OPEN FRACTURES
II – FRACTURES, DISLOCATIONS, NONUNIONS, AND MALUNIONS > General
> CHAPTER 12 – OPEN FRACTURES
prevent infection, achieve bone union, avoid malunion, and restore the
limb and patient to full function as early as possible. Of these, it is
most important to avoid infection, as infection is the most common
complication leading to nonunion and loss of function. The most
important prognostic factor that determines the long-term result in
open fractures is the amount of energy absorbed by the limb at the time
of initial injury. This determines the amount of devitalized soft
tissue and the level of contamination, which are more important than
the configuration of the fracture (1,5,12,30,42).
The latter, however, is a good indicator of whether a fracture is the
result of high-energy or low-energy forces. Comminution and wide
displacement are almost always associated with high-energy injuries.
The classification of open fractures developed by Gustilo and Anderson
is a good guide to the severity of injury and permits some
prognostication and recommendations for treatment (32,35).
of open fractures, it is a mistake to use this as the overriding factor
in determining the classification. Extremely severe soft-tissue
crushing is often associated with punctate wounds. The entire extent of
the injury must be taken into account in applying this classification.
has a wound that is usually less than 1 cm long and is caused by
low-energy forces. Generally, it is caused by the bone piercing the
skin rather than a penetrating object. It is not associated with
significant crushing or muscle damage. Fractures of this type that
occur in highly contaminated environments, such as a farmyard, are
classified as type III fractures.
 |
|
Figure 12.1. Type I open fracture of the tibia.
|
has a wound that is more than 1 cm long and is associated with moderate
deep muscle damage secondary to the high energy absorbed at the time of
injury. A type II open fracture is considered to be transitional
between type I and type III open fractures.
 |
|
Figure 12.2. Type II open fracture of the tibia.
|
is caused by high-energy forces, is usually associated with wounds more
than 10 cm long, and involves extensive muscle damage. The fracture is
often widely displaced or comminuted. Any open fracture with one or
more of the following characteristics is classified as type III:
high-velocity gunshot wounds, shotgun wounds, displaced segmental
fractures, fractures with significant diaphyseal segmental loss,
concomitant vascular injuries requiring repair, and fractures occurring
in highly contaminated environments, such as farmyards. Fractures
associated with crushing caused by high-velocity motor vehicle
accidents are usually type III injuries.
 |
|
Figure 12.3. Type IIIB open fractures of both tibias.
|
In type IIIA open fractures, there is limited periosteal and muscle
stripping from bone, and major plastic reconstructive procedures, such
as flaps, are not required to achieve bone coverage. In type IIIB
fractures,
there
is extensive soft-tissue stripping from bone. Soft-tissue defects that
result in exposed bone require reconstructive procedures to restore
soft tissue coverage. In a type IIIC open fracture, a major vascular
injury requires repair to salvage the limb. The AO/ASIF group has a
classification that grades the soft tissue injury incorporating the
degree of injury to the skin, muscle, tendon, and neurovascular
structures; it is used in conjunction with the AO/ASIF alphanumeric
fracture classification system (62).
Tscherne and associates have reported on an open fracture score that
takes into account the AO/ASIF fracture classification and grades bone
loss; skin, muscle, and soft tissue injury; neurovascular injury;
compartment syndrome; time from injury to initial treatment;
contamination; and results of cultures. Using a combination of these
scores, they grade open fractures into types I to IV. They validated
this score in a study of 651 open fractures (77).
I find the latter two classifications to be too complex for day-to-day
clinical use; instead, they are more suited to clinical research. We
continue to use the Gustilo classification; however, the reader needs
to be aware that even this simple system is subject to significant
variation in interobserver agreement (28).
vital body functions and resuscitate and stabilize as necessary. During
resuscitation and immediate evaluation, splint the patient’s fractures
and cover open wounds with sterile compression dressings. Soak the
dressing immediately adjacent to the wound with a dilute
povidone-iodine solution, particularly if the patient will not be
undergoing immediate debridement. I no longer obtain cultures of open
fracture wounds in the emergency room, as studies have not shown this
to be useful in making therapeutic decisions (52,61).
Use traction for femoral fractures. Immediately after resuscitation and
stabilization, perform a complete history and physical examination.
Evaluate the extremities for neurovascular function, possible
compartment syndrome, and soft-tissue injury, and record the findings.
