ISOLATED POSTERIOR CRUCIATE LIGAMENT INJURY AND POSTEROLATERAL LAXITY
IV – SPORTS MEDICINE > Knee > CHAPTER 90 – ISOLATED POSTERIOR
CRUCIATE LIGAMENT INJURY AND POSTEROLATERAL LAXITY
the two cruciate ligaments and is the primary restraint to posterior
tibial translation at 90° of knee flexion. The recent emphasis on
reconstructive surgery in cases of anterior cruciate ligament (ACL)
injury has stimulated an increased interest in the PCL, and
investigators have begun to study the anatomy, biomechanics, and
function of the PCL in greater detail. Additionally, there have been
attempts to better document the natural history of the PCL-deficient
knee as well as to define the optimum time and method of reconstruction
in cases in which surgery is deemed necessary. Despite the large
numbers of articles published recently on these topics, the management
of injury to the PCL continues to be controversial. Support for
both surgical and nonsurgical management can be found in the orthopaedic literature.
includes the lateral collateral ligament (LCL), popliteus tendon,
fabellofibular ligament, arcuate ligament, popliteofibular ligament,
and the short lateral ligament. The LCL resists straight varus rotation
of the tibia, and the remaining structures restrain external tibial
rotation. Isolated injury of the posterolateral corner is uncommon.
When PLC injury occurs with injury to the PCL, both injuries must be
appropriately diagnosed and treated to obtain a satisfactory outcome.
the epidemiology, mechanism of injury, clinical evaluation, imaging,
treatment, and results of treatment of injuries to the PCL and PLC. A
section at the end of the chapter outlines the preferences of the
senior author (W.G.C.), who has treated more than 400 patients with PCL
insufficiency.
The symptoms and clinical signs of isolated PCL injury, however, may be
subtle both to patient and to physician, and the injury may often be
missed (17,28,77). When diagnosed, the isolated PCL injury is often treated nonsurgically.
injury is higher than that quoted in the literature. It is interesting
to note that approximately 2% to 5% of the players participating in the
National Football League’s predraft physical examinations have evidence
of isolated PCL laxity, and most of these players are unaware of having
had a significant ligamentous injury (4). In a
study that analyzed 500 knee ligament injuries with pathologic motion
as measured by a KT-1000 arthrometer, 63% were found to be ACL
injuries, and 7% were PCL injuries (19).
Seventy-five percent of the ACL injuries were isolated, compared with
49% of the PCL injuries. It is not uncommon for PCL injuries to have
associated injury to the ACL, medial collateral ligament (MCL), and the
posterolateral corner (PLC) (33,34,47).
(i.e., athletic) and high-energy (i.e., motor vehicle accident)
etiologies because of the higher incidence of combined ligamentous
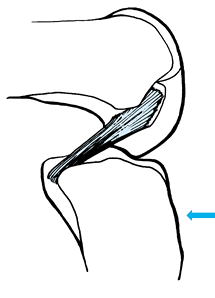
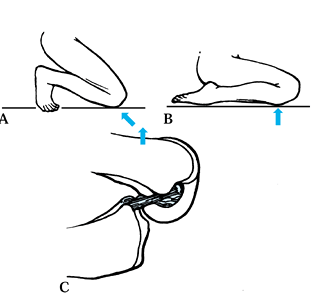
injuries and associated injuries in the latter (62). Injury to the PCL has been described as occurring in one of four ways (Fig. 90.1, Fig. 90.2 and Fig. 90.3): (a) a posterior force applied to the tibia with the knee in flexion (which often results in a midsubstance injury) (22), (b) a fall onto the flexed knee with the foot in plantarflexion (11,25), (c) hyperflexion (28), and (d) hyperextension (45).
Two other less common means of injury have recently been described,
including a noncontact, external rotation/posterior translation injury (67) as well as an external rotation/valgus injury (66).
 |
|
Figure 90.1.
Mechanism of injury to the PCL: a posterior force applied to the proximal tibia with the knee in 90° of flexion. (From DeLee JC, Bergfeld JA, Drez D Jr, Parker AW. The Posterior Cruciate Ligament. In: DeLee JC, Drez D Jr, eds. Orthopaedic Sports Medicine. Principles and Practice. Philadelphia: WB Saunders, 1994, with permission.) |
 |
|
Figure 90.2. Mechanisms of injury to the PCL. A: A fall onto the flexed knee with the foot in dorsiflexion results in force being transmitted through the patellofemoral joint. B:
A fall onto the flexed knee with the foot in plantarflexion results in force being transmitted to the tibial tubercle and hence to the PCL. C: A hyperflexion injury can result in an avulsion of the origin of the PCL from the femur. (From DeLee JC, Bergfeld JA, Drez D Jr, Parker AW. The Posterior Cruciate Ligament. In: DeLee JC, Drez D Jr, eds. Orthopaedic Sports Medicine. Principles and Practice. Philadelphia: WB Saunders, 1994, with permission.) |
 |
|
Figure 90.3.
Mechanism of injury to the PCL: hyperextension. (From DeLee JC, Bergfeld JA, Drez D Jr, Parker AW. The Posterior Cruciate Ligament. In: DeLee JC, Drez D Jr. Orthopaedic Sports Medicine. Principles and Practice. Philadelphia: WB Saunders, 1994, with permission.) |
The result is a varus and rotational moment about the knee.
Hyperextension alone or combined with external rotation and knee
extension have also been implicated in noncontact injuries to the PLC (10,13,80).
can often be confusing, particularly when it occurs acutely and is
isolated. The presence of quadriceps muscle spasm may mask some of the
findings on physical exam, and isolated injury to the PCL may be
dismissed by the athlete as insignificant (4).
A tense effusion such as occurs with an acute ACL injury is usually
absent. For this reason, the history and physical exam are of paramount
importance, not only to diagnose the injury itself but also to
determine the site of the injury and therefore to help determine the
appropriate treatment plan.
suspected PCL injury can help determine the likelihood of injury to the
ligament as well as suggest the potential site of involvement along the
length of the PCL. Injury to the midsubstance of the PCL often occurs
following a direct blow to the anterior proximal tibia with the knee
flexed (27,28).
Midsubstance injuries may also occur after a fall onto the flexed knee
with the foot in plantarflexion, which concentrates the bulk of the
force on the tibial tubercle (25).
with the knee in extension is a common mechanism in sports-related
injuries and also results in midsubstance injury to the PCL as well as
injury to the posterolateral corner structures. A pure hyperflexion
injury without a force being applied directly to the proximal tibia
often results in avulsion of the origin of the ligament from the medial
femoral condyle, offering a chance for primary repair (25) (although the senior author has never seen a successful result of primary repair).
discomfort in the knee while weight bearing in a semiflexed position,
such as ascending or descending stairs or squatting down (18). Aching in the knee when walking long distances is also a common complaint (18).
Approximately 50% of patients with symptomatic PCL insufficiency
complain of instability or a sense of instability in the knee that is
problematic when they are walking on uneven ground (18). Approximately half of the patients reported on by Cross and Powell (17)
complained of retropatellar pain in the knee that was not present
initially but developed at some point after the injury. Swelling and
stiffness may vary and depend on the degree of associated chondral
damage.
reasons. Often the athlete is unaware of having sustained a significant
injury, because many patients have a full range of motion with very
little hemarthrosis (4,11,16,18).
Often it is only the posterior drawer test that causes any pain. The
presence of a contusion over the proximal anterior tibia may be very
helpful in suggesting injury to the PCL.
proximal tibia to the femur when the knee is flexed to 90° cannot be
overemphasized. When the PCL is intact, flexion of the knee to 90°
results in the anterior proximal tibia being positioned approximately 1
cm anterior to the distal femoral condyles (Fig. 90.4), referred to as a normal anterior stepoff. Loss of this normal anterior stepoff signifies injury to the PCL (11). The importance of detecting this posterior subluxation has been emphasized by Clancy et al. (11),
who state that it is best viewed from the side with the knee flexed to
90°. This posterior subluxation of the proximal tibia with the knee
flexed to 90° is also known as the posterior sag sign (of Godfrey).
 |
|
Figure 90.4.
When the PCL is intact, flexion of the knee to 90° should result in the proximal tibial eminence being anterior to the distal femoral condyles by approximately 1 cm. (From DeLee JC, Bergfeld JA, Drez D Jr, Parker AW. The Posterior Cruciate Ligament. In: DeLee JC, Drez D Jr, eds. Orthopaedic Sports Medicine. Principles and Practice. Philadelphia: WB Saunders, 1994, with permission.) |
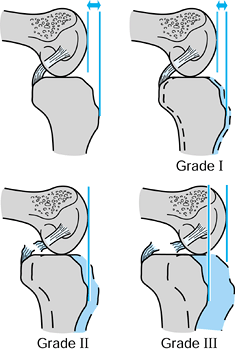
This test is graded with respect to the opposite knee. Loss of the
normal anterior tibial stepoff compared with the opposite side, but
with the proximal tibial eminence remaining anterior to the distal
femur, is considered to be a 1 + posterior drawer. When the proximal
tibial eminence can be translated posteriorly to the point where it is
flush with the distal femoral condyles, the posterior drawer is graded
2 +. It is thought to signify complete disruption of the PCL.
