Lumbar Plexus Blocks
The site of needle insertion is the intersection between the vertical
line drawn from the highest point of the iliac crest and the line drawn
from the posterior superior iliac spine parallel to midline along the
spinous processes of L4 and L5. The needle connected to the nerve
stimulator set at 1.5 mA and 2 Hz is introduced perpendicular to the
skin in search of the transverse process of L4. Then redirect the
needle cranial or caudal and 1 cm deeper until stimulation of the
femoral nerve is elicited (contraction of the quadriceps muscle,
usually the vastus lateralis muscle). Adjust the position of the needle
to maintain the appropriate muscle response with a current of 0.4 to
0.5 mA. Then, after negative aspiration, slowly inject the local
anesthetic solution.
-
This block is more difficult and not free
of complications in a pediatric patient, therefore should only be
performed by anesthesiologists trained in pediatric regional anesthesia. -
It is important to remember the distance
between skin and nerve vary according to the age: 2.5 cm at 1 year
increasing to 8 cm in adolescents. -
There are some contraindications for this
block: coagulation disorders, trauma of the lumbar spine, lumbar
vertebral deformities, peritoneal or visceral infections. -
Complications include:
-
Visceral organ puncture, especially of the kidney. Use the shortest needle that can reach the plexus.
-
Subarachnoid (high or total spinal
anesthesia) or epidural (contralateral anesthesia) spread. Avoid a
medial puncture direction, perform a test dose, inject slowly and while
injecting watch closely blood pressure and heart rate. -
Vessel puncture (paravertebral veins).
D, Matuszczak M, Gebhard R. Continuous posterior lumbar plexus block
for acute postoperative pain control in young children. Anesthesiology 2001;95(6):1521–1523.
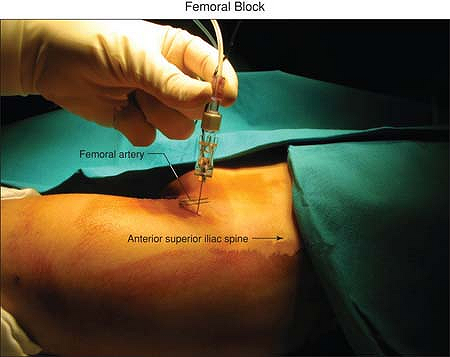
The femoral artery should be palpated and marked. The site of
introduction of the needle is vertically, 0.5 to 1 cm both below the
inguinal ligament and lateral to the femoral artery. Set the nerve
stimulator at a frequency of 2 Hz and a current of 2.5 mA. Connect this
to the pen dedicated for the transcutaneous technique (instead
of
the pen it is possible to use the negative electrode of the ENS) and
point it perpendicular to the skin in an anteroposterior direction
until a motor response of the femoral nerve is elicited (contraction of
the quadriceps muscle with the phenomenon of the “dancing patella”).
Then insert the needle connected to the nerve stimulator set at 1 mA
and 2 Hz, exactly at the point evidenced via transcutaneous in an
anteroposterior direction until the motor response is again elicited.
Adjust the position of the needle to maintain the appropriate muscle
response with a current of 0.4 to 0.5 mA. Then, after negative
aspiration, slowly inject the local anesthetic solution.
 |
|
Figure 49-1. The inguinal ligament and the femoral artery.
|
-
This block has a very high success rate,
around 100%, without any particular contraindications or side effects,
except vessel (femoral vein and artery) puncture. -
This block will be unsuccessful in cases of sartorius muscle stimulation.
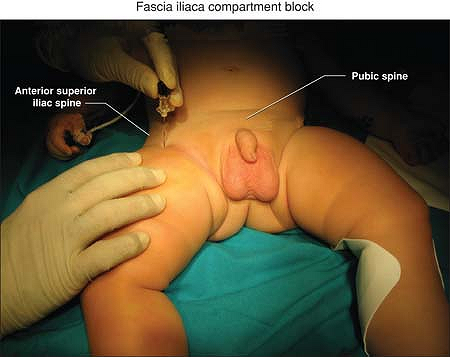
The line uniting the pubic spine to the anterior superior iliac spine
is divided in three equal parts. A short beveled needle is then
introduced vertically 0.5 to 1 cm below the union of the lateral
one-third to the medial two-thirds; that is, at least 2 to 3 cm lateral
to the femoral artery, until two losses of resistance, respectively
corresponding to the fascia lata and the fascia iliaca, are felt. No
electroneurostimulator can be used in performing this block as no motor
fibers are present at this level.
 |
|
Figure 49-2. Inguinal ligament.
|
-
The fascia iliaca compartment block is a
multi-block technique with a single injection. The anesthetic solution
is injected at the inner face of the fascia iliaca along which it
spreads and can contact all the nerves emerging from the psoas
compartment. -
The femoral nerve (100%) and the lateral
femoral cutaneous and the obturator nerves (70% to 90%) are blocked
with this technique.
O, Sallaberry M, Schreiber-Deturmey E, et al. Continuous fascia iliaca
compartment block in children: a prospective evaluation of plasma
bupivacaine concentrations, pain scores, and side effects. Anesth Analg 2001;92(5):1159–1163.
The saphenous nerve, terminal branch of the femoral nerve, is a pure
sensory nerve that runs alongside with the motor nerve supplying the
vastus medialis muscle. The femoral artery and the inguinal ligament.
The site of introduction of the needle is vertically, 0.5 cm lateral to
the femoral artery and 3 to 6 cm (depending on the patient’s age and
size) below the inguinal ligament. Set the nerve stimulator at a
frequency of 2 Hz and a current of 2.5 mA. Connect this to the pen
dedicated for the transcutaneous technique (instead of the pen it is
possible to use the negative electrode of the ENS) and point it
perpendicular to the skin in an anteroposterior direction until a motor
response of the vastus medialis is elicited. Then insert the needle
connected to the nerve stimulator set at 1 mA and 2 Hz exactly at the
point evidenced via transcutaneous in an anteroposterior direction
until the motor response is again elicited. Adjust the position of the
needle to maintain the appropriate muscle response with a current of
0.4 to 0.5 mA. Then, after negative aspiration, slowly inject the local
anesthetic solution.