Then obtain appropriate radiographs. Certain open fracture-dislocations
and dislocations, such as widely displaced dislocations of the ankle,
subtalar joint, knee, or elbow, are best reduced immediately in the
emergency room. This usually can be accomplished with premedication and
no anesthesia. Open fracture-dislocations of the hip and shoulder
almost always require general or regional anesthesia. Fracture
reduction under anesthesia is generally easier for both patient and
surgeon.
and tetanus toxoid. The globulin is not required if the patient has had
toxoid in three or more doses within the last 10 years. Start
intravenous bactericidal antibiotics as soon as possible. In types I
and II open fractures, the antibiotic of choice is usually a
cephalosporin; I prefer cefazolin sodium. For the average adult, a
loading dose of 1 to 2 g, followed by 1 g every 8 h, is effective. For
patients with farmyard injuries or other open fractures in which there
is a risk of infection with Clostridium,
give 4 to 5 million units of penicillin every 6 h as well. In type III
open fractures, give an aminoglycoside intravenously—3 to 5 mg/kg of
lean body weight per day—in divided doses at 8-h intervals. I begin
with gentamicin. Monitor serum levels of the aminoglycosides to ensure
therapeutic levels and to avoid toxicity. Obtain a complete blood
count, urinalysis, blood urea nitrogen level, serum creatinine levels,
liver function test, and audiometry test as soon as practical after the
initiation of therapy and then at appropriate intervals (33,66,67).
be continued remains in question. Common practice in most major trauma
centers in North America is to give antibiotics for the first 3 days (33,36).
Antibiotics are then discontinued unless postdebridement cultures and
the patient’s clinical course suggest that infection has occurred. An
advantage of discontinuing antibiotics after 3 days is that the patient
will not be receiving antibiotics at the time of delayed primary
closure, which takes place about 5 days after injury in uncomplicated
open fractures. At the time of delayed closure, obtain repeat cultures
and reinstitute a 3-day course of antibiotics. If the results of the
cultures are negative, and the patient’s clinical course is progressing
satisfactorily, discontinue the antibiotics at the end of the second
3-day regimen. Detection of organisms on Gram stain of tissues from the
wound at the time of delayed primary closure suggests that there are
more than 10,000 organisms per cubic millimeter in the wound; this
indicates heavy contamination or infection. With this finding, it may
be necessary to continue antibiotics for at least 3 weeks, and closure
may have to be delayed (62). If infection is
evident, cultures and antibiotic sensitivity tests may indicate the
need to change the antibiotic regimen to one that is specific for
treatment of the infecting organism(s). In more extensive, severe type
III open wounds, a continuous course of antibiotics is usually
indicated until successful wound closure. For more information on this
complex topic, see publications by Gustilo (33,36,84), Patzakis (66,68), and others (9,28,58,73,90).
are not commercially available in the United States but can be
manufactured by the surgeon in the operating room by mixing 1 g of
tobramycin powder into one batch of polymethylmethacrylate using a bead
maker (available from Department of Orthopaedics, Hennepin County
Hospital, Minneapolis, MN); this produces a string of 30 6-mm beads on
a wire. Antibiotics leach from the surface of the beads to produce
wound levels of antibiotics several times higher than that achieved by
the intravenous route, and systemic absorption is negligable (20). They are not approved for sale by the Food and Drug Administration.
fracture wounds, which were left open and covered with a watertight,
oxygen-permeable membrane (opsite), producing a “bead pouch” (25).
This not only produces high levels of local antibiotics but also
protects soft tissue and bone from desiccation and further
contamination. The bead pouch is renewed at the time of each
debridement until wound closure.
comparative study, were able to reduce the infection rate using
antibiotics alone from 39% to 7.3% when the bead pouch was added to
their usual systemic antibiotics. Bead pouch treatment remains
investigational at this time but is promising (65).
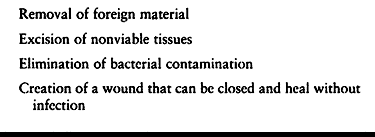 |
|
Table 12.1. Objectives of Irrigation and Debridement
|
with the usual surgical preparation and draping. During preparation,
remove gross debris from the wound, using copious amounts of
preparation solution. In extremity wounds, a tourniquet is placed, if
possible, but is not inflated unless hemorrhage cannot be controlled by
routine surgical means. This is because the hypoxia imposed by a
tourniquet interferes with the physiologic response of muscle necessary
to determine its viability.
-
Irrigate the wound with copious amounts
of normal saline solution. Irrigation is most effective when a
mechanical irrigator with a shower-type head is used. The pulsating
lavage produced is very effective in loosening and washing away debris.
