CHAPTER 66 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
Section – Surgical Techniques of the Posterior Cruciate Ligament and Posterolateral Corner
CHAPTER 66 – Transtibial Tunnel Posterior Cruciate Ligament Reconstruction
Craig J. Edson, MS, PT, ATC,
Kristin N. Reinheimer, PAC,
Raffaele Garofalo, MD
The incidence of posterior cruciate ligament (PCL) injuries is reported to be 1% to 40% of acute knee injuries. This range depends on the population of patients described, and the incidence is approximately 3% in the general population and 38% in reports from regional trauma centers. [2] [3] [8] Our practice at a regional trauma center has a 38.3% incidence of PCL tears in acute knee injuries, and 56.5% of these PCL injuries occur in patients with multiple trauma. Of these PCL injuries, 45.9% are combined anterior cruciate ligament (ACL) and PCL tears; 41.2% are PCL–posterolateral corner tears. Only 3% of acute PCL injuries seen in the trauma center are isolated.
This chapter illustrates my (G. C. F.) surgical techniques for the arthroscopic single-bundle/single femoral tunnel and double-bundle/double femoral tunnel transtibial PCL reconstruction. We also present the Fanelli Sports Injury Clinic 2- to 10-year results of PCL reconstruction by this surgical technique. The information presented in this chapter has also been presented elsewhere, and the reader is referred to these sources for additional information about this topic. [1] [4] [5] [6] [7] [9] [10] [11] [12] [13] [14] [15] [16] [17] [18] [19] [20]
The single-bundle/single femoral tunnel transtibial PCL reconstruction is an anatomic reconstruction of the anterolateral bundle of the PCL. The anterolateral bundle tightens in flexion, and this reconstruction reproduces that biomechanical function. Whereas the single-bundle/single femoral tunnel transtibial PCL reconstruction does not reproduce the broad anatomic insertion site of the normal PCL, there are certain factors that lead to success with this surgical technique:
History and Physical Examination
The typical history of a patient with a PCL injury includes a direct blow to the proximal tibia with the knee in 90 degrees of flexion. Hyperflexion, hyperextension, and a direct blow to the proximal medial or lateral tibia in varying degrees of knee flexion as well as a varus or valgus force will induce PCL-based multiple ligament knee injuries.
Physical examination of the injured knee compared with the noninjured knee reveals a decreased tibial step-off and a positive result of the posterior drawer test. Because concomitant collateral ligament injury is common (posterolateral and posteromedial corner injuries), posterolateral and posteromedial drawer tests, dial tests, and external rotation recurvatum tests may elicit abnormal results; varus and valgus laxity and even anterior laxity may be present.
PCL–Posterolateral Corner Injury
Plain radiographs to evaluate PCL injuries include the following views:
Magnetic resonance imaging is helpful in acute cases, but we have found it to be less beneficial in chronic PCL injuries. Bone scan is used in chronic cases of PCL instability presenting with pain to define early degenerative joint disease.
Our indications for surgical treatment of acute PCL injuries include insertion site avulsions, tibial step-off decreased 6 to 10 mm or more, and PCL tears combined with other structural injuries. Surgical treatment of chronic PCL injuries is indicated when an isolated PCL tear becomes symptomatic as demonstrated by progressive functional instability.
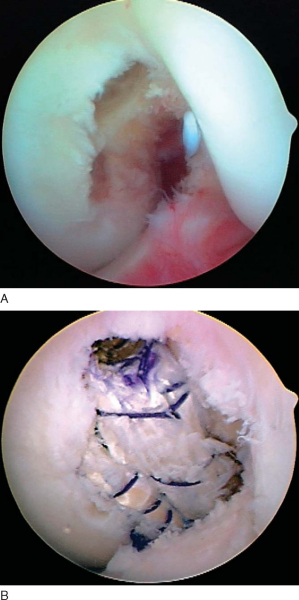
The patient is positioned on the operating table in the supine position, and the surgical and nonsurgical knees are examined under general or regional anesthesia. A tourniquet is applied to the operative extremity, and the surgical leg is prepared and draped in a sterile fashion. Allograft tissue is prepared before the surgical procedure is begun, and autograft tissue is harvested before the arthroscopic portion of the procedure. The arthroscopic instruments are inserted with the inflow through the superior lateral patellar portal, the arthroscope in the inferior lateral patellar portal, and the instruments in the inferior medial patellar portal. The portals are interchanged as necessary. The joint is thoroughly evaluated arthroscopically, and the PCL is evaluated by the three-zone arthroscopic technique.[13] The PCL tear is identified, and the residual stump of the PCL is débrided with hand tools and the synovial shaver.
