DISLOCATIONS OF THE CARPUS
anatomically divided into two rows. From radial to ulnar, the proximal
carpal row is composed of the scaphoid, lunate, triquetrum, and
pisiform (sometimes not classified as a carpal bone because it is a
sesamoid bone within the tendon of the flexor carpi ulnaris). From
radial to ulnar, the distal carpal row is composed of the trapezium,
trapezoid, capitate, and hamate. Each bone has a unique shape, but each
bone may be considered schematically to be cuboid. For the central
bones–the capitate, trapezoid, and lunate—only the dorsal and palmar
surfaces are available for capsular attachments. The remaining four
sides are covered with articular cartilage. In contrast, the marginal
carpal bones have an additional surface available for capsular
attachments: the lateral (radial) surfaces of the trapezium and
scaphoid and the medial (ulnar) surfaces of the hamate and triquetrum.
carpal bones, with the exception of the pisiform. Occasionally, one of
the multiple slips of the abductor pollicis longus inserts into the
scaphoid or trapezium, and the tendon of the extensor carpi ulnaris may
insert into the hamate. Only a few areas on the surfaces of the carpal
bones are not covered by articular cartilage or capsular attachments,
such as the neck of the capitate and the palmar surface of the proximal
pole of the scaphoid. These areas are covered by the synovial layer of
the joint capsule.
the carpal ligaments may be divided into extrinsic and intrinsic
groups. Extrinsic ligaments are those with an attachment proximal or
distal
to
the carpal bones, and intrinsic ligaments attach entirely to carpal
bones. The carpal ligaments may also be classified anatomically as
capsular or intraarticular. As a rule, intraarticular ligaments are
intrinsic, but capsular ligaments may be intrinsic or extrinsic.
Capsular ligaments are well organized structures that are thickenings
of the joint capsule (4).
They are composed of dense fascicles of collagen surrounded by loosely
organized areolar tissue called the perifascicular space. This space
transmits blood vessels supplying the carpal bones, the ligaments, and
a surprising amount of nerve tissue. The nerve tissue in the ligaments
may play a role in joint proprioception. Groups of fascicles, aligned
in a roughly parallel fashion, form the thickening that is called a
capsular ligament. It is covered on the joint surface by a continuous
layer of synovial cells, the synovial stratum; on the superficial
surface, it is covered by nonparallel fibrous elements called the
fibrous stratum (4). The synovial and fibrous
strata are direct extensions of the synovial and fibrous strata
composing the joint capsule in regions where no ligamentous thickening
is present. Morphologically, intraarticular ligaments are similar to
capsular ligaments, but they are surrounded by synovial strata alone (8).
The internal organization of the collagen fascicles is lost to form a
zone of fibrocartilage. A “blue line” separates the fibrocartilage into
mineralized and demineralized zones. The mineralized zone blends into
the cortical bone in a fashion analogous to the formation of Sharpey’s
fibers of tendon insertion.
After dissection of the synovial lining of the carpal tunnel, the
remaining fibers appear to originate proximally from the radial and
ulnar margins of the wrist and course obliquely distally toward the
midline lunate and capitate. The individual ligaments can be more
clearly defined when viewed from within the wrist (Fig. 41.2). Beginning radially, four distinct extrinsic palmar radiocarpal ligaments have been defined (8,9).
Originating from the radial styloid process and the radialmost palmar
lip of the radius is the radioscaphocapitate (RSC) ligament (9,35).
It courses distally as a single ligament to insert into the radial
aspect of the waist of the scaphoid and hemicircumferentially around
the proximal half of the distal pole of the scaphoid. Palmar to the
head of the capitate, it merges with fibers from the triangular
fibrocartilage (TFC) complex and the triquetrum to form a supporting
sling for the head of the capitate, sometimes referred to as the
arcuate ligament. Only a small percentage of fibers from the RSC
ligament join fibers from the scaphocapitate ligament, which is
contiguous and distal to the RSC ligament, to insert into the body of
the capitate. There is no discrete radial collateral ligament, but the
fibers of the RSC ligament that insert into the waist of the scaphoid
form a radial “wall” in the radiocarpal joint capsule and anatomically
are well suited to behave as a radial collateral ligament.
 |
|
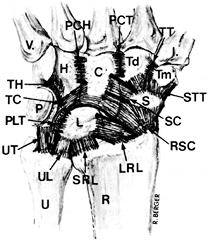
Figure 41.1. The wrist region from a palmar perspective, showing the capsular extrinsic and intrinsic carpal ligaments. Bones: R, radius; U, ulna; S, scaphoid (distal pole); L, lunate; P, pisiform; Tm, trapezium; Td, trapezoid; C, capitate; H, hamate; I, first metacarpal; V, fifth metacarpal. Ligaments: RSC, radioscaphocapitate; LRL, long radiolunate; SRL, short radiolunate; UL, ulnolunate; UT, ulnotriquetral; SC, scaphocapitate; PLT, palmar lunotriquetral; TC, triquetrocapitate; TH, triquetrohamate; STT, scaphotrapeziotrapezoid; TT, trapeziotrapezoid; PCT, palmar capitotrapezoid; PCH,
palmar capitohamate. Notice the interval between LRL and SRL, where the radioscapholunate neurovascular pedicle enters the radiocarpal joint. |
 |
|
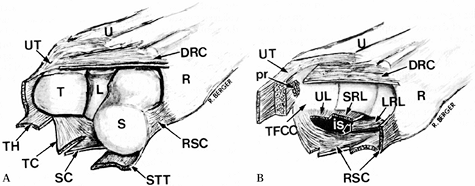
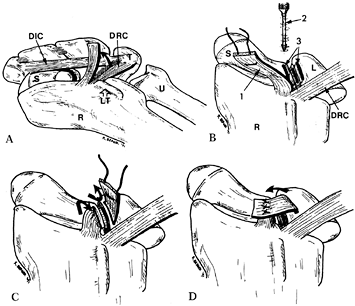
Figure 41.2. A: A wrist from a distal and radial perspective with removal of the distal carpal row of bones. Bones: R, radius; U, ulna; S, scaphoid; L, lunate; T, triquetrum. Ligaments: DRC, dorsal radiocarpal; UT, ulnotriquetral; TH, triquetrohamate; TC, triquetrocapitate; SC, scaphocapitate; STT, scaphotrapeziotrapezoid. B: A wrist from a distal and radial perspective with the proximal and distal carpal rows of bones removed. Bones: R, radius; U, ulna. Ligaments: RSC, radioscaphocapitate; LRL, long radiolunate; SRL, short radiolunate; UL, ulnolunate; TFCC, triangular fibrocartilage complex; pr, prestyloid recess; is,
interligamentous sulcus. The interligamentous sulcus is continuous with the space of Poirier at the tip of the palmar horn of the lunate. Notice the box-like arrangement of the extrinsic ligaments, which essentially envelop the proximal carpal row, resulting in a deepening of the radiocarpal joint. |
small amount of palmar overlap, the long radiolunate ligament takes
origin (9). It is separated from the RSC
ligament throughout its course by the intraligamentous sulcus. The long
radiolunate ligament does not attach directly to the scaphoid but
passes palmar to the proximal pole of the scaphoid and the palmar
portion of the scapholunate interosseous ligament to insert entirely
into the radial margin of the palmar horn of the lunate. Just ulnar to
the origin of the long radiolunate ligament, the radioscapholunate
(RSL) ligament enters the radiocarpal joint space through a defect in
the palmar radiocarpal joint capsule. This structure is not a true
ligament; it is a neurovascular bundle supplied by branches from the
palmar carpal branch of the radial artery, the anterior interosseous
artery, and the anterior interosseous nerve (8).
It is covered by a thick synovial lining, readily appreciated with an
arthroscope. The RSL ligament is continuous with the membranous
proximal portion of the scapholunate interosseous ligament and attaches
to the interfacet prominence, a fibrocartilaginous ridge separating the
scaphoid and lunate
fossae on the distal articular surface of the radius (4,8).
radiocarpal joint capsule, the short radiolunate ligament originates
and courses distally to insert into the palmar horn of the lunate at
the distal limit of the proximal articular surface of the lunate (9).
The fibers of the short radiolunate ligament blend imperceptibly with
fibers originating from the TFC complex, the ulnocarpal ligament
complex. The radialmost aspect of this complex is the ulnolunate
ligament, which attaches to the palmar horn of the lunate just ulnar to
and in continuity with the short radiolunate ligament. More ulnarly,
fibers course distally, deep to the palmar portion of the
lunotriquetral ligament, where they curve radially to merge with fibers
from the RSC ligament palmar to the head of the capitate. Forming the
ulnar “wall” of the radiocarpal joint, the ulnotriquetral ligament
inserts into the ulnar surface of the triquetrum, anatomically behaving
as an ulnar collateral ligament, and continues distally to insert into
the ulnar surface of the hamate. In 60% to 70% of normal adults, a
small defect filled with synovial villi is found between the ulnolunate
and ulnotriquetral ligaments. This defect marks the entrance to the
pisotriquetral joint and is uniformly lined by tufts of synovial villi.
A second defect in the TFC complex–ulnar collateral ligament complex is
found more proximally and in the ulnar wall, which is also lined by
synovial villi. This is the prestyloid recess, which sometimes
communicates with the ulnar styloid process.
