Clavicle Fractures
individuals, especially those who participate in activities or sports
where high-speed falls (e.g., bicycling, motorcycles) or violent
collisions (e.g., football, hockey) are frequent, and they account for
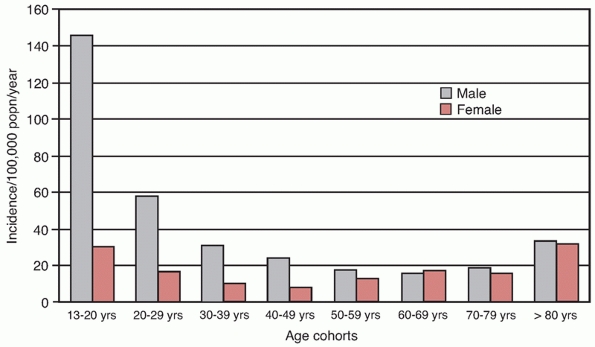
approximately 2.6% of all fractures.* In contrast to most fractures, Robinson137
reported in an epidemiologic study that the annual incidence in males
was highest in the under-20 age group, decreasing with each subsequent
age cohort (Fig. 36-1). The incidence in
females was more constant, with peaks seen in teenagers (e.g., sports,
motor vehicle accidents) and the elderly (e.g., osteoporotic fractures
from simple falls). The annual incidence of fractures in their
population was 29 per 100,000 population per year.137
in the midshaft of the bone, where the typical compressive forces
applied to the shoulder and the narrow cross section of the bone
combine and result in bony failure27,28,29,30,95,137,160 (Fig. 36-2).
Distal third fractures are the next most common type (20%), and
although they can result from the same mechanisms of injury as that
seen with midshaft fractures, they tend to occur in more elderly
individuals as a result of simple falls.52,138,140,141,169 Medial third fractures are the rarest (5%), perhaps because of the difficulty in accurately imaging (and identifying) them.150,163
One recent study of 57 such fractures reported that patients were
typically men in their fifth decade and that the usual mechanism of
injury was a motor vehicle accident.163 These authors also noted a relatively high (20%) associated mortality rate from concomitant head and chest injuries.
benign injury with an inherently good prognosis when treated nonoperatively.100,101,102,103,104
In a landmark 1960 study, Neer reported nonunion in only 3 of 2235
patients with middle-third fractures of the clavicle treated by a sling
or figure-of-eight bandage.100 Rowe144
showed an overall incidence of nonunion of 0.8% in 566 clavicle
fractures treated in a similar fashion. Thus, what was thought to be
the most serious complication following clavicular
fracture—nonunion—appeared to be extremely rare. Also, malunion of the
clavicle (which occurred radiographically on a predictable basis in
displaced fractures) was described as being of radiographic interest
only, with little or no functional consequences. This thinking
dominated the approach to clavicle fractures for decades.
 |
|
FIGURE 36-1
The epidemiology of clavicle fractures in Edinburgh, Scotland. (Adapted from Robinson CM, Court-Brown CM, McQueen MM, et al. Estimating the risk of nonunion following nonoperative treatment of a clavicle fracture. J Bone Joint Surg Am 2004;86A:1359-1365.) |
 |
|
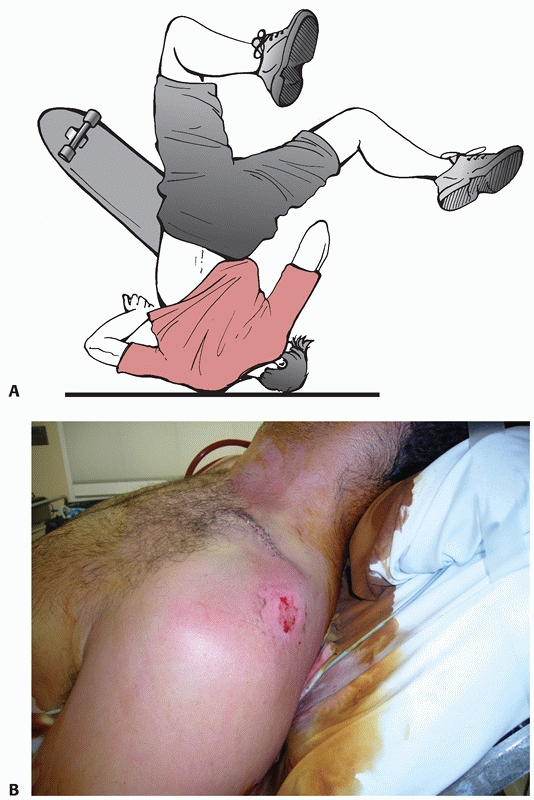
FIGURE 36-2 A. Mechanism of injury. Clavicle fractures are usually produced by a fall directly on the involved shoulder. B. Corresponding clinical photograph demonstrating posterior skin abrasion following displaced midshaft clavicle fracture.
|
the outcome of nonoperatively treated (especially displaced or
shortened) midshaft fractures is not as optimal as was once thought.* In 1997, Hill et al.62
were the first to use patient-oriented outcome measures to examine 66
consecutive patients with displaced midshaft clavicle fractures, and
they found an unsatisfactory outcome in 31%, as well as a nonunion rate
of 15%. In a metaanalysis of the literature from 1975 to 2005,
Zlowodzki et al.185 found that the
nonunion rate for nonoperatively treated displaced midshaft clavicle
fractures was 15.1%, exponentially higher than that previously
described (Table 36-1). Other recent epidemiologic and prospective studies have supported these findings.†
In addition, malunion of the clavicle has been clearly shown by
multiple authors to be a distinct clinical entity with characteristic
signs and symptoms that can be significantly improved by corrective
osteotomy.7,9,20,23,38,76,90,91
Potential explanations for the increased complication rate seen
following the nonoperative care of these fractures may be because of
changing injury patterns (especially from “extreme” sports such as
mountain-bicycling, snowboarding, and all-terrain vehicle riding),
increased expectations of the modern patient, comprehensive follow-up
(including patient-oriented outcome measures), and focusing on adults
(eliminating
children with their inherently good prognosis and remodeling potential).‡
|
TABLE
36-1 Metaanalysis of Nonoperative Treatment, Intramedullary Pinning, and Plate Fixation for Displaced Midshaft Fractures of the Clavicle From Series Published in 1975 through 2005 |
|||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||
complication rate have been reported from a variety of techniques for
primary fixation of displaced fractures of the clavicle, dispelling
some of the pessimism that surrounded prior studies where a poor
understanding of soft tissue handling, a selection bias of patients,
and inadequate implants combined to produce inferior results.§
Zlowodzki et al.’s metaanalysis showed a relative risk reduction of 86%
(from 15.1% to 2.2%) for nonunion with primary plate fixation compared
with nonoperative treatment.185
for, primary fixation of clavicle fractures, it is vital to remember
that the majority of these fractures can and should be treated
nonoperatively. The current research in this area should not provoke a
swing of the operative pendulum into indiscriminate fixation of all
clavicle injuries. Clinical and basic science research in this field
adds objective information to this topic and is directed at prompting a
thoughtful assessment of each injury based on these data and each
case’s individual merits such as the function and expectations of the
patient, the location of the fracture, and the degree of displacement
or comminution. Treatment is then based on this assessment, rather than
pursuing either a blanket condemnation of fixation or an unreasoning
rush to surgery.
common reported mechanism of injury that produces a midshaft fracture
of the clavicle.15,95,137,160
This can occur in a number of ways, including being thrown from a
vehicle or bicycle, during a sports event, from the intrusion of
objects or vehicle structure during a motor vehicle accident, or
falling from a height. A recent prospective trial of more than 130
completely displaced midshaft fractures of the clavicle identified
motor vehicle/motorcycle accidents, bicycling accidents,
skiing/snowboarding falls or collisions, sports injuries, and falls as
the most commonly involved mechanisms.15
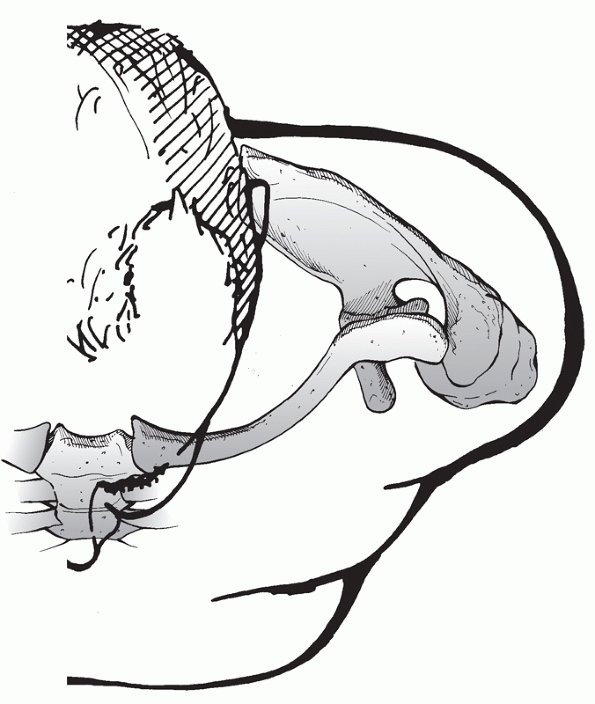
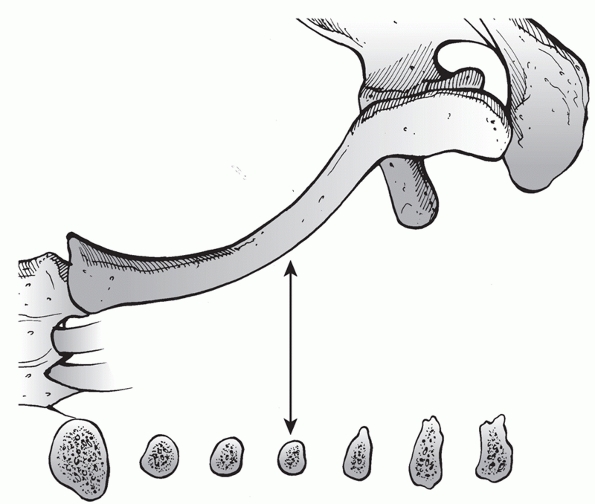
As the shoulder girdle is subjected to compression force directed from
laterally, the main strut maintaining position is the clavicle and its
articulations (Fig. 36-3). As the force exceeds
the capacity of this structure to withstand it, failure can occur in
one of three ways. The acromioclavicular (AC) articulation may fail,
the clavicle may break, or the sternoclavicular (SC) joint may
dislocate. SC injuries are rare and are typically associated with more
direct posterior blows against the medial clavicle (posterior
dislocations) or anterior blows to the distal shoulder girdle (levering
the proximal clavicle into an anterior dislocation).81,158
Presumably, there are subtle nuances of the direction and magnitude of
applied forces and local anatomy that dictate whether the failure
occurs in the AC joint, or in the clavicle, and the magnitude of
displacement that occurs. Most (85%) clavicle fractures occur in the
midshaft of the bone where, as can be seen in a cross section, the bone
is narrowest and enveloping soft-tissue structures (which may help
dissipate injury force) are most scarce.27,28,29,30,137,138
It is typical to see a large abrasion or contusion on the posterior
aspect of the shoulder in patients with displaced midshaft clavicular
fractures, especially those who fall from bicycles, motorcycles, or
other vehicles: this force vector may also contribute to the location
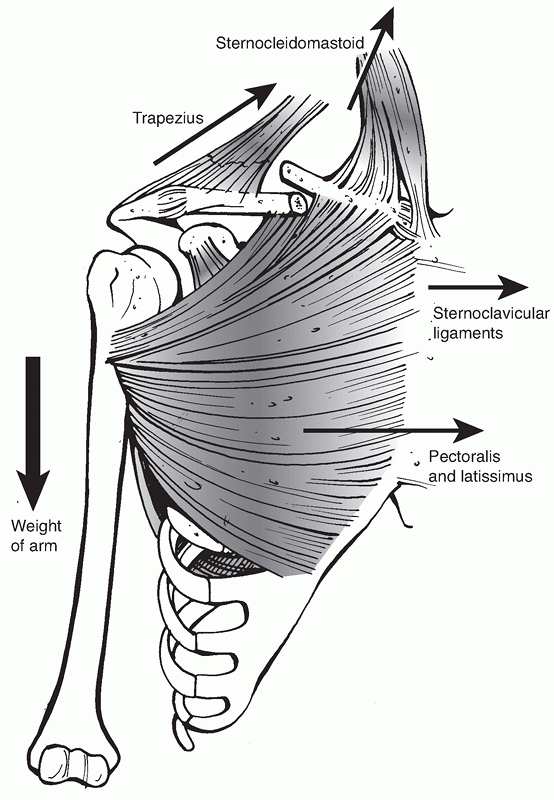
of the fracture. The direction of the initial deforming force and both
gravitational and muscular forces on the clavicle are significant and
result in the typical deformity seen after fracture, with the distal
fragment being translated inferiorly, anteriorly, and medially
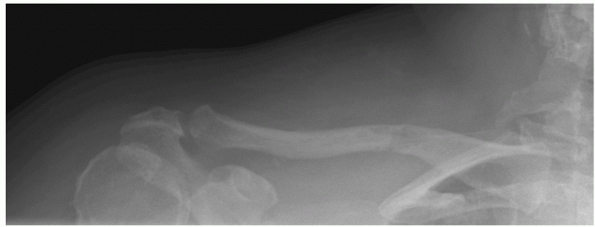
(shortened) and rotated anteriorly (Fig. 36-4).
produce a displaced fracture in a healthy young person but can result
in injury in elderly, osteoporotic individuals: these fractures are
typically seen in the distal third of the clavicle. If the mechanism of
injury is trivial and does not seem commensurate with the fracture
depicted, then a careful investigation for a pathologic fracture should
be performed30,157 (Fig. 36-5).
 |
|
FIGURE 36-3 The strut function of the clavicle, the only bony articulation between the axial skeleton and the upper limb.
|
 |
|
FIGURE 36-4
Muscular and gravitational forces acting on the clavicle with resultant deformity. The distal fragment is translated anteriorly, medially, and inferiorly and rotated anteriorly. This results in the scapula being protracted. |
 |
|
FIGURE 36-5
A 45-year-old previously well woman presented to the fracture clinic with shoulder pain following an episode of minor trauma. Radiographs revealed a fracture through a lytic lesion of the clavicle. This was the presentation of what subsequent investigation revealed to be a widely disseminated metastatic adenocarcinoma of unknown source. |
with fractures of the clavicle, compared with the incidence reported in
older traditional studies.36,40,41,89,162,183
There may be several reasons for this, including more liberal use of
improved diagnostic techniques (i.e., computed tomography [CT]
scanning), the greater speed and violence of many modern sports (e.g.,
motocross and snowboarding), and the improved survivorship of patients
with significant chest trauma who would have died before the
institution of comprehensive treatment of the trauma patient. In fact,
several studies from Level I trauma centers have examined the
characteristics of polytrauma patients with clavicle fractures and have
noted a high mortality rate (20% to 34%) from associated chest and head
trauma.89,162
Presumably, these series of critically injured patients contain
survivors who live to require treatment for the complications of their
clavicle fractures who may not have survived without modern trauma care.
vehicular trauma are more likely to have associated injures to the
thoracic cage, including ipsilateral rib fractures, scapular and/or
glenoid fractures, proximal humeral fractures, and
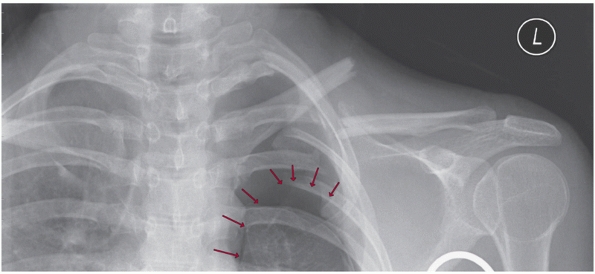
hemothoraces/pneumothoraces28,89,162 (Fig. 36-6).
In addition to simply being good medicine, identification of these
injuries is important for multiple reasons. Patients may require urgent
treatment directed specifically at the associated injury (i.e., tube
thoracostomy for pneumothorax), their presence may influence the
treatment of the clavicle fracture (i.e., an associated displaced
glenoid neck fracture, the “floating shoulder” [see later]), or (as
objective information on this entity increases) they may give an
indication of the likelihood of a negative outcome for the clavicle
fracture (malunion, nonunion) that may have implications regarding
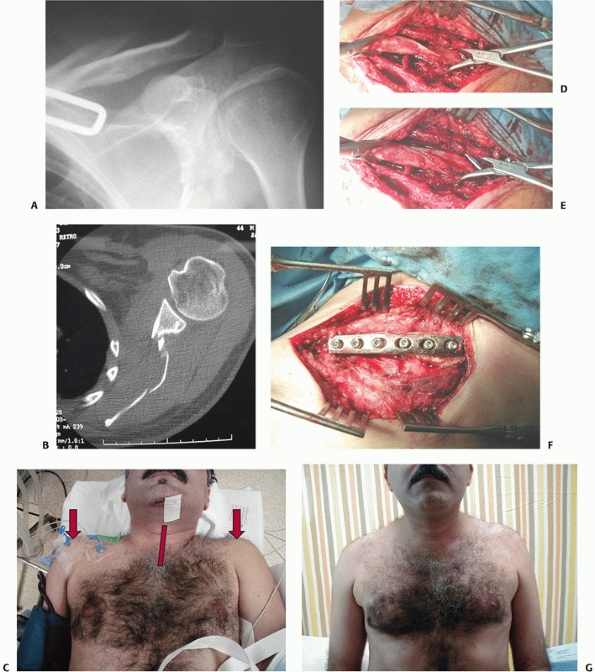
primary fixation (Fig. 36-7). The clavicle can also be injured from penetrating trauma including projectiles, blasts, and sword or machete blows (Fig. 36-8).
In this situation, diagnosing and treating underlying chest and/or
vascular injuries are critically important, and the clavicle can be
treated on its own merits.* However, if a vascular repair
has been performed, clavicular fixation (if possible) provides an
optimally stable environment for healing.
 |
|
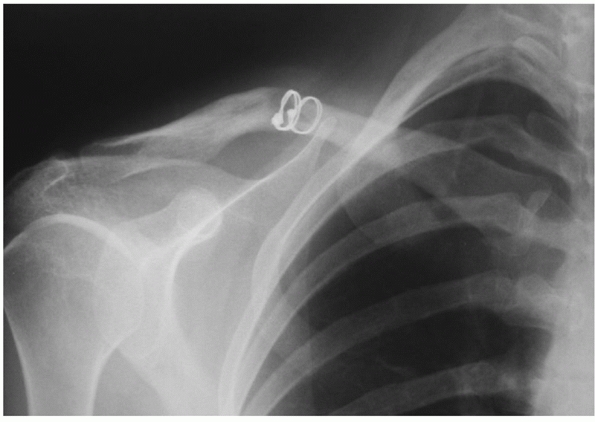
FIGURE 36-6
Anteroposterior radiograph of the clavicle in a 42-year-old man involved in a motor-vehicle collision. Associated injuries include multiple ipsilateral upper rib fractures, an ipsilateral pneumothorax (arrows outlining collapsed lung), and multiple lower extremity fractures. This patient has four relative indications for operative fixation: (i) the severe displacement of the clavicle fracture, (ii) the multiple upper rib fractures, which tend to destabilize the shoulder girdle, (iii) the associated lower extremity fractures and the resultant need for immediate upper extremity use, and (iv) the pneumothorax, which is indicative of the degree of trauma applied to the shoulder. |
optimize the patient’s care. In addition to the standard demographic
data, the details of the mechanism of injury are important. A clavicle
fracture caused by a simple low-energy fall is unlikely to be
associated with other fractures or intrathoracic injuries, whereas
a
fracture that occurs as a result of severe vehicular trauma or a fall
from a height should prompt a search for other injuries. In my
experience, clavicle fractures that result from falls while bicycling
often have associated multiple ipsilateral upper rib fractures. At a
Level I trauma center, McKee et al.89
studied 105 polytrauma patients (multiple system injury and Injury
Severity Score greater than 16) with fractures of the clavicular shaft
and found a mortality rate of 32%, mainly as a result of associated
head and chest injuries. This high incidence of associated head and
chest injuries mandates careful clinical and radiographic
investigation. The physical mechanism of injury is important: while the
majority of fractures will result from a blow to the shoulder, failure
of the bone can also occur from a traction-type injury. This usually
occurs in an industrial or a dockyard
injury
in which the involved arm is forcefully pulled away from the body as it
is caught in machinery. It can also occur in vehicular trauma when the
arm is pinned against or strikes a fixed object as the torso continues
past it. This can lead to scapulothoracic dissociation, as the shoulder
girdle fails in tension at the SC joint, the clavicle, or the AC joint.
