GUNSHOT, CRUSH, INJECTION, AND FROSTBITE INJURIES OF THE HAND
III – THE HAND > Trauma > CHAPTER 45 – GUNSHOT, CRUSH, INJECTION,
AND FROSTBITE INJURIES OF THE HAND
are frequently life changing. Our hands define our vocations,
avocations, pleasures, and even expression. Treatment of these
injuries, then, must take into account the person whom the tragedy has
struck and use all measures necessary to maximize the return toward
normalcy.
different structures in efficient juxtaposition. Planning the treatment
of injuries must take into account the rehabilitation of each
structure. For example, a crushing injury at the metacarpal level with
dorsal skin loss, extensor tendon injury, and fractures may require
stable bony fixation for early mobilization, possible free tissue
transfer for skin coverage and tendon gliding, and even possible
combination flaps such as the dorsalis pedis flap to include extensor
tendons. Isolated treatment of the bony injury may
result
in a favorable radiograph but would certainly compromise hand function.
Treatment of the soft tissue defect without stable bony fixation would
be equally disastrous.
as “go to the bone and stay there” to better appreciate the importance
of soft tissue treatment and healing. Levin coined the term orthoplastic
to emphasize the interplay between soft tissue management and bone
reconstruction. Reconstruction of the soft tissue envelope demands
definition of the layers deficient as well as the size of the defect
before outlining a plan that will treat both the bone and soft tissue
to the best advantage (38).
These were divided into three groups based on the timing of the
free-flap transfer, ranging from less than 72 h to greater than 3
months. He showed that early coverage resulted in a lower rate of
infection, fewer hospital days and operations, and earlier bone
healing. Drawbacks of the study include the wide range of the middle
group (72 h to 3 months). The study did emphasize the supreme
importance of adequate initial debridement, which often will obviate
later debridement and in some cases allow soft tissue coverage at the
initial operation (24).
paint injection, and frostbite is reviewed in this chapter, beginning
with emergency room evaluation and treatment, surgical planning,
staging, options, and, finally, postoperative rehabilitation.
history has made its greatest advances in wartime. More than half of
war wounds involve the extremities, and a fifth of these are hand
wounds (11). Regrettably, injuries once
commonplace only in times of war are now regular and expected
occurrences in emergency rooms around the country. Specific injuries of
the hands are seldom themselves life threatening but are frequently
associated with other wounds and, as a result, are often complicated by
delay in treatment. Maximal function and minimal long-term disability
will be achieved only with thoughtful treatment, couched in a basic
knowledge of ballistics and wound personality, appropriate emergency
care, and reconstruction options.
basis of the velocity of the bullet, with the difference between low
and high velocity ranging from 1,100 to 3,000 ft/s (18,32).
Velocity increases only the potential for increased tissue disruption;
other factors determine the reality of that potential (fragmentation,
yaw, missile shape, and deformation). Another popular reference is to
the kinetic energy of the bullet, an immeasurable concept that reveals
nothing of the magnitude, type, or location of tissue damage or the
forces that cause tissue disruption and distracts from these crucial
elements. Tissue damage from bullet projectiles occurs through two
mechanisms: first, tissue crush by the projectile and any resultant
secondary projectiles; and second, tissue stretch from temporary
cavitation, which occurs in a radial fashion along the course of the
bullet (19,20 and 21,32). Direct tissue damage from the projectile is increased by deformation of the bullet, fragmentation, and bullet yaw and tumble.
itself. Tissues such as skeletal muscle have a high level of elasticity
and are therefore less affected by temporary cavity displacement
pressure (4 atm) than less elastic tissue such as brain, liver, or
spleen. Indeed, most injury to extremities is the result of structures
directly hit by the intact bullet, bullet fragments, or secondary
missiles (19,32,33).
Since the Hague Conferences of 1899 and 1907, full metal jacketed
bullets were adopted by the military of all major countries to limit
unnecessary suffering of war (53). These
standards are obviously not applied to civilian weapons. If a full
metal jacketed bullet and a soft or hollow point bullet are fired from
the same rifle, the latter will result in a much more dramatic wound
from both increased yaw and deformation.
Round projectiles have poor ballistic properties, losing much of their
energy in flight through the air. Their wounds are then reflective of
the increased mass of the projectiles, not their high velocity. The
greater the choke of the barrel, the less spread of pellets at any
given distance. Decreasing the choke (“sawed-off shotgun”) increases
both the ability to conceal the weapon and the ability to hit multiple
targets with one shot as a result of increased dispersion of the
pellets.
 |
|
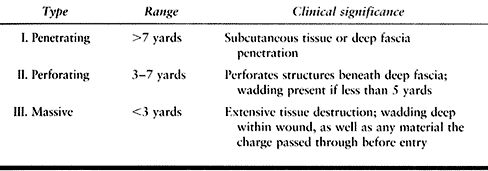
Table 45.1. Classification of Shotgun Wounds
|
increase in muzzle velocity possible with a longer barrel. The M-16
rifle represented a trend toward projectiles of lower weight and very
high velocity (increasing the rounds that a soldier may carry). The
resultant poor ballistic coefficient and high drag of the lighter
bullet demands a closer target but results in greater tissue
destruction, maximizing the wound channel from its high yaw angle after
contact (3). It is possible to have both a
small entrance and exit wound even in the setting of massive tissue
destruction as the bullet yaws early and rights itself for exit. Damage
by a military rifle before it yaws cannot be distinguished from that
caused by a handgun, even by experts (18).
The shorter barrel results in lower bullet velocity and less accuracy.
A revolver is distinguished from a pistol
by
its cylinder versus the vertical magazine in the handle of the pistol.