It originates from the dorsal margin of the distal radius, centered
just distal to Lister’s tubercle, and courses obliquely distally and
ulnarly to insert partially into the dorsal horn of the lunate and more
substantially into the dorsal surface of the triquetrum. It is separate
from the dorsal portion of the lunotriquetral interosseous ligament and
supports the fourth and fifth extensor tendon compartments at the level
of the radiocarpal joint. Overlapping with the insertion of the dorsal
radiocarpal ligament on the triquetrum, the dorsal intercarpal ligament
originates to course distally and radially, passing just distal to the
dorsal horn of the lunate to insert onto the dorsal surface of the
waist and distal pole of the scaphoid. A few fibers also insert into
the dorsal surface of the trapezoid. The dorsal intercarpal ligament
also forms the floor of the fourth and fifth extensor tendon
compartments as they cross the wrist region.
 |
|
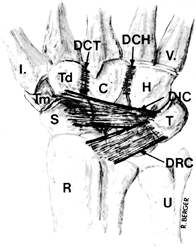
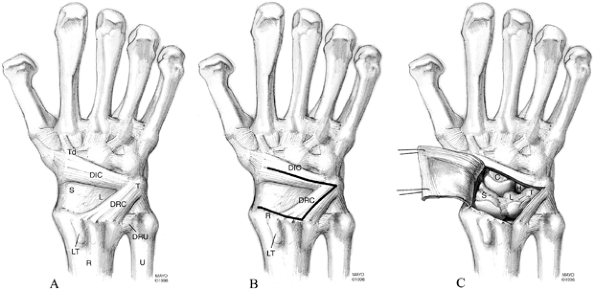
Figure 41.3. The wrist region from a dorsal perspective, showing the capsular extrinsic and intrinsic carpal ligaments. Bones: R, radius; U, ulna; S, scaphoid; T, triquetrum; H, hamate; C, capitate; Td, trapezoid; Tm, trapezium; I, first metacarpal; V, fifth metacarpal. Ligaments: DRC, distal radiocarpal; DIC, dorsal intercarpal; DCT, dorsal capitotrapezoid; DCH, dorsal capitohamate.
|
anatomic feature considering the relatively high range of motion
between the proximal and distal carpal rows. However, stability of the
midcarpal joint depends in part on the following intrinsic ligaments (Fig. 41.1 and Fig. 41.2). On the palmar surface of the carpus, beginning radially,
the first midcarpal ligament is the palmar scaphotrapeziotrapezoidal
(STT) ligament. These fibers originate from the distal half of the
palmar surface of the distal pole of the scaphoid and diverge in a V
pattern to insert onto the proximal surface of the palmar tubercle of
the trapezium and the proximal palmar surface of the trapezoid. Ulnar
to the origin of the STT ligament, the scaphocapitate ligament
originates from the distal pole of the scaphoid (9).
The proximal limit of the scaphocapitate ligament is continuous with
the distal limit of the RSC ligament. The scaphocapitate ligament is a
thick ligament that courses obliquely distally and ulnarly to insert
onto the radial half of the palmar surface of the body of the capitate,
carrying with it some of the distalmost fibers of the RSC ligament.
the distal margin of the palmar surface of the triquetrum, just radial
to the pisotriquetral joint capsule, to course distally and insert onto
the palmar surface of the body of the hamate. A group of fibers from
the origin of the triquetrohamate ligament diverge radially with fibers
from the ulnar collateral ligament to insert into the ulnar half of the
palmar surface of the body of the capitate as the triquetrocapitate
ligament. Dorsally, there is a paucity of ligaments spanning the
midcarpal joint. The distalmost fibers of the dorsal intercarpal
ligament diverge to insert onto the dorsal surfaces of the trapezium
and trapezoid, but there are no significant capsular ligaments
connecting the proximal carpal row to the capitate or hamate dorsally.
function of the intrinsic carpal ligaments. Within the proximal carpal
row, there are two intrinsic ligament systems. The scapholunate
ligament is composed of thick ligaments dorsally and palmarly, with a
proximal and intermediate membranous region, which is continuous with
the RSL ligament (2,4,8,23).
The palmar region of the scapholunate ligament is longer than the
dorsal region and has a more oblique orientation, perhaps allowing more
rotation between the two bones. The dorsal region is a true capsular
ligament, but the palmar region is entirely intraarticular, because the
palmar surface of the scapholunate ligament is covered by, but is
separate from, the long radiolunate ligament. Both the dorsal and
palmar regions of the lunotriquetral ligament are capsular, connected
proximally and intermediately by a membranous region (32).
Both regions of the lunotriquetral ligament are quite thick and roughly
equivalent in length. When intact, the membranous regions of the
scapholunate and lunotriquetral ligaments isolate the midcarpal joint
from the radiocarpal joint. In the distal carpal row, the intrinsic
carpal ligaments form a nearly continuous sheet of fibers, spanning
almost the entire palmar and dorsal surfaces of the trapezium and
trapezoid and the bodies of the capitate and hamate (31).
row, there are no membranous components to the intrinsic ligaments of
the distal carpal row (Fig. 41.4). The
individual regions, although difficult to separate anatomically, are
called the trapeziotrapezoid, capitotrapezoid, and capitohamate
ligaments. There are two deep intrinsic ligaments in the distal carpal
row that are not appreciated until the respective joints are opened.
The deep capitohamate ligament is found in a nearly square recess in
the contiguous articular surfaces of the capitate and hamate, near the
palmar and distal extent of the surfaces. This ligament is thick and
has an average cross-sectional area of 25 mm2. The deep
capitotrapezoid ligament is situated in the mutual articular surfaces
of the trapezoid and capitate, angling obliquely and dorsally toward
the capitate. It is unclear what specific function these deep ligaments
serve, but in addition to being mechanical constraints, they have an
extremely high nerve content, suggesting some proprioceptive function.
 |
|
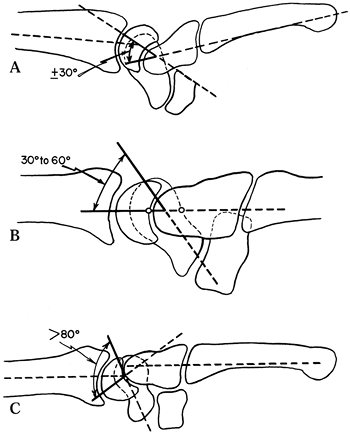
Figure 41.4. These drawings of the forearm, carpus, and central metacarpal area show the alignment of (B) the balanced carpus and (A,C)
the two common collapse positions—volar intercalated segment instability (VISI) and dorsal intercalated segment instability (DISI)—as they would be seen on a sagittal radiograph. A: Collapse in the VISI pattern is signified by a capitolunate angle of -30° or more. B: In the stable, normally balanced wrist, the radius, lunate, capitate, and third metacarpal form an almost colinear alignment. C: In the DISI pattern, a scapholunate angle of 80° or greater and lunate extension are typical. |
remained essentially unchanged from the time of the original
radiographic visualization of the carpus in 1895 (12).
It was thought that the two carpal rows behaved as separate units, with
the scaphoid serving as a link between the rows. Navarro challenged the
row concept by introducing a columnar concept, which is supported by
Taleisnik (35). This view, however, has
generally been accepted in terms of kinetic loading rather than
kinematic behavior. With the development of sophisticated measurement
techniques and the employment of rigid-body mechanical principles, such
as instantaneous screw displacement axes and Eulerian angles, a new and
still evolving understanding of the interrelationships of carpal bone
kinematics began to unfold (5).
circumduction. There is a functional direction of motion referred to as
the “dart throw” axis, which moves the wrist from dorsiflexion and
radial deviation to ulnar deviation and palmar flexion. The radiocarpal
and midcarpal joints are thought to contribute equally to palmar
flexion and dorsiflexion. The midcarpal joint contributes approximately
50% more motion than the radiocarpal joint to radial and ulnar
deviation. The overall center of rotation of the wrist is in the head
of the capitate for both major planes of motion (43).
Negligible translation of the carpal bones has been detected, compared
with the magnitude of rotation. The bones of the distal carpal row
behave very much as a single integrated unit, with minimal intercarpal
motion. They move in the same plane as the metacarpals, mostly because
of the strong ligamentous attachments between the bones of the distal
carpal row. The bones of the proximal carpal row, although overall
behaving as a functional unit, show significant differences of motion
within the row. As the wrist is dorsiflexed, the scaphoid, triquetrum,
and lunate show decreasing magnitudes of rotation in that order.
Overall, the major direction of rotation is similar to that of the
distal carpal row, but as dorsiflexion is achieved, the scaphoid
supinates and the lunate pronates, resulting in a palmar separation of
the two bones (23). The scaphoid also rotates
through a greater arc relative to the lunate, further separating the
palmar aspects of the two bones. The reverse phenomenon occurs in
palmar flexion. There is little difference in the pronation or
supination angles between the lunate and triquetrum. From ulnar
deviation to radial deviation, the major axis of proximal row bone
motion is palmar flexion. The relative pronation and supination
tendencies of the scaphoid and lunate are similar to those found in
palmar flexion of the wrist. The reverse phenomenon occurs in ulnar
deviation, with relative separation of the palmar aspects of the
scaphoid and lunate, as in dorsiflexion of the wrist. The additional
degrees of freedom found in proximal row bone kinematics is probably
due to the relative paucity of interosseous ligaments compared with
those of the distal carpal row. This may explain the predisposition of
the proximal carpal row to mechanical dissociation relative to the
distal carpal row.
been used for years in many different forms, and this has led to
substantial confusion and misuse of the term. Recently, the Anatomy and
Biomechanics Committee of the International Federation of Societies for
Surgery of the Hand published a position statement
dedicated to refining the definition of carpal instability (16).
