Femur
Editors: Morrey, Bernard F.; Morrey, Matthew C.
Title: Master Techniques in Orthopaedic Surgery: Relevant Surgical Exposures, 1st Edition
Copyright ©2008 Lippincott Williams & Wilkins
> Table of Contents > Section II – Lower Extremity > 8 – Femur
8
Femur
Joseph R. Cass
ANTEROMEDIAL APPROACH TO THE FEMUR
Indications
Situations in which combined exposure of the knee and
femoral shaft is necessary, such as for the placement of large revision
knee arthroplasty components.
femoral shaft is necessary, such as for the placement of large revision
knee arthroplasty components.
Extension
The exposure can be extended distally to complete a
medial parapatellar approach to the knee. Proximal extension is limited
by the femoral artery crossing the wound.
medial parapatellar approach to the knee. Proximal extension is limited
by the femoral artery crossing the wound.
Anatomy
The anteromedial approach is distant from any important
neurovascular structures and it involves a transmuscular plane to the
femur. This approach to the femur is performed between the vastus
medialis and rectus femoris in the superficial layer and involves
splitting the vastus intermedius in the deep layer to access the femur.
neurovascular structures and it involves a transmuscular plane to the
femur. This approach to the femur is performed between the vastus
medialis and rectus femoris in the superficial layer and involves
splitting the vastus intermedius in the deep layer to access the femur.
Technique
-
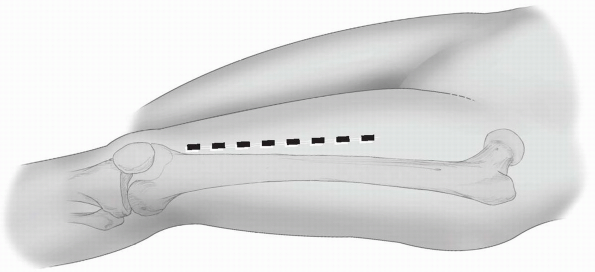
Incision: if it is possible to determine
the location of the medial border of the vastus medialis the incision
should follow this contour, extending proximally from a point just
proximal and medial to the superomedial pole of the patella. If the
vastus medialis contour is unable to be determined, the incision should
be carried in a longitudinal fashion from a point medial and proximal
to the superomedial pole of the patella (Fig. 8-1). -
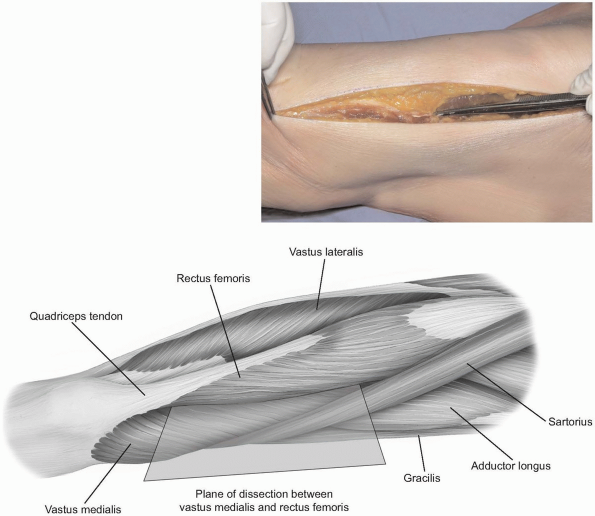
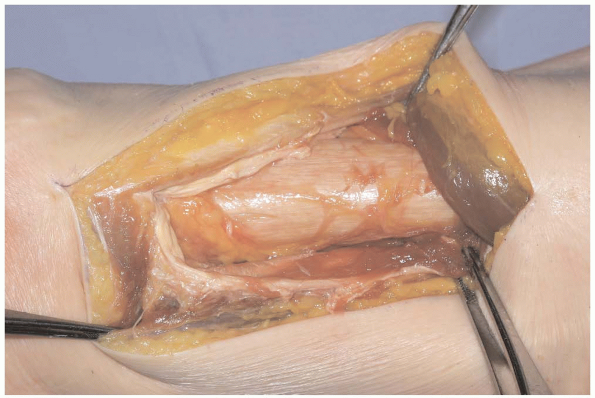
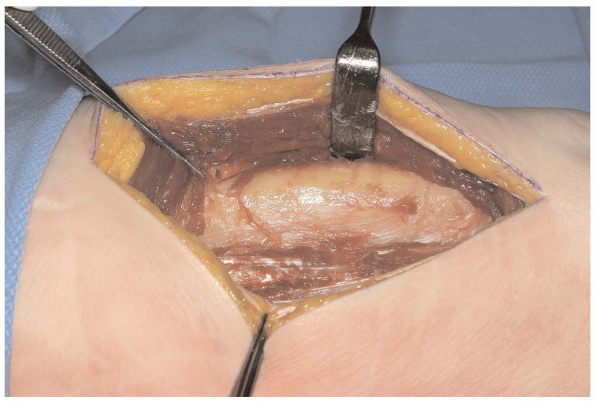
The deep fascia of the thigh is incised in line with the skin incision and flaps are elevated medially and laterally (Fig. 8-2). The interval between the vastus medialis and rectus femoris is identified and is developed with blunt dissection proximally.
