Funduscopic Examination
Authors: Lewis, Steven L.
Title: Field Guide to the Neurologic Examination, 1st Edition
Copyright ©2004 Lippincott Williams & Wilkins
> Table of Contents > Section 2
– Neurologic Examination > Cranial Nerve Examination > Chapter 11
– Funduscopic Examination
– Neurologic Examination > Cranial Nerve Examination > Chapter 11
– Funduscopic Examination
Chapter 11
Funduscopic Examination
PURPOSE
The main purpose of optic funduscopy in the neurologic
examination is to look for swelling of the optic disc. In the clinical
context in which subarachnoid hemorrhage is a consideration, another
purpose of funduscopy is to look for retinal hemorrhages.
examination is to look for swelling of the optic disc. In the clinical
context in which subarachnoid hemorrhage is a consideration, another
purpose of funduscopy is to look for retinal hemorrhages.
WHEN TO PERFORM THE FUNDUSCOPIC EXAMINATION
An attempt at visualization of the optic fundus should
be performed on all patients as part of a standard neurologic
examination.
be performed on all patients as part of a standard neurologic
examination.
NEUROANATOMY OF THE FUNDUSCOPIC EXAMINATION
The optic nerves are formed from the axons of retinal
neurons that converge to exit the eye and send visual information back
to the brain. The optic disc, also called the optic nerve head,
is the portion of the optic nerve that can be visualized when looking
in the optic fundus. The optic discs are located in a slightly medial
position within the retina; this is important to remember when trying
to visualize the optic disc.
neurons that converge to exit the eye and send visual information back
to the brain. The optic disc, also called the optic nerve head,
is the portion of the optic nerve that can be visualized when looking
in the optic fundus. The optic discs are located in a slightly medial
position within the retina; this is important to remember when trying
to visualize the optic disc.
The subarachnoid space that surrounds the brain and
spinal cord also extends into the optic nerves. Therefore, processes
that increase the intracranial pressure can also extend their pressure
along the optic nerves, which may be visualized as swelling of the
optic nerve head (papilledema).
spinal cord also extends into the optic nerves. Therefore, processes
that increase the intracranial pressure can also extend their pressure
along the optic nerves, which may be visualized as swelling of the
optic nerve head (papilledema).
EQUIPMENT NEEDED FOR THE FUNDUSCOPIC EXAMINATION
An ophthalmoscope.
HOW TO EXAMINE THE OPTIC FUNDUS
-
Begin by preparing the ophthalmoscope.
Set the ophthalmoscope to 0 diopters, the optimal initial setting for
most patients and physicians. Set the light of the ophthalmoscope so
that it produces a white circle of light. -
Ask the patient to look straight ahead at
a distant spot in a dim room. It is helpful to show the patient a
specific spot on the wall in front of the patient to fixate on (or a
spot on the ceiling if the patient is lying in bed). Being in a dim
room, rather than a dark room, better allows the patient to see the
spot and helps with fixation. Ask the patient to try to keep fixating
on that spot without moving his or her eyes. -
Hold the ophthalmoscope to your eye. Look
through the ophthalmoscope with your right eye to assess the patient’s
right eye, and look through the ophthalmoscope with your left eye to
examine the patient’s left eye. -
While holding the ophthalmoscope to your
eye and shining it into your patient’s pupil, bring the ophthalmoscope
in from the temporal side of the eye so that you are aiming slightly
toward the medial side of the retina. -
Bring the ophthalmoscope in toward the
patient as you continue to try to visualize the optic disc. Generally
by this time you should be close to the patient. To avoid striking the
patient’s eye with the ophthalmoscope, it is helpful to hold your index
finger slightly outward so that this rests against the patient’s cheek,
using your other fingers to grip the ophthalmoscope tightly. -
Adjust the lens in the positive (black) or negative (red) direction, if needed, to bring the optic disc into focus.
