CHAPTER 49 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 49 – Arthroscopic Meniscus Transplantation: Bone Plug
Thomas L. Wickiewicz, MD
The intact meniscus serves a number of functions in the knee; it increases the tibiofemoral contact area, decreases tibiofemoral contact pressures, provides shock absorption, and aids in joint stability, all of which are beneficial to the underlying articular cartilage. With this improved understanding of the importance of the meniscus, there has been an increased emphasis on the repair of meniscal tears, with indications extending to complex tears and tears in avascular regions. Even with these advanced techniques, there are tears not amenable to repair, for which total or subtotal meniscectomy may be required for symptomatic relief. For these patients, there are few options to slow the known progression of articular cartilage degeneration.[3] First reported in 1881, meniscal allograft transplantation is one option.[14] Several studies have shown that for the ideally suited meniscus-deficient patient, with pain localized to the tibiofemoral compartment and no evidence of advanced degenerative changes, a predictable reduction of pain and improved function can result. [5] [6] [15]
A thorough history and physical examination are critical to the appropriate selection of meniscal allograft transplantation candidates. A pertinent history focuses on the location, character, duration, and quality of pain and any associated swelling or mechanical symptoms. Antecedent trauma or any exacerbating events, such as instability episodes, should be documented along with any history of prior surgery. Prior operative reports, including a detailed description of the procedures performed and comments on the status or quality of the articular cartilage, can be helpful in the surgical decision-making process. It is also imperative to rule out other potential sources of pain, including complex regional pain syndrome, in the patient who has likely had multiple operations. Classic signs and symptoms of meniscus-deficient patients include tibiofemoral joint pain, joint effusion, and a history of prior surgery with total or subtotal meniscectomy.
Routine knee physical examination includes inspection of gait and axial alignment; assessment of range of motion; and evaluation for effusion, joint line tenderness to palpation, and crepitus. Healed incisions should correspond with prior surgeries as gleaned from the surgical history, most notably prior meniscal surgery. Instability examination should be performed to evaluate the cruciates, collaterals, and posterolateral corner. Instability that is detected can be addressed with either staged or combined reconstructive procedures.
Plain radiographic evaluation includes standing posteroanterior, flexion standing posteroanterior, flexion lateral, Merchant, and standing hip-to-ankle radiographs. Standing views are critical for the evaluation of the remaining tibiofemoral joint space; standing flexion views specifically examine the posterior weight-bearing portions of the femur. Degenerative changes on plain radiographs include a decreased joint space, osteophytes, flattening of the posterior femoral condyles, and increased concavity of the tibial plateau. Hip-to-ankle views are important for assessing the mechanical axis of the lower extremity for possible staged or combined corrective osteotomies.
High-resolution magnetic resonance imaging with the appropriate cartilage-specific sequences is useful in the assessment of the meniscus and, more important, in the assessment of the articular cartilage. Magnetic resonance imaging is sensitive and can be used to detect early changes in the articular cartilage manifested as subchondral marrow edema, subchondral remodeling, softening, and fibrillation. These sequences can be useful in deciding whether the patient will be a realistic candidate for transplantation.
Bone scan has also been described for the evaluation of the articular cartilage. Increased uptake is indicative of early degenerative changes in the compartment that are often not manifested on plain film or at the time of arthroscopy.
Preoperative sizing of the meniscal allograft for transplantation is critical for its optimal mechanical function. Plain radiographs, computed tomographic scans, and magnetic resonance images have all been used for preoperative sizing, with no real agreement in the literature as to the best method.[12] Our current method is to use plain radiographs (with an appropriate-size marker) and magnetic resonance images to determine tibial plateau dimensions and then to obtain a matching plateau with an attached meniscus for transplantation.
Indications and Contraindications
Meniscal transplantation is indicated for a meniscus-deficient patient with symptoms of pain in the tibiofemoral compartment and no evidence of advanced degenerative changes on imaging.
Contraindications for meniscal transplantation are advanced degenerative changes, prior joint infection, and axial malalignment or joint instability for which the patient refuses to undergo combined or staged osteotomy or ligament reconstruction. We have not used age criteria as a strict contraindication; however, the likelihood of an older patient’s satisfying all of the criteria is significantly decreased.