In the strictest terms, carpal instability is defined as a condition in
which the wrist is unable to bear loads and does not exhibit normal
kinematics throughout its arc of motion. This may include malalignment,
but malalignment per se does not imply instability. Instability may be
purely mechanical, or it may be clinical, as in a patient who has
symptoms related to the instability. There are three categories of
instability. A grade I or grade II (see Chapter 95)
sprain of the soft-tissue restraint mechanisms of the carpus caused by
a subluxation alters the natural relationships, but less than with a
dislocation. A more severe sprain, perhaps a grade III with complete
rupture, is usually caused by a dislocation (luxation). There is
sufficient disruption of the soft-tissue restraints to cause two or
more normally congruent joint surfaces to lose contact and congruency.
A fracture–dislocation is similar to a dislocation, except that one or
more major fracture fragments (i.e., at least 3–5 mm in greatest
dimension) are produced by the force.
dislocation pattern, which is a combination of radiocarpal and
midcarpal disruption. The possible patterns, in proximal to distal
progression, are radiocarpal, perilunate, midcarpal, axial, or
combinations of these. Various degrees of sprain, dislocation, and
fracture–dislocation can occur at any of the anatomic sites (Table 41.1).
Fractures of a single or multiple carpal bones are often unstable and
are therefore suitable for inclusion under the fracture–dislocation or
subluxation categories, but they are discussed in Chapter 42 on fractures of the carpal bones.
 |
|
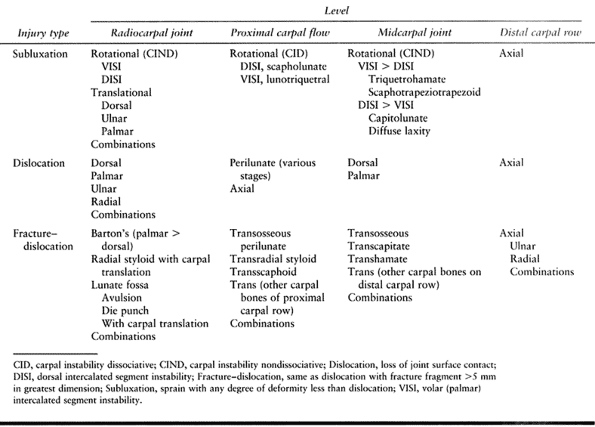
Table 41.1. Carpal Instability Categories
|
complex injuries into certain patterns characterized by the mechanism
of injury and resultant instability pattern (Fig. 41.4):
-
DISI is an acronym for dorsal intercalated segment instability.
-
VISI is derived from volar intercalated segment instability.
is preferred, but VISI is a widely used term and therefore is used
here. The intercalated segment in question is the proximal carpal row;
usage does not differentiate between the entire row and any given
portion of it (27). The position of the lunate,
as visualized on a lateral radiographic view, whether facing dorsally
or palmarly is the clue as to whether it is a DISI or VISI pattern. It
is important to know whether the lunate is still bonded or linked with
none, one, or both of its proximal carpal row neighbors, the scaphoid
and triquetrum. If it is linked, it is termed nondissociated and, if unlinked, dissociated. DISI or VISI may therefore be coupled with the following acronyms: CID, CIND, and CIC (14):
-
CID is an acronym for carpal instability dissociative.
-
CIND stands for carpal instability nondissociative.
-
CIC is an acronym for carpal instability combined or complex.
been used for 20 years and was originally coined to describe the
abnormal relationships occurring after injury at the scapholunate and
triquetrolunate joints (27). Because the most
obvious damage in scapholunate dissociation is to the intrinsic
scapholunate and lunotriquetral ligaments in triquetrolunate
dissociation, it seemed reasonable to use the term nondissociative
for instabilities in which the initial damage appears to be to the
extrinsic ligaments of the carpus. Another way of describing the
difference is that dissociative lesions begin with damage to the
intercarpal ligaments; nondissociative lesions begin with damage to the
intracarpal or forearm–carpal ligaments.
instability as a CIND-VISI or CIND-DISI, depending on whether the
collapse position is in flexion or extension. Because the proximal
carpal row is deforming as a unit, this deformity is entirely different
from the VISI deformity often seen with triquetrolunate dissociation,
in which the deformity takes place within the proximal carpal row. If
the intrinsic and extrinsic ligaments are damaged or if ligamentous
elements at the radiocarpal and midcarpal levels are damaged, the
carpal instability is combined or complex, and the abbreviation CIC is
appropriate. This is often unnecessary because most instabilities
eventually involve both intrinsic and extrinsic stabilizing structures.
Staging of the condition implies various levels of damage to support
structures. This theme is developed further as the specific
instabilities are discussed.
Dynamic may mean progressive, and it is widely interpreted in that way
in Europe. Applied to carpal instabilities, it was and is used to
describe instabilities that do not appear obvious on the standard
posteroanterior (PA) and lateral radiographs but require some stress or
loading with the use of a provocative maneuver or a special imaging
technique to display the instability. In this sense, dynamic has two
different meanings. Static implies that the instability is obvious on
standard radiographs taken without special loading maneuvers or
techniques.
instability diagnoses. The spectrum of possibilities in a given
instability varies from a barely noticeable sprain or contusion to a
severe and seemingly fixed deformity, often with arthritic changes.
 |
|
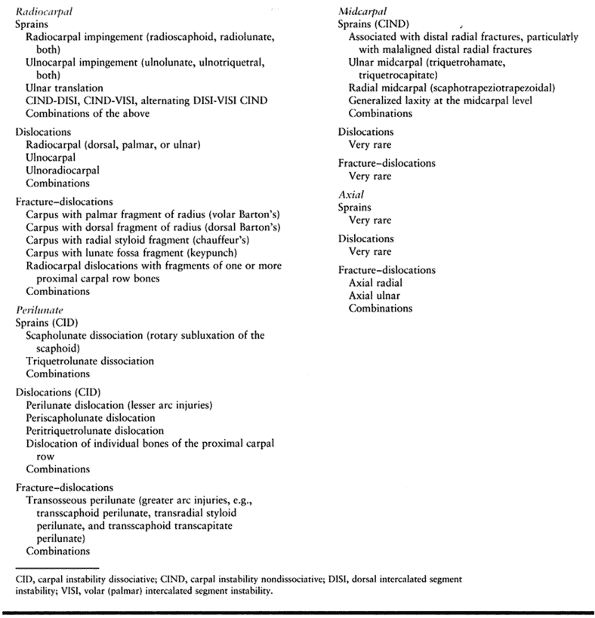
Table 41.2. Types of Carpal Injuries
|
If it is possible, determine whether the injury was a single episode
(with or without a particularly dramatic incident), multiple episodes,
or not related to a memorable episode. Obtain any information relevant
to a prior incident, diagnosis, or treatment involving the same area.
and difficulty in controlling wrist motions are the more common visible
signs (14,26,36).
entrapments, that may result in audible or palpable crepitus at the
wrist, but joint problems also produce noises. These are generally
described as clicks, snaps, clunks, thuds, or creaks. Localize these,
if possible, and relate them to the movement or stress that produces
them. Try to reproduce the patient’s pain and relate it to a particular
sign or maneuver.
-
Localize the tenderness.
-
Test for the presence, power, and excursion of the regional musculotendon units.
-
Test for grip power, grip endurance, pinch power, and pinch endurance.
-
Examine all neurovascular structures in the hand and wrist.
-
Use various provocative maneuvers, which
may be active or passive (see following sections). Include any
maneuvers known by the patient to elicit symptoms.
examining the wrist are those directed at detecting disruptions in the
interosseous ligaments between the scaphoid, lunate, and triquetrum.
Many more maneuvers have been described in one form or another (6), but these form a core of examinations that can be built upon.
provocative maneuvers, ask the patient about pain production and
whether the symptoms produced are similar or identical to or different
from the usual symptoms.
applying convergent pressure to the scaphoid and triquetrum. A positive
test is simply a complaint of pain and does not specifically identify
an injury.
of the scaphoid and the index finger on the dorsal skin over the
scapholunate joint, and palpate the distal pole of the scaphoid at the
point where the tendon of the flexor carpi radialis is no longer
palpable. The scapholunate joint can be located just distal to the
dorsal rim of the radius in line with Lister’s tubercle. Beginning with
the patient’s wrist in ulnar deviation, apply a dorsally directed force
to the distal pole of the scaphoid while passively deviating the wrist
radially. Use the index finger to detect a dorsal shift of the proximal
pole of the scaphoid. A positive test is one in which a subluxation is
palpated or the patient complains of pain in the region of the dorsal
scapholunate joint; it is relatively specific for scapholunate
dissociation (38).
palmar to the pisiform, and apply oppositely directed forces through
the fingers while the patient’s wrist is passively radially and ulnarly
deviated. A positive test is a sense of subluxation through the
lunotriquetral joint and pain with the maneuver (26).
pisiform–triquetrum column with the other hand. The pisiform–triquetrum
column is passively shifted dorsally and palmarly. A positive test is
one in which there is an excessive degree of motion compared to that in
the contralateral wrist, and the patient complains of pain (30).
