Fractures and Traumatic Dislocations of the Hip in Children
Four – Lower Extremity > 21 – Fractures and Traumatic Dislocations
of the Hip in Children
are rare entities in children, comprising less than 1% of all pediatric
fractures.11,84
Pediatric hip fractures typically result from high-energy mechanisms
that can result in other extremity, visceral, or head injuries in 30%
of patients, unlike low-energy adult hip fractures common in elderly
patients (whose fractures are typically associated with osteoporosis).
Occasionally, pediatric hip fractures result from minor trauma
superimposed upon bone that is weakened by tumor or metabolic bone
disease. These fractures can occur through the physis, but more
commonly occur through the femoral neck and the intertrochanteric
region.
presents many important considerations when treating pediatric femoral
neck fractures. Injury to the greater trochanter apophysis following an
intertrochanteric fracture can lead to coxa valga.17
Damage to the epiphyseal plate of the femoral neck from fracture,
necrosis, or from implant use can result in limb length discrepancies
or coxa breva or vara. The surgeon should generally place fixation
across the growth plate in older children with poor bone quality and in
adolescents who have little growth potential remaining. If fixation is
not placed across the physis; it may be less robust and the surgeon has
to be cognizant how to guide weight-bearing status and provide further
immobilization. Most importantly, the physis is a significant barrier
to interosseous blood supply for the femoral head. Because of this, and
the fact that there is little blood supply to the femoral head from the
ligamentum teres, an increased risk of necrosis is present following
fracture and injury to the important retinacular vessels.
high rate of complications and the important lifetime morbidity that
may result from complications. Potential complications from the
fracture and its treatment include chondrolysis, avascular necrosis
(AVN), varus malunion, nonunion, delayed physiolysis, and growth
abnormalities leading to length discrepancy or angular deformities.17
Because the hip is developing in the growing child, deformities can
progress with age. In addition, review of more recent publications is
important because it has been suggested that outcome can be
significantly improved if certain treatment principles are consistently
followed.34,96
loading, torsion, hyperabduction, or a direct blow to the hip. Almost
all hip fractures in children are caused by severe, high-energy trauma.33,90,102
Except for the physis, the proximal femur in children is extremely
strong, and high-energy forces, such as from motor vehicle accidents
and high falls, are necessary to
cause fracture.26
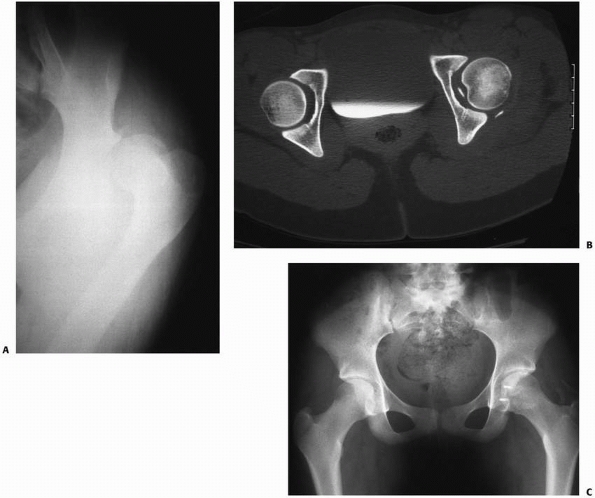
If a child suffers a fracture as a result of insignificant trauma, then
one should suspect an underlying etiology such as prior injury or
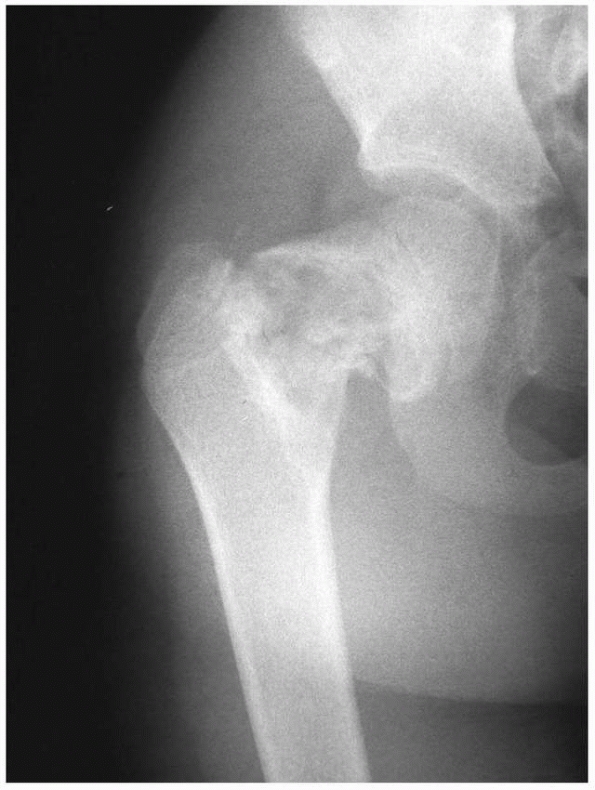
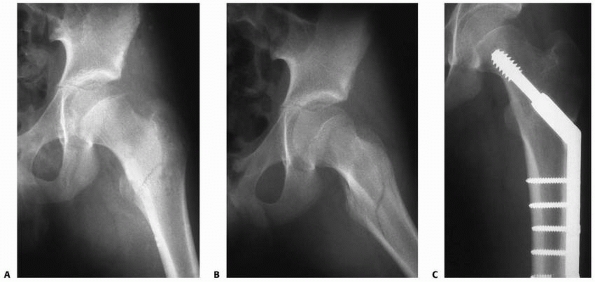
surgery,20 metabolic bone disease, or pathologic processes of the proximal femur (Fig. 21-1).
 |
|
FIGURE 21-1 A 10-year-old boy fractures through a unicameral bone cyst while running for a soccer ball.
|
with a complete fracture is unable to ambulate due to severe pain in
the hip and has a shortened, externally rotated extremity. With an
incomplete or stress fracture of the femoral neck, the patient may be
able to bear weight with a limp and may demonstrate hip or knee pain
only with extremes of range of motion, especially internal rotation. An
infant with a hip fracture holds the extremity flexed, abducted, and
externally rotated. Infants and newborns with limited ossification of
the proximal femur can be challenging patients to diagnose with hip
fractures as the differential diagnosis can include infection and
congenital dislocation of the hip. In the absence of infection
symptoms, pseudoparalysis, shortening, and a strong suspicion are the
keys to a fracture diagnosis in this age group.
trauma, they frequently are accompanied by associated injuries that can
affect the patient’s overall outcome. Pape et al.,78
in a series of 28 patients with a mean follow-up of 11 years, found
favorable outcomes in types II, III, and IV fractures according to
Ratliff’s criteria.84 Poor functional outcomes were attributed to head trauma, amputation, or peripheral neurologic damage.78
In a series of 14 patients with hip fractures, all of which were caused
by vehicular accidents or falls from heights, 12 patients had
associated injuries including head and facial injury, other fractures,
as well as visceral injury.67 In a series of fractures from high-energy trauma, Bagatur and Zorer6
similarly found associated injuries in 4 of their 17 patients. Infants
with hip fractures and without a plausible cause for fracture should be
studied for other signs of nonaccidental trauma by carefully examining
the other extremities, trunk, and head. Careful evaluation by a child
protective team is required to diagnose life-threatening head and
visceral injuries that can be easily missed in this group.
in children documented high rates of coxa vara, delayed union, and
nonunion in patients treated without internal fixation.57,84 Canale and Bourland18
noted that fractures treated by spica casting alone had a greater
incidence of coxa vara. They attributed a lower rate of coxa vara and
nonunion in some of their patients to the use of internal fixation for
all transcervical fractures.18 More
recent literature supports the concept that attempted conservative
treatment can result in unacceptably high rates of coxa vara.102
These high rates of complications may be due to an underappreciation of
the uniqueness of this injury and its requisite necessity for operative
treatment in most patients, which is in contrast to other pediatric
injuries.102 Subsequent authors have
documented lower rates of AVN, coxa vara, and nonunion in patients who
were aggressively treated with anatomic reduction (open or closed) and
internal fixation (with or without supplemental casting) within 24
hours of injury.6,21,33,70,74,90
Therefore, contemporary management is directed at early, anatomic
reduction of these fractures with stable internal fixation and
selective use of supplemental external stabilization (casting), with
the goal of minimizing devastating late complications.21,84,96
history of high-energy trauma and the typical signs and symptoms of the
shortened, externally rotated, and painful lower extremity.
will provide a comparison view of the opposite hip if a displaced
fracture is suspected. For the pelvic radiograph, the leg should be
held in extension and in as much internal rotation as possible without
causing extreme pain to the patient. A cross-table lateral radiograph
should be considered to avoid further displacement and unnecessary
discomfort to the patient from an attempt at a frog-leg lateral view.
Any break or offset of the bony trabeculae near Ward’s triangle is
evidence of a nondisplaced or impacted fracture. Nondisplaced fracture
or stress fractures may be difficult to detect on radiographs. Special
studies may be required to reveal an occult fracture as case examples
of further displacement of nondisplaced fracture have been reported.35
Adjunctive studies for stress fracture diagnosis may include a computed
tomography (CT) scan or a technetium bone scan which can demonstrate
increased uptake at the fracture site. The typical magnetic resonance
imaging (MRI) appearance of a fracture is a linear black line (low
signal) on all sequences surrounded by a high-signal band of bone
marrow edema and hemorrhage. The low signal represents trabeculae
impaction. MRI may detect an occult hip fracture within the first 24
hours after injury.51 In addition,
pathologic fractures may require special imaging to aid diagnosis or to
fully appreciate bone quality which would impact implant placement. MRI
is also a useful test in planning treatment for a pathologic fracture;
this test will delineate soft
tissues in and around the fracture which can provide insight into diagnosis and delineate high-yield areas for biopsy.
epiphyseal separation. Additionally, an ultrasound can determine if the
patient’s epiphysis is located and the presence of an effusion which
may be aspirated to confirm diagnosis of sepsis. A bloody aspirate
establishes the diagnosis of fracture, whereas a serous or purulent
aspirate suggests synovitis or infection, respectively. If performed in
the operating room, an aspiration and confirmatory arthrogram of the
hip can also be useful, especially if closed reductions and cast
immobilization is chosen for the newborn with physiolysis.
evidence of a fracture, other diagnoses must be considered, including
Perthes Disease, synovitis, spontaneous hemarthrosis, and infection. A
complete blood count, erythrocyte sedimentation rate, C-reactive
protein, and temperature are helpful to evaluate for infection. MRI
scan is a useful test to diagnose aseptic AVN as a result of Perthes
Disease or more remote causes of necrosis. In children under 5 years of
age, developmental coxa vara can be confused with an old hip fracture.17
 |
|
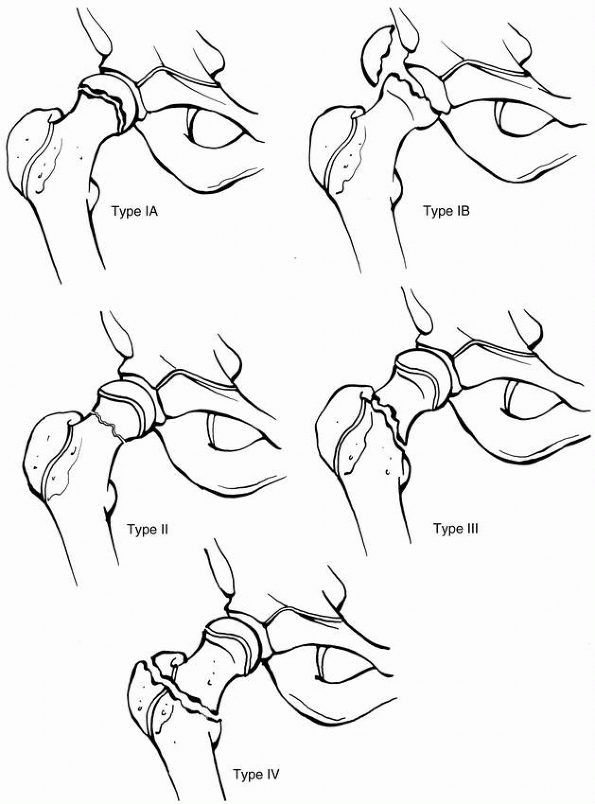
FIGURE 21-2
Delbet classification of hip fractures in children. I, transepiphyseal with (IB) or without (IA) dislocation from the acetabulum; II, transcervical; III, cervicotrochanteric; and IV, intertrochanteric. |
This classification system is one that has stood the test of time
because it is not only descriptive but also has prognostic significance.68
In general, more significant rates of AVN and growth arrest are noted
in Type I and Type II injuries; while lower rates of osteonecrosis are
noted in Type III and Type IV injuries. Conversely, the latter two
groups tend to have higher rates of significant varus malunion if not
treated appropriately. Subtrochanteric fractures have been included by
some in the discussion of proximal femur fractures but they are not
included in the Delbet classification and are discussed elsewhere.