P.40
NORMAL FINDINGS
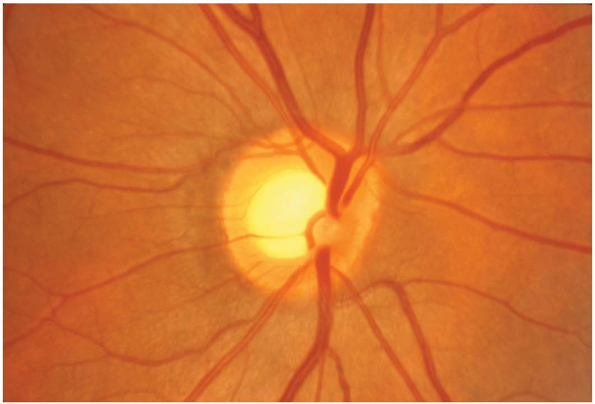
Normally, the optic discs should be sharp, with reasonably well-defined margins, and have a yellowish-orange color (Fig. 11-1). There should be no hemorrhages in the retina.
ABNORMAL FINDINGS
Optic Disc Swelling
-
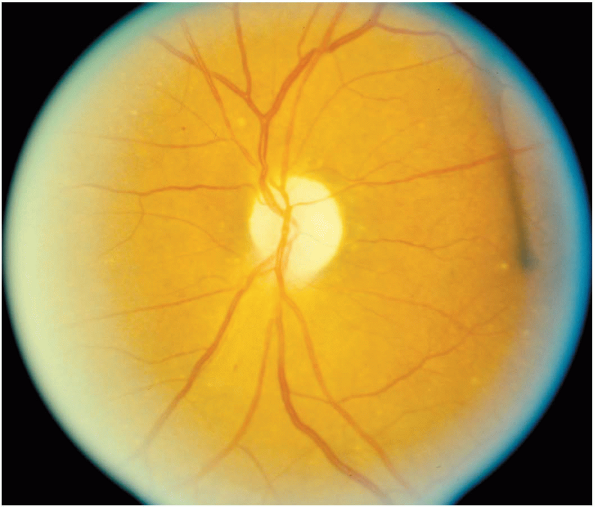
Mild swelling of the optic disc is
manifested by obliteration of the usually sharp disc margins. Severe
swelling of the optic disc is manifested by severe edema and
obliteration of the disc margins (Fig. 11-2); there may also be hemorrhages around the swollen disc. -
Swelling of the optic disc can be due to
increased intracranial pressure (papilledema) or inflammation of the
optic disc (papillitis). These two major causes of optic disc swelling
cannot be differentiated through ophthalmoscopy alone. It is a useful
general rule, however, that acute papilledema does not cause any
significant effect on visual acuity, whereas papillitis causes vision
loss. Papilledema does, however, cause enlargement of the physiologic
blind spot on visual field testing, and chronic papilledema can cause
vision loss.
Retinal Hemorrhages
Hemorrhages in the retina (subhyaloid hemorrhages) can be seen in some patients with subarachnoid hemorrhage (Fig. 11-3).
Optic Atrophy
Optic nerve head atrophy is manifested by severe pallor (whiteness) of the optic disc (Fig. 11-4). Optic atrophy is seen when there is severe chronic optic nerve dysfunction.
ADDITIONAL POINTS
-
Becoming comfortable with ophthalmoscopy to visualize the optic discs requires practice, but it is not really difficult.
-
It is not reasonable for a
nonophthalmologist to be expected to be adept at recognizing subtle
vascular or retinal changes. Concentrate on what you really need to be
able to assess in the neurologic examination: the optic disc. The more
normal optic discs you evaluate, the more likely that you will
recognize an abnormally swollen one. -
It is not usually necessary to use
mydriatic agents (eyedrops that dilate the pupil) to visualize the
optic disc to assess for disc swelling in the routine neurologic
examination. Some patients have small pupils that make visualization of
the optic discs difficult, however. When the optic discs cannot be
visualized and the clinical situation particularly warrants the
examination of the discs to rule out papilledema or hemorrhages,
mydriatic agents can be considered.
 |
|
Figure 11-1 A normal optic disc.
|
 |
|
Figure 11-2 An optic disc with severe papilledema.
|
 |
|
Figure 11-3 Retinal (subhyaloid) hemorrhage in a patient with a subarachnoid hemorrhage.
|
 |
|
Figure 11-4 Optic atrophy in a patient with severe chronic optic nerve dysfunction.
|