Moreover, high volumes of solution can be run through the wound in a
short period of time. The degree of contamination and the size of the
wound determine the extent of initial irrigation. For an average type
II wound of the tibia, begin with 2 L. -
Irrigate the wound at intervals
throughout the debridement process to clear the wound of debris on a
continuous basis. At the completion of debridement, topical antibiotics
can be added to the last 2-L bag of irrigation solution. The type and
concentration of topical antibiotic is the surgeon’s choice. I most
commonly use 50,000 units of bacitracin per liter of solution. -
For large wounds try to use 10 L of
irrigation by the time the debridement is completed. Anglen and
associates compared bulb syringe irrigation to pulse lavage and found
the latter to be 100 times more effective in reducing bacterial count (2).
They also compared adding bacitracin or neomycin or soap detergent
(castile soap) to the solution. They found no benefit from the
antibiotics, but the detergent was very effective in reducing the
bacterial count. Kellam and associates have shown that solutions of
povidone-iodine or hydrogen peroxide decrease osteoblast function;
therefore, they are not recommended as routine irrigation solution (47).
-
Extend the wound as large as necessary to irrigate and debride all contaminated and nonviable tissue using extensile incisions (Fig. 12.4).
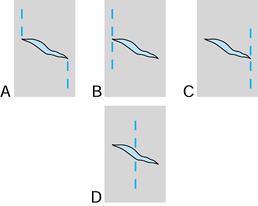 Figure 12.4. Methods of extension of a traumatic transverse or oblique wound. A: This Z-plasty technique produces two large flaps and risks necrosis of the tips of the flaps. B,C: Both of these methods also produce large flaps. D: Crossing the wound results in the smallest flaps. This minimizes the risk of flap necrosis and is the incision of choice.
Figure 12.4. Methods of extension of a traumatic transverse or oblique wound. A: This Z-plasty technique produces two large flaps and risks necrosis of the tips of the flaps. B,C: Both of these methods also produce large flaps. D: Crossing the wound results in the smallest flaps. This minimizes the risk of flap necrosis and is the incision of choice. -
Remove all ragged, contaminated skin
edges, establishing a surgical wound edge that is at right angles to
the skin and suitable for closure. Be conservative in skin removal, as
skin coverage can be a problem in certain areas such as in the lower
extremity distal to the knee and in the hand. Skin flaps with a
length-to-base ratio greater than 2:1, particularly those that are
distally based, will often exhibit some necrosis at the tip of the
flap. It is often difficult to predict flap viability at the time of
initial debridement. Inflating the tourniquet for a brief period of
time and then deflating it to produce hyperemia in the flap will often
delineate devascularized
P.385
portions,
which can then be excised. Leave marginal skin, as it can be debrided
later. If extensive, nonviable flaps are removed and skin coverage is a
potential problem, split-thickness skin grafts can be removed from the
debrided flaps in areas where the skin is in good condition. Use a
Padgett dermatome. This skin can be banked for later use or placed
immediately as a meshed split-thickness skin graft. -
Subcutaneous fat has a poor blood supply.
Debride all contaminated or devascularized fat. The fascia is also
relatively avascular and, if contaminated, should be excised. -
In type II or worse fractures, perform
prophylactic fasciotomy at the time of debridement through the open
fracture wound. If the wound is not large enough to perform the
fasciotomy under direct vision, use a Metzenbaum scissors to split the
fascia beneath the skin. Releasing the fascia of one major compartment,
such as the anterior tibial compartment in the leg, is usually
sufficient. If a significant compartment syndrome is present or
expected, formal four-compartment fasciotomy is indicated. -
Debride all nonviable and contaminated
muscle. Color and bleeding are not good determinants of muscle
viability, as hematoma renders the muscle dark and arteriolar bleeding
can persist in totally nonviable muscle. The best indicators of
viability are the muscle’s response to a stimulus and its ability to
rebound to normal appearance after being pinched gently with a pair of
forceps. Viable muscle fibers contract in response to either the gentle
pinch of a pair of toothed forceps or stimulation with a
nerve-stimulating device or electrical coagulator on a low setting.