Translation of the proximal tibial eminence posterior to the distal
femoral condyles is considered to be grade 3 + and is thought to
signify complete PCL disruption and usually posterolateral ligamentous
injury as well. This test, however, has been reported to be positive in
as few as 10% to as many as 76% of patients with acute PCL disruptions (33,44,53,60).
 |
|
Figure 90.5. Method of grading the posterior drawer test (see text for explanation).
|
2 + posterior drawer, with the tibia held first in neutral and then in
external rotation, is diagnostic of a complete disruption of the PCL.
They also emphasized that 80% of patients with complete disruption of
the PCL would have a normal posterior drawer sign with the tibia held
in internal rotation. This loss of the posterior drawer with the tibia
held in internal rotation is explained by the fact that internal tibial
rotation tightens the meniscofemoral ligaments, which are usually
intact following injury to the PCL. These ligaments are then able to
resist attempted posterior tibial translation during the posterior
drawer maneuver. We have also found meniscal injury to be uncommon both
clinically and at arthroscopy when the PCL is injured. Keep in mind
that muscle spasm and pain can significantly limit the utility of the
posterior drawer test.
These examiners found that the posterior drawer test, including
palpation of the tibial stepoff, was the most sensitive and specific
clinical test for PCL insufficiency. Clinical examination for chronic
PCL injury was 96% accurate, 90% sensitive, and 99% specific. The
interobserver agreement for the grade of the injury was 81%.
limit the effectiveness of the posterior drawer test in the acute
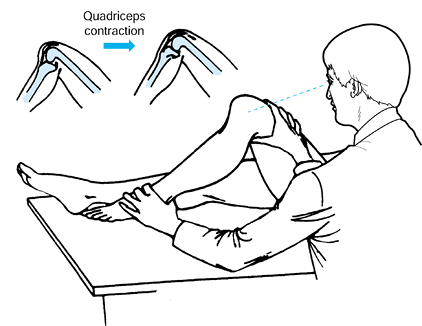
setting, Daniel et al. (20) introduced the quadriceps active drawer test to detect PCL injury (Fig. 90.6).
This test is based on the biomechanical relationship between the line
of action of the patellar tendon and the resultant quadriceps muscle
force. In an intact knee, the line of action
of
the patellar tendon tends to pull the proximal tibia anterior at low
knee-flexion angles. At high knee-flexion angles, the PCL causes the
femur to roll back on the proximal tibia, and the line of action of the
patellar tendon therefore tends to pull the proximal tibia posterior.
 |
|
Figure 90.6.
Performance of the quadriceps active drawer test. See text for explanation. (From Daniel DM, Stone ML, Barnett P, Sachs R. Use of the Quadriceps Active Test to Diagnose Posterior Cruciate Ligament Disruption and Measure Posterior Laxity of the Knee. J Bone Joint Surg 1988;70A:386, with permission.) |
the patellar tendon is directly perpendicular to the surface of the
tibial plateau is called the quadriceps-neutral angle and occurs at 60°
to 90° of flexion in the intact knee. In a knee with the PCL injured or
absent, rollback of the femur on the tibia does not occur with
increasing knee flexion. Therefore, the line of action of the patellar
tendon is always directed anteriorly.
subject relaxed in the supine position with the knee flexed 70° to 90°.
The examiner stabilizes the patient’s foot on the table and then asks
the patient to slide the foot distally on the table. In the normal
knee, the patellar tendon line of action will be directed posteriorly,
and this quadriceps contraction will not cause any anterior translation
of the proximal tibia. In the patient with deficiency of the PCL,
however, the posterior sag of the proximal tibia results in the line of
action of the patellar tendon being directed anteriorly, and this
quadriceps contraction evokes a notable anterior translation of the
proximal tibia. Daniel et al. (20) found the
quadriceps active drawer test to be positive in the knees of 41 of 42
patients with documented disruption of the PCL. Anterior translation
did not occur in the contralateral normal knee of these patients, nor
did it occur in 25 knees with known disruption of the ACL. These
authors found this test to be useful in both acute and chronic cases.
structures are often caused by a blow to the anteromedial tibia with
the knee in extension. This mechanism of injury is not uncommon in
sports-related injuries to the PCL. A blow delivered to the lateral
aspect of the knee causes a valgus force at the knee joint and first
injures the MCL and the posteromedial capsule. Once these structures
have been injured, the cruciate ligaments are the next restraints to
valgus rotation. This mechanism of injury may cause combined ACL/MCL or
PCL/MCL injuries. Finally, impact to the medial aspect of the knee
first causes disruption of the lateral collateral ligament and the
posterolateral corner structures. If the injury is severe enough, the
central pivot ligaments are next to fail. This mechanism results in
combined injury to the ACL and posterolateral structures or to the PCL
and posterolateral structures.
injury often has a significant amount of pain compared with the patient
with an isolated PCL injury. Disruption of the capsule that occurs in
conjunction with collateral ligament injury may allow dissection of the
hemarthrosis into the thigh and leg and therefore limit the amount of
effusion present. The primary concern in the knee with multiple
ligament injuries is the possibility of neurovascular injury. It has
been reported that approximately 50% of knee dislocations become
reduced spontaneously at the time of injury and are consequently not
evident at the time of initial evaluation (24).
with disruption of multiple knee ligaments. Pay careful attention to
the vascular and neurologic status of the extremity. Consult with a
vascular surgeon to determine the need for arteriography or exploration
in cases with any change in the vascular status of the injured
extremity. Arteriography to rule out intimal injury is recommended in
known instances of dislocation, even in the presence of normal pulses.
Bear in mind that in combined PCL and lateral ligamentous injury there
an incidence of peroneal nerve injury that approaches 30% (24).
often complains of instability of the knee that is particularly
bothersome when he is walking on uneven ground. The patient feels the
knee give way at the posterolateral aspect, and he feels pain medially
and posterolaterally. The medial pain is caused by increased medial
joint loads, which are a result of the increased medial compartment
loads secondary to PCL insufficiency (68) as well as of the
varus thrust that is present during gait. The posterolateral pain is a
result of stretching of those structures during the varus thrust
component of gait.
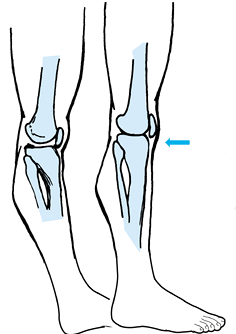
the PCL. Varus laxity with the knee held in 30° of flexion indicates
injury to the fibular collateral ligament as well as possible injury to
the posterolateral structures. Place the leg in the figure-of-four
position to allow palpation of the lateral collateral ligament and
confirmation of its integrity. Use the external rotation recurvatum
test to help determine the presence of injury to the posterolateral
structures. Grasp the great toes of each leg with the knees in
extension and lift each leg off of the examining table. Hyperextension
as well as increased external rotation of the involved leg suggests
significant injury to the posterolateral structures (Fig. 90.7).
The posterolateral drawer test, which is positive when the lateral
tibial plateau rotates externally and posteriorly at the end of the
posterior drawer test, is another test helpful in determining the
presence of injury to the posterolateral structures. It should be
noted, however, that these tests have a relatively low sensitivity,
being positive in only 25% and 33% of patients, respectively (23).
 |
|
Figure 90.7.
The external rotation recurvatum test. (From Hughston JC, Norwood LA. The Posterolateral Drawer Test and External Rotational Recurvation Test for Posterolateral Rotary Instability of the Knee. Clin Orthop 1980;147:82, with permission.) |
that a 15° increase in tibial external rotation at 30° of knee flexion
is indicative of significant injury to the posterolateral structures.
Increased external rotation of the tibia at 90° of flexion indicates
injury to both the PCL and posterolateral ligament complex. The reverse
pivot-shift test, introduced by Jakob et al. (38),
is another test that is used to assess the posterolateral ligaments. In
the reverse pivot-shift test, the knee is reduced in full extension. As
the examiner applies a valgus and external rotation force while flexing
the knee, the lateral tibial plateau can be felt to subluxate
posteriorly. This maneuver creates a shifting sensation similar to that
felt during the classic pivot shift in patients with ACL laxity. All of
these tests are more profoundly positive in the presence of associated
PCL insufficiency.
by looking for increased valgus laxity at both full extension and 30°
of flexion. The above-mentioned tests for PCL injury are also positive.
There will also be a greater posterior translation of the medial tibial
plateau during the posterior drawer test at 90° of knee flexion. It
should be noted that PCL/MCL injury is less common than PCL/PLC injury.
Finally, patients with injury to the PCL as well as both the medial and
lateral sides of the knee exhibit symmetric posterior displacement of
both tibial plateaus during the posterior drawer test.
axial patellofemoral views, usually taken in the case of acute PCL
injury, often are not diagnostic. The lateral radiograph may show an
avulsion of the PCL from its tibial insertion, but this is a relatively
uncommon injury (Fig. 90.8) (75,76,77 and 78).