-
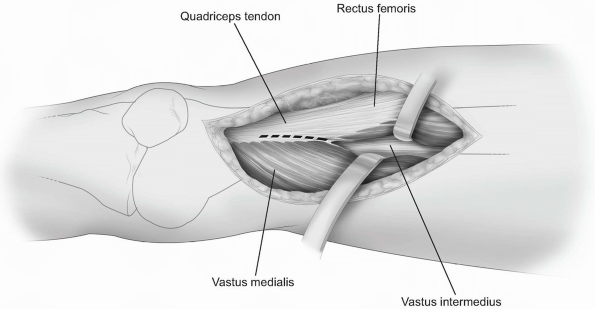
As this interval is continued distally,
the quadriceps tendon is incised close to its medial border, leaving
adequate amount of tendon medially and laterally for later closure (Fig. 8-3). -
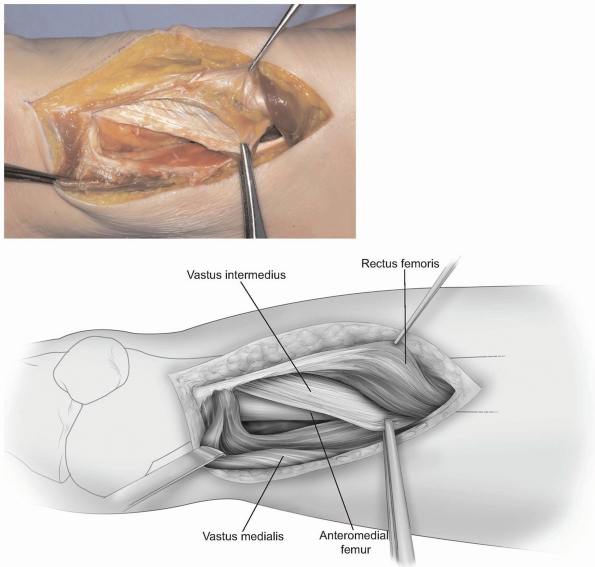
Deep to the vastus medialis and rectus femoris, the vastus intermedius is split in line with its fibers (Fig. 8-4).
-
Subperiosteal dissection along the femoral shaft elevates the vastus intermedius off the femur (Fig. 8-5).
Retraction of the vastus medialis in the lateral and medial direction
allows complete exposure of the anterior aspect of the distal femur.
P.176
 |
|
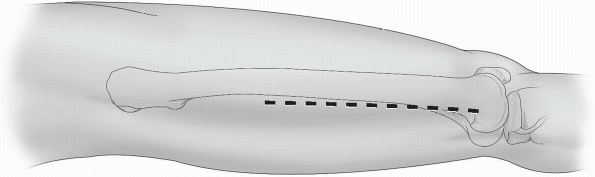
FIGURE
8-1 The skin incision typically extends proximally as needed from a point just medial and superior to the superomedial aspect of the patella. |
Closure
Muscle reapproximation of the vastus intermedius is not
possible. Closure consists of first repairing the incision in the
quadriceps tendon, followed by reapproximating the deep fascia.
possible. Closure consists of first repairing the incision in the
quadriceps tendon, followed by reapproximating the deep fascia.
 |
|
FIGURE
8-2 The deep fascia of the thigh is split to expose the interval between the vastus medialis and rectus femoris. Distally, the muscles join to form the quadriceps tendon. |
P.177
 |
|
FIGURE
8-3 The interval between the vastus medialis and rectus femoris is developed with blunt dissection. Distally, the quadriceps tendon may need to be split in order to access the distal femur and articular surface. |
 |
|
FIGURE 8-4 The vastus intermedius is deep to the interval developed.
|
P.178
 |
|
FIGURE 8-5 Subperiosteal dissection of the vastus intermedius medially and laterally allows exposure of the anterior femur.
|
ANTEROLATERAL APPROACH TO THE FEMUR
Indications
Fractures, bone grafting, total femoral replacement, and extensor mechanism repair.
Extension
The exposure can be extended proximally to expose the
hip joint and distally to expose the knee joint through a lateral
parapatellar approach.
hip joint and distally to expose the knee joint through a lateral
parapatellar approach.
