FRACTURES OF THE DISTAL RADIUS
Department of Orthopaedics and Surgery, Division of Plastic Surgery,
Hand and Upper Extremity Service, University of California, Davis,
School of Medicine, Sacramento, California 95817.
ascertained, it will be a very easy matter to explain the different
phenomena attendant on it, and to point out a method of treatment which
will prove completely successful.
radius fractures often leaves much to be desired. The fracture that
Abraham Colles described in 1814 was nonarticular and occurred during a
fall on the outstretched hand in a somewhat osteoporotic patient. All
distal radius fractures with dorsal displacement are commonly referred
to as “Colles’ fractures” regardless of the fracture configuration,
degree of comminution, age of the patient, or mechanism of the injury.
Because of their frequency, Colles’ fractures are often regarded and
treated casually. Controversy and confusion are found throughout the
medical literature about the best way to treat a fracture of the distal
radius. The fundamental principle of treatment is the restoration of
anatomy with the hope of producing full, painless motion of the wrist.
The method selected to achieve this objective can be determined only
after careful study of the individual fracture pattern.
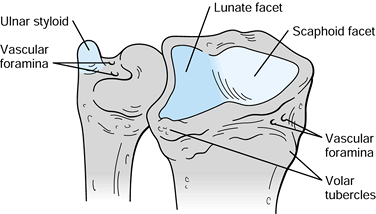
with hyaline cartilage. A smooth anteroposterior ridge divides the
articular surface into two facets: a triangular
lateral facet, which articulates with the scaphoid, and a quadrilateral medial facet, which articulates with the lunate (56).
The medial surface of the distal radius forms a semicircular notch
covered with hyaline cartilage, which articulates with the ulna head.
This articulation enables the radius to swing around the ulna. The
lateral surface elongates into a prominent styloid process, which gives
attachment to the brachioradialis muscle (Fig. 44.1).
 |
|
Figure 44.1. Anterior distal end of the radius and ulna. (From Kaplan EB, Taleisnik J. The Wrist. In Spinner M, ed. Kaplan’s Functional and Surgical Anatomy of the Hand, 3rd ed. Philadelphia: JB Lippincott, 1984. Reprinted with permission.)
|
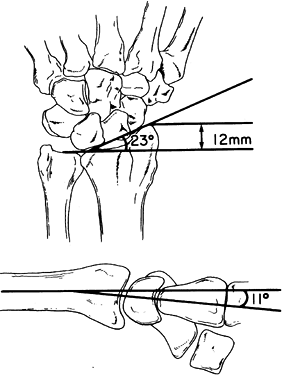
metaphysis is quite thin. There is normally an average of 23° of radial
angulation in the anteroposterior plane (75).
Average radial length from the tip of the radial styloid to the ulna
head is 12 mm, although the variance can be considerable (Fig. 44.2) (31).
 |
|
Figure 44.2.
Measurement of normal average radial angulation, radial length, and palmar angulation. (From Szabo RM, Weber SC. Comminuted Intra-Articular Fractures of the Distal Radius. Clin Orthop1988;230:40. Reprinted with permission.) |
Barton, in his original article, describes a “subluxation of the wrist
consequent to a fracture through the articular surface of the carpal
extremity of the radius” (10). The controversy
in his day was that this injury was frequently not recognized but
instead was diagnosed and treated as a wrist “sprain.” Barton describes
the mechanism of injury as a force met by the palm of the hand that
drives the carpal bones against the dorsal edge of the articulating
surface of the radius, creating a dorsal fracture and subluxation of
the carpus. He said: “Rarely a fracture of similar character occurs on
the palmar side of the radius from the application of force on the back of the hand” (10).
It is therefore better to describe a dorsal Barton’s fracture or a
palmar Barton’s fracture than to inaccurately use the term a “reverse” Barton’s fracture. Until we drop eponyms from the scientific language, we need at least to agree on what we are describing with these terms.
wrist, the magnitude and direction of force, and the physical
properties of the bone. A fall on the outstretched hand with the wrist
in 40° to 90° of dorsiflexion produces a distal radius fracture with
dorsal displacement (37). The radius probably
first fractures in tension on its palmar surface, followed by
compression on the dorsal surface, resulting in dorsal comminution. The
lunate in particular can exert a compressive force on the distal
radius, producing a so-called die-punch fracture (88).
The ulnar styloid fracture component of the Colles’ fracture results
from a force transmitted through an intact triangular fibrocartilage
complex.
are attributed to more than one mechanism of injury. Smith claimed that
this injury results from a fall on the back of the flexed hand (92).
This mechanism of injury is not always implicated, and many of these
fractures result from a fall on the outstretched extended hand. A fall
with the forearm in supination followed by pronation around a fixed
extended wrist may be the more common mechanism of injury (29,100).
(tensile) force generated through the palmar radiocarpal ligaments.
Careful evaluation of other ligamentous injuries (e.g., perilunate
dislocations with or without spontaneous reduction) should be given to
the patient with a radial styloid fracture.
Because there is such a great variation in the fracture types, however,
no simple classification can be relied on to guide optimal treatment or
be of prognostic value. Andersen et al. reported a low degree of
interobserver and intraobserver agreement for the Frykman, Melone,
Mayo, and AO classification systems for distal radius in a clinical
setting using initial plain radiographs (5).
Given the limitations of fracture classifications based solely on plain
radiographs, their use as the sole means for determining the direction
of treatment or for the direct comparison of results among different
studies is not warranted (5).
classification of Colles’ fractures based on the extent of involvement
of the articular surface of the radiocarpal and distal radioulnar
joints (37).
|
treatment-related “Universal Classification” based on the concept and
principle of extraarticular versus intraarticular fractures and stable
versus unstable fractures. This scheme is modeled after the
classifications of Gartland and Werley and of Sarmiento (Table 44.1) (26,39,86).
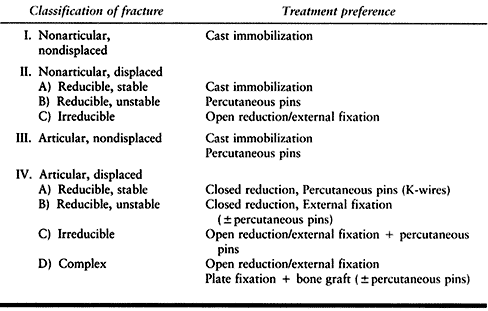 |
|
Table
44.1. Universal Classification of Distal Radius Fractures (From Cooney, WP: Fractures of the Distal Radius. A Modern Treatment-Based Classification. Hand Clinics 24:213, 1993.) |
to identify stable versus unstable patterns, to identify children’s
equivalent injuries, to include associated lesions, and to provide
general recommendations for treatment (Table 44.2) (34,51).