In our practice, these are most often supplemented by stress views
(usually grip-compression or arm-weight-traction views), motion studies
(lateral extension–flexion or PA deviation views), or special
projections, such as carpal tunnel views. If the diagnosis remains
unclear,
a technician scan, fine-cut computed tomography (CT) with
reconstructions, or arthrography of the three carpal spaces may be
helpful. Occasionally, ultrasound, magnetic resonance imaging (MRI)
with and without gadolinium, or three-dimensional reconstruction may be
indicated.
 |
|
Figure 41.5. Posteroanterior (A) and lateral (B)
radiographs of a normal wrist. From the posteroanterior radiograph, one can easily assess the congruency of the carpal bone alignment using Gilula’s lines (I,II,III) as well as assess ulnar variance. From the lateral radiograph, the scaphoid (dashed line) and lunate (solid line) are easily identified. |
equivalent to and sometimes better than the combined imaging
techniques. However, a thorough understanding of normal arthroscopic
anatomy of the wrist is fundamental to making an accurate diagnosis and
formulating a treatment plan (1).
that it provides the opportunity to examine the range-of-motion and
perform provocative maneuvers before, during, and after surgical access
to the wrist. It is fairly common that the information gained about the
wrist in this way alters the treatment plan.
This approach is based on the anatomy of the dorsal radiocarpal and
dorsal intercarpal ligaments. The dorsal radiocarpal ligament attaches
to the dorsal rim of the radius between Lister’s tubercle and the
dorsal edge of the sigmoid notch, and distally to the dorsal lobe of
the triquetrum. At this same level, the dorsal intercarpal ligament
attaches to the triquetrum and spans the midcarpal joint to insert into
the dorsal surface of the
waist of the scaphoid, the lateral surface of the distal pole of the scaphoid, and the dorsal surface of the trapezoid.
 |
|
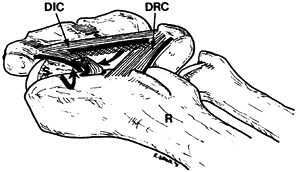
Figure 41.6. A: The dorsal surface of the carpus defining the anatomy of the dorsal radiocarpal ligament (DRC) and the dorsal intercarpal ligament (DIC). (S, scaphoid; L, lunate; T, triquetrum; Td, trapezoid; DRU, distal radioulnar ligament; R, radius; U, ulna; LT, Lister’s tubercle). B:
The dorsal surface of the carpus outlining the landmarks used to create a fiber-splitting capsulotomy. The DRC attaches proximally along the dorsal rim of the radius between LT and the sigmoid notch and distally onto the dorsal lobe of the triquetrum. The DIC attaches ulnarly onto the dorsal lobe of the triquetrum and radially onto the scaphoid and trapezoid. The DRC is split by dividing the distance between LT and the sigmoid notch and connecting this point to the dorsal lobe of the triquetrum. The DIC is split by connecting the dorsal lobe of the triquetrum to the sulcus between the scaphoid and trapezoid. The capsulotomy can be reflected radially by incising the remaining attachment of the capsule along the dorsal rim of the radius to the tip of the radial styloid process. C: The completed fiber-splitting capsulotomy showing the reflected joint capsule. Exposed are the scaphoid, lunate, hamate, and capitate, as well as the radial two-thirds of the radiocarpal joint and the entire midcarpal joint. (From Berger RA, Bishop AT. A Fiber-splitting Capsulotomy Technique for Dorsal Exposure of the Wrist. Tech Hand Upper Extremity Surg 1997;1:2, with permission.) |
-
After performing a dorsal approach to the
wrist capsule using the incision of your preference, identify the
following landmarks by palpation: Lister’s tubercle, sigmoid notch,
dorsal lobe of the triquetrum, and sulcus of the STT joint. -
Make an incision from the central aspect
of the dorsal lobe of the triquetrum proximally to the midpoint between
Lister’s tubercle and the sigmoid notch (splitting the dorsal
radiocarpal ligament) and radially to the sulcus of the STT joint
(splitting the dorsal intercarpal ligament). -
Release the dorsal radiocarpal joint
capsule from the dorsal rim of the radius radially, until reaching the
tip of the styloid process. -
Tangential to the dorsal cortices of the
proximal carpal row, sharply elevate the radially based flap of
capsule, exposing the entire midcarpal joint and the radial two-thirds
of the radiocarpal joint.
dorsal capsular ligaments, offers excellent exposure, and provides
flexibility in performing capsular modifications, such as capsulodesis,
without compromising exposure or stability.
instability is incomplete without emphasizing that the condition has
many presentations, which can be grouped roughly as follows:
-
Symptoms are present, but there is no or questionable deformity, even with imaging and provocative testing.
-
A condition, often referred to as a
dynamic instability, may exist; this means that with appropriate
stress—sometimes no more than wrist movement—a deformity occurs, but it
spontaneously disappears after the stress is discontinued. -
When a deformity is present on standard
radiographs, even at rest, it is often referred to as a static
deformity, for which there are three subdivisions: easily reducible,
only reducible with difficulty, or not reducible at all by nonsurgical
means. -
The final stage of carpal instability is
that of an almost fixed deformity with arthritic changes. The location
and degree of the arthritic change are important.
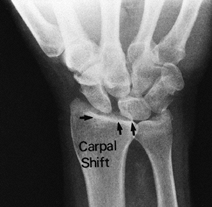
instability at the radiocarpal level and is usually discussed in the
same manner as components of distal radial fractures (14,25,34,36,39) (see Chapter 44). Ulnar translation is the second most common instability at the radiocarpal level (29).
It may occur as the residual of a full radiocarpal or perilunate
dislocation, or it may develop after lesser degrees of trauma. Its
manifestations may be subtle, or there may be a clinically visible
ulnar displacement of the carpus and hand. Radiographs may show a gross
ulnar displacement on the PA view, with the lunate directly distal to
the TFC, or the displacement may be so mild that the lunate overlaps
half on the radius and half over the TFC (a 50:50 lunate), rather than
the usual 60% or more overlap on the radius. If there is a perilunate
(i.e., scapholunate) disruption as well, the scaphoid may remain
anatomic, permitting the lunate with the central and ulnar carpus to
translate ulnarly (Fig. 41.7). Ulnar
translation is a common end point of many carpal instabilities from
either the initial injury itself or from chronic stress due to loading
at the radiocarpal level, even after various reconstructions. If there
is any evidence of ulnar translation instability, reconstructions that
increase radiocarpal loading should be avoided.
 |
|
Figure 41.7. PA view of a combined ulnar translation and perilunate disruption, demonstrating the ulnar shift of the lunate (black arrows), the increased scapholunate gap, and the 40:60 ratio (radial support to TFC support) position of the lunate.
|
ligaments dorsally and palmarly may be worthwhile, if done during the
first 4–6 weeks and protected with percutaneous internal fixation for
approximately 3 months. Even under these circumstances, the tendency
toward ulnar slide is so great that many attempts fail. Decreasing the
radial-to-ulnar angle by a closing wedge osteotomy of the radius added
to the ligament repair or reconstruction has been considered, but
experience with this approach is limited. The only procedure proven to
halt ulnar translation is a limited radiolunate or RSL carpal fusion.
The disruption probably occurs in this manner because the lunate is
strongly bound to the distal radius and weakly bound to the distal
carpus; combined with the strut-like interference of the radially
stabilizing scaphoid, which often fractures, this produces the most
common of the full dislocations of the carpus: transscaphoid perilunate
fracture–dislocation. This and other transosseous perilunate
dislocations are often referred to as greater arc injuries, and the
purely ligamentous perilunate disruptions are called lesser arc
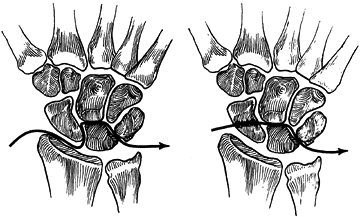
injuries (Fig. 41.9) (22).
 |
|
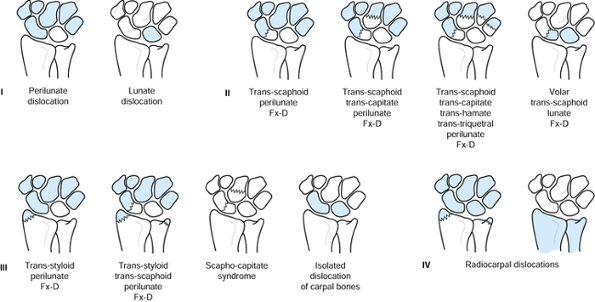
Figure 41.8.
The most common dislocations involving the carpus. Group I, perilunate and lunate dislocations, are usually only different stages of the same disruption pattern. Groups II and III are variations of the transosseous perilunate dislocations plus dislocations of single or paired carpal bones. Group IV includes the radiocarpal dislocations, both ligamentous and transosseous (i.e., fragments of the radius, ulna, or both bones). |
 |
|
Figure 41.9. Coronal-plane sketches of the wrist showing simplified versions of one of the disruption pathways for a lesser arc injury (left) and a greater arc injury (right). Several additional versions of the greater arc injuries are seen in groups II and III of Figure 41.7.
|
application of a body-weight force on an outstretched hand, such as
during a fall, a sports-related impact, or a motor vehicle accident.