Specific Steps (
Box 66-1
)
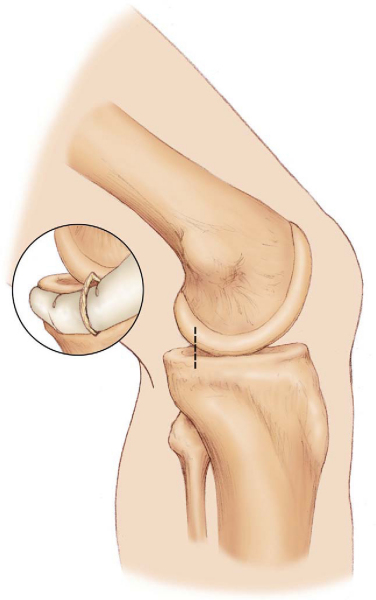
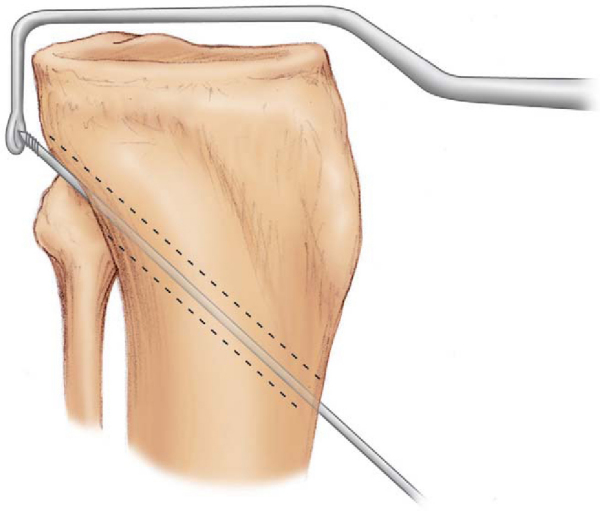
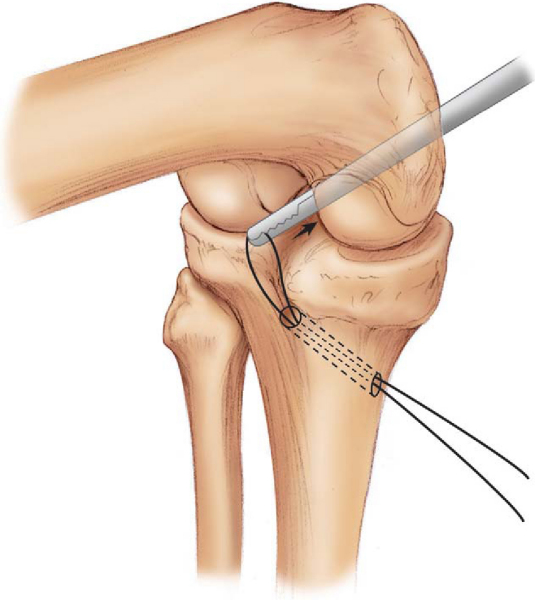
An extracapsular posteromedial safety incision approximately 1.5 to 2.0 cm long is made (
Fig. 66-1
). The crural fascia is incised longitudinally, with precautions taken to protect the neurovascular structures. The interval is developed between the medial head of the gastrocnemius muscle and the posterior capsule of the knee joint, which is anterior. The surgeon’s gloved finger is positioned so that the neurovascular structures are posterior to the finger and the posterior aspect of the joint capsule is anterior to the surgeon’s finger. This technique enables the surgeon to monitor surgical instruments, such as the over-the-top PCL instruments and the PCL-ACL drill guide, as they are positioned in the posterior aspect of the knee. The surgeon’s finger in the posteromedial safety incision also confirms accurate placement of the guide wire before tibial tunnel drilling in the medial-lateral and proximal-distal directions (
Fig. 66-2
). This is the same anatomic surgical interval that is used in the tibial inlay posterior approach.