Anatomy
The interval between the rectus femoris and vastus
lateralis is developed in order to expose the vastus intermedius. The
approach involves splitting the fibers of the vastus intermedius to
access the femoral shaft. The descending branch of the lateral femoral
circumflex artery crosses the plane between the rectus femoris and the
vastus lateralis in the proximal thigh. The artery enters the vastus
lateralis along with the motor branch of the nerve to the vastus
lateralis and should be preserved as it enters the vastus lateralis. A
branch of the vessel continues along the medial side of the vastus
lateralis to join the arterial anastomosis around the knee.
lateralis is developed in order to expose the vastus intermedius. The
approach involves splitting the fibers of the vastus intermedius to
access the femoral shaft. The descending branch of the lateral femoral
circumflex artery crosses the plane between the rectus femoris and the
vastus lateralis in the proximal thigh. The artery enters the vastus
lateralis along with the motor branch of the nerve to the vastus
lateralis and should be preserved as it enters the vastus lateralis. A
branch of the vessel continues along the medial side of the vastus
lateralis to join the arterial anastomosis around the knee.
Technique
-
Incision: the incision is made along a
line from the anterior-superior iliac spine to the lateral aspect of
the patella. The length of the incision is determined by the pathology
being addressed. The skin and subcutaneous tissue are incised in the
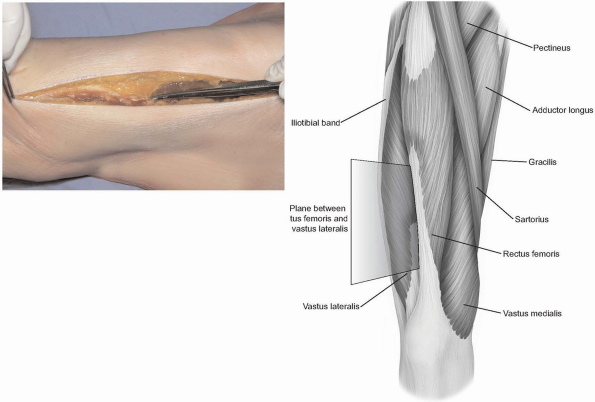
line described (Fig. 8-6) to expose the deep fascia of the thigh. -
The fascia is split in line with the skin
incision and the interval between the rectus femoris and vastus
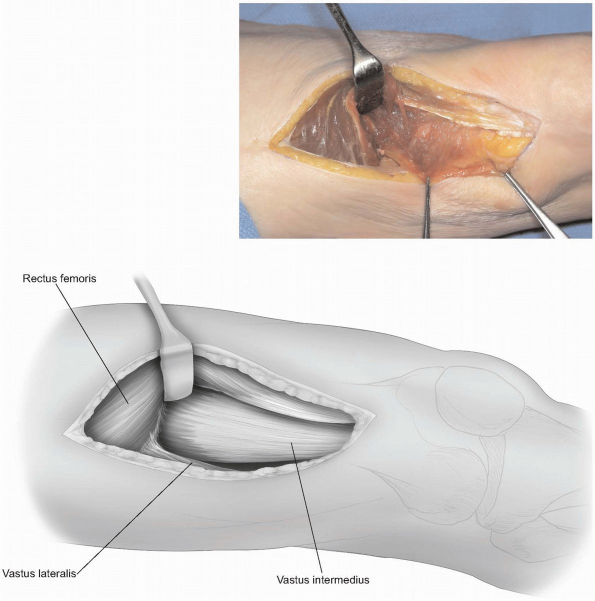
lateralis is identified (Fig. 8-7). -
This interval is easily developed in the
middle of the thigh. In the distal thigh, the muscles are adherent,
connected by an aponeurotic sheet of tissue. This connection will need
to be split in order to access the vastus intermedius in the distal
thigh (Fig. 8-8).
Proximally, care should be taken in order to prevent injury to the
descending branch of the lateral femoral circumflex artery and motor
nerve to the vastus lateralis as they cross from the rectus femoris to
the vastus lateralis together. -
The vastus intermedius muscle belly is
split in line with its fibers to expose the anterior femoral shaft.
Subperiosteal dissection medially and laterally to elevate the vastus
intermedius will further expose the anterior aspect of the femur (Fig. 8-9).
P.179
 |
|
FIGURE
8-6 The skin incision is made along a line connecting the anterior-superior iliac spine and the lateral edge of the patella. The location of the incision along this line depends on the region of the femur that needs to be exposed. |
 |
|
FIGURE
8-7 The deep fascia of the thigh is split in line with the skin incision and the rectus femoris and vastus lateralis muscles are identified. |
Closure
Muscle reapproximation of the vastus intermedius is not
possible. Closure consists of reapproximating the deep fascia followed
by routine subcutaneous tissue and skin closures.
possible. Closure consists of reapproximating the deep fascia followed
by routine subcutaneous tissue and skin closures.
POSTEROLATERAL APPROACH TO THE FEMUR
Indications
Reduction and internal fixation of femoral shaft
fractures, subtrochanteric and intertrochanteric fractures, and biopsy
and treatment of bone tumors.
fractures, subtrochanteric and intertrochanteric fractures, and biopsy
and treatment of bone tumors.
