Arthropathies/Connective Tissue Diseases
Editors: Berquist, Thomas H.
Title: Musculoskeletal Imaging Companion, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Chapter 13 – Arthropathies/Connective Tissue Diseases
Chapter 13
Arthropathies/Connective Tissue Diseases
Thomas H. Berquist
Protocols
Key Facts
-
Routine radiographs remain the primary screening technique for evaluating arthropathies.
-
Anteroposterior (AP), lateral, and
oblique views of involved joints should be obtained. New digital
techniques permit windowing, bone detail techniques, and magnification
to more effectively evaluate subtle bone and soft tissue changes.
-
-
Radionuclide scans are sensitive for
detecting early changes in articular disease. Technetium-99m methylene
diphosphonate is injected intravenously (15 to 20 mCi), and images of
the involved joints are obtained 2 to 3 hours after injection.
Increased radiotracer is seen in bones and joints because of early
synovitis and osseous inflammation. Findings are not specific. -
Ultrasound has demonstrated increased
utility for evaluating ligaments, tendons, and intra-articular
pathology. High-frequency transducers are used for superficial
structures (>7 to 12 MHz). Transverse, longitudinal, and dynamic
images are obtained. -
Computed tomography (CT) is used
primarily for surgical treatment planning. Bone stock and extent of
erosions can be evaluated. Thin sections (1 mm at 0.5-mm intervals)
allow coronal and sagittal reformatting and three-dimensional
reconstructions. -
Magnetic resonance (MR) techniques are
useful for detection of early bone and soft tissue changes. Specific
techniques have gained popularity for evaluating synovium and articular
cartilage.-
Synovial inflammation:
-
T2-weighted spin-echo or fast spin-echo sequences in coronal and axial planes
-
Intravenous gadolinium (0.1 to 0.2
mmol/kg body weight) followed by fat-suppressed T1-weighted images 15
to 60 minutes after injection. Early synovial inflammation is more
easily appreciated. Bolus injections with dynamic fast scan techniques
are useful for evaluating active synovitis and remissions. -
Articular cartilage can be evaluated on
contrast-enhanced images or by using double-echo steady state or
fat-suppressed fast spin-echo proton density sequences.
-
-
P.802
Suggested Reading
Eustace
S, DiMasi M, Adams J, et al. In vitro and in vivo spin-echo diffusion
imaging characteristics of synovial fluid: Potential noninvasive
differentiation of inflammatory and degenerative arthritis. Skel Radiol 2000;29:320–323.
S, DiMasi M, Adams J, et al. In vitro and in vivo spin-echo diffusion
imaging characteristics of synovial fluid: Potential noninvasive
differentiation of inflammatory and degenerative arthritis. Skel Radiol 2000;29:320–323.
Goupille
P, Roulot B, Akoka S, et al. Magnetic resonance imaging: A valuable
method for detection of synovial inflammation in rheumatoid arthritis. J Rheumatol 2001;28:35–40.
P, Roulot B, Akoka S, et al. Magnetic resonance imaging: A valuable
method for detection of synovial inflammation in rheumatoid arthritis. J Rheumatol 2001;28:35–40.
Lin
J, Fessell DP, Jacobson JA, et al. An illustrated tutorial of
musculoskeletal ultrasound: Part 1, introduction and general
principles. AJR Am J Roentgenol 2000;175:637–645.
J, Fessell DP, Jacobson JA, et al. An illustrated tutorial of
musculoskeletal ultrasound: Part 1, introduction and general
principles. AJR Am J Roentgenol 2000;175:637–645.
Rose PM, Demlow TA, Szumowski J, et al. Chondromalacia patella: Fat suppressed MR imaging. Radiology 1994;193:437–440.
P.803
Rheumatoid Arthritis
Key Facts
-
Clinical: Rheumatoid arthritis (RA)
affects 1% to 2% of the general population with permanent deformity and
disability in 10% to 20%. Characteristically, RA is a symmetric
polyarthropathy. Diagnostic criteria of the American Rheumatism
Association are as follows:-
Morning stiffness lasting 1 hour before improvement
-
Soft tissue swelling of three or more joint areas noted on physical examination
-
Swelling of wrists, metacarpophalangeal joints, and proximal interphalangeal (PIP) joints
-
Symmetric swelling
-
Rheumatoid nodules
-
Positive rheumatoid factor
-
Radiographic erosions with or without juxta-articular osteopenic in hand, wrist, or both
-
Criteria 1 to 4 must be present for 6
weeks. If four or more criteria are present, the criteria are 91% to
94% sensitive and 89% specific for RA. -
Age: 25 to 55 years
-
Sex: Females outnumber males 3:1.