Certainly, injuries to the perilunate ligaments can occur with less
impact under certain circumstances. Mayfield et al. (28)
recreated a pattern of progressive perilunate instability by applying
excessive axially directed loads to cadaver specimens positioned in
maximum ulnar deviation, dorsiflexion, and supination. Ulnar-sided
instability patterns are felt to result from similarly directed force
in a radially deviated wrist, although this has not been reproduced in
a laboratory environment. It is also conceivable that ligamentous
injuries can occur with the wrist positioned in palmar flexion.
obvious clinically, resulting in a painful, tender, short, broad, and
thick wrist. On radiographs, overlap of the carpal rows, an empty-cup
lunate, and a displaced capitate
are usually obvious (Fig. 41.10 and Fig. 41.11),
but there is a remarkably high incidence of failure to diagnose this
injury. There are many variants of this injury that do not reflect the
full disruption pattern or that spontaneously reduce and therefore may
be very difficult to diagnose. If the suspicion exists that a carpal
injury may be greater than is obvious, one should investigate further
with movement, traction, compression, and translational provocative
maneuvers, as well as arthrography or arthroscopy. High-resolution
tomography or CT will demonstrate the fracture details.
 |
|
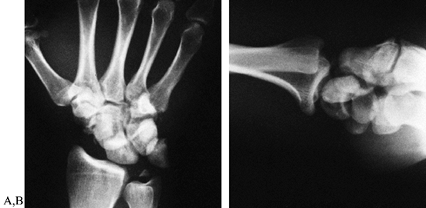
Figure 41.10. PA (A) and lateral (B)
radiographs show details of a complicated transosseous perilunate type of fracture–dislocation. It can be described as a transscaphoid, transulnar styloid, perilunotriquetral dislocation with an associated subluxation of the pisiform. The lunate and triquetrum are still in a relatively normal alignment with the forearm, and all physicians would be willing to call this a perilunate type of dislocation. |
 |
|
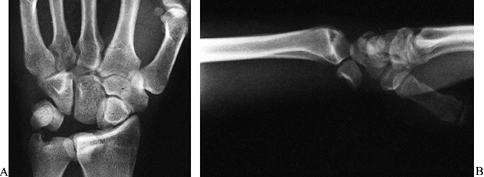
Figure 41.11. PA (A) and lateral (B)
radiographs of the same wrist show the lunate displaced palmarward and ulnarward, permitting the distal carpal row elements, particularly the capitate and hamate, to intrude toward the radius, displacing the scaphoid into flexion and the triquetrum ulnarward. Most physicians would call this a lunate dislocation because the carpal bones, other than the lunate, are fairly well aligned with the forearm. Nevertheless, the lunate is still in contact with a portion of its articular surface with the radius and still has intact ligament connections by its palmar radiolunate ligaments; therefore it is a stage of perilunate dislocation. |
Longitudinal traction with the fingers in Chinese finger traps combined
with manipulation usually results in reduction, especially if
anesthesia is used. Sometimes, closed reduction can be maintained with
the help of three-point molding in a thumb spica cast or splint (see Chapter 10).
Apply dorsally directed pressure with pads and careful cast molding at
the palmar projections of the scaphoid tuberosity and the pisiform, and
palmarly directed pressure with pads and careful cast molding at the
neck and dorsal sulcus of the capitate and Lister’s tubercle. Monitor
the patient closely after reduction to manage pain and swelling, assess
sensory and motor functions, and ensure that the reduction is
maintained. If the reduction is lost, open reduction and internal
fixation, sometimes with a bone graft, is indicated. During open
reduction and fixation, accomplish the following:
-
Inspect and repair extrinsic and intrinsic ligament damage.
-
Remove intraarticular debris and any interposed material.
-
Survey and record the areas of joint cartilage damage and treat, if appropriate.
-
Identify and treat fractures, restoring bone substance, position, and shape.
-
Anatomically realign the carpal elements to each other and to the forearm.
-
Internal fixation, percutaneous fixation, external fixation, or combinations of these are usually required to maintain position.
the injury. Incorporate the hand and forearm in a well padded thumb
spica splint, and elevate the hand. Start immediate motion of the
fingers. Do not remove Kirschner wires (K-wires) for 8 weeks, unless
they are loose or symptomatic. Splint the wrist and do not start
range-of-motion exercises before 3 months.
scaphoid are the same disorder, but the terms focus on differing
aspects of the pathology. One directs attention to the linkage between
the scaphoid and the rest of the proximal carpal row, and the other
focuses on the scaphoid itself; both terms have been expanded to
include the entire spectrum of injuries that disrupt the normal
relationships of the scaphoid to the rest of the carpus. The
pathomechanics of this condition are variable, but the classic
mechanism is the same as that for perilunate dislocation. It is obvious
that scapholunate dissociation as a residuum of perilunate dislocation
is a more unstable variety than scapholunate dissociation as a solo
entity.
occur independently of clinically significant perilunate injuries,
although the entire spectrum of perilunate injuries must be considered
with regard to treatment options. It has been hypothesized that even
partial injuries of the scapholunate ligament may progress with cyclic
loading to complete dissociation over time. In our experience, the
palmar region of the scapholunate ligament is the most commonly
disrupted site. This is probably related to the combined limited
strength of the palmar region of the ligament and the phenomenon of
mutual separation of the palmar regions of the scaphoid and lunate
during wrist dorsiflexion and ulnar deviation.
Although some wrists are so inherently stable that a tear of the
scapholunate interosseous membrane alone may have little clinical
consequence, gradual attenuation of the regional extrinsic support
system leads to increasing dissociation. This, plus the fact that none
of the current treatments predictably restores normal stability and
mobility, explains the continuing confusion about treatment.
Consider reconstruction of a large or chronic scapholunate dissociation
that shows any of the following:
-
Scapholunate gap of greater than 3 mm (Fig. 41.12)
![]() Figure 41.12.
Figure 41.12.
PA radiograph of the wrist showing a large scapholunate gap
representing a static scapholunate dislocation. It also shows that the
proximal pole of the scaphoid is trapped behind (i.e., dorsal or
posterior to) the radial styloid. This is sometimes described as a
scaphoid subluxation or dislocation, but the distal joint relationships
of the scaphoid are still reasonably intact. After the scaphoid is
reduced, treatment is carried out as for any other scapholunate
dissociation. -
Scapholunate angle of greater than 60°
-
A positive arthrogram or arthroscopic
examination confirming a scapholunate ligament tear with increasing
symptoms and minimal joint arthritis
-
Direct initial treatment of the fresh injury at protecting or repairing all the damaged ligaments and capsular structures.
-
Combinations of repair and reconstruction may be used.
treating scapholunate dissociation, only two are described here, in
addition to the recommended management for the acute, reducible injury.
Both surgical methods are best applied if the deformity is easily
reducible. If the deformity is very difficult to reduce or if
unexpectedly severe cartilage damage is found, a salvage procedure,
such as a proximal row carpectomy or a more extensive fusion, may be
indicated.
scapholunate dissociation. These include cast immobilization,
percutaneous pinning, direct ligament repair, capsulodesis, tenodesis,
ligament reconstruction, and intercarpal arthrodesis.
closed because of the following paradox of reduction. In the normal
wrist, the scaphoid and lunate will tend to separate at their anterior
surfaces during dorsiflexion, while at the same time becoming more
rotationally aligned to one another. In scapholunate dissociation, a
diastasis develops between the scaphoid and lunate, and rotational
displacement between the two bones increases. An attempt to close the
scapholunate angle by dorsiflexing the wrist produces an increase in
the diastasis, and an attempt to decrease the diastasis by
palmar-flexing the wrist increases the scapholunate angle.
based on the level of instability as defined by midcarpal arthroscopy,
has been developed by Geissler and Freeland (18) (Table 41.3).
On the basis of this scheme, we adopted the following treatment
algorithm: If the injury is acute and the scapholunate relationship can
easily be restored to normal, the scapholunate ligament should be
allowed to heal primarily in accordance with the options listed in Table 41.4.
For soft-tissue repairs alone to be successful, the reduction must
easily be achieved and maintained, and the security of the soft-tissue
repair must be high.
 |
|
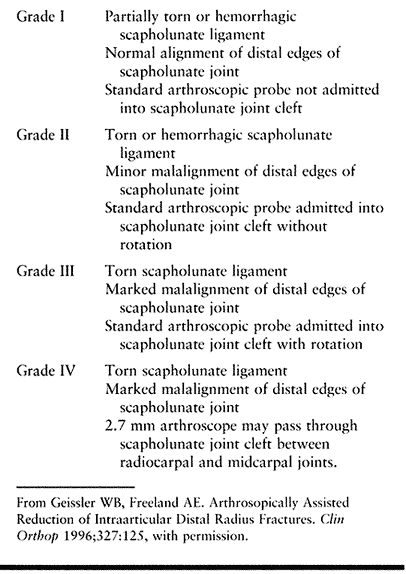
Table 41.3. Arthroscopically Based Grading of Dissociative Carpal Instability (Geissler and Freeland, 1996)
|
 |
|
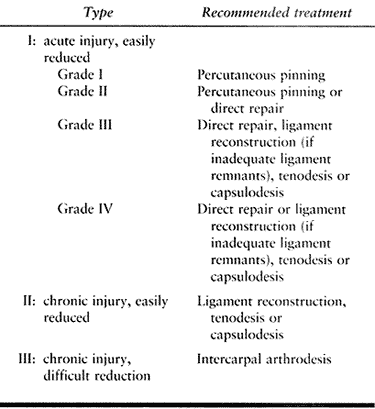
Table 41.4. Recommended Treatment for Scapholunate Dissociation Based on Arthroscopic Grades, Chronicity, and Ease of Reduction
|
-
Perform a dorsal fiber-splitting
capsulotomy as described above. A palmar approach is occasionally
indicated, which necessitates entering the carpal tunnel.