This is evident on the radiographs when a completely displaced,
distracted fracture site is seen (as opposed to the typical overlapping
fracture fragments) (Fig. 36-9).
The high incidence of neurologic and vascular traction injuries seen in
this setting mandates further investigation (i.e., angiography),
because they can be limb threatening.29,36,54,99,122,183
 |
|
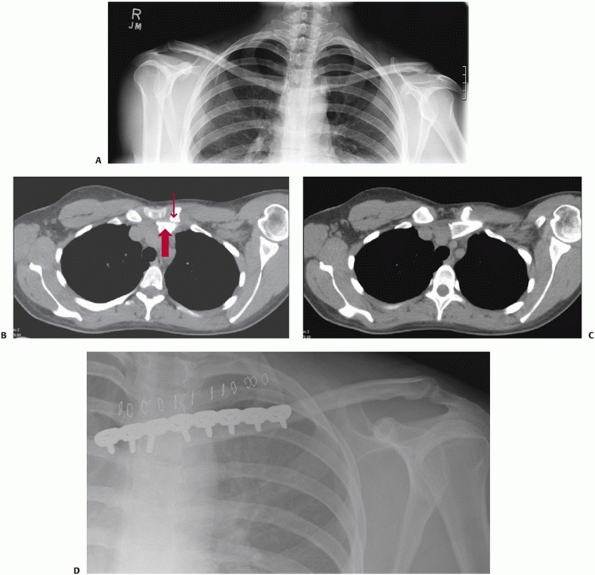
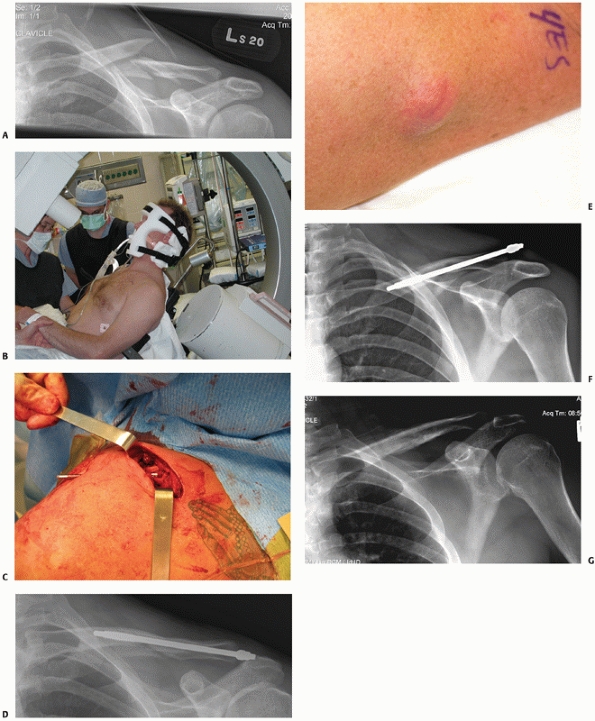
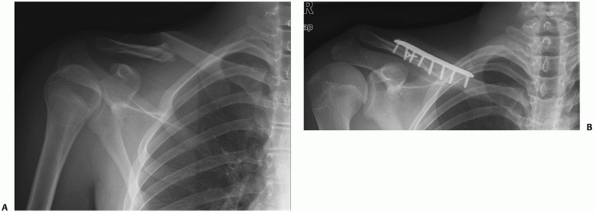
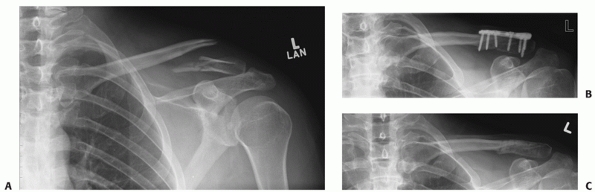
FIGURE 36-7 A “floating shoulder” injury. This patient was injured in a motor vehicle accident. A. Anteroposterior radiograph demonstrates a displaced, shortened left clavicle fracture. B. Computed tomography scan of the shoulder reveals a comminuted glenoid neck fracture. C. There is significant clinical deformity. D. Intraoperatively, the fracture is reduced with the aid of reduction clamps, and an anterior fixation plate is applied (E). Symmetry of the shoulder was restored by clavicle fixation alone (F), and it was not necessary to repair the glenoid fracture. G. There was an excellent clinical result with full restoration of motion and a Constant-Murley Shoulder Outcome Score of 95.
|
 |
|
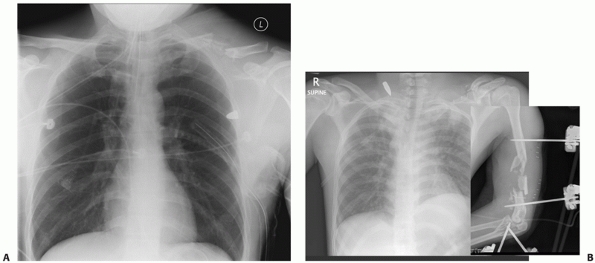
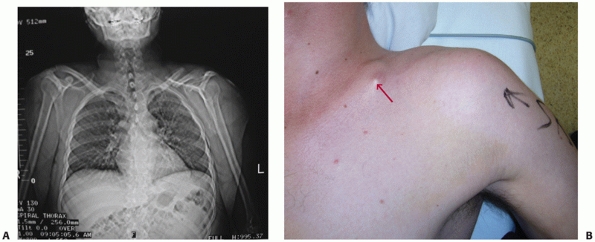
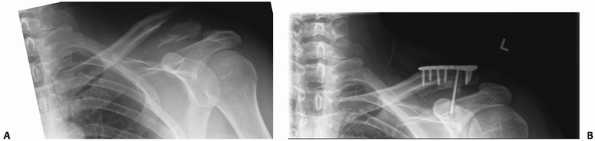
FIGURE 36-8 A.
Comminuted clavicle fracture resulting from a low-velocity gunshot wound with an associated hemopneumothorax and a retained intrathoracic bullet, treated with tube thoracostomy. The degree of clavicular deformity and the associated injuries represent a relative indication for operative repair. B. Severe injuries in a 25-year-old soldier struck by a high-velocity (AK-47) bullet that fractured the humerus, struck the clavicle, shattering the midportion, lacerated the subclavian vein and artery (causing life-threatening hemorrhage), and came to rest in the soft tissues of the neck. In an austere military operating environment, the clavicle fragments were resected and a vascular repair was performed. |
Metabolic processes that weaken bone (i.e., renal disease,
hyperparathyroidism), benign or malignant tumors (i.e., myeloma,
metastases), or pre-existing lesions (i.e., congenital pseudarthrosis
of the clavicle) can result in pathologic fracture. In this setting,
nonoperative treatment of the clavicle fracture is recommended
initially, while intervention is directed toward diagnosis and
treatment of the underlying condition. Once the primary diagnosis has
been made and treatment initiated, the clavicle fracture is treated
based on its individual aspects. Also, repetitive or unusual loads may
induce a stress fracture of the clavicle, typically in bodybuilders or
weightlifters.119,143,152
 |
|
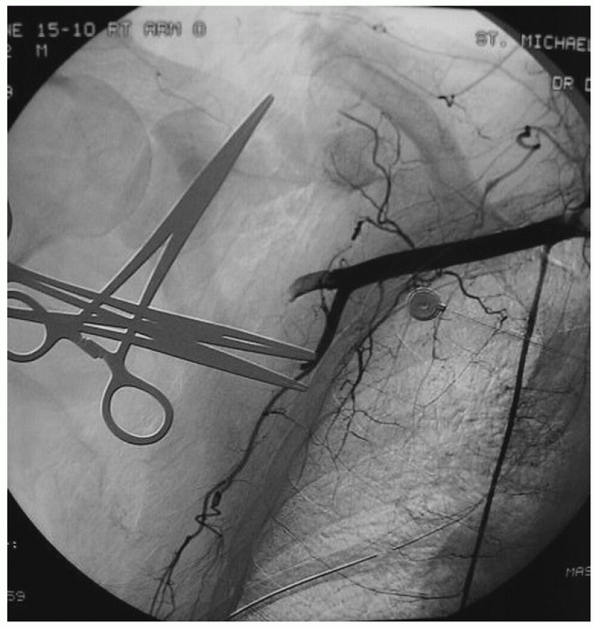
FIGURE 36-9
Emergency angiogram of a patient with scapulothoracic dissociation and wide distraction of a very distal clavicle fracture. There is an associated axillary artery avulsion, a complete brachial plexus injury, and multiple ipsilateral upper extremity fractures. |
fractures was consistently nonoperative, a detailed history of
lifestyle, occupation, and medical conditions was usually perfunctory
at best, since these factors did little to influence decision making.
However, there is increasing evidence that operative intervention is
superior in carefully selected cases of displaced clavicular shaft
fracture, such that additional information gleaned from the history
contributes to the risk/benefit analysis regarding possible surgery.
Compliant patients in the 16-to-60 age group, who have active
recreational lifestyles and/or physically demanding occupations
(especially those that require throwing, repetitive overhead work, or
recurrent lifting), are candidates for primary operative repair if they
are medically fit and have completely displaced fractures with good
bone quality.15,96,125,167,185
Factors associated with noncompliance and a high rate of fixation
failure, such as drug and alcohol abuse, untreated psychiatric
conditions, homelessness, or uncontrolled seizure disorders, are
contraindications for primary operative repair of clavicle fractures.10
majority of clavicle fractures, there was little emphasis placed on a
careful physical examination of the shoulder girdle. However, there are
a
number of findings that are important in surgical decision making.
There is usually swelling, bruising, and ecchymosis at the fracture
site, as well as deformity with displaced fractures. Visible deformity
of the shoulder girdle, best seen when the patient is standing, is an
important feature to recognize. The usual position seen with a
completely displaced midshaft fracture of the clavicle has been
described as shoulder “ptosis,” with a droopy, medially driven, and
shortened shoulder57,68,122,135 (Fig. 36-10).
In addition, the shoulder translates and rotates forward: this is a
deformity that can best be seen by viewing the patient from above.
Because of this malposition of the shoulder girdle, inspection of the
patient from behind may reveal a subtle prominence of the inferior
aspect of the scapula from scapular protraction as it moves with the
distal fragment. Shortening of the clavicle should be measured
clinically with a tape measure. A mark is made in the midline of the
suprasternal notch and another is made at the palpable ridge of the AC
joint: measuring this length gives the difference between the involved
and normal shoulder girdle.155
 |
|
FIGURE 36-10 A.
The “scout” portion of a computed tomography scan in a polytrauma patient with a displaced clavicle fracture demonstrates the typical deformity that occurs with these injuries. B. The corresponding clinical photograph demonstrates blanching of the skin over the medial fragment (arrow). |
involved limb is mandatory, especially if surgical intervention is
contemplated. If a deficit is not noted preoperatively, then it may be
incorrectly attributed to the surgery, which has prognostic,
medicolegal, and treatment implications.27,28,29,30
position, open fractures of the clavicle are relatively rare. Most open
fractures are associated with high-energy vehicular trauma, and
recognition is important for a number of reasons: the fracture itself
will require irrigation, debridement, and fixation, and there is a high
incidence of associated injuries. In the largest series in the
literature focusing on open clavicle fractures, Taitsman et al.
described 20 patients with this injury: 15 patients had pulmonary
injuries, 13 patients had head injuries, 8 patients had scapular
fractures, 11 patients had facial trauma, and there were a variety of
other injuries.162
sufficient to establish the diagnosis of a clavicle fracture. The
diagnosis may also be made from a single AP chest radiograph, which may
be the only available film in an urgent trauma setting. The chest
radiograph can also be used to evaluate the deformity of the involved
clavicle relative to the normal side and to look for associated
skeletal injuries such as rib, glenoid, and scapular fractures. A
measurement of length can be made on the chest radiograph comparing the
injured to the uninjured side: shortening of 2 cm or more represents a
relative indication for primary fixation. To best delineate a
clavicular fracture, as when one is determining whether operative
intervention is warranted, a radiograph should be taken in the upright
position (where gravity will demonstrate maximal deformity). Ideally,
the radiographic beam for the AP radiograph of the clavicle should be
angled 20 degrees superiorly to eliminate the overlap of the thoracic
cage and show the clavicle in profile.27,28,29,30,134,170
Also, if the torso is internally rotated a similar 20 degrees (rotating
internally when standing or by bumping up the opposite side while
supine), this places the scapula and shoulder girdle parallel to the
cassette for a true AP film. CT scanning of midshaft clavicular
fractures is rarely performed in the clinical setting, although this
imaging modality can demonstrate the complex three-dimensional
deformity that affects the shoulder girdle with these injuries,
including significant scapular angulation and protraction.57
It is also useful for evaluating fractures of the medial third of the
clavicle and the remainder of the shoulder girdle, such as the glenoid
neck in cases of a “floating shoulder.”42,130,142
AP radiographs. Centering the radiograph on the acromioclavicular joint
and angling the beam in a cephalic tilt of approximately 15 degrees
(the Zanca view) helps delineate the fracture well, by removing the
overlap of the upper portion of the thoracic cage.29,30
To accurately delineate the degree of fracture displacement, these
radiographs should be taken with the patient standing and the arm
unsupported by slings, braces, or the uninjured arm. On occasion, it
may be useful to obtain a stress view to determine the integrity of the
coracoclavicular ligaments (as this can influence the choice of
fixation): a 5- to 10-pound weight is suspended from the wrist of the
affected arm and then radiographs
are
taken. CT scanning of lateral clavicle fractures is rarely required
clinically but can be useful in selected cases to determine
intra-articular extension or displacement.
involving the SC joint, are notoriously difficult to accurately assess
with plain radiographs. CT scanning is the radiographic procedure of
choice when the anatomy of the fracture is unclear. This investigation
can help distinguish between a medial epiphyseal fracture (common in
individuals up to 25 years of age) and true SC dislocations29,150,163,181 (Fig. 36-11).
 |
|
FIGURE 36-11
Fractures of the medial end of the clavicle are difficult to visualize with conventional radiography. This 32-year-old female equestrian sustained a medial clavicle fracture following a riding accident when her horse fell on her. A. The anteroposterior radiograph reveals some asymmetry of the clavicles, but it is difficult to define the exact nature of the injury due to the overlap of bony axial structures and the spinal column. B. Computed tomography scan clearly demonstrates the medial fracture with a small residual medial fragment (small arrow) and posterior displacement of the shaft (large arrow), (C) impinging on the mediastinal structures. D. Plate fixation was performed, with extension of the plate onto the sternum due to the small size of the medial fragment. Once bony union has occurred (between 3 and 6 months), the plate should be removed. (Case courtesy of Dr. Jeremy A. Hall.) |
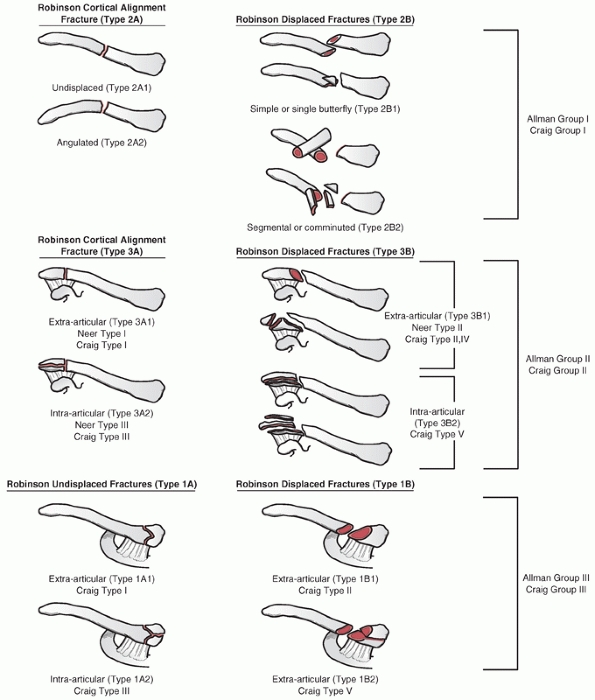
for fractures of the clavicle. These have traditionally been based on
the position of the fracture, with the groups originally divided by
Allman into proximal (group I), middle (group II), and distal (group
III) third fractures. This general grouping has the advantage of
corresponding to the clinical approach to these fractures of most
orthopaedic surgeons.29 Recognizing
that this basic scheme does not take into account factors that
influence treatment and outcome, such as fracture pattern,
displacement, comminution, and shortening, various authorities have
refined the classification to include other variables. Because of their
high rate of delayed and nonunion, Neer101
divided distal clavicle fractures into three subgroups, based on their
ligamentous attachments and degree of displacement (type II was
subsequently modified by Rockwood)29:
with a low rate of interobserver and intraobserver variability, should
help direct treatment, can be used to predict outcome, should be useful
in both the clinical and research realms, and should be simple enough
to be practically useful yet robust enough to include all fracture
patterns. While at the present time there is no classification scheme
that has been rigorously tested to meet all these objectives, modern
schemes based on prospective, comprehensive population-based studies
are available. Nordqvist et al.111
examined more than 2035 fractures of the clavicle over a 10-year period
and essentially expanded on Allman’s original scheme by adding subtypes
based on fracture displacement, including a comminuted category for
midshaft fractures. In a similar population-based study in Edinburgh,
Robinson137 evaluated more than 1000
consecutive fractures of the clavicle and developed a classification
scheme based on prognostic variables from the analysis of the data (Fig. 36-12).
It continues the traditional scheme of dividing the clavicle into
thirds and adds variables that are of proven diagnostic value
(intra-articular extension, displacement, and comminution). However, a
feature of this scheme is that it reverses the traditional numbering
scheme, describing medial fractures as type I, middle third fractures
as type II, and distal third fractures as type III. Because distal
third fractures are firmly entrenched in the orthopaedic lexicon as
“type II” fractures, this can lead to significant confusion. Despite
this drawback, the Robinson classification is based on an extensive
database that includes prospectively gathered, objective clinical data.