There are numerous techniques for meniscal allograft transplantation. Here we describe the arthroscopic plug technique, which we think is ideally suited for the medial meniscus. On the lateral side, we prefer some of the other techniques using a bone bridge because of the proximity of the anterior and posterior horns. These anatomic considerations are important because of the close apposition of the tunnels required on the lateral side and also the increased potential for problems when an additional tunnel for anterior cruciate ligament reconstruction is added.
Before the induction of anesthesia, the graft is thawed and inspected. Potential problems at this time include a damaged graft and the incorrect side, which would result in cancellation of the case before the patient receives an anesthetic. We use only fresh-frozen nonirradiated grafts from a certified and trusted tissue bank.
With a satisfactory, appropriately sized graft in the room, anesthesia is then induced with a regional or general agent. The patient is then placed in the supine position on the operating room table. A well-padded nonsterile tourniquet is placed on the upper thigh in addition to a well-padded thigh post for the application of valgus stress.
Specific Steps (
Box 49-1
)
The room setup is important with appropriate positioning of the patient, camera equipment, and anesthesia staff to maximize efficiency and to minimize the risk of contamination. A separate table for graft preparation should be set up with the appropriate equipment, including oscillating saw, drill, and additional instruments for graft preparation.
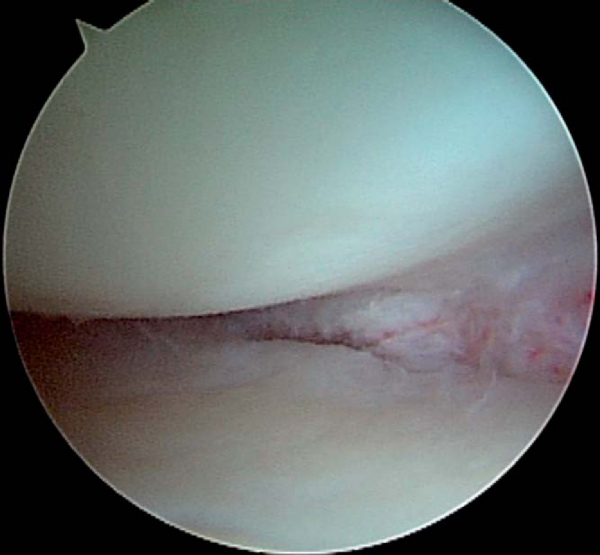
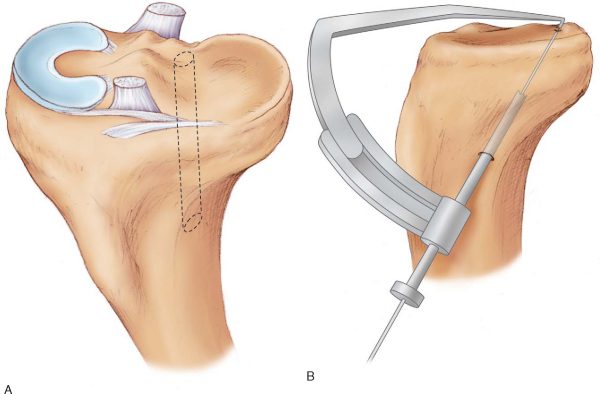
The extremity is prepared from the tourniquet distally with povidone-iodine (Betadine) and draped with a nonimpervious stockinette, half sheets, and an extremity drape. After a standard examination under anesthesia, any combined corrective osteotomies are performed first, followed by a standard diagnostic arthroscopy. Arthroscopy is performed by use of the standard anterolateral viewing portal, anteromedial instrumentation portal, and superomedial or superolateral outflow portal. Diagnostic arthroscopy is useful for confirming the diagnosis and also assessing the status of the articular