-
Make a standard carpal tunnel incision
with a curvilinear proximal extension, preserving the palmar cutaneous
branches of the median nerve. Retract the flexor tendons after blunt
dissection through the mesotenon radially or ulnarly. Take great care
to protect the median nerve, which must be retracted radially, from
excessive compression or tension. -
After visualizing the floor of the carpal
tunnel, perform a synovectomy, using rongeurs; this reveals the fibrous
lining of the palmar carpal ligaments. At this point, verify your
orientation to the carpal anatomy; ligamentous tissue is seen
converging on both the lunate and the capitate. It is easy to become
confused about which bone is which. If there is any question about a
specific level, place a metallic instrument on the bone in question,
and obtain a radiograph.
if ideal alignment is obtained. However, ideal alignment is difficult
to achieve in a true, complete scapholunate dissociation, for the
reasons cited above. Therefore, closed management is best reserved for
the treatment of incomplete scapholunate dissociation, or scapholunate
“sprains,” where the scapholunate rotational and diastatic
relationships are normal.
-
Cast support is similar to that described
for perilunate dislocation. It may be necessary to percutaneously place
temporary multiple K-wires across the scapholunate, radioscaphoid, or
scaphocapitate joint intervals. If satisfactory anatomic alignment
cannot be achieved, perform a dorsal approach to the carpus as
described above. -
After the scaphoid and lunate are
exposed, assess the damage to the scapholunate ligament. If the injury
is acute, there is usually sufficient tissue to perform a direct
repair. Place 0.047 mm K-wires, to be used as joysticks, into the
dorsal aspects of the scaphoid and the lunate; these greatly enhance
the ease of exposure and reduction. -
Reduce the scapholunate joint
anatomically, stabilize it with two K-wires, and then remove the
joysticks. Fully reflect the dorsal radiocarpal joint capsule to the
level of the waist of the scaphoid. Do not completely strip the capsule
from the scaphoid because it is the major source of blood supply to the
bone. -
With the wrist maximally flexed toward
the palm, use a small burr to “freshen” the attachment line of the
scapholunate ligament that has been disrupted, usually along the ulnar
margin of the scaphoid. -
With a 1/32 inch
(0.8 mm) drill point, drill four to six holes from this freshened
margin distally and radially to exit just distal to the proximal
articulating surface near the ridged waist of the scaphoid. Using Keith
needles, pass a nonabsorbable suture (2-0 or 3-0 Mersilene) through the
remnant of the scapholunate ligament and distally through the drill
holes to exit at the waist of the scaphoid, where the sutures are tied
securely (Fig. 41.13). Bring the radiocarpal joint to a neutral position, and take intraoperative radiographs to confirm the reduction.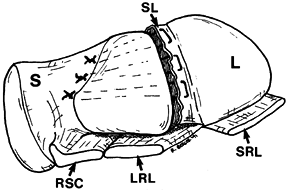 Figure 41.13. Direct repair of the scapholunate ligament. An isolated scaphoid (S) and lunate (L) are viewed from a proximal and slightly radial perspective. The scapholunate ligament (SL)
Figure 41.13. Direct repair of the scapholunate ligament. An isolated scaphoid (S) and lunate (L) are viewed from a proximal and slightly radial perspective. The scapholunate ligament (SL)
has been disrupted traumatically. In direct repair of the scapholunate
ligament, suture material (2-0 or 3-0 Mersilene) is passed through the
remnant of the ligament and drawn through drill holes in the scaphoid
to exit near the waist of the scaphoid, where the suture is drawn tight
and tied. This maneuver is accomplished after the scapholunate
dissociation has been provisionally reduced and secured with a
transosseous K-wire. (RSC, radioscaphocapitate ligament; LRL, long radiolunate ligament; SRL, short radiolunate ligament. -
Then close the wound, taking care to
securely reattach the dorsal radiocarpal ligament and the dorsal
radiocarpal capsule to the radius. If further reinforcement is
indicated, use one or more capsulodesis techniques (described in the
next section).
more difficult to treat than injuries. It may be difficult to
anatomically reduce the subacutely or chronically disrupted
scapholunate joint and obtain a repair that will withstand the demands
that the patient will place on the wrist afterward. Degenerative
changes will influence the choice of procedure. Two operative
approaches are available: soft-tissue repair and augmentation or
limited arthrodeses.
malrotated scaphoid advocate STT fusion or scaphocapitate fusion.
Radiocarpal or midcarpal degenerative changes detected radiographically
are strong indications for intercarpal fusion. Important objectives
with the STT or scaphocapitate fusion include reduction of the
malrotated vertically displaced scaphoid, achieving parallelism and
congruity of the proximal scaphoid and scaphoid sulcus,
closure of the scapholunate interval, and maintenance of carpal height.
-
Approach the STT joint region through a
transverse incision centered over the STT joint or through the
longitudinal approach described previously, with a distal extension. If
there is any question about the integrity of the articular surfaces of
the midcarpal or radiocarpal joints, conduct a preliminary arthroscopic
evaluation. -
With dorsal exposure of the STT joint
region, adequately decorticate the distal articular surface of the
scaphoid and the proximal articular surfaces of the trapezium and
trapezoid. -
Position the scaphoid, with radiographic
confirmation, so that the radioscaphoid angle is 40° to 45° and the
carpal height is restored. Stabilize the three bones in this position
with multiple K-wires, Herbert screws or AO screws, or staples, and
pack autogenous bone graft from the iliac crest or ipsilateral radial
metaphysis into the decorticated region. -
If scaphocapitate fusion is preferred,
expose the scaphocapitate interval through the dorsal longitudinal
approach. Decorticate the radial articulating surface of the capitate
and the ulnar articulating surface of the distal one-half of the
scaphoid. Mobilize, reduce, and bone-graft, as with the STT
arthrodesis. Some surgeons advocate carrying out a radial styloidectomy
to prevent radioscaphoid impingement, but this may lead to further
destabilization due to disruption of the radiocarpal ligaments. Great
care must be taken in performing a radial styloidectomy to preserve the
origins of the palmar radiocarpal ligaments. -
After an STT or scaphocapitate fusion, we
recommend postoperative immobilization with a thumb spica short-arm
cast followed by a supporting splint for 4–6 weeks. Use radiographic
evaluation on a regular basis to estimate consolidation of the fusion
mass. This evaluation may be enhanced with the use of trispiral
tomography.
dissociation with an essentially fixed deformity, which is difficult to
reduce and tends to recur, or if there are periscaphoid degenerative
changes or other special situations such as coexisting Kienböck’s
disease, the arthrodesis techniques described previously, including STT
and scaphocapitate limited fusions, are preferable. If the deformity is
relatively easy to reduce and there are no obvious signs of
periscaphoid degenerative changes, soft-tissue repair and augmentation
may be preferred. The basic prerequisite for soft-tissue repair and
augmentation is the ability to reduce and maintain all relationships of
the carpus, particularly the abnormal ones at the radioscaphoid,
radiolunate, scapholunocapitate, scapholunate, and STT joints.
Restoration of these relationships is achieved if the scapholunate gap
is reduced to 3 mm or less, the scapholunate angle is about 40°, and
the capitolunate angle is less than +15°. The soft-tissue procedures
center on repair of the remnant of the scapholunate ligament, as
described in the section on acute scapholunate injury, supplemented by
a capsular flap or a tendon graft flap. The augmentation can be carried
out with several capsulodesis techniques or by passing an extrinsic
tendon graft through the scaphoid and lunate to enhance stability. The
capsulodesis described by Blatt (10) uses the
dorsal radiocarpal joint capsule with a proximal base; the distal edge
of the flap is tethered to the dorsal aspect of the distal scaphoid.
The tissue used for this procedure is relatively isotropic, and the
resistance to chronic linear shear in tension is suspect.
a capsuloligamentous flap theoretically promises greater resistance to
deforming forces. This flap is based distally over the STT region and
incorporates essentially the proximal one-half of the dorsal
intercarpal ligament (Fig. 41.14).
 |
|
Figure 41.14.
Dobyns and Linscheid’s capsulodesis for augmenting scapholunate ligament repair. The exposed carpal region is seen from a proximal, dorsal, and radial perspective, and the dorsal radiocarpal ligament (DRC) and dorsal intercarpal ligament (DIC) are outlined. After adequate exposure, detach the proximal half of the DIC from its insertion onto the dorsal aspect of the triquetrum. Very carefully, leaving the synovial lining of the joint capsule intact, elevate the DIC, leaving a distally based attachment onto the scaphoid, trapezium, and trapezoid. Rotate the free-flap proximally, passing over the scapholunate interosseous region, to which it may be sutured, and then through a small channel created in the dorsal lip of the distal radius, and suture it back onto itself. Provisional reduction of the scapholunate dissociation and primary repair of the scapholunate ligament, if possible, should be carried out before this maneuver (R, radius; S, scaphoid). |
-
Approach the carpus through the longitudinal incision described previously.