-
Distribution: PIP joint,
metacarpophalangeal joint, wrist, metatarsophalangeal (MTP) joint,
ankles, knees, shoulders, and, to a lesser extent, hips, and spine
-
-
Laboratory findings: positive rheumatoid factor, elevated erythrocyte sedimentation rate
-
Radiographic features:
Early Soft tissue swelling around involved joints Juxta-articular osteopenia Subtle marginal bone erosions Late Osteopenia (diffuse) Joint space narrowing Obvious erosions Joint subluxations Soft tissue atrophy Rheumatoid nodules
P.804
 |
|
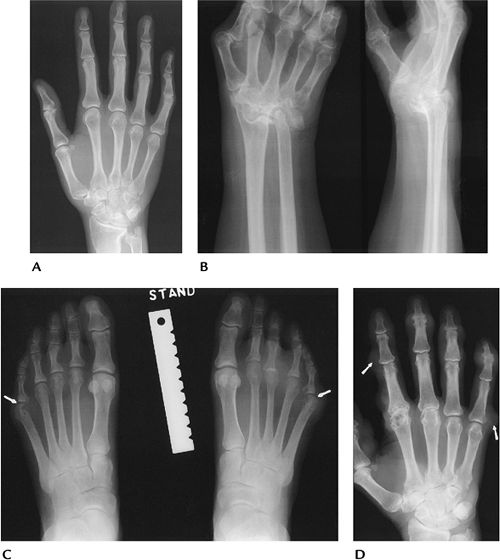
FIGURE 13-1 Early RA. (A,B) Bilateral posteroanterior views of the hands showing subtle swelling (arrows) and juxta-articular osteopenia.
|
P.805
 |
|
FIGURE 13-2 Coronal contrast-enhanced fat-suppressed T1-weighted image demonstrates early changes of RA with erosions (arrowheads) and synovial enhancement.
|
P.806
 |
|
FIGURE 13-3 Advanced RA. (A) Erosive changes in the ulna and distal radius. (B) Several years later, there is complete erosion of the wrist. (C) Different patient with swelling and characteristic erosions of the fifth MTP joints (arrows). (D) Advanced RA in the hand with multiple subcutaneous nodules (arrows).
|
Suggested Reading
Brower AC. Arthritis in black and white, 2nd ed. Philadelphia: WB Saunders; 1997:195–224.
Huh
YM, Suh JS, Jeong EK, et al. Role of inflamed synovial volume of the
wrist in redefining remission of rheumatoid arthritis with gadolinium
enhanced 3D-SPGR MR imaging. J Magn Reson Imaging 1999;10:202–208.
YM, Suh JS, Jeong EK, et al. Role of inflamed synovial volume of the
wrist in redefining remission of rheumatoid arthritis with gadolinium
enhanced 3D-SPGR MR imaging. J Magn Reson Imaging 1999;10:202–208.
P.807
Psoriatic Arthritis
Key Facts
-
Clinical:
-
Psoriatic arthritis occurs in 2% to 6% of
patients with psoriasis. Psoriatic arthritis comprises approximately 5%
of patients with polyarthropathy. Arthritis may precede or coincide
with skin manifestations. -
Age: 25 to 55 years
-
Sex: no sex predilection
-
Distribution: hands, feet, sacroiliac joints (50%), and spine, in order of decreasing frequency
-
-
Laboratory findings: negative rheumatoid
factor, elevated erythrocyte sedimentation rate, human leukocyte
antigen (HLA)-B27 antigen often positive. -
Imaging features:
-
Bilateral, but asymmetric involvement
-
Fusiform (entire digit) soft tissue swelling
-
Normal bone density (no osteopenia)
-
Marked joint space narrowing
-
“Pencil in cup” erosions
-
Bone proliferation
-
Distal joints (distal interphalangeal
[DIP] and PIP) of hands and feet (compared with proximal) are more
commonly involved in RA.