cartilage. At our institution, the status of the cartilage is assessed preoperatively by cartilage-sensitive magnetic resonance imaging. Without these special sequences, it may be important to counsel the patient that the decision to proceed with meniscal transplantation is contingent on the suitability of the articular cartilage. After completion of the diagnostic arthroscopy, the meniscal remnant is débrided with a combination of arthroscopic baskets and motorized shavers, ideally leaving a cuff of 2 to 3 mm of native meniscus as a substrate for firm reattachment of the meniscal allograft (
Fig. 49-1
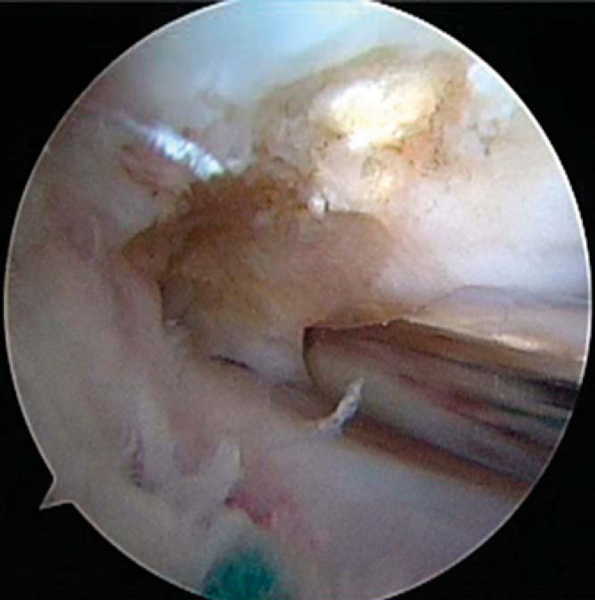
). The adjacent capsule and meniscal remnant are then rasped to stimulate bleeding for the reparative response. Notchplasty is then performed on the medial femoral condyle with a 4.5-mm motorized shaver, making sure that there is adequate arthroscopic access to the posterior horn of the meniscus for visualization and anatomic placement of the meniscal allograft (
Fig. 49-2
). Any indicated concomitant cartilage resurfacing procedures are performed at this time. Similarly, with a combined ligamentous reconstruction, bone tunnels are drilled at this time.
|
|
|
|
Figure 49-1 |
|
|
|
|
Figure 49-2 |
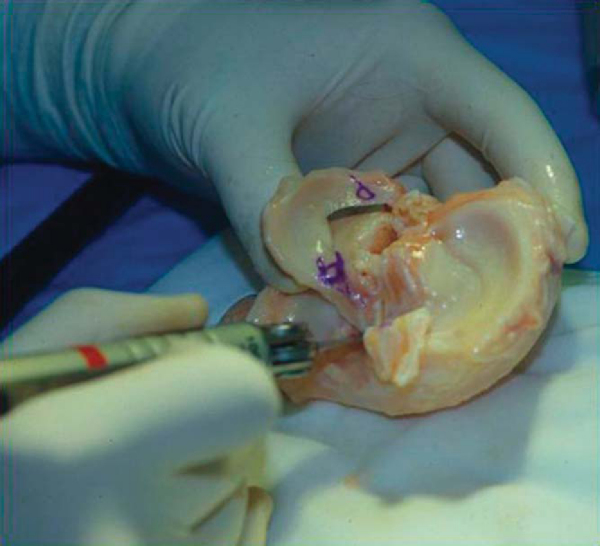
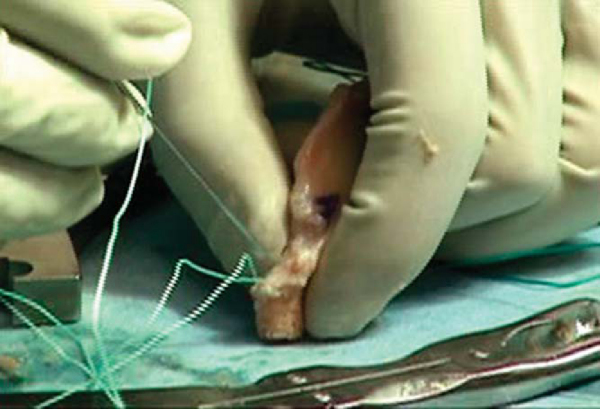
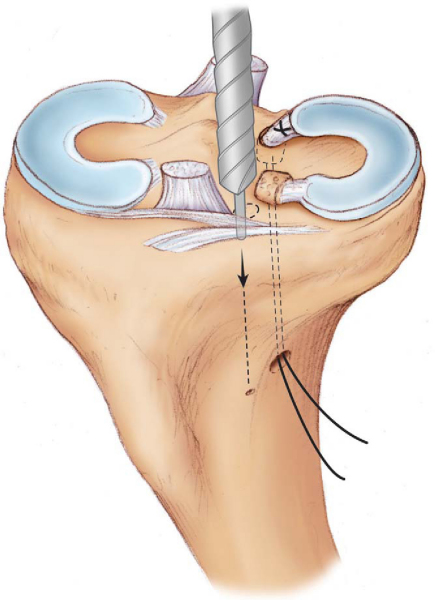
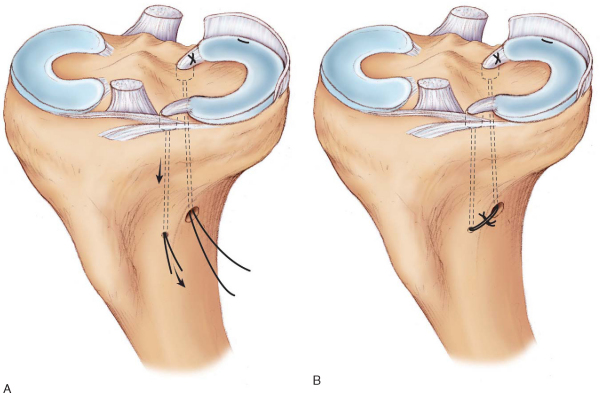
After it is determined that the patient is a reasonable candidate, an appropriately sized allograft can be prepared. The superior surface of the graft is marked with an A adjacent to the anterior horn and a P adjacent to the posterior horn to avoid any confusion at implantation in regard to orientation. By use of an oscillating saw, the plateau is trimmed to bone plugs attached to the anterior and posterior horns of the meniscus (
Fig. 49-3
). The anterior horn bone plug should be fashioned to a size of 10 mm in diameter and 15 mm in length. The posterior bone plug should be fashioned to a size of 8 mm in diameter and 15 mm in length. With use of a 2-mm drill bit, two drill holes are made in each bone plug. One No. 5 nonabsorbable Ethibond (Ethicon, Inc., Somerville, NJ) suture is passed in a retrograde and then antegrade fashion through each bone plug in addition to one No. 5 Ethibond locking suture in the meniscus adjacent to the bone plugs for tibial tunnel fixation (Figs. 49-4 and 49-5 [4] [5]). It is important that the bone plug sutures exit at the inferior surface of the bone plug to help guide the nose of the bone plug into the tibial tunnel during graft passage.
