Dupuytren Contracture
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Dupuytren Contracture
Dupuytren Contracture
Darryl B. Thomas MD
Dawn M. LaPorte MD
Description
-
Dupuytren contracture is a proliferative
disorder of subcutaneous palmar fibrous tissue (fascia) that occurs in
the form of nodules and cords and results in contractures of the finger
joints (Fig. 1). -
It occurs typically in men in the 5th to 7th decades.
-
Younger patients are more likely to have rapid progression of disease with poorer long-term results and frequent recurrences.
-
Aggressive, early onset is seen in a subgroup of patients with Dupuytren diathesis.
-
Synonym: Dupuytren disease
Epidemiology
Incidence
-
Greatest in Northern Europe and in immigrants of Celtic origin
-
Incidence in the United States is 2–3% that of the general population.
-
Hand dominance not a factor
-
More frequent and severe in patients with diabetes
-
Increased incidence in patients with epilepsy and chronic obstructive pulmonary disease
-
Possible link to alcoholism and tobacco is controversial (1,2).
-
More common in males than in females (2:1–10:1)
-
In females, usually later onset and less severe disease
Risk Factors
-
Caucasian
-
Northern European descent
-
Increased age
-
Family history
 Fig.
Fig.
1. Dupuytren contracture most commonly involves the ring and small
fingers and produces cordlike tightening over the flexion tendon.
Genetics
-
The disorder is autosomal dominant with variable penetrance.
-
Only 10% of patients with Dupuytren contractures have a positive family history.
Etiology
-
Unknown
-
Strong evidence for hereditary factors, possibly through transmission of defective genes responsible for collagen formation
Associated Conditions
-
Alcoholism (controversial)
-
Epilepsy
-
Diabetes
-
Chronic obstructive pulmonary disease
Signs and Symptoms
-
Usually begins with 1 or more nodules in the palmar fascia of the ring and little finger rays
-
Often associated with skin dimpling over or around the nodules
-
Often bilateral (45%) (3)
-
Rarely symmetric
-
As the disease progresses, the digital
fascia becomes involved, usually producing contractures, first of the
MCP joints, and then of the PIP joints (Fig. 2). -
Web space contractures can occur.
-
Knuckle pads over the dorsum of the PIP joints are present in ~20% of patients.
-
These usually are unnoticeable, but if large and prominent, they may be painful when hit.
-
-
In the subgroup of patients with Dupuytren diathesis, the disease involves the hands, feet, and penis.
-
Often associated with knuckle pads, plantar fibromatosis (Ledderhose disease), and penile fibromatosis (Peyronie disease)
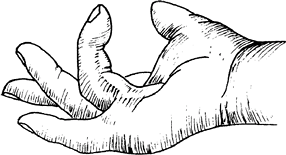 Fig. 2. In advanced Dupuytren contracture, the finger is drawn up and impairs the use of the hand.
Fig. 2. In advanced Dupuytren contracture, the finger is drawn up and impairs the use of the hand.
-
Physical Exam
-
The Hueston table-top test (4)
is positive when the palm is placed on a flat surface and the digits,
because of joint contractures, cannot be simultaneously placed fully on
the same surface. -
A positive test often is an indication for the consideration of surgical management.
Tests
Pathological Findings
-
Histologically, the important cells are the myofibroblasts, which seem to undergo pathologic proliferation.
-
An increase in the ratio of type III to type I collagen is found in Dupuytren disease (5).
Differential Diagnosis
-
Arthritis
-
Joint capsule contractures
General Measures
In the absence of contracture, or when a contracture is
progressing slowly and is not disabling, the patient should be observed
every 3–6 months.
progressing slowly and is not disabling, the patient should be observed
every 3–6 months.
Special Therapy
Physical Therapy
-
The goals are to maintain the extension
gained by the surgical procedure and to restore preoperative flexion
and function of the hand. -
A comfortable, well-fitted splint is an important adjunct to therapy.
-
Physical therapists play a major role in recovery, and their programs should stress performance of independent exercises.
Medication (Drugs)
-
Nonoperative management:
-
Vitamin E and splinting have been ineffective (5).
-
Cortisone injection of nodules that have not yet formed cords has been shown to suppress their development (6).
-
Injection also may be helpful in treating knuckle pads (6).
