Cervical Spine Anatomy and Examination
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Cervical Spine Anatomy and Examination
Cervical Spine Anatomy and Examination
Sergio A. Glait BS
Sanjog Mathur MD
A. Jay Khanna MD
Description
-
Anatomy:
-
The cervical spine contains 7 cervical vertebrae, from which arise 8 nerve roots.
-
The normal cervical spine has a lordotic curvature.
-
Intact functional cervical vertebrae are vital because they protect both the spinal cord and the vertebral artery.
-
Of the 8 nerve roots that arise from the
cervical vertebrae, all but 1 (C8) exit above their numbered vertebral
body through the vertebral foramina; C8 exits below its numbered
vertebral body.
-
-
-
Vertebral anatomic structures consist of 2 lamina, 2 arches, 2 pedicles, 2 transverse processes, a spinous process, and a body.
-
C1 and C2 are unique in that C1 (atlas)
lacks a vertebral body and C2 (axis) has a bony protrusion on the
superior side of the body called the “odontoid process.” -
Most flexion and extension occurs at the atlanto-occipital joint, whereas rotation occurs mostly at the atlantoaxial joint (1).
Signs and Symptoms
Physical Exam
-
The cervical spine provides support and stability to the head while allowing for a wide ROM.
-
A thorough neck examination should evaluate the soft tissues and bony structures while also testing neurologic function.
-
Motor examination:
-
Levator scapulae: Resisted elevation (C3, C4, sometimes C5)
-
Deltoids: Shoulder abduction (C5)
-
Biceps: Arm flexion (C6)
-
Wrist extension (C6)
-
Triceps: Elbow extension (C7)
-
Wrist flexion (C7)
-
Finger extension (C7)
-
Finger flexion and thumb adduction (C8)
-
-
Deep tendon reflexes:
-
An abnormal reflex response may be indicative of spinal stenosis or nerve root compression.
-
Reflex amplification is a symptom of
spinal stenosis with myelopathy, whereas diminished reflexes indicate
nerve root compression.-
Biceps (C5)
-
Brachioradialis (C6)
-
Triceps (C7)
-
-
-
Sensation:
-
When tracing abnormal sensation, patients should be asked to be as specific as possible.
-
C2, C3, and C4 sensation should move from the posterior to the anterior neck.
-
C5–T2 has very specific dermatomes on the arm, wrist, and fingers.
-
C5: Lateral shoulder
-
C6: Radial 2 digits
-
C7: Middle finger
-
C8: Ulnar 2 digits
-
T1: Medial forearm
-
-
-
Inspection: It is important to evaluate:
-
Posture of the head
-
Posture of the body, motion, gait
-
Pain
-
Scars on the anterior or posterior neck
-
-
Bony palpation: Anterior (2):
-
Note any abnormalities such as tenderness, lumps, asymmetries, or misalignments.
-
May use surface landmarks to localize cervical spine level:
-
Hyoid bone: C3 vertebral body
-
Superior notch of thyroid cartilage: C4 vertebral body
-
1st cricoid ring: C6 vertebral body (swallowing allows easier palpation.)
-
Carotid tubercle: C6 transverse process
(the 2 carotid tubercles of the C6 vertebra should be palpated
separately because simultaneous palpation can restrict the flow of both
carotid arteries). -
Trachea: Make sure no deviations are present from the midline and palpate for abnormalities.
-
-
-
Bony palpation: Posterior (2)
-
Occiput:
-
Inion: The lower, most palpable part of the occiput
-
-
Spinous processes:
-
C7 and T1 are the most prominent.
-
All the spinous processes should be aligned.
-
Any deviation may be secondary to a unilateral facet dislocation.
-
C3–C5 may be bifid.
-
-
Facet joints: Approximately 2.5 cm lateral to the spinous processes, the most common joint involved in osteoarthritis is C5–C6 (3).
-
-
Soft-tissue palpation: Anterior:
-
Sternocleidomastoid
-
Parotid gland
-
Lymph nodes
-
Thyroid gland: Symmetric and smooth
-
Carotid pulse
-
Supraclavicular fossa: Palpate for bulges or cervical ribs.
-
-
Soft-tissue palpation: Posterior:
-
Trapezius: Evaluate for lymph nodes, palpable only because of pathologic causes
-
Greater occipital nerves: If palpable, may be secondary to whiplash injury.
-
Ligamentum nuchae: Inion to C7 spinous process
-
-
ROM:
-
Active ROM is a crucial part of the
cervical neck examination and includes flexion, extension, lateral
bending, and rotation of the neck. -
Flexion and extension:
-
50% occurs between the occiput and C1, and the remainder is distributed from C2–C7.
-
Slightly greater motion occurs at the C5–C6 level.
-
Tests sternocleidomastoid muscle (flexor) and paravertebral extensor and trapezius (extensors) (4)
-
-
Rotation:
-
50% occurs between C1–C2, and the remainder is evenly distributed in the remainder of the cervical spine.
-
To examine, rotate the chin 60–80° to the right and left.