For this reason, it is the classification I prefer to use clinically as
it can help predict outcome and hence guide treatment, including the
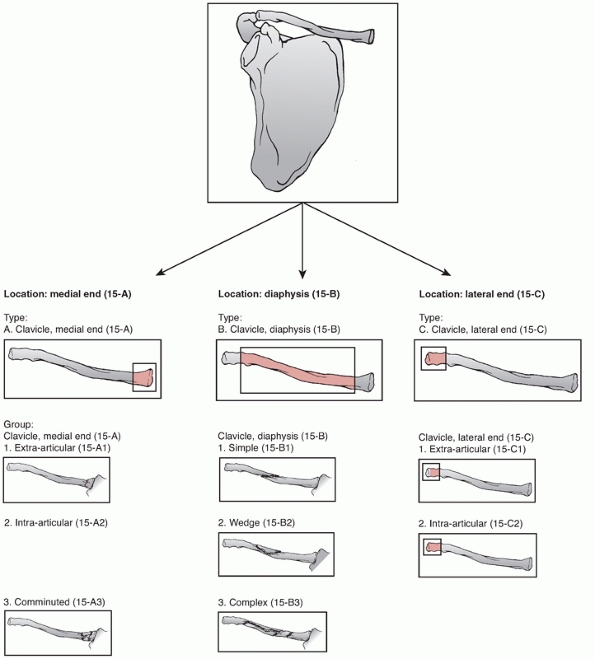
decision to operate and fixation methods chosen. The AO/OTA Fracture and Dislocation Classification Compendium
was updated in 2007 to include recent developments including a unified
numbering scheme and measures to improve observer reliability (Fig. 36-13).
The clavicle is designated as segment 15 and is divided into the
standard medial metaphyseal, diaphyseal, and lateral metaphyseal
fractures.85 An important difference
is that the metaphyseal fractures in this scheme are not one third of
the length of the bone but are shorter segments, according to the AO
“rule of squares.” For the all-important diaphysis, there are simple
(15-B1), wedge (15-B2), and complex (15-B3) subtypes.
medial and lateral expansions where it articulates with the sternum and
acromion, respectively (Fig. 36-14). It has two
distinct curves: the larger, obvious curve is in the coronal plane
giving the bone its characteristic “S” shape (medial end convex
anterior and lateral end concave anterior).95 There is also a more subtle superior curve delineated in a cadaver study by Huang et al.64
This milder superior bow had its apex laterally a mean of 37 mm from
the acromial articulation, with a mean magnitude of 5 mm. The medial
superior surface of the clavicle was found to be flat. This article
also described the fit of a precontoured clavicular plate to 100 pairs
of cadaver clavicles. The authors found that there were significant sex
and racial differences in the fit of the plate from best (black male
clavicles) to worst (white female clavicles). This article helps
explain why intraoperatively it often is necessary to adjust or contour
even “anatomic” plates for the clavicle to achieve an optimal fit.64
The bone in the relatively thin diaphysis is typically hard cortical
bone best suited for cortical screws, whereas the medial and lateral
expansions are softer cancellous bone where larger pitch cancellous
screws can be inserted without tapping.
joint, and the supporting soft tissue structures are correspondingly
thick. Medially, the clavicle is secured to the sternum by the SC
capsule, and although there are not easily demonstrable “ligaments,”
the thickening of the posterior capsule has been determined to be the
single most important soft tissue constraint to anterior or posterior
translation of the medial clavicle. There is also an interclavicular
ligament that runs from the medial end of one clavicle, gains purchase
from the superior aspect of the sternum at the sternal notch, and
attaches to the medial end of the contralateral clavicle. Acting as a
tension wire at the base of the clavicle, this ligament helps prevent
inferior angulation or translation of the clavicle. In addition, there
are extremely stout ligaments that originate on the first rib and
insert on the undersurface or the inferior aspect of the clavicle.18
A small fossa inferomedially, the rhomboid fossa, has been described as
an attachment point for these ligaments, which are primary resistors to
translation of the medial clavicle.
trapezoid (more lateral) and conoid (more medial), which are stout
ligaments that arise from the base of the coracoid and insert onto the
small osseous ridge of the inferior clavicle (trapezoid)
and
the clavicular conoid tubercle (conoid).These ligaments are very strong
and are the primary resistance to superior displacement of the lateral
clavicle. Their integrity, or lack thereof, plays an important role in
the decision making and fixation selection for the treatment of
displaced lateral third clavicle fractures. Clavicle fractures in this
location will often have an avulsed inferior fragment to which these
ligaments are attached, especially in younger individuals. Inclusion of
these fragments in surgical fixation selection enhances the stability
of the operative repair. The capsule of the AC joint is thickened
superiorly and is primarily responsible for resisting AP displacement
of the joint. It is important to repair this structure, which is
usually reflected surgically as part of the deep myofascial layer, when
operating on the lateral end of the clavicle. If one is inserting a
hook plate for fixation of a very distal fracture, a small defect can
be made in the posterolateral aspect of the capsule for insertion of
the hook portion into the posterior subacromial space.22,39,75,169,182
 |
|
FIGURE 36-12 Robinson classification scheme of clavicle fractures.
|
 |
|
FIGURE 36-13 AO/OTA classification scheme of clavicle fractures.
|
of muscle origin but still serves as the attachment site of several
large
muscles.
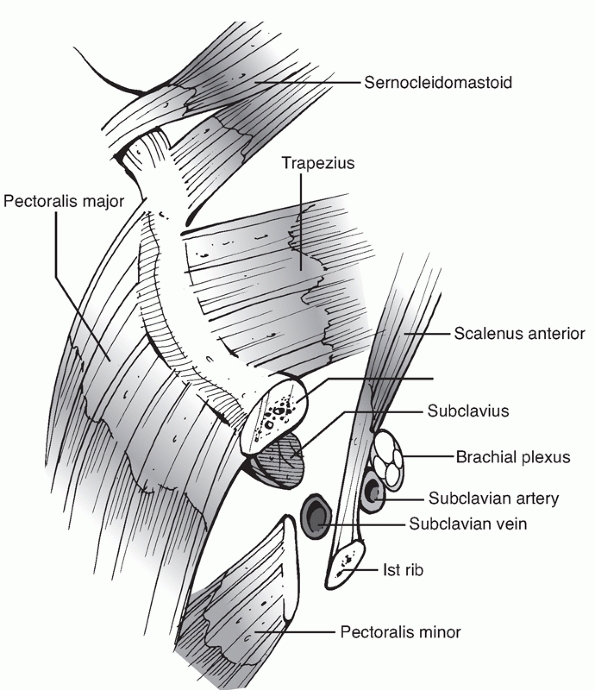
Medially, the pectoralis major muscle originates from the clavicular
shaft anteroinferiorly, and the sternocleidomastoid originates
superiorly. The pectoralis origin merges with the origin of the
anterior deltoid laterally, while the trapezius insertion blends
superiorly with the deltoid origin at the lateral margin (Fig. 36-15).
Muscle attachment plays a significant role in the deformity that
results after fracture: the medial clavicular fragment is elevated by
the unopposed pull of the SC muscle, while the distal fragment is held
inferiorly by the deltoid and medially by the pectoralis major. The
undersurface of the clavicle is the insertion site of the subclavius
muscle, which is of little significance functionally but serves as a
soft tissue buffer in the subclavicular space superior to the brachial
plexus and subclavian vessels. The platysma, or “shaving muscle,” is
variable in terms of thickness and extent but usually envelopes the
anterior and superior aspects of the clavicle and runs in the
subcutaneous tissues, extending superiorly to the mandible and deeper
facial muscles. It is divided during the surgical approach and is
typically included in the closure of the superficial, or
skin/subcutaneous, layer.
 |
|
FIGURE 36-14
The cross-sectional and topographic anatomy of the clavicle. The clavicle is narrowest in its midportion, explaining the high incidence of fractures in this area. |
C3 and C4 and exit from a common trunk behind the posterior border of
the sternocleidomastoid muscle. There are typically three major
branches (anterior, middle, and posterior) that cross the clavicle
superficially from medial to lateral and are at risk during surgical
approaches. If they are divided, an area of numbness is typically felt
inferior to the surgical incision, although this tends to improve with
time. A more difficult problem can be the development of a painful
neuroma in the scar, which, although rare, can negatively affect an
otherwise good surgical outcome. For this reason, some authorities
recommend identification and protection of these nerves during
operative repair.69,70,154
More vital neurovascular structures lie inferior to the clavicle. The
subclavian vein runs directly below the subclavius muscle and above the
first rib, where it is readily accessible (for central venous access)
and vulnerable (to inadvertent injury). More posteriorly lie the
subclavian artery and the brachial plexus, separated from the vein and
clavicle by the additional layer of the scalenus anterior muscle
medially. The plexus is closest to the clavicle in its midportion,
where the greatest care needs to be taken in not violating the
subclavicular space with drills, screws, or instruments. Despite the
proximity of these vital structures, iatrogenic injury is surprisingly
rare (see later).
applicable to the fixation of clavicle fractures, each with its own
advantages and disadvantages, as follows:
Its advantages include a general familiarity with this approach in most
surgeons’ hands, the ability to extend it simply to both the medial and
lateral ends of the clavicle, and clear radiographic views of the
clavicle postoperatively. Its disadvantages include the trajectory of
screw placement (from superior to inferior),
which
can be difficult, and inadvertent “plunging” with the drill, which can
place the underlying lung and neurovascular structures at risk. Also,
the clavicle is fairly narrow in its superoinferior dimension, and
typically the length of screws inserted ranges from 14 to 16 mm in
females to 16 to 18 mm in males. In thin individuals, hardware
prominence can be problematic and may lead to hardware removal. The
surgical approach and technique are detailed later (see “Authors’ Preferred Method of Treatment”).
 |
|
FIGURE 36-15
Applied anatomy of the clavicle. Anterosuperiorly, the pectoralis major muscle and fascia envelope the medial 60% of the clavicle, while the lateral 40% is covered by the deltoid muscle and its fascia. Posterosuperiorly, the trapezius muscle attaches to the clavicle. |
Advantages of this technique include an easier screw trajectory with
less likelihood of serious injury with inadvertent overpenetration of
the drill (although the incidence of iatrogenic nerve injury is very
low), the ability to insert longer screws in the wider AP dimension of
the clavicle, and decreased hardware prominence. It is also technically
easier to contour a small-fragment compression plate along the anterior
border as opposed to the superior surface: however, the advent of
precontoured plates has largely negated this particular advantage.
Collinge et al. reported on the use of this technique in 58 patients
and described one fixation failure, one nonunion, three infections, and
only two hardware removals.25
Potential disadvantages of this technique include the lack of general
familiarity with the approach and that the plate tends to obscure the
fracture site radiographically. Also, although there remains some
controversy on the matter, biomechanical studies have in general shown
that the most advantageous position for plate placement is the superior
surface.
supine position with a bump or pad between the scapulae to help restore
length and improve exposure. The arm can be free-draped to aid in
fracture reduction. The skin incision is centered over the fracture
site along the inferior palpable edge of the clavicle, roughly in a
line drawn from the sternal notch to the anteroinferior aspect of the
AC joint. As experience with the technique grows, a smaller skin
incision and extensive subcutaneous mobilization for exposure are
possible. Any identifiable supraclavicular nerves are protected, and
the clavipectoral fascia is incised and reflected inferiorly. The
fracture site is identified, cleaned, and reduced with reduction
forceps. A lag screw(s) is placed if possible, or the fracture can be
temporarily secured with K-wires. Following this, fixation proceeds
with the chosen plate being contoured to fit along the anteroinferior
surface of the clavicle. Since the contouring of the plate is performed
in the long axis of the plate, it is much simpler to contour a straight
compression plate to the anterior, as opposed to the superior surface (Fig. 36-16).
Additionally, it is usually possible to place screws that are 2 to 4 mm
longer in the AP dimension of the clavicle. Following fracture
fixation, a two-layer soft tissue closure is performed in as standard
fashion. Postoperative care is similar to that instituted following
anterosuperior plating.
clavicle.93 This resource summarizes the available objective evidence about recommendations for the optimal treatment of these injuries (Table 36-2). The grades of recommendation are as follows:
 |
|
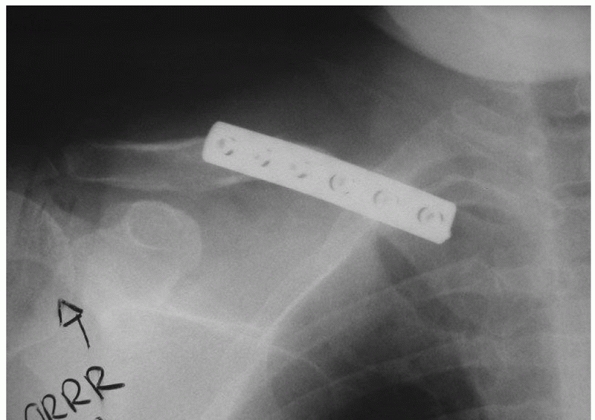
FIGURE 36-16
Anteroinferior plating of the clavicle with a conventional 3.5-mm compression plate. It is much simpler to contour a conventional straight plate in this plane compared with superior placement. |
(high-quality prospective, randomized clinical trials [RCTs] with
consistent findings) recommending for or against intervention
(lesser-quality RCTs, prospective comparative studies, case-control
series) recommending for or against intervention
the treatment of clavicle fractures, most tend to be retrospective
reviews, although there are an increasing number of prospective and/ or
randomized trials being published.15,61,68,139 My personal recommendations for treatment must be considered in light of the evidence available in Tables 36-1 and 36-2.
|
TABLE 36-2 Recommendations for the Optimal Treatment of Displaced Midshaft Fractures of the Clavicle
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||
good results following nonoperative treatment of clavicle fractures,
and it is my opinion that the majority of clavicle fractures can, and
should, be treated in this fashion.3,40,47,72,100,144
However, there are serious deficiencies in these reports, including the
inclusion of children (who have an intrinsically good result and
remodeling potential), large numbers of patients lost to follow-up, and
radiographic and/or surgeon-based outcomes that are insensitive to
residual deficits. Recent evidence from prospective and randomized
clinical trials has suggested that there is a subset of individuals who
benefit from primary operative care15,61,68,125,139,172 (Fig. 36-17).
Operative repair in this setting should be reserved for medically well,
physically active patients who stand to benefit the most from a rapid
restoration of normal anatomy and stable fixation. There are multiple
potential indications for primary operative fixation, outlined in Table 36-3.
displaced midshaft fracture of the clavicle was recorded in the “Edwin
Smith” papyrus dating from the 30th century B.C. Hippocrates described
the typical deformity resulting from this injury and emphasized the
importance of trying to correct it.1
It is usually possible to obtain an improvement in position of the
fracture fragments by placing the patient supine, with a roll or
sandbag behind the shoulder blades to let the anterior displacement and
rotation of the distal fragment correct with gravity, followed by
superior translation and support of the affected arm. Unfortunately, it
is difficult or impossible to maintain the reduction achieved. For this
reason, over the millennia that followed the first description of
treatment of this fracture, there have been hundreds of descriptions of
different devices designed to maintain the reduction, including
splints, body jackets, casts, braces, slings, swathes, and wraps.1,3,16,27,87
At the present time, there is no convincing evidence that any of these
devices reliably maintains the fracture reduction or improves clinical,
radiographic,
or
functional outcomes. For many years, the standard of care in North
America was the “figure-of-eight” bandage: Andersen and colleagues3
examined its utility in a prospective, randomized, controlled clinical
trial comparing it to a simple sling in 60 patients. They could
demonstrate no functional or radiographic difference between the two
groups, and in general the patients preferred the sling (2 of 27
dissatisfied with the sling compared with 9 of 34 dissatisfied with the
figure-of-eight bandage, P = 0.09). In a retrospective review of 140 patients treated nonoperatively, Stanley and Norris159 did not find any difference between a standard sling and a figure-of-eight bandage, a finding confirmed by other authors.123,124
Also, I have seen several temporary lower trunk brachial plexus palsies
from figure-of-eight bandages that resulted from overtightening. For
this reason, in my practice, if nonoperative care is selected, a
simple, conventional sling with a padded neckpiece is applied, and no
attempt at reduction is made.
 |
|
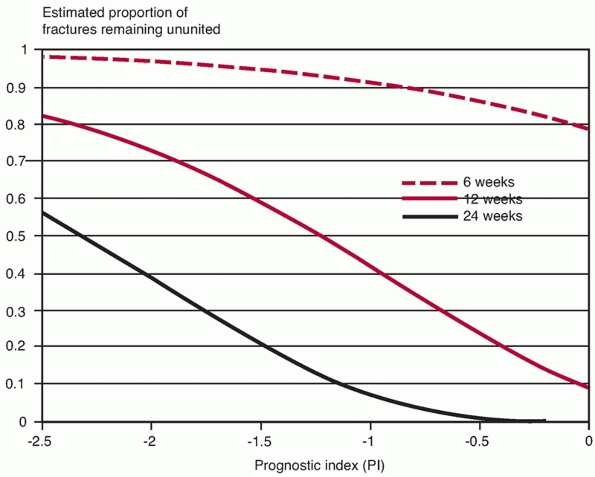
FIGURE 36-17
Probability of nonunion at various time points following a midshaft clavicle fracture. The PI (Prognostic Index) decreases with each of the following factors: increasing age, increasing comminution, increasing displacement, and female sex. (Adapted from Robinson CM, Court-Brown CM, McQueen MM, et al. Estimating the risk of nonunion following nonoperative treatment of a clavicle fracture. J Bone Joint Surg Am 2004;86A:1359-1365.) |
|
TABLE 36-3 Relative Indications for Primary Fixation of Midshaft Clavicle Fractures
|
||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||
This method takes advantage of the intrinsic healing ability of the
clavicle and allows restoration of length and translation without the
scarring or morbidity of a surgical approach. Also, there is no
retained hardware at the conclusion of treatment. Schuind et al.148
reported on a series of 20 patients treated with external fixation for
clavicular injuries, many of whom had local soft tissue compromise;
union occurred in all. Tomic et al.164
described the treatment of 12 patients with nonunion of the clavicular
shaft by application of a modified Ilizarov device. Union was achieved
in 11 of 12 patients with an increase in the mean Constant-Murley
Shoulder Outcome Score from 30 preoperatively to 69 postoperatively. It
is clear that this technique is technically possible to perform and may
be useful in certain specific situations. Unfortunately, the practical
difficulties associated with the position and prominence of the
fixation pins, coupled with a lack of patient acceptance in the North
American population, has resulted in minimal use of this technique.
the clavicle has several advantages. These are similar to the benefits
seen with IM fixation of long bone fractures in other areas, although
this technique had not been as consistently successful in the clavicle as series in the femur or tibia have reported.8,29,45,48,56,67,94
Advantages include a smaller, more cosmetic skin incision, less soft
tissue stripping at the fracture site, decreased hardware prominence
following fixation, technically straightforward hardware removal, and a
possibly lower incidence of refracture or fracture at the end of the
implant. Recently, modifications to the technique have included a
radiographically guided completely “closed” technique.24
Since, at the present time, there is no consistently reliable way to
“lock” an IM clavicle pin, complications include those common to all
unlocked IM devices, namely failure to control axial length and
rotation, especially with increasing fracture comminution and
decreasing intrinsic fracture stability. A biomechanical study of
clavicular osteotomies by Golish et al.53
comparing 3.5-mm compression plates to 3.8-mm or 4.5-mm IM pins showed
that the plated constructs were superior in resisting displacement in a
number of different testing modes (maximal load, cyclical stress)
compared with both IM nail constructs.
semisitting position on a radiolucent table, with an image intensifier
on the ipsilateral side. By rotating the image 45 degrees caudal and
cephalad, orthogonal views of the clavicle can be obtained. A small
incision is then made over the posterolateral corner of the clavicle 2
to 3 cm medial to the AC joint (Fig. 36-18).