Innovation in the characteristics of the bullets has dramatically
changed the level of tissue destruction even in the setting of
decreased velocity. For example, a Glasser safety slug is a lightweight
hollow copper bullet filled with number 12 birdshot pellets with a top
sealed with a plastic cap. It ruptures on contact, releasing pellets in
every direction, each of which rapidly decelerates, releasing its
energy quickly (3).
according to 1994 estimates. This represents 200 million guns, 60
million handguns, and 3 million assault rifles (50).
Washington and Lee reported in 1995 that 14 children younger than 19
years old will die in gun-related incidents each day in the United
States (70). Ordog reported on 16,316 patients
with 18,349 extremity gunshot wounds treated in Los Angeles from 1978
to 1992. The mean age was 24 years old, and 94% were male; 83% were
from handguns, 6% rifles, and 6% shotguns. The majority of shots
originated from a passing car. Thirteen percent of upper extremity
wounds were associated with a vascular injury, and a vascular injury
was four times more likely when the patient had a “major” fracture
versus a “minor” or no fracture (50).
Charlotte, NC, reviewed 218 gunshot fractures from 1985 to 1989. Male
victims again predominated at 91%, 79% were uninsured, and 65% could be
connected with the use of illicit drugs; medical charges averaged
$13,108 (27). Another Los Angeles study
reviewed gunshot wounds to the hands specifically, with 91 wounds
representing 78 men and 13 women. Multiple injuries were present in 56
(58.2%), and 11% involved shotguns. The authors noted a greater injury
with hollow point, fluid-filled, or partially jacketed bullets even in
the setting of lower velocity (54). Further
experience at the Martin Luther King, Jr., General Hospital in Los
Angeles catalogued 387 children who sustained gunshot wounds, 117 of
whom suffered extremity wounds (70). Finally,
at Grady Memorial Hospital in Atlanta, of 72 gunshot wounds, the most
consistent region involved was the hand and wrist (34).
wounds (GSW) of the hand based on the experience at the Martin Luther
King, Jr., General Hospital in Los Angeles (Table 45.2) (54).
 |
|
Table 45.2. Classification of GSWs to the Hand
|
-
Adhere to the principles of advanced
trauma life support. More than half of gunshot wounds to the hand are
associated with multiple gunshot injuries (54).
In Ogden’s study of extremity gunshot wounds, 6% of through-and-through
extremity wounds were associated with missile penetration of another
“major” body area. Do not allow the obvious hand injury to distract
from diagnosing a possibly life-threatening occult wound. Disrobe the
patient and inspect all surfaces, including the back. -
Begin specific examination of the wounded
upper extremity with assessment of entrance and exit wounds, their size
and character, swelling and deformity in the region between, and a
mental note of vital structures potentially involved in the path of the
bullet. -
Check pulses and circulation by Allen’s
test. With the high collateral flow in the distal upper extremity, the
mere presence of pulses does not rule out a significant vascular injury
proximally. Avoid tourniquets for control of brisk bleeding; rather,
apply direct pressure. Resist the urge to clamp or coagulate blindly,
as future vascular and nerve repair will likely be compromised by
inadvertent injury to underlying structures. If an extremity wound is
ever fatal, it is most likely related to initial blood loss (64). -
Perform a neurologic examination
documenting the function in the radial, median, and ulnar nerves.
Document profundus and superficialis tendon function as well as the
bony architecture of the hand. -
Following examination, gently rinse with saline solution and apply a moist saline dressing and splint as appropriate.
-
Administer intravenous first-generation cephalosporin or ceftriaxone.
-
Give a tetanus booster in patients with
known active immunity and tetanus toxoid plus human recombinant
antitoxin to the nonimmunized, according to the guidelines of the
Committee on Trauma of the American College of Surgeons. -
Bullet sterilization from the heat of firing was disproven in 1892 (18).
The bullet will carry bacteria from the body surface and any other
tissue through which it passes (such as colon). The most important
cause of death from missile wounds on the battlefield in the
preantibiotic era was streptococcal bacteremia, not clostridial
myositis (19). -
Treatment of low-velocity gunshot wounds
following emergency room treatment is controversial, with
recommendations ranging from a minimum of 24 to 48 h coverage with IV
cephalosporin to oral antibiotics given to outpatients only after
manifestation of signs and symptoms of infection (29,34,50,70).
Marcus advises that “the judgment of the physician performing the
initial examination is the most important factor determining the
appropriate treatment of a gunshot wound”(42). See the discussion that follows on surgical indications. -
Radiographically image the entire
involved extremity and do a chest radiograph as well. Complex
associated fractures may then be further imaged using CT, especially
with involvement of the carpus. -
Do not overlook compartment syndrome,
other associated gunshot wounds, and missile emboli. Suspect
compartment syndrome of the hand when the hand is swollen. This
presentation may be confused by associated skeletal and nerve injury.
The hand will almost invariably be held in an intrinsics minus
position. Naidu and Heppenstall find that excruciating pain with
passive motion of the MCP joint of the involved digit is the most
sensitive clinical indicator (49). -
Measure intracompartmental pressures.
Recommendations for fasciotomy vary, ranging from intracompartmental
pressures of over 30 mm Hg up to pressures within 30 mm Hg of the
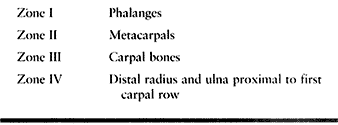
diastolic systemic pressure (26,52). There are 10 separate compartments in the hand (Table 45.3).
Most frequently, release is necessary of one or two dorsal
compartments, the hypothenar, and the thenar, with release of the
transverse carpal ligament. The finger is enclosed in a tight investing
fascia supported by unyielding volar skin. Occasionally midaxial finger
incisions are also required to avoid tissue loss (49,52). The reader is referred to Chapter 13 and Chapter 65 for further discussion of compartment syndromes in the upper extremity.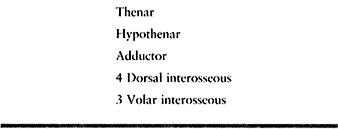 Table 45.3. Compartments of the Hand
Table 45.3. Compartments of the Hand -
Missile emboli most frequently occur with
close-range shotgun injuries. They should be suspected when the primary
wound cannot account for peripheral ischemia. Embolization has also
been reported with 22-caliber missiles; the energy of the bullet is
spent entering the vessel, and it is then swept along in the flow of
blood until the lumen size limits further travel. Reported distant
emboli sites include the posterior tibial artery, middle cerebral
artery, popliteal artery, femoral artery, anterior tibial artery, and
the ulnar artery (5,73).