-
Identify the insertion of the dorsal intercarpal
P.1350
ligament over the triquetrum and, with careful, sharp dissection,
elevate the proximal one-half of the dorsal intercarpal ligament from
the synovial lining of the joint capsule, beginning at the triquetrum
and proceeding toward the STT region. Preserve the synovial lining of
the joint capsule. The remaining dorsal intercarpal ligament spanning
the distance between the triquetrum and the STT region should limit the
risk of midcarpal destabilization. -
Reflect the distally based flap
proximally over the proximal pole of the scaphoid and, if possible,
over the scapholunate joint cleft dorsally. Then, attach it to the
region of capsular attachment in the dorsal rim of the radius, or pull
it through a channel drilled through the dorsal rim of the radius and
suture it back onto itself. -
Adjust the tension to prevent the
proximal pole of the scaphoid from translating dorsally. After this
tension is set, pass several nonabsorbable sutures through the flap
into the substance of the dorsal aspect of the scapholunate ligament.
inadequate for repair, particularly dorsally, a third capsulodesis
technique may be considered. This technique uses the distal one-half of
the dorsoradial carpal ligament in a fashion similar to that described
previously employing the dorsal intercarpal ligament (Fig. 41.15).
 |
|
Figure 41.15. Dorsal scapholunate ligament reconstruction and capsulodesis technique. A: The exposed carpus is seen from a proximal, dorsal, and radial perspective, with the dorsal radiocarpal (DRC) and dorsal intercarpal (DIC) ligaments also exposed (S, scaphoid; R, radius; U, ulna; T, triquetrum; LT, Lister’s tubercle). In the same fashion by which the DIC flap was elevated in Dobyns and Linscheid’s technique (Fig. 41.14),
the radial half of the DRC is elevated by detaching its insertion onto the dorsal triquetrum, with the proximal flap left attached to the dorsal rim of the radius. B: Using a high-speed drill or burr, make channels in the dorsal cortices of the scaphoid and lunate adjacent to the scapholunate articulation. These vertical channels are connected to horizontal channels passing just on the dorsal margin of the mutual articular surfaces of the scaphoid and lunate within the joint cleft. C: Pass the proximally based DRC flap into the dorsal opening of the scaphoid channel and across the scapholunate articulation through the mutual articular channels to exit through the dorsal channel of the lunate. D: Draw the DRC flap over the dorsal aspect of the scapholunate ligament and suture it onto itself, after adjusting the tension. Before final suturing, provisionally reduce the scapholunate dissociation and repair the scapholunate ligament, if possible. |
-
Through a longitudinal approach, identify
the triquetral insertion of the dorsal radiocarpal ligament. Elevate
the distal and radial half of the dorsal radiocarpal ligament
P.1351
subperiosteally
from the triquetrum, and separate it from the synovial lining of the
radiocarpal joint capsule proximally to its attachment through the
dorsal rim of the radius just distal to Lister’s tubercle (Fig. 41.15A).
Careful dissection allows elevation of this ligament without disruption
of the synovial lining of the dorsal radiocarpal joint capsule. -
Using a small, high-speed burr, establish
channels in the dorsal cortex of the scaphoid and lunate 2 mm away from
the joint surface (Fig. 41.15B). Through the
dorsal aspect of the mutual articulating surfaces within the joint
cleft, create communicating channels perpendicular to these dorsal
channels. -
Pass the free end of the ligament flap
through the scaphoid channel, beginning dorsally and then out into the
scapholunate joint cleft. Then, pass the ligament into the lunate
channel in the joint cleft to exit through the dorsal channel of the
lunate (Fig. 41.15C). Several options are now
available, including suturing the flap back onto itself to enhance
stability of the dorsal aspect of the scapholunate interosseous
ligament, or passing it distally and suturing it into the capsule over
the dorsal aspect of the capitate or base of the third metacarpal, if
length permits (Fig. 41.15D). This provides a dorsal tether between the lunate and capitate to resist the tendency for a DISI deformity.
augment intrinsic repair is technically demanding. This procedure
requires a dorsal and palmar approach and uses a split, distally based
strip of extensor carpi radialis longus or flexor carpi radialis, which
is passed through drill holes in the scaphoid and lunate in a
closed-loop fashion. The blood supply to the proximal pole of the
scaphoid and lunate is fragile, and the drill holes do place these
bones at risk for avascular necrosis; however, proponents of this
technique think that it provides strong static control of the scaphoid.
is a “tenodesis” procedure utilizing a distally based strip of flexor
carpi radialis. A drill hole is created in a dorsopalmar orientation
through the distal pole of the scaphoid, through which the tendon strip
is passed. It is then passed proximally and secured to the dorsal rim
of the radius. The rationale behind this procedure is the author’s
theory that advanced rotational subluxation of the scaphoid requires
not only compromise of the scapholunate ligament but also instability
at the STT joint. The tendon strip of the flexor carpi radialis
stabilizes the STT joint and prevents excessive palmar flexion of the
scaphoid.
bone–ligament–bone autografts for the scapholunate ligament in patients
with prearthritic scapholunate dissociation in whom inadequate ligament
is present for direct repair. A recent laboratory study evaluating the
strength and constraint properties of the subregions of the
scapholunate ligament identified the dorsal region of the ligament as
the strongest and the major constraint to translation and distraction (7).
Proposed substitutes have included bone–ligament–bone complexes based
on extensor retinaculum, intertarsal ligaments, and carpometacarpal
ligaments. These carry significant promise, but clinical experience is
very preliminary at this point. One should be cautioned that the
strength of the transplanted tissue should approach that of the native
scapholunate ligament and that care should be taken to avoid iatrogenic
instability at the donor site (20,21,41).
both bony and soft-tissue repair techniques. Support the wrist in the
neutral position for 8 weeks or more, removing K-wires between 8 and 12
weeks (sooner if required). Immediately initiate shoulder, elbow, and
digit range-of-motion exercises; introduce forearm motion gradually if
there is no associated ulnocarpal or forearm problem. Begin wrist
motion between 8 and 12 weeks. Keep the exercise limited, light, and
isokinetic until 20 weeks. Begin grip strengthening at 6 months. Wrist
stress loading may begin at 1 year, contingent on comfort and a benign
examination. Earlier rehabilitation may succeed, but the risk of
overstressing the wrist is great and it pays to be cautious.
relative simplicity. It is important to know that the radioscaphoid
joint, which takes most of the loading for the carpus, is in good
condition; it is vital that this joint be reduced and maintained at its
most congruent fit. If these two conditions are not met, rapid
radioscaphoid joint deterioration may occur. After STT fusions,
impingement between the distal scaphoid and the radial styloid may
occur, and it has been suggested that a small styloidectomy of the
radius be performed at the time of the fusion. The long-term concern
with radial column fusions is the effect of increased loading on one
joint system over a prolonged period. There is not sufficient
experience with these methods to respond to this concern. The virtue of
the soft-tissue techniques is that, at their best, they restore a more
normal distribution of stress across the carpal joints. The problems
are the relative complexity of the repair techniques and the large
forces that must be resisted by damaged and other questionable tissues.
Because of these problems, partial or complete recurrence of deformity
was common in the early days of soft-tissue repair and reconstruction.
The current techniques appear to be giving improved short-term results, but they must pass the test of time (24).
techniques, but as in all musculoskeletal procedures, other
complications are seen, including pain dysfunction syndromes,
neurovascular and compartment compromise, and infection. The last two
are infrequent but serious and must be identified early and treated
vigorously. Pain is so common that it should be assumed to be a likely
occurrence. Plan on good pain control with particular attention to the
control of swelling, autonomic dysfunction, and an early start of
rehabilitation. Support with transcutaneous nerve stimulants, nerve
blocks, and other measures.
common types of carpal instability listed in “Terminology and
Classification” above and in Table 41.1 and Table 41.2.
See the references listed for triquetrolunate dissociation, CIND of the
midcarpal and radiocarpal joints, combined types, and axial
instabilities (17,25,30,37,42). The most salient features of each of these are discussed in the following sections.
dissociation) may occur as an isolated injury, but it more commonly
occurs as part of the spectrum of perilunate dislocations. Due to the
extensive ligamentous insertion into the triquetrum on the dorsal,
ulnar, and palmar surfaces, this injury is generally more stable than
its counterpart in the scapholunate joint. Lunotriquetral dissociation
is often associated with other ulnar wrist problems, including
ulnocarpal impingement, TFC-complex tears, and distal radioulnar joint
instabilities. Patients complain of pain localized to the ulnar half of
the wrist that is often accompanied by a sensation of weakness.
Examination reveals tenderness specific to the lunotriquetral
articulation and exacerbation of discomfort with ballottement of the
unstable triquetrum. Unless there is a significant static deformity
resulting in a VISI pattern on lateral radiographs of the wrist,
radiographic documentation of lunotriquetral dissociation may be
difficult. Arthrography and MRI can demonstrate a defect in the
lunotriquetral membrane suggesting triquetrolunate dissociation.
necessary if symptoms are relieved after correction of the associated
conditions. If an acute triquetrolunate dissociation with minimal
deformity is discovered, external support with a cast or splint may be
all that is necessary. Percutaneous K-wire fixation may be useful,
particularly when the arthroscopic grading noted in Table 41.3 is followed.
is angular deformity, open surgical intervention may be indicated.
Several options are available. Direct repair of the interosseous
ligament in a fashion similar to that described for the scapholunate
ligament may be carried out and augmented with capsular flaps similar
to those described for scapholunate dissociation. If the direct repair
cannot satisfactorily correct the deformity, two other options are
available: augmentation of the ligament repair with a strip of distally
based flexor carpi ulnaris passed through drill holes in the triquetrum
and lunate, or a lunotriquetral arthrodesis, which is more successful
in achieving union than scapholunate arthrodesis. Complications of
lunotriquetral arthrodesis, including nonunion, persistent VISI
deformity, and persistent subjective complaints, occur in 33% of
patients undergoing this procedure. In patients with a fixed VISI
deformity, a radiolunate arthrodesis may be necessary to counter the
tendency for a VISI deformity to recur after appropriate treatment of
lunotriquetral dissociation.
 |
|
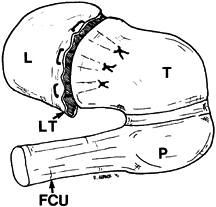
Figure 41.16.