The posterior clavicle at this point is identified and the canal
breached with a drill consistent with the planned fixation device. A
reduction of the fracture is then performed, either through a small
open incision or, as experience increases, in a completely closed
fashion using a percutaneous reduction clamp on the medial fragment and
a “joystick” in the proximal fragment. Alternatively, the fixation
device can be inserted using a “retrograde” technique where it is
passed out from the fracture site through the lateral fragment. The
fracture is then reduced and the IM device is inserted into the medial
fragment under direct vision. It is important to accurately reduce
length and rotation, although the latter can be quite difficult if done
closed and no visual clues from the fracture configuration are
available. A small incision may be necessary to reduce vertically
oriented comminuted fragments and “tease” then back into alignment.
Following this, the canal is drilled to the appropriate size to accept
the planned IM device. Options include headed pins, partially threaded
pins or screws, cannulated screws, and smooth wires. Although some
series report favorable results with smooth wires, the North American
experience with smalldiameter smooth pin fixation includes breakage and
migration and is, in general, dismal.78,83,97,108
Smooth wires are contraindicated for fracture fixation about the
shoulder in general and for the clavicle in particular. It is important
not to distract the fracture site with the fixation device, which can
occur as the pin is inserted into the unyielding opposite cortex as the
S-shaped clavicle comes into contact with the end of the straight pin.
If this occurs, the pin must be withdrawn slightly or a shorter pin
used. The head of the pin or screw can be left prominent to facilitate
early removal through a small posterior incision or can be left flush
with the bone to decrease soft tissue irritation (Fig. 36-19).
Some authors advocate leaving the pin in a prominent position
subcutaneously for easy access in the clinic at the time of early (7 to
8 weeks postoperatively) hardware removal. This step depends on the
type of fixation device used and the philosophy of the treating
surgeon. The incisions are closed in a fashion similar to that used for
plate fixation, although they are typically smaller. If the surgeon is
confident with the stability of the repair, early motion is instituted
similar to that performed following plate fixation.
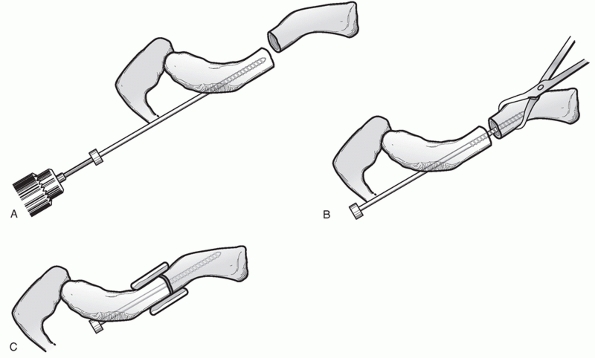 |
|
FIGURE 36-18 Intramedullary fixation with a headed, distally threaded pin (modified Haigie pin). A. Retrograde drilling of the distal fragment. B. Reduction and fixation of the fracture. C. Addition of bone graft or bone graft substitute.
|
 |
|
FIGURE 36-19 A. Comminuted, displaced, midshaft fracture of the clavicle. B. Photograph showing the operative setup with the image intensifier in place. C. Small incision is made and the fracture is reduced in an open fashion followed by retrograde insertion of the pin. D. Postoperative radiograph revealing reduction of the fracture. E. Radiograph demonstrating bony union. F. Skin irritation over prominent pin. G. Follow-up radiograph following uneventful union and pin removal. (Case courtesy of, and copyright by, Dr. David Ring.)
|
of operative repair of a midshaft clavicle fracture, it is important to
remember that the majority of midshaft fractures can be treated
nonoperatively. A careful physical examination (see earlier) is
mandatory to rule out other injuries, which may influence the
anesthetic (i.e., an ipsilateral pneumothorax) or the surgery (damaged
skin or deficient soft tissue, neurovascular injury). The skin in this
area is typically bruised, with extensive swelling, following a
displaced midshaft fracture. Since the difficulty of reduction and
fixation does not increase until approximately 2 weeks following
injury, it may be prudent to delay operative intervention (as one would
in other areas) until the soft tissue in the vicinity of the planned
surgical approach is more robust. Radiographs of the injured clavicle
are usually sufficient. The surgeon should observe the severity of the
displacement, the number of fracture fragments, and the location of the
main fracture line (Fig. 36-20). There is often
a vertically oriented anterosuperior fragment, which may benefit from
lag screw fixation, and mini-fragment screws should be available as
this fragment may
be
quite narrow. Also, the number of screws that can be potentially placed
into the distal fragment can be determined preoperatively, so that the
appropriate plate can be available. Older series describing fixation of
clavicle fractures have described poor results when inadequate fixation
such as cerclage wires alone or plates of inadequate size or length are
used100,102,127,144 (Figs. 36-21 and 36-22).
A fixation set that includes plates that are precontoured, or
“anatomic,” to fit the “S” shape of the clavicle is ideal. Although
these plates may require some intraoperative adjustments, they
typically save significant time associated with the extensive
contouring required to make a straight plate fit the bone. They help to
decrease the soft tissue irritation that occurs when the end of a
straight plate protrudes past the end of the bone as the clavicle
curves away.
 |
|
FIGURE 36-20 A.
Anteroposterior radiograph of a displaced midshaft clavicle fracture. Note the difference in diameter of the proximal and distal fragments at the fracture site, suggesting that a significant degree of rotation has occurred. B. Intraoperative photograph of a displaced fracture, (C) reduced anatomically and held with a small fragment reduction forceps. D. Postoperative radiograph after open reduction and internal fixation with an anterior-to-posterior lag screw followed by fixation with an anatomic plate. |
 |
|
FIGURE 36-21
Cerclage wiring in isolation is inadequate to control the deforming forces at the site of a displaced clavicle fracture. It results in all of the risks of surgical intervention with few of the benefits and is to be avoided. |
 |
|
FIGURE 36-22
Anteroposterior radiograph of a 35-year-old man who weighed more than 200 pounds, whose clavicle nonunion was fixed with a 3.5-mm pelvic reconstruction plate. Early mechanical failure occurred through deformation of the plate. This type of plate may be suitable for smaller, low-demand individuals but has a higher failure rate when used in larger, more physically active patients, especially given the current availability of stronger, precontoured plates. |
semisitting position on a regular operating room table with an attached
foot-piece to support the legs. It has not been routinely necessary to
use special tables or positioners. The head is placed on a round
support and, if general anesthesia is to be used, the endotracheal tube
is taped to the opposite side. The arm does not need to be free-draped
for isolated injuries and is usually padded and strapped to the
patient’s side. It is helpful to place a small pad behind the involved
shoulder to elevate it and check to ensure that the anticipated
superior drill trajectory is free from obstruction. This is less of a
concern if an anteroinferior plate application is chosen.
technique because of the simplicity of the surgical approach, the
wellproved clinical record of superior plate application, and several
biomechanical studies that have suggested that the optimal location for
plate placement is superior.55,66
An oblique skin incision is made centered superiorly over the fracture
site. The subcutaneous tissue and platysma muscle are kept together as
one layer and extensively mobilized, especially proximally and
distally. As experience with the technique increases, a smaller
incision using “minimally invasive” principles can be used. Care is
taken to identify, isolate, and protect any visible, larger branches of
the supraclavicular nerves: smaller ones may need to be divided. It is
usually wise to warn patients that they may experience some numbness
inferior to the incision, which will typically improve with time. The
myofascial layer over the clavicle is incised and elevated in one
contiguous layer. Therefore, at the conclusion of the procedure,
fracture site, and plate coverage are enhanced by having two soft
tissue layers (skin/subcutaneous tissue, myofascial layer) to close.
Care is taken to preserve the soft tissue attachments to any major
fragments, especially the vertically oriented fragment of the
anterosuperior clavicle that is often seen. It is not necessary to
completely denude these fragments to reduce them.
identified and cleaned of debris and hematoma, and a fixation strategy
is formulated. If there is a free fragment of sufficient size to be
structurally important (one third of the clavicle circumference or
greater), it can be reduced to the proximal or distal clavicle from
which it arose and fixed with a lag screw, simplifying the fracture to
a simple pattern (Fig. 36-23). The proximal and
distal fragments are then reduced with the aid of reduction forceps;
they can be held temporarily with a K-wire or, ideally, with a lag
screw. A precontoured plate of sufficient length is then applied to the
superior surface. If a lag screw has been placed, then it is usually
sufficient to secure the fracture with three bicortical screws (six
cortices) both proximally and distally. If it is not possible to place
a lag screw, then four screws should be inserted proximally and
distally. If the main fracture line is of a stable configuration,
compression holes can be used to apply compression. If the fracture is
comminuted or of an unstable pattern, then the plate should be applied
in a “neutral” mode.
Care
must be taken not to violate the subclavicular space and the vital
structures therein. If there is any concern intraoperatively about
violation of the pleural space, a Valsalva maneuver should be performed
to identify any leakage of air.
 |
|
FIGURE 36-23 A.
Displaced midshaft fracture of the clavicle in a 16-year-old boy, with abrasion and tenting of the skin, approximately 2.5 cm of shortening, and an obvious clinical deformity. B. The intervening fragments were fixed with a lag screw followed by plate fixation. Prompt, anatomic healing occurred, as might be expected in an adolescent. |
young active patients with high quality bone, and for this reason screw
purchase is usually excellent, especially in the cortical area.
Although there has been increasing interest in the use of locking-plate
technology in this area, there have been few reports on this technique
in the clavicle. Celestre et al.19
reported that a superiorly placed locking plate was biomechanically
superior to a conventional compression plate, although there is little
clinical information regarding their use at the present time. One small
retrospective series described their use in recalcitrant clavicular
nonunions: all 11 fractures eventually healed. I have not found that
locking plates are routinely necessary for the fixation of clavicle
fractures, and I have no experience with them. Following fixation, it
is important to close both soft tissue layers with interrupted,
nonabsorbable sutures. Postoperative radiographs are taken in the
recovery room.
basis. Postoperatively, the arm is placed in a standard sling for
comfort and gentle pendulum exercises are allowed, and the patient is
seen in the fracture clinic at 10 to 14 days postoperatively. The wound
is checked and radiographs are taken. The sling is discontinued, and
unrestricted range-of-motion exercises are allowed, but no
strengthening, resisted exercises or sporting activities are allowed.
At 6 weeks postoperatively, radiographs are taken to ensure bony union.
If acceptable, the patient is allowed to begin resisted and
strengthening activities. If delayed union is evident, then more
aggressive activities are avoided. It is generally advised that contact
(football, hockey) and/or unpredictable (mountain biking, snowboarding)
sports be avoided for 12 weeks postoperatively. However, compliance in
this predominantly young, male population is variable and many
individuals return to such activities earlier than recommended.
and hardware prominence following plate fixation is a clinical concern.
Previously, prior to the advent of plates specifically designed for the
clavicle, it was often necessary to contour a straight compression
plate to fit the bone by twisting the plate on its long axis so that
the plate faced the bone as the underlying clavicle curved away from it.88,96
In addition to making screw placement difficult, this led to undue
prominence of the ends of the plate and a high incidence of subsequent
plate removal. With the current availability of stronger, curved,
low-profile plates, symptomatic prominence of the plates is much lower
and routine plate removal is not typically required.
-
Patient selection is critical: operative
intervention is reserved for young, healthy, physically active patients
with good bone quality and completely displaced fractures who stand to
benefit most from operative fixation with an intrinsically low
complication rate. -
Noncompliance and substance abuse (be it
alcohol, illicit drugs, or prescription narcotics) are
contraindications to surgical intervention. No clavicular fixation is
strong enough to withstand an unprotected fall down stairs or a
physical altercation in the immediate postoperative period.47,125,126 -
Clinically, a visibly deformed shoulder on inspection usually corresponds to a minimum of 2 cm of shortening radiographically (Fig. 36-24).
-
It is critical to develop, protect, and
securely close the two soft tissue layers. The superficial layer is the
skin and subcutaneous tissue, and the deep layer is the deltotrapezial
myofascial layer. This helps protect against deep infection and ensures
plate coverage if there is a superficial infection. -
Comminuted fragments, especially the
vertically displaced anterosuperior fragment often seen, should be
gently “teased” back into position, maintaining soft tissue
attachments. They can be secured with mini- or small-fragment screws.
Reduction is important but not at the cost of denuding all of soft
tissue attachment (Fig. 36-25). -
While typically it is not necessary to
dissect in the subclavicular space to place protective retractors, it
is very important not to
P.1127“plunge”
into this area with drills or taps. If a lung injury is suspected
intraoperatively, the wound is filled with saline and the anesthetist
performs a Valsalva maneuver. The presence of air escape indicates
pleural injury and should prompt a chest radiograph and consultation
for pleural drainage (catheter or chest tube). -
A plate of size and strength commensurate
with the patient’s size and compliance should be used. In general,
3.5-mm compression plates or precontoured plates are ideal, especially
for larger individuals (>150 pounds) or those who will rehabilitate
aggressively.
 |
|
FIGURE 36-24
The typical clinical deformity following a displaced left midshaft clavicular fracture with a short, droopy, “ptotic” shoulder with anterior translation and rotation of the distal fragment and limb. |
clavicle and planned operative site is important. As with midshaft
fractures, temporizing until the soft tissue status improves may be
prudent. The major technical challenges in these injuries are purchase
in the distal fragment and resisting the primary displacing forces,
which draw the proximal fragment superiorly and the distal fragment
(secured by the AC and coracoclavicular ligaments to the coracoid and
scapula) inferiorly.4,22,39,71,75,116
Also, the cancellous bone of the distal fragment may be inferior in
quality to that of the shaft, and there may be unrecognized
comminution. The treating surgeon should template the fracture
preoperatively to determine the number of screws that will have
purchase in the distal fragment: there are a number of precontoured
“anatomic” plates available for this purpose. If it is anticipated that
there will be insufficient distal purchase, then alternative fixation
strategies need to be considered. These can include augmenting fixation
into the coracoid process or achieving purchase to or under the
acromion. In this instance, theuse of a hook plate (a precontoured
plate with a projection or “hook” that is inserted posteriorly in the
subacromial space) can be extremely useful, especially with very distal
fractures.48,52,182
 |
|
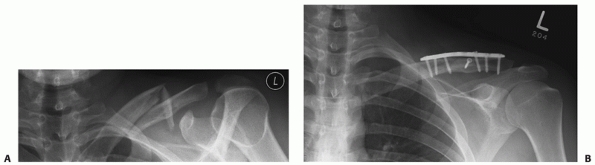
FIGURE 36-25 A.
Anteroposterior radiograph with 20-degree cephalad tilt demonstrating a completely displaced midshaft clavicle fracture with shortening. There are often vertically oriented fracture fragments that arise from the anterosuperior surface of the clavicle at the site of displaced midshaft fractures, giving many fractures a “Z” pattern. If possible, they should be gently teased back into place and fixed with small or mini-fragment screws, followed by plate fixation. It is important not to denude the fragment when attempting to fix it. Reduction is performed by reducing the vertical intercalated fragment to the distal fragment and securing it with a 2.7-mm lag screw. The distal assembly is then reduced to the proximal assembly with the aid of two towel clip reduction forceps, followed by plate fixation with a precontoured plate. B. Postoperative radiograph revealing restoration of length and anatomic reduction. |
semisitting position, similar to the position used for midshaft
fractures. A small pad or bump is placed behind the involved shoulder
to elevate it into the surgical field. The head is placed on a round
support and rotated out of the way of the operative field. Recently,
frames and supports designed to give greater exposure of the shoulder
(i.e., for shoulder arthroscopy) have become popular. This type of
operative setup can also be used and may facilitate intraoperative
radiography. It is not usually necessary to free-drape the involved
arm, although this can be done if there is any difficulty anticipated
with the reduction (i.e., if the fracture is severely displaced or
greater than 2 to 3 weeks old).
superior plating of the clavicle. A skin incision placed directly
superiorly over the distal clavicle, extending approximately 1 cm
past
the AC joint, is made. The skin and subcutaneous layer are developed,
and the deltotrapezial myofascial layer is incised directly over the
distal clavicle and reflected anteriorly and posteriorly. The AC joint
is identified. This can be done by inserting an 18-gauge needle into
the joint from the superior aspect, and an arthrotomy can be avoided.
It is possible to use an anteroinferior approach for plate fixation of
distal clavicle fractures, although in my experience this involves a
significant amount of detachment of the deltoid and it is not possible
to convert easily to coracoclavicular screw augmentation or hook plate
fixation.179
 |
|
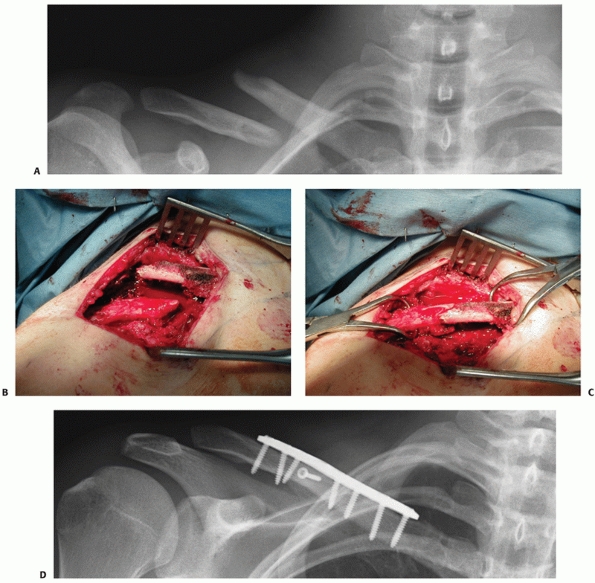
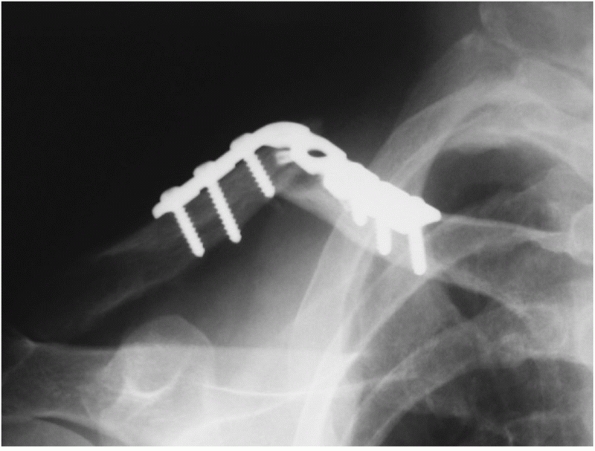
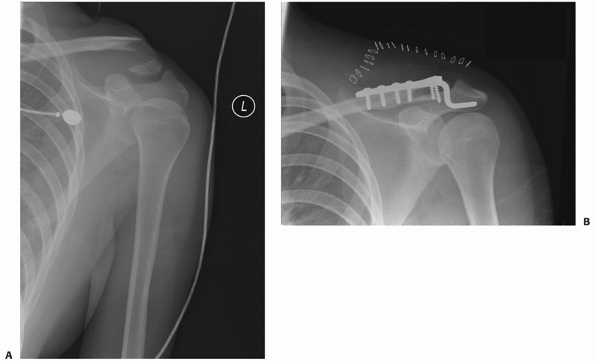
FIGURE 36-26 A.