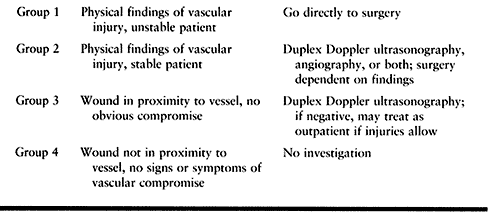
In addition, multiple wounds in the same extremity and potential
arterial compromise may merit arteriography if the condition of the
patient allows, to better plan the surgical approach and intervention.
 |
|
Table 45.4. Ordog’s Indications for Vascular Imaging
|
determined by the severity of the injury. Very often, little
information is available regarding the type of weapon, the
range
at which the injury occurred, or the specific ammunition used. The
treating physician must base a reasonable decision not on conjecture as
to the velocity of the bullet but on the characteristics of the wound
under examination. As previously mentioned, it is possible to have
small entrance and exit wounds in the presence of massive underlying
soft tissue and bony destruction. This is evidenced by massive
swelling, loss of bone stability, and neurologic and vascular deficits,
which require emergent surgery. Small entrance and exit wounds in the
absence of these clinical signs may, in contrast, be treated with
simple wound cleansing and dressing on an outpatient basis. Hampton’s
review of 368 bullet wounds of the extremities, more than half of which
had associated fracture, showed that over 300 did not require
debridement, and no sepsis resulted (28).
wounds of the extremities and grouped them on the basis of both
debridement technique and presence or absence of fracture. Nonoperative
treatment was defined as excision of wound margins under local
anesthesia in the emergency room and wound irrigation with saline, with
or without antibiotics. He found no difference in outcomes between
those treated with surgical debridement and antibiotics and those
without aggressive treatment (42).
When they are lodged in the hand, their mere size may necessitate
removal. When retained around joints or joint areas where exposure to
synovial fluid and abrasion is possible, excision is also recommended
to avoid mechanical damage as well as lead arthropathy (23).
When they are lodged in the physis of a child, removal is mandatory.
Washington and Lee reviewed their experience with gunshot wounds in
children and reported that all physeal arrests were easily predicted on
the admission radiographs (70). It was
previously thought that the physis was highly susceptible to
high-velocity injury if the track of the bullet was nearby.
exploration in and of itself, as many are neurapraxias. Phillips
recommends no exploration before 3 months, then electrical studies to
establish the need for repair or grafting (54).
-
Acute debridement serves two purposes: to
remove nonviable tissue and foreign debris, and to decompress the
wounded hand. With the close juxtaposition of many crucial structures
in the hand, when there is any doubt about the viability of an
important structure, delay excision until the second debridement. -
Debride skin conservatively with little or no excision of skin (31). Extend small wounds for adequate exposure of injured structures.
-
Bony fragments may be retained, even if detached, unless grossly contaminated.
-
There is rarely a good argument to be
made for primary closure of wounds following the initial debridement.
Sherman studied shotgun wounds and their complications and found that
31% of wounds primarily closed following debridement required further
operative care for infection (61). -
Manage wounds open with moist dressings and splints.
-
Carry out a second debridement 48 to 72 h
following the first. Debridement is a learned art, as emphasized by
Brown, who recommends: “Don’t get wounded in the first 2 months of the
war” (11). -
Complete or near amputations of the hand
or digits rarely are appropriate for replantation. Salvage of skin,
tendons, bone, nerve tissue, and even digits themselves
P.1440
may
be valuable in reconstruction of the remainder of the injured limb. The
viable skin covering near-amputations may be valuable in skin coverage. -
Skeletal stability is crucial for soft
tissue healing as well as for mobilization of the hand to hasten
rehabilitation. Restore both the longitudinal and transverse arches of
the hand, even at the time of the initial debridement. In cases of bony
loss, use Kirschner wire bayonet spacers, cross-pinning of metacarpals,
or external fixation to achieve stability pending secondary bony
reconstruction. -
Nerve repair in the hand may be carried
out at the time of initial or secondary debridement, or the nerve ends
may be marked for later repair or grafting. Stein and Strauss recommend
primary repair only in cases of clean transection, whereas Hennessy
advocates primary repair whenever possible, using nerves from nonviable
parts of the injured hand when available (31,64). -
When vascular repair is necessary, gain
control of the injured vessel both proximally and distally with
adequate exposure. In the repair of the radial or ulnar artery in the
distal forearm following a close-range shotgun wound, use caution to
avoid peripheral embolization of pellets. Vascular repair almost always
will require segmental resection, as the zone of injury often extends
beyond the area visibly damaged. Vein grafting is usually necessary (5,26,32,50,61,64,73). -
Skin coverage options after the final
debridement include delayed primary closure, healing by secondary
intent, local flaps, or distant flaps. -
Postoperatively, support the wounded
tissues with a dressing firm enough to eliminate dead spaces without
inhibiting venous return. The dressing absorbs blood and exudates,
provides a barrier to further contamination, increases patient comfort,
and facilitates mobilization of uninjured parts. Place the hand in an
intrinsics-plus position unless that compromises the repairs. Elevate
the limb and begin early range-of-motion exercise for the shoulder and
elbow to avoid stiffness.
understanding of his role and responsibility as an active member of the
rehabilitation team. Begin patient education after application of the
first postoperative dressing or in the emergency room for those treated
nonoperatively. Mobilization of all parts possible, edema control,
wound care, and splinting in functional positions are all elements of
success in returning the injured limb to useful function.
