Fractures of the Femur
-
Mechanism of injury.
Femoral neck fractures account for just over half of all proximal
femoral fractures and are most common in patients older than the age of
50 years; elderly patients account for approximately 95% of the total
number of cases (1,2).
These fractures become more common with increasing age because of the
unhappy combination of osteoporosis and an increasing propensity for
falls. Besides osteoporosis, other factors associated with an increased
risk of femoral neck fracture are early menopause (or low estrogen
state), alcoholism, smoking, low body weight, steroid therapy, history
of stroke, phenytoin treatment, and lack of exercise. Excessive use of
sedative drugs has also been implicated (3).
Typical patients are female, fair, and thin. Eating a high fat diet is
“poor dietary habit,” but does not put one at risk. Efforts at
preventing falls in elderly persons seem to have the most potential for
controlling this phenomenon. Trochanteric pads may lessen the risk of
fracture with falls (4), but compliance is poor and their usefulness has been questioned (5). In the elderly, hip fractures result in an increased 1-year mortality rate of 12% to 18%.Femoral neck fractures in younger patients usually
result from high-energy trauma. In addition to traumatic injuries,
stress fractures of the femoral neck may occur in active patients.
Stress fractures that occur along the superior aspect of the femoral
neck are called tension fractures and have a high propensity to progress to complete fractures. The compression stress fracture, which occurs at the base of the femoral neck, is less likely to displace. -
Classification of fractures. From the clinical standpoint, femoral neck fractures are of four basic types:
displaced, nondisplaced, impacted, and the stress fracture. Radiographs
can distinguish these, although some nondisplaced fractures may be
radiographically occult and are only diagnosed after magnetic resonance
imaging (MRI). Approximately two thirds of femoral neck fractures are
displaced (2). -
Symptoms and signs of injury. Patients with stress fractures, nondisplaced fractures, or impacted fractures may complain only of pain in the groin
or sometimes pain in the ipsilateral knee. The patients with stress
fractures have a history of a recent increase in activity and may
believe themselves to have a muscle strain. In contrast, patients with
nondisplaced or impacted fractures have some history of trauma. They
generally have a higher intensity of pain, can associate the onset with
a traumatic event, and are seen early for medical treatment. In all
three groups of patients, there is no obvious deformity on physical
examination, but there is generally pain with internal rotation. A high
index of suspicion must be maintained to avoid delay in diagnosis.
Patients with displaced femoral neck fractures complain of pain in the
entire hip region and lie with the affected limb shortened and
externally rotated. Anteroposterior and high-quality cross-table
lateral (obtained by flexing the uninjured, not the injured, hip)
radiographs of the hip are necessary and sufficient to diagnose
displaced, nondisplaced, and impacted fractures and for planning
treatment. MRI (with Short TI Inversion Recovery STIR images) has been
shown to be the quickest, most cost-effective way of correctly
identifying radiographically occult fractures. Pending treatment,
patients should be non–weight bearing and allowed to rest with the
limbs in the most comfortable position, which is generally in slight
flexion on a pillow. Traction is not necessary and may increase pain. -
Treatment
-
Stress fractures.
These fractures commonly occur in young, vigorous individuals and
require careful evaluation. A high index of suspicion for this injury
should be kept for active patients presenting with groin pain (6). Patients with femoral neck stress fractures often have decreased bone density compared to age-matched controls (7).
Femoral neck stress fractures often heal uneventfully but have the
potential to displace, especially if on the superior/lateral side. Upon
diagnosis, patients should be treated by restricted weight bearing. Use
of crutches or a walker is mandatory, but patients should also be
cautioned not to attempt straight-leg raising exercises and not to use
the leg for leverage in rising or in changing positions, particularly
getting up out of a chair. Partial weight bearing is safe within 6
weeks, with full weight bearing in 12 weeks, as long as the fracture
shows roentgenographic evidence of healing, which is evidenced by
sclerosis at the superior femoral neck. Because of the potentially
severe complications of displacement (nonunion, osteonecrosis, need for
surgery), in-situ pinning should be considered in active or unreliable
patients or any patient with a tension (superior) fracture. Compression
types of fractures in elderly individuals generally do well with
limiting activity as outlined above. Functional complaints may persist
for years in patients with femoral neck stress fractures (8). -
Impacted fractures
-
These can be treated either nonoperatively or operatively (1,9).
With the nonoperative method, the patient usually is kept in bed for a
few days with the leg protected from rotational stresses until the
muscle spasms subside. A program of protected ambulation, as outlined
for stress fractures, is then initiated. In a series of over 300
patients with impacted femoral neck fractures treated nonoperatively,
displacement only occurred in 5% of younger, healthy patients (9). When displacement occurred in these patients, operative treatment led to a successful outcome in all cases (9).
Although the authors of this study suggest that surgery is only
necessary in patients over age 70 with multiple medical problems,
others would argue that even a 5% risk of late displacement is
unacceptable. -
Internal fixation
of impacted fractures has many advantages over nonoperative methods,
especially using percutaneous technique. Although the rate of avascular
necrosis may not be different, a union rate of 100% in operative cases
has been reported, compared to 88% with closed management. The authors
recommend multiple screw fixation, either percutaneous or by open
technique, because it allows immediate weight bearing and avoids the
risk of late displacement (10) (see I.F).
-
-
Displaced fractures.
The management of displaced femoral neck fractures continues to be an
area of controversy. The treatment decision is best based on the
activity level of the patient before the fracture because this is a
direct measure of the functional demands of the patient that should be
restored and because activity level correlates with bone density (1).
Patient’s must be treated with understanding of their physical and
mental abilities. Those that are most debilitated often need the
surgery most. For example, the patient with poor cardiac function,
while not an ideal surgical candidate, also needs to be as active as
possible. The patient with dementia may need surgery as many do not
understand recommendation for non–weight bearing. It is important to
rapidly arrange family discussions and indepthly explain the risks and
benefits of surgical intervention.-
Currently, there is disagreement about
how to best manage displaced fractures in active patients. Certainly,
fractures in healthy patients less than age 60, with or without slight
comminution, should be reduced, impacted, and internally fixed.
Such surgery should be done as quickly as possible. When surgical
repair was carried out within the first 12 hours, a 25% rate of
avascular necrosis was reported, increasing to 30% with surgery between
13 and 24 hours, 40% between 24 and 48 hours, and 100% after 1 week.
P.319
Intracapsular
tamponade from fracture hematoma has an unfavorable effect on femoral
head blood flow, as does nonanatomic position, so there is a rationale
for proceeding with some urgency (1,11,12,13,14,15,16).