In cases of chronic PCL insufficiency, radiographs may show evidence of
arthrosis of the medial and patellofemoral articulations.
 |
|
Figure 90.8.
Lateral radiograph of the knee demonstrating avulsion of the insertion of the PCL from the tibia. (From Cooper DE, Warren RF, Warner JJP. The Posterior Cruciate Ligament and Posterolateral Structures of the Knee: Anatomy, Function and Patterns of Injury. Instr Course Lect 1991;40:249, with permission.) |
radiographs using a plumb line to determine the mechanical alignment of
the limb (54). If the patient with
posterolateral laxity and varus alignment has a ligamentous
reconstruction without correction of the mechanical axis by osteotomy,
the abnormal stresses imposed on the reconstruction by the varus
alignment would be expected to result in failure of the reconstruction.
in documenting the presence of injury to the PCL. Radiographs taken at
70° to 90° of flexion with first an anterior and then a posterior
stress are helpful for diagnosis of PCL insufficiency as well as for
comparison with postoperative stress radiographs in order to allow an
objective evaluation of results among investigators. Correction of the
total AP translation to that present in the normal opposite knee is one
objective way of suggesting that the restoration of normal biomechanics
of the knee has been achieved.
radiographs in the documentation of complete PCL injury as well as in
the differentiation between complete and partial tears of the PCL.
These investigators found that 8 mm or more of increased posterior
translation occurring with the application of an 89-N posterior load at
70° of flexion was indicative of a complete rupture of the PCL. They
also found that stress radiographs were superior to both KT-1000
arthrometry and clinical exam in assessing the status of the PCL.
the accuracy with which acute ligamentous injuries of the knee may be
detected and correctly diagnosed and has allowed the detection of other
associated injuries to the menisci, cartilage, and subchondral bone (79). Not only can MRI confirm suspected injury to the PCL, it can also determine the site of injury to the ligament (Fig. 90.9).
One of us (W.G.C.) has also noted that MRI may show a lesion in
continuity of the PCL. This injury is characterized by increased signal
in the midsubstance of the ligament without evidence of complete
disruption and is characterized by laxity of the PCL on clinical exam.
This injury may heal with a decrease in the initial laxity.
 |
|
Figure 90.9.
Lateral MRI of the knee demonstrating midsubstance disruption of the PCL. (From DeLee JC, Bergfeld JA, Drez D Jr, Parker AW. The Posterior Cruciate Ligament. In: DeLee JC, Drez D Jr. Orthopaedic Sports Medicine. Principles and Practice. Philadelphia: WB Saunders, 1994, with permission.) |
a patient with pain and isolated PCL insufficiency. Isolated chronic
PCL insufficiency rarely leads to instability, and the disability from
this injury is more often a result of pain secondary to articular
cartilage changes. For this reason, it has been suggested that serial
bone scanning may allow early diagnosis of changes of the articular
cartilage in the patient who is being treated nonsurgically. Early
recognition of increased joint contact pressures secondary to the
abnormal knee biomechanics present in the knee with PCL insufficiency
may allow a reconstruction to arrest these changes before irreversible
progression takes place. This argument, however, assumes that
reconstruction of the PCL restores the knee biomechanics to normal and
prevents further deterioration of the articular cartilage. To date, no
scientific study has confirmed this hypothesis.
controversial, and recommendations have been made for both surgical and
nonsurgical management. A large part of the controversy arises from the
fact that there are very few studies
that
document the long-term results of any form of treatment. Many studies
do not differentiate between results obtained with isolated PCL injury
versus combined injury patterns, or between results obtained in cases
of chronic versus acute PCL insufficiency. The relative infrequency of
PCL injury combined with the limited indications for operative
treatment also make it difficult for one surgeon to gain a large
experience in the treatment of the PCL-insufficient knee.
When the PCL is torn, the patella and patellar tendon take on a more
prominent role in the prevention of posterior tibial translation (8,17).
Also, the increased posterior tibial sag that occurs in the
PCL-deficient knee shortens the moment arm of the quadriceps,
decreasing its mechanical advantage (71).
Therefore, nonoperative management of PCL injuries should emphasize
quadriceps strengthening as a key component of the rehabilitation
program (57). Restoration of satisfactory quadriceps strength, however, does not necessarily ensure a good long-term clinical result (42).
muscles that act to prevent posterior tibial translation, particularly
the quadriceps, while minimizing gravity-induced posterior tibial sag (50).
Avoid open-kinetic-chain hamstring exercises (performed with the foot
free, compared with closed-kinetic-chain exercises, which are performed
with the foot fixed), which cause posterior tibial translation in the
PCL-deficient knee (49). Closed-kinetic-chain exercises such as the squat cause less shear force at the tibiofemoral joint (49) and are the preferred method for strengthening the quadriceps.
the leg extension may be used if certain precautions are followed.
Green et al. (31) found that open-kinetic-chain
extension exercises in the range from 70° to 0° of flexion minimized
posterior tibial translation. Placement of the resistance pad distally
on the leg during the exercise routine lessens articular contact
pressures in the medial compartment and diminishes the posterior
stresses on the secondary restraints (14,46).
PCL injury involves three phases: (a) a maximum protection phase, which
is used during the first 2 weeks following injury; (b) a moderate
protection phase, used from week 4 to week 6 after injury; and (c) a
minimal protection phase, used 6 to 8 weeks after injury.
PCL injury and progress over the first 2 to 3 weeks. Encourage weight
bearing as tolerated using two crutches. Use a brace permitting range
of motion from 0° to 60°. When the individual is comfortable, begin
straight-leg raises, knee extension from 60° to 0°, quadriceps
isometrics at 60°, 40°, and 20°, and minisquats and leg presses from 0°
to 45°. Over the next 2 to 3 weeks, progress to full weight bearing,
begin cycling for range of motion, and increase leg-press range of
motion up to 60° of flexion.
to 6 after the injury. Increase range of motion to normal as tolerated
and discontinue bracing. Increase resistance exercises and begin
activities such as the use of rowing and stairclimber machines. Running
may be initiated in the pool during this phase. Introduce light
resistance hamstring curls and step-ups.
Continue all strengthening exercises and begin a running program, if
appropriate. Patients may gradually return to sporting activities.
Criteria to be met before returning to sports include absence of pain,
tenderness, and swelling as well as isokinetic testing documenting at
least 85% strength, comparing the injured to the normal side.
chronic isolated injury to the PCL with the above rehabilitation
program. Patients with injury to another major knee ligament in
addition to the PCL, as well as those with isolated PCL injuries who
continue to have pain or instability despite use of the above rehab
program for at least 3 months, require evaluation for surgical
reconstruction.
Treat undisplaced fractures with immobilization of the knee in
extension, using the intact collateral ligaments to help prevent
posterior sag (55,56).
 |
|
Figure 90.10.
Avulsion of the PCL from the tibia fixed with a screw. (From Bowen MK, Warren RF, Cooper DE. Posterior Cruciate Ligament and Related Injuries. In: Insall JN, Windsor RE, Scott WN, et al., eds. Surgery of the Knee. New York: Churchill Livingstone, 1993:536, with permission.) |
 |
|
Figure 90.11.
Tibial avulsion of the PCL reattached with sutures placed through the bony fragment and secured over a button. (From Bowen MK, Warren RF, Cooper DE. Posterior Cruciate Ligament and Related Injuries. In: Insall JN, Windsor RE, Scott WN, et al., eds. Surgery of the Knee. New York: Churchill Livingstone, 1993:536, with permission.) |
PCL has given almost uniformly excellent results, whereas nonsurgical
treatment has a significant incidence of residual instability (46,77).
with avulsion fractures of the tibial insertion of the PCL using cast
immobilization in small or nondisplaced fractures and staple fixation
in large or displaced fragments. All patients had excellent or good
result at an average of 4 years of follow-up. He
reported
satisfactory results in fractures less than 7 weeks old, whereas
repairs delayed beyond 11 weeks resulted in less satisfactory outcomes.
 |
|
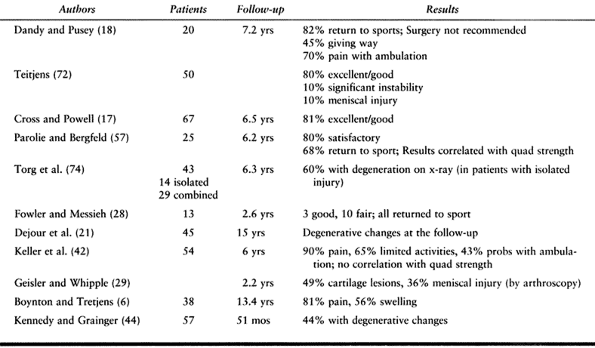
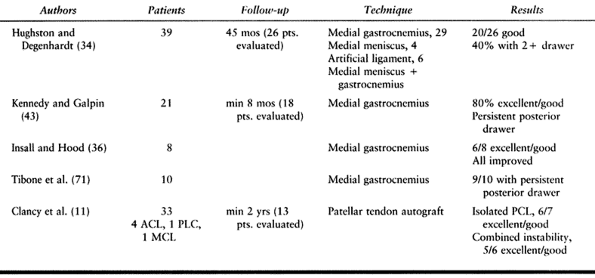
Table 90.1. Results of Nonoperative Treatment for Isolated PCL Injuries
|
-
The subjective results of nonsurgical treatment of the isolated PCL injury are not excellent (42). There is a 20% to 25% failure rate, and the majority of patients continue to complain of knee pain and activity limitations (42).