associated gunshot wounds, underestimated vascular injury, and peri- or
intraarticular lead particles. Lead near or in joints will be dissolved
over time by acidic synovial fluid and incite a proliferative
synovitis, which may result in focal articular cartilage erosion and
degenerative arthritis. Radiographically, lead may resemble
chondrocalcinosis, with metallic not calcific deposits. Remove
intraarticular lead particles soon after injury. If lead arthropathy is
suspected, measure serum lead levels. Delay surgical procedures until
levels have been reduced with chelating agents such as D-penicillamine (23).
impairment following low-velocity gunshot wounds to the hand was loss
of motion secondary to fractures and joint disruption, and this
surpassed the disability from infection and tendon, nerve, or vascular
injury. Most marked losses involved the proximal interphalangeal (PIP)
joint. They strongly recommend stable internal fixation with early
mobilization (16).
the hand is to treat individually each wound rather than mindlessly
following protocols established for high- versus low-velocity weapons.
impact associated with these injuries. Sensitivity to these issues and
cooperation with counselors, social workers, and others can strongly
influence the final outcome.
rollers will produce a true crush injury. Such trauma usually occurs in
the workplace from a printing press or with a home laundry machine—the
classic “wringer arm” (43). The nature of the
damage and the severity of the wound produced by these wringers or
rollers are determined by a number of factors (17,60).
Important ones include clearance between the rollers, the type of
surface (steel or rubber), and the temperature of the crushing device.
The speed of the roller partially determines the force applied; skin
avulsion occurs at higher speeds.
is created when the large extremity is propelled into the small gap
between the rollers. Compression results in tissue contusion. A friction abrasion force characteristically produces a distally based flap and often tears the skin. Last, a shearing force moves the soft tissues over deeper fixed structures, resulting in lacerations,
subcutaneous hematomas, and disruption of musculotendinous junctions.
The degree of injury is related to the roller size, clearance, duration
of compression, and the method of extraction. The severity and depth of
injury produced by the compression and shearing forces may not be
readily evident. Skin that has been completely removed from its blood
supply will undergo necrosis (67).
Hemorrhage may further separate the subcutaneous tissues from the deep
fascia and require drainage. Swelling or bleeding beneath the forearm
fascia can produce increased pressure (see Chapter 13 and Chapter 65)
and muscle ischemia and result in Volkmann’s contracture. Although this
is often described in the forearm, ischemic contracture involving the
intrinsic muscles can occur in the hand (51).
When examining the severely crushed, edematous hand, if pain is
produced by the intrinsic stretch test and compartment pressures are
significantly elevated, perform decompression of the interossei. If
peripheral circulation is impaired and/or distal pulses are not
palpable, evaluate further with a Doppler device and do an arteriogram
if necessary. Test sensibility: two-point discrimination values greater
than 10 mm are suggestive of nerve compression but may represent a
traction injury to a nerve. Because fractures occur in 25% of roller
injuries, obtain appropriate radiographs (43).
An injury that is frequently unrecognized is dislocation of the
metacarpal trapezial joint. This occurs when the transverse arch of the
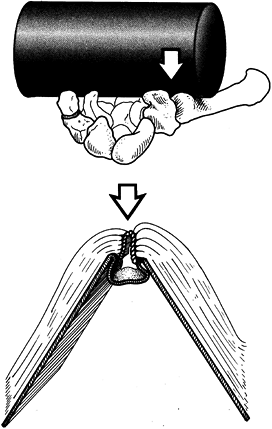
hand is flattened and compressed (Fig. 45.1) (71).
 |
|
Figure 45.1. Roller or crush injuries extending to the level of the wrist (A) can dislocate the basal (trapezial–metacarpal) joint and (B) are similar to breaking the binding of a book.
|
household laundry wringer were once common occurrences; fortunately,
this device has almost disappeared with the advent of modern clothes
dryers, and such injuries are now rare. Wringer injuries usually occur
in children younger than 15 years of age and most often between ages 3
and 5 years. The maximal injury is usually located at the area most
proximally involved (45). Damage usually occurs
up to the level of the elbow, with more proximal trauma occurring in
younger patients. The most frequent injuries encountered are friction
burns from abrasion and soft tissue contusion, which can occasionally
lead to tissue necrosis. Lacerations, joint injuries, and vascular
trauma occur less frequently (65).
-
Cleanse the entire limb.
-
Reduce dislocations and fractures.
-
Suture lacerations.
-
Open wound care may be appropriate, particularly with marginally perfused skin flaps.
-
Apply a light nonconstrictive dressing
and splint. The rare patient with a limb-threatening vascular injury or
a major soft-tissue injury requires prompt surgical treatment. As with
other crush injuries, the greatest difficulty is in assessing the
initial depth of a wringer injury in a child. The most common surgical
procedure required after a wringer injury is skin grafting. Antibiotics
are indicated in patients with open fractures or obviously contaminated
wounds (25).
-
Prepare and drape the entire extremity.
-
Do not use a tourniquet.
-
Do a methodical layer-by-layer debridement and irrigation of open wounds.
-
If a compartment syndrome is present in the hand, wrist, or forearm, perform appropriate fasciotomies (15,49,51).
Decompressions of the hand often require dorsal incisions for the
interossei and separate incisions for the hypothenar and thenar
compartments. For decompressions of the hand and/or forearm, include a
carpal tunnel release. -
Nerve injuries are difficult to assess,
as loss of function most commonly results from a neuropraxia, but
direct crushing and traction injury may be present (66).
If the nerves are visible in wounds or fasciotomy incisions, inspect
them; otherwise, simply observe them as they recover without surgical
intervention. -
Stabilize fractures, as this enhances soft tissue management and facilitates rehabilitation.
-
Repair tendon lacerations or avulsions.