Anteroposterior radiograph of a displaced distal clavicle fracture in a 38-year-old patient after falling off a mountain bike at high speed. Although the fracture was closed, there was significant bruising and swelling over the shoulder. The degree of displacement of this fracture suggests a high likelihood that delayed union or nonunion would result with nonoperative treatment. After the soft tissue swelling had subsided 10 days postinjury, operative fixation was performed with a plate specifically designed for the distal clavicle, allowing for the placement of four screws in the small distal fragment (B). The fracture healed uneventfully and the patient was able to return to work within a week of the surgery. C. Final follow-up radiograph following hardware removal for local soft tissue irritation, a common problem in this area, shows solid union. |
and hematoma. The fracture is reduced, and it may be held with either a
K-wire or a lag screw. Elevating the distal fragment to meet the
proximal fragment may aid in reduction. If the main fracture line is in
the coronal plane, it may be possible to lag the fracture from anterior
to posterior through a small anterior stab incision separate from the
primary incision. Once the fracture is reduced and provisionally
stabilized, the optimal type of plate is chosen. Anatomic plates that
fit the distal clavicle are now available, and placing four bicortical,
fully threaded, cancellous screws in the distal fragment should be the
goal (Fig. 36-26). Following fixation, the
surgeon must judge whether the number and quality of distal fragment
screws are sufficient to provide stability until union occurs. If this
is judged to be inadequate, there are several options at this point.
Since the primary deforming force at the fracture site is superior
displacement of the proximal fragment, it is possible to augment
fixation by securing the proximal fragment to the coracoid with a
longer screw inserted through one of the plate holes (Fig. 36-27).
This screw, typically 30 to 40 mm long, helps secure the proximal
fragment to the coracoid and prevent the superior displacement. Since
there is some intrinsic motion between the clavicle and the coracoid
and scapula, with time this screw either loosens or it may break, but
it will give 6 to 8 weeks of stability and fracture healing before
doing so. Alternatively, it may be necessary to augment fixation by
using a hook
plate
with fixation under the acromion to prevent superior migration of the
proximal fragment. This technique is selected when there is
insufficient bony purchase in the distal fragment with conventional
screws.49,52,182 This may be readily apparent during preoperative planning (Fig. 36-28)
or may only be realized intraoperatively. The advantage of subacromial
fixation is that conventional plating can be rapidly converted to this
technique intraoperatively. The AC joint is identified, and the
posterior edge of the distal clavicle is dissected free. An entrance
into the subacromial space is then made with a pair of heavy curved
scissors that will create the path of the “hook” extension of the
plate. It is important that this space is made posteriorly, so that
there will be no impingement of the rotator cuff in the critically
tight anterior subacromial space. Once this path has been created, the
hook is placed in it and the plate reduced to the shaft of the
clavicle. Several different hook depths and lengths for this plate are
currently available, and trial reductions can be performed to determine
the optimal plate type. Alternatively, the plate can be “walked down”
onto the clavicular shaft by sequential placement of the screws from
distal to proximal: this can be a very effective technique of fracture
reduction as this maneuver “levers” the distal fragment to the proximal
fragment. On occasion, it may be necessary to contour the shaft of the
plate to prevent overreduction of the fracture; however, if excessive
contouring appears to be required, a more likely explanation is that
the fracture is not reduced and that there is residual superior
angulation. It is possible to securely repair even very distal
fractures (that are essentially AC joint fracture-dislocations) with
this technique: minimal, if any, purchase is required in the distal
fragment. Unlike static fixation across the AC joint, which is doomed
to loosening or fatigue failure, hook plate fixation allows some
intrinsic motion between the bones. A cadaver study revealed that this
technique most closely reflected the biomechanics of the native AC
joint—namely, secure enough to provide reliable fixation yet
physiologically flexible.182
Following fixation, the wound is thoroughly irrigated and a two-layer
closure similar to that for midshaft fractures is performed.
 |
|
FIGURE 36-27 A.
It is possible to augment fixation in distal clavicle fractures with poor-quality bone or a very small distal fragment by placing a screw through the plate into the coracoid process, which helps resist the forces that displace the fracture (superior displacement of the proximal fragment, inferior displacement of the distal fragment). Since there is 10 to 15 degrees of rotational motion between the clavicle and the coracoid, this fixation will eventually loosen (as it has in this case) or break (B). However, typically it provides augmented fixation for 6 to 8 weeks postoperatively, which is usually sufficient for the fracture to heal. |
 |
|
FIGURE 36-28 A.
Anteroposterior radiograph of a very distal clavicle fracture in a 22-year-old female pedestrian struck by a street car. The fracture was open with significant soft tissue damage, near transection of the superior deltoid and trapezius, and severe instability of the shoulder girdle. It can be anticipated that conventional plating may be inadequate given the small size of the distal fragment and the associated shoulder girdle instability. B. Radiograph following irrigation and débridement, hook plate fixation, and deltoid/ trapezial muscle repair. Early motion was initiated and an excellent result ensued. |
early active motion in the form of pendulum exercises. At 10 to 14 days
postoperatively, the wound is checked and the stitches are removed. The
sling is then discarded and full range-of-motion exercises are
instituted; sling protection can be extended if the quality of fixation
is questionable. At 6 to 8 weeks, if radiographs are favorable,
resisted and strengthening exercises are instituted. Return to full
contact or unpredictable sports (i.e., mountain biking) is usually
discouraged until 12 weeks postoperatively. While hardware removal is
typically optional for those with conventional plates, it can be
anticipated that a high percentage of individuals with hook plate
fixation will require plate removal to regain terminal shoulder flexion
and abduction. This is usually performed at a minimum of 6 months
postoperatively.
-
The rate of delayed union and nonunion
for completely displaced distal clavicle fractures treated
nonoperatively is approximately 40%. -
Even minimally displaced fractures may
take an excessive period of time to heal or may develop a fibrous
union. However, without displacement, they are often not symptomatic
enough to warrant surgical intervention. -
The technical challenge faced during
operative treatment of distal clavicle fractures is fixation of the
distal fragment; the surgeon should be prepared to deal with unexpected
comminution
P.1130or poor screw purchase in the distal fragment using anatomic plates, coracoclavicular fixation, or hook plates.
-
Hook plate fixation is an effective
alternative to conventional plate fixation when faced with inadequate
distal purchase. To avoid subacromial impingement, the hook should be
placed just posteriorly -
A high percentage of patients treated
with hook plate fixation will require plate removal to regain full
range of shoulder motion. -
Rigid transacromial fixation has a high
rate of loosening and fatigue failure because of the intrinsic motion
at the AC joint and is therefore not routinely recommended
and scapular neck has traditionally been called the “floating
shoulder,” which has been considered to be an unstable injury that may
require operative fixation.42,130,142,166,168,175,176
In fact, this injury pattern can be considered to be a subgroup of the
“double disruption of the superior shoulder suspensory complex (SSSC),”
a concept introduced by Goss.54,122
This describes the bone and soft tissue circle, or ring, of the
glenoid, coracoid process, coracoclavicular ligament, clavicle
(especially its distal part), AC joint, and the acromion. This complex
is extremely important biomechanically, as it maintains the anatomic
relationship between the upper extremity and the axial skeleton. The
clavicle is the only bony connection between the two, and the scapula
is suspended from it by the coracoclavicular and AC ligaments. Thus,
any injury that disrupts this ring at two or more levels is considered
inherently unstable and one whose cumulative effect may be greater than
the sum of its individual constituents.178
Long-term functional problems have been reported following
significantly displaced injuries of this nature, including shoulder
weakness and stiffness, impingement syndrome, neurovascular
compression, and pain.* Such injuries have been considered relative indications for operative intervention (Fig. 36-7).
Combined scapular (or glenoid neck) and clavicle fractures are the
commonest type of double disruptions of the SSSC, and there remains
considerable controversy over optimal treatment.
results in 14 of 15 patients with this injury pattern following
fixation of both the clavicle and glenoid fractures.79 However, Herscovici et al.59
described excellent results in seven of nine patients who had their
floating shoulder treated with reduction and fixation of the clavicular
fracture only. These findings were confirmed in a study performed by
Rikli et al.,135 who performed
clavicle fixation is isolation in 11 patients with combined clavicle
and glenoid fractures. They described an average Constant-Murley
Shoulder Outcome Score in the operated shoulders of 95% of the
unaffected side. These studies support the concept, in selected cases,
of clavicular fracture reduction and fixation alone. It is postulated
that reduction of the clavicle helps to reduce and stabilize the
glenoid fracture, eliminating the requirement for operative fixation of
the glenoid. This is an important point, since open reduction and
internal fixation (ORIF) of the glenoid can be a difficult and complex
procedure with a high complication rate, especially if the surgeon
lacks experience in this anatomic area.
described the results of nonoperative treatment in 16 patients with
ipsilateral fractures of the clavicle and glenoid. Eleven patients had
a complete recovery to near normal status, although one had a
significant malunion of the glenoid neck and three had significant
shoulder asymmetry. Edwards et al.40
reported good results (“pleased” or “satisfied”) in 16 of 20 patients
with floating shoulder injuries treated nonoperatively. There were four
patients who were “dissatisfied” or “unhappy” with their outcome. While
the outcome assessment of these patients was suboptimal, it would
appear that nonoperative treatment may be considered, especially for
minimally displaced fractures. Interestingly, two of the four patients
with poor results had severely displaced clavicular fractures. In a
clinical study, Williams and colleagues176
evaluated 9 of 11 patients with a floating shoulder treated
nonoperatively and found five excellent, one good, and three fair
results. They found that the worse clinical results were strongly
associated with 3 cm or more of medial displacement of the glenoid and
recommended nonoperative care for lesser amounts of displacement.
Similarly, van Nort et al.166
performed a questionnaire review including 31 of 35 floating shoulder
patients treated nonoperatively and found that only 3 required late
operative reconstruction for clavicular malunion or nonunion. They
found that results in the nonoperative group (a mean Constant-Murley
Shoulder Outcome Score of 76) deteriorated with increasing degrees of
glenoid displacement. Interestingly, they also found that three of the
four patients who had their clavicle fracture fixed primarily had a
poor result because of scapular malunion. They believed that this
failure of indirect glenoid reduction following clavicular reduction
and fixation was because of associated ligamentous injuries that caused
a dissociation of the two structures.
the intuitive clinical finding that increasing degrees of fracture
displacement in floating shoulder injuries corresponds to poorer
results if left unreduced. Williams et al.175
performed a cadaver biomechanical study by establishing a scapular neck
fracture and investigating the effect of an ipsilateral clavicle
fracture, a coracoacromial ligament injury, and an AC ligament injury.
They found that substantial instability (lack of resistance to a
medially directed force) only occurred after associated ligamentous
disruption. Although there are limitations to this study (such as the
uniaxial direction of the applied deforming force), it remains one of
the only biomechanical studies on this topic.
this injury, there is a paucity of prospective, randomized, or
comparative trials on which to base treatment recommendations. What is
clear is that earlier recommendations for routine operative fixation
for all floating shoulder injuries were too liberal and that poor
results occur regularly with badly displaced fractures that are treated
nonoperatively. In addition, the aggressiveness of treatment must be
commensurate with the risk of intervention and the expected functional
demands of the patient. Thus, an operative approach may be indicated in
a young healthy individual who requires extensive overhead activity for
work (painter, plasterer, electrician, etc.), whereas the same fracture
pattern may be treated nonoperatively in an elderly, low-demand patient
with multiple medical comorbidities. Further research in this area may
help identify currently unknown factors
that may predict outcome and hence guide treatment.73 Current standard operative indications include the following:
-
A clavicle fracture that warrants, in isolation, fixation (see Operative Indications, earlier)
-
Glenoid displacement of greater than 2.5 to 3.0 cm
-
Displaced intra-articular glenoid fracture extension
-
Patient-associated indications (i.e., polytrauma with a requirement for early upper extremity weight bearing)
-
Severe glenoid angulation, retroversion, or anteversion greater than 40 degrees (Goss type II)
-
Documented ipsilateral coracoacromial
and/or AC ligament disruption or its equivalent (i.e., coracoid
fracture [AC joint disruption])
reduction and internal fixation of the clavicle is typically performed
first, and the shoulder is then reimaged. If fixation of the clavicle
results in indirect reduction of the glenoid such that its alignment is
within acceptable parameters, then no further intervention is required
apart from close follow-up. If the glenoid remains in an “unacceptable”
position, then fixation of the glenoid neck, typically performed
through a posterior approach, is indicated (see Chapter 37). Also, Oh et al.117
reported the failure of isolated clavicle fixation in two cases of
floating shoulder. If this first method is chosen in this setting, the
clavicle may experience greater loads than with isolated fractures, and
the size and length of the fixation device selected should be
commensurate with these anticipated loads.117
complications following fixation of displaced clavicular fractures, and
earlier series described an unacceptably high rate of deep infection.2,27,50,100
However, significant improvements have been made in a number of areas
that are well recognized to decrease infection, including perioperative
antibiotics, selective operative timing with regard to soft tissue
conditions, better soft tissue handling, two-layer soft tissue closure,
and fixation that is superior biomechanically.* In a recent
metaanalysis that examined operative series from 1975 to 2005,
Zlodwodzki et al. reported a superficial infection rate of 4.4%, and a
deep infection rate of only 2.2%; these figures are significantly
improved compared with earlier studies.185
If infection does occur and it is superficial, then it is usually
possible to temporize with local wound care and systemic antibiotics
until fracture union has occurred. At this point, plate removal,
débridement, and thorough irrigation have a high success rate in
infection eradication.
more complex problem. If it appears that there is progressive bone
formation, then temporizing until union occurs followed by hardware
removal and debridement may be successful. If there is no obvious
progress toward union, then operative intervention is indicated.
Hardware removal followed by radical débridement of infected bone and
dead or devitalized tissue and subsequent irrigation is performed. At
this point there are several options. If the patient is healthy without
comorbidities (as is usually the case) and the infecting organism is a
sensitive one, then immediate reconstruction with plating, bone
grafting, and local antibiotics may be warranted. Alternatively,
especially with polymicrobial infections or resistant organisms (i.e.,
methicillin-resistant Staphylococcus aureus),
local antibiotic-impregnated polymethlymethylacrylate cement beads or
an antibiotic-impregnated bone substitute is implanted into any
residual dead space following debridement and systemic antibiotics are
administered until clinical and hematologic markers indicate the
infection has been eradicated. Delayed reconstruction can then be
performed. If there is a significant soft tissue deficiency, then the
assistance of a plastic surgeon who can perform soft tissue coverage,
typically with a rotational pectoralis major flap, is ideal.161,174
been described as being less than 1% of all fractures. This was based
on two sentinel studies—one by Neer100 in 1960 that described 3 nonunions in 2235 patients and one by Rowe144
in 1968 in which only 4 of 566 patients developed nonunion after a
fracture of the clavicle. More recently, however, the nonunion rate
following closed treatment of completely displaced midshaft fractures
of the clavicle has been described as being exponentially higher, in
the 15% to 20% range.15,62,139,185
The reason for this difference is unclear but probably includes more
complete follow-up in recent studies, the exclusion of children (with
their inherently good natural history), changing mechanisms of injury
(mountain biking, all-terrain vehicles, parachuting), and modern
patients’ intolerance of prolonged immobilization. In addition, several
prospective population-based studies have been helpful in elucidating
factors associated with the development of nonunion (Fig. 36-17). Robinson et al.139
identified increasing age, female sex, fracture displacement, and
comminution as risk factors for nonunion in midshaft fractures. Lateral
third fractures had higher nonunion rates as patient age and fracture
displacement increased.138 Nowak et al.113
prospectively followed 208 patients with radiographically verified
clavicle fractures and, 9 to 10 years postinjury, found that 96 (46%)
still had sequelae. They identified no bony contact between the
fracture fragments as the strongest predictor for sequelae. Nonunion
occurred in 15 patients (7%). Zlowodzki et al.185
performed a metaanalysis of all series of displaced midshaft fractures
from 1975 to 2005 and identified 22 published manuscripts. They found
that, for the specific entity of completely displaced midshaft
fractures of the clavicle, the nonunion rate with nonoperative
treatment was 15.1%, while the nonunion rate following operative
treatment was 2.2%. This represents a relative risk reduction (for
nonunion) of 86% (95% confidence interval, 71% to 93%). This
meta-analysis, in addition to recent prospective studies examining
primary operative fixation of clavicle fractures, definitively
terminated the postulation that primary fixation was associated with a
higher, not lower, nonunion rate (Table 36-1). This observation was based on early operative studies with poor patient selection, inadequate fixation (Figs. 36-21 and 36-22),
and inferior soft tissue management. Undoubtedly, there are other
factors that contribute to the incidence of nonunion (i.e., associated
fractures, soft tissue interposition, rotation at the fracture site)
that have yet to be clarified.129,159,171,173
Therefore, at the present time, factors associated with the development
of nonunion include complete fracture displacement (no contact between
the main proximal
and
distal fragments), shortening of greater than 2 cm, advanced age, more
severe trauma (in terms of both mechanism of injury and associated
fractures), and refracture. Primary operative fixation, however, is not
associated with a higher nonunion rate.
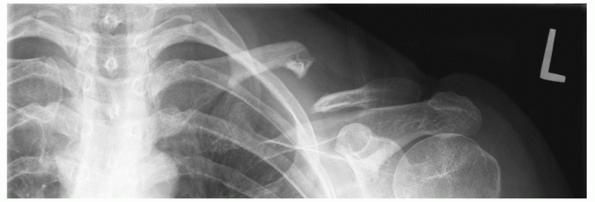 |
|
FIGURE 36-29
Atrophic nonunion of the clavicle. The degree of bone loss demonstrated in this case suggests that an intercalary graft may be required to restore length and obtain union. |
treatment of an established clavicular nonunion that is symptomatic
enough to warrant operative intervention.† Successful
nonunion repair usually decreases pain and improves function. Described
methods range from noninvasive techniques such as electrical
stimulation and low-intensity ultrasound to minimally invasive
techniques (isolated bone grafting, screw fixation) to formal ORIF with
iliac crest bone grafting. Apart from isolated case reports, or cases
described in larger series of standard treatments, there is very little
objective evidence to support the use of electrical stimulation or
ultrasound in this area.13,29,30
In rare cases where there is minimal deformity or shortening, a stable
hypertrophic nonunion with good soft tissue coverage and no infection,
and a biologically favorable host (i.e., no smoking or diabetes), such
techniques may occasionally be successful in promoting union. However,
the majority will require mechanical stabilization and biological
stimulation.
fixation and IM screw or pin fixation. The gold standard treatment
against which other methods must be compared is ORIF with a compression
plate and iliac crest bone graft. Reported success rates with this
technique are high if appropriate size and length plates are used.
Manske and Szabo84 (10 of 10 healed), Eskola et al.46 (20 of 22 healed), Jupiter and Leffert69 (16 of 19 healed), Boyer and Axelrod11 (7 of 7 healed), Olsen et al.118 (16 of 17 healed), and Bradbury et al.12
(31 of 32 healed) all describe excellent results with a low
complication rate. It is important to note that the forces generated by
deformity correction and the longer healing time will mean that the
operative construct for a nonunion will require greater stability for a
longer period of time than that for an acute fracture. Multiple authors
stress that short four-hole plates, weak 1/3 tubular plates, or even
3.5-mm pelvic reconstruction plates in larger (>200 pounds) patients
are inadequate for this type of fixation and have higher failure rates (Fig. 36-22).