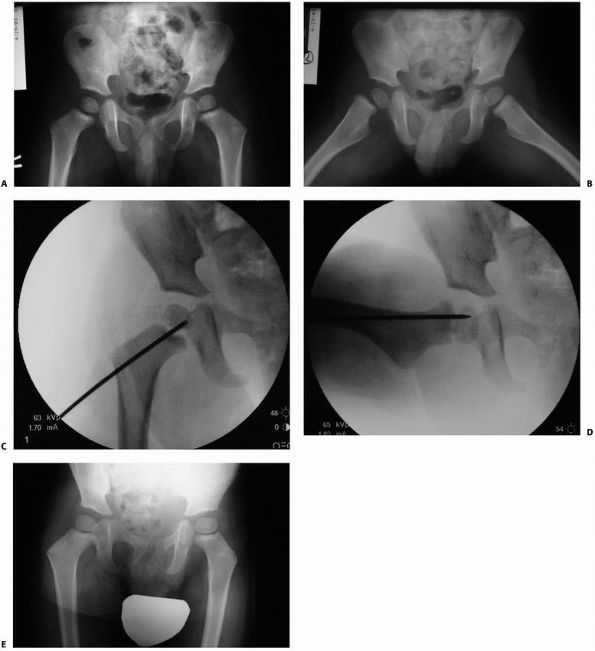
of the femoral head from the acetabulum (Fig. 21-3). Such fractures are rare, constituting 8% of femoral neck fractures in children.50
 |
|
FIGURE 21-3 This 2-year-old boy fell on the trampoline and subsequently complained of right hip pain. A. AP radiographs were not grossly abnormal. B. Frog lateral radiograph revealed a transepiphyseal fracture. C,D. Closed reduction in the operating room was stabilized with a percutaneous pin. E. At 8 months, he was asymptomatic and there was no evidence of AVN. E
|
occur between the physis and are above the intertrochanteric line, and
by definition are consider intracapsular femoral neck fractures.
fractures are, by definition, located at or slightly above the anterior
intertrochanteric line and are the second most common type of hip
fracture in children, representing about 34% of fractures.50
It is conceivable that a certain portion of these fractures may be
intra- and extracapsular as a result of anatomic differences in capsule
insertion.
associated with a dislocation of the capital femoral epiphysis. True
transphyseal
fractures tend to occur in young children after high-energy trauma18,30
and are different from unstable slipped capital femoral epiphysis of
the preadolescent, which usually follows a prodrome of activity-related
hip or knee pain. Unstable slipped capital femoral epiphysis differs
from traumatic separation as it occurs following minor trauma which is
superimposed on a weakened physis from a combination of multiple
factors including obesity and subtle endocrinopathy.
It is possible that these patients had unrecognized physeal injury at
the time of dislocation or, alternatively, the epiphysis may be
displaced with vigorous reduction methods.
have a better prognosis then those with dislocation. Similarly, in
children under 2 or 3 years of age, a better prognosis exists than in
older children. AVN in younger children is unlikely, although coxa
vara, coxa breva, and premature physeal closure can cause subsequent
leg length discrepancy.17,20
In cases of femoral head dislocation, the outcome is dismal because of
AVN and premature physeal closure in virtually 100% of patients.18,30
better prognosis and a lower rate of AVN than displaced fractures,
regardless of treatment.18,68,84
Necrosis can still occur in minimally displaced fractures, and this may
be due to the fact that it is difficult to document how much
displacement occurs at the time of trauma. Moon and Mehlman68
recently performed a meta-analysis of available literature and
documented a 28% incidence of AVN in Type II fractures. The occurrence
of AVN is thought by these and other investigators to be directly
related to fracture displacement, which may lead to disruption or
kinking of the blood supply to the femoral head. In addition, the
meta-analysis study demonstrated higher rates of AVN in children
greater than 10 at the time of their injury.68
Because the pediatric hip capsule is tough and less likely to tear,
some have hypothesized that a possible etiology of vascular impairment
in minimally displaced fractures is a result of intra-articular
hemarthrosis leading to vessel compression from tamponade.18,50
much lower complication rate than displaced fractures. Displaced type
III fractures are similar to type II fractures in regard to the type of
complications that can occur. For instance, the incidence of AVN is 18%
and is slightly less than in type II fractures68; the risk of AVN is directly related to the degree of displacement at the time of injury.14 Premature physeal closure occurs in 25% of patients, and coxa vara in can also occur in approximately 14% of patients.50
has the lowest complication rate of all four types. Nonunion in this
fracture is rare, and Moon and Mehlman68
documented a rate of AVN of only 5%, which is much lower in comparison
to intracapsular fractures. Coxa vara and premature physeal closure
have occasionally been reported.18,50,57,83,84
difficult delivery and can be confused on radiographs with congenital
dislocation of the hip. Type I fracture in a neonate deserves special
attention. This injury is exceedingly rare and, because the femoral
head is not visible on plain radiographs, the index of suspicion must
be high. The differential diagnosis includes septic arthritis and hip
dislocation. Plain radiographs may show a high-riding proximal femoral
metaphysis on the involved side, thus mimicking a congenital hip
dislocation.
physiolysis; with this test, the cartilaginous head remains in the
acetabulum but its dissociation from the femoral shaft can be
appreciated. The diagnosis can be missed if there is no history of
trauma (such as in child abuse) or if there is an ipsilateral fracture
of the femoral shaft.2 In the absence of a history of significant trauma in a young child, battered child syndrome should be suspected.100
result in hip or knee pain and a limp. Pain associated with
long-distance running, marching, or a recent increase in physical
activity is suggestive of stress fracture. Close scrutiny of
high-quality radiographs may identify sclerosis, cortical thickening,
or new bone formation. Undisplaced fractures may appear as faint
radiolucencies. If radiographs are inconclusive, adjunctive tests such
as MRI, CT or bone scintigraphy may be helpful.
femoral epiphysis (SCFE) can be indistinguishable from a traumatic Type
I fracture; however, a SCFE is caused by an underlying abnormality of
the physis and occurs after trivial trauma, usually in preadolescents,
whereas Type I fractures usually occur in young children.
possibly from systemic disease, tumors, cysts, and infections. If the
physical and radiographic evidence of trauma is significant but the
history is not consistent, nonaccidental trauma must always be
considered.4,100
hip fractures that are overshadowed by more dramatic or painful
injuries. Radiographs of the proximal femur should be examined
carefully in patients with femoral shaft fractures because ipsilateral
fracture or dislocation of the hip is not unusual.2
In early childhood, only a single proximal femoral chondroepiphysis
exists. During the first year of life, the medial portion of this
physis grows faster than the lateral, creating an elongated femoral
neck by 1 year of age. The capital femoral epiphysis begins to ossify
at approximately 4 months in girls and 5 to 6 months in boys. The
ossification center of the trochanteric apophysis appears at 4 years in
boys and girls.50 The proximal
femoral physis is responsible for the metaphyseal growth in the femoral
neck, whereas the trochanteric apophysis contributes to the
appositional growth of the greater trochanter and less to the
metaphyseal growth of the femur.58 Fusion of the proximal femoral and trochanteric physes occurs at about the age of 14 in girls and 16 in boys.46
The confluence of the greater trochanteric physis with the capital
femoral physis along the superior femoral neck and the unique vascular
supply to the capital femoral epiphysis make the immature hip
vulnerable to growth derangement and subsequent deformity after a
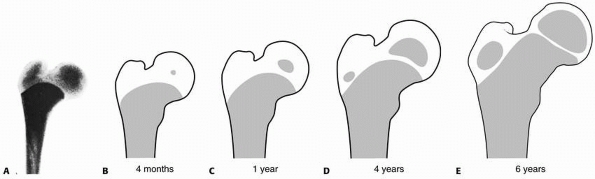
fracture (Fig. 21-4).
 |
|
FIGURE 21-4
The transformation of the preplate to separate growth zones for the femoral head and greater trochanter. The diagram shows development of the epiphyseal nucleus. A. Radiograph of the proximal end of the femur of a stillborn girl, weight 325 g. B-E. Drawings made on the basis of radiographs. (Reprinted from Edgren W. Coxa plana. A clinical and radiological investigation with particular reference to the importance of the metaphyseal changes for the final shape of the proximal part of the femur. Acta Orthop Scand 1965: 84(suppl):24, with permission.) |
Postmortem injection and microangiographic studies have provided clues
to the vascular changes with age. These observations are as follows:
-
At birth, interosseous continuation of
branches of the medial and lateral circumflex arteries (metaphyseal
vessels) traversing the femoral neck predominately supply the femoral
head. These arteries gradually diminish in size as the cartilaginous
physis develops and forms a barrier thus preventing transphyseal
continuity of these vessels into the femoral head. Thus metaphyseal
blood supply to the femoral head is virtually nonexistent by age 4. -
When the metaphyseal vessels diminish,
the intracapsular lateral epiphyseal vessels predominate and the
femoral head is primarily supplied by these vessels, which extend
superiorly on the exterior of the neck, bypassing the physeal barrier
and then continuing into the epiphysis. -
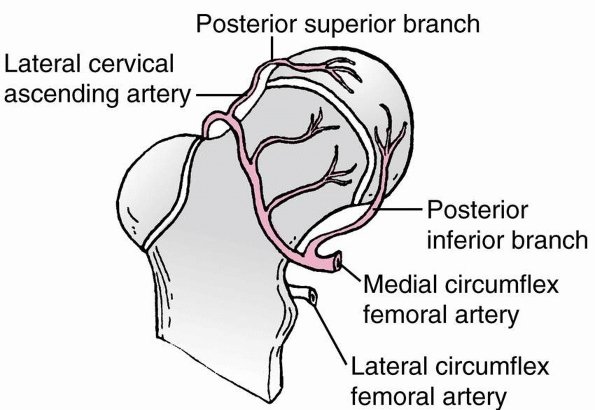
Ogden76
noted that the lateral epiphyseal vessels consist of two branches: the
posterosuperior and posteroinferior branches of the medial circumflex
artery (Fig. 21-5). At the level of the
intertrochanteric groove, the medial circumflex artery branches into a
retinacular arterial system (the posterosuperior and posteroinferior
arteries). These arteries penetrate the capsule and traverse proximally
(covered by the retinacular folds) along the neck of the femur to
supply the femoral head peripherally and proximally to the physis. The
posteroinferior and posterosuperior arteries persist throughout life
and supply the femoral head. At about 3 to 4 years of age, the lateral
posterosuperior vessels appear to predominate and supply the entire
anterior lateral portion of the capital femoral epiphysis. -
The vessels of the ligamentum teres are
of virtually no importance. They contribute little blood supply to the
femoral head until age 8, and then only about 20% as an adult.
 |
|
FIGURE 21-5
Arterial supply of the proximal femur. The capital femoral epiphysis and physis are supplied by the medial circumflex artery through two retinacular systems: the posterosuperior and posteroinferior. The lateral circumflex artery supplies the greater trochanter and the lateral portion of the proximal femoral physis and a small area of the anteromedial metaphysis. |
instance, the multiple small vessels of the young coalesce with age to
a limited number of larger vessels. As a result, damage to a single
vessel can have serious consequences; for example, occlusion of the
posterosuperior branch of the medial circumflex artery can cause AVN of
the anterior lateral portion of the femoral head.17
capsulotomy should be performed in order to decrease iatrogenic injury
to existing blood supply (Fig. 21-6A,B). It is
suspected that anterior capsulotomy does not damage the blood supply to
the femoral head as long as the intertrochanteric notch and the
superior lateral ascending cervical vessels are avoided.
that is considered less likely to tear than in adult hip fractures.
Bleeding within an intact capsule may lead to a tense hemarthrosis
after intracapsular fracture which can tamponade the ascending cervical
vessels and may have implications in the development of AVN. The hip
joint is surrounded on all sides by a protective cuff of musculature;
as such, open hip fracture is rare. In the absence of associated hip
dislocation, neurovascular injuries are rare.
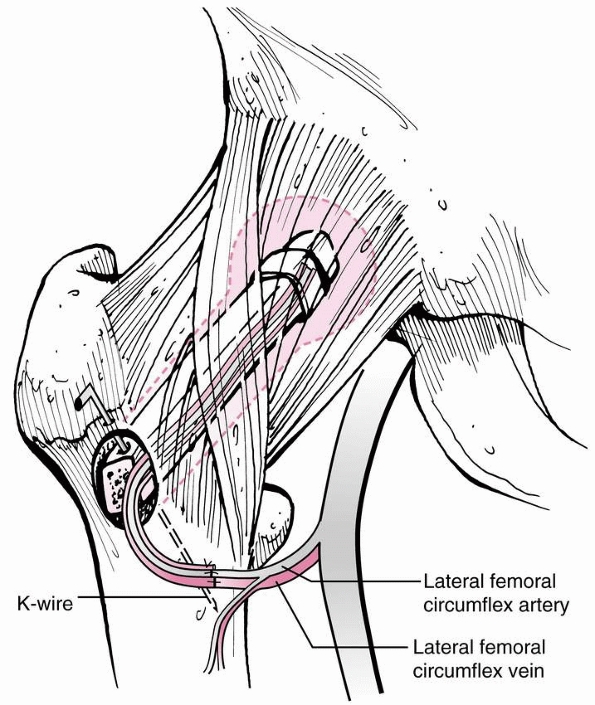
the quadratus medial to the greater trochanter. The lateral femoral
cutaneous nerve lays in the interval between the tensor and sartorius
muscles and supplies sensation to the lateral thigh. This nerve must be
identified and preserved during an anterolateral approach to the hip.