-
Leave all wounds open at the time of
initial debridement. A common injury is a palmar laceration with a
distally based skin flap and crush of the thenar and hypothenar
muscles. Further necrosis may occur, requiring serial debridements. -
Cover the wounds with moist dressings and
splint the extremity with the wrist in extension, the MP joints flexed,
and the interphalangeal joints extended. -
Return to the operating room at 36- to 72-h intervals or as often as necessary to complete debridement of nonviable tissue.
-
Skin loss will require resurfacing with either grafts or flaps (9,36,39).
-
Crush injuries involving the dorsum of
the hand usually have damage to skin, extensor tendons, and bone and
joints. Conventional treatment of these injuries has been with staged
reconstruction, first obtaining soft-tissue coverage and then
performing bone repair and tendon grafts. Recent studies have suggested
that immediate reconstruction with primary tendon and bone grafting
along with skin closure results in faster return of motion and fewer
surgical procedures. -
Injuries that involve both surfaces of the hand frequently result in amputation of some portion.
immediately following surgery. While the surgical dressing immobilizes
the injured tissues in the appropriate position, move the uninvolved
portions of the hand. After the wound has stabilized, direct a more
vigorous mobilization program at overcoming the most common problems of
chronic edema and stiff joints (72).
elevation and active motion. Retrograde massage may prove helpful, and
thermoelastic gloves can provide continual compression and warmth. To
prevent joint stiffness and contractures, promptly mobilize all joints
within the limits of pain tolerance. Try to move each joint through as
great an arc of motion as possible at least three times a day, and
preferably once each hour. With further healing, and when the patient
has less pain, dynamic splinting may be added to the exercise program.
Although splinting of the hand in metacarpophalangeal joint flexion and
interphalangeal joint extension (safe position) prevents the most
serious joint contractures, this attitude of the fingers increases the
chance of developing contracture of the intrinsic muscles. Persistent
dorsal edema of the hand predisposes to intrinsic muscle contracture
even if these muscles have not been compromised initially. An intrinsic
stretching exercise program can prevent contracture.
also restores the gliding of tendons and increases both tendon strength
and wound healing. Motion begun too early may sometimes compromise
soft-tissue healing; therefore, carefully monitor the patient.
Persistent drainage from a wound indicates inadequate debridement with
the presence of necrotic tissue or retained foreign material.
scar contractures, tendon adherence, nerve compression, and chronic
pain (12). The blood supply to skin flaps that
have been markedly contused is usually poor and often distally based.
Excise all obviously nonviable skin primarily. Suture borderline tissue
flaps without tension and carefully observe them. By 3 to 5 days after
injury, tissue viability should be clarified, and the wound can be
debrided of all necrotic material.
simplest techniques that will provide a satisfactory result, such as a
skin graft, either split thickness or full thickness. A local flap can
be used to cover a small full-thickness defect resulting in exposed
bone or tendon that requires vascularized tissue. More proximal flaps
from the arm (posterior interosseous artery or radial forearm) can be
employed for coverage of larger defects. More distant flaps (abdominal
or groin) and free tissue transfers should also be considered. The
latter may be composed of skin, muscle, fascia, or composite tissues.
Although detached skin may be defatted and used as a full-thickness
skin graft, if it is severely traumatized it will fail to heal. The
decision as to which coverage is most appropriate depends on the
requirements of future reconstructive surgery.
skin grafting or with a surgical incision required for a fasciotomy.
Prevention of the latter can be achieved by application of the
principles for incision placement (40). Contracted skin grafts can be resected and the defect treated with local soft-tissue mobilization or tissue expansion (47).
A graft may be replaced by a flap if additional tissue is required
after the contracture is released. This is important if the location is
one that will receive considerable pressure with use or that will be
subject to tissue breakdown. For example, split-thickness skin grafting
on the palm may not withstand normal shearing forces, and primary
closure of a wound involving a flexion crease ultimately worsens the
contracture. Occasionally contractures can be released with a Z-plasty or a local flap.
considered after a crush injury, direct muscle trauma with necrosis and
fibrosis is more common. Selective muscle debridement is part of
treating an open injury. Although adherence of injured muscles or
tendons is common, prompt remobilization can limit the loss of motion
in the
hand.
However, fractures and joint injuries will compound the problem.
Tenolysis should be considered only after all the tissues in the
extremity are well healed and the patient obtains full passive motion
in the fingers. Adherence proximal to the musculotendinous junction
will not respond to a lysis and should not be attempted, as it will not
improve distal motion.
injury. External compression can occur at the site where a nerve passes
adjacent to traumatized muscle or injured fixed tissues, that is,
ligaments or bone. Crushing trauma is even more likely to produce an
intraneural injury. The question is whether there is external nerve
compression or internal fibrosis of the nerve. The production of
paresthesias on percussion over a nerve may localize the injury but
will not clarify the diagnosis. Electromyelograms and nerve conduction
studies may help differentiate external or internal compression from
traction.
Several weeks after the initial trauma, the patient should be able to
control pain with a nonnarcotic medication. If the patient still has
considerable pain after this, a chronic problem must be acknowledged
and will require the combined efforts of several specialties. If the
patient is to participate actively in an exercise program, pain must be
controlled. Supportive splinting and a variety of modalities including
transcutaneous electrical nerve stimulator are indicated. The
possibility of the patient developing a chronic pain syndrome must be
recognized from the onset. Successful treatment requires early
recognition and a rapid response.
the hand alone, they need to be considered in light of the broader
classification of mutilating hand injuries. This is a topic too large
to be included in this chapter, but a few principles need to be
understood. Reconstructive surgery after a mutilating wound will be
more effective if the primary treatment minimizes the amount of scar
tissue. Soft-tissue coverage is critical. The preservation or sacrifice
of tissue must be designed to gain the greatest function at the least
risk. When the hand has been mutilated, normal function may be an
unrealistic expectation in the setting of anatomic loss, but useful
function may be created with what remains. Microsurgical techniques
have expanded the repertoire of the reconstructive surgeon.
recognize the depth and significance of the original injury. The most
critical element after such an injury is the correct timing of
treatment. The judgment required to make these critical decisions
arises from knowledge and experience.
caused by grease, paint, or paint thinner occur frequently. Although
the wound may initially appear innocuous, these injuries are surgical
emergencies that require prompt exploration, decompression, and
debridement (41).