However, patients with dehydration or unstable cardiac conditions
should be medically stabilized before surgery to minimize the risk of
fatality (17). There is consensus that accurate reduction and impaction at the fracture site are essential to a good end result.-
Authorities who stress an anatomic reduction with impaction
believe that this allows the maximum opportunity for reestablishment of
the vascular supply. Any stretch or kinking of the vessels of the
ligamentum teres or retinaculum is avoided while stability of the
fracture is optimized (13). Internal fixation with three pins or screws secures fracture stability; there is no value in using more than three implants (10).
An exception to this generalization is the fracture comminuted with
posterior comminution; in this instance the addition of a fourth screw
may confer a little more stability (18). -
Authorities who stress a valgus reduction
believe that this position allows for maximum bone-on-bone stability
and a reduced varus moment arm on the repaired fracture. In a valgus
nailing, the nail or screw is near the center of the head, but the nail
is rested along the calcar of the femoral neck to reduce the distance
between the fulcrum of the nail or screw and the head. This positioning
produces a shorter biomechanical moment and less stress on the device.
Concern that the fixation cuts out superiorly or anteriorly can be
eliminated by proper impaction of the fracture and the use of multiple
pins or a sliding fixation apparatus (10,13).
When valgus nailing is performed, it is more likely that screws will
exit the femoral shaft at or distal to the lesser trochanter, which
increases the risk of late subtrochanteric fracture.
-
-
The authors believe
that an anatomic reduction is preferable to the valgus reduction, but
when faced with a choice between slight valgus and any varus, then
slight valgus is chosen.
-
-
-
Reduction techniques
-
The authors favor a closed reduction
on a fracture table that then allows for the insertion of internal
fixation under two-plane image-intensifier control. Manipulative
reduction should be gentle, and the authors have found the techniques
of McElvenny and Deyerle to be the most satisfactory. Frequently,
however, the fracture is reduced by the maneuver of applying traction
on the limb with neutral adduction-abduction with internal rotation to
bring the femoral neck parallel to the floor. Nonanatomic reduction
should not be accepted; if acceptable reduction is not obtainable by
closed means then open reduction should be considered.-
In McElvenny’s technique,
both extremities are placed in traction with the hips in extension. The
affected leg is lined up with the long axis of the body and is then
maximally internally rotated by rotating the knee rather than the foot
to reduce stress on the knee ligaments. Traction then is released on
the contralateral side. After viewing follow-up radiographs, if more
valgus is required, the traction may be reapplied to the affected leg.
Just before releasing the traction on the opposite leg, an abduction
force at the knee is applied along with a simultaneous pushing inward
over the trochanter. -
The Deyerle technique
achieves final alignment of the femoral neck and head in the lateral
plane by a direct push posteriorly by two hands placed anteriorly over
the greater trochanter while the pelvis on the contralateral side is
supported to prevent ligament stress. This procedure is carried out
after traction and internal rotation have reduced the fracture in the
anteroposterior plane and before placement in slight valgus as
described in a.
-
-
Open methods. Open reduction is performed through either a Smith-Petersen anterior approach or a Watson-Jones anterolateral approach
P.320
when a satisfactory closed reduction cannot be obtained in a patient in whom prosthetic replacement is contraindicated (1).
Although fracture site visualization may be best with the anterior
approach, the screws have to be inserted through a separate lateral
incision. The Watson-Jones interval is a more familiar approach for
many surgeons, but fracture visualization may be a little more
difficult.
-
-
Operative techniques
-
Multiple screws.
The multiple screw method, using three implants, is the simplest method
of obtaining internal fixation. This method can be a percutaneous
procedure, thus reducing the risk of infection and the operative
morbidity in elderly patients, extremely poor-risk patients, and
bedridden patients. The alternative of prosthetic replacement in the
low functional demand patient is chosen except when these criteria
apply (19). When an adequate (anatomic) closed
reduction is obtained, the screws can be placed through a small lateral
incision, but a capsulotomy is recommended by extending the deep
dissection anteriorly. When the reduction is nonanatomic, open
reduction is advised (1,16). -
Sliding hip screw fixation
is an alternative to multiple screw fixation. With anatomic reduction,
no mechanical advantage is obtained with the hip screw because fracture
stability is most dependent on the quality of the reduction and the
density of the bone in the femoral head. However, with a nonanatomic
reduction, there is an advantage to the use of a hip screw because the
fixation relies on the lateral cortex rather than opposition of the
fracture surface (10,13).
A sliding screw plate appears to have the advantage of firm fixation of
the head, as well as allowing for impaction through sliding in a fitted
barrel. An additional threaded pin or cancellous screw should be placed
superiorly in the neck and head for improved torsional control (13).
Regardless of the particular type of mechanism used, it is essential to
obtain maximum holding capacity in the head, which necessitates the use
of a 135-degree angle device in most individuals when anatomic
reduction is obtained. When a valgus reduction is chosen, it is
important to use a 150-degree nail plate device and to position the
nail or screw in the deepest portion of the head. -
Prosthetic replacement.
Many studies have demonstrated improved functional outcomes and
dramatically lower reoperation rates with hemiarthroplasty and total
hip replacement when compared with internal fixation of displaced
femoral neck fractures. However, arthroplasty procedures carry a higher
risk of deep infection, dislocation, and potential need for revision (20). Use of an anterior or lateral approach significantly decreases the risk of dislocation (20).
Hemiarthroplasty of the hip may be performed with unipolar or bipolar
components. Traditionally, a unipolar prosthesis is used for patients
with very low functional demand, while bipolar devices are used in
patients with higher functional demands. However, recent studies have
failed to demonstrate any significant difference in outcomes with
either type of device (21), while bipolar components may contribute polyethylene wear particles with time (22).
Total hip arthroplasty provides the best functional results but is
considered to be associated with a higher risk (10%) of dislocation (23).
Fortunately, the risk of recurrent dislocation and reoperation are not
different than those after primary total hip arthroplasty (24).
The use of larger femoral heads with cross-linked polyethylene and
avoidance of posterior approaches should reduce the risk of
dislocation, although this has not yet been demonstrated in the
literature. Total hip replacement is the procedure of choice when
femoral neck fractures occur in patients with rheumatoid arthritis.
Such fractures are exceedingly rare in patients with degenerative
arthritis of the hip, but total hip arthroplasty would also be
appropriate in these cases. -
The authors’ preference. Multiple screw fixation or a sliding hip screw with an additional pin or screw appears to offer optimum fixation (1,16).
P.321
The techniques are not easily learned or applied and are only effective
with anatomic reduction and maximum fracture impaction at the time of
surgery. Given the difficulties inherent with either technique, the
uncertain end-results if anatomic reduction is not obtained, and the minimum of a 12% avascular necrosis rate,
the surgeon should consider femoral prosthetic replacement as an
alternative in the older patient with low functional demands and poor
bone quality or the very active older patient who will have the best
function after total hip replacement (20).
-
-
Failed primary fixation.