|
|
|
|
Figure 66-1 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
|
|
|
|
Figure 66-2 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
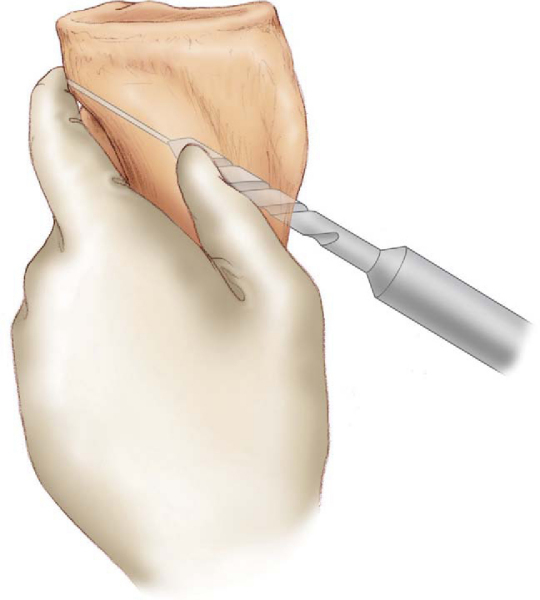
2. Elevation of the Posterior Capsule
The curved over-the-top PCL instruments are used to carefully lyse adhesions in the posterior aspect of the knee and to elevate the posterior knee joint capsule away from the tibial ridge on the posterior aspect of the tibia. This capsular elevation enhances correct drill guide and tibial tunnel placement (
Fig. 66-3
).
|
|
|
|
Figure 66-3 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
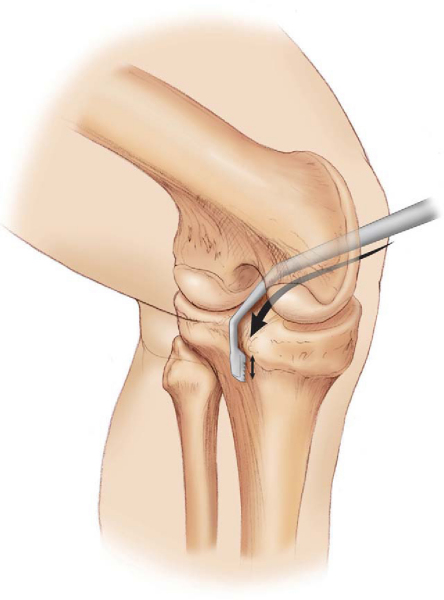
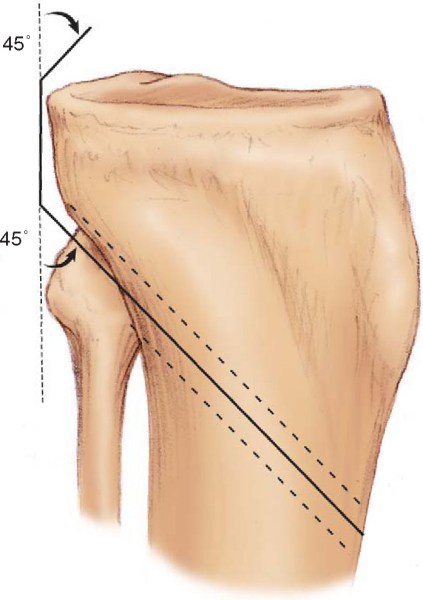
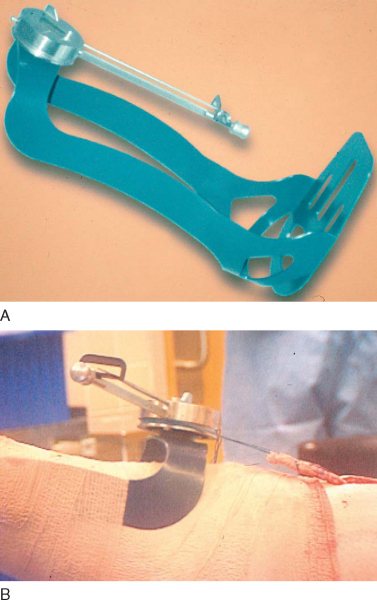
The arm of the Arthrotek Fanelli PCL-ACL drill guide is inserted into the knee through the inferior medial patellar portal and positioned in the PCL fossa on the posterior tibia (
Fig. 66-4
). The bullet portion of the drill guide contacts the anterior medial aspect of the proximal tibia approximately 1 cm below the tibial tubercle, at a point midway between the tibial crest anteriorly and the posterior medial border of the tibia. This drill guide positioning creates a tibial tunnel that is relatively vertically oriented and has its posterior exit point in the inferior and lateral aspect of the PCL tibial anatomic insertion site. This positioning creates an angle of graft orientation such that the graft will make two smooth 45-degree angle turns on the posterior aspect of the tibia, eliminating a 90-degree graft angle referred to as the “killer turn” (
Fig. 66-5
).