A small fragment compression plate, a precontoured “anatomic” plate, or
their equivalent with a minimum of three bicortical screws in each
fragment is recommended* (see “Author’s Preferred Method of Treatment,” next).
open bone grafting for the treatment of clavicular nonunions. A smaller
incision with better cosmesis, less soft tissue stripping, decreased
hardware irritation, and easier hardware removal (often under a local
anaesthetic) are proposed benefits compared with plate fixation. There
are several reports describing good results including Boehme et al.8 (20 of 21 healed) and Enneking et al.45 (13 of 14 healed). In the only comparative study of fixation techniques for clavicle nonunion, Wu et al.178
described union in 9 of 11 patients treated with plate fixation and 16
of 18 of those treated with IM fixation. However, Wilkins and Johnston173
reported pin failure in two of four patients treated in this fashion,
and the two failed IM fixations in the series by Wu et al.178
both healed with subsequent plate fixation. In addition to IM fixation
being weaker biomechanically and not controlling length and rotation as
well as a plate, others have reported difficulty with pin migration and
breakage using this technique.73,83,97,108 A randomized, prospective study comparing plate and IM fixation is required to define their respective roles in this setting.
associated with multiple failed operative procedures and infection, can
complicate the reconstruction of recalcitrant clavicular nonunions. The
final treatment option in such circumstances is clavicular excision or
claviculectomy (either partial or total).29,30,177
Considering the important strut effect of the clavicle for upper
extremity function and the availability of modern treatment options,
this must be considered a salvage procedure. While reasonable results
with retention of a full range of motion and relief of pain have been
described in selected cases with severe preoperative pathology, a
significant decrease in strength (especially overhead) and a loss of
shoulder girdle stability typically result.
of the clavicle is ORIF with a precontoured anatomic clavicular plate
with the addition of an iliac crest bone graft or osteoinductive bone
graft substitute. Patient positioning and draping are similar to those
used for the fixation of acute midshaft fractures, with the exception
of having an iliac crest bone graft site prepared (typically the
contralateral side) if bone grafting is anticipated (see later). The
surgical approach is similar to that used for a fracture, taking care
to reflect and preserve the myofascial layer for later closure, and the
superior surface of the clavicle at the nonunion site is identified.
The ends of the nonunion are identified, and judicious soft tissue
dissection is performed around them to allow correction of deformity.
This usually involves bringing the distal fragment out to length and
translating it superiorly and posteriorly. The distal fragment is often
rotated anteriorly, and derotating it brings the flat superior surface
directly superiorly,
facilitating
plate placement on the superior surface. The sclerotic ends of the
proximal and distal fragments are identified and a rongeur is used to
clear them back to bleeding bone. It is rarely necessary to resect
excessive bone to do this. The medullary canals are then reestablished
with a drill to allow the free egress of osteoprogenitor cells to the
nonunion site. Reduction forceps are then placed on the proximal and
distal fragments and a reduction is performed. Remembering that there
is a slight apex superior bow to the native clavicle, excess superior
callous is rongeured away to allow the plate to fit on the superior
surface of the clavicle. Any excess callous removed in the approach,
débridement or deformity correction is saved, morcellized, and inserted
into the fracture site at the conclusion of the procedure. If possible,
the nonunion is then fixed with an anterior-to-posterior small- or
mini-fragment lag screw (Fig. 36-30).
The chance of success of this helpful step can be increased by
recognizing the orientation of the nonunion line during the approach
and debridement. Lag screw fixation helps hold the reduction while the
plate is applied and also increases the construct stability. If this is
not possible, then a 2.0-mm K-wire can be inserted to hold the
reduction while a precontoured clavicle plate is applied to the
superior surface. I typically use an eight-hole plate: this allows for
one or even two empty holes at the nonunion site (often necessary
because of bony configuration or lag screw interference) while
providing for three bicortical screws both proximal and distal, which I
consider to be the absolute minimum for fixation. If the nonunion is
transverse in nature, the first screws on each side are inserted in a
compression mode and tightened after the provisional K-wire has been
removed. Although they are available, I have not found it routinely
necessary to use locking screws or plates in the clavicle. If the
nonunion is hypertrophic (the minority), then the morcellized autograft
from the local bone is applied to the nonunion site and a standard
closure, as for a fracture case, is performed. Thorough irrigation and
hemostasis are achieved before closure, and drains are not used.
autograft from the iliac crest or an osteoinductive bone substitute,
such as a bone morphogenic protein, is packed in and around the
nonunion site. Bone substitutes with little osteoinductive capability,
such as calcium phosphates or sulfates, allograft, or demineralized
bone, are to be avoided. A structural or intercalary graft may be
required in certain cases where there has been excessive loss of length
or previous surgery has failed. Shortening can often be determined
preoperatively by comparing the length of the clavicle radiographically
to the measured clinical length. If there appears to be significant
bone loss, then an intercalary graft, according to the technique of
Jupiter and Ring,70 can be used. Postoperative care is similar to that following malunion reconstruction or acute fracture fixation.
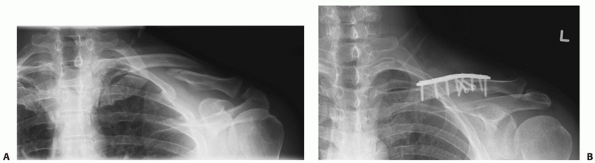 |
|
FIGURE 36-30 A. Atrophic nonunion 14 months following nonoperative care of a completely displaced fracture of the clavicle. B.
Successful repair with correction of deformity, plate fixation, and the addition of bone morphogenetic protein to the nonunion site. The oblique nature of the nonunion in the coronal plane facilitated fixation with two anterior-to-posterior lag screws. |
clavicle (which was ubiquitous with displaced fractures) was of
radiographic interest only, and success in the clinical setting was
defined as fracture union. However, more recently, a number of
investigators have described a fairly consistent pattern of patient
symptomatology (with orthopaedic, neurologic, “functional,” and
cosmetic features) following malunion of displaced midshaft fractures
of the clavicle.7,20,57,68,76,90,122,135
While all of the factors that contribute to the development of this
condition are unclear, it is typically diagnosed in young, active
patients with significant degrees of shortening at the malunion site (Fig. 36-31).
As could be reasonably anticipated, shortening of the shoulder girdle
(with the typical inferior displacement and anterior rotation of the
distal fragment) results in a variety of biomechanical and anatomic
abnormalities that translate directly into patient complaints.
Orthopaedically, shortening of the muscle-tendon units that traverse
the malunion site results in a sense of weakness and rapid
fatigability, with a loss of endurance strength. It has been previously
shown that there are significant, objective deficits in maximal
strength and endurance (especially of abduction) following the healing
of displaced midshaft fractures of the clavicle treated nonoperatively92,155 (Fig. 36-32).
Narrowing and displacement of the thoracic outlet (the inferior border
of which is the clavicle) result in numbness and paraesthesias, usually
in the C8-T1 nerve root distribution, exacerbated by provocative
overhead activities. Because of their deformity, patients complain of
the appearance of their shoulder and difficulty with backpacks, hiking
packs, military gear, and shoulder straps: this has been termed a
deficit in “functional cosmesis.” Patients with this condition also
complain of upper back pain and periscapular aching, especially with
repetitive activity. There is objective evidence that the displacement
of
the distal fragment (to which the scapula is attached) results in
malalignment of the scapulothoracic joint and a form of scapular
winging: this produces periscapular muscle spasm and fatigue pain.57,131
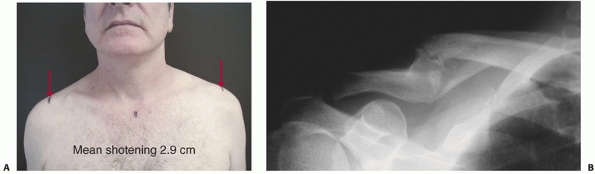 |
|
FIGURE 36-31 Typical clinical features of clavicle malunion (A) with a corresponding radiograph (B). Note the shoulder asymmetry and the difference in the position of the acromioclavicular joints (arrows).
|
development of this condition is shortening at the malunion site. Hill
et al.61 found that shortening of 2
cm or more was associated with poor functional outcome and a high rate
of patient dissatisfaction. McKee et al.90
described a series of 15 patients with a symptomatic clavicular
malunion who had a mean degree of shortening of 2.9 cm, and Bosch et al.9 described an “extension osteotomy” in four patients with shortening of 0.9 to 2.2 cm. In a retrospective study, Eskola et al.47
reported on 83 patients with displaced fractures and found that
shortening of 1.2 cm or more was associated with increased pain at
final follow-up. However, this point remains controversial. In
retrospective reviews, Nordqvist et al.112 (225 midshaft clavicle fractures) and Oroko et al.120
(41 midshaft clavicle fractures) could not demonstrate a relationship
between shortening and a poor outcome. It is probable that length is
just one component of a complex three-dimensional deformity, which,
combined with the intrinsic variability of human response to skeletal
injury, explains why some individuals with malunion function well and
others determinedly seek operative correction. For patients with a
symptomatic malunion who have failed a course of physiotherapy for
muscle strengthening, the options are to accept the disability or have
a corrective osteotomy.
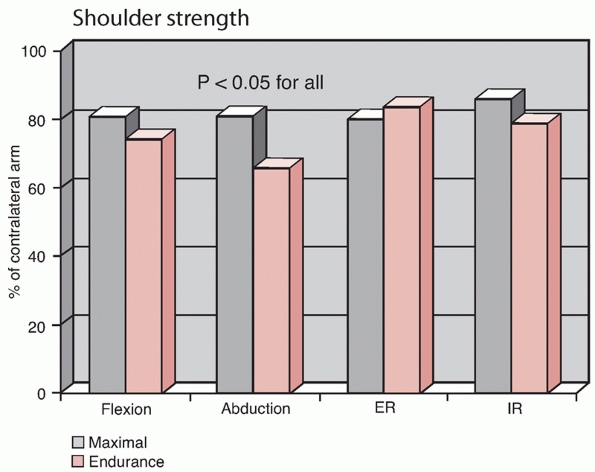 |
|
FIGURE 36-32
Objectively measured shoulder strength following nonoperative treatment of displaced midshaft fracture of the clavicle (maximal, endurance) compared with normal contralateral side. Patients were a minimum of 14 months postinjury, with a mean of 54 months. |
signs and symptoms of malunion that are specific to the condition and
sufficiently symptomatic to warrant surgery. A vague and generalized
ache about the shoulder (especially in a patient with medicolegal or
compensation issues) and a radiographic malunion is not necessarily an
indication for surgery. Patients selected for surgery are typically
young, active, and healthy with good bone stock. The primary goal of
surgery is to correct the deformity, and preoperative planning is
important (Fig. 36-33). Careful measurement both clinically
and radiographically defines the degree of length to be restored. A
posteroanterior thorax or chest radiograph that includes both clavicles
has been shown to be a reliable way of comparing length to the opposite
(normal) clavicle.155
Inferior displacement and anterior rotation of the distal fragment is
corrected by having the plate applied to the superior surface flush
both medially and laterally; some contouring of the plate may be
required in the anterosuperior plane as there is a slight caudal bow to
the clavicle.
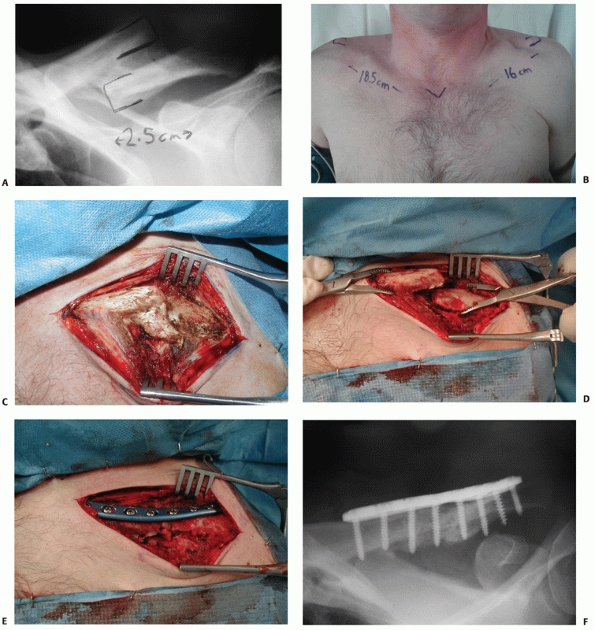 |
|
FIGURE 36-33 A. Anteroposterior radiograph of a symptomatic clavicle malunion with 2.5 cm of shortening. B.
Corresponding clinical photograph shows the measurement of clavicular length from the sternal notch to the acromioclavicular joint. C. Intraoperative photograph of the malunion site demonstrates the typical displacement of the distal fragment with medial, inferior, and anterior translation. This also shows the abundant local bone that is usually present at the malunion site. While it is difficult to appreciate, there is often anterior rotation of the distal fragment as well. D. Intraoperative photograph following osteotomy of the malunion showing recreation of the original fracture line and rongeuring of excess callus (which will be used to graft the osteotomy site) and distraction of the fragments to their correct length and position. It is typically not necessary to perform an intercalary bone graft, as there is rarely absolute bone loss, and the original proximal and distal fragments can be reestablished using a combination of a microsagittal saw and osteotomes. E. Intraoperative photograph following reduction and plate fixation using an anatomic precontoured plate. F. Anteroposterior radiograph following union. The patient’s preoperative symptoms resolved promptly. |
The exception is that in certain cases it is prudent to have an iliac
crest bone graft site prepared (see later). In general, it has not been
routinely necessary to insert an intercalary graft to restore length.
It is usually possible to identify the position of the proximal and
distal fragments in most patients. The malunion site is cleared, a mark
is made in the bone proximally and distally, and the length is
measured. This enables the surgeon to calculate how much length has
been gained by remeasuring the distance between the two marks at the
conclusion of the osteotomy. Next, the osteotomy to recreate the
original fracture and proximal and distal fragments is made with a
combination of a microsagittal saw and osteotomes. Care is taken not to
violate the subclavicular space. Following the osteotomy, the proximal
and distal fragments are grasped with reduction forceps and gently
distracted to the desired position. Routinely, it is not necessary to
free-drape the arm for traction. For difficult cases, a minidistractor
can be used to correct length and maintain position while fixation is
applied. Care must be taken to not overdistract the fragments as
neurologic injury may result.136
Depending on the configuration of the bone ends, after the osteotomy is
performed it is often possible to fashion an interdigitating or step
cut contour to improve intrinsic stability and increase the bony
surface area for healing. The medullary canals are reestablished with a
drill, and the osteotomy is temporarily secured with a Kirschner wire.
It is then measured for correction of deformity and length. On
occasion, an absolute bone deficit may be encountered, such that
reduction of the fragments does not restore length. Options at this
point include accepting some shortening or using an intercalary graft.
This situation can be anticipated preoperatively when the measured
clinical shortening (i.e., 3 cm) is significantly greater than the
degree of shortening seen on the radiograph of the involved clavicle.
Once deformity correction is confirmed, definitive fixation is
performed: there are several precontoured “anatomic” plates designed
for clavicular fixation that are ideal for this purpose.64
If a lag screw can be placed across the osteotomy, then three
additional screws both proximally and distally are usually sufficient.
If not, four screws proximally and distally are recommended. Additional
local bone can be morcellized and added to the osteotomy site. Wound
closure and postoperative care are the same as those for acute fracture
fixation or nonunion repair.
subclavian vessels, neurovascular injury is surprisingly rare, given
the number of severely displaced clavicular shaft fractures seen in
practice.* In general, neurovascular injuries associated
with clavicle fractures can be divided into three groups: acute
injuries, delayed injuries, and iatrogenic injuries.
critical with any clavicular injury, especially those associated with
high-energy trauma. If the indications of vascular injury are present,
an angiogram is indicated. In addition to being diagnostic, with the
refinement of interventional techniques such as embolization and
stenting, this procedure can also be therapeutic (Fig. 36-34).
While direct impalement of bony fragments can occur, most neurovascular
injuries occur from excessive traction, which in its most severe form
is termed scapulothoracic dissociation.
The unique feature of these injuries is that the associated clavicular
fracture is typically distracted, rather than shortened. This can be a
limb- or life-threatening injury: a study by Ebraheim et al.36 reported 3 deaths in 15 patients, and Zelle et al.183
described 3 deaths and 6 amputations in 22 patients in their series
from a major European trauma center. If limb salvage is to be
performed, shoulder girdle stabilization is indicated to create an
optimal healing environment for the soft tissue structures. There have
been case reports of direct neurologic injury from clavicular fracture
fragments: in this situation, operative decompression of the brachial
plexus by reduction and fixation of the clavicle fracture is indicated.6,10,32,51,63,132,145
of the thoracic outlet, from either displacement of the borders (i.e.,
from clavicular displacement caused by malunion or nonunion) or
encroachment from inferior callus formation (this phenomenon can be
especially severe in patients with a concomitant head injury [Fig. 36-35]).
In the case reports describing this entity, debridement of local callus
with realignment and fixation of the clavicle injury is indicated.24,44,132
The most common reason for brachial plexus irritation following
clavicular fracture is the chronic thoracic outlet syndrome (TOS) that
results from clavicular malunion (see earlier). In this setting,
operative treatment should be directed toward reestablishing the
preinjury dimensions of the thoracic outlet through a corrective
clavicular osteotomy.7,9,20,90
Simply removing the “bump” around the fracture site or conventional
treatments for TOS such as first rib resection have a high failure
rate. This is because the fundamental anatomic problem is the change in
position, orientation, and contour of the thoracic outlet from the
displacement of the distal clavicular segment, rather than from local
impingement of callus or normal structures (i.e., the first rib).
Connolly and Ganjianpour26 reported
the case of a patient with TOS following a clavicular malunion that was
treated with first rib resection to no avail, while corrective
clavicular osteotomy resulted in prompt resolution of symptoms. McKee
et al.90 reported resolution of TOS
symptoms in 16 patients who underwent corrective clavicular osteotomy
to treat a malunion. Chronic impingement of the thoracic outlet leading
to TOS is probably the most common form of neurovascular “injury”
following displaced clavicular fractures.
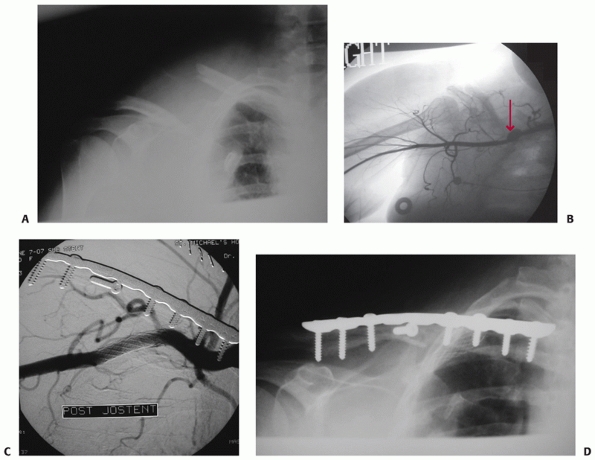 |
|
FIGURE 36-34 A.