The femoral neurovascular bundle is separated from the anterior hip
joint by the iliopsoas. Thus, any retractor placed on the anterior
acetabular rim should be carefully placed deep to the iliopsoas to
protect the femoral bundle. Inferior and medial to the hip capsule,
coursing from the deep femoral artery toward the posterior hip joint,
is the medial femoral circumflex artery. Placement of a distal Hohmann
retractor too deeply can tear this artery, and control of the bleeding
may be difficult.
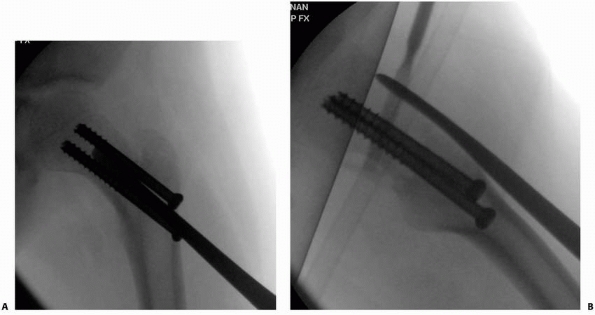 |
|
FIGURE 21-6 A,B.
Percutaneous placement of a periosteal elevator along the anterior femoral neck should allow fenestration of the capsule while protecting the posterior and superior blood supply. |
necessary, the Watson-Jones approach is a useful and direct approach to
the femoral neck. A lateral incision is made over the proximal femur,
slightly anterior to the greater trochanter (Fig. 21-7A). The fascia lata is incised longitudinally (Fig. 21-7B).
The innervation of the tensor muscle by the superior gluteal nerve is 2
to 5 cm above the greater trochanter, and care should be taken not to
damage this structure. The tensor muscle is reflected anteriorly. The
interval between the gluteus medius and the tensor muscles will be used
(Fig. 21-7C). The plane is developed between the muscles and the underlying hip capsule (Fig. 21-7D).
If necessary, the anterior-most fibers of the gluteus medius tendon can
be detached from the trochanter for wider exposure. After clearing the
anterior hip capsule, longitudinal capsulotomy is made along the
anterosuperior femoral neck. A transverse incision can be added
superiorly for wider exposure (Fig. 21-7E).
Once the hip fracture is reduced, guide wires for cannulated screws can
be passed perpendicular to the fracture along the femoral neck from the
base of the greater trochanter.
Care should be taken to identify and protect the lateral femoral
cutaneous nerve. The sartorius and rectus muscles can be detached to
expose the hip capsule. Medial and inferior retractors should be
carefully placed to avoid damage to the femoral neurovascular bundle
and medial femoral circumflex artery, respectively. Care must be taken
not to violate the intertrochanteric notch and the lateral ascending
vessels. Because the lateral aspect of the greater trochanter is not
exposed, wires must be passed percutaneously once the hip fracture is
reduced.
adequate closed reduction can be obtained thus avoiding the need to
open the hip joint for reduction purposes. However, the surgeon may
feel advised to perform a capsulotomy in order to decompress the hip
joint. The authors prefer to do this from a lateral approach. With this
method, a 4-cm incision is made distal and lateral to the greater
trochanter. From this incision, the fascia lata is incised and guide
pins for cannulated screws are placed and screws are inserted in the
standard manner. The anterior fibers of the gluteus medius are elevated
allowing incision of the anterior capsule with a Cobb elevator, knife,
or osteotome.
presence of femoral head dislocation, and fracture stability after
reduction. In toddlers under 2 years of age with nondisplaced or
minimally displaced fractures, simple spica cast immobilization is
likely to be successful. Because the fracture tends to displace into
varus and external rotation, the limb should be casted in
mild
abduction and neutral rotation to prevent displacement. Close follow up
in the early postinjury period is critical. Displaced fractures in
toddlers should be reduced closed by gentle traction, abduction, and
internal rotation. If the fracture “locks on” and is stable, casting
without fixation is indicated. If casting without fixation is done,
repeat radiographs should be taken within days to look for displacement
because the likelihood of successful repeat reduction decreases rapidly
with time and healing in a young child.
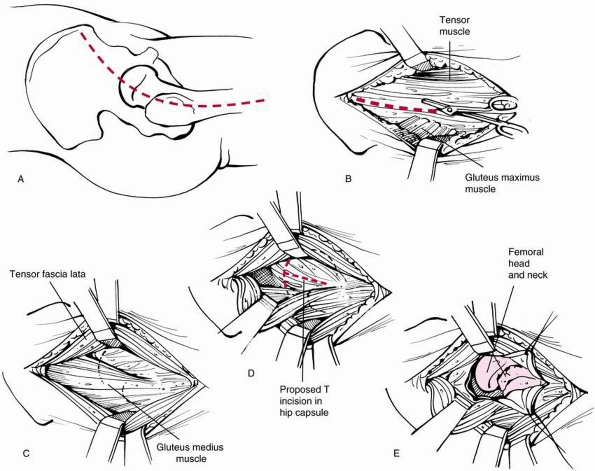 |
|
FIGURE 21-7 Watson-Jones lateral approach to the hip joint for open reduction of femoral neck fractures in children. A. Skin incision. B. Incision of the fascia lata between the tensor muscle (anterior) and gluteus maximus (posterior). C.
Exposure of the interval between the gluteus medius and tensor fascia lata (retracted anteriorly). Development of the interval will reveal the underlying hip capsule. D. Exposure of the hip capsule. E. Exposure of the femoral Mac after T incision of the capsule. |
smalldiameter (2-mm) smooth pins that cross the femoral neck and into
the physis. Use of smooth pins will theoretically decrease risk of
physis injury in younger patients with a transphyseal fracture. An
arthrogram after reduction and stabilization of the fracture may be indicated to insure alignment is anatomic. An arthrogram prior to reduction and pinning may obscure bony detail and hinder assessment during reduction.
fixation, even if the fracture is nondisplaced; because the
complications of late displacement may be great, fixation should cross
the physis into the capital femoral epiphysis. Smooth pins can be used
in young children, but cannulated screws are better for older, larger
children and adolescents. In this older group (>10 years of age) the
effect of eventual limb length discrepancy is small and is a reasonable
tradeoff for the superior fixation and stabilization needed to avoid
complications in larger and older children.
attempted, but immediate open reduction is necessary if a single
attempt at closed reduction is unsuccessful. Internal fixation is
mandatory. The surgical approach should be from the side to which the
head is dislocated, generally posterolateral. Parents must be advised
in advance about the risk of AVN.
all but the oldest and most reliable adolescents who have large
threaded screws crossing the physis. Fixation may be removed shortly
after fracture healing to enable further growth in patients.
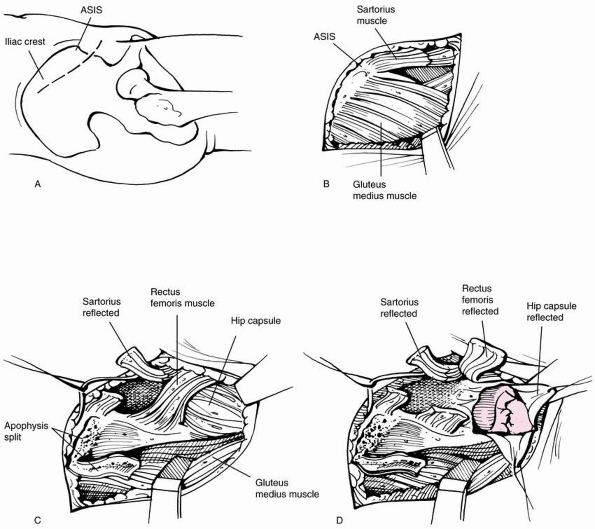 |
|
FIGURE 21-8 Smith-Petersen anterolateral approach to the hip joint. A. Skin incision. Incision is 1 cm below the iliac crest extends just medial to the anterior superior iliac spine. B.
Skin is retracted, exposing the fascia overlying the anterior superior iliac spine. The interval between the Sartorius and the tensor fascia lata is identifiable by palpation. C. The Sartorius is detached from the anterior superior iliac spine. Splitting of the iliac crest apophysis and detachment of the rectus femoris (shown attached to anterior inferior iliac spine) will facilitate exposure of the hip capsule. D. The hip capsule is exposed. A T incision is made to reveal the femoral head and neck. |
reduction and, in most cases, internal fixation. In rare cases,
children under 5 years of age with nondisplaced and completely stable
type II and cervicotrochanteric fractures can be managed with spica
casting and close follow-up to detect varus displacement in the cast.27,50,57 However, in almost all cases, internal fixation is recommended by most investigators for nondisplaced transcervical fractures35,50
because the risk of late displacement in such fractures far outweighs
the risk of percutaneous screw fixation, especially in young children.15
reduction and stable internal fixation to minimize the risk of late
complications. Coxa vara and nonunion were high in several large series
of displaced transcervical fractures treated with immobilization but
without internal fixation.18,57,102
However, when an anatomic closed or open reduction and internal
fixation was used, the rates of these complications were much lower.18,33,70,96
accomplished with the use of longitudinal traction, abduction, and
internal rotation. Open reduction frequently is necessary for displaced
fractures and should be done through a Watson-Jones surgical approach.
lesser trochanter. Two to three screws should be placed; if possible,
the most inferior screw will skirt along the calcar with the remaining
screws spaced as widely as possible.15
Usually, the small size of the child’s femoral neck will accommodate
only two screws. Care should be taken to minimize unnecessary drill
holes in the subtrochanteric region because they increase the risk of
subtrochanteric fracture.
the sequelae of premature physeal closure and trochanteric overgrowth
are much less than those of nonunion, pin breakage, and AVN. Treatment
of the fracture is the first priority, and any subsequent growth
disturbance and leg length discrepancy are secondary. Consideration may
be given to simultaneous capsulotomy or aspiration of the joint to
eliminate pressure from a hemarthrosis at the time of surgery.
to have a complication rate similar to that for type II fractures and
should be treated similarly. If possible, screws should be inserted
short of the physis in type III fractures. Fixation generally does not
need to cross the physis in type III fractures. Alternatively, a
pediatric hip compression screw can be used for more secure fixation of
distal cervicotrochanteric fractures in a child over 5 years of age.
Spica casting is routine in most type II and III fractures, except in
older reliable children where the screws cross the physis.33
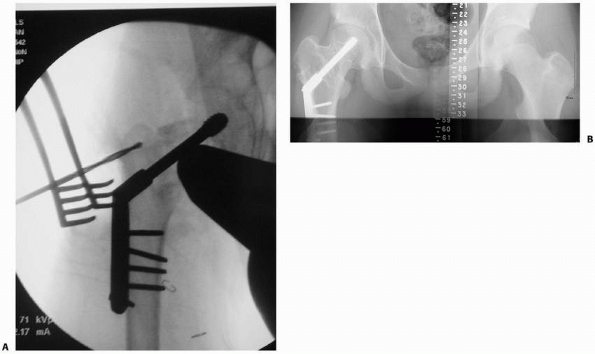
most intertrochanteric fractures, regardless of displacement. Traction
and spica cast immobilization are effective.14
Instability or failure to maintain adequate reduction and polytrauma
are indications for internal fixation. Children old enough to use
crutches or those with multiple injuries can be treated with open
reduction and internal fixation (Fig. 21-9). A pediatric hip screw provides the most rigid internal fixation for this purpose.
 |
|
FIGURE 21-9 A. A 14-year-old boy who fell from a tree swing sustained this nondisplaced left intertrochanteric hip fracture. B. Lateral radiograph shows the long spiral fracture. C. Three months after fixation with an adult sliding hip screw.
|
toddlers up to age 2 should be treated in a spica cast without internal
fixation. The limb should be casted in a position of abduction and
neutral rotation to prevent displacement into varus. If the fracture
requires reduction or moves significantly during reduction or casting
maneuvers, then internal fixation is mandatory. Two millimeter smooth
Kirschner-wires are inserted percutaneously to cross the physis. We
recommend two or three wires. Wires should be cut off and bent below
the skin for retrieval under a brief general anesthetic when the
fractures healed. We do not recommend leaving the wires outside the
skin. Frequent radiographs are necessary to check for migration of the
pins into the joint space. A spica cast is always applied in this age
group and should remain in place for at least 6 weeks.33
Even if type I fractures in children older than 2 years are
anatomically reduced, these patients should always have stabilization
with internal fixation. While Kirschner-wires are appropriate for small
children, 4.0- to 4.5-mm cannulated screws crossing the physis can be
considered in older, larger children after closed reduction.