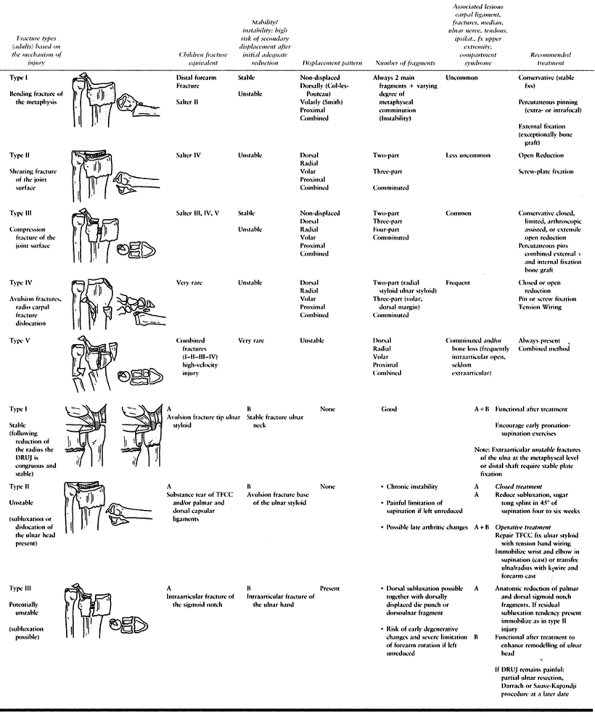 |
|
Table
44.2. A Practical, Treatment Oriented Classification of Fracrures of the Distal Radius and Associated Distal Radioulnar Joint Lessons. By Diego L. Fernandez, M.D. PD |
classifications draw attention to the intraarticular fracture
components and fit into subdivisions of the Universal Classification
type IV. The Comprehensive Classification of Fractures (AO/ASIF) (76)
divides fractures into three types based on the presence or absence of
articular involvement, with subdivisions into three groups that are
further subdivided into three more groups, creating 27 categories.
|
it is important to analyze which types of fractures are being discussed
in any given series.
attention given to the status of the median nerve. If decreased median
nerve function is found in a patient with a swollen wrist, carpal canal
pressures are measured and used to differentiate median nerve contusion
from an acute compressive neuropathy. The patient with a median nerve
contusion may be observed, but immediate operative decompression is
recommended for acute carpal tunnel syndrome (42,95).
The radiographs are analyzed, and the direction of displacement, degree
of shortening and comminution, articular involvement, and ipsilateral
carpal injuries are determined.
restoration and healing of the fracture, the goal of treatment is to
obtain and maintain anatomic position. This goal must be met without
compromising nerve function or digital motion.
What constitutes stability? Many distal radius fractures redislocate in
a plaster cast. Despite early radiographic assessment followed by
remanipulation within the first 2 weeks of treatment, malunion remains
a common problem. Early redisplacement accounts for a small proportion
of final displacements (about 5%) and is caused by movement at the
fracture as a consequence of acute instability (50). The remaining displacements represent late deterioration in the fractures’s position as a result of chronic instability (50). Intraarticular involvement and comminution are cited as the most sensitive indicators of stability (25,44,57). Both Jenkins (50) and Abbaszadegan (1)
have found that malunion may be predicted by radial shortening and loss
of radial angle on initial presentation independent of articular
involvement. Shortening indicates initial metaphyseal comminution.
Based on a study of 267 consecutively treated Colles’ fractures,
Abbaszadegan et al. (2) demonstrated that the
probability of an acceptable anatomic result by closed treatment, if
initial radial axial shortening is 5 mm or greater, was 20%.
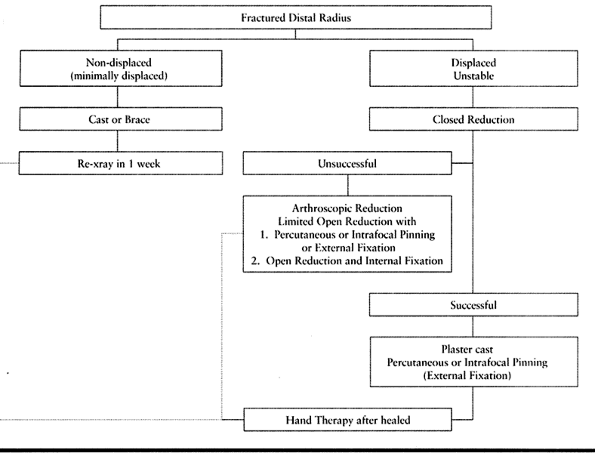 |
|
Table 44.3. Treatment of Distal Radius Fractures
|
fractures are correctly managed with closed reduction and
immobilization in mild flexion (10° to 20°) and ulnar deviation (15°),
followed by early mobilization. This group includes Frykman type I and
II and Smith’s type I and III fractures. Immobilization in pronation
and supination for Colles-type fractures has been advocated
empirically, but no significance in results has been demonstrated in
prospective trials comparing the two (18,31,69,86,87,102,104).
Because the hand is more functional in a neutral or slightly pronated
position, this is probably the preferred position for immobilization;
however, careful examination of the distal radioulnar joint is
warranted. Its injury should be considered in choosing a position of
forearm immobilization. Smith fractures are more stable in supination.
Reduction
is performed by traction to the hand manually or with Chinese finger
traps and countertraction to the humerus with the elbow flexed. The
displacement is reduced gently after disimpaction of the fracture.
Initial immobilization is maintained with above-elbow dorsal and palmar
plaster slabs in the position previously mentioned.
reported improved early results with cast bracing for Colles’
fractures, but others demonstrated no anatomic or functional advantage
for this form of treatment (94). I have used plaster because it is readily available and easy to work with.
-
Mold the plaster splints so that three-point pressure is applied to maintain reduction.
-
Trim the plaster just proximal to the
proximal palmar wrist crease and around the base of the thumb to allow
full finger flexion and thumb opposition. -
Take radiographs after reduction and at frequent intervals over the next few weeks.
-
After swelling decreases, the splints may become loose and need to be replaced.
-
After 3 to 4 weeks, set the elbow free, and continue immobilization of the wrist for a total of 6 weeks.