Anteroposterior radiograph of a morbidly obese 57-year-old woman who sustained a severely displaced midshaft fracture of the clavicle in a fall from a standing height. B. She also had a partial brachial plexus injury and a partial laceration of the subclavian artery with pseudoaneurysm formation (arrow), shown on the preoperative angiogram. C. The patient was treated with immediate stenting of the resultant pseudoaneurysm, followed by plate fixation of the fracture with a 3.5-mm limited contact dynamic compression plate. D. The indications for fixation included reducing the severe displacement and creating an optimal environment for neurologic and vascular healing. Uneventful bony and soft tissue healing ensued. |
catastrophic injury from intraoperative penetration by drills or taps
is very rare. Shackford151 reported
a case of subclavian pseudoaneurysm formation with distal embolization
from screw penetration after plate fixation of a clavicular nonunion,
and Casselman et al.17 described a
similar case. Iatrogenic injury can occur, but it is thought to occur
in specific situations where distraction can occur. Ring and Holovacs136
described three cases of brachial plexus palsy after IM fixation of
clavicle fractures. They postulated that the distraction of the
fracture site (a prerequisite for reduction and pin insertion) and the
delayed presentation (patients were diagnosed several weeks after their
injury) led to a traction injury of the brachial plexus. Fortunately,
all three patients with palsies recovered completely with nonoperative
care. It appears that distraction of a shortened clavicular fracture,
especially one that presents or is treated some weeks or months
following initial injury, creates a risk for a traction-type injury to
the adjacent brachial plexus. Overdistraction at the fracture site or
any violation of the subclavicular space is to be avoided during
operative repair of clavicular injuries. Fortunately, with the
information presently available, these injuries are usually transient
in nature and, with time, a full recovery can usually be expected.
clavicle is surprisingly rare. It has been my experience that many
individuals who have claimed to have sustained multiple fractures of
the clavicle in fact, a nonunion following their initial fracture that
never healed completely. Recurrent episodes of trauma prompt medical
attention, and new radiographs are misinterpreted as showing a
“refracture.” The few cases that are reported describe a higher
nonunion rate following “refracture”: regardless of the exact etiology,
patients with this condition should be counseled about the high rate of
unsatisfactory outcome and that they may benefit from fixation.15,29,30
displaced clavicle fractures and the patient population involved, it is
not surprising that fractures at the end of a plate used for fixation
of a prior clavicle fracture are being encountered. This typically
occurs from recurrent high-energy trauma. Large prospective series are
not available and recommendations are based on only a few cases. In
general, a fracture in the upper extremity that occurs at the end of a
stable implanted diaphyseal plate has a poor natural history and a high
chance of delayed union or nonunion. It is my experience that these
fractures, if displaced, generally require repeat fixation. Attempts
should be made to
fix the fracture and span the area of bone previously repaired (Fig. 36-36). If the fracture is minimally displaced, a trial of nonoperative care with the arm at rest in a sling is reasonable.
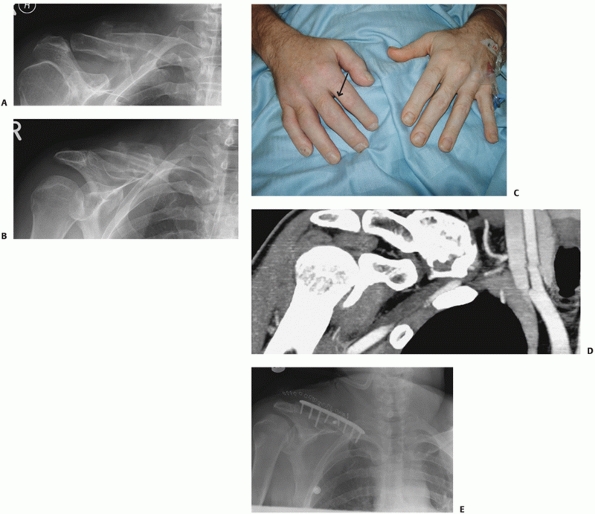 |
|
FIGURE 36-35 A.
Initial anteroposterior radiograph of a 46-year-old polytrauma patient with a head injury demonstrates a displaced clavicle fracture. B. Anteroposterior radiograph at 6 weeks postinjury reveals abundant callus formation around the fracture. The patient had increasing neuralgic pain in the associated upper extremity with progressive objective muscle weakness in the hand. The involved hand (C, arrow) had signs of venous obstruction with swelling, loss of skin wrinkle definition, and violaceous discoloration. D. Computed tomography scan confirmed severe obstruction of the thoracic outlet due to a combination of severe shortening and displacement of the fracture site and exuberant callus formation. This patient was treated with operative correction of the deformity, complete resection of the supraclavicular callus, and judicious resection of infraclavicular callus followed by plate fixation. E. Prompt resolution of symptoms, complete neurologic recovery, and uncomplicated fracture union ensued. |
may have multiple etiologies, and has been anecdotally reported to
occur following the nonoperative treatment of displaced midshaft
fractures of the clavicle.131 Rasyid et al.131
reported two cases of winging of the scapula, one from a “neglected”
fracture of the clavicle with 2 cm of shortening. The typical clavicle
malunion or nonunion with deformity results in a shortened, protracted
shoulder. Since the scapula moves with the distal end of the clavicle
(through its only bony attachment at the AC joint), this can lead to
scapular malposition with a shortened, protracted shoulder (Fig. 36-37). This scapular malposition has recently been quantified in a series of patients with clavicle malunion by Hall et al.57
using three-dimensional CT scanning in which mean clavicular shortening
of 16 mm resulted in 10 mm of lateral scapular displacement, with
anterior rotation of 8 degrees and 10 millimeters of elevation from the
posterior chest wall (Fig. 36-38). They postulated that this rotation and displacement result in the winging seen in their patients.57
The negative mechanical effects of this shoulder position are well
documented, with a mean decrease in rotational strength ranging from
13% to 24% in one study.156 This may
also explain the characteristic periscapular muscular fatigue pain that
these patients describe. Future research should elucidate the risk
factors for and potential treatment of this condition.
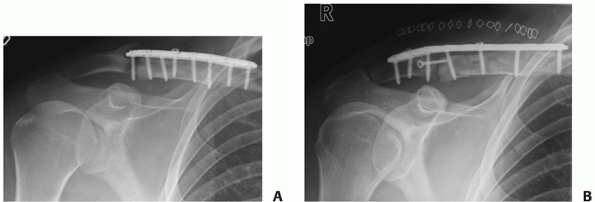 |
|
FIGURE 36-36 A.
A 40-year-old professional motorcycle racer had plate fixation of a midshaft clavicle nonunion that developed following a displaced midshaft fracture. The nonunion healed uneventfully, but 2 years later, following another high-velocity crash, he sustained a fracture at the lateral end of the plate. B. This fracture also developed into a nonunion, and required repeat fixation with a longer plate. This is a potential risk for individuals with plate fixation of the clavicle who continue to participate in high-risk activities. |
 |
|
FIGURE 36-37
Clinical photograph of scapular winging of left shoulder associated with a midshaft clavicle malunion with 3 cm of shortening. There is a characteristic protrusion of the inferior angle of the scapula, produced as the scapula rotates and translates anteriorly with the distal clavicular fragment. |
nonoperatively, but recent studies have shown that the union rate for
displaced midshaft fractures of the clavicle may not be as favorable as
previously described. In a prospective series of 868 patients with
clavicle fractures treated nonoperatively, Robinson et al.139
reported a significantly higher nonunion rate (21%) in displaced
comminuted midshaft fractures. An analysis of this paper by Brinker et
al.14 suggested a nonunion rate varying between 20% and 33% for displaced comminuted fractures in males. Hill et al.62
studied 66 consecutive displaced midshaft clavicle fractures and found
a 15% nonunion rate and a 31% rate of patient dissatisfaction with
nonoperative care. Based on their data, they concluded that
displacement of the fracture fragments of greater than 2 cm was
associated with an unsatisfactory result. A metaanalysis of studies of
clavicle fractures from 1975 to 2005 revealed that displaced midshaft
clavicle fractures treated nonoperatively had a nonunion rate of 15.1%.
This metaanalysis also showed that primary plate fixation was, contrary
to prevailing opinion, a safe and reliable procedure.185 Nowak et al.113,114
examined the late sequelae in 208 adult patients with clavicle
fractures at 10 years postinjury. Interestingly, 96 (46%) still had
symptoms despite the fact that only 15 (7%) had an established
nonunion. McKee et al. reported on a series of patients who has
nonoperative treatment of a displaced midshaft clavicle fracture a mean
of more than 4 years earlier. Objective muscle strength testing
revealed significant strength deficits, especially of shoulder
abduction and flexion, which help explain some of the patient
dissatisfaction seen despite bony union.92
 |
|
FIGURE 36-38
Three-dimensional computed tomography scan reconstruction of a patient with a right-sided clavicular malunion. A reference line through the coronal plane of the body reveals the significant anterior translation of the shoulder girdle. |
exists in outcome between previous reports on clavicle fractures and
contemporary studies, one possibility may be the inclusion of children
in the older reports, which, because of their inherent healing
abilities and remodeling potential, may artificially improve the
overall results. Also, patient-oriented outcome measures, as used by
Hill et al. and McKee et al., have been shown to reveal functional
deficits in the upper extremity that have not been detected
traditionally.15,62,92
A focus on radiographic outcomes would not reveal such problems.
Patient expectations and injury patterns are changing. Several studies
that examined clavicular shaft fractures in polytrauma patients found
that the presence of a clavicle fracture was associated with a 20% to
30% mortality rate (mainly from concomitant chest and head injuries),
and that survivors displayed a significant level of residual disability
in the involved shoulder.89,161
Thus, there is a surviving patient population (with clavicle fractures)
that has an intrinsically worse prognosis where long-term sequelae may
be more common.
cosmesis is important to patients, and an unsightly scar has been a
traditional deterrent to operative treatment of clavicular fractures.28,29,30,100,105,121,127
However, to a body image-conscious patient (predominantly young, male
population), a droopy shoulder is also of significant cosmetic concern.
In a recent randomized clinical trial (RCT) comparing operative and
nonoperative treatment, despite the incidence of hardware prominence
and incisional complications (numbness, sensitivity) in the operative
group, more patients in this group answered “yes” to the question, “Are
you satisfied with the appearance of your shoulder?” than in the
nonoperative group (52 of 62 versus 26 of 49, P=0.001; Table 36-4).
This study also showed superior surgeon-based (Constant-Murley Shoulder
Outcome Score and patient-based Disabilities of the Arm, Shoulder, and
Hand [DASH] questionnaire) upper extremity outcomes.15
|
TABLE 36-4 Cosmesis Following Operative versus Nonoperative Care
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
studies on the primary plate fixation of acute midshaft clavicle
fractures have reported high success rates with union from 94% to 100%
and low rates of infection and surgical complications. A recent
metaanalysis of plate fixation for 460 displaced fractures revealed a
nonunion rate of only 2.2%. With improved implants, prophylactic
antibiotics, and better soft tissue handling, one can conclude that
plate fixation is a reliable and reproducible technique.15,74,125,126,185
of patients, especially those with shortened, displaced fractures, who
would benefit from primary operative repair of clavicular injuries.15,62,139
However, these early interventions are not without risk and consume
significant health care resources. Also, there are patients who appear
to have multiple prognostic factors for a poor outcome following a
clavicular fracture (i.e., displacement greater than 2 cm) and yet heal
promptly (albeit in a “displaced” position) with minimal symptomatology
and full function of the involved shoulder. While some of the
explanation for this is undoubtedly due to the inherent variability of
patient response to musculoskeletal injury, there may be other factors
that are not clearly defined or understood at present. For example,
while most studies use the magnitude of shortening when defining
fracture displacement, this alone is a relatively simplistic linear
measurement of what is typically a complex three-dimensional deformity.
Since most of the major muscle groups of the shoulder have a scapular
origin, it may be that the final position of the scapula relative to
the trunk and upper arm (which is difficult to measure; see “Scapular Winging”) may be the dominant factor in determining prognosis.57 While the prognostic index published by Robinson et al.139
is a dramatic advance in providing objective information and
facilitating our ability to predict outcome, there are still
significant improvements that can be made so that intervention can be
selected specifically for those patients for whom the risk/benefit
ratio of surgery is favorable. It is also clear that patient
noncompliance, especially when associated with substance abuse, is a
clear contraindication for surgery. Bostman et al.,10
in a study of 103 consecutive adults with acute, displaced midshaft
fractures of the clavicle, stated, “Patient noncompliance with the
postoperative regimen could be suspected to have been a major cause of
the failures.”
is for displaced midshaft clavicle fractures in individuals who are
deemed appropriate for surgical fixation. There are proponents of both
IM fixation and plate fixation. The method of plate fixation is also
controversial, with some authorities recommending plate placement on
the superior surface of the clavicle, while others recommend the
anterior/inferior surface.10,15,25,27,74,184
There are no direct comparative studies between these various operative
techniques available at the present time, although it is hoped that
prospective studies that are currently under way comparing these
techniques will clarify the issue. While there are many theoretical
advantages to IM fixation, it appears that the results of this method
with currently available implants are more unpredictable than the
results reported for plate fixation. Biomechanically, they appear to be
inferior in resisting displacement compared with plate fixation.55
Two clinical studies comparing IM fixation to nonoperative treatment
failed to show any advantage in the IM fixation group. Grassi et al.96
described a high complication rate with IM fixation including eight
infections, three “refractures,” two delayed unions, and two nonunions
with hardware failure in 40 patients. Judd et al.,68
in a randomized trial, failed to show an advantage of IM fixation over
nonoperative care in 57 patients, with nearly half the operative group
losing some degree of reduction. The metaanalysis by Zlowodzki et al.185
did not reveal any significant differences between plate and IM
fixation, although this analysis was hampered by the lack of any direct
comparative studies. Conversely, Chuang et al.24
described 100% union with no significant complications in a group of 34
patients with an acute midshaft fractures of the clavicle treated with
an IM cannulated screw. At the present time, IM fixation does not
appear to be as reliable in most series as plate fixation, and it
remains to be seen whether refinements in this technique and the
associated fixation devices can provide more consistent results.
plate irritation than placement of the plate on the superior surface of
the clavicle, at least with previously available plate systems. In the
one direct comparison (nonrandomized) between the two techniques, Lim
et al.82 reported a significantly better pain visual analogue scale for patients in the anteroinferior fixation group (P = 0.05). This finding awaits confirmation from further studies.
treatment is appropriate for most, if not all, fractures of the
clavicle, even severely displaced injuries, with the assumption that
the reconstructive repair of those that developed nonunion or
symptomatic malunion would produce results similar to that of primary
operative repair of the original fracture. Since these injuries are
nonarticular, and the reported “success” rate of reconstruction is
high, this approach seems to have inherent merit. However, there is
recent evidence that while operative reconstruction of malunion or
nonunion is a reliable procedure, with increasing refinement of outcome
measures and objective muscle strength testing, it is apparent that
there are residual deficits compared with what primary operative repair
can provide. Potter et al.128
examined a cohort of 15 patients who had undergone late reconstruction
with plate fixation for clavicular nonunion or malunion (“delayed
group”) a mean of 63 months postinjury and compared them to a similar
cohort of 15 patients who had primary plate fixation of a clavicle
fracture a mean of 0.5 month after injury (“acute group”). The groups
were similar in age, sex, original fracture characteristics, and
mechanism of injury. They found that there were subtle but significant
differences between the two groups with regard to shoulder scores (a
Constant-Murley Shoulder Outcome Score of 89 in the delayed group and
95 in the acute group, P = 0.02), and the
delayed group demonstrated inferior endurance strength in the involved
shoulder. They concluded that while late reconstruction is a reliable
and reproducible procedure, there were subtle decreases in outcome
compared with acute fixation and recommended that this information be
used in decision making when counseling patients with displaced
midshaft fractures of the clavicle. Rosenberg et al.142
reported similar results in a group of 13 patients who had late
reconstruction for clavicular malunion and nonunion. While osseous
healing occurred in all cases, there was a mean 20-point deficit in
Constant-Murley Shoulder Outcome Score (61 versus 81, P
= 0.01) in the affected shoulders. The authors thought that “lasting
functional impairment” was possible even with objective success. With
time, significant adaptive changes (muscle atrophy, soft tissue
contracture, bone loss) occur in the shoulder girdle of individuals
with clavicular malunion or nonunion that will compromise the outcome
of late reconstructive surgery to some degree compared with the results
of primary plate fixation. This is useful, objective information in
evaluating the risk/benefit ratio of early operative intervention.
enhances our knowledge and aids in the decision making regarding the
treatment of fractures of the clavicle. While the majority of clavicle
fractures will heal with nonoperative care (a simple sling is probably
best) and a prompt return of near normal shoulder function can be
expected, there is a subset of fractures that benefit from operative
intervention. Poor prognostic signs include increasing fracture
displacement (especially shortening), fracture comminution, and an
increasing number of fracture fragments, especially in older patients.
In prospective studies of carefully selected patients, operative plate
fixation provides a more rapid return to a superior level of shoulder
function with a consistently low complication rate compared with
nonoperative care. Anteroinferior plate placement may have some
advantages over superior plate positioning with respect to soft tissue
irritation. IM fixation has many theoretical advantages and a high rate
of success in skilled hands, although results in the literature remain
inconsistent. While the difference is small, primary plate fixation
provides significantly improved results in terms of strength and
shoulder scores compared with delayed reconstruction. Malunion of the
clavicle is a definite clinical entity that benefits from corrective
osteotomy, which can usually be performed without a bone graft.
Scapular winging is a common finding following the failure of primary
nonoperative care and the development of a nonunion or a symptomatic
malunion, and it can lead to significant patient symptoms. Future
studies that are randomized, prospective, and comparative are needed to
refine the indications for primary operative repair, investigate the
role that scapular malposition plays, and determine the ideal method of
fixation.
K, Jensen PO, Lauritzen J. The treatment of clavicular fractures:
figure-of-eight bandage versus a simple sling. Acta Orthop Scand
1987;58:71-74.
FT, Gerber C. Coracoclavicular screw fixation for unstable fractures of
the distal clavicle. A report of five cases. J Bone Joint Surg Br
1991;73B:291-294.
FT, Lambert SM, Hertel R. Decortication and plate osetosynthesis for
nonunion of the clavicle. J Shoulder Elbow Surg 1998;7:581-585.
O, Malghem J, Delaere O, et al. Injury to the brachial plexus by a
fragment of bone after fracture of the clavicle. J Bone Joint Surg Br
1997;79B:534-536.
D, Curtis RJ, DeHaan JT, et al. Nonunion of fractures of the midshaft
of the clavicle. Treatment with a modified Haigie intramedullary pin
and autogenous bonegrafting. J Bone Joint Surg Am 1991;73A:1219-1226.
O, Manninen M, Pihlajamaki H. Complications of plate fixation in fresh
displaced midclavicular fractures. J Trauma 1997;43:778-783.
MI, Axelrod TS. Atrophic nonunion of the clavicle: treatment by
compression plate, lag-screw fixation, and bone graft. J Bone Joint
Surg Br 1997;79B:301-303.
N, Hutchinson J, Hahn D, et al. Clavicular nonunion: 31/32 healed after
plate fixation and bone grafting. Acta Orthop Scand 1996;67:367-370.
CT, Pollick SR. Treatment of recalcitrant nonunion with a capacitively
coupled electrical field: a preliminary report. J Bone Joint Surg Am
1985;67A:577-585.
Orthopaedic Trauma Society (MD McKee, principal investigator). Plate
fixation versus nonoperative care for acute, displaced midshaft
fractures of the clavicle. J Bone Joint Surg 2007;89A:1-11.