|
|
|
|
Figure 66-4 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
|
|
|
|
Figure 66-5 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
The tip of the guide in the posterior aspect of the tibia is confirmed with the surgeon’s finger through the extracapsular posteromedial safety incision (see
Fig. 66-2
). Intraoperative anteroposterior and lateral radiographs may also be obtained, as well as arthroscopic visualization to confirm drill guide and guide pin placement. A blunt spade-tipped guide wire is drilled from anterior to posterior and can be visualized with the arthroscope, in addition to being palpated with the finger in the posteromedial safety incision. We consider the finger in the posteromedial safety incision the most important step for accuracy and safety.
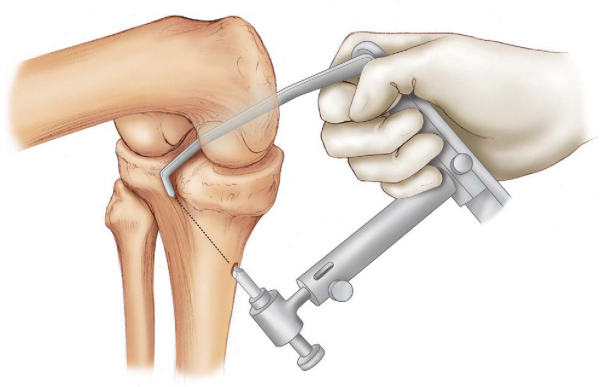
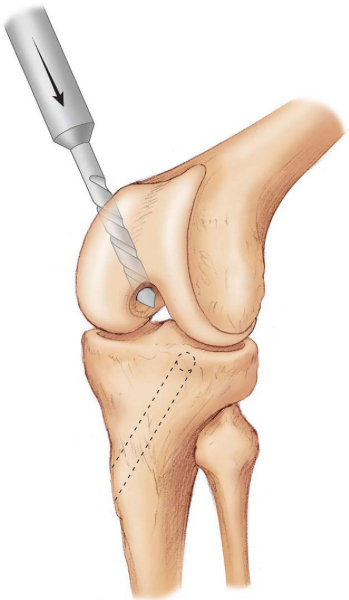
The appropriately sized standard cannulated reamer is used to make the tibial tunnel. The closed curved PCL curet may be positioned to cup the tip of the guide wire (
Fig. 66-6
). The arthroscope, when it is positioned in the posteromedial portal, visualizes the guide wire being captured by the curet and ensures protection of the neurovascular structures. The surgeon’s finger in the posteromedial safety incision is monitoring the position of the guide wire. The standard cannulated drill is advanced to the posterior cortex of the tibia. The drill chuck is then disengaged from the drill, and completion of the tibial tunnel reaming is performed by hand. This gives an additional margin of safety for completion of the tibial tunnel. The tunnel edges are chamfered and rasped with the PCL-ACL system rasp (
Fig. 66-7
).