-
Begin gentle wrist exercises and have the patient wear a removable palmar splint for an additional few weeks.
greater treatment challenge. Most orthopaedic surgeons agree that the
results of treatment correlate directly with restoration of normal
anatomy (4,6,8,9,22,25,32,37,39,43,44,45 and 46,48,77,88,97,98).
Three techniques have been advocated to manage these injuries:
percutaneous pinning, traction maintained by transfixing pins
incorporated in
plaster
or with an external fixation device, and open reduction with internal
fixation. For elderly patients (>75 years old) with an unstable
extraarticular distal radius fracture, Kiyoshige has advocated open
reduction and the use of bone cement to fill the void caused by
osteoporotic bone loss (59).
This technique has been used more often in Europe than in the United
States but may be replaced by the introduction of newer materials such
as injectable calcium phosphate.
This technique is limited to the fractures in which anatomic reduction
can be obtained by traction and in which there are no more than two
intraarticular fragments. I prefer a technique similar to that
described by Clancy (21).
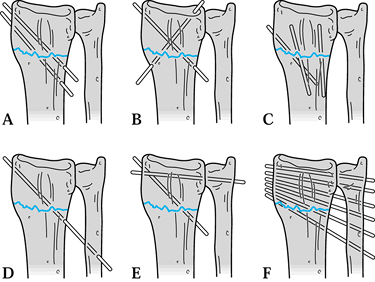 |
|
Figure 44.3. Different techniques of percutaneous pinning. A: Pins placed through the radial styloid. B: Crossed pins. C: Kapandji intrafocal technique. D: Ulna-to-radius pinning without transfixation of the distal radioulnar joint. E: A radial styloid pin and transfixation of the distal radioulnar joint. F:
Multiple pins from the ulna to the radius including transfixation of the distal radioulnar joint (Rahyack technique). (From Fernandez D, Jupiter J. Fractures of the Distal Radius. A Practical Approach to Manangement. New York: Springer-Verlag, 1995:129.) |
-
Obtain fracture reduction and check with a C-arm recorder
-
Insert two crossed 0.062-in. smooth
Kirschner wires percutaneously with a wire driver. Introduce the first
wire at the radial styloid between the first and second dorsal wrist
extensor compartments at a 45° angle with the long axis of the radius
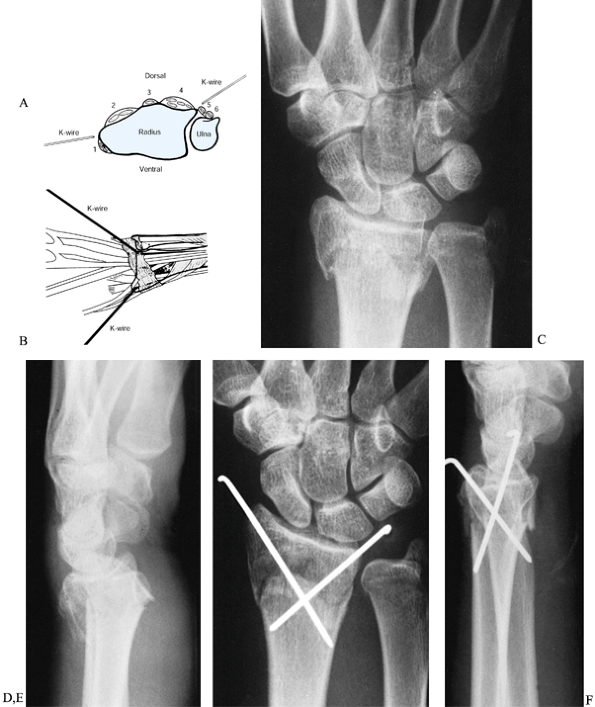
and 10° dorsally (Fig. 44.4).![]() Figure 44.4. Technique for percutaneous Kirschner wire fixation of Colles’ fractures. A:
Figure 44.4. Technique for percutaneous Kirschner wire fixation of Colles’ fractures. A:
Schematic cross section of the distal parts of the radius and ulna,
demonstrating the extensor canals (numbered) and the starting points
for both Kirschner wires. B: Dorsal view
of the wrist, showing correct placement and orientation of both
Kirschner wires for insertion into the distal part of the radius while
avoiding the extensor tendons. C,D: Anteroposterior and lateral radiographs of distal radius fracture suitable for percutaneous pinning. E,F: Postoperative radiographs demonstrating anatomic reduction and proper fixation. (A,B from Clancy GJ. Percutaneous Kirschner Wire Fixation of Colles’ Fractures. J Bone Joint Surg1984;66-A:1008. Reprinted with permission.) -
Engage the Kirschner wire into the ulnar
cortex of the proximal radius and go no farther. Palpate the radial
artery in the anatomic snuff box and avoid it. -
Introduce the second Kirschner wire
between the fourth and fifth dorsal wrist extensor compartments,
starting at the ulnar corner of the distal radius, avoiding the
semicircular notch. Direct this wire 45° to the long axis of the radius
and 30° palmarly and insert it into the radial cortex of the proximal
radius, but go no farther. -
Under fluoroscopy, check the stability of the fracture, quality of reduction, and position of the Kirschner wires.
-
Cut both Kirschner wires below the skin or bend the wires and leave them superficial to the skin.
-
Place the extremity in well-padded, long-arm dorsal and palmar plaster splints with the forearm in slight supination.
-
Four weeks after surgery, convert this
form of immobilization into a below-elbow cast, maintaining the wrist
in neutral position. -
Remove the pins at 6 to 8 weeks, and continue immobilization with a below-elbow cast for an additional 2 weeks.
fracture fragments, and union is delayed. Late recurrence of deformity
may be produced by early mobilization. Therefore, continue protection
of the wrist until the fracture is clinically and radiographically
healed.
the Kirschner wires are used to buttress the fracture fragments by
being inserted into the fracture site dorsally, parallel to the
fracture line. The indications for this technique are unstable
extraarticular distal radius fractures in young patients (54,55).
-
Insert a 0.062-in. smooth Kirschner wire
percutaneously between the first and second extensor compartments
parallel to the fracture line (use a small incision and blunt spreading
to avoid placing any wires in tendons). -
Insert a second wire between the third and fourth dorsal extensor compartments, also parallel to the fracture line.
-
Next, advance both wires with a power
wire driver obliquely at a 45° angle to the long axis of the radius to
engage the intact proximal cortex. -
Apply a plaster cast (my preference is to go above the elbow). Split the cast when dry.