Fluoroscopically laying a guide-pin across the femoral head and neck
allows one to locate the proper site for a small incision overlying the
lateral femur in line with the femoral neck. Two guide pins are placed
into the epiphysis, and the wires are overdrilled to the level of the
physis (but not across in order to avoid growth arrest as much as
possible). The hard metaphysis and lateral femoral cortex are tapped
(in contrast to elderly patients with osteoporosis) to the level of the
physis and stainless steel screws are placed.
approach is preferred for type IA fractures. For type IB fractures, the
choice of approach is dictated by the position of the femoral
epiphysis. If it is anterior or inferior, a Watson-Jones approach
should be used. On the other hand, most type IB fractures are displaced
posteriorly, in which case a posterior approach should be selected.
Under direct vision, the fracture is reduced and guide wires are passed
from the lateral aspect of the proximal femur up the neck perpendicular
to the fracture; predrilling and tapping are necessary before the
insertion of screws. All children are immobilized in a spica cast.
similar reduction methods on a fracture table, and the fracture is
stabilized after closed or, if needed, open reduction. Larger 6.5- or
7.3-mm screws are needed and are placed after predrilling and tapping
over the guide pins. Through a lateral incision, the screws are placed,
and an anterior capsulotomy is performed. Such stout fixation usually
obviates the need for spica casting in an adolescent but, if future
patient compliance or fracture stability is in doubt, a spica cast is
used.
unsuccessful, we prefer reduction through a Watson-Jones approach
because it provides the most direct exposure of the femoral neck for
gentle fracture reduction. This approach allows the fracture to be
anatomically reduced under direct vision. Guide wires are then placed
up the femoral neck perpendicular to the fracture. If possible,
penetration of the physis should be avoided.20,32
However, in most unstable Type II fractures, penetration of the physis
may be necessary to achieve stability and avoid the complications
associated with late displacement.14,70
Good fixation of type III fractures generally is possible without
penetration of the physis. Type II and III fractures should be
stabilized with 4.0- to 4.5-mm cannulated screws in small children up
to age 8 years. After the age of 8 years, fixation with 6.5-mm
cannulated screws is appropriate. Two or three appropriately sized
screws should be used, depending on the size of the child’s femoral
neck. As in type I fractures, we recommend placing at least two guide
pins, and predrilling and tapping of the femoral neck is necessary to
avoid displacement of the fracture while advancing the screws. Finally,
we believe that if the physis is not crossed with implants,
supplementary spica casting is needed to prevent malunion or nonunion.
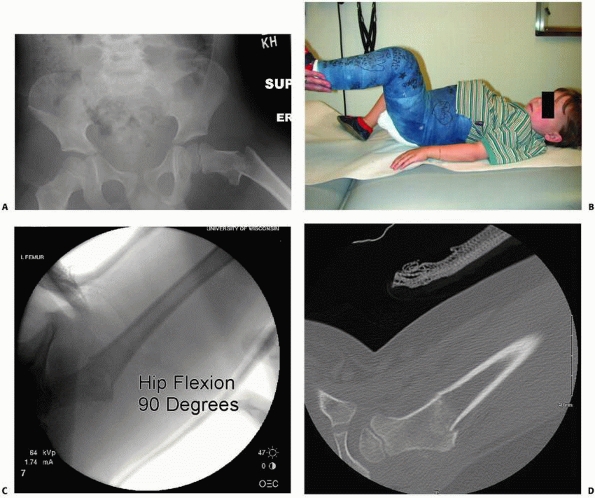
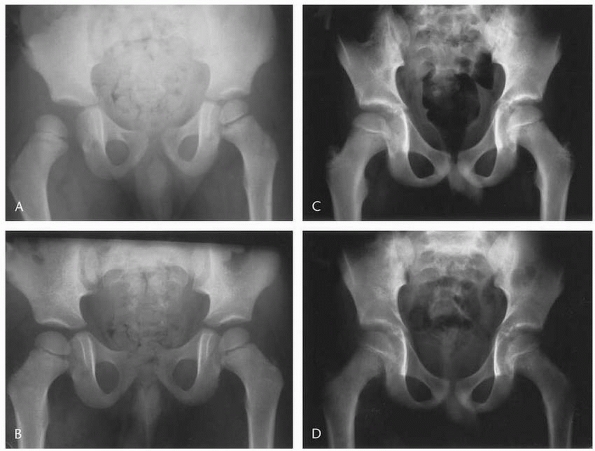
to 4 years are treated without internal fixation with immobilization in
a spica cast for 12 weeks. Great care is needed to cast the limb in a
position that best aligns the bone (Fig. 21-10A,B).
Frequent radiographic examination is necessary to assess for late
displacement, particularly into varus. In some cases, it may be
difficult to assess reduction in a spica cast so that alternative
testing such as a limited CT scan may be useful to compare to
intraoperative positioning (Fig. 21-10C,D).
Displaced type IV fractures in all children more than 3 years of age
should be treated with internal fixation with a pediatric or juvenile
compression hip screw placed into femoral neck short of the physis. It
is important to place an antirotation wire before drilling and tapping
the neck for the dynamic hip screw. Closed reduction often is possible
with a combination of traction and internal rotation of the limb. If
open reduction is necessary, a lateral approach with anterior extension
to close reduce the fracture is preferred.
considered for the majority of patients with proximal femoral
fractures. For instance, casting is indicated in all type I fractures
except in the rare adolescents who have been treated with two to theree
large screws that cross the physis and who will be obviously compliant
with restricted weight bearing. For type II and III fractures, we
recommend a hip spica cast to be used in all patients whose implants do
not cross the femoral epiphysis for at least 6 weeks. This
recommendation makes sense when one considers that in children younger
than 10, we try to avoid crossing the physis, and these patients
usually do well with these casts. On the other hand, children greater
than 12 years of age can be treated with transphyseal fixation that
will be stable enough to avoid cast fixation and which coincidently
also tends to be poorly tolerated in this age group. For children 10 to
12 years of age, the use of a postoperative cast depends on the
stability of fracture fixation and the patient’s compliance; if either
is in doubt, a single hip spica cast is used.
plate do not require cast immobilization. Formal rehabilitation usually
is unnecessary unless there is a severe persistent limp, which may be
due to abductor weakness. Stiffness is rarely a problem in the absence
of ON.
-
Table 21-1
summarizes the pearls of surgical stabilization of pediatric hip
fractures, including recommended choices of implants for internal
fixation. -
For young, small patients, the operation
should be done on a radiolucent operating table rather than on a
fracture table, which is more appropriate for older and larger
adolescents. -
Because the femoral bone in children is
harder than the osteoporotic bone in elderly patients, predrilling and
pretapping are necessary for insertion of all screws. -
Multiple attempts at wire placement
should be avoided because they result in empty holes in the
subtrochanteric region of the femur. This predisposes to late
subtrochanteric fracture below or at the level of the screw heads after
removal of the spica cast. -
A hip spica cast must be used to
supplement internal fixation in all patients who are younger than 10
years. For older patients, if the stability of the fracture is
questionable or if the child’s compliance is doubtful, the surgeon
should not hesitate to apply a hip spica cast. The quality of reduction
and the stability of the fixation have a direct impact on the
occurrence of nonunion.33,57,70,84 -
Growth of the femur and the contribution
of the proximal femoral physis are important; however, this physeal
contribution to growth is only 13% of the entire extremity, or 3 to 4
mm per year on average. Once the decision for internal fixation of a
fracture of the head or neck of the femur is made, stable fixation of
the fracture is a higher priority than preservation of the physis. If
stability is questionable, the internal fixation device should extend
into the femoral head for rigid, stable fixation, regardless of the
type of fracture or the age of the child.
 |
|
FIGURE 21-10 A. A 4-year-old boy fell from his window, causing a displaced type IV. B. Positioning of the hip in a spica cast is usually in hip flexion and confirmed under fluoroscopy. C. Fluoroscopic radiographs in 90 degrees of hip flexion insure anatomic correctness. D. At 1-week follow-up, radiographs were inconclusive; a CT scan assists in confirming location.
|
|
TABLE 21-1 Surgical Tips and Pearls for Hip Fractures in Children
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||
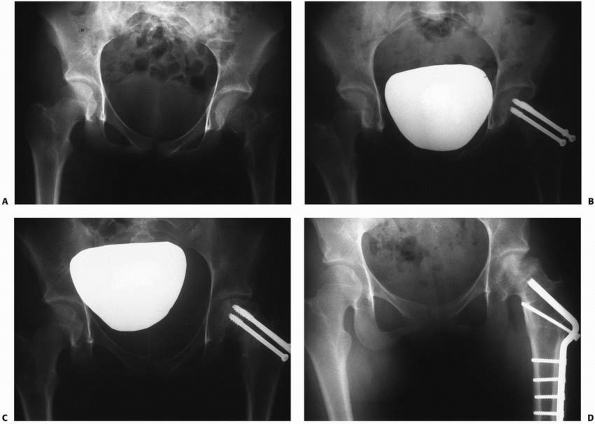
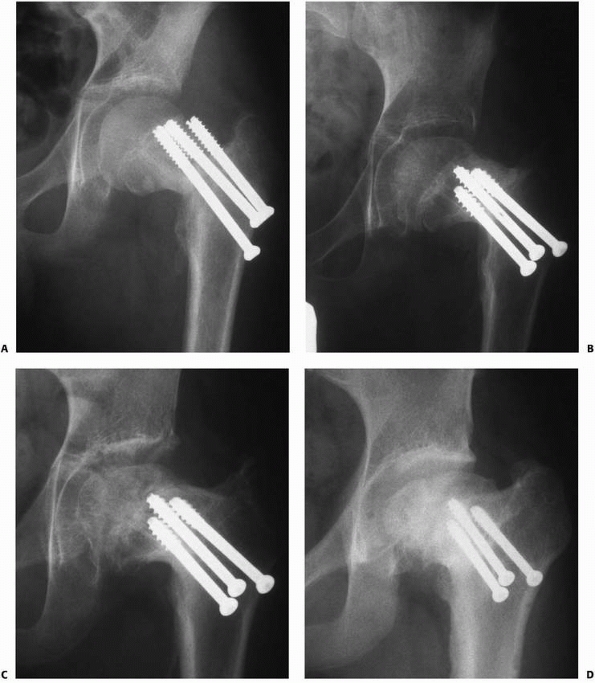
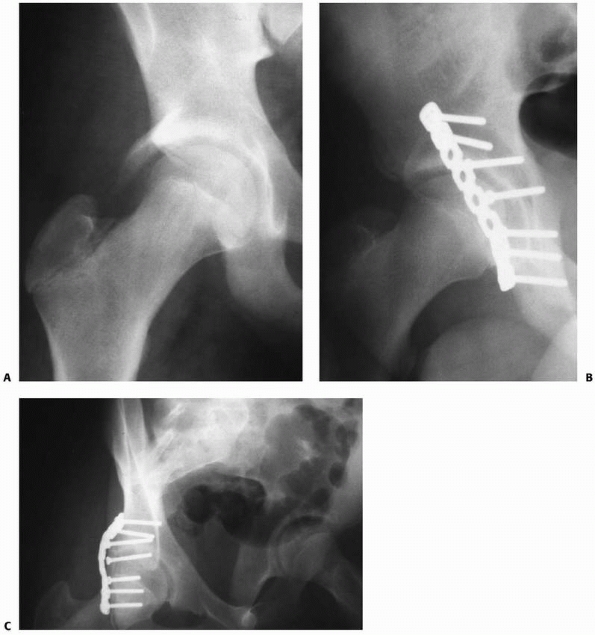
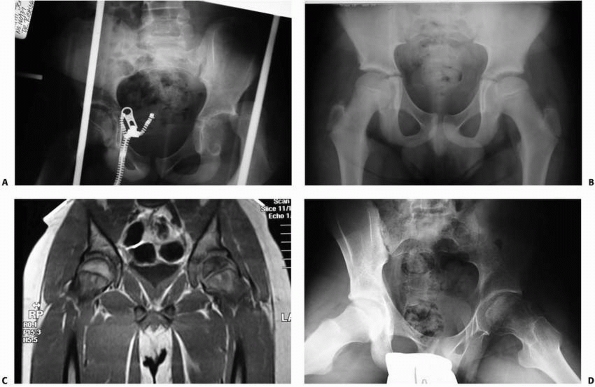
fractures in children and is the primary cause of poor results after
fractures of the hip in children. Its overall prevalence is
approximately 30%, based on the literature.21,50,71 The risk of AVN is highest after displaced type IB, II, and III fractures (Fig. 21-11).14 In the recent meta-analysis by Moon and Mehlman,68
the incidence of AVN in type I through type IV is 38%, 28%, 18%, and
5%, respectively. In addition to location of the fracture (via Delbet
classification), AVN is felt to be increased with increased fracture
displacement and older age at the time of injury.61
Several studies report lower rates of AVN in their series of patients
treated within 24 hours of injury with prompt reduction and internal
fixation.21,33,96
This approach to early reduction and stabilization may decrease AVN by
preventing further injury to the tenuous blood supply, and open
reduction or capsulotomy
may decrease intra-articular pressure caused by fracture hematoma.50,71,97
The later concept has equivocal support in the literature with some
papers reporting that aspirating the hematoma may decrease the
intracapsular pressure and increase blood flow to the femoral head21,71; others suggest that this may have little effect.50,64,78A
final important factor that may reduce AVN is stability and quality of
reduction: this is highlighted in a recent 30-year experience of hip
fractures from Mayo Clinic.90 In
this paper, AVN was associated with inadequate reduction and use of
older implant styles. In our institution, we recognize that the die may
already be cast at the time of injury, but we still advocate emergent
anatomic reduction and stabilization of the fracture in order to reduce
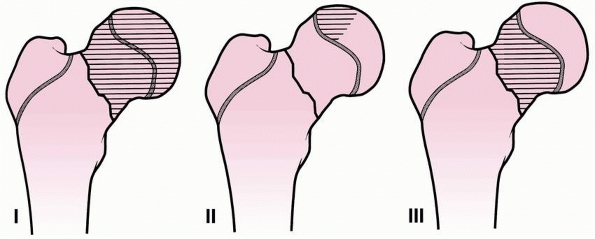
risk of AVN. AVN has been classified by Ratliff as follows: type I,
involvement of the whole head; type II, partial involvement of the
head; and type III, an area of necrosis of the femoral neck from the
fracture line to the physis (Fig. 21-12).84
Type I is the most severe and most common form and has the poorest
prognosis. Type I probably results from damage to all of the
retinacular epiphyseal vessels, type II from localized damage to one or
more of the lateral epiphyseal vessels near their insertion into the
anterolateral aspect of the femoral head, and type III from damage to
the superior metaphyseal vessels. Type III is rare but has a good
prognosis provided the fracture goes on to heal.84
Signs and symptoms of AVN usually develop within the first year after
injury, but many patients may not become symptomatic for up to 2 years.50,83
Some authors have utilized bone scanning for early detection of AVN as
further collapse may be prevented with use of bisphosphonate therapy.