Extension
The posterolateral approach to the femur can be extended
proximally and combined with multiple hip exposures to expose the
proximal femur. Distally, the exposure is easily extended to a lateral
parapatellar approach to the knee joint.
proximally and combined with multiple hip exposures to expose the
proximal femur. Distally, the exposure is easily extended to a lateral
parapatellar approach to the knee joint.
P.180
 |
|
FIGURE
8-8 In the proximal thigh, the plane between the rectus femoris and vastus lateralis is easily developed. It is recommended to begin developing the interval proximally and then working in a distal direction. Distally, the muscles are adherent and separation requires sharp dissection. Once divided, the vastus intermedius is visible. |
 |
|
FIGURE
8-9 The vastus intermedius has been split along the anterior aspect of the femur in line with its fibers. Subperiosteal dissection medially and laterally allows elevation of the vastus intermedius and exposure of the anterior femur. |
P.181
 |
|
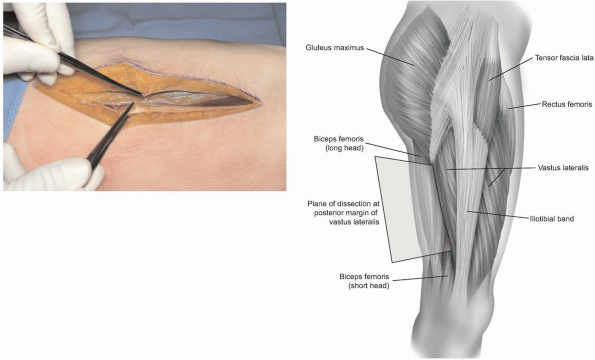
FIGURE
8-10 The skin incision is located along a line from the posterior edge of the greater trochanter to the posterior aspect of the lateral femoral condyle, parallel to the femoral shaft. |
Anatomy
The posterolateral approach to the femur utilizes the
plane between the vastus lateralis and the posterior intermuscular
septum. There are no important nerves at risk in this exposure.
Perforating vessels which pierce the lateral intermuscular septum are
at risk during this approach and need to be ligated in order to access
the femoral shaft.
plane between the vastus lateralis and the posterior intermuscular
septum. There are no important nerves at risk in this exposure.
Perforating vessels which pierce the lateral intermuscular septum are
at risk during this approach and need to be ligated in order to access
the femoral shaft.
Positioning
The patient is placed in the supine position with a sandbag under the ipsilateral hip.
Technique
-
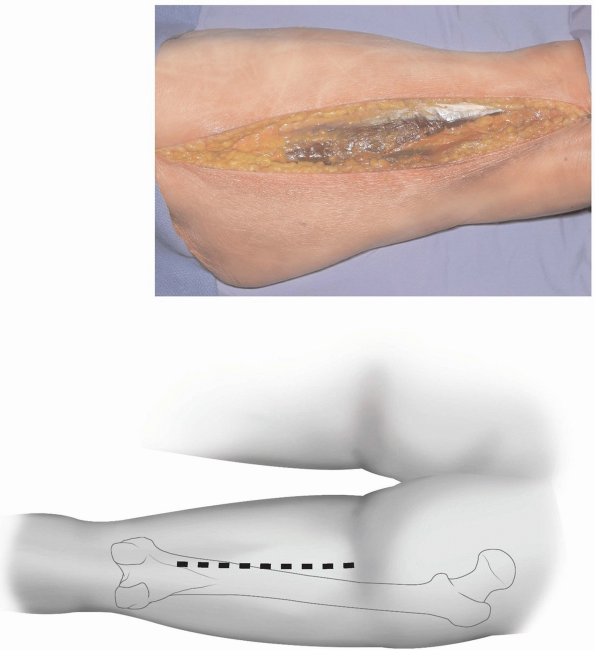
Incision: the incision is parallel to the
femoral shaft on a line from the posterior aspect of the greater
trochanter to the posterior edge of the lateral femoral condyle (Fig. 8-10).
Depending on the part of the femur that needs exposure, the location of
the incision can be adjusted proximally and distally along this line.
The subcutaneous tissue and fat are dissected in line with the skin
incision towards the fascia lata and posterolateral aspect of the
femoral shaft. -
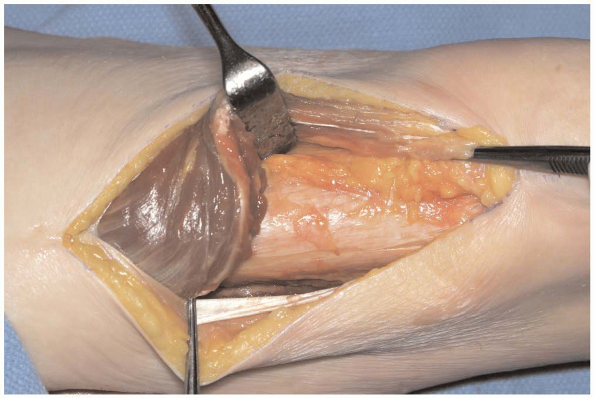
The fascia lata is split in line with its
fibers along the posterolateral aspect of the femur. This will allow
for exposure of the posterior margin of the vastus lateralis (Fig. 8-11). -
The femoral shaft should be palpated through the fascia lata prior to splitting the fascia lata.