The most frequent complications following internal fixation of
displaced femoral neck fracture are loss of reduction, protrusion of
the screw or pins into the acetabulum, and collapse with symptomatic
avascular necrosis. All of these complications are reliably salvaged by
total hip arthroplasty. -
Postoperative care and rehabilitation.
The aim of treatment is to return the patient to preoperative status by
the quickest, safest method. Therefore, rehabilitation planning should
begin at the time of admission because most patients are elderly and do
not tolerate prolonged periods away from familiar environments (17).
Surgery is carried out as soon as possible, and the procedure should be
one that allows immediate partial or full weight bearing, the first
step in rehabilitation. Attempting to maintain a patient in
non–weight-bearing status is frustrating for the surgeon, therapist,
and family. The use of bedpans and the practice of straight-leg raising
of the intact leg while in bed have been shown to produce considerable
stress across the femoral neck. It is fallacious to attempt to protect
the hip by non–weight-bearing with crutches, because approximately half
the body weight is transmitted across the so-called non–weight-bearing
hip. If the knee and hip are fully flexed, the forces at the hip
approximate total body weight. The dependent position without the
normal pumping action of muscles also predisposes to edema, venous
stasis, and thrombophlebitis. The authors’ experience indicates that,
as long as stable internal fixation is achieved, gains from early
weight bearing far outweigh the risks. Patients are encouraged to
ambulate and to apply as much weight as is comfortable. Initially, a
walker is used, and then gradual progress is made to crutches, if
practical, and eventually a cane. In the case of the patient with
balance problems, the walker or cane may be used indefinitely to help
prevent more falls. -
Nonunion and avascular necrosis
-
In the past, nonunion
has been an important complication, but with proper reduction,
impaction, and internal fixation, its incidence should be reduced to
less than 10% (1,20).
Most fractures heal promptly and the union is well established within 4
months. Occasionally, there is some resorption at the fracture site,
probably a result of insufficient impaction at surgery and therefore
some fracture instability. Further impaction and eventual healing
usually occur, but the incidence of avascular necrosis is significantly
higher than in patients who obtain primary union. -
Avascular necrosis
-
The roentgenographic signs
of avascular necrosis, with associated collapse, can occur at any time
postoperatively. For practical purposes, however, changes with collapse
are usually seen within 3 years. The incidence of avascular necrosis is
variously reported to be within 12% to 35%, and it must be appreciated
that for displaced femoral neck fractures, the head, or at least a
major portion of it, is rendered avascular at the time of injury (1,20).
The lower figure of 12% is identical to that reported by most authors
for impacted valgus fractures and probably represents the lowest
possible incidence. When avascular changes are identified, the patient
should be managed according to symptoms. In many older patients, the
condition may not be severe enough to warrant any further surgery, but
in patients with complete collapse of the femoral head and increasing
pain, early total hip replacement is the treatment of choice. -
The role of bone grafting for either prevention or treatment of avascular necrosis remains uncertain. Currently, evidence for use of bone grafting for either of these conditions on a routine basis is lacking.
-
-
-
Prognosis.
Anticipated complications and end results have been discussed for each
fracture. Because of the advanced age of the typical patient,
development of degenerative articular changes over a long period is
difficult to assess, but it does not appear to be a frequent
complication. The morbidity and mortality rates
(12% for the 12 months following fracture) are high, but they can be
notably decreased by treating this fracture with early reduction and
early ambulation. The mortality rates return to those of age-matched control subjects after 1 year. -
Fractures of the neck of the femur in children (25,26,27)
-
Treatment
-
Transepiphyseal fractures
are uncommon, and there is no series of sufficient size to make any
conclusions about the treatment of choice. The authors recommend
reduction with capsulotomy and fixation with smooth pins (27). -
Undisplaced and minimally displaced cervicotrochanteric fractures
carry a risk of avascular necrosis. The pathophysiology may involve
intracapsular tamponade of the vessels supplying the femoral head (27).
The authors recommend capsulotomy, reduction if necessary, and fixation
with lag screws short of the femoral head epiphysis. The screws are
generally sufficient because of the density of the bone. In children 8
years old and younger, postoperative spica cast immobilization is also
used for 6 to 12 weeks. Displaced fractures are treated in the same
way. These fractures must be treated emergently to minimize the
complication of avascular necrosis.
-
-
Prognosis. These fractures have nearly a 100% rate of union with optimum management.
-
Complications
-
Coxa vara. Although this complication is commonly reported, it is generally associated with nonoperative management.
-
Avascular necrosis.
This complication affects 0% to 17% of patients who undergo emergent
treatment. The long-term consequence is generally degenerative
arthritis, which requires total hip arthroplasty in patients in their
40s to 60s. -
Premature closure of the epiphysis occurred in 7% of the patients in Lam’s series (26). This complication is not a significant long-term problem except when it occurs in children younger than 8 years.
-
-
-
Surgical anatomy
-
The classic intertrochanteric fracture occurs in a line between the greater and lesser trochanters.
Although in theory such a fracture is totally extracapsular, the
distinction between an intertrochanteric fracture and a basilar femoral
neck fracture is not always clear. In peritrochanteric fractures, the
internal rotators of the hip remain with the distal fragment, whereas
usually at least some of the short, external rotators are still
attached to the proximal head and neck fragment. This factor becomes
important in reducing the fracture because, in order to align the
distal fragment to the proximal one, the leg must be in some degree of
external rotation. This is in contrast to the internal rotation often
needed to reduce transcervical femoral neck fractures and requires a
distinctly different maneuver in the operating room with the patient on
the fracture table to reduce the fracture. -
When the forces producing the fracture
are increased, the greater trochanter and lesser trochanter can be
separately fractured and appear as separated fragments (three- and four-part fractures).
Secondary comminution is not infrequent and usually involves one of the
four major fragments. Anatomic restoration becomes a major undertaking
but is not necessary to obtain a satisfactory result from a functional
point of view. Occasionally, a subtrochanteric extension of the
fracture is encountered.
-
-
Mechanism of injury.
The intertrochanteric fracture almost invariably occurs as a result of
a fall in which both direct and indirect forces are acting. Direct
forces act
P.323
along
the long axis of the femur or directly over the trochanter. Indirect
forces include the pull of the iliopsoas muscle on the lesser
trochanter and that of the abductors on the greater trochanter. -
Classification. A number of classifications and subclassifications have been proposed (29,30).
From the standpoint of treatment and prognosis, a simple classification
into stable or unstable fractures is most satisfactory.-
A stable intertrochanteric fracture
is one in which it is possible for the medial cortex of the femur to
butt against the medial cortex of the calcar of the femoral neck
fragment. Not uncommonly, the lesser trochanter is fractured off as a
small secondary fragment, but this does not interfere with the basic
stability of the fracture. -
The unstable intertrochanteric fracture
is one in which there is comminution of the posteromedial-medial cortex
(along the calcar femorale). In the most common unstable pattern, a
large posteromedial fragment encompasses the lesser trochanter, with or
without a fracture through the greater trochanter (four-part fracture).