The substance fired at such velocity through a small nozzle enters the
skin and spreads along fascial planes, tendon sheaths, or neurovascular
bundles—the paths of least resistance (35).
Tissue within the hand may be mechanically damaged by pressure and
rendered ischemic. In addition, the material injected produces an acute
chemical inflammation, which may be associated with additional soft
tissue and vascular damage (14).
is not completely removed, chronic inflammation, fibrosis, foreign body
granuloma (oleomas), and sinus formation with chronic tissue breakdown
may occur. Paint produces an acute inflammatory response, whereas
grease causes a delayed chemical reaction resulting in fibrosis and
stiffness. The volume of material that enters the hand is directly
proportional to the pressure produced by the gun. The greater the
volume of material that has been injected, the greater is the amount of
soft tissue damage that occurs.
minimal, with only a burning discomfort at the injection site. Within a
short time, the finger usually becomes distended, pale, and numb with
throbbing pain. Subsequently, greater pain and mottling of the skin
appear. The pain may be related to ischemia, the injection having
created a compartment syndrome of the digit. If a considerable volume
of material has been injected, enlargement of the finger is immediate.
The left hand is involved more frequently than the right, and the
patients are usually men. Common injection sites include the distal
segment of the index finger, thumb, or middle finger, which are usually
used to check a presumed “plugged” injection tip. The palm and other
digits are damaged less frequently.
demonstrate how deeply the grease or paint has extended. Many greases
are radiopaque because of the lead that has been added as a lubricating
agent. If routine x-rays do not yield enough information,
xeroradiographs may provide useful information. Patients can develop
systemic effects, which include fever, lymphangitis, and an elevated
leukocyte count. These signs usually appear within 2 days after the
injury and may last 4 to 5 days (13).
-
High-pressure injection injuries require immediate surgery.
-
Local anesthetic blocks in the palm are
usually contraindicated, and the extremities should obviously not be
wrapped with a pressure bandage before application of the tourniquet (35). -
Use a modified midlateral incision to
explore the finger. A zig-zag approach, although providing better
exposure, is more likely to result in skin slough and may lead to
further tissue compromise in wounds left open for subsequent
debridement. If necessary, continue the incision into the palm in a
curvilinear fashion, extending it past the wrist and into the forearm
if needed. -
After surgical exposure, remove all the
abnormal material such as grease or paint. Excise any fat or fascia
that is involved. Resect tendon sheaths in part if they are involved,
taking care to leave essential portions of the fibro-osseous sheath
system. A small curet or rongeur may be helpful in removing the
material. -
Nerves and arteries that are functional but have the foreign substance embedded in them should be left intact and not resected.
-
Even after a meticulous dissection, some
foreign material may remain. Solvents for grease or paint are
inefficient and are not employed for fear of causing more tissue
damage. Pack open the wounds with the intention of performing a
secondary exploration and closure in 2 to 3 days. -
An alternative choice is to close the wounds loosely over drains.
-
A third choice is to leave the wound
completely open, allowing it to heal by secondary intention. Skin
grafts may be required to close wounds if critical structures are
exposed. -
Perform wound cultures at the time of all
surgeries, as infections are not infrequent. Many surgeons recommend
antibiotic coverage for 2 weeks, but the use of prophylactic
antimicrobial drugs is not clearly indicated unless there is an active
infection (41). -
Immobilize the hand in a safe position (MP flexion and interphalangeal joint extension).
healing by secondary intention with early motion and whirlpools as well
as an intensive active exercise program. Patients whose wounds have
been packed open should be considered for the same treatment or have
their wounds reevaluated in the operating room for redebridement in 2
to 3 days. When it has been determined that all the foreign material
has been removed, involve the patient promptly in the remobilization
program as mentioned above. Make no attempt to close small defects with
skin grafts. Except during exercise, place the patient’s hand at rest
in a position to prevent contractures, particularly flexion
contractures at the PIP joint. Eventual impairment is related to the
amount of tissue destroyed by foreign material. Paint gun injuries
generally inflict greater damage than do grease guns, and injections
into the palm have a better prognosis than injury to the digits.
result from failure to debride the wound sufficiently and premature
wound closure. Although much has been written about the toxicity of
both grease and paint, injected paint thinner is the most difficult to
detect and completely remove (63). Injuries from paint thinner should never be closed primarily; multiple debridements and reexplorations can be anticipated.
result often occurs because the patient or physician initially
evaluating the injury is unaware of its significance (22).
In one recent series, the only patients requiring amputation were those
initially evaluated 3 to 8 days following injury. Although prompt
surgery is recommended, this alone does not always ensure a good
result. It is also possible to obtain a satisfactory result when
surgical treatment has been delayed, particularly with grease gun
injuries (62).
patient initially and remain under consideration should delayed healing
or complications arise. Retention of the tip of a digit that has
required extensive soft-tissue and skin resection is not beneficial.
The patient will be left with a painful atrophic finger with little
function. The period of disability can be extensive, and it averaged 7
months in one study (22). In a more recent
study where patients were treated with open wound management (wide
debridement, drainage, open packing, and delayed closure), all the
patients returned to work, 92% to their previous job (55).