-
Note:
Opening the fascia lata too anteriorly will cause difficulty in
dissection of the vastus lateralis posteriorly to the linea aspera.
Separating the fascia lata proximally will require splitting the tensor
fascia lata in line with its muscle fibers.
-
-
The fascia over the vastus lateralis is
exposed beneath the fascia lata and incised in line with the fibers
close to the lateral intermuscular septum. Blunt dissection using
elevators allows separation of the vastus lateralis muscle from the
fascia and lateral intermuscular septum towards the linea aspera (Fig. 8-12).
Elevation of the muscle fibers is accomplished with distal to proximal
elevation to elevate the fibers as they originate from the femur and
intermuscular septum. -
As the linea aspera is approached, the
perforating vessels are encountered. Careful blunt dissection along the
interval between the muscle and lateral intermuscular septum will
expose the vessels as they perforate the lateral intermuscular septum,
allowing them to be carefully ligated (Fig. 8-13).-
Pearl:
Proper control of the perforators cannot be overstated. Inadvertent
transaction may result in retraction of the vessels, making hemostasis
problematic.
-
-
Subperiosteal elevation anteriorly along
the femur will allow retractor placement over the anterior aspect of
the femur for exposure and anterior retraction of the entire vastus
lateralis (Fig. 8-14).
Closure
The muscle belly of the vastus lateralis is allowed to
fall posteriorly against the lateral intermuscular septum. Repair of
the fascia of the vastus literalist is performed next, followed by the
closure of the fascia lata. Separation of the fascia lata in a line
more anteriorly than the vastus lateralis fascia will allow the vastus
lateralis fascia and fascia lata closure to be in separate, overlapping
layers.
fall posteriorly against the lateral intermuscular septum. Repair of
the fascia of the vastus literalist is performed next, followed by the
closure of the fascia lata. Separation of the fascia lata in a line
more anteriorly than the vastus lateralis fascia will allow the vastus
lateralis fascia and fascia lata closure to be in separate, overlapping
layers.
P.182
 |
|
FIGURE
8-11 The fascia lata has been split in line with its fibers along the posterolateral border of the femur, exposing the fascia over the vastus lateralis deep in the wound. The interval formed by the posterior margin can then be elevated to gain access to the posterolateral femur. |
 |
|
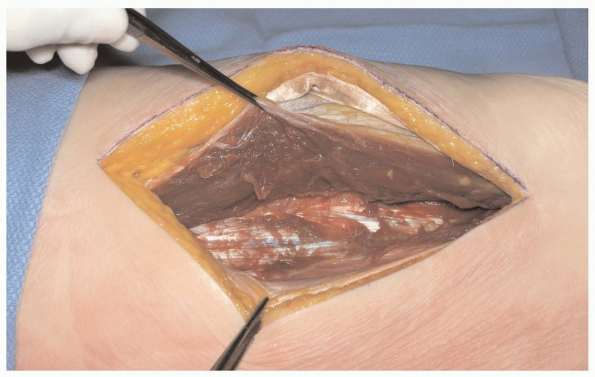
FIGURE
8-12 The posterior margin of the vastus lateralis has been elevated from its insertion on the lateral intermuscular septum. The fibers of the vastus lateralis are separated from the lateral intermuscular septum using an elevator in the distal to proximal direction, in order to elevate all the fibers as a unit and not separate the muscle fibers. |
 |
|
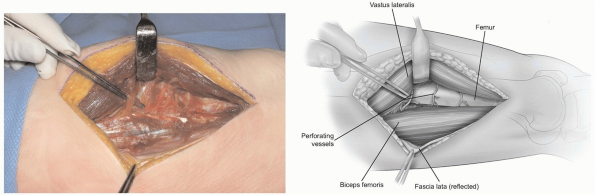
FIGURE
8-13 Perforating and crossing vessels should be identified as they emerge between the bone and intermuscular septum. These vessels are ligated to allow subperiosteal dissection toward the linea aspera for exposure of the lateral femur. |
P.183
 |
|
FIGURE 8-14 Retractors placed over the femur will retract the vastus lateralis anteriorly in order to expose the femur.
|
POSTERIOR APPROACH TO THE FEMUR
Indications
The direct posterior approach to the femur is rarely
used. It can be used to access the femoral shaft for posterior bone
grafting of nonunions.
used. It can be used to access the femoral shaft for posterior bone
grafting of nonunions.