Recently, Little and his colleagues59
treated 17 children and adolescents with early bone scan changes of AVN
from slipped capital femoral epiphysis or femoral neck fracture. The
group was treated with an intravenous bisphosphonate (pamidronate or
zolendronate) for an average of 20 months, which greatly improved the
outcome at 3 year follow-up.82 The
long-term results of established AVN are likely related to age of the
patient and extent and location of the necrosis within the head;
results are usually poor in over 60% of patients.18,27,34,74 There is no clearly effective treatment for established posttraumatic AVN in children.50,83
Older children (more than 10 years of age) tend to have worse outcomes
than younger children. Treatment of AVN is controversial and
inconclusive and is beyond the scope of this text. Ongoing research
includes the role of redirectional osteotomy,62 distraction arthroplasty with external fixation, core decompression, vascularized fibular grafting (Fig. 21-13), and direct bone grafting.
 |
|
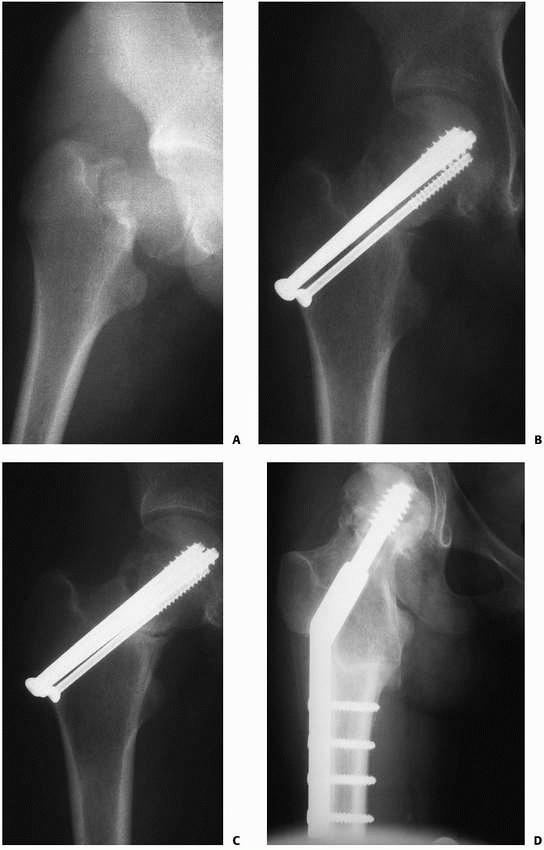
FIGURE 21-11 A. A 14-year-old girl with a type II fracture of the left femoral neck. B. After fixation with three cannulated screws. C. AVN with the collapse of the superolateral portion of the femoral head. D. After treatment with valgus osteotomy.
|
 |
|
FIGURE 21-12
The three types of AVN. Type I, whole head; type II, partial head; and type III, femoral neck. (Reprinted from Ratliff AHC. Fractures of the neck of the femur in children. J. Bone Joint Surg Br 1962:44:528, with permission.) |
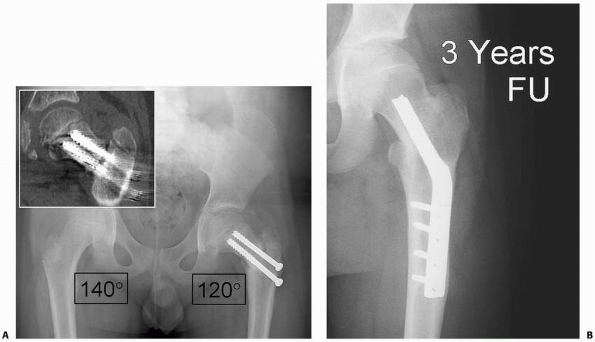
Severe coxa vara raises the greater trochanter in relation to the
femoral head, causing shortening of the extremity and leading to
inefficiency of the abductors. Remodeling of an established malunion
may occur if the child is less than 8 years of age, or with a
neck-shaft angle greater than 110 degrees. Older patients with
progressive deformity may not remodel and subtrochanteric valgus
osteotomy may be considered to heal nonunion, restore limb length, and
the abductor moment arm (Fig. 21-15).50
 |
|
FIGURE 21-13
Vascularized fibular grafting for osteonecrosis of the femoral head. (Redrawn after Aldrich JM III, Berend KR, Gunneson EE, et al. Free vascularized fibular grafting for the treatment of postcollapse osteonecrosis of the femoral head. J Bone Joint Surg Am 2004;86:87-101, with permission). |
The risk of premature physeal closure increases with penetration by
fixation devices or when AVN is present. It is most common in patients
who have Type II or III ON (see Fig. 21-14).83,84
growth of the entire extremity and normally closes earlier than most of
the other physes in the lower extremity. As a result, shortening due to
premature physeal closure is not significant except in very young
children.14,52 Treatment for leg length discrepancy is indicated only for significant discrepancy (2.5 cm or more projected at maturity).50
If femoral growth arrest is expected due to the implant use or injury
to the physis, the surgeon may consider concomitant greater
trochanteric epiphysiodesis to maintain a more normal articular
trochanteric relationship (Fig. 21-16).
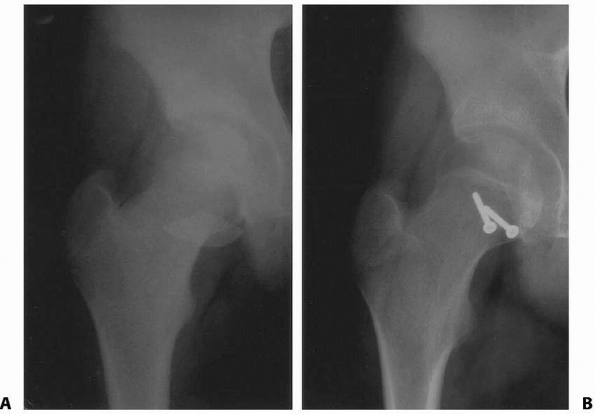
Nonunion is a complication seen in type II and III fractures and is not
generally seen after type I or type IV fractures. The primary cause of
nonunion is failure to obtain or maintain an anatomic reduction.14,16
After femoral neck fracture in a child, pain should be gone and
bridging new bone should be seen at the fracture site by 3 months after
injury. A CT scan may be helpful to look for bridging bone. If no or
minimal healing is seen by 3 to 6 months, the diagnosis of nonunion is
established. Nonunion should be treated operatively as soon as
possible. Either rigid internal fixation or subtrochanteric valgus
osteotomy should be performed to allow compression across the fracture (Fig. 21-17).58
Because the approach necessary for bone grafting is extensive, it
should be reserved for persistent nonunion. Internal fixation should
extend across the site of the nonunion, and spica cast immobilization
should be used in all but the most mature and cooperative adolescents.
is consistent with the expected infection rate in any closed fracture
treated surgically with open reduction and internal fixation.
Chondrolysis is exceedingly rare and has been reported only in two
series.6,34
Care must be taken to avoid persistent penetration of hardware into the
joint, which can cause chondrolysis in conditions such as slipped
capital femoral epiphysis. Finally, a case report of a slipped capital
femoral epiphysis has been reported after fixation of an ipsilateral femoral neck fracture.51
 |
|
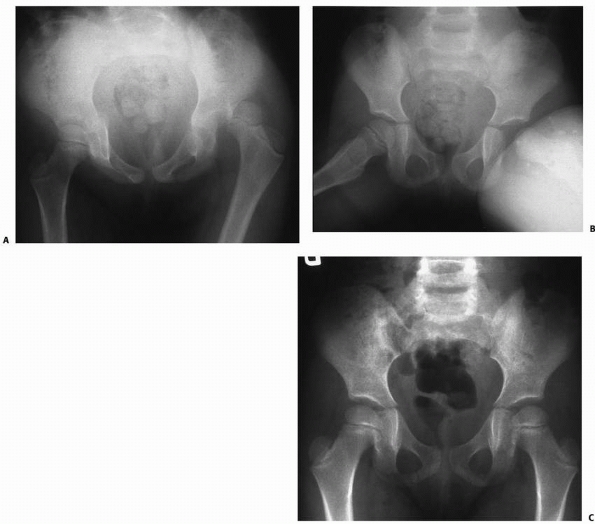
FIGURE 21-14 A. A 12-year-old boy with a type III left hip fracture. Poor pin placement and varus malposition are evident. B. The fracture united in mild varus after hardware revision. C. Fourteen months after injury, collapse of the weight-bearing segment is evident. D.
Six years after injury, coxa breva and trochanteric overgrowth are seen secondary to avascular necrosis, nonunion, and premature physeal closure. |
are extremely uncommon in children, and only a few cases have been
published in the English-language literature. In one study of 40 stress
fractures in children, there was only one femoral neck stress fracture.28
The rarity of such fractures underscores the need for a high index of
suspicion when a child has unexplained hip pain. The differential can
be long for hip pain in children, and early diagnosis and treatment are
essential to avoid complete fracture with displacement.
of the femoral neck in children usually result from repetitive cyclic
loading of the hip, such as that produced by a new or increased
activity. A recent increase in the repetitive activity is highly
suggestive of the diagnosis. An increase in intensity of soccer,12
and an increase in distance running are examples of such activities.
Younger children often present with a limp or knee pain and may not
have a clear history of increased activity.65
Underlying metabolic disorders or immobilizations that weaken the bone
may predispose to stress fracture. In adolescent female athletes,
amenorrhea, anorexia nervosa, and osteoporosis have been implicated in
the development of stress fractures of the femoral neck.44
 |
|
FIGURE 21-15 A.
A 10-year-old boy with a type III fracture treated without cast immobilization develops progressive varus deformity 4 months after surgery. Inset CT scan demonstrates delayed union. Valgus osteotomy is indicated for his progressive varus deformity and delayed healing. B. Three years after valgus osteotomy, the fracture is healed and the deformity corrected. |
groin pain with or without a limp. The pain may be perceived in the
thigh or knee and may be mild enough so that it does not significantly
limit activities. In the absence of displacement, examination typically
reveals slight limitation of hip motion with increased pain, especially
with internal rotation. Usually plain radiographs reveal the fracture,
but in the first 4 to 6 weeks after presentation, plain films may be
negative. If there are no changes or only linear sclerosis, a bone scan
will help identify the fracture. MRI has been documented as a sensitive
test for undisplaced fractures of the femoral neck. If a sclerotic
lesion is seen on plain radiographs, the differential diagnosis should
include osteoid osteoma, chronic sclerosing osteomyelitis, bone
infarct, and osteosarcoma. Other causes of hip pain, include slipped
capital femoral epiphysis, Legg-Calvé-Perthes disease, infection,
avulsion injuries of the pelvis, eosinophilic granuloma,
and
bony malignancies. Stress fractures unrelieved by rest or treatment may
progress with activity to complete fracture with displacement.98 For this reason, prompt diagnosis and treatment are important.
 |
|
FIGURE 21-16 A.
Greater trochanteric epiphysiodesis is performed at time of open reduction and internal fixation of a pathologic femoral neck fracture (see Fig. 21-1) in 10-year-old boy. Because the implant crosses the physis, growth arrest is expected and trochanteric arrest may minimize trochanteric overgrowth. B. Seven-year follow-up shows that growth arrest occurred and some trochanteric mismatch is present despite prior epiphysiodesis. |
 |
|
FIGURE 21-17 A. A 15-year-old girl with a markedly displaced type II femoral neck fracture. B.