-
Remove pins and cast at 6 weeks.
-
Start mobilization of the wrist when clinically and radiographically healed.
Although pins and plaster have been used successfully in the treatment
of fractures that cannot be held reduced by plaster alone, external
fixation has the advantage of being adjustable if fracture displacement
occurs and avoids the complications of circumferential plaster (18,22,46,47,52,88).
External fixation relies on the principle of “ligamentotaxis,” in which
a distraction force applied to the carpus aligns the fracture fragments
by means of intact ligaments. DePalma has shown in a Colles’ fracture
created in the laboratory that disruption to the carpal ligaments is
rare. As investigators have gained experience with arthroscopy and open
reduction of distal radius fractures, however, injury to these soft
tissues has been reported (14,80,99).
Distraction with external fixation frequently improves length and
alignment, but intraarticular displacement may be increased and palmar
tilt is often not restored (11). In selected
cases in which traction restores length and intraarticular alignment, I
use external fixation as the definitive treatment (Fig. 44.5).
 |
|
Figure 44.5.
A 37-year-old, right-hand-dominant woman sustained Frykman VII right distal radius fracture (anteroposterior and lateral views). A: Injury radiographs. B: Radiographs after application of an external fixation device. Notice anatomic restoration of an articular surface. C: Radiographs 5 months after original injury show preservation of the articular surface. (From Szabo RM, Weber SC. Comminuted Intraarticular Fractures of the Distal Radius. Clin Orthop1988;230:44. Reprinted with permission.) |
alone, I prefer to perform open reduction and internal fixation of the
main fragments, most commonly through a dorsal approach to obtain
restoration of the articular surface. The previously applied external
fixator then functions as a neutralization device (Fig. 44.6).
If a fracture requires open reduction, it usually requires supplemental
iliac crest bone grafting. Autogenous cancellous bone can fill the gaps
created by reducing the articular fragments. Leung demonstrated that
bone grafting hastens healing of comminuted fractures of the distal
radius and allows early removal of the external fixator without
subsequent collapse (65). Many commercially
available bone substitutes are being promoted that are made from
allograft or synthetic materials. They have the advantage of avoiding
donor site morbidity, but they are expensive. One product that stands
out from the rest is injectable calcium phosphate; it is being
evaluated in clinical trials (61). Calcium
phophate is attractive because it is osteoconductive, has high
compressive strength, and is gradually replaced by bone (36).
 |
|
Figure 44.6. Comminuted distal radius fracture sustained in car accident with metal particles imbedded in the skin. A,B: Preoperative radiographs, anteroposterior and lateral views. C,D:
Postoperative radiographs, anteroposterior and lateral views, demonstrating application of external fixation with supplemental percutaneous pin fixation. The external fixation device used in this case was a WristJack. |
fixation, avoiding the extensive dissection and periosteal stripping
required to fix the fracture with a plate. External fixation is
maintained for 8 to 10 weeks, after which protected range-of-motion
exercises are started. If additional internal fixation has been used, I
usually remove the pins a few weeks before removing the external
fixation device. Axelrod and McMurty (8)
reported 20 patients with comminuted distal radius fractures treated by
open reduction and internal fixation without the addition of external
fixation. Although articular congruency was restored in 88%, the
overall complication rate was 50%. Half of all complications were
directly related to the use of a plate and screws (8).
are available, each with small advantages over the others. In general,
two threaded 3-mm half-pins are inserted distally and proximally.
-
Make a longitudinal skin incision over
the proximal half of the index metacarpal along its radial aspect.
Dissect the subcutaneous tissues bluntly, and retract to avoid the
small branches of the radial nerve. -
Elevate the portion of the first dorsal interosseous muscle over the metacarpal flare.
-
Use a 2-mm drill to penetrate the proximal cortex of the index metacarpal at its metaphyseal flare.
-
Insert the first pin with a power driver
through this hole in the index metacarpal, and go into the base of the
long finger metacarpal but not beyond this point. -
Insert a second pin parallel to the first
in a similar fashion with the aid of a guide or the distal portion of
the external fixation frame (the technique varies, depending on which
external fixation frame is chosen). The depth of penetration of the
second pin should be no farther than the ulnar cortex of the index
metacarpal. -
Make a 3-cm longitudinal skin incision
along the midradial aspect of the radius, beginning about 10 cm from
the distal wrist crease. Dissect the subcutaneous tissues bluntly, and
protect the sensory branch of the radial nerve. Retract the wrist
extensors dorsally and the brachioradialis and sensory radial nerve
palmarly. -
Use a 2-mm drill to penetrate the radial
cortex of the radius at the level of the insertion of the pronator
teres. Drill a 3-mm threaded half-pin into this hole while aiming at
the ulnar shaft until it penetrates the ulna cortex of the radius. -
Insert a second pin distal and parallel
to the first with the aid of a guide or the proximal portion of the
external fixation frame. -
Close skin incisions loosely and apply sterile dressings to the wounds. Apply the external fixation frame.
-
Perform fracture reduction with usual techniques or with the assistance of the fixator.
-
Obtain anteroposterior and lateral radiographs to confirm proper positioning of the fixation pins and alignment of the fracture.
alignment cannot be obtained, however, open reduction and additional
internal fixation should be considered. Additional incisions and pin
placement are dictated by the fracture fragments that do not align with
distraction alone.
radioulnar joint is severely comminuted, or the distal ulna is dorsally
subluxed, a long-arm plaster splint maintaining the wrist in supination
may be needed for additional immobilization.
I routinely use this long-arm plaster immobilization postoperatively for the initial 4 weeks.
the WristJack (developed by Dr. John M. Agee, Sacramento, CA). Its
mechanics permit independent adjustment of length, fracture alignment
in the lateral and anteroposterior planes, and the position of the
wrist in the flexion-extension plane. Distraction and flexion have a
detrimental effect on the functional position of the hand, creating
excess tension forces on the extensor tendons and resulting in a
“clawing” of the hand (extrinsic extensor plus position). Clawing of
the fingers is associated with hand stiffness. This observation and the
difficulty in rehabilitating the hand when the wrist is in the flexed
position led to the development of the WristJack, which allows for
Colles’ fracture fixation with the wrist in the extended position.
comminuted distal radius fractures, my colleagues and I demonstrated
that anatomic reduction could be maintained despite a wrist neutral or
extended position during external fixation. Most patients were
performing active digital motion on the day of surgery, and 95%
maintained functional finger motion during treatment (4).