-
There may be some correlation between quadriceps strength and outcome.
-
There does not appear to be a strong association between subjective results and ligamentous stability.
-
A substantial number of patients with
isolated PCL injury will go on to develop degenerative changes of the
knee, particularly in the medial compartment, with time.
injury to the PCL, one must be convinced that the results of
reconstruction are superior to those of nonoperative management.
Unfortunately, there are no prospective randomized studies of operative
versus nonoperative treatment. Very few reports divide the patients
into isolated PCL versus combined PCL injuries. Bianchi (5) and Loos et al. (47)
noted mixed results in surgically treated isolated PCL insufficiency,
with the majority rated good or fair. Objective stability was often not
restored, but patients rarely complained of functional instability.
Richter et al. (61) reported an 8-year
follow-up of 53 patients with isolated and combined PCL instabilities
treated surgically with only 13% graded as nearly normal.
reported excellent results in 15 patients treated operatively for acute
PCL insufficiency, using ligament repair supplemented with a central
third patellar tendon autograft passed through bony tunnels. Although
this study offers good early results, it remains to be seen whether
there is a decrease in the long-term incidence of degenerative
arthritis.
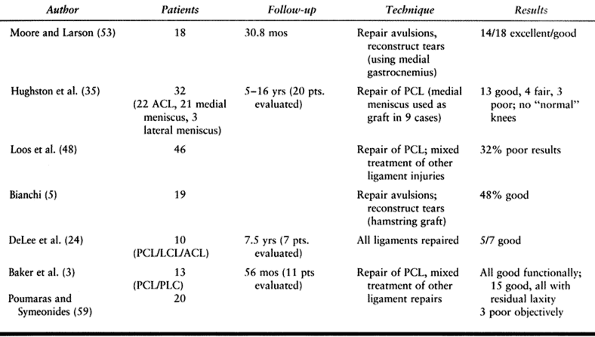
is usually a result of higher-energy injury but may also occur in
sports. These injuries result in gross instability of the knee;
therefore, most authors advocate operative treatment. For this reason,
there are no large long-term studies of the results of nonoperative
treatment; thus, it is impossible to determine whether surgical
management improves on the natural history of these combined injuries.
A wide variety of surgical approaches and tissues for augmentation and
reconstruction have been advocated.
injured PCL is superior to reconstruction. For reconstruction, they
recommended passing hamstring tendons through drill holes in the tibia
and medial femoral condyle, a procedure originally proposed by
Hey-Groves. McCormick et al. (51)
described reconstruction of a PCL and LCL injury using the tendon of
the popliteus passed through drill holes in the medial femoral condyle.
Soughmayd and Rubin (69) reported similar use of the semimembranosus tendon, preserving its distal attachment.
Despite the fact that the materials used for repair or reconstruction
were inferior to those used today, the results were a satisfactory
functional outcome in the majority of patients. The stability of the
knee after these procedures, however, is far from normal. Newer
anatomic methods of PCL reconstruction using more than one graft and
multiple femoral tunnels appear promising both biomechanically and
clinically, but results using these methods are still preliminary.
 |
|
Table 90.2. Surgical Treatment of PCL and Combined Ligament Injuries
|
from degenerative changes in the medial and patellofemoral compartments
or from instability with subsequent stretching of the secondary
restraints, particularly the posterolateral corner. There are few
reports of successful nonsurgical management of chronic lesions.
Hughston and Degenhardt (34), however,
demonstrated that nearly half of their patients obtained functional
stability with an aggressive rehabilitation program. These patients may
have had lesser degrees of instability, however (22).
using lateral meniscus as a graft, had mixed results in seven patients.
He advocated use of the meniscus because its length and size are
appropriate, it is not dependent on revascularization, and it is a
nearby intraarticular structure.
results of surgical treatment of chronic PCL insufficiency. Most of
these studies used the medial head of the gastrocnemius muscle or
meniscus as a substitute for the PCL; more recently, the central third
of the patellar tendon and hamstring autografts, as well as patellar
tendon and Achilles tendon allografts, have been used. Autografts
provide strong, readily available tissue without the risk of disease
transmission, whereas allografts have the advantage of no donor site
morbidity. These reconstructions emphasize placement of bony tunnels at
the sites of origin and insertion of the PCL, followed by insertion of
strong graft tissue to substitute for the ligament. Paulos (58) has described an arthroscopically
assisted technique using an Achilles tendon allograft.
 |
|
Table 90.3. Surgical Treatment of Chronic PCL Injuries
|
their experience in 33 patients with chronic PCL insufficiency in whom
reconstruction was done using the central third of the patellar tendon
as autograft. Twenty-three of 33 patients had evidence of degenerative
changes on preoperative radiographs. Of 13 patients available for
evaluation at a minimum of 2 years, four patients had associated ACL
repairs, one had repair of the posterolateral corner, and one had
repair of the MCL. All but two patients had good or excellent results.
associated laxity of the posterolateral structures, none specifically
mentioned the preoperative alignment of the limb. Several authors have
recently stressed the significance of varus alignment of the limb and,
more important, of a varus thrust during gait (14,26,37).
Soft-tissue procedures performed on the posterolateral corner in a limb
that has a varus thrust during gait will tend to stretch out and fail
over time. Despite the lack of studies demonstrating a long-term
benefit, many authors (26,37) feel that the most reliable procedure in such a setting is a high tibial osteotomy.
majority of properly selected individuals who undergo PCL
reconstruction for either isolated or combined injuries will obtain a
satisfactory subjective result. It appears that the majority of
individuals treated surgically for isolated PCL insufficiency will
return to their preinjury activity level and have subjective, but not
objective, stability. The results of surgery in combined PCL and other
major knee ligament injuries are less predictable but offer
satisfactory subjective results in the majority of patients. None of
these operations, however, reliably restores objective stability,
re-creates normal biomechanics, and prevents or delays the onset of
degenerative disease. Although newer methods of reconstruction using
multiple grafts to recreate both anatomic bundles of the PCL appear
promising both biomechanically and clinically, long-term outcomes are
currently unavailable.
than 400 patients for symptomatic isolated or combined PCL
insufficiency. The following outlines his indications and preferred
techniques.
injuries without surgery. For displaced fractures of the origin or
insertion of the PCL, we do an open reduction and internal fixation,
followed by early motion. Incomplete injuries with a 1 + drawer test
are a tear in continuity with interstitial lengthening, which can be
seen on MRI. These injuries often tighten as healing progresses, and
the posterior drawer test often diminishes to trace. Nonsurgical
treatment is appropriate.
with a complete disruption of the PCL. In the absence of other major
ligamentous injuries, we treat this injury without surgery. We advise
surgery only if the patient exhibits continued instability or medial
joint pain secondary to increased contact pressures in the medial
compartment. In the patient with medial joint line pain and normal
radiographs, we have found a technetium bone scan to be useful in
defining the source of the pain. Laxity of 3+ on posterior drawer
testing indicates injury to the PCL and secondary restraints, most
commonly the posterolateral corner structures. The treatment of these
injuries is discussed in the section below.
weeks of injury; early treatment permits primary repair rather than
reconstruction. Splint the knee until the acute pain subsides and
encourage active and active-assisted range of motion. Allowing 5 to 7
days to elapse from the time of injury until the time of surgery
permits the joint capsule to seal and avoids extravasation of
arthroscopy fluid into the leg from the injured posterolateral
structures during the arthroscopic part of the procedure. We repair the
PCL first, using the procedure outlined below, and then repair the PLC
structures through a standard lateral approach. If a satisfactory
primary repair is not possible, we do a biceps femoris tenodesis when
the biceps femoris tendon is intact. We perform posterolateral corner
reconstruction with an Achilles tendon allograft when the popliteus and
biceps tendon complex are irreparable. These techniques are described
below.
unrecognized knee dislocations, requiring thorough neurovascular
evaluation. Once the knee is reduced, splint it until the acute pain of
the injury subsides, in a few days. Begin active range of motion within
the limits of pain; once full extension and approximately 120° of
flexion are achieved, perform elective reconstruction of the ACL and
PCL. Reconstruct the ACL using an endoscopic technique with a patellar
tendon graft. Reconstruct the PCL using the technique described below.
Also see Chapter 91.