Muscle that does not respond and in which a prominent forceps imprint
is left is usually nonviable and should be debrided. In type III open
fractures, entire compartments or muscle–tendon units may appear
nonviable. It may be quite difficult to determine nonviability at the
time of initial debridement. In major wounds, leave intact marginal
muscle necessary to preserve muscle–tendon units that are important for
future function. A tendon with only 10% of the muscle remaining
produces surprisingly good function. If marginal muscle is left intact,
repeat debridement within 24 to 36 h and then as frequently as
necessary to remove all nonviable muscle. -
Exposed tendons and bone not covered by
peritenon or periosteum will desiccate and die within several days,
particularly if not kept moist. Therefore, irrigate peritenon and
periosteum copiously rather than debriding it. Try to cover tendons
without peritenon and bone without periosteum with soft tissue. -
Totally detached cortical fragments of
bone that are contaminated are generally discarded. If internal
fixation is performed, and the bone fragment is critical to the
construct, and if it can be adequately debrided, retain it. If
infection occurs, the fragment must be discarded. When large nonviable
fragments such as these are reimplanted, bone grafting is almost always
advisable. Try to preserve all soft-tissue attachments to bone
fragments. Free fragments of cancellous bone that can be debrided
adequately are left in the fracture bed as bone graft. Swiontkowski has
described criteria for bone debridement using laser Doppler flowmetry (83).
the traumatic wound open. The infection rates with type I open
fractures are equal to those reported in elective orthopaedic surgery,
however (18,35,49,72). Therefore, many surgeons do primary closure of type I open fractures and occasionally of mild type II wounds (24).
The surgeon who elects to close these wounds must exercise caution: gas
gangrene can be a complication of primary closure of type I or mild
type II open fracture wounds if the surgeon has underestimated the
degree of contamination. Most type I wounds are so small that closure
will occur spontaneously, without surgical closure. Never close type
III open fracture wounds primarily, and the same applies to most type
II wounds. This is particularly true if primary internal fixation using
plates has been done.
-
Cover bone without periosteum, tendons
without peritenon, and neurovascular structures with muscle, fascia, or
subcutaneous fat. Perform this without formal wound closure. In wounds
with large flaps, where retraction of skin edges may occur, place loose
tacking sutures to prevent flap retraction. In either of the latter two
instances, if closed spaces are created, place a suction tube for
drainage. -
With types I and II wounds, a return to
surgery within less than 5 days after the initial operation is usually
unnecessary. Type III wounds, as well as heavily contaminated wounds,
however, require repeat debridement before 5 days, and usually within
36 h. Repeat the debridements at 36- to 48-h intervals until a clean
completely viable wound is present. -
After 5 days, if the wound appears clean
and little or no nonviable tissue is present, delayed primary closure
can be performed after irrigation and minimal debridement. Delay
closure of the wound for a few more days if significant debridement is
required. Accomplish delayed closure without tension. Split-thickness
skin grafting is often necessary. Wounds that can be closed to within 1
cm can be allowed to close by secondary intention, provided vital
structures are not exposed and scarring is not a major consideration.
Strive to achieve coverage of bone by 5 to 10 days. Wounds requiring
local flaps or free microvascularized flaps are often ready for flap
coverage within 5 to 10 days, sometimes earlier. In my opinion,
applying flaps to close the wound before 5 days is usually not
indicated. When performing delayed closure, use as little suture
material as possible; monofilament sutures are best.
Restoring normal length and alignment of the extremity minimizes dead
space and restores muscle planes to their normal position. This reduces
the space available for serum and hematoma, which are pabulum for
bacterial growth. Stabilizing the soft tissues may increase local wound
resistance to infection by facilitating neovascularization, white blood
cell migration, and diffusion of nutrients. Bone fixation often
eliminates the need for casts, splints, and skeletal traction, thereby
allowing optimal access to the limb for wound care. Early stability
provides an opportunity for early muscle and joint rehabilitation,
which, in turn, reduces edema, facilitates lymphatic and venous return,
lowers the incidence of deep vein thrombosis, and improves the overall
physiology of the limb.
fractures with stable configurations when external or internal fixation
is unnecessary. This usually applies to fractures distal to the elbow
and knee (10,26).
Immobilize only the necessary muscle groups and joints. Encourage early
joint and muscle rehabilitation. Administer isometric exercises to
immobilized muscles.
diaphysis in patients who do not have multiple injuries where delayed
nailing is planned.
immediately. In type IIIC fractures, immediate skeletal stabilization
is nearly always indicated. Although traction and cast bracing may
constitute definitive treatment, skeletal traction is most often used
for temporary immobilization until closed intramedullary nailing is
done. Skeletal traction may also be useful for some fractures of the
humerus and the tibia in which soft-tissue injuries mitigate against
casts or splints and when subsequent early internal fixation is
planned. Skeletal traction for definitive treatment of fractures of the
tibia is not advisable because of the high incidence of nonunion.
