Blount Disease
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Blount Disease
Blount Disease
Paul D. Sponseller MD
Description
-
Bowing of the legs can be a normal stage of growth for infants and toddlers.
-
This phase is called “physiologic bowing” and resolves spontaneously by approximately 2 years of age.
-
The vast majority of children presenting with bowed legs have this benign physiologic state.
-
-
More rarely, bowed legs may be pathologic.
-
The most common cause of this condition is Blount disease.
-
It is an abnormality of the proximal tibial growth plate secondary to overload.
-
It causes progressive varus alignment of the knees (bowed legs) in children or adolescents (1,2) (Fig. 1).
-
-
Classification:
-
Infantile form: Presents in children 0–4 years old
-
Juvenile form: Presents at >4–9 years of age in obese children
-
Adolescent form: Presents in children >10 years old; has excellent prognosis with surgery
-
-
Synonyms: Infantile tibia vara (0–4
years); Juvenile tibia vara (>4–9 years); Adolescent tibia vara
(10–16 years); Pathologic bowlegs
General Prevention
-
Weight control
-
Extremely early standing or walking should not be encouraged.
-
Early bracing sometimes is effective.
Epidemiology
Incidence
-
Infantile tibia vara is the most common cause of pathologic bowing in young children and accounts for <1% of all bowed legs (2).
-
The juvenile form is much less common: Only 60 reports in the literature in the United States.
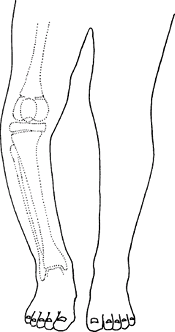 Fig. 1. In Blount disease, the varus is focal at the upper tibia.
Fig. 1. In Blount disease, the varus is focal at the upper tibia. -
The adolescent form is becoming more commonly recognized.
Prevalence (1,2)
-
The infantile form is more common in girls.
-
The juvenile or adolescent form is more common in boys.
-
The disorder is more common in African American children than those of other races.
Risk Factors
-
African American ethnicity
-
Obesity
-
Early age of walking
-
Varus greater on the tibial than the femoral side is a risk factor for infantile and juvenile Blount disease (1).
Genetics
-
No genetic pattern has been proved.
-
More likely, patients inherit a body habitus that predisposes them to the disorder.
Pathophysiology
-
The growth plate shows islands of densely
packed cartilage cells with more hypertrophy than normal, islands of
almost acellular fibrous cartilage, and abnormal groups of capillaries (2). -
Biopsy is not indicated.
Etiology
Decreased growth of the proximal medial tibial growth
plate (physis) causes varus angulation (bowing) and internal rotation
of the proximal tibia secondary to weight-related overload of this
portion of the growth plate.
plate (physis) causes varus angulation (bowing) and internal rotation
of the proximal tibia secondary to weight-related overload of this
portion of the growth plate.
Associated Conditions
Obesity
Signs and Symptoms
-
Patients with infantile tibia vara
usually present between 14 and 40 months of age with increasingly bowed
legs (usually bilateral involvement). -
Adolescent presentation also involves
progressive varus deformity (bowing), but many of these patients also
have medial knee pain and often only 1 leg is affected. -
If untreated, the infantile form may progress to become severe.
-
The juvenile and adolescent forms rarely become as severe.
-
Some internal tibial torsion usually is present along with the bowing.
Physical Exam
-
Record the patient’s height, weight, and percentiles.
-
The finding of short stature suggests rickets or a skeletal dysplasia.
-
Note the location of any pain.
-
Record the gap between the medial sides of the knees and check knee ROM and ligamentous laxity.
-
Assess tibial torsion by the thigh–foot angle.
-
Perform a routine knee examination,
observe gait, and measure the foot progression angle (angle of the feet
with the direction of walking).
Tests
Lab
-
Testing is indicated if rickets is suspected.
-
In Blount disease, calcium, phosphorus, alkaline phosphatase, and renal function tests are all normal (2).
Imaging
-
Radiography:
-
Appropriate radiographs: A long leg AP view of the tibia and femur to evaluate the tibiofemoral angle and mechanical axis (1–5).
-
The radiograph should show the whole limb from the hip to the ankle, and it should be a true AP view of the knee (4).
-
The metaphyseal–diaphyseal angle differentiates Blount disease and physiologic varus:
-
<11° is physiologic varus.
-
≥16° indicates Blount disease.
-
Values between 11° and 16° signify a risk of potential Blount disease.
-
-
Reveals a medial physeal bar (disappearance of the growth plate with metaphysis–epiphysis fusion) in more advanced disease
-
-
CT or MRI:
-
Can be useful in delineating the physeal damage that later may form a bar.
-
Patients with adolescent Blount disorder (Fig. 2)
show less deformation of the epiphysis and rarely form a bar, but they
usually have some deformity on the femoral as well as on the tibial side
-
Differential Diagnosis
-
Physiologic bowed legs
-
Hypophosphatemic rickets
-
Trauma to metaphysis or growth plate
-
Osteochondroma
-
Metaphyseal chondrodysplasia
-
Focal fibrocartilaginous dysplasia
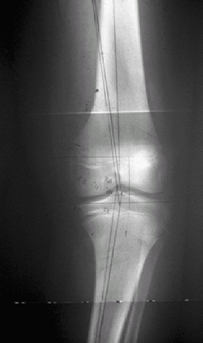 Fig. 2. Adolescent Blount disease. Note the physeal widening and relative preservation of the epiphysis of the tibia.