-
 |
|
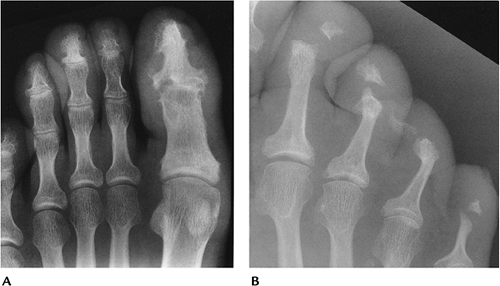
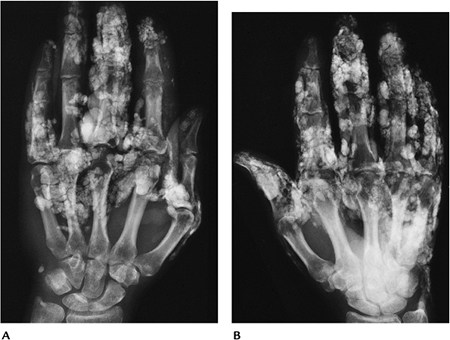
FIGURE 13-4 Psoriatic arthritis involving the foot. (A)
Osteolysis and reparative new bone in the first and third DIP joints. The erosive changes in the first DIP is a common location for psoriatic arthritis. (B) Advanced changes in the DIP joints of the lesser toes with no bone demineralization. |
P.808
 |
|
FIGURE 13-5
Psoriatic arthritis both hands. Erosive changes in the interphalangeal and DIP joints. Subluxations are not usually a prominent feature of psoriatic arthritis. |
Suggested Reading
Resnick D, Kransdorf MJ. Psoriatic arthritis. In: Resnick D, Kransdorf MJ, eds. Bone and joint imaging, 3rd ed. Philadelphia: Elsevier-Saunders; 2005:288–297.
P.809
Reiter Syndrome
Key Facts
-
Clinical:
-
Reiter arthropathy typically is
associated with conjunctivitis and urethritis. Patients also may have
fever and weight loss. This triad is sexually transmitted. In females,
the arthropathy is associated with dysentery. -
Age: 15 to 35 years
-
Sex: most common in males
-
Distribution: feet, ankles, knees, sacroiliac joints. Upper extremity involvement uncommon.
-
-
Laboratory findings: HLA-B27 antigen positive in 75%
-
Imaging features:
-
Bilateral asymmetric joint involvement
-
Fusiform (entire digit) soft tissue swelling
-
Joint space narrowing
-
Bone proliferation
-
Ill-defined erosions
-
Normal mineralization
-
 |
|
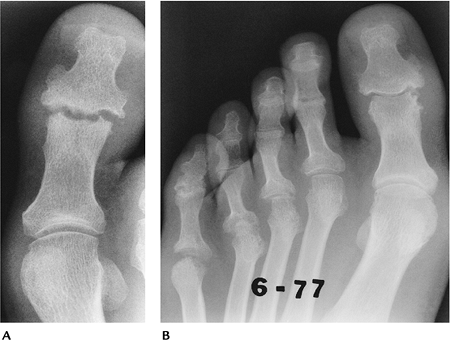
FIGURE 13-6 Reiter involvement of the sacroiliac joint. Involvement is bilateral but asymmetric.
|
P.810
 |
|
FIGURE 13-7 Reiter involvement of the plantar aspect of the calcaneus with irregular bone proliferation.
|
P.811
 |
|
FIGURE 13-8 (A) Reiter involvement of the right great toe with distal joint erosions, normal bone density, and fusiform soft tissue swelling. (B) Reiter involvement of the forefoot and phalangeal and MTP joints.
|
Suggested Reading
Weldon WW, Scaletter R. Roentgen changes in Reiter syndrome. AJR Am J Roentgenol 1961;86:344–350.
P.812
Ankylosing Spondylitis
Key Facts
-
Clinical:
-
Ankylosing spondylitis is an inflammatory
condition that affects primarily the axial skeleton. Patients typically
are young males who present with low-back pain. Patients also may have
weight loss and low-grade fever. -
Age: 15 to 35 years
-
Sex: Males outnumber females 4:1 to 10:1.
-
Distribution: sacroiliac joints, spine
(lumbar to cervical), hips, knees, shoulders. Peripheral joints of
hands and feet less common (10% with long-standing disease).
