanism
or the MP joint capsule increase thumb extension and stability, but
they are recommended only for patients with combined nerve palsies in
which a single insertion may result in stretching out of the thumb
ulnar collateral ligament (1,2,20).
-
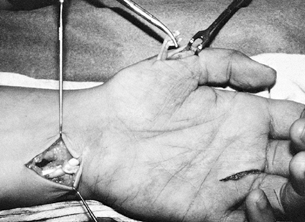
Incise the proximal flexor sheath, and divide the FDS (Fig. 56.1, Fig. 56.2, Fig. 56.3, Fig. 56.4, Fig. 56.5, Fig. 56.6 and Fig. 56.7). Be careful not to divide the FDS too distally, or hyperextension of the proximal interphalangeal (PIP) joint may occur.
![]() Figure 56.1. The three incisions required for an opposition transfer using the ring finger superficialis are shown.
Figure 56.1. The three incisions required for an opposition transfer using the ring finger superficialis are shown. Figure 56.2.
Figure 56.2.
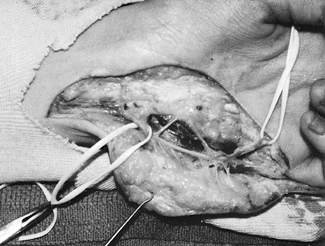
The flexor carpi ulnaris tendon stump has been created, the
superficialis passed beneath the intact portion of the wrist flexor,
and a subcutaneous pathway produced with the tendon passer.![]() Figure 56.3. The superficialis has been transferred and the tendon loop formed.
Figure 56.3. The superficialis has been transferred and the tendon loop formed.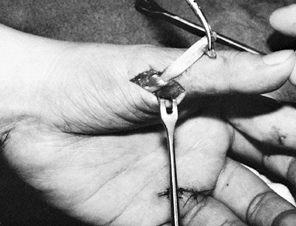 Figure 56.4. The superficialis has been passed through the substance of the thenar intrinsic tendon.
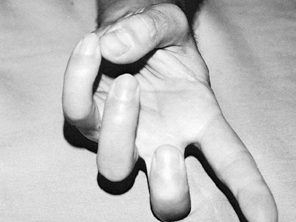
Figure 56.4. The superficialis has been passed through the substance of the thenar intrinsic tendon.![]() Figure 56.5. Lack of active opposition as a result of median nerve palsy.
Figure 56.5. Lack of active opposition as a result of median nerve palsy.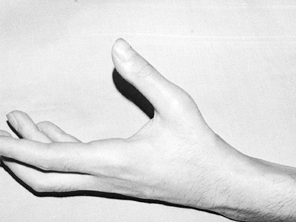 Figure 56.6. Same patient is shown as in Figure 56.5 after superficialis transfer (palmar abduction).
Figure 56.6. Same patient is shown as in Figure 56.5 after superficialis transfer (palmar abduction).![]() Figure 56.7. The same patient is shown (opposition).
Figure 56.7. The same patient is shown (opposition). -
At a point 2 cm proximal to the wrist, expose and withdraw the FDS.
-
Transect the radial half of the FCU 2 cm
from its insertion, leaving a distally based stump that is sutured to
itself, forming a loop. -
Pass the FDS dorsal to the FCU, then through the loop of the FCU.
-
Expose the intrinsic tendon on the radial side of the thumb metacarpal-phalangeal (MP) joint.
-
Pass a large clamp from the thumb incision to retrieve the FDS.
-
Place the thumb in opposition to the ring finger.
-
Interweave the FDS into the intrinsic at half the potential excursion of the transfer.
-
Expose and divide the extensor indicis
proprius (EIP) with a thin strip of radial MP extensor hood. Suture the
defect in the hood. -
Withdraw the EIP just proximal to the retinaculum.
-
Place a large clamp into a 2 cm incision at the distal ulnar aspect of wrist.
-
Retrieve the EIP and continue as for a FDS transfer.
possible. This transfer is not as powerful as a FDS transfer, but it
has the advantage that it does not weaken the patient’s grip (6).
-
Make sure that before the extensor digiti quinti (EDQ) is divided that there is a ring—to—small communis slip (Fig. 56.8).
 Figure 56.8.
Figure 56.8.
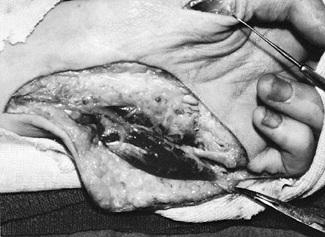
The EDQ has been divided, and a clamp has been used to form a
subcutaneous passage between the distal forearm and the thenar eminence. -
Divide the EDQ at the small finger MP and withdraw it via an additional incision proximal to the rentinaculum.
-
Complete the procedure as for an EIP transfer.
-
Expose the distal ECU and divide it at its insertion (Fig. 56.9, Fig. 56.10, Fig. 56.11 and Fig. 56.12).
![]() Figure 56.9. The insertion of the ECU has been transsected.
Figure 56.9. The insertion of the ECU has been transsected. Figure 56.10. The extensor pollicis brevis has been divided at its musculotendinous junction and its insertion exposed.
Figure 56.10. The extensor pollicis brevis has been divided at its musculotendinous junction and its insertion exposed.![]() Figure 56.11. The transposed extensor pollicis brevis, without traction.
Figure 56.11. The transposed extensor pollicis brevis, without traction. Figure 56.12. The extensor pollicis brevis, with traction.
Figure 56.12. The extensor pollicis brevis, with traction. -
Divide the extensor pollicis brevis at the musculotendinous juncture and bring it out at the thumb MP.