Dynamic external fixators have been used to allow for early motion of
the wrist joint, but one study demonstrated a statistically significant
loss of radial length compared with that in the static-fixator group (4
mm compared with 1 mm), with more frequent complications in the
dynamic-fixator group (93). Another study showed increasing recurrent dorsal angulation with dynamic external fixation (58).
necessary for managing the displaced intraarticular distal radius
fracture with palmar dislocation of the carpus (Smith’s fracture, type
II) (Fig. 44.7). Experience has shown that this
fracture seldom is stable. Although acceptable reduction can often be
obtained by closed means, redisplacement of the fracture is common. Two
surgical approaches to the distal radius are useful to apply a plate
palmarly. They are described here as techniques A and B.
 |
|
Figure 44.7. A,B: Comminuted Smith type II distal radius fracture, anteroposterior and lateral preoperative radiographs. C,D: Anteroposterior and lateral radiographs demonstrate postoperative reduction and fixation with a palmar T -plate.
|
-
Make an anterior incision, starting at
the distal wrist crease along the radial border of the flexor carpi
radialis tendon and extend it 6 to 8 cm proximally. -
Identify the flexor carpi radialis tendon
and the radial artery. Incise the deep fascia between the flexor carpi
radialis and radial artery. Divide the pronator quadratus at its radial
insertion. -
Insert retractors on the ulnar and radial aspects of the radius and analyze the fracture pattern.
-
Select a small fragment T-plate
that will fit the width of the distal radius. Determine the length of
the plate with respect to the proximal extension of the fracture so
that the final result will provide stable internal fixation. -
Fix the plate first to the proximal
fragment. The fracture is reduced by the buttress effect of the plate.
If the distal fragments are large, obtain additional fixation with
cancellous screws through the horizontal holes in the plate. -
Obtain radiographs to confirm the fracture reduction and the position of the internal fixation device.
-
Reattach the pronator quadratus and close the tissues in layers.
-
Technique B uses a modified carpal tunnel
incision. This incision allows extension into the carpal tunnel if
release is necessary and avoids the palmar cutaneous branch of the
median nerve and radial artery, which are vulnerable in technique A. -
Make an incision paralleling the ulnar
crease, cross the distal wrist crease in an ulnar direction, and then
curve back to the midline. Extend the incision 6 to 8 cm proximally
from the distal wrist crease. -
Split the fascia proximal to the flexor retinaculum medial to the tendon of the palmaris longus.
-
Identify and tag the median nerve. Incise
the fascia and, if necessary, the flexor retinaculum (transverse carpal
ligament) along the ulnar border of the median nerve. -
Retract the median nerve, palmaris
longus, flexor pollicis longus, and flexor carpi radialis radially, and
retract the flexor digitorum superficialis and flexor digitorum
profundus ulnarly. -
Insert the T-plate and complete the procedure as described in technique A.
-
After surgery, place the extremity in a
bulky plaster-reinforced compression dressing until suture removal.
Continue immobilization for a total of 5 to 6 weeks in a short-arm
cast. Place the wrist in neutral to 15° of dorsiflexion, not in palmar
flexion, particularly if the carpal tunnel is opened.
internal fixation of distal radius fractures when articular
incongruities exceed 1 mm (33,101) to 2 mm (15,60).
One of the problems in evaluating this approach is the unreliability of
measuring displacement accurately. Cole et al. found a poor correlation
between measurements made on images and plain radiographs with a gap or
step displacement over 2 mm (23). Thirty
percent of measurements from plain radiographs compared to computed
tomography significantly underestimated or overestimated displacement.
The authors concluded that computed tomography using an arc method of
measurement that they describe, is more reliable for quantifying
articular surface incongruities of the distal radius (23). They followed this study with an outcome study (20)
(see below) that raised the question: Despite the well-established
correlation between the development of posttraumatic osteoarthrosis of
the radiocarpal joint and residual displacement of articular fragments,
what amount of displacement of articular fragments is compatible with a
good outcome?
fractures with plates and screws have led to many problems, including
nonrigid fixation, lack or loss of operative reduction, and tendon
irritation or rupture, to mention a few (35). This has led surgeons to develop new implants to try to solve these problems (17,19,81,82). The surgical approach is similar except for the Forte plate, which requires a more elaborate exposure (17,19)]; the choice of implant is the surgeon’s preference.
-
Apply traction longitudinally either with temporary external fixation or finger trap traction. Apply a pneumatic tourniquet.
-
Make a 10-cm dorsoradial incision
parallel to the radius between the second and third dorsal extensor
compartments in line with Lister’s tubercle. Plan the incision so that
the articular surface can be exposed through a dorsal capsulotomy and
there is enough proximal exposure for the plate. Open the extensor
retinaculum between the second and third dorsal extensor compartments
and mobilize the extensor pollicis longus tendon after tagging it with
an umbilical tape. -
Expose the radius subperiosteally between
the extensor carpi radialis brevis and extensor digitorum communis
tendons by elevating the fourth compartment. Do not enter the fourth
dorsal compartment. -
Insert small Hohman retractors along the radial and ulnar cortices of the radius for retraction of the extensor tendons.
-
Incise the dorsal wrist capsule and visualize the joint surface.
-
Disimpact and manipulate the articular
fragments into anatomic position. Accomplish this by inserting small
elevators or curets into the metaphyseal fracture and pushing the
fragments into place. -
Fill residual defects with autogenous cancellous bone graft from the iliac crest.
-
Check the reduction with fluoroscopy.
-
Contour the plate and apply it to the distal radius. Lister’s tubercle can be removed to accommodate the plate.
-
Drill, tap, and insert the screws according to the implant chosen.
-
Confirm reduction and fixation device placement with radiographs in two planes.
-
Close the extensor retinaculum and obtain
complete coverage of the implant. Leave the extensor pollicis longus
above the retinaculum. -
Close the skin and use a drain if deemed necessary.
-
Immobilize the wrist in a long-arm bulky
plaster-reinforced dressing for 2 weeks. At 2 weeks, remove the sutures
and apply a cast (consider above-elbow immobilization) for an
additional 4 weeks or until the fracture is clinically and
radiographically healed (Fig. 44.8).![]() Figure 44.8.