She underwent open reduction and internal fixation with two 7.3-mm cannulated screws and one 4.5-mm cannulated screw. Primary bone grafting of a large defect in the superior neck was also performed. C. Radiograph at 5 months showing a persistent fracture line D. Six weeks after valgus intertrochanteric osteotomy. The fracture is healing. |
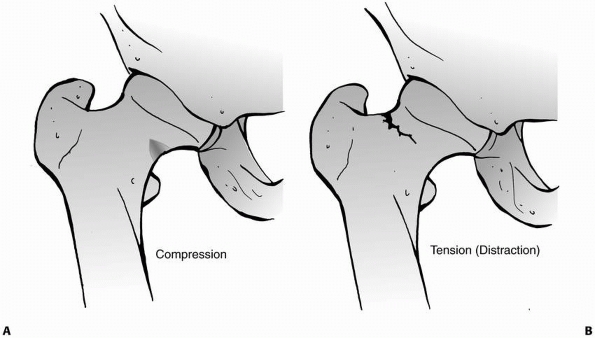
The compression type appears as reactive bone formation on the inferior
cortex without cortical disruption. This type rarely becomes completely
displaced but may collapse into a mild varus deformity,29 and compression types have been reported to progress to complete fracture without early treatment (Fig. 21-18).98
The tension type is a transverse fracture line appearing on the
superior portion of the femoral neck. This type is inherently unstable
because the fracture line is perpendicular to the lines of tension.
Tension stress fractures have not been reported in children but may
occur in skeletally mature teenagers.98
fractures generally can be treated with a period of nonweight bearing
on crutches. Partial weight bearing can be allowed at 6 weeks with
progression to
full
weight bearing at 12 weeks provided that the pain is resolved and there
is radiographic evidence of healing. Close follow-up and careful
evaluation is mandatory to insure that the fracture heals without
propagation. Underlying conditions should be evaluated and addressed.
In small or uncooperative children, spica casting may be necessary.
Displacement into varus, however minimal, mandates internal fixation.
Tension fractures are at high risk for displacement and should be
treated with in situ compression fixation using cannulated screws.
the most common complication of untreated compression-type fractures.
Acute displacement of this type also has been described.108
Once displaced, the stress fracture is subject to all the complications
of Type II and Type III displaced femoral neck fractures.
 |
|
FIGURE 21-18 A line drawing of stress fractures, comparing compression (A) and stress (B) types.
|
The character of the injury tends to vary in that children under age 6
commonly suffer isolated hip dislocation from a low-energy injury,
whereas older children require a high-energy mechanism to dislocate the
hip, and these injuries are often associated with more severe trauma.5,10,36,43,75,88
Most hip dislocations in children can be reduced easily, and long-term
outcome is generally good with prompt and complete reduction. Delay in
reduction or neglected dislocations routinely do poorly, with a high
incidence of AVN.7,8
Incomplete reductions can occur from interposed soft tissue or bony
fragments, and postoperative imaging is mandatory to insure complete
reduction.22,106
Difficult reductions or those that occur during the early teenage years
(with a widened proximal femoral physis) should be performed with
anesthesia, muscle relaxation, and the use of fluoroscopy to ensure
that physeal separation does not occur.48,74
Open reduction may be needed if the hip cannot be reduced or if there
is a femoral head fracture or an incarcerated fragment. Incomplete
reductions may be treated open or arthroscopically.54
Complications, although uncommon, may occur, and these patients should
be closely followed for recurrent subluxation, dislocation, and AVN.5,46,88
Anterior dislocations can occur superiorly or inferiorly and result
from forced abduction and external rotation. If the hip is extended
while undergoing forced abduction and external rotation, it will
dislocate anteriorly and superiorly; if the hip is flexed while
abducted and externally rotated, the femoral head
tends
to dislocate anteriorly and inferiorly. In very rare cases, the femoral
head may dislocate directly inferiorly, a condition known as luxatio
erecta femoris or infracotyloid dislocation. Although this condition is
extremely rare, it tends to occurs more commonly in children than
adults.87
 |
|
FIGURE 21-19 A typical posterior dislocation of the hip.
|
 |
|
FIGURE 21-20 An anterior (inferior) dislocation of the hip.
|
 |
|
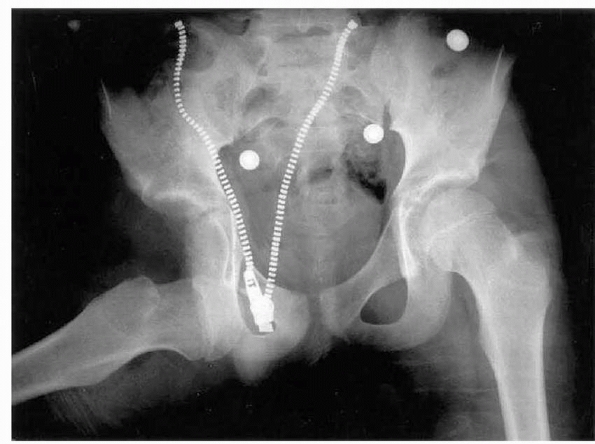
FIGURE 21-21 A.
A girl age 4 years and 7 months presented with a posterior dislocation of the left hip. This is often the result of a low-energy injury, such as a fall from play. B. Frog-leg lateral radiograph at injury. C. Eight months after successful closed reduction, radiographic appearance is normal. |
surprisingly little force, such as a fall while at play. The mechanism
for hip dislocations in older children and adolescents is similar to
that of adults in that significant trauma is needed. In a recent French
study,5 the authors assessed
children with hip dislocations and divided them into two groups by age:
those under 6 years old (7 patients) and those age 6 and older (7
patients). All the children in the under age 6 group had low-energy
mechanisms and isolated hip dislocations without other injuries, but
often had predisposing factors, such as hyperlaxity, coxa valga, or
decreased acetabular coverage (Fig. 21-21). In the over 6-year-old group, all the dislocations were a result of higherenergy injuries and often had associated injuries.5 Football and motor vehicle accidents are the most common etiology, combining
for over 50% of the dislocations in older children and adolescents.66
Children sometimes feel the pain in the knee rather than in the hip.
The hallmark of the clinical diagnosis of dislocation of the hip is
abnormal positioning of the limb, which is not seen in fracture of the
femur. Dislocations may spontaneously reduce, leaving the child with an
incompletely reduced hip that is commonly misdiagnosed. Price et al.81
reported on 3 children who presented with a history of trauma and an
incongruous hip. In all cases, the diagnosis was originally missed.81
mechanism of injury often present with associated injuries. In one
study of 42 patients, there were 17 fractures in 9 patients and 1
closed head injury. Of the 17 fractures, 6 were posterior acetabular
wall factures and 1 required open reduction and internal fixation.66
Careful evaluation of this injury in younger children with MRI is
important because standard radiographic assessments and CT may
underestimate the size of the fragment.86
Posterior dislocations of the femoral head can result in injury to the
sciatic nerve in about 10% of adults and 5% of children. Partial
recovery occurs in 60% to 70% of patients.25 The function of the sciatic nerve should be specifically tested at the time of the initial assessment and after reduction.
 |
|
FIGURE 21-22 A. A girl aged 13 years and 11 months sustained a left posterior hip dislocation in a motor vehicle accident. B. CT scan after reduction showed intra-articular bony fragments. C.
At open reduction and capsulorrhaphy, the bony fragments were removed. Suture anchors were used to reattach capsule to bone. Ten months after injury, there is no sign of ON. Heterotopic ossification is seen. Bony fragments can also be removed arthroscopically. |
neurovascular bundle, and femoral nerve function and perfusion of the
limb should be assessed. Tears of the capsule or acetabular labrum
occur and prevent concentric reduction of the hip. Postreduction
imaging must be carefully evaluated to insure that there is not
interposed soft tissue, such as the labrum or capsule, or osteochondral
fragments (Fig. 21-22). Rupture of the ligament teres is common in hip dislocations and can rarely be a cause of residual pain in some patients.16
high-energy injuries. One study evaluated the ipsilateral knees in 28
adults who had a traumatic hip dislocation and found that 75% had knee
pain and 93% had MRI evidence of a knee injury; effusion, bone bruise,
and meniscal tears were the most common findings.89
Traumatic dislocations with spontaneous reductions may be more subtle
and are often missed. Radiographs should be examined for fracture of
the acetabular rim and proximal femur, which may be associated with
dislocation. Any asymmetry of the joint space, as compared to the
contralateral hip, is a common finding with interposed tissue. MRI or
CT scanning is useful for evaluating the acetabulum and may be useful
in localizing intra-articular bony fragments or soft tissue
interposition after reduction.47,66,106 The identification of nonbony fragments is difficult by CT without the use of concomitant arthrography.47
MRI is useful for evaluating soft tissues that may be interposed
between the femoral head and acetabulum. MRI is especially helpful in
nonconcentric reductions when the initial direction of dislocation is
unknown, and in younger children with less boney ossification (Fig. 21-23).86,106
and the diagnosis is commonly missed if it is not considered. The
presence of air in the hip joint, which may be detectable on CT scan of
the pelvis, is evidence that a hip dislocation has occurred.32 Dislocation and spontaneous reduction with interposed tissue can occur and lead to late arthropathy if untreated.77
Widening of the joint space on plain radiographs suggests the
diagnosis. In patients with hip pain, a history of trauma, and widening
of the joint space, consideration should be given to MRI or
arthrography to rule out dislocation with spontaneous relocation
incarcerating soft tissue. If incarcerated soft tissues or osseous
cartilage fragments are found, open or arthroscopic removal is required
to obtain concentric reduction of the hip.54
depending on where the femoral head lies in relation to the pelvis,
namely posterior, anterior superior, anterior inferior, or
infracotyloid.105 The dislocation is
posterior more than 90% of the time. The Stewart-Milford classification
is based on associated fractures. Grade I is defined as dislocation
without an associated fracture or only a small bony avulsion of the
acetabular rim, grade II is a posterior rim fracture with a stable hip
after reduction, grade III is a posterior rim fracture with an unstable
hip (Fig. 21-24), and grade IV is a dislocation that has an associated fracture of the femoral head or neck.
 |
|
FIGURE 21-23 Two examples of partial reduction after reduction of a dislocated hip. In the first case the asymmetry is well visualized (A), labral entrapment was identified and removed and complete reduction was achieved (B). The asymmetry is less obvious in the second case (C), yet arthrotomy was still needed to remove an osteochondral fragment and achieve complete reduction (D).
|
head or the acetabulum is much more unusual in children than in adults.
Older adolescents may sustain adult-type fracture-dislocations of the
hip, and these are most commonly classified by the methods of Pipkin.79 He classified the head fractures as occurring either caudal to the fovea with a resultant small fragment (type 1) (Fig. 21-25),
cranial to the fovea with a resultant large fragment (type 2), any
combined femoral head and neck fracture (type 3), and any femoral neck
fracture with an acetabular fracture (type 4). The youngest patient in
his series from 1957 was 20, and most of these fractures were due to
the relatively new phenomena of traffic accidents.
children. In this condition, the child can actually voluntarily
dislocate the hip. Many factors may contribute to this ability,
including generalized ligamentous laxity or hyperlaxity disorders,
excessive anteversion of the femur and acetabulum, and coxa valga.95
A commonly confused condition is snapping of the iliotibial band over
the greater trochanter, and often the patient will describe this as
“dislocating their hip.” Yet, the hip remains well seated both before
and after snap, which can be quite dramatic. The more common iliotibial
band snapping can usually be differentiated from a true hip dislocation
by exam, or if needed, radiographs with the hip “in” versus “out.” A
snapping iliotibial band will demonstrate a well seated hip on both
radiographs.
by the articulation of the rounded head of the femur and the cup-like
acetabulum of the pelvis. If this is injured early in childhood, the
growth of the acetabulum can be affected and result in acetabular
dysplasia13,93 or impingement.37,42,73
 |
|
FIGURE 21-24 A.
A 12-year-old boy was tackled from behind in football. The right hip was dislocated. Reduction was easily achieved, but the hip was unstable posteriorly as a result of fracture of the posterior rim of the acetabulum. This is the most common accompanied fracture. B. The fracture and capsule were fixed via a posterior approach. C. Oblique view shows reconstitution of the posterior rim. |
 |
|
FIGURE 21-25 A.
A posterior dislocation associated after reduction with a femoral head fracture caudal to the ligament teres (Pipkin type 2). This is uncommon in children. This was treated with open reduction and internal fixation, with follow-up radiographs taken 1 year after the injury (B). |
is to obtain concentric reduction as soon as possible. Reduction of a
pediatric or adolescent hip dislocation should be considered an
orthopaedic emergency. Generally, closed reduction should be attempted
initially. Successful closed reduction can be achieved with intravenous
or intramuscular sedation in the emergency room in many patients.85
Complete muscle relaxation is required for others, and this is best
provided in the operating room with a general anesthetic. Open
reduction is indicated if closed reduction is unsuccessful or
incomplete. In children, especially in their early teenage years, cases
of proximal physeal separation with attempted closed reduction have
been reported, and therefore the uses of fluoroscopy to assess the
stability of the proximal femoral physis is highly recommended.48,74
for reduction of posterior dislocations. With any type of dislocation,
traction along the axis of the thigh coupled with gentle manipulation
of the hip often affects reduction after satisfactory relaxation of the
surrounding muscles.
maneuver in which the patient is placed supine and the reducing surgeon
stands above the patient. For this reason, either the patient must be
placed on the floor or the surgeon must climb onto the operating table.