Although skeletal traction can be used for the definitive treatment of
fractures of the humerus, the prolonged hospitalization required and
high incidence of nonunion makes external or internal fixation the
treatment of choice.
the need for circumferential plaster dressings. Compared with internal
fixation, external fixation has several advantages: external fixation
devices are relatively easy to apply and are easily adjusted during
healing; there are no metallic implants at the fracture site; and there
is usually ready access to the wound. Its disadvantages include the
awkwardness of the frame for patients; the potential for pins to injure
neurovascular structures and to tie down muscle–tendon units, thereby
interfering with joint motion and rehabilitation; possible interference
by the pins in plastic reconstructive procedures; and pin loosening and
secondary infection, which remain significant problems. In addition,
external fixation has a higher incidence of delayed and nonunion,
particularly in the tibia. The primary indication for external fixation
is very severe, highly contaminated type III open fractures where
plating or nailing is either contraindicated or not technically
feasible. Open unstable fractures of the pelvis are usually best
initially stabilized with external fixation (76).
Intra-articular fractures require internal fixation; however, external
fixation is useful for providing neutralization when more extensive
internal fixation is impossible or contraindicated. Hybrid frames are
commonly used today to treat high-energy fractures of the metaphysis
such as bumper fractures of the proximal tibia and pylon fractures of
the distal tibia (87). Ring, Ilizarov-type
fixators are useful in similar problems, especially where there is
segmental bone loss that may be amenable to bone segment transport (55,78).
that are stable, as well as type I and mild type II open fractures for
which casts and splints are adequate. The
thick
muscle coverage of the femur and the humerus makes external fixation
less suitable and internal fixation safer. When fixation crosses a
joint, external fixation can be used, but internal fixation may be
preferable.
tibia, the surgeon may choose to initially apply external fixation with
a plan for early conversion to either an intramedullary nail or a
plate. Superior results to primary nailing have been reported (2). This alternative is discussed in detail in Chapter 11 and Chapter 24.
Over the past several years, however, many trauma centers have reported
the use of primary internal fixation in open fractures with good
results and an acceptable rate of complications (18,20,23,49,54,63,71,72). In the combined results of three earlier reports, 403 open fractures were treated with early internal fixation (18,20,72).
The acute infection rate was 8.2%; most of the infections occurred in
type III open fractures. The incidence of late, chronic osteomyelitis
was only 0.5%, however. There was a 2.2% incidence of amputation, all
in type III open fractures of the tibia.
-
Fractures in patients with multiple
injuries in whom external fixation is impractical and stabilization is
necessary to preserve life. -
Patients with severely mutilated or amputated limbs undergoing reimplantation in whom external fixation is impractical.
-
Intra-articular fractures.
-
Open fractures of the major long bones,
in elderly patients, where external fixation is impractical and where
immediate mobilization for the salvage of life and function justifies
the risk of the procedure. -
Major vascular injuries requiring repair that accompany open fractures and where external fixation is not the best choice.
-
Selected fractures of the hand, forearm, and foot (6,22,69,70,88).
-
Open fractures of the shafts of the
femur, tibia, humerus, radius, and ulna are now generally stabilized
primarily using reamed or unreamed intramedullary nails in the femur,
tibia, and occasionally the humerus; the forearm bones and humerus are
generally plated, except where the fracture is not suitable for
internal fixation or the severity of the soft tissue injury and level
of contamination preclude immediate internal fixation.
fixation of open fractures of the femur and the humerus is usually
necessary (27). Open fractures of the pelvis
are generally stabilized with external fixation. If internal fixation
is required to obtain a satisfactory functional result, it is delayed
until the risk of infection is minimized and is usually done
posteriorly using percutaneous techniques if possible (see Chapter 17).
anatomic reduction of the joint surface must be achieved with
interfragmentary lag screw fixation, and early joint motion must be
instituted (9). This requires rigid internal
fixation. In type I open intraarticular fractures, primary internal
fixation should be done, as the incidence of infection is the same as
with elective orthopaedic surgery. Type II open fractures treated with
primary internal fixation are associated with reported infection rates
of 5% to 8%, and type III fractures in the recent past have been
reported to have infection rates of 26% to 41% (16,18,20,49,72).