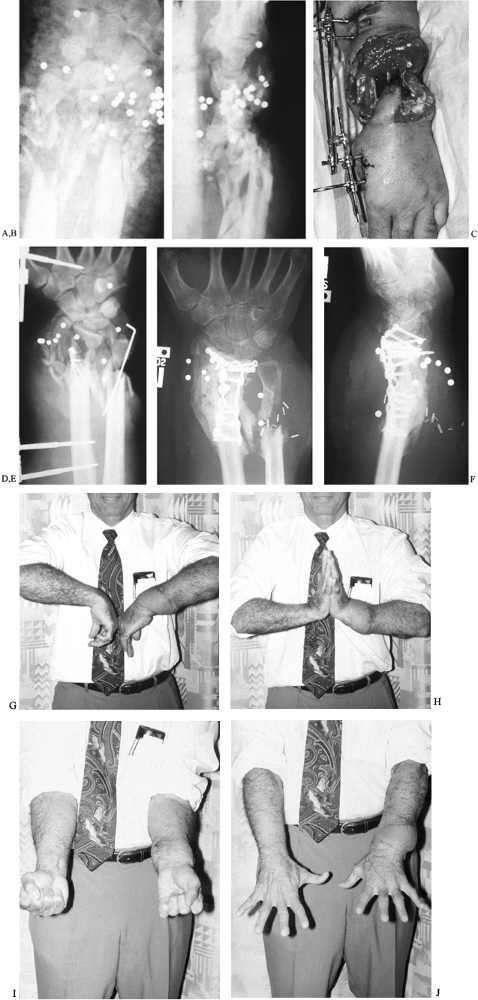
Figure 44.8.
Treatment of a severe comminuted distal radius fracture with massive
soft tissue loss from a close-range shotgun injury. Initial management
was irrigation and debridement followed by external fixation with
limited Kirshner wire fixation. Definitive treatment consisted of
obtaining soft tissue coverage with a microvascular free tissue
transfer using a scapular flap. The articular surface was reconstructed
with a π-plate and iliac crest bone graft at the same time as soft
tissue coverage. The distal ulna was allowed to form a pseudarthrosis.
Preoperative (A) anteroposterior and (B) lateral radiograph. C: After initial incision and debridement and external fixation. D: Anteroposterior radiograph after external fixation. E: Anteroposterior radiograph after internal fixation. F: Lateral radiograph after internal fixation. G: Seven months postoperative wrist flexion. H: Seven months postoperative wrist extension. I: Seven months postoperative pronation with finger extension. J: Seven months postoperative supination with finger flexion.
fixation that allows for visualization of the articular surface is
arthroscopically assisted reduction combined with either external or
internal fixation (3,27,40,41,66,67,80,106). In one study, 49 of 50 patients had concomitant ligament injuries, and one third had chondral injuries (67).
These additional injuries may explain different outcomes unrelated to
radiographic findings, as no correlation could be established between
x-ray findings and ligamentous injuries (80).
-
Wait 2 to 4 days after the acute injury to avoid extravasation of fluid into the soft tissues.
-
Wrap the forearm with an elastic bandage
or Coban (3M, Minneapolis, MN) to prevent further extravasation. Apply
4 to 7 kg of traction to the index and long fingers and attempt a
closed manipulative reduction. -
Use a traction tower, 2.7 mm 30° angle arthroscope, and standard arthroscopic techniques as described in Chapter 75.
-
Place the arthroscope in the 3-4 portal and an outflow cannula in the 6-R portal.
-
Lavage the joint thoroughly. Use a
small-radius shaver to remove synovium and cartilage debris until the
fracture is well visualized. -
Disimpact the fragments by prying between fracture lines with a hook or small osteotome inserted through the 4-5 portal.
-
Insert 0.045-in. Kirschner wires percutaneously into the fracture fragments or into the fracture line (as described in the Kapandji technique above) and use these wires as joysticks to manipulate the fragments into anatomic positions.
-
Advance the wires across the fracture into intact cortex to maintain reduction.
-
Check reduction and position of pins under fluoroscopy.
-
Apply a plaster cast (my preference is to
go above the elbow). Split the cast when dry. Alternatively, use an
external fixator as a neurtalization device. -
Remove pins and cast at 6 weeks.
-
Start mobilization of the wrist when clinically and radiographically healed.
-
Combined internal and external fixation is often needed for the treatment of severe distal radius fractures (12). With open fractures, this approach may be staged as illustrated.
encouraged to move their fingers immediately. Patients are instructed
to elevate the hand for the first week after treatment. Fractures are
immobilized until clinically and radiographically healed. A recent
study suggests that ultrasound signal may accelerate the healing of
fractures of the distal radial metaphysis and decrease the loss of
reduction during fracture healing (62). Further
study of this technique is warranted before its value is assessed. When
healed, patients are referred for supervised hand therapy to regain
wrist motion and strength. Therapy is individually tailored for each
patient, depending on severity of the fracture, age of the patient,
functional demands, and postfracture problems.
functional result? Aro studied 146 patients with distal radius
fractures (7). Ninety-six percent of the
patients with radial shortening of less than 3 mm had a good functional
result. Twenty-five percent of patients with radial shortening of 3 to
5 mm and 31% of patients with greater than 5 mm radial shortening had
an unsatisfactory result, regardless of displacement or angular
malalignment of the radial fragment. Even minor shortening of the
radius significantly alters the load pattern across the wrist joint,
causing functional limitation.
mechanics, creating an alignment that permits the carpus to collapse
dorsally, leading to dorsal midcarpal instability (98).
Malreduction with loss of angulation toward the ulna leads to radial
deviation of the hand and tends to palmar flex the scaphoid, which
leads to increases in the scapholunate angle. Shortening, alone or in
combination with angulation, disrupts the congruence of the distal
radioulnar joint (DRUJ). This may cause pain in the distal radioulnar
joint, interference with pronation/supination, and, because it results
in an ulnar plus hand, may interfere
with radial and ulnar deviation of the carpus from ulnar impingement and/or impaction.
plaster immobilization, Roth found that 27 remained symptomatic, and 16
had marked functional limitations at the end of treatment (84). Poor end results were associated with loss of radial angle, palmar tilt, and radial length.
radiographic outcomes in a series of young adults in whom an acute
displaced intraarticular fracture of the distal aspect of the radius
had been treated with operative reduction and stabilization (20).