A fracture with high obliquity may be considered unstable because of
the high shearing force at the fracture site despite anatomic reduction
and internal fixation.
-
-
Physical examination.
The fracture occurs primarily in the elderly, the average age reported
being 66 to 76 years, which is slightly older than for femoral neck
fractures. There is a predominance in women, with a ratio of occurrence
in women to men of 2:1 to 8:1. The leg is shortened and lies in marked
external rotation. Any movement of the extremity is painful and should
not be attempted. If traction is applied with a Thomas splint for
patient transport, it should be removed before radiographs are obtained
because the ring interferes with proper assessment of the fracture.
Both anteroposterior and lateral radiographs should be made to confirm
the diagnosis and to delineate the fracture pattern. The lateral film
is obtained as a cross-table view, which can be obtained by flexing the
uninjured hip. -
Treatment.
Operative treatment is the procedure of choice if a skilled
anesthesiologist and surgeon are available. The more debilitated the
patient, the more urgent the indications. The goal of treatment must be
to restore the patient to preoperative status as early as possible,
which can be achieved best through reduction and internal fixation in a
stable fashion so as to allow early ambulation. As with intracapsular
fractures, if the patient is first seen with unstable medical
conditions, these should be stabilized before surgery to minimize the
risk of perioperative morbidity and mortality (17).
If there are complicating injuries or illnesses that make it impossible
to carry out operative reduction and fixation, well-leg traction is
remarkably well suited to this situation. The leg must be held in some
external rotation to maintain reduction of the fracture. This treatment
allows movement from bed to chair and eliminates cumbersome traction
apparatus for transport. Because treatment necessitates the use of
crutches following the period of bed rest, weights should be used for
strengthening the upper extremities. Great care must be taken to avoid
secondary complications such as pressure areas over the sacrum and the
heels, equinus contractures of the foot, and thromboembolic disease.
Traction must be maintained until there is callus seen on radiographs
usually approximately 8 weeks. Following this period, mobilization may
begin using non–weight bearing and parallel bars, a walker, or
crutches. The hip must be protected until there is mature callus and
bridging bone an additional 4 to 6 weeks. The use of a cane in the
opposite hand should be encouraged indefinitely to help prevent
subsequent falls and injury.-
Operative treatment of intertrochanteric fractures.
Currently, the sliding hip screw is the “gold standard” for the
fixation of stable and unstable trochanteric fractures of the femur (31). “Fixed angle” devices that do not allow collapse of the fracture produce inferior results (29).
There has been renewed interest in the use of intramedullary devices
whose use is perceived as less invasive and associated with less
perioperative morbidity. However, structured literature reviews show no
difference in outcomes between intramedullary devices and sliding hip
screws, except for a greater incidence of
P.324
both intraoperative and late femur fracture associated with intramedullary fixation (32,33).
Most of the current available internal fixation devices for treatment
of intertrochanteric fractures can be expected to yield satisfactory
results.-
When using a sliding hip screw,
the fracture must be reduced to a stable position; that is, the medial
cortices must abut each other anatomically. What is potentially a
stable fracture can be converted into an unstable situation by
inadequate reduction of the medial cortices. The reduction is
accomplished on a fracture table by direct traction, slight abduction,
and external rotation. If these maneuvers do not produce an anatomic
reduction, the fracture site should be opened to ensure stability of
the reduction. Not infrequently, there is some posterior displacement
at the fracture site that requires the femur shaft to be lifted
anteriorly to secure an anatomic reduction at the time of fixation.
Regardless of the internal fixation used, in the elderly osteoporotic
patient, the neck itself might be little more than a hollow tube; to
gain purchase, it is essential to insert the nail or screw well into
the head. The authors recommend insertion to within 0.5 inch of the
subchondral bone. The position should be in the center of the femoral
head on both views (34,35).
Baumgaertner has popularized the “tip-apex distance” as a way to
emphasize the center/center position within the femoral head. The plate
should be securely fixed across both femoral cortices by four screws. The
authors believe that a properly inserted sliding screw plate with the
wide, threaded, blunt-nosed screw offers the best mechanical fixation
for intertrochanteric fractures (Fig. 23-1). With unstable fracture patterns, a trochanteric plate may be used to prevent excessive collapse (31). -
When intramedullary devices
such as the Gamma nail are used, one must be careful to ream adequately
and always insert the nail by hand to avoid intraoperative fracture.
Long devices should be used to prevent later fracture at the tip of the
stem; however, long intramedullary implants risk perforation of the
distal anterior femoral cortex (33,36,37). -
In osteoporotic patients with highly comminuted fractures, hemiarthroplasty in total hip replacement may rarely be indicated (38). Comparative data are lacking to know whether outcomes are any different with arthroplasty compared to internal fixation.
-
A special fracture that deserves mention is the reverse obliquity fracture (Fig. 23-2).
With this pattern, the primary fracture line is parallel to the axis of
the femoral neck and the sliding vector of the hip screw. This results
in tremendous instability and very high failure rates when sliding hip
screws are used (39). Fractures with this pattern are better stabilized with intramedullary implants or fixed-angle 95-degree devices.
-
-
-
Postoperative treatment.
There is little agreement in the literature as to what constitutes the
best postoperative management of intertrochanteric fractures. Our
recommendation for rehabilitation is that patients be moved to at least
a sitting position on the first postoperative day. In 2 to 3 days, they
should be taken to the physical therapy department where ambulation can
be started using the parallel bars. Patients may be allowed to place as
much weight on the fractured extremity as they wish. They are not
forced to go beyond what is comfortable for them but are reassured that
some weight bearing is desirable and not to be feared. As soon as they
feel secure using the parallel bars, patients should be transferred to
a walker or crutches, depending on their abilities based on their
prefracture status. With this program, it is rare that individuals who
were able to walk without support before fracture cannot be returned to
a self-sufficient state within 10 to 14 days using either a walker or
crutches. Patients may disregard the walker or crutches at any time
they feel secure. The long-term use of a cane is encouraged as a
preventive measure in elderly patients to avoid falls and injury. -
Prognosis and complications. Because of the age of patients (many suffer from other debilitating conditions at the time of injury), mortality and morbidity rates
P.325
.
will always be significant
With an aggressive treatment program, mortality rate should be 10% to
15% for the first year after the fracture; subsequently, the mortality
rate returns to that of age-matched controls. Mechanical failure and
non-union can be reduced to 1% or less. Avascular necrosis is rare but
has been reported (40). Infection is still a
problem, with most series reporting an incidence of deep infections of
1% to 5%. This rate can be significantly decreased by careful soft
tissue technique (11,41) and the use of prophylactic antibiotics for 24 hours.