|
|
|
|
Figure 49-3 |
|
|
|
|
Figure 49-4 |
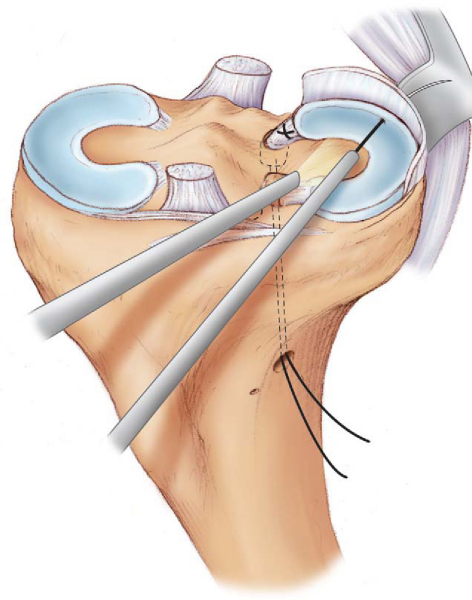
After completion of the meniscal bed preparation and notchplasty, the leg is exsanguinated and the tourniquet is adjusted to an appropriate pressure. A 5-cm anteromedial arthrotomy is made for graft passage, and a standard posterior medial approach for inside-out suture passage is made. The anteromedial arthrotomy should include the anteromedial portal and also incorporate the intended bone tunnel sites. With use of an anterior cruciate ligament guide set at the appropriate angle, a pin is inserted from adjacent to the tibial tubercle to the anatomic insertion site of the posterior horn of the medial meniscus under direct visualization (
Fig. 49-6
). The guide wire is then overreamed with a 10-mm reamer, and the tunnel edges are chamfered with a curved 4.5-mm shaver. A looped 20-gauge wire is advanced in the tibial tunnel in a retrograde fashion and retrieved out of the arthrotomy with a grasper (
Fig. 49-7
). The sutures in the posterior bone plug are then passed through the wire loop and retrieved through the tunnel. The graft is then passed through the arthrotomy and into the knee with the knee in 15 to 20 degrees of flexion and under a maximum valgus stress (
Fig. 49-8
). The meniscus is then reduced into position with direct pressure by use of a probe, a technique similar to the reduction of a bucket-handle meniscal tear. In some instances, this may require release of the superficial fibers of the medial collateral ligament for adequate clearance in the medial compartment. Once the meniscus is reduced, the posterior bone plug is seated in the tunnel with the aid of a probe and traction on the plug sutures. The posterior bone plug is purposely undersized by 2 mm for ease of passage at this stage. A snap is placed on the posterior bone plug suture limbs as they exit the distal tibial tunnel to maintain tension until the rest of the meniscus can be secured.