|
|
|
|
Figure 66-6 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
|
|
|
|
Figure 66-7 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
5. Drilling of the Femoral Tunnel
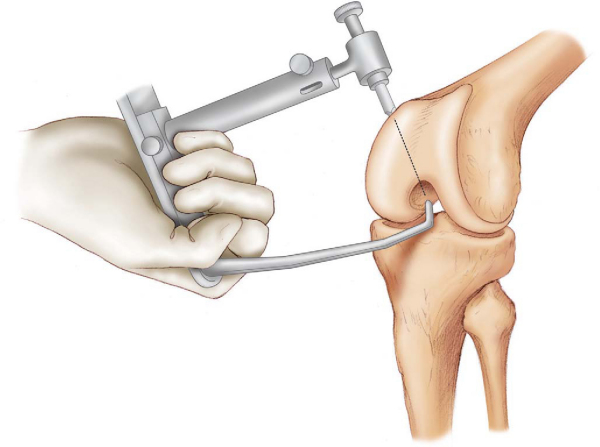
The Arthrotek Fanelli PCL-ACL drill guide is positioned to drill the femoral tunnel (
Fig. 66-8
). The arm of the guide is introduced into the knee through the inferior medial patellar portal and positioned such that the guide wire will exit through the center of the stump of the anterolateral bundle of the PCL. The blunt spade-tipped guide wire is drilled through the guide, and just as it begins to emerge through the center of the stump of the anterolateral bundle of the PCL, the drill guide is disengaged. The accuracy of the guide wire position is confirmed arthroscopically by probing and direct visualization. Care must be taken to ensure that the patellofemoral joint has not been violated by arthroscopic examination of the patellofemoral joint before drilling of the femoral tunnel.
|
|
|
|
Figure 66-8 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
The appropriately sized standard cannulated reamer is used to make the femoral tunnel over a guide wire from outside in or from inside out per the surgeon’s preference (
Fig. 66-9
). When the double-bundle/double femoral tunnel surgical technique is performed, the two tunnels are placed at the anatomic insertion sites of the anterolateral and posteromedial bundles to approximate the anatomic footprint of the PCL femoral insertion site (
Fig. 66-10
). The reaming debris is evacuated with a synovial shaver to minimize fat pad inflammatory response with subsequent risk of arthrofibrosis. The tunnel edges are chamfered and rasped.
|
|
|
|
Figure 66-9 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
|
|
|
|
Figure 66-10 |
6. Tunnel Preparation and Graft Passage
The Arthrotek Magellan suture-passing device is introduced through the tibial tunnel and into the knee joint; it is retrieved through the femoral tunnel with an arthroscopic grasping tool (
Fig. 66-11
). The traction sutures of the graft material are attached to the loop of the Arthrotek Magellan suture-passing device, and the PCL graft material is pulled into position.
|
|
|
|
Figure 66-11 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
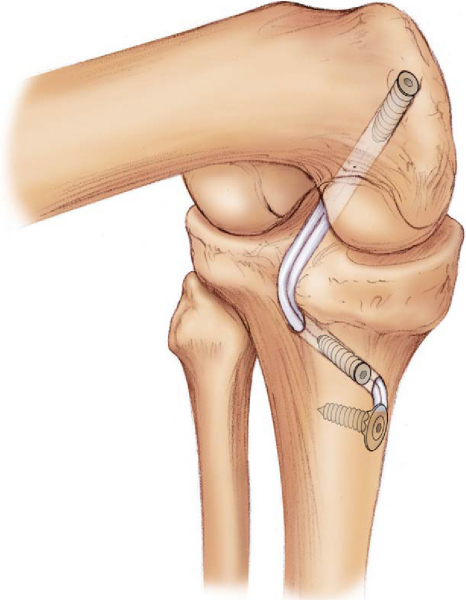
7. Graft Tensioning and Fixation
Fixation of the PCL substitute is accomplished with primary and backup fixation on both the femoral and tibial sides. Our preferred graft source for PCL reconstruction is the Achilles tendon allograft alone for single-bundle reconstructions and Achilles tendon and tibialis anterior allografts for double-bundle reconstructions. Femoral fixation is accomplished by cortical suspensory backup fixation with polyethelene ligament fixation buttons, and aperture opening fixation is achieved with the Arthrotek Bio-Core bioabsorbable interference screws. The Arthrotek graft tensioning boot is applied to the traction sutures of the graft material on its distal end, set for 20 pounds, and the knee is cycled through 25 full flexion-extension cycles for graft pretensioning and settling (
Fig. 66-12
). During single-bundle PCL reconstructions, the graft is tensioned in approximately 70 degrees of knee flexion. During double-bundle reconstructions, the anterolateral bundle is tensioned at approximately 70 degrees of knee flexion, and the posteromedial bundle is tensioned at approximately 30 degrees of knee flexion. Tibial graft fixation is achieved with primary aperture opening fixation with the Arthrotek Bio-Core bioabsorbable interference screw; backup fixation is performed with a ligament fixation button or screw and post or screw and spiked ligament washer assembly (
Fig. 66-13
).