Grade I or II MCL injuries combined with PCL disruption can usually be
treated without surgery, and the emphasis is on early range of motion
and quadriceps strengthening. Grade III MCL injuries, characterized by
laxity to valgus stress applied at full extension, have injury to the
posterior oblique portion of the MCL as well as the anterior
longitudinal portion. We treat these injuries with splinting and early
range-of-motion exercises followed by early repair of the MCL and
posterior oblique ligament as well as reconstruction of the PCL. It is
important to ensure isometric repair of the MCL and posterior oblique
ligament to avoid creating a flexion contracture. Reconstruct the PCL
as described below.
may not have concomitant injury to the posterolateral structures. In
isolated PCL injuries, we prescribe a rehab program to strengthen the
quadriceps. Failure of this program to result in improvement of
symptoms after 3 months results in our offering the patient the option
of a PCL reconstruction. More commonly, the symptomatic patient also
has some laxity of secondary restraints, particularly the
posterolateral structures. In this setting we offer the patient a PCL
reconstruction as well as reconstruction of the posterolateral
structures using a tenodesis of a portion of the biceps tendon (9).
When this procedure has been performed previously and failed, or when
injury to the biceps tendon has occurred, we use an Achilles tendon
allograft. Both of these techniques are described below.
-
Two approaches for fixation of the displaced avulsion of the tibial insertion of the PCL have been advocated. Trickey (78)
recommends the direct posterior approach, which gives the best view of
the avulsion and allows easier internal fixation of the fragment with a
screw. Perform the surgery in conjunction with an arthroscopic
evaluation of the knee joint to allow treatment of any coexisting
pathology. -
The second approach is that of a combined
anterior medial arthrotomy and, when needed, a posterior medial
arthrotomy performed through a medial parapatellar skin incision, as
recommended by Hughston and associates (33,34). -
Tensile testing of knee ligament
preparations in which bony avulsions occurred suggests that plastic
deformation may occur within the ligament, resulting in a permanent
increase in length. If this is the case, any bony avulsion should be
countersunk at the time of fixation so that proper functional length
and isometricity will result. -
Deliver the PCL and the attached bony
avulsion through the intercondylar notch anteriorly. If there is a
ligament of Humphrey or Wrisberg, and it is blocking delivery of the
avulsion, transect it. -
Drill Steinmann pins from the anterior
tibia and direct them posteriorly into the bed of the avulsion site,
using the posteromedial capsulotomy to protect the deeper structures.
Pass right-angle curets through the intercondylar notch to deepen the
bed and allow countersinking of the avulsed fragment. -
Drill holes in the bone fragment and pass
#2 or #5 nonabsorbable sutures through them. Then put the sutures in
suture passers that have been placed through the holes previously
drilled in the tibia. Pull these sutures through the tibial drill holes
and tie them anteriorly while applying an anterior drawer with the knee
flexed to 90°. -
Then place the knee in a splint in full
extension, using the taut posterior capsule to prevent tibial dropback
from gravity, which will occur if the knee is held in flexion. Use the
splint for 6 to 8 weeks, but remove it daily to perform range-of-motion
exercises as outlined in the postoperative rehabilitation protocol.
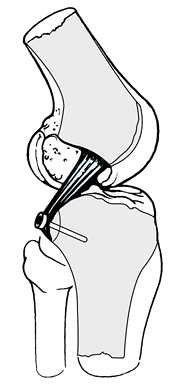
evidence to support the theory that the PCL acts primarily as two
separate functional bundles, with the anterolateral or anterocentral
portion of the ligament acting predominantly in flexion and the
posteromedial or posterior oblique portion of the ligament acting
predominantly in extension (15). Because of the
size of the sites of origin and insertion of the PCL, reconstruction of
the ligament using a single graft requires that only one of these two
bundles be reconstructed.
reconstruct the anterolateral or anterocentral portion of the ligament
and have recommended tensioning the graft at 90° of flexion (7,70).
This method reduces the posterior drawer as measured at the time of
surgery, but laxity seems to develop with time. We feel that the laxity
occurs as this portion of the PCL tightens with flexion and loosens
with extension. Because the majority of functional activities are
performed at less than 70° of flexion, the graft is subjected to
posterior stresses at flexion angles that are
significantly less than those at which it was tensioned. The result is cyclic fatigue and lengthening of the graft.
PCL contain some fibers that exhibit isometric behavior under certain
conditions, but placement of a 10- to 11-mm graft at the sites of
origin and insertion of these fibers results in a large portion of the
graft being outside the anatomic boundaries of the PCL.
pass two separate grafts through two separate femoral tunnels. These
grafts are then passed through a single tibial tunnel, with the
anterolateral/anterocentral graft being tensioned at 90° of flexion and
the posteromedial/posterior oblique graft being tensioned at 30° of
flexion, as described below.
Attention to detail and satisfactory performance of each of these steps
in the proper order is necessary to ensure a satisfactory result.
-
Step 1: Perform and document a complete examination of the knee under anesthesia.
-
Step 2: Perform an arthroscopic
inspection of the knee joint. Following the examination under
anesthesia, prepare and drape the knee and insert a 30° arthroscope via
a medial peripatellar portal. We do not use a tourniquet for any of our
repairs. Make this portal with a vertical stab wound along the medial
border of the patellar tendon at the level of the inferior pole of the
patella, with the knee in approximately 30° of flexion. Inspect the
knee in a systematic fashion, with particular attention to the medial
and patellofemoral compartments. Substantial involvement of these
compartments with degenerative changes is a relative contraindication
to PCL reconstruction. Inspect the intracondylar notch, and identify
the site of injury to the PCL. Chronic cases of PCL injury often show
only laxity of the ligament, which may be most evident as diminished
tension of the ligament at its insertion site into the tibia. There may
also appear to be abnormal laxity of the anterior cruciate ligament,
which is usually due to the abnormal posterior position of the tibia
and which is eliminated with placement of the proximal tibia into its
normal position with respect to the distal femur. -
Step 3: Harvest the graft from the
central third of the patellar tendon. Harvest of the graft at this
point in the procedure allows subsequent creation of a central portal
through the fat pad at the site of the defect in the patellar tendon,
and this portal will be used both to debride the remnant of the PCL
from the femur as well as to position the tibial guide for the tibial
tunnel. Extend the incision along the medial border of the patellar
tendon both proximally and distally and define the medial and lateral
borders of the patellar tendon. We prefer to harvest a 10-mm-wide graft
from the central third of the patellar tendon and take 10-mm-wide,
20-mm-long grafts from both the patella and the tibial tubercle.
Prepare the graft to allow easy passage through 10-mm tunnels and place
three #5 ethibond sutures through each end of the graft. -
Step
4: Debride the PCL remnant from the femur. Reinsert the arthroscope
into the knee through the medial peripatellar portal and introduce the
motorized shaver through the defect left by harvest of the patellar
tendon. Debride the origin of the PCL from the medial femoral condyle.
Preserve a portion of these fibers during the debridement; they are a
valuable landmark for later tunnel placement. Preserve the curved ridge
on the medial femoral condyle; it is also a helpful landmark because no
PCL fibers occur posterior to this point. -
Step 5: Debride the tibial insertion site
of the PCL through a posteromedial portal created at the level of the
junction of the proximal medial tibia with the posterior portion of the
medial femoral condyle. Advance the arthroscope into the intracondylar
notch and insert the motorized shaver through the posteromedial portal.
Debride with the shaver always facing toward the tibia to avoid
inadvertent damage to the posterior capsule or neurovascular
structures. Identify the tibial fovea. Define it using a curved shaver
placed through the central fat pad portal, followed by use of an angled
curet. Fully visualize the insertion site of the PCL to ensure proper
placement of the tibial guide pin and to avoid popliteal artery or
tibial nerve damage during subsequent drilling. -
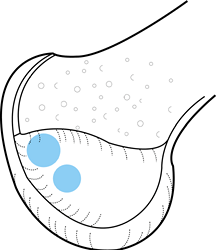
Step 6: Create the tibial tunnel (Fig. 90.12). Once the
P.2407
site of insertion of the PCL has been fully identified, drill a guide
pin from the anterior tibia, approximately 12 to 15 mm distal to the
site of graft harvest from the tibial tubercle into the center of the
insertion of the PCL. This entry point is quite important because it
creates a rather vertical tunnel that eases graft passage into the
tibia and also facilitates tensioning of the graft. It also avoids
creating an oblique hole at the exit site of the tunnel in the fovea.
Drilling a hole that enters medial or lateral to the tibial tubercle
creates an oblique exit hole in the tibial fovea and may result in
excessive medial or lateral placement of the graft. Run a 10-mm reamer
over the guide wire, followed by a 12-mm reamer. Keep the arthroscope
in the posteromedial portal during reaming to ensure that neither the
guide pin nor the reamers penetrate the knee joint. Once the tibial
tunnel has been reamed, debride the foveal site of any remaining
tissue. Next pass a #5 ethibond suture through the tibial drill hole
and out the central fat pad portal. This suture will be used during
passage of the graft into the tibial tunnel.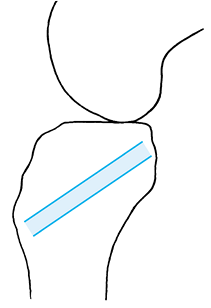 Figure 90.12.
Figure 90.12.
Ideal site for the tibial tunnel, which enters the tibia distal to the
site of graft harvest from the tibial tubercle and exits the proximal
tibia in the center of the insertion site of the PCL. -
Step 7: Creation of the femoral tunnels (Fig. 90.13 and Fig. 90.14).