Direct repair of the lunotriquetral ligament. The lunotriquetral complex is shown in an isolated fashion from a proximal and ulnar perspective. The lunotriquetral interosseous ligament (LT) has been traumatically disrupted, and strong suture (2-0 or 3-0 Mersilene) has been passed through the remnant of the ligament and into channels drilled through the substance of the triquetrum to exit ulnarly. After provisional reduction is achieved, these sutures are drawn tight and tied (L, lunate; T, triquetrum; P, pisiform; FCU, flexor carpi ulnaris tendon). |
-
After exposing the lunotriquetral joint
dorsally by entering the radiocarpal joint through the interval between
the fourth and fifth extensor compartments, freshen the triquetral
insertion of the lunotriquetral ligament with a burr, and drill paired
holes distally and
P.1353
ulnarly.
It may be necessary to subperiosteally elevate the triquetral insertion
of the TFC complex ulnarly to visualize the exit point of the drill
holes. Do not perform this procedure without direct visualization
because the extracapsular sutures may accidentally incorporate isolated
cutaneous branches of the ulnar nerve. -
Pass the sutures through the remnant of
the lunotriquetral ligament, which is usually attached to the lunate,
and then through the drill holes, and tie them. Transarticular K-wire
fixation is recommended. Postoperative care is similar to that outlined
for reconstructions of the scapholunate ligament.
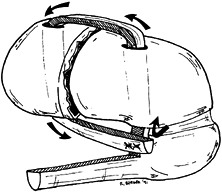
augmentation of the lunotriquetral joint with a distally based slip of
flexor carpi ulnaris. Refer patients requiring this procedure to
surgeons who are experienced in this technique (Fig. 41.17).
Through these incisions, test the supporting extrinsic ligaments (i.e.,
lunotriquetral portion of the dorsal radiolunotriquetral ligament and
the overlapping portions of the palmar ulnolunate and ulnotriquetral
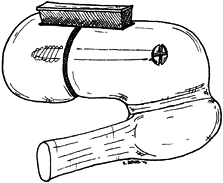
ligaments), and tighten them, if needed. Lunotriquetral arthrodesis,
carried out through a dorsal incision, consists of exposure of
subchondral bone on both sides of the lunotriquetral articulation,
insertion of a corticocancellous wedge of distal radius or iliac crest
bone graft across the lunotriquetral joint, and fixation with K-wires
or a transarticular compression screw (Fig. 41.18).
 |
|
Figure 41.17.
Reconstruction of the lunotriquetral ligament using the flexor carpi ulnaris tendon (FCU). At least 6–8 mm of the dorsal half of the FCU tendon is elevated from a hemitranssection proximally and delivered distally, with maintenance of its attachment onto the pisiform. Preserve the ulnar artery and ulnar nerve, just lateral to this tendon. Vertically oriented drill holes, just larger than the diameter of the free tendon slip, are made through the triquetrum, exiting palmarly just proximal to the pisotriquetral articulation, and through the lunate. The distally based free slip of FCU is delivered dorsally through the triquetrum and across the lunotriquetral articulation. After provisional reduction is achieved, tension is adjusted in the slip, and it is sutured to itself near its attachment to the pisiform. |
 |
|
Figure 41.18.
Arthrodesis of the lunotriquetral articulation. After complete removal of articular cartilage from the mutual articulating surfaces of the lunate and triquetrum and after removal of subchondral bone until bleeding bone is apparent, the lunate and triquetrum are mutually aligned, with care taken to preserve the normal intercarpal space. A corticocancellous iliac crest bone graft is harvested. Some is fashioned to fit in a slot that is created on the dorsal surfaces of the lunate and triquetrum, spanning the lunotriquetral joint; the remainder of the graft is morcelized and packed into the lunotriquetral interval. Supplemental fixation may be achieved with a transosseous screw. |
instability patterns (i.e., DISI and VISI) that indicate scapholunate
dissociation and triquetrolunate dissociation, but no clear disruption
of the connections between the bones of the proximal row and between
the bones of the distal row is evident. In this condition, the
instability is generated through an alteration in the restraints of the
radiocarpal joint, the midcarpal joint, or both, although this
condition is most often referred to as midcarpal instability in the
literature. Common clinical presentations include a “loose jointed”
individual, presentation with a snap or a clunk, a normal arthrogram,
and an abnormal motion pattern of the entire proximal row on
cineradiography or videotaped fluoroscopy. Radiocarpal and midcarpal
arthroscopy can help determine the cause of the problem.
CIND because there are many causes. Treatment is directed at the
abnormalities that are thought to generate the instability. Often,
palmar and dorsal approaches are necessary if capsular repairs are
anticipated. Each of the techniques described previously for the
nondissociative type of carpal instabilities, including direct capsular
repair of the space of Poirier, limited intercarpal fusions (e.g., STT,
scaphocapitate, and other midcarpal arthrodeses
and
capsulodesis procedures to control proximal carpal row instability),
and proximal row carpectomy are all viable options. In some
circumstances, radiocarpal arthrodesis may provide a reasonable option.
Clinical experience with this problem is limited. It is recommended
that treatment be done by a surgeon who has accumulated experience with
this condition.
also extraarticular abnormalities that generate similar conditions
termed carpal instability adaptive. For
example, a malunion of a distal radial fracture, with resultant dorsal
angulation of the distal articular surface, can initiate a zigzag type
of collapse that can simulate a DISI deformity. In this situation,
treatment involves corrective osteotomy of the radius with an opening
wedge osteotomy employing bone graft and plate fixation (see Chapter 44).
Although not strictly a CIND, malunion of the scaphoid may also result
in a DISI deformity. In this situation, operative treatment is an
opening wedge osteotomy of the scaphoid with bone grafting and K-wire
or screw fixation across the fracture site.
longitudinal direction of the carpus, generally resulting from
high-energy impact of the hand (17). They are
often accompanied by tearing or avulsion of the individual components
of the transverse carpal ligament system, frequently with separation of
the metacarpal bases. A history of a high-energy impact with the
involved hand raises suspicion of this injury. A high index of
suspicion is required to diagnose this condition. Standard radiographs
generally enable the diagnosis to be made, but because of the
superimposition of the carpal bones, particularly on the lateral view,
the findings may be subtle. If there are questions about the
possibility of this injury and the standard radiographs do not resolve
them, take stress radiographs or perform tomography, CT, or MRI.
Coexisting soft-tissue injuries, such as stretching or tearing of
contiguous vessels, nerves, or musculotendinous structures, often
present a greater problem than the skeletal injury itself.
neurovascular and musculotendinous integrity of the affected extremity.
Simple reduction of the dislocation may restore blood flow or nerve
supply. Look for and decompress a compartment syndrome if it occurs.
Repair of injured neurovascular and other soft tissues is often needed.
Traction is often helpful in obtaining reduction, and the reduction can
be maintained by K-wires and lag screws, as indicated. As a rule,
transcarpal or transmetacarpal K-wire fixation is indicated to prevent
redisplacement. Postoperatively, initiate early motion of the hand to
prevent extrinsic tendon adhesions. The reduction must be stable enough
to endure early motion.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
RA, Imeada T, Berglund L, An KN. Constraint and Material Properties of
the Subregions of the Scapholunate Interosseous Ligament. J Hand Surg [Am] 1999;24:953.
RA, Kauer JMG, Landsmeer JMF. The Radioscapholunate Ligament: A Gross
Anatomic and Histologic Study of Fetal and Adult Human Wrist Joints. J Hand Surg [Am] 1991;16:350.
G. Capsulodesis in Reconstructive Hand Surgery: Dorsal Capsulodesis for
the Unstable Scaphoid and Volar Capsulodesis following Excision of the
Distal Ulna. Hand Clin 1987;3:81.
GA, Brunelli GR. Une Nouvelle Intervention pour la Dissociation
Scapho-lunaire. Proposition d’Une Nouvelle Technique Chirurgicale pour
l’Instabilite Carpienne avec Dissociation Scapho-lunaire. Ann Chir Main Memb Super 1995;14:207.
TH. On Certain Points in the Anatomy and Mechanism of the Wrist Joint
Reviewed in Light of a Series of Roentgen Ray Photographs of the Living
Hand. J Anat Physiol 1896;31:59.
EJ, Hanel D, Knight JB, Tencer AF. Autograft Replacements for the
Scapholunate Ligament: A Biomechanical Comparison of Hand-based
Autografts. J Hand Surg [Am] 1999;24:963.
DJ, Ritt MJPF, Bos KE. Tarsal Autografts for Reconstruction of the
Scapholunate Interosseous Ligament: A Biomechanical Study. J Hand Surg [Am] 1999;24:968.
CJ, Taleisnik J, Cohen M. Treatment of Subacute and Chronic
Scapholunate Dissociation by Ligament Repair and Capsulodesis.
Presented at the 45th Annual Meeting of the American Society for
Surgery of the Hand, Toronto, Canada, September 24–27, 1990.
RL, Dobyns JH, Beabout JW, Bryan RS. Traumatic Instability of the
Wrist: Diagnosis, Classification and Pathomechanics. J Bone Joint Surg Am 1972;54:1612.
TW, Dobyns JH, Linscheid RL. Carpal Instability Non-dissociative.
Presented at the 45th Annual Meeting of the American Society for
Surgery of the Hand, Toronto, Canada, September 24–27, 1990.
Y, McMurtry RT, Flatt A E, Gillespie TG. Kinematics of the Wrist. I. An
Experimental Study of Radial-Ulnar Deviation and Flexion-Extension. J Bone Joint Surg Am 1978;60:423.