Because of the possible prolonged morbidity, several authors have
recommended early amputation, especially after a paint gun injury (35,57). Prompt amputation often allows the patient to return to work within 6 to 8 weeks of the injury.
breakdown, ulceration, and sinus formation with discharge of foreign
material. Delayed infection rarely occurs if one can obtain wound
healing within 2 weeks of the original injury. However, retention of
foreign material, necrotic tissue, and chronically open wounds can
produce sepsis.
casualties in the 1982 Falkland Islands conflict were related to
frostbite. Unfortunately, frostbite is also a civilian concern, even in
urban, populated areas today. The human body is equipped with many
mechanisms for the dissipation of heat but must rely on largely
conscious measures for heat conservation. The strongest human defense
against frostbite is the conscious decision to wear adequate clothing
and seek shelter. Not surprisingly, then, urban frostbite most commonly
occurs in those with altered mental states such as psychiatric illness
and substance abuse. The homeless, elderly, and children are also at
risk.
Wind velocity, ambient temperature, altitude, and duration of exposure
set the environmental stage, acting on host factors such as protective
clothing, systemic and vascular disease, previous cold injury, and
ability to seek adequate shelter and treatment.
 |
|
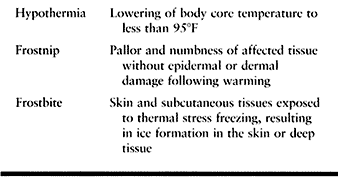
Table 45.5. Differentiation of Cold Injuries
|
frostbite injuries in Saskatoon, Saskatchewan, concluded, “Fit,
well-prepared people without cerebral impairment rarely present with
significant frostbite injury” (69). In this
series, 78% of victims were male and 46% associated with alcohol
consumption, 17% with psychiatric illness, and 19% with trauma. The
distribution of injury was 19% upper extremity, 31% upper and lower,
and 47% lower extremity. Of the 63 patients with upper extremity
frostbite, 13 required major amputation and 18 minor (69).
frostbite cases at Cook County Hospital in urban Chicago were reported
over 10 winters. The mean age of the patients was 43 years, with over
76% between the ages of 30 and 60. Upper extremity involvement (47%)
was slightly less than lower extremity (53%). Children showed almost
exclusively upper extremity involvement, many with bilateral
“glove-like” lesions. Hand amputations, when required, were most common
at the finger MCP joint and the thumb IP joint (7).
predictors of poor outcome such as major tissue loss. Strong
association was found with impaired cerebral function (alcohol,
psychiatric illness), lower extremity involvement, infection on
presentation, and delay in seeking medical attention (68).
Inadequate protective clothing and exposure to metal or wetness was
also correlated with severity of injury by Knize in a Denver, Colorado
study (37).
cold environment. The spinal cord signals the hypothalamus, resulting
in increased muscle tone (shivering) and release of catecholamines and
thyroxine. Increase in basal metabolic rate, vasoconstriction, and
decreased sweating result. The most important organ in temperature
regulation is the skin, specifically that of the extremities, which
represents more than 50% of total body surface area. Blood flow to the
skin during cold stress can virtually cease or can increase as much as
200-fold for heat loss (8). The “hunting
reaction,” described by Sir Thomas Lewis in 1830, preserves both core
temperature and extremity viability during cold exposure by cyclically
alternating vasoconstriction and vasodilation to the limbs (8,48,56).
This regulatory mechanism ceases when the core temperature drops,
prioritizing preservation of core temperature over extremity viability.
of tissue. Slow freezing results in extracellular ice crystal
formation, which increases the osmotic pressure of the interstitium,
pulling out intracellular water. Intracellular fluid does not
crystallize, as it is continuously lost with a corresponding reduction
of freezing point (48). Cell membrane damage,
most marked in endothelium, occurs by mechanical damage from crystals
and dramatic osmotic changes. Endothelial cell injury is seen
microscopically with separation from the internal elastic lamina of the
arterial wall. Ice crystal formation in plasma resulting in red cell
sludging further compromises circulation. Cartilage cells, especially
in epiphyseal cartilage, are very susceptible to even brief freezing.
Muscle, blood vessels, and nerves are damaged more quickly than bone
and connective tissue (8,48,56).
10°C/min. This results in immediate cell death by intra- and
extracellular crystal formation. Exposure to cold metal or volatile
liquids is the most common mechanism.
and damaged endothelial-lined capillaries dilate and leak fluid and
protein into the interstitium. Intracellular swelling occurs in any
viable cells, as they were previously dehydrated and regain water lost.
Red and white blood cells and platelets aggregate, contributing to
microcirculatory failure, a significant cause of tissue loss (8,48). Continued
tissue injury following reperfusion may also be related to prostaglandin-induced vasoconstriction (PGF2α, thromboxane A2),
similar to factors found in burn injury. These factors have been found
in significant concentration in clear blisters associated with
frostbite, leading some to recommend their debridement to limit further
loss of viable tissue. Aloe vera is an inhibitor of thromboxane A2, and aspirin or ibuprofen controls prostanoid production (30,44).
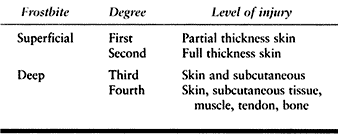
burn injury and indicates level of tissue loss. The prediction of level
is often less than accurate, leading some to recommend a simplified
version indicating only superficial and deep. Table 45.6 demonstrates both systems. Table 45.7 coordinates clinical presentation with degree of injury.
 |
|
Table 45.6. Classification of Frostbite by Level of Tissue Loss
|
 |
|
Table 45.7. Classification of Frostbite by Clinical Presentation
|
protection of the injured part from mechanical trauma, avoiding
pressure, rubbing, or exercise. If there exists any possibility of
further cold exposure, rewarming is strongly contraindicated.
Refreezing results in much greater tissue necrosis than the persistence
of freezing until definitive and controlled rewarming can occur.
Salimi, in a rabbit foot model, demonstrated that rapid rewarming was
effective in limiting necrosis only when performed immediately after
freezing. He recommends it only if it is performed immediately
following removal from freezing (58).
Unfortunately, most patients’ injuries have already spontaneously
thawed on presentation, 88% in the large Chicago Cook County Study (7).