-
-
Laboratory findings: HLA-B27 antigen frequently positive, elevated erythrocyte sedimentation rate
-
Imaging features:
-
Bony ankylosis of involved joints
-
Bilateral symmetric involvement of sacroiliac joints
-
Bone mineral normal early; osteopenic after ankylosis
-
Minimal erosive changes
-
 |
|
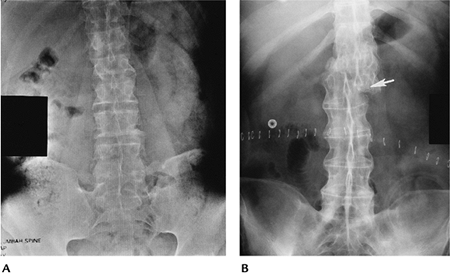
FIGURE 13-9 Ankylosing spondylitis. (A) AP radiograph of the pelvis showing symmetric ankylosis of the sacroiliac joints. (B) Long-standing ankylosing spondylitis with syndesmophytes, spinous ligament ossification, and a shear fracture (arrow). Patients with ankylosing spondylitis are more susceptible to spine fractures.
|
P.813
 |
|
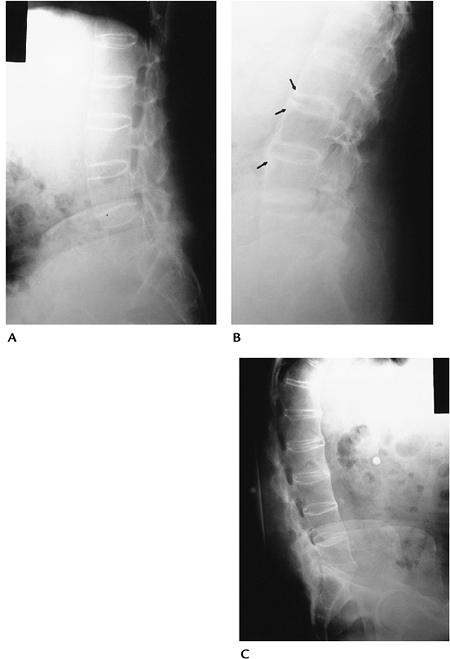
FIGURE 13-10 Ankylosing spondylitis of the spine seen on lateral radiographs. (A) Early changes with incomplete ankylosis. There is squaring of the vertebral bodies. (B) Early changes of ankylosing spondylitis. Note the shiny corners at the vertebral margins (arrows). (C) Advanced changes with more uniform ankylosis.
|
Suggested Reading
Brower AC. Arthritis in black and white, 2nd ed. Philadelphia: WB Saunders; 1997:257–272.
P.814
Osteoarthritis
Key Facts
-
Clinical:
-
Osteoarthritis is the most common
arthropathy and increases in incidence with age. Osteoarthritis may
occur after other arthropathies (secondary osteoarthritis).
Degenerative joint disease may be genetic, or the result of age,
occupation, or multiple factors. Patients present with pain and
swelling in the involved joints. -
Age: more than 50 years
-
Sex: no sex predilection
-
Distribution: hands (DIP and PIP joints), feet, knees, and hips. Elbows and shoulders less commonly involved.
-
-
Laboratory findings: none
-
Imaging features:
-
Asymmetric joint space narrowing
-
Subchondral sclerosis
-
Subchondral cysts
-
Osteophyte formation
-
Subluxations (less dramatic than RA)
-
Unilateral or bilateral involvement, but asymmetric
-
P.815
 |
|
FIGURE 13-11
Osteoarthritis. PA view of the hand and wrist showing typical distal and PIP joint involvement with narrowing of the metacarpophalangeal joints. There are also typical changes at the scapho-trapezio-trapezium joints. |
P.816
 |
|
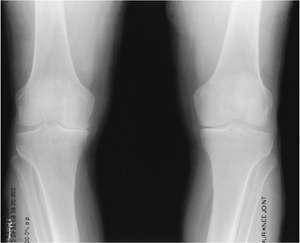
FIGURE 13-12 Standing views of the knees showing typical asymmetric medial compartment narrowing.
|
P.817
 |
|
FIGURE 13-13 AP radiograph of the pelvis demonstrating advanced degenerative arthritis in the right hip with osteophytes and bone sclerosis.
|
Suggested Reading
Smith
D, Braunstein EM, Brandt KD, et al. A radiographic comparison of
erosive osteoarthritis and idiopathic nodular osteoarthritis. J Rheumatol 1992;19:896–904.
D, Braunstein EM, Brandt KD, et al. A radiographic comparison of
erosive osteoarthritis and idiopathic nodular osteoarthritis. J Rheumatol 1992;19:896–904.