|
|
|
|
Figure 49-6 |
|
|
|
|
Figure 49-7 |
|
|
|
|
Figure 49-8 |
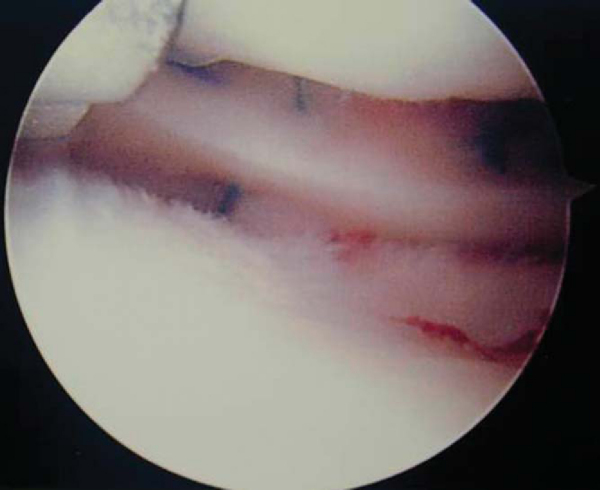
Next, the ideal location for the anterior bone plug is determined on the basis of the native anatomy and after the knee is ranged from full flexion to extension. Through the arthrotomy, with retractors in place, a reamer guide wire is drilled perpendicular to the articular surface in the appropriate position to a depth of 20 mm under direct vision (
Fig. 49-9
). Care is taken to provide enough room anteriorly to leave a rim of anterior cortex after reaming. This guide wire is then overreamed with a 10-mm reamer to a depth of 15 mm. Drill holes in the anterior cortex of the tibia are made with a 2-mm drill bit communicating with the anterior tunnel. Suture limbs from the anterior bone plug are then retrieved through these drill holes by use of a suture shuttle device, and the anterior bone plug is seated with gentle traction under direct vision. The suture limbs are snapped to maintain tension on the anterior bone plug. With the arthroscope in the anterolateral portal, a standard inside-out meniscal repair with zone-specific cannulas is performed with 2-0 nonabsorbable Ethibond suture in a vertical fashion at approximately 8- to 10-mm intervals (
Fig. 49-10
). Each suture is placed and secured and tied over the capsule while the apposition of the meniscus to the capsule is observed (
Fig. 49-11
). As you proceed anteriorly, repair can be difficult arthroscopically but can easily be performed under direct vision through the arthrotomy with 2-0 nonabsorbable Ethibond suture. An alternative technique is to perform a standard outside-in repair for the anterior horn if visualization is poor or in trying to minimize the incision. After completion of the meniscal reapproximation, the bone plug suture limbs are tied under appropriate tension over the bone bridge to each other or individually to a Teflon button, making sure not to recess the bone plugs below the level of the articular surface (
Fig. 49-12
). The meniscus is then probed for stability and its position re-evaluated through a full range of motion and rotation. It is important to make sure that the bone plugs are not overrotated or recessed in the tunnels. If the position is acceptable, the tourniquet is let down, hemostasis is achieved with electrocautery, and the wounds are closed in a standard fashion. Sterile dressings are applied, and the patient’s leg is wrapped loosely with an elastic bandage. The patient is then placed in a double upright brace with the knee locked in extension.
|
|
|
|
Figure 49-9 |
|
|
|
|
Figure 49-10 (Redrawn from Noyes FR, Barber-Westin SD, Rankin M. Meniscal transplantation in symptomatic patients less than fifty years old. J Bone Joint Surg Am 2005;87:149-165.) |
|
|
|
|
Figure 49-11 |
|
|
|
|
Figure 49-12 |
The patient is maintained in a double upright, hinged knee brace for the first 6 weeks. The orders are non weight bearing with the knee locked in extension for the first 4 weeks, partial weight bearing for weeks 5 and 6, and then full weight bearing after 6 weeks with an unloader brace for an additional 6 weeks. Range-of-motion exercises are started immediately, including full extension with flexion limited to 90 degrees to avoid increased stress on the meniscus. Closed-kinetic-chain strengthening exercises are started in the third week while observing the flexion limits. Light, sports-specific exercises are begun at 4 months, with return to straight-line running at 6 months. Squatting or hyperflexion activities are discouraged for 6 months. Return to high-load activities, including jumping, cutting, and pivoting, in the current state of meniscal transplantation is not recommended. In addition, as part of our protocol, magnetic resonance imaging is repeated at 6 to 12 months for all patients to evaluate the graft for healing, position, and possible extrusion or tearing. These protocols should serve as guidelines and would obviously be modified as a result of concomitant procedures performed.