Drill the femoral tunnels using the remaining fibers of the PCL on the
medial femoral condyle as a guide. We drill a 10-mm anterior/proximal
tunnel and an 8-mm posterior/distal tunnel, keeping the tunnels
separated by a 3- to 4-mm bony bridge. Use a 00 curette to make marks
in the medial femoral condyle at the desired tunnel sites. Insert the
anterior/proximal tunnel guide pin in the intracondylar notch at the
10:30 position in a left knee (the 1:30 position in a right knee),
approximately 6 mm posterior to the articular surface of the medial
femoral condyle. Place the posterior/distal tunnel approximately 5 mm
posterior and 5 mm distal to the anterior/proximal tunnel, taking care
to keep the tunnel sites within the anatomic site of origin of the PCL.
Both tunnels must be entirely anterior to the ridge in the medial
femoral condyle (see Step 4, above). Make an
incision over the vastus medialis muscle at the level of the adductor
tubercle and elevate the fibers of the vastus medialis anteriorly. Use
a vector guide to place a pin from the region of the adductor tubercle
into the desired position of the anterior/proximal tunnel and drill
with a 10-mm reamer over this guide. Drive a second guide pin from a
separate site in the medial femoral condyle into the desired site of
the posterior/distal tunnel and drill with an 8-mm reamer over this
guide pin. Make sure that an adequate bony bridge separates these two
tunnels. Pass two separate #5 ethibond sutures (which will be used
later for graft passage) through these tunnels and out the central fat
pad portal.![]() Figure 90.13.
Figure 90.13.
Ideal sites for the positions of the femoral tunnels, as viewed from
the side of a left knee with the lateral femoral condyle removed.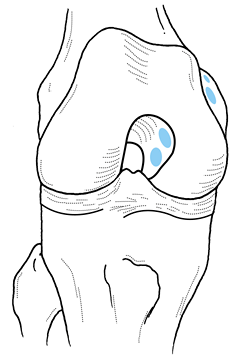 Figure 90.14. Ideal sites for the positions of the femoral tunnels, as viewed in a right knee.
Figure 90.14. Ideal sites for the positions of the femoral tunnels, as viewed in a right knee. -
Recently we placed the femoral tunnels
using endoscopic technique. Using this method, we marked the femoral
tunnel sites with the 00 currette as described above. We then use a
specially designed custom guide and flexible guide pins and reamers to
ream the two tunnels from the inside of the notch. Each tunnel is
reamed to a depth of 25 to 30 mm with the appropriate-sized reamer, and
a 4.5-mm drill is used to drill out the medial femoral cortex. The
grafts are then fixed using an Endobutton device (Smith and Nephew,
Andover, MA), allowing an entirely endoscopic reconstruction. -
Step 8: Harvest the hamstring or
quadriceps tendon graft that you will use to reconstruct the
posteromedial/posterior oblique portion of the PCL. Depending on your
preference, use either the quadriceps tendon or the semitendinosus
tendon. If you use the quadriceps tendon, make a separate vertical
incision centered over the superior pole of the patella. Identify the
quadriceps insertion into the patella and harvest an 8-mm-wide,
20-mm-long bone plug from the patella. Take an 8-mm-wide strip of
quadriceps tendon that runs the length of
P.2408
the
tendon. If the quadriceps tendon is excessively thick, harvest only the
superficial lamina of the tendon. Place a #5 nonabsorbable braided
suture through the tendon, which will be used to fix the tendon in the
tibia. -
The semitendinosus tendon may be used
instead of the quadriceps tendon. Harvest it in standard fashion, using
the distal end of the original incision. Double the tendon over itself
to form a double-stranded graft and fix it in the femur using either a
standard button or an Endobutton (if an endoscopic technique is chosen). -
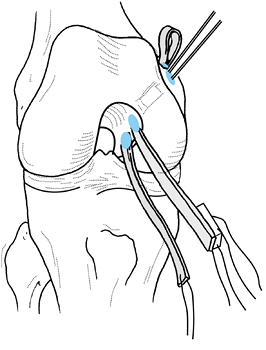
Step 9: Pass the grafts into the femur (Fig. 90.15).
Pass the grafts into the femoral tunnels using the previously placed
sutures through the central fat pad portal and the femoral tunnels.
Place the quadriceps or semitendinosus graft first and then fix it at
the medial femoral condyle using either a simple button (open
technique) or an Endobutton (endoscopic technique). Following femoral
fixation of this graft, pass the patellar tendon graft into the femur
and fix it in a similar fashion.![]() Figure 90.15. Passage of the hamstring and patellar tendon grafts into the femur in a right knee (see text for explanation).
Figure 90.15. Passage of the hamstring and patellar tendon grafts into the femur in a right knee (see text for explanation). -
Step 10: Pass the grafts into the tibia (Fig. 90.16 and Fig. 90.17).
Once both grafts have been fixed at the medial femoral condyle, pass
them through the central fat pad portal and into the tibia. Use the
previously placed suture through the tibial tunnel. A graft passer
(Depuy), which encloses the grafts and provides a smooth surface to
slide through the tibial tunnel, facilitates the process. We have found
that application of an anterior drawer at the time of graft passage
into the tibia helps the graft to turn the corner at the proximal part
of the tibial tunnel.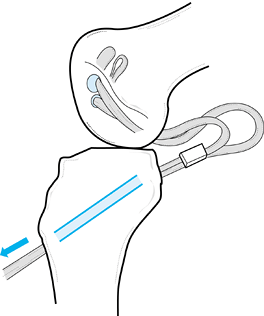 Figure 90.16. Passage of the hamstring and patellar grafts into the tibia in a left knee (see text for explanation).
Figure 90.16. Passage of the hamstring and patellar grafts into the tibia in a left knee (see text for explanation).![]() Figure 90.17.
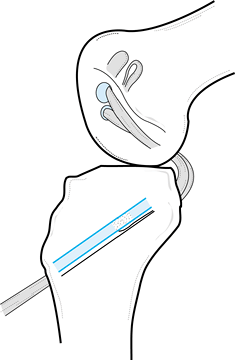
Figure 90.17.
Final view of a two-bundle PCL reconstruction as it would appear in a
left knee, seen from the lateral side with the lateral femoral condyle
removed. -
Step 11: Fix the grafts. The final step
in the procedure is fixation of the grafts to the tibia. Fix the
patellar tendon graft first. Tension it at 90° of flexion with an
anterior drawer test. Tie the sutures from the patellar bone plug over
a screw and washer and tighten them at the end of the procedure.
Tighten the quadriceps or hamstring graft at 30° of flexion and tie
these sutures over the same screw as those from the patellar tendon
graft. Then irrigate the wounds and close in routine fashion. Begin a
standardized rehab protocol on the first postoperative day. The patient
is usually discharged from the hospital on the second postoperative day.
-
Perform the procedure with a proximal
thigh tourniquet and the patient in the supine position. Prep the leg
and drape it free. Arthroscope the knee, and treat any injury to
meniscal or ligamentous structures before doing the posterolateral
surgery. -
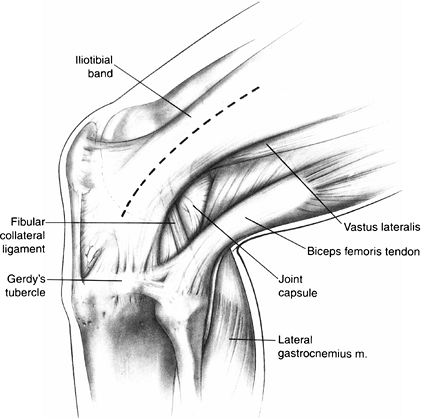
Flex the knee to 90° and make a lateral
curvilinear incision centered proximally over the lateral femoral
epicondyle and progressing distally to the interval between Gerdy’s
tubercle and the fibular head (Fig. 90.18).
Develop a posterior subcutaneous flap. Identify the common peroneal
nerve posterior to the biceps tendon and protect it throughout the
procedure.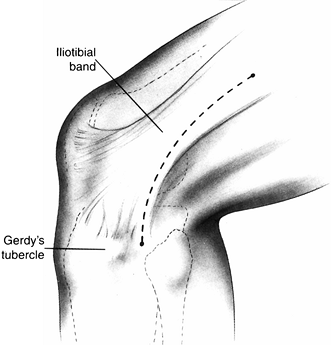 Figure 90.18.
Figure 90.18.
The skin incision and its relationship to the iliotibial band and
Gerdy’s tubercle. (From Martin SD, Clancy WG. Posterolateral
Instability of the Knee: Treatment Using the Clancy Biceps Femoris
Tenodesis. Op Tech Sports Med 1996;4:182, with permission.) -
Split the iliotibial band parallel to its
fibers from its midsubstance at the level of the lateral femoral
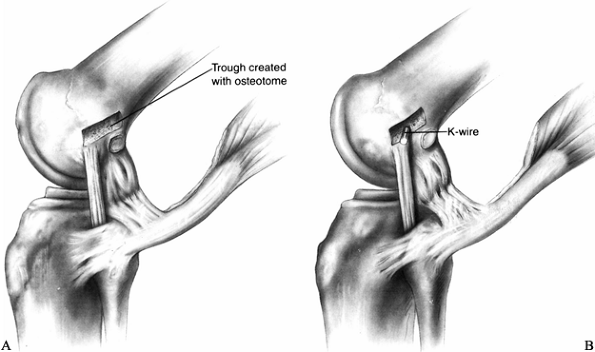
epicondyle to its distal insertion (Fig. 90.19).