Because of the risk of infection in more severe fractures, consider
fixation of the joint surface fragments with screws and wires and
stabilization of the metaphyseal portion of the fracture with external
fixation. This can then be converted to plate fixation when the wound
status permits, if necessary.
shaft of the tibia. Although external fixation has been the fixation
method of choice in the recent past, the more recent literature
overwhelmingly supports primary intramedullary nailing as the
stabilization method of choice (3,8,21,39,46,78,79,82).
Most reports are on unreamed nailing; however, minimally reamed or
fully reamed nails inserted acutely or on a delayed basis have received
more attention recently because of the breakage rates in the smaller
nails and screws required for nonreamed nailing as well as the
significant incidence of delayed union. See Table 12.2 and Chapter 24 on fractures of the tibia for more detail.
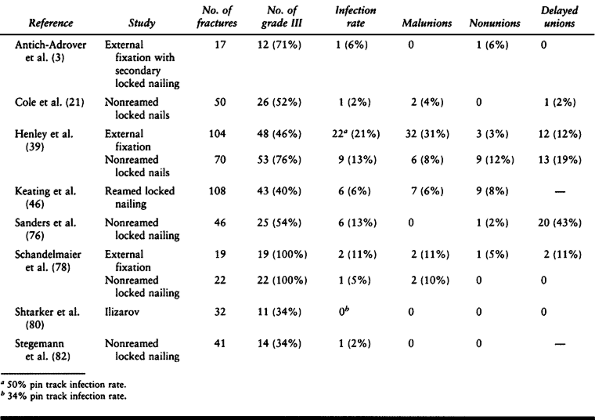 |
|
Table 12.2. Results of Intramedullary Nailing and/or External Fixation of Open Tibial Fractures
|
-
Start appropriate intravenous antibiotics as soon as possible.
-
To minimize the risk of infection, perform a meticulous irrigation and debridement as described above.
-
After debridement, reprep the limb and redrape unless the wound is exceptionally clean. Use a new and separate surgical setup.
-
Perform internal fixation through the
open fracture wound or through an extensile exposure from the open
fracture wound. Separate, elective incisions are rarely necessary. -
Minimize soft tissue dissection, preserve bone vascularity as best possible, and assure that the fixation is stable.
-
Close the elective portion of the wound;
try to cover the implants and any exposed bone with soft tissue; and,
in the vast majority of cases, leave the traumatic wound open, closing
it by delayed primary closure if indicated.
fractures, adjunctive measures to accelerate and assure fracture
healing such as dynamization of intramedullary nails, use of electrical
stimulation or ultrasound, and autogenous, cancellous bone grafting are
often indicated (see Chapter 26) (4).
Bone grafting is recommended for severely comminuted fractures,
fractures with bone loss, and particularly fractures fixed with plates
and screws. Primary bone grafting, often from local bone, is done when
reconstruction of articular and juxta-articular fractures requires
cancellous bone graft to fill defects.
grafting is of concern. Type I fractures in which delayed primary
closure is unnecessary can be grafted immediately. Fractures subjected
to delayed primary closure can be grafted at the time of delayed
closure. In severe type III open fractures, or in wounds that are
marginal, it is best to delay cancellous bone grafting until after the
soft tissues have recovered from the acute trauma and the risk of
infection is minimal. This is generally 6 to 12 weeks after injury in
most severe open fractures.
of inadequate bone. This usually occurs when bone is taken from the
anterior iliac crest. For most major open fractures, insufficient bone
is present in the anterior crest. I recommend that bone grafts be taken
from the area of the posterosuperior iliac spine. This requires
preoperative planning, as the patient must be in the prone or lateral
decubitus position to remove this graft.
-
Severe open fractures with associated
vascular injuries requiring repair (type IIIC) when the injury cannot
be repaired or the warm ischemia time is over 8 h. -
The limb is so severely crushed that minimal viable tissue remains for revascularization.
-
There is irreversible associated soft
tissue injury and neurologic damage that will result in final function
worse than that provided by a prosthesis. -
The presence of multiple injuries where
immediate amputation to control hemorrhage or to reduce the adverse
systemic effects of retaining low-viability or infected tissue may be
life-saving. -
When limb salvage may be life-threatening
in the presence of severe chronic disease such as diabetes mellitus
with severe peripheral vascular disease and neuropathy. -
A mass casualty situation where salvage
of life, transportation of the victim, or the need to direct scarce
resources to more severely injured casualties is indicated.
salvage may require repeated operations and prolonged disability for 2
years or more. The personal, emotional, sociologic, and economic
consequences of expensive and prolonged treatment may cause the patient
to select amputation early during treatment. Lange argues that type
IIIC open fractures of the tibia with laceration of the posterior
tibial nerve should be amputated and provides relative indications
similar to those discussed above (51). Johanson and associates developed the “mangled extremity severity score” (MESS) (43).