| PEARLS AND PITFALLS | |||||||||||||||||||||||||||||||||
|
Potential complications include persistent pain, infection, loss of range of motion, and neurovascular complications. Specific to this procedure, graft failure is the most concerning complication and can be due to a number of factors. Repeated tearing or failure of the meniscal allograft most often occurs in the setting of coexisting osteoarthritis with advanced changes in the articular cartilage and remodeling of the femoral condyles. [5] [6] Technical considerations include anatomic placement of the anterior and posterior horns of the meniscus and proper graft sizing. Proper placement of the horns of the meniscus restores the meniscal functions, including load transmission and shock absorption. [1] [7] The type of fixation is also important, and it has been shown that secure anatomic fixation of bone plugs is required to best restore normal contact mechanics.[7] Improper sizing can result in an abnormal distribution of loads; undersized grafts show increased loads due to poor conformity, and oversized grafts are likely to extrude and not transmit any tibiofemoral forces. [1] [7] Partial tears of the graft can be treated with partial meniscectomy, whereas worsening of symptoms or graft failure may require graft removal.
In evaluating the literature, the results of meniscal allograft transplantation are difficult to assess because of a number of factors. Most studies have small numbers with limited followup. Methods of graft sizing and tissue processing are varied. different surgical techniques include techniques with bone plugs, dovetail, slot, and soft tissue fixation only. A large number of patients had concomitant procedures that were performed in either a staged or combined fashion, including corrective osteotomy, ligament reconstruction, and cartilage procedures. Another confounding variable is the degree and extent of articular cartilage degeneration that is present in these patients. Because of the number of confounding variables and lack of objective findings, we think it is difficult to draw any definitive conclusions from the literature. A summary of the current literature is seen in
Table 49-1
.
| Study | No. of Grafts | Mean Followup | Concomitant Procedures | Clinical Results | Comments |
|---|---|---|---|---|---|
| Garret[4] (1993) | 43 | 2-7 years | 24 ACL reconstructions 13 osteotomies 11 osteochondral allografts |
Failures related to grade III-IV chondromalacia | |
| Cameron and Saha[2] (1997) | 67 | 31 months | 5 ACL reconstructions 28 tibial osteotomies 6 femoral osteotomies 7 ACL reconstructions and tibial osteotomies |
87% good–excellent 13% poor–fair | No shrinkage in 67 gamma-irradiated deep-frozen allografts |
| Wirth et al[16] (2002) | 22 | 14 years | 22 ACL reconstructions 19 femoral advancements of MCL |
Deterioration during followup 100% lyophilized with abnormal MRI signal 100% deep-frozen with normal MRI signal |
Frozen grafts better than lyophilized |
| Noyes et al[5] (2004) | 40 | 40 months | 7 ACL reconstructions 1 PCL reconstruction 1 MCL reconstruction 16 osteochondral autografts |
89% rated knee improved 59% increase in number of patients who participated in light sports 68% had no tibiofemoral pain |
Concomitant cartilage and ligament procedures improved knee function and did not increase the rate of complications |
| Verdonk et al[15] (2005) | 100 | 7.2 years | 3 ACL reconstructions 4 osteochondral autografts 3 microfractures 15 tibial osteotomies 2 femoral osteotomies |
79% success rate Mean cumulative survival: 11.6 years | Survival analysis: beneficial effect remained in about 70% of patients at 10 years |
|
ACL, anterior cruciate ligament; MCL, medial collateral ligament; MRI, magnetic resonance imaging; PCL, posterior cruciate ligament. |
We do believe that for the appropriately selected meniscus-deficient patient, a well-performed meniscal allograft transplantation can provide a predictable result of improved pain relief and increased function. With future studies, we hope to answer the question of whether these known improvements in symptoms and function correlate to delayed progression or arrest of articular cartilage degeneration.