P.818
Enteric Arthropathies
Key Facts
-
Clinical:
-
Arthropathies may accompany enteric
conditions, such as Crohn disease, ulcerative colitis, and Whipple
disease. Findings may be similar radiographically to ankylosing
spondylitis. Incidence of sacroiliitis associated with these conditions
varies from 2% to 26%. -
Age: 20 to 40 years
-
Sex: no sex predilection
-
Distribution: sacroiliac joints, spine, hips, knee; peripheral joints less common
-
-
Laboratory findings: HLA-B27 antigen positive in approximately 90%
-
Imaging features:
-
Sacroiliac joint involvement bilateral
-
Spondylitis similar to ankylosing spondylitis
-
Peripheral joint swelling and osteopenia
-
Joint space narrowing and erosions rare
-
 |
|
FIGURE 13-14
Enteric arthropathy. AP radiograph of the spine and sacroiliac joints showing inflammatory arthropathy symmetrically involving the sacroiliac joints. |
P.819
Suggested Reading
Resnick D, Kransdor MJ. Enteric arthropathies. In: Resnick D, Kransdorf MJ, eds. Bone and joint imaging, 3rd ed. Philadelphia: Elsevier-Saunders; 2005:306–315.
P.820
Systemic Lupus Erythematosus
Key Facts
-
Clinical:
-
Systemic lupus erythematosus is a
connective tissue disorder with immunologic abnormalities. Multiple
organ systems are involved. Myositis occurs in 30% to 50% of patients,
and joint involvement occurs in 75% to 90% of patients. -
Age: 20 to 40 years
-
Sex: Females outnumber males by a wide margin. Blacks outnumber whites.
-
Distribution: symmetric bilateral involvement of hands, knees, and shoulders
-
-
Laboratory findings: anemia, leukopenia, positive rheumatoid factor, lupus erythematosus cells, and antinuclear antibodies
-
Imaging features:
-
Soft tissue swelling
-
Juxta-articular osteoporosis
-
Subluxations
-
Erosions rare
-
Osteonecrosis
-
Bilateral symmetric involvement
-
 |
|
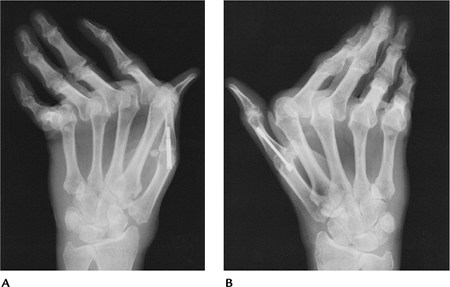
FIGURE 13-15 Systemic lupus erythematosus. (A,B) Radiographs of the hands showing metacarpophalangeal subluxations with no erosions. Note prior fusions of both thumbs.
|
P.821
Suggested Reading
Resnick D, Kransdorf MJ. Systemic lupus erythematosus. In: Resnick D, Kransdor MJ, eds. Bone and joint imaging, 3rd ed. Philadelphia: Elsevier-Saunders; 2005:321–327.
P.822
Scleroderma
Key Facts
-
Clinical:
-
Scleroderma is a connective tissue
disorder that affects multiple organ systems, including the skin,
musculoskeletal system, gastrointestinal tract, heart, lungs, and
kidneys. Patients often present with pain and pallor of the hands when
exposed to cold temperatures. Joint involvement is common initially,
and up to 97% eventually have articular disease. -
Age: 30 to 50 years
-
Sex: Females outnumber males.
-
Distribution: fingers, wrists, ankles
-
-
Laboratory findings: elevated erythrocyte
sedimentation rate, positive rheumatoid factor (30% to 40%),
antinuclear antibodies (35% to 96%) -
Imaging features:
-
Hand: soft tissue atrophy, calcification, resorption of distal phalangeal tufts
-
Osteolysis in other sites, including phalanges, wrist, ribs, clavicle, mandible, and shoulder
-
P.823
 |
|
FIGURE 13-16 Scleroderma. Radiograph of the hand showing soft tissue calcification, soft tissue atrophy, and tuft resorption.
|
Suggested Reading
Bassett LW, Blocka KLN, Furst DE, et al. Skeletal findings in progressive systemic sclerosis (scleroderma). AJR Am J Roentgenol 1981;136:1121–1126.