P.326
With prompt internal fixation and an aggressive postoperative
rehabilitation program stressing early weight bearing, complications
from thromboembolic disease can be sharply reduced. The authors
recommend the use of sequential compression devices and aspirin for all
patients with the use of a low-dose warfarin of enoxaparin regimen. Even
with optimum treatment, it is scarcely possible to return more than 40%
of the patients to their true prefracture status, but one can obtain
satisfactory results from treatment in approximately 80% of patients. Prophylactic antibiotics are recommended as discussed in Chap. 8, IV.E, and Chap. 10, I.B.2.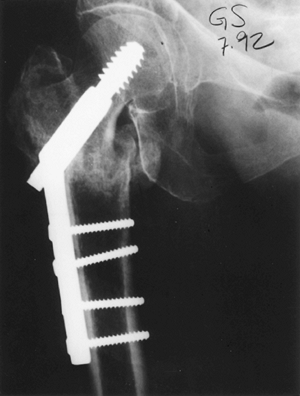 Figure 23-1.
Figure 23-1.
A sliding screw plate. Note the proper positioning for maximum fixation
with the screw centrally seated in the head within 1 cm of the
subchondral bone. Four screws are used to insert the slide plate onto
the femur.![]() Figure 23-2. Reverse obliquity fracture.
Figure 23-2. Reverse obliquity fracture.
-
Isolated avulsion or comminuted fractures of the greater trochanter occasionally are seen. Unless displacement of the fragment is greater than 1 cm,
the fracture is treated as a soft-tissue injury with protected weight
bearing until the patient is asymptomatic. Several days of bed rest are
usually required, followed by walker
P.327
or crutch ambulation for 3 to 4 weeks. In elderly patients, even with separation greater than 1 cm, operative treatment with internal fixation rarely is indicated. -
In the younger patient, when displacement is greater than 1 cm,
it is advisable to fix the fracture fragment internally with either two
cancellous screws or a wire loop to secure fragments. This maneuver
reconstitutes the functional integrity of the abductor mechanism.
Postoperatively, the extremity is protected until soft-tissue healing
is secured. Then the patient is allowed to ambulate without weight
bearing for 3 to 4 weeks, followed by partial weight bearing for
another 3 to 4 weeks until limp-free walking can be achieved.
-
With displacement greater than 2 cm,
it is advisable to stabilize the avulsed fragment with a cancellous
screw or a cortical screw, securing it to the opposite cortex. This
procedure is most readily accomplished through a medial approach to the
hip. Complications are minimal, and the end result is most satisfactory.
-
Subtrochanteric fractures occur as extensions of intertrochanteric fractures or as independent entities (11).
The mechanism is direct trauma, and significant forces usually are
required. This type of fracture is ordinarily seen in younger
individuals as compared with the intertrochanteric or femoral neck
fracture. Subtrochanteric fractures, which are extensions of
intertrochanteric fractures, are also seen in elderly patients. Thus,
these fractures have a bimodal distribution. -
Classification. Fielding (see Selected Historical Readings)
classified subtrochanteric fractures as occurring in three zones: zone
I, those at the level of the lesser trochanter; zone II, those 1 to 2
in below the upper border of the lesser trochanter; zone III, those 2
to 3 in below the upper border of the lesser trochanter. Seinsheimer’s
classification and results have emphasized the importance of the
posteromedial fragment. Internal fixation then acts as a tension band
on the outer (distracting) cortex and allows for impaction and weight
bearing directly through the medial cortex. If this internal fixation
is not possible, the fracture pattern is unstable. The most practical
classification of subtrochanteric fractures is the system of Russell (75)
et al., which divides such injuries into high and low fractures and has
direct implications for the most appropriate type of internal fixation (39).
High fractures occur above the lesser trochanter and may or may not
involve the greater trochanter and piriformis fossa of the proximal
femur. Fractures that involve the piriformis fossa require plate
fixation or trochanteric nailing. High fractures not involving the
piriformis fossa may be treated by reconstruction nailing. Low
fractures occur below the lesser trochanter, may or not be comminuted,
and have varying degrees of extension down the femoral shaft. These
fractures, regardless of pattern, are readily treated with standard
intramedullary nails. -
Physical examination.
Because the forces required to produce the fracture are substantial,
other injuries in the same extremity and elsewhere in the body often
occur. Emergency splinting in a Thomas splint generally is required.
Hemorrhage in the thigh may be significant, so the patient should be
monitored for hypovolemic shock, and blood replacement may be
necessary. Good anteroposterior and lateral radiographs are necessary
to clearly assess the extent of the fracture. -
Treatment.
Operative stabilization to allow early rehabilitation is the treatment
of choice. Traction may rarely be necessary for the severely comminuted
fracture, but the healing time is longer than for an intertrochanteric
fracture, and delayed unions and malunions frequently are encountered.
Skeletal traction should be used and applied in such a way as to align
the distal fragment to the proximal fragment. If the lesser
trochanteric fragment with its attached iliopsoas muscle remains intact
on the head and neck fragment, it is necessary to flex and externally
rotate the distal fragment to obtain reduction. The strong adductors
attached to the femoral shaft tend to cause varus angulation, and
attempts to correct this by abduction of the hip often exert pull on
the adductors and cause bowing at the fracture site or medial
displacement of the shaft fragment. In this event, it is best for the
patient to undergo treatment in a neutral position with reference to
abduction-adduction and to increase the traction. When the fracture is
comminuted and the lesser trochanter is off as a separate piece,
treatment is the same as for intertrochanteric fractures. If traction
treatment is used, it should be maintained until there is
roentgenographic evidence of union. The patient is then placed in a
single spica cast or hip abduction brace for protected weight bearing
until the callus matures. -
Operative treatment
-
Fractures involving the lesser trochanter
(Fielding zone I). Fractures in this region not involving the
piriformis fossa may be treated with intramedullary nailing using a
second-generation (reconstruction) nail with fixation into the femoral
neck and head. When there is comminution involving the piriformis,
there are two potential options. The first is to proceed with
intramedullary nailing using a trochanteric nail, again with proximal
fixation in the femoral neck and head. This may be difficult because
the nail may still need to be inserted directly through the fracture
site. In the author’s opinion, use of a 95-degree fixed-angle device
such as a blade plate or dynamic condylar screw is the ideal method for
these fractures. With either method, the procedure is facilitated by
use of a fracture table and with the patient in the lateral position. Indirect reduction techniques
should be used to restore length, rotation, and alignment; it is not
necessary to expose, manipulate, or bone-graft the comminuted region of
the lesser trochanter. -
Fractures below the lesser trochanter (Fielding zones II and III). These fractures represent proximal femoral shaft fractures and are usually amenable to
P.330
the same techniques of fixation (i.e., intramedullary nailing) (42).
