Cavus Foot
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Cavus Foot
Cavus Foot
Clifford L. Jeng MD
Description
Cavus foot is defined by an elevation of the medial
longitudinal arch, often with an associated deformity of the hindfoot
or forefoot (Fig. 1).
longitudinal arch, often with an associated deformity of the hindfoot
or forefoot (Fig. 1).
Epidemiology
Incidence
Cavus feet are common and may be associated with several underlying conditions that affect the muscle balance of the foot.
Risk Factors
-
Neuromuscular disorders
-
Trauma
-
Connective-tissue disorders
-
Congenital deformities
Genetics
-
Several of the diseases responsible for the development of cavus feet are hereditary.
-
The most common hereditary cause is Charcot-Marie-Tooth disease, which is autosomal dominant.
Pathophysiology
Neuromuscular disorders are the etiologic factor for
most cavus foot deformities, causing muscle imbalance that leads to
atrophy or fibrosis, deformity, and joint contractures.
most cavus foot deformities, causing muscle imbalance that leads to
atrophy or fibrosis, deformity, and joint contractures.
Etiology
-
Causes include:
-
Muscle imbalance, such as peroneus longus or posterior tibialis overpull
-
Weakness of the intrinsic muscles of the foot with overpull of the long flexor tendons
-
Connective-tissue disorders, such as Marfan syndrome
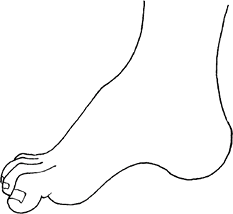 Fig. 1. A relatively high arch, which may be flexible or rigid, characterizes a cavus foot.
Fig. 1. A relatively high arch, which may be flexible or rigid, characterizes a cavus foot.
-
Associated Conditions
-
Charcot-Marie-Tooth disease
-
Friedreich ataxia
-
Spina bifida, syringomyelia
-
Diabetic neuropathy
-
Poliomyelitis
-
Previous compartment syndrome of the leg or foot
-
Partially treated clubfoot
-
Idiopathic clubfoot
-
Marfan syndrome
-
Beal syndrome
Signs and Symptoms
-
High arch
-
Calluses on forefoot or hindfoot
-
Difficulty with shoe wear
-
Patient:
-
May have heel varus or plantarflexion of the 1st metatarsal
-
May be asymptomatic
-
May complain of metatarsalgia (pain under metatarsal head region)
-
May develop recurrent ankle instability and/or sprains secondary to severe varus heel malalignment
-
Physical Exam
-
Measure the motor strength of all muscles crossing the ankle on both legs.
-
Look for associated claw-toe deformities.
-
Assess for plantar fascia contracture.
-
Check reflexes and sensation to light touch.
-
Examine the upper extremities, especially for intrinsic wasting.
-
Observe the spine for dimples, markings, and scoliosis.
Tests
-
Coleman block testing determines whether the hindfoot varus is flexible or rigid (1).
-
The patient stands on a block with the first metatarsal and hallux suspended freely in the air.
-
This position eliminates contribution
from a relatively plantarflexed 1st metatarsal, which in turn causes
varus alignment of hindfoot. -
In a flexible cavus deformity, Coleman block testing removes forefoot contribution and allows the hindfoot varus to correct.
-
In a rigid deformity, no hindfoot correction occurs.
-
Lab
Electromyography and nerve conduction studies are
helpful in diagnosing Charcot-Marie-Tooth disease, hereditary motor
sensory neuropathies, and lumbar radiculopathy.
helpful in diagnosing Charcot-Marie-Tooth disease, hereditary motor
sensory neuropathies, and lumbar radiculopathy.
Imaging
-
Standing radiographs of the foot should
be obtained to evaluate the calcaneal pitch angle (angle between the
calcaneus and the floor) and the Meary angle (angle between the talus
and the 1st metatarsal). -
As part of the workup for undiagnosed
cavus foot deformity, plain radiographs and MRI of the spine may be
indicated to identify occult abnormalities.
Differential Diagnosis
Muscle atrophy may cause the arch to appear higher.
General Measures
-
No treatment is indicated if the patient is asymptomatic and the skin is in good condition.
-
A padded insole with an arch support and/or metatarsal bar may relieve metatarsalgia.