P.824
Dermatomyositis/Polymyositis
Key Facts
-
Clinical:
-
Polymyositis involves skeletal muscle and
dermatomyositis muscle and skin. The cause is unknown. Five criteria
are established for diagnosis:-
Progressive proximal muscle weakness
-
Increased serum muscle enzymes
-
Abnormal electromyogram
-
Inflammatory changes on biopsy
-
Skin disease (dermatomyositis)
-
-
-
Classifications:
-
Typical polymyositis: most common
category. Seen in women, more than men, 30 to 50 years old. Proximal
muscle weakness in pelvis and thighs. Arthralgias with or without skin
involvement. -
Typical dermatomyositis: more common in
females. Muscle weakness with erythematosus skin rash. Older age group,
typically 50 to 70 years old. -
Dermatomyositis with malignancy: more
common in men more than 40 years old. Skin rash, muscle weakness, and
malignancy. Tumors found in lung, prostrate, breast, and
gastrointestinal and genitourinary tracts. -
Childhood dermatomyositis: girls more
often affected than boys. Muscle weakness, edema, skin calcification,
vasculitis, joint contractures. -
Acute myolysis: uncommon form with acute myonecrosis. Most common in adolescents and young adults. Outcome often fatal.
-
-
Imaging features:
Radiographic features: Soft tissue calcification, usually more extensive in children. Swelling about involved joints without bone changes. MRI: Inflammatory changes in muscles easily detected and useful for biopsy site selection.
P.825
 |
|
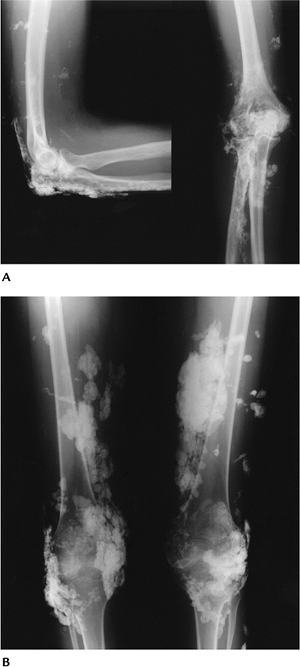
FIGURE 13-17 Dermatomyositis. (A) Radiographs of the elbow showing soft tissue calcification that is greater along the extensor surface. (B) AP radiographs of the knees with extensive soft tissue calcifications.
|
P.826
 |
|
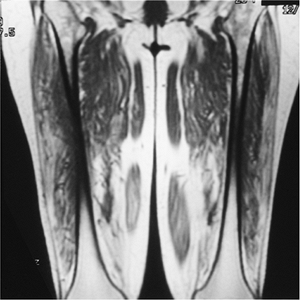
FIGURE 13-18 Myositis. Coronal T1-weighted image of the thighs showing fatty infiltration of the muscles caused by chronic myopathy.
|
Suggested Reading
Frazer DD, Frank JA, Dalakas MC. Inflammatory myopathies. MR imaging and spectroscopy. Radiology 1991;179:341–344.
P.827
Mixed Connective Tissue Disease/Overlap Syndromes
Key Facts
-
Clinical:
-
Mixed connective tissue disease presents
with a combination of features resembling scleroderma, systemic lupus
erythematosus, dermatomyositis, and RA. Joints are involved in 90% to
100%. -
Age: children and adults
-
Sex: slightly more common in females than males
-
Distribution: hands, feet
-
-
Laboratory findings: presence of antibodies to saline extractable nuclear antigen
-
Imaging features:
-
Juxta-articular osteopenia
-
Soft tissue swelling
-
Erosions similar to RA
-
Scleroderma-like changes in tufts
-
Soft tissue calcification
-
Joint subluxations
-
P.828
 |
|
FIGURE 13-19
Mixed connective tissue disease. AP radiograph of the right hand showing periarticular soft tissue calcification, most obvious in the thumb, soft tissue swelling, joint subluxation in the phalangeal joints, and joint space narrowing. |
P.829
 |
|
FIGURE 13-20 Mixed connective tissue disease. (A,B) Radiographs of both hands showing juxta-articular osteopenia and extensive soft tissue calcifications.
|
Suggested Reading
Resnick
D, Kransdorf MJ. Mixed connective tissue disease and collagen vascular
overlap syndromes. In: Resnick D, Kransdorf MJ, eds. Bone and joint imaging, 3rd ed. Philadelphia: Elsevier-Saunders; 2005:349–352.
D, Kransdorf MJ. Mixed connective tissue disease and collagen vascular
overlap syndromes. In: Resnick D, Kransdorf MJ, eds. Bone and joint imaging, 3rd ed. Philadelphia: Elsevier-Saunders; 2005:349–352.