-
Tests sternocleidomastoid muscle (primary rotator) (4)
-
-
Lateral bending:
-
Evenly distributed throughout the
cervical spine and usually not a pure movement but, rather, functions
in conjunction with rotation -
To examine, touch the ear to the ipsilateral shoulder without moving the shoulder; normal lateral bending is 45°.
-
Tests scalene muscles (4).
-
-
-
Special maneuvers to help to identify the cause of the cervical spine symptoms:
-
Modified Spurling maneuver (5):
-
Extend the neck and rotate the head to 1 side as axial pressure is applied.
-
A positive test is specific for cervical root compression but with low sensitivity.
-
-
Distraction test (2):
-
Apply vertical traction to the head in slight flexion and extension.
-
Symptoms of compressed nerve roots may regress temporarily.
-
-
Lhermitte test (2):
-
Patient flexes head forward.
-
If shooting pain is noted down the arms and/or legs, an anterior compressive lesion may be present.
-
-
Hoffmann test:
-
Rapidly flex the nail of the middle finger.
-
If muscles of the hand and thumb flex, then a positive sign exists, indicative of an upper motor neuron lesion (myelopathy).
-
-
Static/dynamic Romberg test (2):
-
The patient stands with hands out and palms up (arms in 90° of flexion).
-
Proprioceptive deficit is present if the
patient loses balance with the eyes closed or if the arms rise slowly
above the parallel.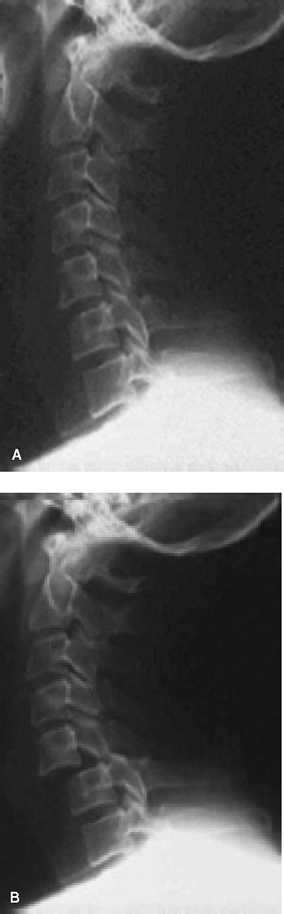 Fig. 1. Radiographs of an adult patient showing a normal lateral cervical spine radiograph (A) and bilateral C5–C6 facet dislocation (B).
Fig. 1. Radiographs of an adult patient showing a normal lateral cervical spine radiograph (A) and bilateral C5–C6 facet dislocation (B).![]() Fig.
Fig.
2. Sagittal T2-weighted MRI scan showing severe stenosis at C3–C4 and
C4–C5 secondary to large disc herniations with cord signal change at
C4–C5.
-
-
P.65
Tests
Imaging
-
Radiography (Fig. 1):
-
AP and lateral views are used to screen for most conditions.
-
Oblique views are used to detect facet dislocation and subluxation.
-
The open-mouth view is used to detect
odontoid and Jefferson burst fractures (for patients with neck pain who
have struck their heads). -
When viewing radiographs of young children, ossification centers may be present and should not be mistaken for fractures (6).
-
-
MRI is used to detect and define disc
herniation, facet hypertrophy, or ligamentum flavum hypertrophy that
may be impinging on the spinal cord or cervical nerve root foramen (Fig. 2). -
CT is used to define the anatomy of the osseous cervical spinal structures.
References
1. Aptaker RL. Neck pain. Part 1: Narrowing the differential. Phys Sportsmed 1996;24:37–46.
2. Albert
TJ, Vaccaro AR. Physical examination of the cervical spine. In:
Physical Examination of the Spine. New York: Thieme, 2005:13–63.
TJ, Vaccaro AR. Physical examination of the cervical spine. In:
Physical Examination of the Spine. New York: Thieme, 2005:13–63.
3. Hunt WE, Miller CA. Management of cervical radiculopathy. Clin Neurosurg 1986;33:485–502.
4. Tachdjian
MO. The neck and upper limb. In: Clinical Pediatric Orthopaedics: The
Art of Diagnosis and Principles of Management. Stamford, CT: Appleton
and Lange, 1997:263–324.
MO. The neck and upper limb. In: Clinical Pediatric Orthopaedics: The
Art of Diagnosis and Principles of Management. Stamford, CT: Appleton
and Lange, 1997:263–324.
5. Viikari-Juntura
E, Porras M, Laasonen EM. Validity of clinical tests in the diagnosis
of root compression in cervical disc disease. Spine 1989;14:253–257.
E, Porras M, Laasonen EM. Validity of clinical tests in the diagnosis
of root compression in cervical disc disease. Spine 1989;14:253–257.
6. Fesmire FM, Luten RC. The pediatric cervical spine: developmental anatomy and clinical aspects. J Emerg Med 1989;7:133–142.
FAQ
Q: What is a commonly made mistake when reading a radiograph of a young child’s cervical spine?
A: Ossification centers may still be present in young children and should not be confused with a fracture.
Q: What does the Hoffmann sign evaluate?
A: The Hoffmann sign evaluates for an upper motor neuron lesion, such as cervical spinal stenosis with myelopathy.