Compression plating is equally satisfactory in the hands of persons
familiar with its application, but it is not used routinely because of
the large surgical dissection required.
-
-
Postoperative management.
Stable subtrochanteric fractures or those that can be rendered stable
by operative treatment can be managed much as intertrochanteric
fractures. The unstable subtrochanteric fracture must be supported and
protected from weight bearing until the union is secure. -
Complications.
In the event of a frank nonunion or a delay in union of an
intertrochanteric or subtrochanteric fracture, a careful assessment of
the cause of this failure should be made. Too often it is caused by
less-than-strict adherence to the treatment principles outlined. If the
fixation is secure and the reduction adequate, bone grafting may
suffice. As soon as problems with union are recognized, optimal
position of the fracture should be obtained and standard internal
fixation combined with fresh autogenous cancellous grafting carried
out. Osteotomy may be required, especially if there is varus
malposition of the proximal femur. Once this process is completed, the
management is the same as for a fresh fracture, except that it may be
necessary to delay patient activity until discomfort from the graft
donor site has subsided.
aligning the distal fragment to the proximal one. Often, this requires
that traction be applied with the hip and knee flexed (90-90 traction).
Traction is maintained until the fracture is stable (4–6 weeks), at
which time the extremity is placed in a single spica cast for
immobilization until union is solid (approximately 12 weeks).
Increasingly, percutaneous pin or screw fixation with supplemental
spica casting is used. The authors favor reduction and percutaneous
Steinmann pin fixation followed by supplemental spica casting.
-
Diaphyseal fractures of the femur are the result of significant trauma and usually are associated with considerable soft-tissue damage.
Blood loss of 2 to 3 units is common. In addition, these fractures have
a high incidence of associated injury in the same extremity (46,47), including fractures of the femoral neck (48), posterior fracture-dislocations of the hip, tears of the collateral ligaments of the knee (47), and osteochondral fractures involving the distal femur or patella and fractures of the tibia (46). -
Examination.
Diagnosis usually does not present any clinical problem if care is
taken to rule out the other associated injuries by physical examination
and radiographs. -
Radiographs. Films are obtained primarily to confirm the diagnosis and for preoperative planning. It is essential
to view the joint above and the joint below the fracture. Films of the
uninjured femur are helpful for selecting the appropriate internal
fixation device. An anteroposterior and lateral roentgenogram of the
injured femur should be supplemented by the anteroposterior pelvis to
obtain optimum views of the femoral neck (49).
Unpublished data indicate that routine computed tomographic (CT)
imaging of the femoral neck reduces the rate of missed ipsilateral
femoral neck fracture. -
Treatment
-
Emergency treatment consists of the
immediate application of a Thomas or Hare splint before radiographs are
obtained. Unless there is gross comminution or the patient is not a
surgical candidate, fractures of the shaft of the femur from the lesser
trochanter to approximately 10 cm above the knee joint should be
treated by closed antegrade interlocking nailing (see Fig. 25-3), with reaming of the canal using flexible reamers and prebent nails (44,45).
Current areas of controversy include the role of retrograde nailing and
the timing of surgery. In general, once associated body cavity and
other extremity injuries are ruled out, the patient should receive
urgent operative stabilization. The more severely injured the patient,
the more critical stable fixation of the femur fracture becomes. Early
fixation has been shown to be
P.331
associated
with decreased narcotic use, reduced pulmonary complications (e.g.,
adult respiratory distress syndrome), and decreased mortality rate (43).
Even patients with isolated femoral shaft fractures, including elderly
patients, benefit from urgent (within 24 hours of admission)
stabilization of the femur with an interlocking nail (43,50,51).
These procedures are carried out on a fracture table in the operating
room under fluoroscopic control, although some authors report good
results with nailing on a standard radiolucent table (52).
Although many authors recommend routine supine positioning because of
the ease of placement of locking bolts, we favor the lateral position
on the fracture table when the patient does not have chest, abdominal,
or pelvic injuries. This allows greater ease of access to the greater
trochanter and use of smaller incisions in large patients. When the
patient is severely traumatized, especially those with traumatic brain
injuries at risk for secondary brain insults, fracture stability can be
achieved with external fixation or plates much more rapidly on a
standard table. The fixator is generally exchanged for an interlocking
nail within the first 5 to 7 days when the patient’s condition has
stabilized. Primary interlocking nailing immediately following
debridement is the procedure of choice for most open femoral shaft
fractures (53). Some advocate the use of small
diameter locked nails without reaming, especially in patients with
severe cardiopulmonary trauma; this has been associated with longer
healing time and implant failure (54,55,56). -
Recently, implants for retrograde locked nailing have been developed (57,58).
Indications for retrograde nailing include severe obesity, pregnancy,
bilateral fractures, and ipsilateral tibia, patella, or acetabular
fractures (that require repair via a posterior hip approach) (59). -
Balanced suspension skeletal traction may
be used until a cast-brace can be applied only when the equipment or
expertise necessary for locked nailing is unavailable and when the
patient cannot be transported (60).
-
-
Complications
-
Associated vascular and nerve damage,
especially a transient peroneal or pudendal nerve palsy, is not
uncommon. These problems are generally associated with excessive or
prolonged traction. -
Shortening and malrotation of the extremity frequently occur (61),
even with intramedullary nailing. Slight shortening is associated with
earlier fracture union, and shortening up to 0.5 inch should be
accepted without hesitation. -
Skin breakdown over bony prominences and pin track infections are complications of traction.
-
Infection is extremely rare with the closed nailing technique (62).
-
Nonunion
occurs in approximately 1% of fractures treated with nailing. This
problem is easily managed with nail removal, reaming, and repeat
nailing. Healing complications are more common when small-diameter
nails are used. -
Rotational malunion occurs in 10% to 20% of patients; the deformity is generally external rotation (63).
-
Weakness of the abductor muscles and hip pain can occur in one third of patients (64,65).
-
Knee injuries are common after femoral shaft fractures (66).
-
-
For children younger than 6 to 8 years
with an uncomplicated, isolated femoral shaft fracture, a spica cast
can be used for primary treatment. The technique is as follows (67):-
When the patient’s general condition has
stabilized, usually after at least 24 hours of observation in 2 to 3 lb
of Buck’s traction, the patient is placed under general anesthesia on a
fracture table. The feet are placed in stirrups, and traction is
applied. If necessary, a sling attached to an overhead bar may support
the fractured thigh to restore the normal anterior bow of the femur.