Anatomy
Understanding the position of the sciatic nerve as is
passes through the posterior thigh is paramount in performing the
posterior approach successfully. In the proximal thigh, the posterior
approach requires dissection lateral to the long and short heads of the
biceps femoris, with the sciatic nerve retracted medially and protected
by the two heads of the biceps femoris. When the exposure is performed
in the distal aspect of the thigh, the dissection is carried medial to
the long and short heads of the biceps femoris and the sciatic nerve is
retracted laterally and again protected by the two heads of the biceps
femoris.
passes through the posterior thigh is paramount in performing the
posterior approach successfully. In the proximal thigh, the posterior
approach requires dissection lateral to the long and short heads of the
biceps femoris, with the sciatic nerve retracted medially and protected
by the two heads of the biceps femoris. When the exposure is performed
in the distal aspect of the thigh, the dissection is carried medial to
the long and short heads of the biceps femoris and the sciatic nerve is
retracted laterally and again protected by the two heads of the biceps
femoris.
Technique
-
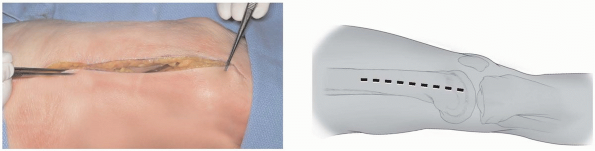
Incision: the skin incision is centered
over the posterior aspect of the femur and is directed longitudinally,
beginning at the gluteal fold and extending to the popliteal crease (Fig. 8-15). The subcutaneous tissue beneath the skin is dissected in line with the skin incision to the deep fascia of the thigh. -
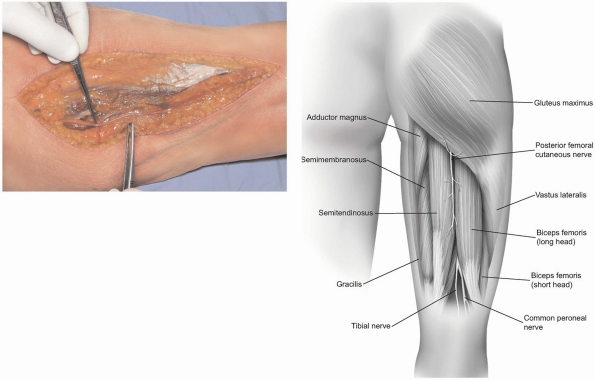
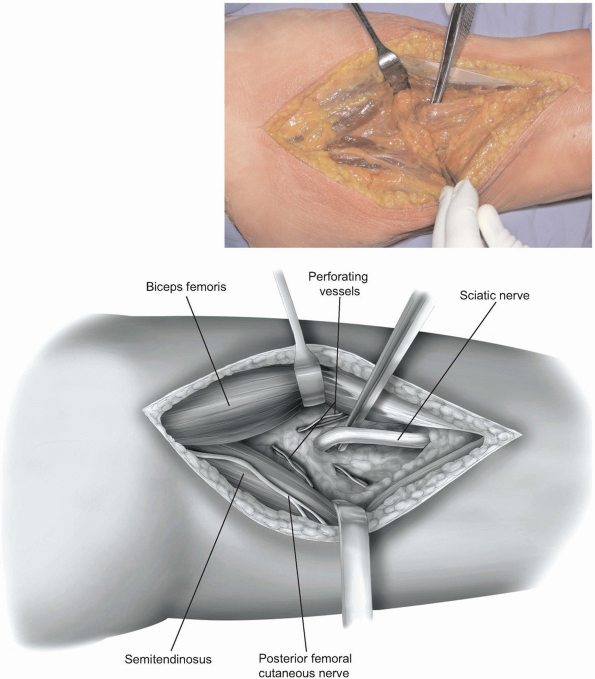
The deep fascia of the thigh is split
longitudinally to expose the long head of the biceps femoris. The
posterior femoral cutaneous nerve of the thigh lies in the groove
between the long head of the biceps and the semitendinosus (Fig. 8-16). Care must be taken when opening the deep fascia as the posterior femoral cutaneous nerve lies just beneath the fascia. -
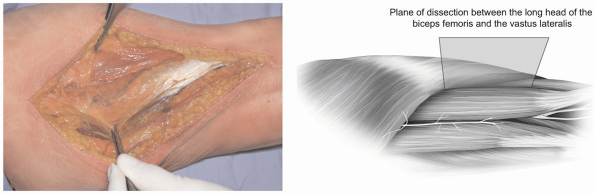
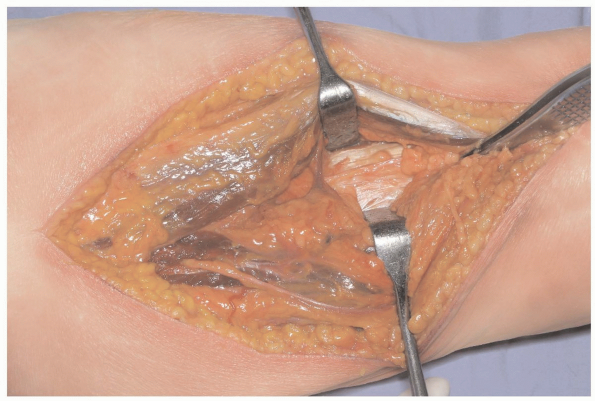
In the proximal thigh, the dissection is
carried into the interval between the long head of the biceps femoris
and the vastus lateralis (Fig. 8-17). The long head of the biceps femoris is retracted medially to expose the short head. -
At this deeper level, the interval
between the short head of the biceps femoris and the vastus lateralis
is developed to access the linea aspera of the femoral shaft.