The knee is flexed to relax the hamstrings. While an assistant
stabilizes the pelvis, the surgeon applies longitudinal traction along
the axis of the femur and gently manipulates the femoral head over the
rim of the acetabulum and back into the acetabulum.
method but after traction, the femoral head is then levered into the
acetabulum by abducting, externally rotating, and extending the hips.
This is a more forceful maneuver and may cause damage to the articular
surfaces of hip or even fracture the femoral neck; this technique is
not therefore recommended and must be performed with caution,
especially in children.
entails placing the patient prone with the lower limbs hanging over the
edge of a table. An assistant stabilizes the patient while the surgeon
applies gentle downward pressure with the knee and hip flexed 90
degrees, in an attempt to pull the femoral head anteriorly over the
posterior rim of the acetabulum and back into the socket. Gentle
internal and external rotation may assist in the reduction.
using reasonable measures, it is appropriate to proceed with open
reduction and inspection of the joint, to remove any obstructing soft
tissues, and identify intra-articular osteochondral fragments. Imaging
can be performed prior to reduction but it should not delay treatment.
with the femur and gently manipulating the femoral head back into the
acetabulum should be performed. A controlled reduction with sedation or
general anesthesia and muscle relaxation is preferable, and aggressive
techniques should not be attempted without muscle relaxant. The use of
fluoroscopy to monitor the reduction, especially in children over 12
with open physis, is important to insure that proximal femoral
epiphysiolysis does not occur. Surgery is indicated for dislocations
that are irreducible or for nonconcentric reductions. More advanced
imaging (CT or MRI) should be considered after reduction to assess for
interposing fragments of bone, cartilage, or soft tissue.
performed through a posterolateral (Kocher-Langenbeck) approach. The
patient is positioned in the lateral decubitus position with the
dislocated side facing up. The incision is centered on and just
posterior to the greater trochanter and goes up into the buttock.
Generally, a straight incision can be made with the hip flexed
approximately 90 degrees. Once the fascia lata is incised, the femoral
head can be palpated beneath or within the substance of the gluteus
maximus muscle. The fibers of the gluteus maximus can then be divided
by blunt dissection, exposing the dislocated femoral head. The path of
dislocation is followed through the short external rotator muscles and
capsule down to the acetabulum. The sciatic nerve lies on the short
external rotators and should be identified and inspected. The
piriformis may be draped across the acetabulum, obstructing the
reduction. It may be necessary to detach the short external rotators to
see inside the joint. After the joint is inspected, repair of the
fracture of the posterior acetabular rim can be performed if present in
the standard fashion.
anterior approach. This can be done through a bikini incision that uses
the interval between the sartorius and the tensor fascia lata. The deep
dissection follows the defect created by the femoral head down to the
level of the acetabulum.
acetabulum should be inspected for damage. Any intra-articular
fragments should be removed. The labrum and capsule should be inspected
for repairable tears. Labral fragments that cannot be securely replaced
should be excised, but repair should be attempted. Frequently, the
labrum or hip capsule is entrapped in the joint. The femoral head
should be dislocated and any interposed soft tissue extracted. A
headlight may be needed for visualization, and a Schanz screw or bone
hook may be needed to displace the femur enough to see inside the joint.
and the traumatic defect enlarged if necessary. The hip joint is then
reduced under direct vision. Postreduction radiographs should be taken
to confirm concentric reduction. If the joint appears slightly widened,
repeat investigation to rule out interposed tissue. Slight widening may
be due to fluid in the hip joint or decreased muscle tone, and this may
improve over the next few days. The capsule is repaired if possible.
irrigation and débridement. The surgical incision should incorporate
and enlarge the traumatic wound. Inspection should proceed as detailed
above. Capsular repair should be attempted if the hip joint is not
contaminated. The wound should be left open or should be well drained
to prevent invasive infection.
As in all open fractures, intravenous antibiotics should be administered and patients should be screened for tetanus.
be instituted. In younger children, a spica cast can be used for 4 to 6
weeks; older cooperative children can be treated with hip abduction
orthosis, total hip precautions and gradually return to ambulation with
crutches.45,88,91
-
Reduce the hip urgently. The most
devastating outcome is AVN, and prolonged time to reduction (more than
6 hours) appears to be the greatest risk factor. In multitrauma
patients, this concept need to be expressed to the trauma team so that
it can be prioritized properly. -
Look for associated fractures and other
injuries. In older children, it is important to evaluate the posterior
rim of the acetabulum after posterior dislocation to rule out fracture.
Relying on plain radiographs and CT may underestimate the extent of
damage to the posterior wall of the acetabulum in children due to the
incomplete ossification of the pediatric bone. MRI may be required to
adequately assess the posterior wall of the acetabulum in children.86 -
Fractures at other sites in the femur
must be considered. It is important to obtain radiographs that show the
entire femur to rule out ipsilateral fracture. Careful evaluation of
the entire patient is needed especially for high-energy injuries that
result in a hip dislocation in older children and adults. -
Separation of the capital femoral
epiphysis and femoral neck fracture has been reported in association
with dislocation of the hip and the attempted reduction. Children in
their early teenage years, aged 12 to 16, should have their reduction
performed with fluoroscopy under general anesthesia when possible. This
strategy may avoid the possibility of displacing the proximal femoral
epiphysis (with attendant increased AVN risk) during attempted closed
reduction (Fig. 21-26). -
Spontaneous relocation of a dislocation
of the hip may occur with subsequent soft tissue or osteocartilaginous
interposition. Failure to appreciate the presence of hip dislocation
may lead to inadequate treatment. Traumatic hip subluxation may go
undetected or may be treated as a sprain or strain if the diagnosis is
not considered.69,81
After dislocation and spontaneous reduction, soft tissue may become
interposed in the hip joint potentially resulting chronic arthropathy.
In a child with posttraumatic hip pain without obvious deformity, the
possibility of dislocation-relocation must be considered. -
Always image the hip for evaluation of
interposed tissue after reduction. The incidence of widened joint space
after hip reductions is as high as 26%.106
After reduction, hemarthrosis may initially cause the hip joint to
appear slightly wider on the affected side, but this should decrease
after a few days. If the hip fails to appear concentric, the
possibility of interposed soft tissue must be considered and MRI or CT
scan should be performed.39,45,77,85,94 -
Long-term follow-up is important in
children who undergo hip dislocation. Injury to the triradiate
cartilage my cause acetabular dysplasia with growth. AVN, although
uncommon, may lead to early arthrosis, and this may not be identified
radiographically for several years. If there has been a significant
delay in time to reduction or the patient is otherwise at higher risk
for AVN, then consideration of a bone scan or MRI to evaluate for AVN
may be warranted, especially if early treatment with bisphosphonates is
considered.
 |
|
FIGURE 21-26 A. An 11-year-old boy dislocated his left hip while wrestling. B. The hip was easily reduced. C. After 5 months, hip pain led to an MRI, which shows ON of the capital femoral epiphysis. D. At 10 months after injury, there are typical changes of ON despite non-weight bearing.
|
If the force of hip dislocation is so strong as to disrupt the
obturator externus muscle, the posterior ascending vessels may be torn.72
In the rare case of dislocation with an intact capsule, increased
intracapsular pressure as a result of hemarthrosis may have a role in
developing AVN.85 The type of postreduction care has not been shown to influence the rate of AVN.
images detects AVN as an area of decreased uptake. Findings on
T2-weighted images are abnormal but of variable signal intensity. MRI
may be falsely negative if performed within a few days of injury80; conversely, many perfusion defects seen on MRI spontaneously resolve after several months.41,80
As treatment for early AVN develops this algorithm may change, and
early assessment maybe considered for those at high risk of AVN. If
hips are followed by serial radiographs for AVN, it is recommended that
they be studied for at least 2 years after dislocation, because
radiographic changes may appear late.10
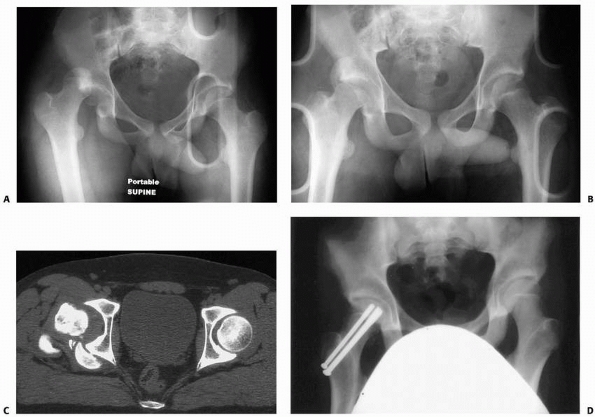 |
|
FIGURE 21-27 A. A 15-year-old male who was involved in a motor vehicle accident and sustained a right posterior hip dislocation. B.
After attempted closed reduction under conscious sedation in the emergency department. The proximal femoral epiphysis remains displaced posterior to the acetabulum while the neck is reduced into the acetabulum. C. A CT scan showing the posteriorly displaced proximal femoral epiphysis. D. Anterior posterior radiograph after open reduction and internal fixation of the proximal femur, with 3 cannulated screws. |
Priorities are to maintain mobility and containment of the femoral head
to maximize congruity after resolution. AVN in older children should be
treated as in adults and may require hip fusion, osteotomy, or
reconstruction. If identified early, medical treatment with
bisphosphonates or revascularization techniques, such as a vascularized
fibular bone graft, can be considered.1,92
by medical means, and treatment should be symptomatic.
Anti-inflammatory medicines and weight-relieving devices should be used
as needed. Hip joint distraction with a hinged external fixator may
improve range of motion and decrease pain.101 If the joint fails to reconstitute, fusion or reconstruction should be considered.
unrelated to trauma. Many factors may contribute to this ability,
including generalized ligamentous laxity, excessive anteversion of the
femur and acetabulum, and coxa valga. Initial management should include
counseling the child to cease the activity (with or without psychiatric
counseling) and observation. If episodes of dislocation persist,
permanent changes such as secondary capsular laxity or
osteocartilaginous deformation of the hip may occur. These changes may
lead to pain, residual subluxation, or degenerative joint disease.
Conservative treatment should be initially attempted and may include
simple observation with or without psychiatric counseling or
immobilization with cast or brace. Hip stabilization by surgical means
may be indicated for persistent painful episodes of hip despite
conservative treatment.55,95
Corrective surgery, if considered, should be performed only to correct
specific anatomic abnormality and may include capsular plication,
redirectional pelvic osteotomy, or osteotomy of the proximal femur.95
reduction of hip dislocations in children. In one study, 3 children
(all under 16 years of age) developed heterotopic ossification, one of
which required surgical excision.66
result in complete failure of closed reduction. Muscle, bone, articular
cartilage, and labrum have been implicated.19,36,39,45,81,94 CT arthrography or MRI provide information on obstacles to complete reduction and the direction of the initial dislocation.39,94 Open reduction generally is necessary to clear impeding tissues from the joint.19,39,45,75,81,94 Untreated nonconcentric reduction may lead to permanent degenerative arthropathy.77
incapacitating symptoms. Ambulation may even be possible. As a result,
treatment may be delayed or the diagnosis missed until shortening of
the limb and contracture are well established, making reduction
difficult. Nearly all patients with a delayed treatment of traumatic
hip dislocation develop AVN.7,56 Prolonged heavy traction may be considered as method to effect reduction.43
Failing success, preoperative traction, extensive soft tissue release,
or primary femoral shortening should be considered if open reduction is
required. Open reduction will likely be difficult and will not always
be successful. Even if the hip stays reduced, progressive arthropathy
may lead to a stiff and painful hip. The likelihood of a good result
decreases with the duration of dislocation.
femoral head after a posterior dislocation of the hip in 2% to 13% of
patients.31,88,91 If the hip is expediently reduced, nerve function returns spontaneously in most patients.31,45
If the sciatic palsy is present prior to reduction, the nerve does not
need to be explored unless open reduction is required for other
reasons. If sciatic nerve function is shown to be intact and is lost
during the reduction maneuver, the nerve should be explored to ensure
that it has not displaced into the joint. Other nerves around the hip
joint are rarely injured at dislocation. Treatment is generally
expectant unless laceration or incarceration is suspected; if so,
exploration is indicated.
occurs most frequently after posterior dislocation in children under 8
years of age7,38
or in children with known hyperlaxity (Down syndrome, Ehlers-Danlos
disease). The incidence of recurrence is estimated less than 3%.75
Recurrence can be quite disabling, and in the long-term may result in
damage to the articular surfaces as a result of shear damage to the
cartilaginous hip. Prolonged spica casting (at least 3 months) may be
effective.107 Surgical exploration with capsulorrhaphy can be performed if conservative treatment fails.7,38,105 Prior to hip reconstruction, arthrography is recommended to identify a capsular defect or redundancy.7
In older children, recurrent dislocation can occur as a result of a
bony defect in the posterior rim of the acetabulum similar to that in
adults and may require posterior acetabular reconstruction.
described after anterior hip dislocation in children, and this may
occur in 25% of patients.91 The hip
should be relocated as soon as possible to remove the offending
pressure from the femoral vessels. If relocation of the hip fails to
restore perfusion, immediate exploration of the femoral vessels is
indicated.
new surgical and medical treatments options for hip disorders. Although
most do not directly apply to the urgent reduction of hip dislocations,
they are applicable to the sequelae that occur. The use of
bisphosphonates and other medications that inhibit bone resorption is
an active area of research and may have direct affects on limiting
collapse of the femoral head if AVN occurs.1
This could soon change our paradigm for the evaluation of a hip after
reduction of a dislocation, and early MRI or bone scans may be
indicated.
as a result of necrosis or hip instability. Techniques to increase
vascularity, such as vascularized bone grafting, remain a controversial
method to improve the natural history. Hinged distraction across the
hip is now more commonly performed and much easier technically, given
the newer generation of external fixation devices designed just for
this purpose. Hinged distraction may play a role as a primary treatment
(i.e., for chondrolysis) or as an adjunct to other techniques.101
Hip arthroscopy is much more commonly performed and allows for a much
less invasive approach to removing loose bodies in the hip and
assessing and treating soft tissue injuries.15,54
Together, these new techniques offer future opportunities to decrease
the severity of known complications and potentially improve functional
outcomes. Time and follow-up will be required to determine if these
methods improve the natural history of these post traumatic sequelae.