S. Toward evidence-based emergency medicine: best BETS from the
Manchester Royal Infirmary. Collar and cuff or sling after fracture of
the clavicle. J Accid Emerg Med 1999;16:140.
P, Robertson C, Mahar A, et al. Biomechanical evaluation of clavicle
fracture plating techniques: does a locking plate provide improved
stability? J Orthop Trauma 2008;22:241-247.
CH, Ch WJ, Shih CH. Surgical treatment for distal clavicle fractures
with coracoclavicular ligament disruption. J Trauma 2002;52:7-8.
TY, Ho WP, Hsieh PS, et al. Closed reduction and internal fixation for
acute midshaft clavicular fractures using cannulated screws. J Trauma
2006;60:1315-1321.
C, Devinney S, Herscovici D, et al. Anteroinferior plate fixation of
middle third fractures and nonunions of the clavicle. J Orthop Trauma
2006;20:680-686.
JF, Ganjianpour M. Thoracic outlet syndrome treated by double osteotomy
of a clavicular malunion. J Bone Joint Surg Am 2002;84A:437-440.
EV. Fractures of the clavicle. In: Rockwood CA, Green DP, Bucholz RW,
Heckman JD, eds. Rockwood and Green’s Fractures in Adults.
Philadelphia: Lippincott-Raven, 1996:1109-1161.
EV. Fractures of the clavicle. In: Rockwood CA, Matsen FA, eds. The
Shoulder, 3rd ed. Philadelphia: WB Saunders, 1998:428-482.
AH. Fractures of the shoulder girdle, arm and forearm. In Willis CC,
ed. Campbell’s Operative orthopaedics, 8th ed. St. Louis: Mosby-Year
Book, 1992: 989-995.
PH, Luitse JS, Strating RP, et al. Operative treatment for delayed
union and nonunion of midshaft clavicular fractures: AO reconstruction
plate fixation and early mobilization. J Trauma 1996;40:985-986.
Santa D, Narakas A, Bonnard C. Late lesions of the brachial plexus
after fracture of the clavicle. Ann Chir Main Memb Super
1991;10:531-540.
B, Atesalp AS, Sehirlioglu A, et al. Preliminary results of the use of
Ilizarov fixation in clavicular nonunion. Arch Orthop Trauma Surg
2006;126:401-405.
A, Malhotra SK, Kumar V. A fractured clavicle and vascular compression:
a nonorthopedic indication of figure-of-eight bandage. Anesth Analg
2003;96:910.
NA, Mekhail AO, Darwich M. Open reduction and internal fixation with
bone grafting of clavicular nonunion. J Trauma 1997;42:701-704.
SG, Whittle AP, Wood GW. Nonoperative treatment of ipsilateral
fractures of the scapula and clavicle. J Bone Joint Surg Am
2000;82A:774-780.
SG, Wood GW, Whittle AP. Factors associated with Short Form-36 outcome
in nonoperative treatment for ipsilateral fractures of the clavicle and
scapula. Orthopedics 2002;25:733-738.
KA, Connor PM, Karunakar MA, et al. The floating shoulder: clinical and
functional results. J Bone Joint Surg Am 2001;83A:1188-1194.
TJ, Hartlief MT, Fontijine WP. Rushpin fixation for midshaft clavicular
nonunions: good results in 13/14 cases. Acta Orthop Scand
1999;70:514-516.
A, Vainionpaa S, Myllynen P, et al. Outcome of clavicular fracture in
89 patients. Arch Orthop Trauma Surg 1986;105:337-338.
CY, Chiu FY, Chuang TY, et al. Transacromial Knowles pin in the
treatment of Neer type 2 distal clavicle fractures. A prospective
evaluation of 32 cases. J Trauma 2004;56:1102-1105.
T, Ristiniemi J, Hyvonen P, et al. Surgical treatment of unstable
fractures of the distal clavicle: a comparative study of Kirschner wire
and clavicular hook plate fixation. Acta Orthop Scand 2002;73:50-53.
K, Matsuda K, Sakai Y, et al. Late thoracic outlet syndrome secondary
to malunion of the fractured clavicle: case report and review of the
literature. J Trauma 2001;50: 332-335.
JA, Bruce WJ, Sonnabend DH, et al. Type 2 fractures of the distal
clavicle: a new surgical technique. J Shoulder Elbow Surg
1997;6:380-382.
SR, Oliviero JA, Francke EI, et al. A biomechanical study of plate
versus intramedullary devices for midshaft clavicle fixation. J Orthop
Surg 2008;3:28.
T, Markert RJ, Anderson CG, et al. Biomechanical evaluation of a
precontoured clavicle plate. J Shoulder Elbow Surg 2008;17:815-818.
FA, Tajana MS, D’Angelo F. Management of midclavicular fractures:
comparison between nonoperative treatment and open intramedullary
fixation in 80 patients. J Trauma 2001;50:1096-1100.
JA, Farrugia M, Potter J, et al. The radiographic quantification of
scapular winging following malunuion of displaced clavicular shaft
fractures [abstract]. COA Abstract Supplement 2007;June 1:43.
H, Ito H. Clinical outcome of the treatment of floating shoulder by
osteosynthesis for clavicular fracture alone. J Shoulder Elbow Surg
2003;12:589-591.
D Jr, Fiennes AG, Allgower M, et al. The floating shoulder: ipsilateral
clavicle and scapular neck fractures. J Bone Joint Surg Br
1992;74B:362-364.
JM. Closed treatment of displaced middle-third fractures of the
clavicle gives poor results [letter to the editor]. J Bone Joint Surg
Br 1998;80B:558.
JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third
fractures of the clavicle gives poor results. J Bone Joint Surg Br
1997;79B:537-539.
FM, Shafer SJ. Injuries to the clavicle with neurovascular
complications. A study of 14 cases. J Bone Joint Surg Am
1965;47A:1335-1346.
JI, Toogood P, Chen MR, et al. Clavicular anatomy and the applicability
of precontoured plates. J Bone Joint Surg Am 2007;89A:2260-2265.
PL, Amadio PC, Bombardier C. Development of an upper extremity outcome
measure: The DASH. Upper Extremity Collaborative Group (UECG). Am J Ind
Med 1996;29:602-608.
MR, Crosby LA, Stafford P, et al. Effects of plate location and
selection on the stability of midshaft clavicle osteotomies: a
biomechanical study. J Shoulder Elbow Surg 2002;11:457-462.
A, Andermahr J, Schiffer G, et al. Elastic stable intramedullary
nailing of midclavicular fractures with a titanium nail. Clin Orthop
Relat Res 2003;408:279-285.
DB, Bottoni CR, Pallis MP, et al. Intramedullary fixation versus
nonoperative treatment for midshaft clavicle fractures. In Proceedings
of the 72nd Annual Meeting of the American Academy of Orthopaedic
Surgeons. Washington DC, February 2005.
JB, Leffert RD. Nonunion of the clavicle. Associated complications and
surgical management. J Bone Joint Surg Am 1987;69A:753-760.
JB, Ring D. Fractures of the clavicle. In: Iannotti JP, Williams GR,
eds. Disorders of the Shoulder: Diagnosis and Management. Philadelphia:
Lippincott Williams & Wilkins, 1999.
FC, Chao EK, Chen CH, et al. Treatment of distal clavicle fracture
using Kirschner wires and tension band wires. J Trauma 2001;51:522-525.
SA, Shamshery P, Gupta V et al. Locking compression plate in
longstanding clavicular nonunions with poor bone stock. J Trauma
2008;64:439-441
KC, Rhee KJ, Shin HD, et al. Can the glenopolar angle be used to
predict outcome and treatment of the floating shoulder? J Trauma
2008;64:174-178.
J, Bosse JM, Staeheli JW, et al. Type II distal clavicle fractures: a
retrospective review of surgical treatment. J Orthop Trauma
1990;4:115-120.
M, Leeks N, Ackland T, et al. Short malunions of the clavicle: an
anatomic and functional study. J Shoulder Elbow Surg 2005;14:349-354.
J, Jalovaara P. Migration of Kirschner wires following fixation of the
clavicle: report of 2 cases. Acta Orthop Scand 1999;70:517-519.
KS, Lam TP. Open reduction and internal fixation of ipsilateral
fractures of the scapular neck and clavicle. J Bone Joint Surg Am
1993;75A:1015-1018.
S, Jupiter JB. LC-DC plating with bone graft in posttraumatic nonunions
in the middle third of the clavicle. Swiss Surg 1998;4:89-94.
K, Bassett GS. Complete posterior sternoclavicular epiphyseal
separation. A case report and review of the literature. Clin Orthop
1992;281:84-88.
M, Kang J, Kim K, et al. Anterior inferior reconstruction plates for
the treatment of acute midshaft clavicle fractures. In proceedings from
the 19th Annual Meeting of the Orthopaedic Trauma Society. Salt Lake
City, Utah, October 2003.
JL, Slongo TF, Agel J, et al. Fracture and dislocation classification
compendium: 2007 Orthopaedic Trauma Association Classification,
Database, and Outcomes Committee. J Orthop Trauma 2007;21:S1-S74.
K, Miyamoto K, Sumi H, et al. Upper extremity injuries in snowboarding
and skiing: a comparative study. Clin J Sport Med 2002;12:354-359.
DN, Mowbray MA. Treatment of displaced fractures of the clavicle. Sling
versus figure-of-eight bandage. Practitioner 1979;223:266-267.
MD, Seiler JG, Jupiter JB. The application of the limited contact
dynamic compression plate in the upper extremity: an analysis of 114
consecutive cases. Injury 1995;26:661-666.
MD, Stephen DJG, Kreder HJ, et al. Functional outcome following
clavicle fractures in polytrauma patients. J Trauma 2000;47:616.
MD, Pedersen EM, Jones C, et al. Deficits following non-operative
treatment of displaced, midshaft clavicle fractures. J Bone Joint Surg
Am 2006;88A:35-40.
SH, Heppenstall RB, Brighton CT, et al. Clavicle nonunion: results of
treatment with electricity, AO dynamic compression plating and
autogenous bone grafting, and excision of the nonunion in 43 patients.
Orthop Trans 1994;18:1072.
J, Maraval M, Kieffer E, et al. Fractures of the clavicle and injuries
of the subclavian artery. Report of 10 cases. J Cardiovasc Surg
(Torino) 1975;16:541-547.
C. Fractures of the clavicle. In: Rockwood CA, Green DP, eds. Fractures
in Adults, 2nd ed. Philadelphia: JB Lippincott, 1984:707-713.
RJ, Neviaser JS, Neviaser TJ. A simple technique for internal fixation
of the clavicle. A long term evaluation. Clin Orthop 1975;109:103-107.
C, Parkpian V, Patradul A. Fixation of fractures of the midshaft of the
clavicle with Kirschner wires. Results in 108 patients. J Bone Joint
Surg Br 1998;80B: 106-108.
A, Petersson C, Redlund-Johnell I. The natural course of lateral
clavicle fracture. Fifteen (11-21) year follow-up of 110 cases. Acta
Orthop Scand 1993;64: 87-91.
A, Petersson CJ, Redlund-Johnell I. Midclavicle fractures in adults:
end result study after conservative treatment. J Orthop Trauma
1998;12:572-576.
J, Holgersson M, Larsson S. Can we predict long-term sequelae after
fractures of the clavicle based on initial findings? A prospective
study with 9 to 10 years follow-up. J Shoulder Elbow Surg
2004;13:479-486.
J, Mallmin H, Larson S. The aetiology and epidemiology of clavicular
fractures. A prospective study during a 2-year period in Uppsala,
Sweden. Injury 2000;35: 353-358.
D, Kutty S, McCabe JP. Long-term functional outcome assessment of plate
fixation and autogenous bone grafting for clavicular nonunion. Injury
2004;35: 575-579.
CW, Kyung HS, Kim PT, et al. Failure of internal fixation of the
clavicle in the treatment of ipsilateral clavicle and glenoid neck
fractures. J Orthop Sci 2002;6: 601-603.
BS, Vaesel MT, Sojbjerg JO. Treatment of midshaft clavicular nonunion
with plate fixation and autologous bone grafting. J Shoulder Elbow Surg
1995;4:337-344.
RA, Langdon JD. Stress fracture of the clavicle. A rare late
complication of radical neck dissection. J Maxillofac Surg
1986;14:281-284.
MS, Kristiansen B, Thomsen F, et al. [Conservative treatment of
clavicular fractures.] Ugesker Laeger 1993;155:3832-3834.
J, Reiler T, Fischer W. [Plating of fresh clavicular fractures.
Experience with 60 operations.] Unfallchirurgie 1988;14:26-37.
J, Lones C, Wild LM, et al. Does delay matter? The restoration of
objectively measured shoulder strength and patient-oriented outcome
after immediate fixation versus delayed reconstruction of displaced
midshaft fractures of the clavicle. J Shoulder Elbow Surg
2007;16:514-518.
L, Mencia R, Alonso A, et al. Conservative treatment of ipsilateral
fractures of the scapula and clavicle. J Trauma 1997;42:239-242.
HN, Nakajima T, Hamada K, et al. Winging of the scapula caused by
disruption of “sternoclavicular linkage”: report of two cases. J
Shoulder Elbow Surg 2000;9:144-147.
D, Seiber G. Early secondary lesions of the brachial plexus: a rare
complication following clavicular fracture. Unfallchirurgie
1987;13:91-92.
RJ, de Bruijin AJ, Aarts HC, et al. Endovascular treatment of a
pseudoaneurysm of the subclavian artery. J Trauma 2003;55:969-971.
BL, Butterfield SL, Daffner RH, et al. The abduction lordotic view of
the clavicle: a new technique for radiographic visualization. J Orthop
Trauma 1991;5:392-394.
D, Regazzoni P, Renner N. The unstable shoulder girdle: early
functional treatment utilizing open reduction and internal fixation. J
Orthop Trauma 1995;9:93-97.
D, Holovacs T. Brachial plexus palsy after intramedullary fixation of a
clavicle fracture. J Bone Joint Surg Am 2005;87A:1834-1836.
CM, Cairns DA. Primary nonoperative treatment of displaced lateral
fractures of the clavicle. J Bone Joint Surge Am 2004;86A:778-782.
CM, Court-Brown CM, McQueen MM, et al. Estimating the risk of nonunion
following nonoperative treatment of a clavicle fracture. J Bone Joint
Surg Am 2004; 86A:1359-1365.
AS, Eisenberg DP, Gallagher MA, et al. A comparison of nonoperative and
operative treatment of type II distal clavicle fractures. Bull Hosp
Joint Dis 2003;61: 32-39.
N, Neumann L, Wallace AW. Functional outcome of surgical treatment of
symptomatic nonunion and malunion of midshaft clavicle fractures. J
Shoulder Elbow Surg 2007;16:510-513.
KM, Da Silva VF, Preston DN, et al. Brachial-plexus injury after
clavicular fracture: case report and literature review. Can J Surg
1991;34:264-266.
R, Visconti V, Lorini S, et al. Displaced comminuted midshaft clavicle
fractures: Use of Mennen plate fixation system. J Trauma
2007;63:951-954.
F, Pay-Pay E, Andrianne Y, et al. External fixation of the clavicle for
fracture or nonunion in adults. J Bone Joint Surg Am 1988;70A:692-695.
GS, Aoki J, Karakida O, et al. Case report: nonunion of a medical
clavicular fracture following radical neck dissection: MRI diagnosis.
Orthopedics 1999;22:985-986.
SR. Taming of the screw: a case report and literature review of
limb-threatening complications after plate osteosynthesis of a
clavicular nonunion. J Trauma 2003; 55:840-843.
JS, Glaser DL, Drezner JA. Distal clavicular stress fracture in a
female weight lifter: a case report. Am J Sports Med 2004;32:1755-1758.
CA, Rudd J, Crosby LA. Results of operative versus nonoperative
treatment for 100% displaced midshaft clavicle. Proceedings from the
16th Annual Open Meeting of the American Shoulder and Elbow Surgeons,
March 18, 2000, p 41.
V, Deml C, Irenberger A et al. Length determination in midshaft
clavicle fractures: validation of measurement. J Orthop Trauma
2008;22:458-462
J, Dietrich CT, Kotajarvi BR, et al. The effect of scapular protraction
on isometric shoulder rotation strength in normal subjects. J Shoulder
Elbow Surg 2006;15: 339-343.
EE, Kuhn JE. Biomechanical analysis of reconstructions for
sternoclavicular joint instability. J Bone Joint Surg Am
2004;86A:98-105.
D, Trowbridge EA, Norris SH. The mechanism of clavicular fracture. A
clinical and biochemical analysis. J Bone Joint Surg Br
1988;70B:461-464.
S, Bumbasirevic M, Lesic A, et al. Modification of the Ilizarov
external fixator for aseptic hypertrophic nonunion of the clavicle: an
option for treatment. J Orthop Trauma 2006;20:122-128.
DH, Slabaugh PB, Carlson PA. Injury to the axillary artery by a closed
fracture of the clavicle. A case report. J Bone Joint Surg Am
1980;62A:1372-1374.
O, Pittoors K, Van Glabbeek F, et al. Plate Fixation of middle-third
factures of the clavicle in the semiprofessional athlete. Acta Orthop
Belg 2005;71:17-21.
B, Seife B, Alonso P. The apical oblique view of the clavicle: its
usefulness in neonatal and childhood trauma. Skeletal Radiol
1991;20:201-203.
RR, Anson PS, Kristiansen T, et al. Adult clavicle fractures:
relationship between mechanism of injury and healing. Orthop Trans
1989;13:514-515.
M, Muller EJ, Kollig E, et al. Midshaft fractures of the clavicle with
a shortening of more than 2 cm predispose to nonunion. Arch Orthop
Trauma Surg 2001;121: 207-211.
GR, Koffler K, Pepe M, et al. Rotation of the clavicular portion of the
pectoralis major for soft-tissue coverage of the clavicle. An
anatomical study and case report. J Bone Joint Surg Am
2000;82A:1736-1742.
GR, Naranja J, Klimkiewicz J, et al. The floating shoulder: a
biomechanical basis for classification and management. J Bone Joint
Surg Am 2001;83A:1182-1187.
GR Jr, Silverberg DA, Iannotti JP, et al. Nonoperative treatment of
ipsilateral clavicle and glenoid neck fractures. American Shoulder and
Elbow Surgeons 15th Open Meeting, Anaheim, CA, 1999.
CC, Shin CM, Chen WJ, et al. Treatment of clavicular aspectic nonunion:
Comparison of plating and intramedullary nailing techniques. J Trauma
1999;45:512-516.
H, Arakawa H, Kobayashi M. Results of the Bosworth method for unstable
fractures of the distal clavicle. Int Orthop 1998;22:366-368.
KR, Ray S, Neer CS 2nd. Conservative management of a displaced medial
clavicular physeal injury in an adolescent athlete. A case report and
literature review. Am J Sports Med 1989;17:833-836.
BA, Pape HC, Gerich TG, et al. Functional outcome following
scapulo-thoracic dissociation. J Bone Joint Surg Am 2004;86A:2-8.
EJ Jr, Krieg JK, Rosen MJ. Open reduction and internal fixation of
clavicular fractures. J Bone Joint Surg Am 1981;63A:147-151.
M, Zelle BA, Cole PA, et al. Treatment of midshaft clavicle fractures:
systemic review of 2144 fractures. J Orthop Trauma 2005;19:504-507.