For a
P.332
child
younger than 2 years, it may be desirable to flex the hip and knee to
90 degrees. For the older child, the hip is flexed approximately 20 to
30 degrees, abducted 20 degrees, and externally rotated to best align
the distal fragment to the proximal fragment. The knees are kept
extended. Radiographs are made to verify the reduction. The object of
manipulation is to provide approximately 1 cm of overriding of the
fragments (bayonet apposition in good alignment in both planes). When
this position has been achieved, the skin between the knees and ankles
is then sprayed with medical adhesive. A single layer of bias-cut
stockinet is wrapped over the entire area as described for extremity
casting (see Chap. 7).
Quarter-inch felt, sponge rubber, or several additional turns of Webril
may be used over bony prominences except between the knee and ankle. A double hip spica cast
is then applied, molded carefully around the pelvis, and extended to
embrace the rib margin. When the cast has hardened, the foot pieces of
the fracture table are removed, and if radiographs confirm the proper
position, the cast is extended to include both feet and ankles, which
are well padded, in a neutral position. A crossbar is added to the cast. -
Postcasting treatment.
Follow-up radiographs are made at 1, 2, and 3 weeks to be certain of
the maintenance of position. The cast is worn for 6 to 12 weeks,
depending on the age of the patient and the type of fracture. The
family must be instructed in cast care and told to alert the physician
if there is any evidence of pain, fever, or loss of extension of the
great toe.
-
-
Children older than 8 years
are not ideally managed with spica casts and usually receive some sort
of operative fixation. Antegrade interlocking nails, as used in adults,
are not appropriate in skeletally immature patients because of the risk
of osteonecrosis of the hip. For transverse, length stable fractures,
retrograde flexible nailing has gained increased acceptance (68).
Trochanteric nails may be considered for the teenage child with
fractures of the diaphysis of the femur. The starting point for the
nail should be moved slightly lateral to decrease the risk of avascular
necrosis. Compression plating remains a very good option (69); percutaneous submuscular plating is another recent option. -
Children with head injuries
or multiple trauma should be managed with operative stabilization. In
patients younger than 12 years, this should involve plates, retrograde
flexible nails, or external fixators. Children older than 12 years may
undergo treatment with intramedullary nails.
-
Mechanism of injury.
In older individuals, these fractures are sustained with minimal
trauma. In young people, these fractures generally are caused by
massive trauma and often are associated with vascular and other
soft-tissue injuries. This fracture has a bimodal age distribution as
well. -
Examination.
A careful assessment of nerve and vascular status distal to the
fracture is critical here as with any fracture. Care must be taken to
ascertain any injuries to the soft tissues about the knee and whether
the fracture extends into the joint. -
Radiographs. Anteroposterior, lateral, and, occasionally, oblique views are necessary.
-
Treatment
-
Displaced unicondylar fractures
should be treated by open reduction and internal fixation. Although
good results can be anticipated with use of traditional devices such as
the dynamic condylar screw or blade plate (35),
newer periarticular plates may be an advantage. Retrograde nailing is
advocated by many; its advantages include a less invasive approach and
better stabilization in severely osteoporotic patients. -
Undisplaced supracondylar fractures
or fractures displaced less than 1 mm involving the joint surface may
be treated by percutaneous screw fixation, generally with cannulated
screw systems. Alternatively, a hinged knee brace or cast-brace may be
used, but frequent radiographs must be obtained. In either case, early
motion must be initiated to optimize results.
P.333
Inferior results with nonoperative management for these fractures has been documented (70). -
Extra-articular distal femur fractures or those occurring above total knee replacements can be nicely managed with retrograde supracondylar nails (71,72) or standard antegrade nails (73).
-
Displaced intra-articular or supracondylar fractures are managed by internal fixation (41,58,74,75).
The fracture requires open reduction of the joint surface via a lateral
or anterolateral approach to ensure that it is anatomically reduced.
Minimal stripping of the soft-tissue attachments to the extra-articular
fragments must be completed. This speeds union and decreases the need
for bone grafting while minimizing infection (76).
A 95-degree condylar blade plate or dynamic condylar screw is the
optimum device for fixing these fractures, but they require 1.5 to 2.0
cm of intact bone proximal to the compression screw or blade (75).
With extremely comminuted fractures, a condylar buttress plate is
required, which allows for more screws into the distal fragment.
Fixed-angle locking plates have revolutionized the care of these
fractures (74). Medial or varus collapse is
prevented, and fixation in osteoporotic bone is improved. Minor
malunion is common with the use of fixed angle devices (77).
If the expertise or equipment to perform these procedures does not
exist and the patient cannot be transported to a facility where they
are available, skeletal traction can be used. A tibial pin is inserted
with the knee flexed 20 degrees, and balanced suspension is used. Early
active quadriceps exercises are necessary to prevent joint fibrosis.
Because of the pull of the gastrocnemius, which extends the fracture,
the flexed position should be maintained for the first several weeks.
The distal fragment must be aligned to the proximal fragment, which is
usually in external rotation.
-
-
Postoperative care.
Continuous passive motion is used while the patient is in the hospital
and may be extended to the early posthospitalization period (first 3
weeks) in most cases in which stable internal fixation has been
achieved. A hinged-knee brace is generally used for 6 weeks. The goal
of full extension and 120 degrees of flexion by 6 weeks postoperatively
is standard. Full weight bearing is delayed for 10 to 12 weeks.
Strengthening exercises can then be initiated. Patients in traction
require aggressive physical therapy to regain full extension and 90
degrees of flexion. Active and gentle passive motion protocols are
initiated once the fracture is clinically and radiographically healed
at about 8 weeks after injury. Some permanent loss of motion is
expected for fractures treated this way as well as for severe
intra-articular fractures managed operatively (74).
internal fixation (ORIF) of fracture with multiple pins/ screws for all
impacted and nondisplaced fractures and for displaced fractures in
active patients with good bone density. Patients with pre-existing
arthritis or significant osteoporosis should receive a prosthetic
replacement (hemiarthroplasty or total hip replacement).
Hemiarthroplasty done through an anterior or posterior approach to the
hip rehabilitation is easier with the anterior approach but access to
the proximal femur is slightly more difficult. In active elderly
patients, total hip replacement is considered, and when done, a large
(36–40 mm) head is used with highly cross-linked polyethylene.
pelvis and lateral hip radiographs, clinical examination. Patient’s leg
will be shortened and externally rotated.
with sliding hip screw or trochanteric nail. The latter is used for
reverse oblique fractures and at surgeon discretion. Rarely, extremely
comminuted fractures in extremely osteoporotic individuals are treated
with prosthetic replacement.
pelvis and lateral proximal femur radiographs, clinical examination.
Again, patient’s leg will be shortened and externally rotated.
involvement of the piriformis fossa. Fractures below the piriformis
fossa are treated by closed reduction and interlocking nail placement.