P.830
Juvenile Chronic Arthropathy
Key Facts
-
Juvenile chronic arthropathy includes a
spectrum of disorders, including juvenile spondyloarthropathies,
seropositive RA, and seronegative (Still disease) arthritis. -
Most disorders occur in older children or adolescents and, therefore, have findings similar to the adult disorder.
-
Still disease occurs in younger children
and accounts for 70% of juvenile chronic arthropathies. Three
categories exist with some overlap:-
Systemic disease without joint involvement
-
Polyarthropathy with less significant systemic manifestations
-
Monoarticular arthropathy without systemic disease
-
-
Distribution: Knee is the most common
site for monoarticular disease. Wrists involved more than hands, feet,
hips, and cervical spine (similar to RA). -
Imaging features:
-
Bilateral symmetric disease for polyarticular form
-
Soft tissue swelling
-
Osteopenic
-
Epiphyseal overgrowth
-
Premature physeal closure
-
Ankylosis
-
P.831
 |
|
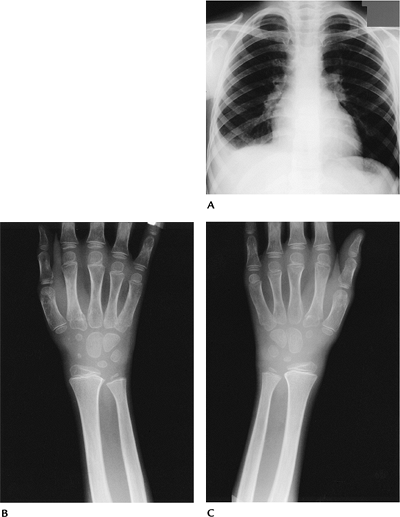
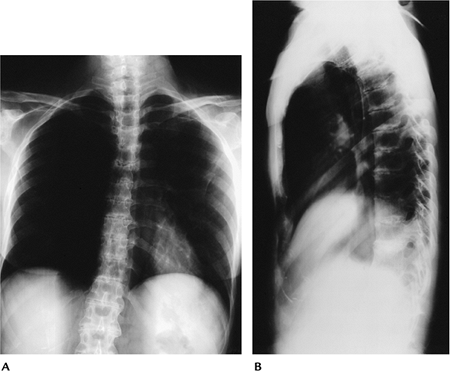
FIGURE 13-21 Still disease. (A) Chest radiographs showing a right pleural effusion. (B,C) Radiographs of both wrists showing osteopenia and soft tissue swelling.
|
P.832
 |
|
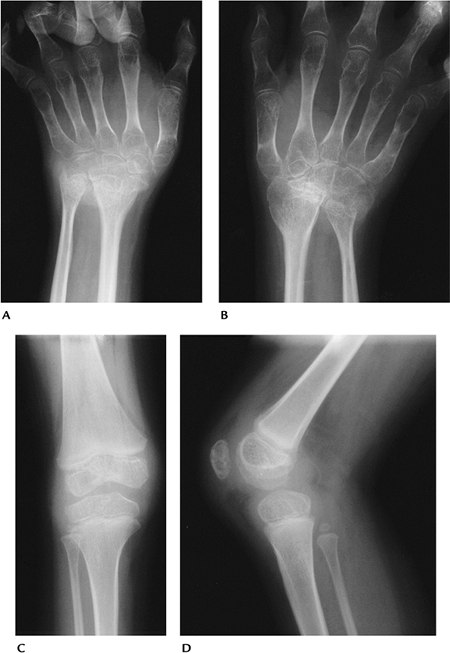
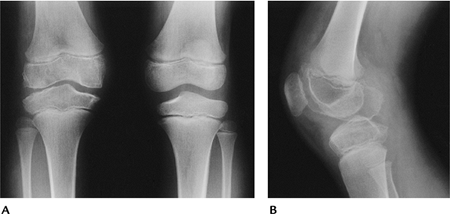
FIGURE 13-22 Juvenile chronic arthropathy. (A,B) AP radiographs of the wrists showing marked osteopenia with carpal collapse. AP (C) and lateral (D) radiographs of the knee showing epiphyseal hyperemia and soft tissue involvement (synovitis).
|
P.833
Suggested Reading
Ansell BM, Kent PA. Radiological changes in juvenile chronic polyarthritis. Skel Radiol 1977;1:129–144.
P.834
Hemophilia
Key Facts
-
Arthropathy of hemophilia is the result of repetitive hemorrhage.