|
|
|
|
Figure 66-12 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
|
|
|
|
Figure 66-13 (Redrawn with permission of Arthrotek, Inc., Warsaw, Ind.) |
When multiple ligament surgeries are scheduled at the same operative session, the PCL reconstruction is performed first, followed by the ACL reconstruction, followed by the collateral ligament surgery. The reader is referred to other sections of this textbook for descriptions of multiple ligament surgeries of the knee. At the completion of the procedure, the tourniquet is deflated, and the wounds are irrigated. The incisions are closed in the standard fashion.
The knee is immobilized in a long leg brace in full extension for 6 weeks, with non–weight bearing with use of crutches. Progressive range of motion occurs during weeks 4 through 6. The brace is unlocked between 3 and 6 weeks, and progressive weight bearing at 25% body weight per week is instituted during postoperative weeks 7 through 10. The crutches are discontinued at the end of postoperative week 10. Progressive strength training and range-of-motion exercises are performed. Return to sports and heavy labor occurs after the sixth to ninth postoperative month, when sufficient strength, range of motion, and proprioceptive skills have returned.
PCL reconstruction is technically demanding surgery. Complications encountered with this surgical procedure include failure to recognize associated ligament injuries, neurovascular complications, persistent posterior sag, osteonecrosis, knee motion loss, anterior knee pain, and fractures. A comprehensive preoperative evaluation, including an accurate diagnosis, a well-planned and carefully executed surgical procedure, and a supervised postoperative rehabilitation program, will help reduce the incidence of these complications.
| PEARLS AND PITFALLS | ||||||||||||||||||||||||
|
Fanelli Sports Injury Clinic Results
After PCL reconstruction by the single-bundle surgical technique tensioned with the Arthrotek graft tensioning boot, both a normal posterior drawer test result and a normal tibial step-off are restored in 86.6% of the combined ACL-PCL reconstruction group[12] and in 91.7% of the PCL–posterolateral reconstruction group.[11] These results are outlined in
Table 66-1
.
| Author | Followup | Outcome |
|---|---|---|
| Fanelli and Edson[10] (2002) | 2 to 10 years | 46.0% normal posterior drawer test results and tibial step-offs, and 54.0% grade 1 posterior drawer and tibial step-offs in combined ACL-PCL reconstructions; no Arthrotek graft tensioning boot was used |
| Fanelli and Edson[11] (2004) | 2 to 10 years | 70% normal posterior drawer test results and tibial step-offs for the overall study group, and 91.7% normal posterior drawer test results and tibial step-offs in the subgroup with the Arthrotek graft tensioning boot in combined PCL-posterolateral reconstructions |
| Fanelli et al[12] (2005) | 2 years | 86.6% normal posterior drawer test results and tibial step-offs in combined ACL-PCL reconstructions with the Arthrotek graft tensioning boot |
The arthroscopically assisted single-bundle transtibial PCL reconstruction technique is a reproducible surgical procedure. There are documented results demonstrating statistically significant improvements from preoperative to postoperative status evaluated by physical examination, knee ligament rating scales, arthrometer measurements, and stress radiography. Factors contributing to the success of this surgical technique include identification and treatment of all pathologic changes (especially posterolateral instability), accurate tunnel placement, placement of strong graft material at anatomic graft insertion sites, minimization of graft bending, performance of final graft tensioning at 70 to 90 degrees of knee flexion with the Arthrotek graft tensioning boot, use of primary and backup fixation, and appropriate postoperative rehabilitation program. Because of a more anatomic reconstruction, double-bundle reconstruction may provide better results. This will need to be demonstrated in long-term clinical studies.