They found that at an average of 7.1 years, osteoarthrosis of the
radiocarpal joint was evident on the plain radiographs and computerized
tomography scans of 16 of 21 wrists (76%), and there was a strong
association between the development of osteoarthrosis of the
radiocarpal joint and residual displacement of articular fragments at
the time of osseous union. The functional results, however, as
determined by physical examinations and responses to questionnaires,
did not correlate with the extent of the residual displacement at the
time of fracture healing. Furthermore, all patients had a good or
excellent functional outcome irrespective of radiographic evidence of
osteoarthrosis of the radiocarpal or the distal radioulnar joint or
nonunion of the ulnar styloid process (20).
secondary deformity of the distal radius, midcarpal instability, and
arthritis (60,98).
Median nerve damage may occur in the form of acute and late carpal
tunnel syndrome, contusion, or stretch. Ulnar nerve damage has also
been reported. Radial nerve damage occurs with the placement of
external fixation pins percutaneously and can be avoided by a skin
incision and proper identification of the sensory branch. A painful,
stiff hand and reflex sympathetic dystrophy (49)
are best prevented by minimizing swelling, starting digital motion
immediately, not immobilizing in extreme positions, and avoiding
constrictive dressings. The rate of complications related to fixation
pins is as high as 60% in some series (105).
Pin loosening is the most common problem, but metacarpal fractures, pin
track infections, and intrinsic muscle tie-down have all been
experienced.
contractures, TFC tears, and arthritis may require further
reconstructive surgery to restore wrist motion (pronation–supination)
and eliminate pain. Flexor tendon adhesions and tendon ruptures
(particularly extensor pollicis longus ruptures) are known
complications (13,30,107).
The use of titanium distal radius plates has raised concern over
increased tendon ruptures, with the use of internal fixation becoming
more popular (53). Nonunion of the distal
radius is extremely rare. Segalman and Clark recommend that if 12 mm of
subchondral bone remains, union should be attempted with bone grafting
and internal or external fixation (89).
radius, including operations directed at correcting the distal
radioulnar joint problem (Chapter 43), carpal tunnel release (Chapter 56), radiocarpal or limited intercarpal arthrodesis (Chapter 72), and tendon transfers or reconstructions (Chapter 48, Chapter 49 and Chapter 50), are described elsewhere in this book. Corrective osteotomy of the distal radius is the subject of this discussion.
of the distal radius is 25° greater than that in the normal wrist and
if there is significant shortening (6 mm) of the radius. This amount of
deformity usually results in a symptomatic patient. Besides restoring
normal anatomy, a dorsal opening wedge reduces the traction and
decompresses the median nerve, often making carpal tunnel release
unnecessary in symptomatic patients with a distal radius malunion (63).
Contraindications to osteotomy include advanced degenerative changes in
the wrist, significant intraarticular incongruency, fixed carpal
malalignment, or a stiff hand. The surgical technique used is that
described by D. L. Fernandez (Fig. 44.9) (32). Viegas has described this procedure with minimal internal fixation combined with external fixation across the carpus (103)
and Meléndez uses direct rigid external fixation to the osteotomy thus
maintaining correction while allowing early wrist exercises (71).
 |
|
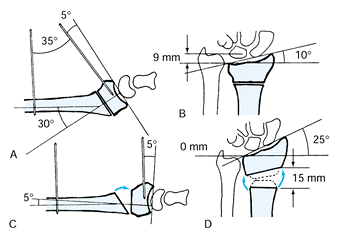
Figure 44.9. Preoperative planning of the osteotomy. A:
For correction in the sagittal plane, the dorsal tilt (30° in this patient) is measured between the perpendicular joint surface and the long axis of the radius on the lateral radiograph. The Kirschner wires are introduced so that they subtend the angle that corresponds to the dorsal tilt plus 5° of palmar tilt (30° + 5° = 35° in this patient). B: After opening the osteotomy by the correct amount, the Kirschner wires lie parallel to each other. C: For correction in the frontal plane, shortening (9 mm in this patient) is measured between the head of the ulna and the ulnar corner of the radius on the anteroposterior radiograph. The lines for the measurement are perpendicular to the long axis of the radius. The ulnar tilt is reduced to 10° in this patient. D: To restore the ulnar tilt to normal (average 25°), the osteotomy is opened more on the dorsoradial than on the dorsoulnar side. (From Fernandez DL. Correction of Post-Traumatic Wrist Deformity in Adults by Osteotomy, Bone Grafting, and Internal Fixation. J Bone Joint Surg64-1982;A:1169. Reprinted with permission.) |
the radiographs of the affected and the normal wrist. Particular
attention is directed at the ulnar variance to restore the normal
anatomic relationship with the distal radioulnar joint. The osteotomy
must correct the palmar tilt in the sagittal plane, the ulnar tilt in
the frontal plane, and rotational deformities in the horizontal plane.
-
Make a 10-cm dorsoradial incision parallel to the radius beginning 2 cm distal to Lister’s tubercle.
-
Expose the radius subperiosteally between
the extensor carpi radialis brevis and extensor digitorum communis
tendons. Do not enter the fourth dorsal compartment. -
Mark the osteotomy site with an osteotome (about 2.5 cm proximal to the wrist joint).
-
Insert a 0.045-in. Kirschner wire
perpendicular to the radius 4 cm proximal to the osteotomy site. Insert
a second 0.045-in. Kirschner wire into the distal radius so that it
subtends an angle with the first Kirschner wire that is 5° more than
the amount of deformity (Fig. 44.8). -
Make the osteotomy parallel to the joint
surface while protecting the soft tissues with subperiosteal
retractors. This is facilitated by placing a fine Kirschner wire along
the articular surface of the radius to act as a guide. -
Open the osteotomy dorsally until the two
Kirschner wires are parallel to each other (a small Lamina spreader is
useful for this maneuver). -
Open the osteotomy on the radial side to
correct radial shortening. Rotate the distal fragment to correct any
pronation or supination deformity. -
Shape a corticocancellous iliac crest
graft into a trapezoid to fill the gap created by the osteotomy. Pack
the area with cancellous graft material. -
Maintain the reduction with oblique, crossed Kirschner wires, and obtain anteroposterior and lateral radiographs.
-
Obtain rigid fixation by applying a contoured T-plate
to the dorsum of the radius. (I have preferred the 2.7-mm ASIF blade
plate, which is easiest to cover with soft tissues.) An optional next
step is to remove the Kirschner wires; it is acceptable to use only the
Kirschner wires for fixation, but postoperative immobilization until
union must be maintained. Lister’s tubercle may be removed for better
fit of the plate. -
Examine the distal radioulnar joint
clinically and radiographically. If needed, perform a Sauvé-Kapandji or
Darrach procedure (see Chapter 43). -
Close the tissues in layers, making certain that there is good coverage of the plate.