-
A lateral heel wedge may help correct a flexible hindfoot varus deformity.
-
A brace may help stabilize a severely weakened cavus foot or concurrent chronic ankle instability.
-
Stretching may help prevent worsening deformity and maintain flexibility.
-
In general, cavovarus foot is tolerated
poorly because of progressive deformity, shoe wear difficulties, ankle
instability, and arthritis.
P.59
Special Therapy
Physical Therapy
-
Stretching of a tight plantar fascia and of other tight muscles may help slow progression of the condition.
-
Muscle strengthening, proprioceptive
training, and closed-chain balance exercises may help if the cavovarus
deformity has led to ankle instability.
Surgery
-
Usually, surgery is indicated for
progressive deformity, recalcitrant pain, chronic ankle instability,
difficulty with shoe wear, or rigid deformity with resultant arthritis. -
Careful examination helps to identify the
components of the deformity and the degree of flexibility or rigidity,
leading to a customized stepwise surgical plan to address all aspects. -
Flexible deformities can be addressed
with soft-tissue rebalancing procedures, whereas rigid deformities
require bony osteotomies or arthrodesis (fusion) procedures for
correction. -
Plantar fasciotomy may help lower the high arch.
-
Midfoot and metatarsal osteotomies are needed for a rigid cavus foot (2).
-
A lateral closing-wedge calcaneal osteotomy is performed if the heel varus is rigid (2).
-
Tendon lengthening procedures or tendon transfers are necessary to treat muscle imbalance.
-
Chronic ankle instability is addressed by ligament reconstruction and often concomitant tenodesis stabilization.
-
Triple arthrodesis is reserved mainly as
a salvage procedure if other surgical treatments fail or if the patient
has painful arthritis.
-
Patients with a cavus foot deformity must
be followed regularly by an orthopaedic surgeon for progression of the
deformity or muscle weakness. -
Progression may necessitate earlier reconstructive surgery to avoid fusion.
Issues for Referral
All patients with symptomatic cavus feet should be referred for orthopaedic consultation.
Prognosis
-
Patients with cavus feet secondary to neuropathy usually experience progressive deformity over time.
-
Patients with diabetes and
Charcot-Marie-Tooth disease may lose protective sensation and develop
neuropathic ulcerations that eventually lead to osteomyelitis and
amputation. -
Therefore, great care and attention must
be paid to appropriate orthoses and shoe wear to prevent abnormal skin
pressure from occurring.
References
1. Coleman SS, Chesnut WJ. A simple test for hindfoot flexibility in the cavovarus foot. Clin Orthop Relat Res 1977;123:60–62.
2. Sammarco GJ, Taylor R. Cavovarus foot treated with combined calcaneus and metatarsal osteotomies. Foot Ankle Int 2001;22:19–30.
Additional Reading
Alexander IJ, Johnson KA. Assessment and management of pes cavus in Charcot-Marie-tooth disease. Clin Orthop Relat Res 1989;246:273–281.
Dwyer FC. The present status of the problem of pes cavus. Clin Orthop Relat Res 1975;106:254–275.
Kirchner JS. Charcot-Marie-Tooth disease and the cavovarus foot. In: Richardson EG, ed. Orthopaedic Knowledge Update: Foot and Ankle 3. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2004:135–143.
Wapner KL. Pes cavus. In: Myerson MS, ed. Foot and Ankle Disorders. Philadelphia: WB Saunders Co., 2000:919–941.
Codes
ICD9-CM
-
754.59 Cavovarus foot
-
754.71 Cavus foot
FAQ
Q: What is the cause of most cavus feet?
A:
Neurologic disorders cause many cavus foot deformities secondary to
muscle imbalance between plantarflexor-invertors and
dorsiflexor-evertors.
Neurologic disorders cause many cavus foot deformities secondary to
muscle imbalance between plantarflexor-invertors and
dorsiflexor-evertors.
Q: When is surgery indicated for cavus foot deformity?
A:
Surgery is indicated in symptomatic cavus feet that show progressive
deformity, ankle instability, claw toes, and metatarsalgia or failure
of shoe wear modifications and orthotic use.
Surgery is indicated in symptomatic cavus feet that show progressive
deformity, ankle instability, claw toes, and metatarsalgia or failure
of shoe wear modifications and orthotic use.