1.
Arthrotek PCL Reconstruction Surgical Technique Guide : Fanelli PCL-ACL Drill Guide System,
Warsaw, Ind, Arthrotek, Inc., 1998.
2.
In: Daniel DM, Akeson W, O’Conner J, ed. Knee Ligaments: Structure, Function, Injury, and Repair,
New York: Raven Press; 1990.
3.
Fanelli GC: Posterior cruciate ligament injuries in trauma patients.
Arthroscopy 1993; 9:291-294.
4.
Fanelli GC: Arthroscopic posterior cruciate ligament reconstruction: single bundle/single femoral tunnel.
Arthroscopy 2000; 16:725-731.
5.
Fanelli GC: Arthroscopic evaluation of the PCL.
In: Fanelli GC, ed. Posterior Cruciate Ligament Injuries. A Guide to Practical Management,
New York: Springer-Verlag; 2001.
6.
Fanelli GC: Arthroscopic PCL reconstruction: transtibial technique.
In: Fanelli GC, ed. Posterior Cruciate Ligament Injuries. A Guide to Practical Management,
New York: Springer-Verlag; 2001.
7.
Fanelli GC: Complications in PCL surgery.
In: Fanelli GC, ed. Posterior Cruciate Ligament Injuries. A Guide to Practical Management,
New York: Springer-Verlag; 2001.
8.
Fanelli GC, Edson CJ: Posterior cruciate ligament injuries in trauma patients. Part II.
Arthroscopy 1995; 11:526-529.
9.
Fanelli GC, Edson CJ: Management of posterior cruciate ligament and posterolateral instability of the knee.
In: Chow J, ed. Advanced Arthroplasty,
New York: Springer-Verlag; 2001.
10.
Fanelli GC, Edson CJ: Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction: 2- to 10-year followup.
Arthroscopy 2002; 18:703-714.
11.
Fanelli GC, Edson CJ: Combined posterior cruciate ligament–posterolateral reconstruction with Achilles tendon allograft and biceps femoris tendon tenodesis: 2- to 10-year followup.
Arthroscopy 2004; 20:339-345.
12.
Fanelli GC, Edson CJ, Orcutt DR, et al: Treatment of combined anterior cruciate–posterior cruciate ligament–medial-lateral side knee injuries.
J Knee Surg 2005; 28:240-248.
13.
Fanelli GC, Giannotti B, Edson C: The posterior cruciate ligament: arthroscopic evaluation and treatment.
Arthroscopy 1994; 10:673-688.
14.
Fanelli GC, Giannotti BF, Edson CJ: Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction.
Arthroscopy 1996; 12:5-14.
15.
Fanelli GC, Giannotti B, Edson CJ: Arthroscopically assisted posterior cruciate ligament/posterior lateral complex reconstruction.
Arthroscopy 1996; 12:703-714.
16.
Fanelli GC, Monahan TJ: Complications of posterior cruciate ligament reconstruction.
Sports Med Arthrosc Rev 1999; 7:296-302.
17.
Fanelli GC, Monaghan TJ: Complications and pitfalls in posterior cruciate ligament reconstruction.
In: Malek MM, Fanelli GC, Johnson D, Johnson D, ed. Knee Surgery: Complications, Pitfalls, and Salvage,
New York: Springer-Verlag; 2001.section eds.
18.
Fanelli GC, Monaghan TJ: Complications in posterior cruciate ligament and posterolateral complex surgery.
Oper Tech Sports Med 2001; 9:96-99.
19.
Malek MM, Fanelli GC: Technique of arthroscopically assisted PCL reconstruction.
Orthopedics 1993; 16:961-966.
20.
Miller MD, Cooper DE, Fanelli GC, et al: Posterior cruciate ligament: current concepts.
Instr Course Lect 2002; 51:347-351.