Perforating and crossing vessels near the linea aspera should be
identified and ligated as the short head of the biceps femoris is
retracted medially (Fig. 8-18).
The sciatic nerve will be protected by the medial retraction of the
long and short heads of the biceps femoris. Subperiosteal dissection of
the short head of the biceps off the posterior femur will allow
placement of retractors medially and laterally along the femoral shaft. -
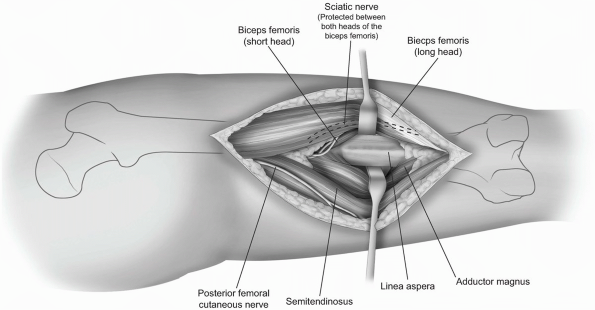
If access to the posterior aspect of the
distal femoral shaft is necessary, the deep fascia is again split in
the longitudinal direction and the long head of the biceps femoris
P.184
is again identified (Fig. 8-19).
The dissection is then carried in the interval between the two heads of
the biceps femoris laterally and the semitendinosus and semimembranosus
medially. The sciatic nerve is lateral to the plane of dissection,
surrounded by fatty tissue. -
Lateral retraction of the biceps femoris and sciatic nerve allows exposure of the linea aspera (Fig. 8-20).
-
Subperiosteal dissection along the linea
aspera medially results in the elevation of the adductor magnus, while
lateral subperiosteal elevation lifts the short head of the biceps off
the femur to expose the femoral shaft (Fig. 8-21).
 |
|
FIGURE
8-15 The skin incision is centered over the posterior aspect of the femur and may be extended from the gluteal fold to the popliteal crease. |
 |
|
FIGURE
8-16 The deep fascia of the thigh is split to expose the long head of the biceps femoris. The posterior femoral cutaneous nerve of the thigh lies just deep to the deep fascia and should be preserved. |
P.185
 |
|
FIGURE
8-17 In the proximal thigh, the plane between the long head of the biceps femoris and the vastus lateralis is developed, exposing the short head of the biceps femoris. Dissection should be carried out lateral to the short head of the biceps femoris. |
Closure
Closure of this approach requires only reapproximation
of the deep fascia of the thigh followed by routine closure of the
subcutaneous tissue and skin.
of the deep fascia of the thigh followed by routine closure of the
subcutaneous tissue and skin.
 |
|
FIGURE
8-18 Perforating and crossing vessels should be ligated to allow subperiosteal dissection along the linea aspera for exposure of the posterior femur. |
P.186
 |
|
FIGURE
8-19 In the distal thigh, the plane of dissection is between the biceps femoris laterally and the semitendinosus and semimembranosus medially. Care should be taken to identify the sciatic nerve which is encountered between the biceps and semitendinosus. |
P.187
 |
|
FIGURE
8-20 The plane between the long head of the biceps and hamstrings is developed and the long head is retracted laterally to expose the short head of the biceps femoris. |
 |
|
FIGURE
8-21 The short head of the biceps femoris is retracted laterally and the semimembranosus and semitendinosus are retracted medially to expose the femur. Subperiosteal dissection along the posterior shaft of the femur allows retraction of these muscle groups as well as the adductor magnus. The sciatic nerve is retracted laterally, protected by the two heads of the biceps femoris. |
P.188
MEDIAL APPROACH TO THE FEMUR
Indications
For internal fixation of distal femoral fractures
requiring medial buttress plating, supracondylar osteotomies, and
resection of benign tumors of the femur.
requiring medial buttress plating, supracondylar osteotomies, and
resection of benign tumors of the femur.
Extension
Proximally, extension of this approach is limited by the
femoral artery crossing from anterior to posterior. Distally, the
exposure can be extended to combine with a medial subvastus approach to
the knee.
femoral artery crossing from anterior to posterior. Distally, the
exposure can be extended to combine with a medial subvastus approach to
the knee.