Dissect the distal attachment of the iliotibial band free from the
intermuscular septum to permit later passage of the biceps tendon.
Strip any muscle fibers attached to the biceps femoris tendon distally
so as not to interfere with the tenodesis (Fig. 90.20).
Leave the lateral collateral ligament and its origin from the inferior
half of the lateral epicondyle undisturbed. Use a ¼-in. osteotome to
create a trough centered in the upper half of the lateral epicondyle,
measuring 1 cm in width and 3 cm in length. Insert a 3.2-mm guide wire
for a 7.0-mm cannulated cancellous screw into the trough, starting at
the point anterior to the most proximal edge of origin of the lateral
collateral ligament (Fig. 90.21). Drill the wire medially
P.2410P.2411
and slightly cephalad to avoid any tunnels used in cruciate ligament reconstruction.![]() Figure 90.19.
Figure 90.19.
Proper level of division of the iliotibial band for exposure of the
lateral epicondyle. (From Martin SD, Clancy WG. Posterolateral
Instability of the Knee: Treatment Using the Clancy Biceps Femoris
Tenodesis. Op Tech Sports Med 1996;4:182, with permission.)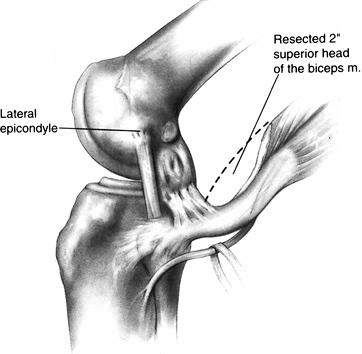 Figure 90.20. Relationship of the peroneal nerve to the biceps tendon. Dotted line
Figure 90.20. Relationship of the peroneal nerve to the biceps tendon. Dotted line
indicates the level of resection of the superior head of the biceps
muscle. (From Martin SD, Clancy WG. Posterolateral Instability of the
Knee: Treatment Using the Clancy Biceps Femoris Tenodesis. Op Tech Sports Med 1996;4:182, with permission.)![]() Figure 90.21. A: Proper exposure of the lateral structures and location of the bony trough in the superior half of the lateral epicondyle. B:
Figure 90.21. A: Proper exposure of the lateral structures and location of the bony trough in the superior half of the lateral epicondyle. B:
Proper placement of the K-wire in the bony trough. (From Martin SD,
Clancy WG. Posterolateral Instability of the Knee: Treatment Using the
Clancy Biceps Femoris Tenodesis. Op Tech Sports Med 1996;4:182, with permission.) -
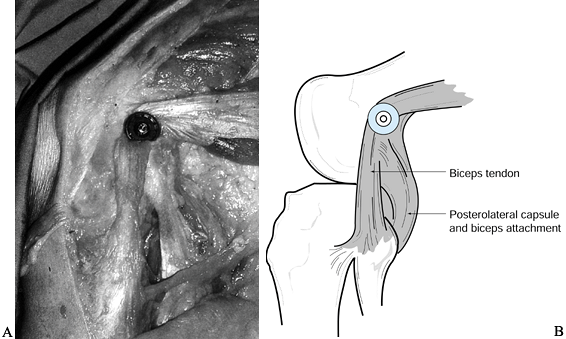
Pass the biceps tendon beneath the
inferior portion of the iliotibial tract and over the guide wire. Place
a retractor around the transferred tendon to protect it from being cut
by the threads of the screw (Fig. 90.22).
Tighten the cancellous screw and a spiked ligament washer while
tensioning the graft with the knee flexed to 30° and the tibia
internally rotated (Fig. 90.23). The tip of the
screw should engage the opposite cortex. Close the wound in routine
fashion over a drain and place the leg in an extension splint. Allow
weight bearing to tolerance and begin range-of-motion exercises at 6
weeks. Remove the screw and washer at 6 months.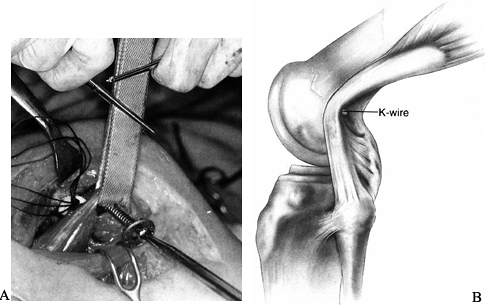 Figure 90.22. A: Intraoperative photograph showing protection of the biceps tendon with a retractor during screw placement. B:
Figure 90.22. A: Intraoperative photograph showing protection of the biceps tendon with a retractor during screw placement. B:
Proper location of the biceps tendon transfer to the bony trough. (From
Martin SD, Clancy WG. Posterolateral Instability of the Knee: Treatment
Using the Clancy Biceps Femoris Tenodesis. Op Tech Sports Med 1996;4:182, with permission.)![]() Figure 90.23. A: Intraoperative photograph showing transferred tendon fixed with a screw and spiked washer. B:
Figure 90.23. A: Intraoperative photograph showing transferred tendon fixed with a screw and spiked washer. B:
Transfer and fixation of biceps tendon leads to advancement of
posterolateral capsule. (From Martin SD, Clancy WG. Posterolateral
Instability of the Knee: Treatment Using the Clancy Biceps Femoris
Tenodesis. Op Tech Sports Med 1996;4:182, with permission.)
-
Use the same incision as for biceps
tenodesis. Divide the midportion of the iliotibial tract longitudinally
in similar fashion. Retract the biceps tendon and lateral head of the
gastrocnemius from the posterior tibia and fibula. -
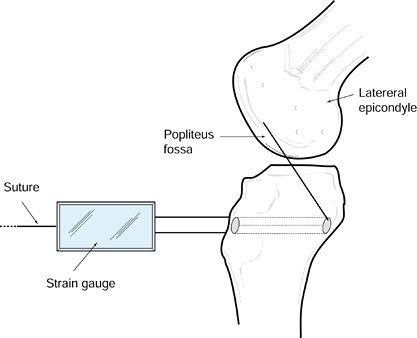
Drive a Kirschner (K-) wire through the
tibia from anterior to posterior, entering just below Gerdy’s tubercle
and exiting just medial to the midsection of the fibular head at the
posterolateral corner of the tibia. This maneuver will place the tunnel
at the musculotendinous junction of the popliteus (Fig. 90.24).
Drive a K-wire into the lateral epicondyle at the anterior superior
aspect of the popliteal fossa. Use a suture through the tibial tunnel
and then tie it to the K-wire to determine isometry as the knee is
taken through a range of motion. The K-wire is ideally located when
excursion of the suture is 3 mm or less through a full range of motion (Fig. 90.25). Once proper tunnel location is determined, drive a 10-mm reamer to a depth of 25 mm in the lateral epicondyle.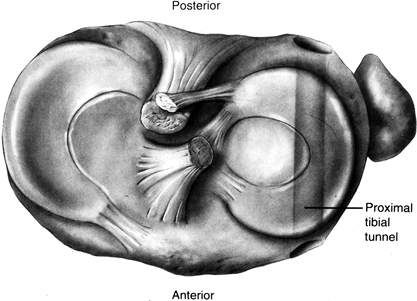 Figure 90.24.
Figure 90.24.
Proper orientation of tibial tunnel for posterolateral corner
reconstruction. (From Martin SD, Clancy WG. Posterolateral Instability
of the Knee: Treatment Using the Clancy Biceps Femoris Tenodesis. Op Tech Sports Med 1996;4:182, with permission.)![]() Figure 90.25.
Figure 90.25.
Proper placement of K-wire at the superior aspect of the popliteal
fossa and proper orientation of the tibial tunnel in the sagittal
plane. (From Martin SD, Clancy WG. Posterolateral Instability of the
Knee: Treatment Using the Clancy Biceps Femoris Tenodesis. Op Tech Sports Med 1996;4:182, with permission.) -
Fashion an Achilles tendon allograft with the calcaneus bone plug measuring 10 × 25 mm. Weave #5 nonabsorbable
P.2412
suture through the proximal end of the tendon to assist in graft
passage. Fix the bone plug in the lateral epicondyle with a 7 × 25-mm
interference screw. Pass the tendon medial to the iliotibial band and
through the tibial tunnel from posterior to anterior. Put the knee
through a range of motion to pretension the graft. Fix the graft to the
proximal tibia with the knee flexed 30° and internally rotated. Provide
fixation with two staples (Fig. 90.26) or with the #5 suture tied over a screw and washer if the graft is too short.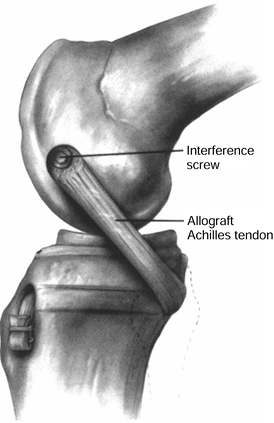 Figure 90.26.