Factors they graded include energy dissipation, hemodynamic status, age
of the victim, and limb ischemia. A score of 7 or higher on their scale
predicted amputation with a high degree of confidence. Amputation is
most frequently an issue in open fractures of the tibia. Chapter 24
contains an extensive discussion of these issues. In borderline
situations it may be best to defer the decision about amputation for a
second look, as this gives an opportunity to discuss the situation with
the patient and family and to take into account all of the issues (75).
In spite of the recent pessimism in the literature regarding the
outcomes in the salvage of severe open fractures, Hertel et al. (40),
in an analysis of 39 type IIIB or IIIC open fractures, found the
long-term functional outcomes to be better and costs less with limb
salvage.
-
The injuries are often less severe.
-
The healing capacity of the soft tissues is excellent.
-
Bone that is devitalized can be saved if it is not contaminated or left exposed.
-
The bone-healing capacity of children is remarkable, particularly those under the age of 12 years (31). Bone defects will often heal spontaneously, and bone grafting is usually not required.
-
Infection is rare if adequate irrigation and debridement are performed.
-
Where the soft tissue injury is mild, cast immobilization often suffices.
-
External fixation works well where the
soft tissue injury requires ready access or the fracture is unstable.
It can usually be left in place until union of the fracture (4). -
The general principles of care as outlined in this chapter apply except as noted above.
-
The social and psychological impact of
these severe injuries, particularly in terms of time lost from school,
should not be underestimated (53).
osteomyelitis, nonunion, malunion, and loss of function. Remarkable
progress has been made since the early 1970s in reducing the rate of
these complications. A review of Table 24.7 in Chapter 24 on tibial fractures and Table 12.2
in this chapter shows a drop in acute infection rates of up to three-
to fourfold and similar trends in the other complications as well.
Infection rates of 6% or less are now reported (3,8,21,46,78,79 and 80,82).
These excellent results reflect compulsive adherence to the principles
of treatment outlined in this chapter. For specific details on the
management of these complications, please refer to the chapters on the
fracture of concern and to the following chapters dealing with the
management of complications: Chapter 132, Chapter 133, and Chapter 135 on infection and Chapter 26, Chapter 27, Chapter 28, Chapter 29, Chapter 30, Chapter 31 and Chapter 32 on nonunions and malunions.
the principles outlined in this chapter. I use antibiotic bead pouches
with tobramycin when the wound severity and level of contamination
justify their use. I strive to close all wounds by 10 days after injury
with full-thickness coverage. I work closely with my orthopaedic and
plastic surgery colleagues, whose skills in local and free flaps are
essential to achieving an optimal result (see Chapter 8, Chapter 35, and Chapter 36).
following preferences. In type I and low-grade type II fractures, I
usually perform primary internal fixation if indicated by the fracture,
leaving the traumatic wound open and closing it on a delayed primary
basis. In type III fractures, I use the following protocol:
-
In intra-articular fractures, I use
interfragmentary fixation of the articular portion with “biological”
plate fixation of the metaphyseal portion in low-grade fractures and
hybrid or other external fixation in high-grade open fractures.
Occasionally I will convert the external fixation to internal fixation
when the soft tissue envelope permits and the conversion is the best
alternative for the patient. -
For fractures in the upper extremity, I use primary internal fixation with plates and screws in most cases (17),
reserving external fixation for those where the bone is not amenable to
internal fixation or where the wound makes primary internal fixation
inadvisable. -
In hip fractures, I use primary internal fixation except where not fixable.
-
For femoral shaft fractures, I favor reamed locked intramedullary nailing in most cases (15,20);
I use nonreamed locked nailing in patients with multiple injuries,
where the speed of surgery is important and compromised pulmonary
status is a problem. -
For supracondylar femur fractures, see the item above on intra-articular fractures.
-
For tibial plateau and pylon fractures, see the item above on intra-articular fractures.
-
For tibial shaft fractures, I use locked
intramedullary nailing, either nonreamed or with gentle reaming
sufficient to place a nail (usually 10 mm in diameter) that permits the
use of large cross locking screws (4.5 to 5.0 mm in diameter) (42,45,89).