Anatomy
The interval utilized is between the vastus medialis and
the medial intermuscular septum. The saphenous nerve crosses from
anterior to posterior, entering and exiting the sartorius as it passes
distally in the leg. The femoral vessels cross from anterior to
posterior through the hiatus in the adductor magnus tendon. The medial
superior genicular artery and the articular branch of the descending
genicular artery cross deep in the wound on the surface of the medial
femur.
the medial intermuscular septum. The saphenous nerve crosses from
anterior to posterior, entering and exiting the sartorius as it passes
distally in the leg. The femoral vessels cross from anterior to
posterior through the hiatus in the adductor magnus tendon. The medial
superior genicular artery and the articular branch of the descending
genicular artery cross deep in the wound on the surface of the medial
femur.
Technique
-
Incision: the skin incision is parallel
to the femoral shaft, located midway between the posterior border of
the medial femoral condyle and the medial aspect of the patella, near
the adductor tubercle. It can be extended proximally 10 to 13 cm from
the knee joint, limited by the location of the femoral artery crossing
the wound (Fig. 8-22). -
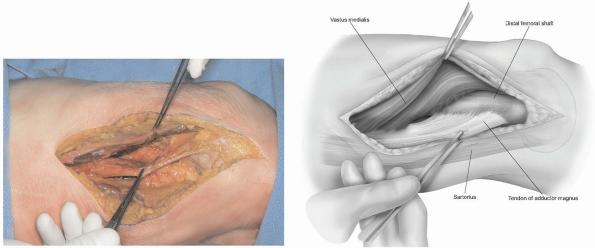
The deep fascia of the thigh is split in
line with the skin incision. The adductor magnus tendon and the vastus
medialis muscle belly are identified, as the dissection will continue
in the plane between these two structures. The saphenous nerve should
be identified and retracted posteriorly in the wound (Fig. 8-23). -
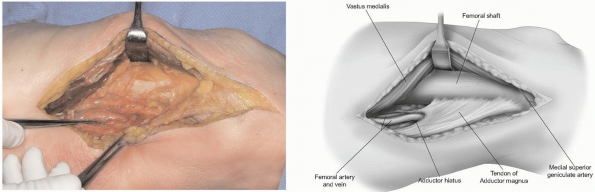
The muscle fibers of the vastus medialis
are elevated off the medial intermuscular septum from distal to
proximal. Blunt elevation of these fibers will allow identification of
the perforating arteries so ligation can be completed (Fig. 8-24). -
As the femur is approached, the muscular branch of the descending genicular artery is encountered and ligation can be performed (Fig. 8-25).
-
Subperiosteal dissection along the medial
and anterior femur allows retraction of the vastus medialis anteriorly,
exposing the distal femoral shaft.
 |
|
FIGURE
8-22 The skin incision is made over the adductor tubercle, at a point halfway between the medial border of the patella and the posterior aspect of the medial femoral condyle. The incision is made parallel to the femur and may extend 10 to 13 cm proximally from the knee joint. |
P.189
 |
|
FIGURE
8-23 The deep fascia of the thigh is split in line with the skin incision and the interval between the vastus medialis and adductor magnus is identified. The saphenous nerve is identified crossing from anterior to posterior in the wound and retracted posteriorly. |
 |
|
FIGURE
8-24 The muscle fibers of the vastus medialis are elevated off the medial intermuscular septum. Using an elevator, the muscle can be teased off the septum with distal to proximal strokes of the elevator to minimize damage to the muscle. |
 |
|
FIGURE
8-25 Subperiosteal dissection along the femur allows anterior retraction of the vastus medialis to expose the femur. Note femoral vessels as it enters adductor hiatus. |
P.190
RECOMMENDED READING
Chapman MW, Finkemeier CG. Treatment of supracondylar nonunions of the femur with plate fixation and bone graft. J Bone Joint Surg Am 1999;81(9):1217-1228.
Checroun AJ, Mekhail AO, Ebraheim NA, et al. Extensile medial approach to the femur. J Orthop Trauma 1996;10(7):481-486.
Della Valle CJ, Berger RA, Rosenberg AG. Surgical exposures in revision total knee arthroplasty. Clin Orthop Relat Res 2006;446:59-68.
Kregor
PJ. Distal femur fractures with complex articular involvement:
management by articular exposure and submuscular fixation. Orthop Clin North Am 2002;33(1):153-175, ix.
PJ. Distal femur fractures with complex articular involvement:
management by articular exposure and submuscular fixation. Orthop Clin North Am 2002;33(1):153-175, ix.
O’Beirne J, O’Connell RJ, White JM, et al. Fractures of the femur treated by femoral plating using the anterolateral approach. Injury 1986;17(6):387-390.
Wang
JW, Weng LH. Treatment of distal femoral nonunion with internal
fixation, cortical allograft struts, and autogenous bone-grafting. J Bone Joint Surg Am 2003;85A(3):436-440.
JW, Weng LH. Treatment of distal femoral nonunion with internal
fixation, cortical allograft struts, and autogenous bone-grafting. J Bone Joint Surg Am 2003;85A(3):436-440.