-
P.107
Surgery
-
Not indicated for static, painless nodules and rarely for knuckle pads
-
Early surgical intervention is indicated
for any degree of proximal IP joint involvement or in the presence of
progression of contracture or loss of function. -
5 surgical procedures are used in treating Dupuytren contractures:
-
Subcutaneous fasciotomy
-
Partial (selective) fasciectomy
-
Complete fasciectomy
-
Fasciectomy with skin grafting
-
Amputation
-
-
To choose the best procedure for a given patient, the clinician must consider:
-
The degree of contracture
-
Patient’s age, occupation, and general health
-
Nutritional status of the palmar skin
-
Presence or absence of arthritis
-
-
The frequency and duration of splinting after surgery vary with the severity of the disease.
-
A minimum of 3 months usually is
required; many patients are instructed to wear a splint at night for up
to an additional 3 months. -
Return to normal activity usually is anticipated within 2–3 months after surgical intervention.
-
Prognosis
-
The normal postoperative expectation is a full range of flexion and extension in 80% of patients seen primarily.
-
The disease is likely to progress more rapidly and to recur more frequently in young male patients with a strong family history.
-
Patients with epilepsy, diabetes, and alcoholism tend to develop more severe disease.
-
Although long-term recurrence rates vary
from 26–80%, often only the young patient with a strong diathesis will
need multiple repeat procedures.
Complications
-
Joint stiffness usually can be prevented with early physical therapy and patient education.
-
1–3% risk of nerve injury during surgery
-
50% risk of recurrence after 5–10 years
-
Unfortunately, long-term complications often depend on the diathesis of the patient.
Patient Monitoring
-
Patients must be followed closely (each
week during the 1st postoperative month) to help assess wound healing
and to prevent stiffness. -
Once healed, follow-up may be on an as-needed basis.
References
1. Burge P, Hoy G, Regan P, et al. Smoking, alcohol and the risk of Dupuytren’s contracture. J Bone Joint Surg 1997;79B:206–210.
2. Hurst
LC, Badalamente MA. Associated diseases. In: McFarlane RR, McGrouther
DA, Flint MH, eds. Dupuytren’s Disease: Biology and Treatment.
Edinburgh: Churchill Livingstone, 1990:253–260.
LC, Badalamente MA. Associated diseases. In: McFarlane RR, McGrouther
DA, Flint MH, eds. Dupuytren’s Disease: Biology and Treatment.
Edinburgh: Churchill Livingstone, 1990:253–260.
3. Calandruccio JH. Dupuytren contracture. In: Canale ST, ed. Campbell’s Operative Orthopaedics, 9th ed. St. Louis: Mosby-Year Book Inc., 1998:3675–3684.
4. Hueston JT. Dupuytren’s contracture. In: Jupiter JB, ed. Flynn’s Hand Surgery, 4th ed. Baltimore: Williams & Wilkins, 1991: 864–889.
5. Hurst
LC. Dupuytren’s disease. In: Manske PR, ed. Hand Surgery Update.
Rosemont, IL: American Society for Surgery of the Hand, 1994:271–279.
LC. Dupuytren’s disease. In: Manske PR, ed. Hand Surgery Update.
Rosemont, IL: American Society for Surgery of the Hand, 1994:271–279.
6. Ketchum LD, Donahue TK. The injection of nodules of Dupuytren’s disease with triamcinolone acetonide. J Hand Surg 2000;25A:1157–1162.
Additional Reading
McGrouther DA. Dupuytren’s contracture. In: Green DP, Hotchkiss RN, Pederson WC, et al., eds. Green’s Operative Hand Surgery, 5th ed. Philadelphia: Elsevier Churchill Livingstone, 2005:159–185.
Codes
ICD9-CM
728.6 Dupuytren contracture
Patient Teaching
-
Patients should be aware that although MCP deformities usually can be corrected surgically, PIP deformities often may not.
-
The patient also must realize that surgery cannot cure Dupuytren disease.
Prevention
No effective means of prevention is known.
FAQ
Q: When is surgery indicated for a Dupuytren contracture?
A:
Surgery is not indicated unless the patient has a functional disability
and progression of the contracture. Typically, surgery is not
considered until a >30° contracture is present at the MCP joint
and/or some contracture at the PIP joint.
Surgery is not indicated unless the patient has a functional disability
and progression of the contracture. Typically, surgery is not
considered until a >30° contracture is present at the MCP joint
and/or some contracture at the PIP joint.
Q: Why is recurrence frequent?
A:
The goal of surgery is release of contracture. Dupuytren contracture is
a genetic condition, and surgery does not alter the genes, so
recurrence is to be expected.
The goal of surgery is release of contracture. Dupuytren contracture is
a genetic condition, and surgery does not alter the genes, so
recurrence is to be expected.