40°C to 42°C water containing a mild antibacterial agent until a
flushed appearance to the part indicates reperfusion. Continuous
monitoring of water temperature is imperative. Dry rewarming is
contraindicated to avoid risk of burn injury. Narcotic analgesics will
be required during rewarming. Give tetanus booster and antitoxin if not
up to date. Obviously, if hypothermia exists, systemic treatment and
measures take priority over rapid rewarming, although they often may be
instituted simultaneously. Antibiotic prophylaxis is controversial and
likely appropriate only in severe cases with delayed presentation.
edema. Debride clear blisters but leave hemorrhagic blisters
undisturbed. The goals of wound care are to preserve viable tissue and
to prevent infection. Whirlpool treatment is recommended for open
wounds. Escharotomy and fasciotomy may occasionally be required.
Dressing wounds with topical agents such as aloe vera may be helpful in
counteracting the vasoconstrictive effects of thromboxane A2, and oral aspirin or ibuprofen counteracts the effects of prostanoids (30,44).
Systemic vasoconstrictive agents such as nicotine are obviously
prohibited. Multiple other treatments have been studied, but their
usefulness has not been established; these include dextran, heparin,
pluronic F-68, hyperbaric oxygen, phenformin ethylestrenol,
streptokinase, urokinase, and reserpine. Hyperbaric oxygen is not
helpful and may cause vasoconstriction and reduction in blood flow (56).
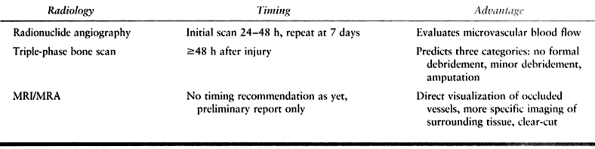
and wait before you ablate” characterize the historical treatment of
frostbite. Difficulty in prediction of tissue loss has led to a very
conservative approach, often awaiting autoamputation. Earlier
prediction is now possible through triple-phase bone scanning,
radionuclide angiography, and magnetic resonance imaging/MRA (Table 45.8).
 |
|
Table 45.8. Imaging for Frostbite
|
guillotine fashion, with delayed closure or coverage. Acute amputation
is necessary only in the setting of infection, most common in patients
with a delayed presentation.
surgically. Reserpine infusion intraarterially into the affected limb
causes depletion of arterial wall norepinephrine for up to 2 to 4 weeks
(56); however, no difference has been shown in
conservation of tissue, edema resolution, pain reduction, or improved
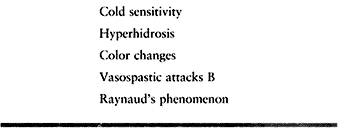
function. Surgical sympathectomy plays a delayed role in treatment of
vasospastic syndromes following a cold injury.
hands without digits or loss of all but the proximal thumb.
Reconstruction of this difficult problem is possible through tissue
transfers and free flaps. An excellent report of 25 digitless hand
reconstructions by Borovikov demonstrated a reliable technique of
toe-to-hand transfers to regain opposition (6).
Intrinsic injury affects strength and fine motor control in relation to
both direct muscle freezing and neurologic injury. Arvesen studied 40
Norwegian soldiers following local cold injuries. Nerve conduction
velocities were still markedly decreased 3 to 4 years following injury
to the nerves in previously cold-injured limbs, even proximal to the
level of injury (2).
 |
|
Table 45.9. Vasospastic Symptoms
|
and the destruction of articular cartilage by ice crystal formation
explain the arthritis that can occur as early as months following
injury. In children, both the physis and the epiphysis are susceptible.
Classic radiographic findings in the juvenile frostbite injury include
total absence of the distal phalangeal epiphysis and damage to the
middle phalangeal epiphyses. Distal metaphyses are frequently irregular
even in the absence of clinical frostbite (56).
of previous cold injuries, 20 to 30 years following injury, similar to
burns or chronic osteomyelitis.
improving the outcome of frostbite injury is its prevention. The
important role of inflammatory mediators in perpetuating tissue damage
following cold injury will be a future focus of research to modulate
this effect. Acute management must focus on the basic principle of
doing no further harm and protecting viable tissue. Rapid rewarming may
be of great benefit only when a patient presents with frozen tissue.
Later reconstruction must be tailored to the unique
needs of the injured individual, often requiring tissue transfer.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
F, Johs SM, Leighton TA, Klein SR. Peripheral Arterial Shotgun Missile
Emboli: Diagnostic and Therapeutic Management—Case Reports. J Trauma 1991;31:1426.
GT, Fisher JC, Edgerton MT. “Wringer Arm” Re-evaluated: A Survey of
Current Surgical Management of Upper Extremity Compression Injuries. Ann Surg 1973;177:362.
KK, Weaver LD, Todd AO, et al. Efficacy of Ceftriaxone versus Cefazolin
in the Prophylactic Management of Extra-articular Cortical Violation of
Bone Due to Low-Velocity Gunshot Wounds. Orthop Clin North Am 1995;26:9.
WB, Dustman JA. Preservation of Functional Following Complete Degloving
Injuries to the Hand: Use of Simultaneous Groin Flap. Random Abdominal
Flap and Partial-Thickness Skin Graft. J Hand Surg 1981;6:82.
GJ, Balasubramanium S, Wasserberger J, et al. Extremity Gunshot Wounds:
Part One—Identification and Treatment of Patients at High Risk of
Vascular Injury. J Trauma 1994;36:358.
P, Hansraj KK, Cox EE, Ashley EM. Gunshot Wounds to the Hand. The
Martin Luther King, Jr., General Hospital Experience. Orthop Clin North Am 1995;26:95.
MR, Turkula-Pinto LD, Cooney WP, et al. High-Pressure Injection
Injuries of the Hand: Review of 25 Patients Managed by Open Wound
Technique. J Hand Surg 1993;18A:125.