I use external fixation only when the fracture configuration or
surgical situation does not permit nailing. I try to convert external
fixation to a nail early if it is feasible (57,60). -
For foot fractures, I favor primary internal fixation using small fragment screws and plates and wires.
following scheme: *, classic article; #, review article; !, basic
research article; and +, clinical results/outcome study.
MN, McDonald K, Stephens JG. A Study of the Effect of Open and Closed
Treatment on the Rate of Healing and Complications in Fractures of the
Tibial Shaft. J Trauma 1961;1:290.
P, Marti-Garin D, Murias-Alvarez J, Puente-Alonso C. External Fixation
and Secondary Intramedullary Nailing of Open Tibial Fractures. J Bone Joint Surg 1997;79B:433.
GCH, Edwards P, Widmark PH. Shaft Fractures of the Tibia: Etiology of
Poor Results in a Consecutive Series of 173 Fractures. Acta Chir Scand 1962;124:386.
TJ, Endicott M, Capra SE. Treatment of Open Ankle Fractures. Immediate
Internal Fixation Versus Closed Immobilization and Delayed Fixation. Clin Orthop 1989;240:47.
EG, Dobbie JJ, Siewers CF. Fractures of the Tibia and Fibula.
Comparative End Results from Various Forms of Treatment in a Teaching
Hospital. Arch Surg 1952;64:443.
MW, Goldstein J, Redman S. Results in the Treatment of 259 Open
Fractures. Paper presented at the Annual Meeting of the AAOS, Atlanta,
1984.
JB Jr, Henry SL, Mangino PD, Seligson D. Wound and Serum Levels of
Tobramycin with the Prophylactic Use of Tobramycin-Impregnated
Polymethylmethacrylate Beads in Compound Fractures. Clin Orthop 1988;237:213.
I, Pompeius R. Shaft Fractures of the Lower Leg: Comparing the Early
Results of Open and Closed Treatment in 120 Cases. Acta Chir Scand 1959;118:339.
MB, Chapman JR, Agel J, et al. Treatment of Type II, IIIA, and IIIB
Open Fractures of the Tibial Shaft: A Prospective Comparison of
Unreamed Interlocking Intramedullary Nails and Half-Pin External
Fixators. J Orthop Trauma 1998;12:1.
JL, Swiontkowski MF, Sanders R. Treatment of Open Fractures of the
Tibial Shaft: Ender Nailing Versus External Fixation. A Randomized,
Prospective Comparison. J Bone Joint Surg 1989;71-A:1231.
K, Daines M, Howie T, et al. Objective Criteria for Amputation after
Lower Extremity Trauma. Paper presented at the Orthopaedic Trauma
Association Annual Meeting, Dallas, 1988.
J, Ramp W, Nisholason N, Kaysinger K. Effects of Wound Irrigation
Solutions on Osteoblast Function. Paper presented at the Orthopaedic
Trauma Association, New Orleans, l993.
AY, Shelton ML. Primary Internal Fixation of Open Fractures: A
Retrospective Study of the Use of Metallic Internal Fixation in Fresh
Open Fractures. J Trauma 1972;12:756.
DJ, Merkow RL, Gustilo RB. Infection after Intramedullary Nailing of
Severe Open Tibial Fractures Initially Treated with External Fixation. J Bone Joint Surg 1989;71-A:835.
EB, Von Bonsdorff H, Hakkinen S, et al. Primary Operative Fixation of
Long Bone Fractures in Patients with Multiple Injuries. J Trauma 1977;17:111.
D, On E, Hadas N, et al. Microbiologic Flora Contaminating Open
Fractures: Its Significance in the Choice of Primary Antibiotic Agents
and the Likelihood of Deep Wound Infection. J Orthop Trauma 1989;3:283.
R, Jersinovich I, Anglen J, et al. The Treatment of Open Tibial Shaft
Fractures Using an Interlocked Intramedullary Nail Without Reaming. J Orthop Trauma 1994;8:504.
LS, Kelley M, Yang E, et al. The Use of Combination Internal Fixation
and Hybrid External Fixation in Severe Proximal Tibia Fractures. J Orthop Trauma 1995;9:244.
P, Slack R, Harvey L, Mawhinney R. The Prevention of Infection in Open
Fractures. An Experimental Study of the Effect of Antibiotic Therapy. J Bone Joint Surg 1988;70-A:1341.