Fig. 2. Adolescent Blount disease. Note the physeal widening and relative preservation of the epiphysis of the tibia.
P.41
General Measures
-
Children <3 years old who present with
Blount disease may be braced, preferably with a long brace from the hip
to the ankle that is locked at the knee (2). -
Full-time bracing (22 hours a day) puts a
corrective valgus stress on the knee (more knock-kneed) and decreases
the stress on the medial physis.-
If bracing is begun when the deformity is mild, this treatment allows the growth plate to “catch up” the growth medially.
-
-
If the patient is being braced, full weightbearing is encouraged.
-
If bracing fails to correct the
deformity, or if a patient >3 years old presents with moderate to
severe deformity, an osteotomy is needed (6,7). -
If osteotomy is performed, the patient is
kept nonweightbearing until healing (8–12 weeks) of the osteotomy; then
full weightbearing can be resumed. -
Hemiepiphysiodesis is also an alternative in juveniles if the deformity is moderate (6).
Activity
-
No activity restriction on unbraced patients
-
Bracing restricts participation in sports.
Special Therapy
Physical Therapy
-
Does not help improve knee varus
-
Crutch training after osteotomy
-
Regaining knee ROM after osteotomy
Surgery
-
Osteotomy (cutting and realigning the proximal tibia) will decrease the stress on the medial physis and can allow healing.
-
If a physeal bar has formed:
-
An osteotomy often is combined with completion of the closure of the proximal tibial physis.
-
The whole growth plate should be fused to prevent the lateral portion of the growth plate from causing recurrent varus (5); patients with advanced cases may have a secondary deformity of the distal femur and/or the distal tibia.
-
-
If substantial leg-length inequality
develops, it may be treated by lengthening the short limb or by growth
plate closure of the longer limb. -
Adolescent Blount disease may be treated
with tethering (“stapling”) of the lateral sides of the growth plate to
allow the bone to correct itself. -
In more advanced cases, osteotomy of the tibia and/or the femur is needed.
Prognosis
-
Because the recurrence rate is higher in
patients treated after 4 years of age (70–75%) than in patients treated
before age 4 (20–30%) (2), early osteotomy (before age 4) should be performed if bracing is not successful. -
Patients with late treatment or incomplete treatment have an increased risk of arthritis of the knee.
Complications
-
Recurrence of deformity leads to abnormal limb alignment and degenerative arthritis.
-
Limb-length inequality may result.
-
Postosteotomy complications include neurovascular complications and compartment syndrome.
Patient Monitoring
-
Patients should be followed until skeletal maturity.
-
The interval between visits is determined by the severity of the disease.
References
1. Bowen
RE, Dorey FJ, Moseley CF. Relative tibial and femoral varus AS a
predictor of progression of varus deformities of the lower limbs in
young children. J Pediatr Orthop 2002;22:105–111.
RE, Dorey FJ, Moseley CF. Relative tibial and femoral varus AS a
predictor of progression of varus deformities of the lower limbs in
young children. J Pediatr Orthop 2002;22:105–111.
2. Schoenecker PL, Rich MM. The lower extremity. In: Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopaedics, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006:1157–1211.
3. Doyle BS, Volk AG, Smith CF. Infantile Blount disease: long-term follow-up of surgically treated patients at skeletal maturity. J Pediatr Orthop 1996;16:469–476.
4. Gordon JE, Heidenreich FP, Carpenter CJ, et al. Comprehensive treatment of late-onset tibia vara. J Bone Joint Surg 2005;87A:1561–1570.
5. Stanitski DF, Stanitski CL, Trumble S. Depression of the medial tibial plateau in early-onset Blount disease: myth or reality? J Pediatr Orthop 1999;19:265–269.
6. Gordon JE, King DJ, Luhmann SJ, et al. Femoral deformity in tibia vara. J Bone Joint Surg 2006;88A:380–386.
7. Henderson RC, Kemp GJ, Jr, Greene WB. Adolescent tibia vara: alternatives for operative treatment. J Bone Joint Surg 1992;74A:342–350.
Codes
ICD9-CM
732.4 Blount’s disease
Patient Teaching
-
The patient’s family must understand the benefit of regular monitoring and weight reduction.
-
If they elect to use bracing in patients
with infantile Blount disease, the braces must be worn 22 hours a day
to exert their corrective effect on growth.
FAQ
Q: How can Blount disease be distinguished from physiologic bowing of the tibia?
A:
They can be distinguished by the metaphyseal–diaphyseal angle in young
children (<3 years old) being >11° and by the shape of the tibial
deformation in older children.
They can be distinguished by the metaphyseal–diaphyseal angle in young
children (<3 years old) being >11° and by the shape of the tibial
deformation in older children.
Q: What is the cause of Blount disease?
A: The cause is overload of the medial growth plate of the upper tibia.
Q: Is surgery always necessary?
A: Surgery is recommended for all patients who are symptomatic or who have varus of >10°.
Q: Does adolescent Blount disease develop from infantile Blount disease?
A: No, adolescent Blount disease develops spontaneously in older-aged children than does infantile Blount disease.