Open reduction may be required in certain fracture patterns to ensure
proper placement of the implant. If the lesser trochanter is not
attached to the proximal fragment, a “second-generation” interlocking
nail where the proximal interlocking screws are directed into the
femoral head and neck are required. Fractures above the piriformis
fossa may be treated by a sliding hip screw, 95-degree condylar screw,
blade plate, or proximal femoral nail.
isolated fractures, the implant is inserted with the patient on the
fracture table in the lateral decubitus position. Nailing of fractures
as described is preferred; rarely a 95-degrees device such as a
condylar screw or blade plate is preferred based on fracture pattern
considerations.
and lateral radiographs of the femur, clinical examination. CT imaging
of the hip is routinely reviewed for occult femoral neck fracture.
isolated fractures, closed interlocking nail placement on the fracture
table with the patient in the lateral decubitus position. For patients
with multisystem trauma, the nailing can be done with the patient
supine on a radiolucent table with a C-arm. Rarely, a plate or the
temporary use of an external fixator followed by conversion to an
interlocking nail is indicated within the first 2 weeks after injury.
Retrograde nails are used for specific indications, including the
morbidly obese and ipsilateral tibial or patellar fractures.
with plate and screws for most younger patients with articular
extension. Retrograde nailing with or without lag screws for patients
who are obese, osteoporotic, have a fracture above a knee prosthesis.
Active range-of-motion (AROM) and limited weight bearing for 12 weeks.
S, Ogunremi L, Chinappen U. Acceptability and compliance with hip
protectors in community-dwelling women at high risk of hip fracture. Rheumatology 2003;42:769–772.
MF, Harrington RM, Keller TS, et al. Torsion and bending analyses of
internal fixation techniques for femoral neck fractures: the role of
implant design and bone density. J Orthop Res 1987;5:433–444.
B. Femoral head vitality after intracapsular hip fracture: 490 cases
studied by intravital tetracycline labeling and TC-MDP radionuclide
imagery. Acta Orthop Scand 1983;54(S200):1–71.
JE, McCarthy RE, Lowell JD, et al. Hip fracture mortality: relation to
age, treatment, preoperative illness, time of surgery, and
complications. Clin Orthop 1984;186:45–56.
JI, Simon JA, Kummer FJ, et al. Internal fixation of femoral neck
fractures with posterior comminution: a biomechanical study. J Orthop Trauma 1999;13:155–159.
JM, Barrington R. Internal fixation vs. hemiarthroplasty for the
displaced subcapital fracture of the femur: a prospective randomized
study. J Bone Joint Surg (Br) 1981;63:357–361.
GL, Keller RB, Littenberg B, et al. Outcomes after displaced fractures
of the femoral neck: a meta-analysis of one hundred and six published
reports. J Bone Joint Surg (Am) 1994;76:15–25.
SH, Bansal M, Cornell CN, et al. Failure of bipolar hemiarthroplasty: a
retrospective review of 31 consecutive bipolar prostheses converted to
total hip arthroplasty. Am J Orthop 2001;30:313–319.
JA, Patel RV, Booth RE, et al. Outcomes of total hip arthroplasty are
similar for patients with displaced femoral neck fractures and
osteoarthritis. Clin Orthop 2004;421:151–154.
MF, Winquist RA, Hansen ST. Fractures of the femoral neck in patients
between the ages of twelve and forty-nine years. J Bone Joint Surg (Am) 1984b;66:837–846.
GC, Gibson GF, Ackrund CE, et al. The fixation and prognosis of
trochanteric fractures. A randomized, prospective controlled trial. Clin Orthop 1990;254:242–246.
S, Friberg S, Hansson LI. Trochanteric fractures; influence of
reduction and implant position in impaction and complications. Clin Orthop 1990;259:130–138.
MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails
versus extramedullary implants for extracapsular hip fractures. Cochrane Database Syst Rev 2002;1:pCD000093.
MR, Curtin SL, Lindskog DM, et al. The value of the tip-apex distance
in predicting failure of fixation of peritrochanteric fractures of the
hip. J Bone Joint Surg (Am) 1995;77:1058–1064.
DCR, Descamps PY, Krallis P, et al. Use of an intramedullary hip-screw
compared with a compression hip-screw with a plate for
intertrochanteric femoral fractures: a prospective, randomized study of
one hundred patients. J Bone Joint Surgery (Am) 1998;80:618–630.
S, Moore T, Proano F. Bipolar prosthetic replacement for the management
of unstable intertrochanteric hip fractures in the elderly. Clin Orthop 1987;224: 169–177.
BR, Carmen B, Clifford P. The results of open reduction and internal
fixation of distal femur fractures using a biologic (indirect)
reduction technique. J Orthop Trauma 1996;6:372–377.
D, Fleming CH, Matta JM, et al. Comminuted and rotationally unstable
fractures of the femur treated with an interlocking nail. Clin Orthop 1986;212:35–47.
DJ, Kreder HJ, Schemitsch EH, et al. Femoral intramedullary nailing:
comparison of fracture-table and manual traction. A prospective,
randomized study. J Bone Joint Surg (Am) 2002;84:1514–1521.
M, Guyatt GH, Tong D, et al. Reamed versus nonreamed intramedullary
nailing of lower extremity long bone fracture: a systematic overview
and meta-analysis. J Orthop Trauma 2000;14:2–9.
KD, Johnston DWC, Parker B. Comminuted femoral-shaft fractures:
treatment by roller traction, cerclage wires, and an intramedullary
nail, or an interlocking intramedullary nail. J Bone Joint Surg (Am) 1984;66:1222–1235.
SK, Melder I, Henley MB, et al. Closed interlocking nailing of femoral
shaft fractures: assessment of technical complications and functional
outcomes by comparison of a prospective database with retrospective
review. J Orthop Trauma 1993;7:118–122.
J, Bliss MJ, Eberson CP, et al. Social and economic benefits of
flexible intramedullary nails in the treatment of pediatric femoral
shaft fractures. Orthopedics 2002;25:1067–1070.
MS, Krikler SJ, Ali MS. Displaced fractures of the distal femur in
elderly patients; operative vs. non-operative treatment. J Bone Joint Surg (Br) 1995;77: 110–114.
RJ, Toal TR, Murphy-Zane MS, et al. Immediate weight-bearing after
treatment of a comminuted fracture of the femoral shaft with a
statically locked intramedullary nail. J Bone Joint Surg (Am) 1999;81:1538–1544.
KS, Shen WY, So WS, et al. Interlocking intramedullary nailing for
supracondylar and intracondylar fractures of the distal part of the
femur. J Bone Joint Surg (Am) 1991;73:333–340.
PJ. Distal femur fractures with complex articular involvement:
management by articular exposure and submuscular fixation. Orthop Clin North Am 2002;33: 153–175.
MK, Marohesi DG, Burch H, et al. Alignment of
supracondylar/intracondylar fractures of the femur after internal
fixation by AO/ASIF technique. J Orthop Trauma 1992;6:318–326.