S, Jain D, Joshi VR, et al. Efficacy of alendronate, a bisphosphonate,
in the treatment of AVN of the hip. A prospective open-label study.
Rheumatology (Oxford) 2005;44(3):352-359.
Yoe LE. A Suggested Improvement to the Allis’ Method of Reduction of
Posterior Dislocation of the Hip. Ann Surg 1940;112(1):127-9.
N, Wojcik AS. Traumatic separation of the upper femoral epiphysis in a
15-month-old girl: an unusual mechanism of injury. Injury
1995;26:695-696.
K, Trigui M, Gdoura F, et al. Traumatic hip dislocations in children.
Rev Chir Orthop Reparatrice Appar Mot 2008;94(1):19-25.
AE, Zorer G. Complications associated with surgically treated hip
fractures in children. J Pediatr Orthop B 2002;11:219-228.
AK, Spiegel DA, Shrestha S, et al. Open reduction for neglected
traumatic hip dislocation in children and adolescents. J Pediatr Orthop
2007;27(2):187-191.
A. Natural history of avascular necrosis following traumatic hip
dislocation in childhood: a review of 145 cases. Acta Orthop Scand
1982;53:815-820.
A. Traumatic hip dislocation in childhood. A report of 26 cases and
review of the literature. Acta Orthop Scand 1979;50:549-553.
D, Pankalla T, Böhm H, et al. Hip pain related to femoral neck stress
fracture in a 12-year-old boy performing intensive soccer playing
activities—a case report. Int J Sports Med 2003;24:593-596.
ST, Beaty JH. Pelvic and hip fractures. In: Rockwood CA Jr, Wilkins KE,
Beaty JH, eds. Fractures in Children, 4th ed. Philadelphia:
Lippincott-Raven; 1996: 1109-1193.
ST, Bourland WL. Fracture of the neck and intertrochanteric region of
the femur in children. J Bone Joint Surg Am 1977;59(4):431-443.
ST, Casillas M, Banta JV. Displaced femoral neck fractures at the
bone-screw interface after in situ fixation of slipped capital femoral
epiphysis. J Pediatr Orthop 1997;17(2):212-215.
JC, Tang N. Decompression and stable internal fixation of femoral neck
fractures in children can affect the outcome. J Pediatr Orthop
1999;19:338-343.
KA, Morcuende J, El-Khoury GY. Entrapment of the acetabular labrum
following reduction of traumatic hip dislocation in a child. Skeletal
Radiol 2004;33(12):728-731.
W. Coxa plana. A clinical and radiological investigation with
particular reference to the importance of the metaphyseal changes for
the final shape of the proximal part of the femur. Acta Orthop Scand
Suppl 1965;84:1-129.
KJ, Mulligan ME, Murphey MD, et al. Gas bubbles in the hip joint on CT:
an indication of recent dislocation. AJR Am J Roentgenol
1995;164(4):931-934. Comment in AJR Am J Roentgenol 1996;166:472-473.
JM, Wong KL, Yeh GL, et al. Displaced fractures of the hip in children.
Management by early operation and immobilization in a hip spica cast. J
Bone Joint Surg Br 2002;84:108-112.
E, Guille JT, Kumar SJ, et al. Transepiphyseal fractures of the neck of
the femur in very young children. J Pediatr Orthop 1992;12:164-168.
N, Ramseier LE, Exner GU. Undisplaced femoral neck fractures in
children have a high risk of secondary displacement. J Pediatr Orthop B
2006;15(2):131-133.
R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for
early osteoarthritis of the hip. Clin Orthop Relat Res 2003;417:112-120.
JM, Merrot T, Bergoin V, et al. X-ray transparency interpositions after
reduction of traumatic dislocations of the hip in children. Eur J
Pediatr Surg 1996;6:288-293.
A, Powell HDW. Traumatic dislocation of the hip in children. An
analysis of 47 patients. J Bone Joint Surg Br 1961;43:29-37.
CJ, Pietrobon R, Carothers JT, et al. Comprehensive morphologic
evaluation of the hip in patients with symptomatic labral tear. Clin
Orthop Relat Res 2006;453: 277-285.
RC, Shravat BP. Reduction of neglected traumatic dislocation of the hip
by heavy traction. J Bone Joint Surg Am 1977;59:249-251.
FS, Bann S, Hill RA, et al. Displaced stress fracture of the femoral
neck in an active amenorrhoeic adolescent. Br J Sports Med
1997;31:70-72.
CF. Appearance and fusion of ossification centers in the human
skeleton. AJR Am J Roentgenol Radium Ther Nucl Med 1962;88:476-482.
JA, Price CT, Reuss BL, et al. Proximal femoral epiphysiolysis during
reduction of hip dislocation in adolescents. J Pediatr Orthop
2006;26(3):371-374.
LO, Beaty JH. Current concepts review: fractures of the head and neck
of the femur in children. J Bone Joint Surg Am 1994;76:283-292.
JV, Smith DK, Aufdemorte TB, et al. Anatomic significance of magnetic
resonance imaging findings in hip fracture. Clin Orthop Relat Res
1996;332:209-214.
R, Karlsson J. Outcome after transphyseal hip fractures. Four children
followed 34 to 48 years. Acta Orthop Scand 1997;68:235-238.
B, Mulpuri K. Delayed separation of the capital femoral epiphysis after
an ipsilateral transcervical fracture of the femoral neck. J Orthop
Trauma 2000;14(6): 446-448.
N, Suzuki S, Seto Y. Arthroscopic treatment for traumatic hip
dislocation with avulsion fracture of the ligamentum teres. Arthroscopy
2001;17(1):67-69.
JM, Papavasiliou KA, Kyrkos MJ, et al. Multidirectional habitual
bilateral hip dislocation in a patient with Down syndrome. Clin Orthop
Relat Res 2005;(435): 263-266.
M, Ward K, Brown RR, Muns CF, Cowell CT, Little DG. Intravenous
bisphosphonate therapy for traumatic osteonecrosis of the femoral head
in adolescents. J Bone Joint Surg Am 2007;89(8):1727-34.
S, Kita A, Fujii G, et al. Avascular necrosis associated with fractures
of the femoral neck in children: histological evaluation of core
biopsies of the femoral head. Injury 2003;34:283-286.
NK, Singh R, Sharma AK, et al. Modified Pauwels intertrochanteric
osteotomy in neglected femoral neck fractures in children: a report of
10 cases followed for a minimum of 5 years. J Orthop Trauma
2007;21(4):237-243.
NK, Singh R, Sharma A, et al. Treatment of pathologic femoral neck
fractures with modified Pauwel osteotomy. Clin Orthop Relat Res
2005;437:229-235.
JI, Barrios C, Gomar-Sancho F. Intracapsular hip pressure after femoral
neck fracture. Clin Orthop Relat Res 1997;340:172-180.
T. Fractures of the neck of the femur in children: an experience at the
Aseer Central Hospital, Abha, Saudi Arabia. Injury Int J Care Injured
2002;33:823-827.
ES, Mehlman CT. Risk factors for avascular necrosis after femoral neck
fractures in children: 25 Cincinnati cases and meta-analysis of 360
cases. J Orthop Trauma 2006;20(5):323-329.
CT 3rd, Warren RF, Hershman EB, et al. Traumatic posterior hip
subluxation in American football. J Bone Joint Surg Am
2003;85:1190-1196.
GP, Cole WG. Effect of early hip decompression on the frequency of
avascular necrosis in children with fractures of the neck of the femur.
Injury 1996;27:419-421.
HP, Siebenrock KA, Hempfing A, et al. Perfusion of the femoral head
during surgical dislocation of the hip. Monitoring by laser Doppler
flowmetry. J Bone Joint Surg Br 2002;84:300-304.
HP, Wyss TF, Stoecklin CH, et al. The contour of the femoral head-neck
junction as a predictor for the risk of anterior impingement. J Bone
Joint Surg Br 2002;84(4): 556-560
T, Glorion C, Pannier S, et al. Traumatic dislocation of the hip with
separation of the capital epiphysis: 5 adolescent patients with 3 to 9
years of follow-up. Acta Orthop Scand 2003;74(1):49-52
O, Landin LA, Johansson A. Traumatic hip dislocation with spontaneous
reduction and capsular interposition. Acta Orthop Scand 1994;65:476-479.
H, Krettek C, Friedrich A, et al. Long-term outcome in children with
fractures of the proximal femur after high-energy trauma. J Trauma
1999;46:58-64.
JJ, Callaghan JJ, Spritzer CE, et al. Changes on magnetic resonance
images after traumatic hip dislocation. Clin Orthop Relat Res
1995;319:249-259.
CT, Pyevich MT, Knapp DR, et al. Traumatic hip dislocation with
spontaneous incomplete reduction: a diagnostic trap. J Orthop Trauma
2002;16:730-735.
M, Ward K, Brown RR, et al. Intravenous biphosphonate therapy for
traumatic osteonecrosis of the femoral head in adolescents. J Bone
Joint Surg Am 2007; 89:1727-1734.
H, Pennig D, Klein W, et al. Traumatic dislocation of the hip in young
children. Arch Orthop Trauma Surg 1991;110:114-117.
IF, Kloen P, Potter HG, et al. MRI assessment of the posterior
acetabular wall fracture in traumatic dislocation of the hip in
children. Pediatr Radiol 2002;32: 435-439.
GL, Sciulli R, Altman GT. Knee injury inpatients experiencing a
high-energy traumatic ipsilateral hip dislocation. J Bone Joint Surg Am
2005:87:1200-1204.
Research Committee of the Pennsylvania Orthopaedic Society. Traumatic
dislocation of the hip in children. Final report. J Bone Joint Surg Am
1968;50:79-88.
SP, Aaron RK, Urbaniak JR. Survival analysis of hips treated with core
decompression or vascularized fibular grafting because of avascular
necrosis. J Bone Joint Surg Am 1998;80(9):1270-1275.
M, Karapinar H, Kazimoglu C, et al. Fracture dislocation of sacroiliac
joint associated with triradiate cartilage injury in a child: a case
report. J Pediatr Orthop Br 2008; 17(2):65-68.
KP, Kalamachi A, Thompson GH. Acetabular epiphysis-labrum entrapment
following traumatic anterior dislocation of the hip in children. J
Pediatr Orthop 1986;6: 215-219.
KS, Choi IH, Sohn YJ, et al. Habitual dislocation of the hip in
children: a report of eight additional cases and literature review. J
Pediatr Orthop 2003;23:178-183.
KS, Kim YS, Sohn SW, et al. Arthrotomy and open reduction of the
displaced fracture of the femoral neck in children. J Ped Orthop Br
2001;10:205-210.
R, Johnson LH, Johnson RA. Variations in the intra-articular pressure
of the hip joint in injury and disease. J Bone Joint Surg Am
1964;46:509-516.
Pierre P, Staheli LT, Smith JB, et al. Femoral neck stress fractures in
children and adolescents. J Pediatr Orthop 1995;15:470-473.
MM, Feldman DS, Madan SS, et al. Hinged distraction of the adolescent
arthritic hip. J Pediatr Orthop 2005;25(2):178-182.
E, Bayram H, Gulsen M, et al. Fractures of the femoral neck in
children: long-term follow-up in 62 hip fractures. Injury
2005;36:123-130.
R, Pannier S, Odent T, et al. Imaging of traumatic dislocation of the
hip in childhood. Pediatr Radiol 2004;34(12):970-979.
ME, Pappas AM. Unusual complications in traumatic dislocation of the
hip in children. J Pediatr Orthop 1985;5:534-539.