Figure 90.26.
Posterolateral allograft reconstruction with interference screw
fixation on the femoral side and staple fixation on the tibial side.
(From Martin SD, Clancy WG. Posterolateral Instability of the Knee:
Treatment Using the Clancy Biceps Femoris Tenodesis. Op Tech Sports Med 1996;4:182, with permission.)
-
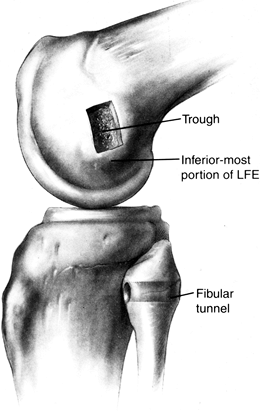
If significant varus laxity exists after
reconstruction of the posterolateral corner, reconstruct the fibular
collateral ligament using patellar tendon allograft or autograft. -
Fashion a 10-mm graft with a 20- to 25-mm
bone plug. Make a bony trough of similar dimensions in the lateral
epicondyle. The inferior aspect of the trough should not extend beyond
the inferior aspect of the lateral epicondyle (Fig. 90.27).
Alternatively, a 10-mm tunnel can be created at the lateral epicondyle.
Secure the bone block with a screw and washer for trough fixation or a
7-mm interference screw for tunnel fixation.![]() Figure 90.27.
Figure 90.27.
Proper location of bony trough at the lateral femoral epicondyle for
fibular collateral ligament reconstruction. Also note site of tunnel
placement through the fibular head. (From Martin SD, Clancy WG.
Posterolateral Instability of the Knee: Treatment Using the Clancy
Biceps Femoris Tenodesis. Op Tech Sports Med 1996;4:182, with permission.) -
Make a transverse tunnel from anterior to posterior at the base of the fibular head (Fig. 90.27)
with a ¼-in. drill bit. Protect the peroneal nerve during this
procedure. Split the 10-mm graft longitudinally into two 5-mm strips
and pass #0 suture through the tendon ends to allow graft passage. Pass
the free tendon ends in opposite directions through the fibular tunnel
and suture
P.2413
the
ends to one another over the fibular head while applying a valgus force
to the knee. Then close the longitudinal rent in the graft, which
allows further tensioning (Fig. 90.28).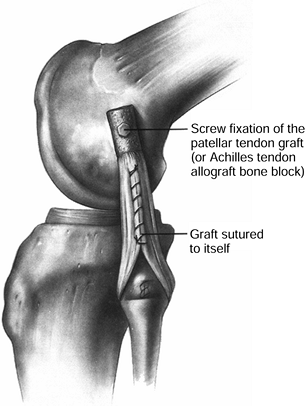 Figure 90.28.
Figure 90.28.
Completed fibular collateral ligament reconstruction with screw
fixation of bone plug on the lateral femoral condyle and suturing of
tendon ends together after graft passage through the fibular head.
(From Martin SD, Clancy WG. Posterolateral Instability of the Knee:
Treatment Using the Clancy Biceps Femoris Tenodesis. Op Tech Sports Med 1996;4:182, with permission.)
reconstruction into five phases: (a) immediate postoperative phase
(first 2 weeks after surgery), (b) maximum protection phase (weeks 2 to
6), (c) controlled ambulation phase (weeks 6 to 12), (d) light activity
phase (weeks 12 to 16), and (e) return-to-activity phase (weeks 16 to
24).
patient to bear 50% of weight as tolerated using two crutches and to
perform ankle and hip exercises and knee extensions from 60° to 0°.
weight bearing, multiangle quad isometrics at 60°, 40°, and 20°, leg
press and squats from 0° to 60°, and well-leg bicycling. By week 4,
range of motion should be to 90°, and bicycling can be encouraged for
range of motion and endurance. Begin pool exercises at week 5.
strength by initiating swimming, closed-kinetic-chain rehabilitation,
and a stretching program. By week 12, begin lateral step-ups, cycling
for endurance (30 minutes), hamstring curls from 0° to 60° with low
weight, and a walking program.
exercises and allows a light running program. By 5 to 6 months after
the surgery, the patient should be performing plyometric exercises as
well as agility and balance drills and may return to sport when
KT-2000, isokinetic testing, and functional testing are satisfactory.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
WC, Draganich LF, Pyevich M, Reider B. The Effect of Femoral Tunnel
Position and Graft Tensioning Technique on Posterior Laxity of the
Posterior Cruciate Ligament-Reconstructed Knee. Am J Sports Med 1995;23:424.
WG, Shelbourne KD, Zoellner GB. Treatment of Knee Joint Instability
Secondary to Rupture of the Posterior Cruciate Ligament. J Bone Joint Surg 1983;65A:310.
DE, Warren RF, Warner JJP. The Posterior Cruciate Ligament and
Posterolateral Structures of the Knee: Anatomy, Function and Patterns
of Injury. Instr Course Lect 1991;40:249.
DM, Stone ML, Barnett P, Sachs R. Use of the Quadriceps Active Test to
Diagnose Posterior Cruciate Ligament Disruption and Measure Posterior
Laxity of the Knee. J Bone Joint Surg 1988;70A:386.
DL, Torzilli PA, Warren RJ. The Role of the Posterolateral and Cruciate
Ligaments in the Stability of the Human Knee: A Biomechanical Study. J Bone Joint Surg 1987;69A:233.
TE, Noyes FR, Lee MD. Diagnosis of Complete and Partial Posterior
Cruciate Ligament Ruptures. Stress Radiography Compared with KT-1000
Arthrometer and Posterior Drawer Testing. Am J Sports Med 1997;25:648.
KA, Otis JC. Anteroposterior Tibiofemoral Displacements During
Isometric Extension Efforts. The Roles of External Load and Knee
Flexion Angle. Am J Sports Med 1985;13:254.
JC, Hawkins RJ, Willis RB, Danylchuk KD. Tension Studies of Human Knee
Ligaments. Yield Point, Ultimate Failure, and Disruption of the
Cruciate and Tibial Collateral Ligaments. J Bone Joint Surg 1976;58A:350.
GE, Palmitier RA, An KN, Chao EYS. Comparison of Tibiofemoral Joint
Forces During Open-Kinetic-chain and closed-kinetic-chain exercises. J Bone Joint Surg 1993;75A:732.
Cruciate Ligament Reconstruction Using Fresh Frozen Allograft Tissue:
Indications, Techniques, Results and Controversies. Presented as
a Scientific Exhibit at the Annual Meeting of The American Academy of
Orthopaedic Surgeons, San Francisco, February 1993.
WC, Bagg RJ, Kennedy CW Jr, Leudins CA. Reconstruction of the Posterior
Cruciate Ligament. Preliminary Report of a New Procedure. Clin Orthop 1976;118:30.
JM, Bergfeld JA. Long-term Results of Nonoperative Treatment of
Isolated Posterior Cruciate Ligament Injuries in the Athlete. Am J Sports Med 1986;14:35.
M, Kiefer H, Hehl G, Kinzl L. Primary Repair for Posterior Cruciate
Ligament Injuries. An Eight-Year Follow-up of Fifty-Three Patients. Am J Sports Med 1996;24:298.
RA Jr, Shelbourne KD. Diagnosis of Posterior Cruciate Ligament Injuries
and Indications for Nonoperative and Operative Treatment. Op Tech Sports Med 1993;2:99.
RA Jr, Shelbourne KD, McCarroll JR, et al. The Accuracy of the Clinical
Examination in the Setting of Posterior Cruciate Ligament Injuries. Am J Sports Med 1994;22:550.
KD, Mesko JW, McCarroll JR, et al. Combined Medial Collateral
Ligament–Posterior Cruciate Rupture. Mechanism of Injury. Am J Knee Surg 1990;3:41.
KD, Rubinstein RA. Isolated Posterior Cruciate Ligament Rupture: An
Unusual Mechanism of Injury. A Report of 3 Cases. Am J Knee Surg 1993;6:84.
MJ, Warren RF, Ortiz GJ, et al. The Effects of Sectioning of the
Posterior Cruciate Ligament and the Posterolateral Complex on the
Articular Contact Pressures within the Knee. J Bone Joint Surg 1993;75A:694.
JE, Antich TJ, Perry J, Moynes D. Functional Analysis of Untreated and
Reconstructed Posterior Cruciate Ligament Injuries. Am J Sports Med 1988;16:217.
T. Avulsion Fracture of the Tibial Attachment of the Posterior Cruciate
Ligament. Indications and Results of Delayed Repair. Clin Orthop 1979;143:107.
EL. Injuries to the Posterior Cruciate Ligament. Diagnosis and
Treatment of Early Injuries and Reconstruction of Late Instability. Clin Orthop 1980;147:76.
AD, Marks PH, Fowler PJ, Munro TG. Occult Post-traumatic Osteochondral
Lesions of the Knee: Prevalence, Classification, and Short Term
Sequelae Evaluated with MR Imaging. Radiology 1991;178:271.