-
Transfer the EPB subcutaneously across the palm and suture it into the ECU.
-
Through a palmar incision, dissect the PL and elongate it with palmar fascia.
-
Pass the tendon subcutaneously and suture it into the APB tendon.
release, PL transfer is a weak transfer that provides good abduction
but poor pronation (Fig. 56.13).
 |
|
Figure 56.13. The palmeris longus has been exposed and prolonged with a strip of palmar fascia.
|
-
Expose the entire muscle and tendon to the ADQ.
-
Identify the ulnar artery or nerve and neurovascular pedicle to the ADQ.
-
Divide the insertion and attachments to the FCU and pisiform.
-
Turn the muscle like the page of a book,
and pass it through a generous tunnel toward the thumb. Suture it into
the abductor pollicis brevis (APB).
 |
|
Figure 56.14. The ADQ muscle has been exposed and the ulnar nerve and artery carefully dissected and retracted with vessel loops.
|
 |
|
Figure 56.15. The origin and insertion of the ADQ have been divided and the conjoined thenar intrinsic tendon exposed.
|
 |
|
Figure 56.16. Active palmar abduction regained after ADQ transfer.
|
-
Reroute the FPL after osteotomy of the proximal phalanx or before interphalangeal joint fusion.
palmar abduction rather than true opposition is obtained. Better
results occur with FPL transfer using the FDS technique.
-
Expose the FPL and the FDS through a midvolar forearm incision.
-
Divide the FDS and interweave it into the FPL so that the interphalangeal joint of the thumb rests in 30° of flexion.
-
Release the extensive insertion and fully
mobilize the brachioradialis (BR) well up the forearm. The BR does not
have equivalent excursion to the FPL and requires a large incision to
release the insertion fully. -
Attach the BR tendon to the FPL with an interweave technique.
-
Expose all of the FDP tendons in the distal forearm.
-
Suture side to side the weakened tendons to the active ones.
not strength. If the FDS are functioning, distal interphalangeal (DIP)
joint fusions are preferable.
-
Divide the extensor carpi radialis brevis (ECRB) at the 3rd metacarpal.
-
Pass it through a large window in the interosseous membrane.
-
Interweave into the paralyzed FDP.
postoperative immobilization. If the purpose of the surgery is to
regain digital flexion, place the wrist in 30° of palmar flexion, the
MP joint in maximal flexion, and the interphalangeal joint flexed
approximately 20°. Protect opposition transfers for 1 month by
immobilizing the thumb in maximal palmar abduction with the wrist in a
neutral position unless an extensor was transferred. Extensor transfer
requires mild wrist flexion to relieve suture line tension.
reeducation process begun. The patient should exercise for 5 to 10
minutes every 1 to 2 hours. More prolonged activity may fatigue the
transfer. Encourage active motion to activate the transfer and permit
passive motion, which does not stress the tendon juncture. Gentle
resistance, such as squeezing a wet sponge or crumpling a newspaper, is
permitted at postoperative week 6. Muscle reeducation can be encouraged
by having the patient activate both hands simultaneously. Muscle
massage and biofeedback may be helpful. If after 6 weeks adequate
digital motion has not been achieved, splint the MP joint in extension
in order to generate more power at the interphalangeal joint.
continue to flex rather than abduct the thumb. Inhibit this tendency by
splinting the interphalangeal joint in extension. Eight weeks after
tendon transfer surgery, encourage the strengthening process using
putty and free weights. At this time, passive stretching of the
transfer can be prescribed if the resting tension of the transfer is
too high or if contractures are developing.
occurs because of uncorrected preoperative joint stiffness, errors in
surgical technique, or inability of the muscle to
be
reeducated. If adequate mobility is caused by either excessive or
inadequate tension of the transfer, revision surgery can be done to
alter the tension. Occasionally, disruption of the transfer occurs,
which is usually the consequence of excessive loading in the first few
months after surgery. If you recognize this condition, perform an
expeditious repair.
transfer of the FDS. If this tendon is divided close to its insertion
and the volar plate is or becomes lax, a swan-neck deformity can ensue.
Minimize this problem by dividing the tendon in the palm, thereby
retaining the distal portion of the superficialis tendon. Although this
technique minimizes PIP hypertension, the reverse complication, i.e.,
PIP joint flexion contracture, can occur if the patient was not
instructed to extend the joint fully subsequent to transfer injury.
divided, use an extension block splint. Conversely, if the finger
develops a flexion contracture, apply a dynamic extension splint. Loss
of index MP joint extension and radial subluxation of the extensor
digitorum communis are known complications of the extensor digiti
propius (EIP) opposition transfer. Avoid these problems by careful
closure of the extensor hood. Positioning the wrist in marked flexion
after a simultaneous carpal tunnel release and tendon transfer to
restore opposition can result in palmar subluxation of the median nerve
and flexor tendons. Subluxation can produce scar entrapment of the
nerve, bow-stringing of the flexor tendons, and a wrist flexion
contracture. Excessive loss of finger extension may result after
transfer of the extensor carpi radialis to the digital flexors because
the excursion of a wrist motor is significantly less than that of a
digital flexor. Avoid this problem by making sure that at the time of
transfer, the fingers can be passively extended fully with the wrist in
no more than 20° of flexion.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
GS, Miller RC. The Transfer of Wrist Extensor Muscles to Restore or
Reinforce Flexion Power of the Fingers and Opposition of the Thumb. J Bone Joint Surg 1947;29:993.