-
After surgery, immobilize the wrist in a
long-arm bulky plaster-reinforced dressing for 2 weeks. At 2 weeks,
remove the sutures and begin protective active range-of-motion
exercises. -
The osteotomy usually is healed in 8 to 12 weeks, at which time unrestricted activity is allowed.
-
For correction of distal radius fractures
with palmar tilt (Smith’s fractures) a palmar opening wedge osteotomy
is performed by an approach identical to that described for the acute
care of Smith’s type II fractures (technique B) (91).
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
H, Jonsson U. External Fixation or Plaster Cast for Severely Displaced
Colles’ Fractures? Prospective 1-Year Study of 46 Patients. Acta Orthop Scand1990;61:528.
DJ, Blair WF, Steyers CM Jr, et al. Classification of Distal Radius
Fractures: An Analysis of Interobserver Reliability and Intraobserver
Reproducibility. J Hand Surg [Am]1996;21A:574.
R, Saldana M. Intra-articular Fractures of the Distal Radius: A
Cadaveric Study to Determine if Ligamentotaxis Restores Radiopalmar
Tilt. J Hand Surg [Am]1990;15A:18.
RL, Blair WF, Hubbard PP. Results of Combined Internal and External
Fixation for the Treatment of Severe AO-C3 Fractures of the Distal
Radius. J Hand Surg [Am]1995;20A:373.
JS, Wollstein R, Citron ND. Rupture of Flexor Pollicis Longus Tendon: A
Complication of Volar Plating of the Distal Radius. J Bone Joint Surg [Br]1998;80:225.
RA, Amadio PC. Predicting Palmar Radio-Carpal Ligament Disruption in
Fractures of the Distal Articular Surface of the Radius Involving the
Palmar Cortex. J Hand Surgery [Br]1994;19B:108.
J, Amadio P, Cooney W III. Open Reduction and Internal Fixation of
Displaced Comminuted Intra-articular Fractures of the Distal End of the
Radius. J Bone Joint Surg1989;71A:839.
PR, Frederick HA, Laseter GF. Open Reduction and Internal Fixation of
Unstable Distal Radius Fractures with a Low-Profile Plate: A
Multicenter Study of 73 Fractures. J Hand Surg [Am]1998;23A:300.
LW 3rd, Cole RJ, Gelberman RH, et al. Displaced Intra-articular
Fractures of the Distal Aspect of the Radius. Long-Term Results in
Young Adults after Open Reduction and Internal Fixation. J Bone Joint Surg1997;79A:1290.
RJ, Bindra RR, Evanoff BA, et al. Radiographic Evaluation of Osseous
Displacement Following Intra-articular Fractures of the Distal Radius:
Reliability of Plain Radiography Versus Computed Tomography. J Hand Surg [Am]1997;22A:792.
O, Lundborg G. Rupture of the Extensor Pollicis Longus Tendon after
Fracture of the Lower End of the Radius: A Clinical and
Microangiographic Study. Hand1979;2:76.
G. Fractures of the Distal End of the Radius, Including
Sequelae—Shoulder, Hand, Finger Syndrome, Disturbance in the Distal
Radioulnar Joint and Impairment of Nerve Function: A Clinical and
Experimental Study. Acta Orthop Scand [Suppl]1967;108:1.
GK, Axelrod TS. Complications of the AO/ASIF Titanium Distal Radius
Plate System (Pi Plate) in Internal Fixation of the Distal Radius: A
Brief Report. J Hand Surg [Am]1998;23A:737.
A. L’Ostéosythése par Double Embrochage Intrafocal. Traitement
Functionnel des Fractures Non Articulaires de l’Extremité Inférieure du
Radius. Ann Chir1976;30:903.
A. Treatment of Articular Distal Radial Fractures by Intrafocal Pinning
with Arum Pins. In Saffar P, Conney W III, eds. Fractures of the Distal Radius. London: Martin Dunitz, 1995:160.
JP, Karaharju EO, Porras M, et al. Functional Recovery after Fractures
of the Distal Forearm. Analysis of Radiographic and Other Factors
Affecting the Outcome. Ann Chir Gynaecol1988;77:27.
S, Sawada K, Nabeta Y, et al. Recurrent Dorsal Angulation of the Distal
Radius Fracture During Dynamic External Fixation. J Hand Surg [Am]1998;23A:920.
TK, Ryaby JP, McCabe J, et al. Accelerated Healing of Distal Radial
Fractures with the Use of Specific, Low-Intensity Ultrasound. A
Multicenter, Prospective, Randomized, Double-Blind, Placebo-Controlled
Study. J Bone Joint Surg [Am]1997;79A:961.
H. Fractures of the Distal Radius in the Adult: Anatomy, Trauma
Mechanisms, Fracture Types, and Typical Associated Injuries. Unfallheilkunde1979;82:1.
RS, Bennett JD, Roth JH, Milne K Jr. Arthroscopic Diagnosis of
Intra-articular Soft Tissue Injuries Associated with Distal Radial
Fractures. J Hand Surg [Am]1997;22A:772.
D, Jupiter JB, Brennwald J, et al. Prospective Multicenter Trial of a
Plate for Dorsal Fixation of Distal Radius Fractures. J Hand Surg [Am]1997;22A:777.
A, Zagorski J, Sinclair W. Functional Bracing of Colles’ Fractures: A
Prospective Study of Immobilization in Supination versus Pronation. Clin Orthop1980;146:175.
M. Long-term Follow-up of Treatment of Comminuted Fractures of the
Distal End of the Radius by Transfixation with Kirschner Wires and
Cast. J Bone Joint Surg1962;44A:337.
K, Fernandez DL, Jupiter JB, Martin C Jr. Corrective osteotomy for
malunited, volarly displaced fractures of the distal end of the radius.
J Bone Joint Surg [Am]1997;79:1816.
TG, Seeman M, Silliman J, et al. Dynamic external fixation of unstable
fractures of the distal part of the radius. A prospective, randomized
comparison with static external fixation. J Bone Joint Surg [Am]1994:76A:1149.
H, Innes A, Burke F. Functional Cast-Bracing for Colles’ Fractures: A
Comparison between Cast-Bracing and Conventional Plaster Casts. J Bone Joint Surg1984:66B:749.
JB, Shi D, Gu YQ, Zhang QG. Can cast immobilization successfully treat
scapholunate dissociation associated with distal radius fractures? J Hand Surg [Am]1996;21A:583.