-
Hemarthrosis occurs in up to 90% of patients with hemophilia.
-
Most hemorrhagic episodes occur in childhood.
-
Distribution: knee, elbow, ankle, hip, shoulder
-
Imaging features resemble juvenile chronic arthritis:
-
Asymmetric distribution
-
Dense soft tissue swelling (blood)
-
Epiphyseal overgrowth
-
Subchondral cysts
-
Late degenerative arthropathy
-
Osseous pseudotumors
-
 |
|
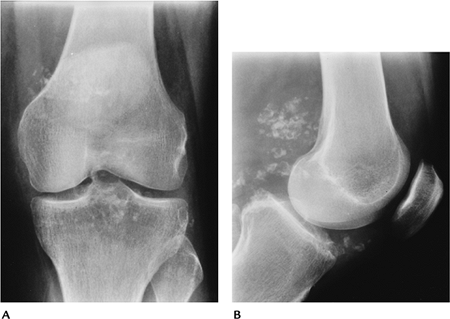
FIGURE 13-23 Hemophilic arthropathy. AP (A) and lateral (B) radiographs of the right knee showing epiphyseal overgrowth and dense soft tissue swelling.
|
P.835
 |
|
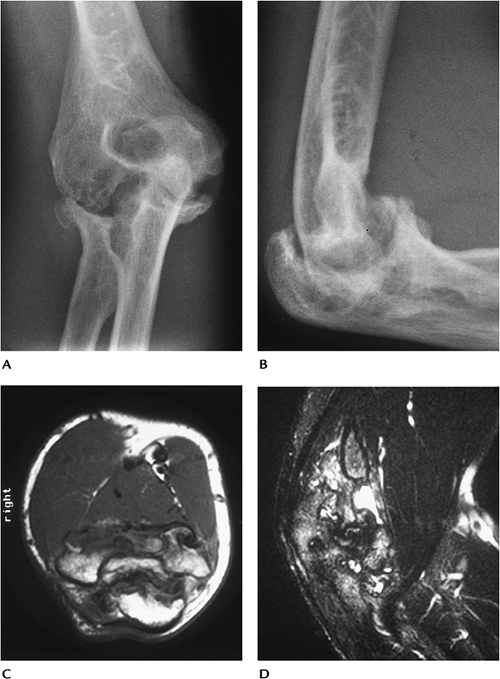
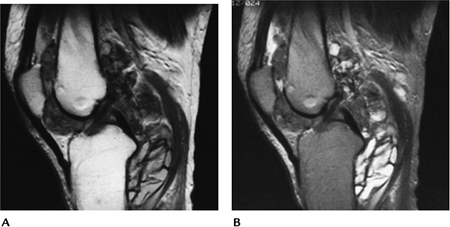
FIGURE 13-24 Hemophilic arthropathy. AP (A) and lateral (B) radiographs of the elbow showing marked joint deformity with new bone formation. Axial T1-weighted (C) and sagittal T2-weighted (D) images showing synovitis and effusion. Osseous anatomy is distorted.
|
Suggested Reading
Pettersson H, Ahlberg A, Nilsson IM. Radiologic classification of hemophilic arthropathy. Clin Orthop 1980;149:153–159.
P.836
Gout
Key Facts
-
Gouty arthropathy is the result of deposition of monosodium urate crystals.
-
Males are affected much more frequently than females.
-
Radiographic changes take years to manifest.
-
Distribution: feet most common (85%); ankles, hands, wrists, elbows. May present as olecranon bursitis in the elbow.
-
Laboratory findings: hyperuricemia
-
Imaging features:
-
Asymmetric polyarthropathy
-
Tophi
-
Well-defined erosions with sclerotic margins
-
Overhanging edge
-
Normal bone density
-
 |
|
FIGURE 13-25 Gout. Well-defined erosion with a large calcified tophus.
|
P.837
 |
|
FIGURE 13-26 Gout. Swelling of the right hand and wrist with a well-defined erosion (arrow) at the fifth PIP joint.
|
 |
|
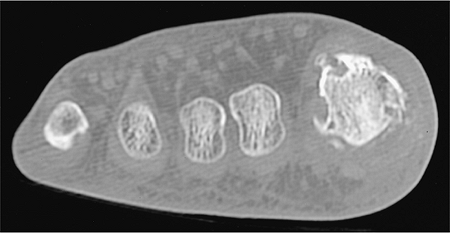
FIGURE 13-27 Gout. Axial CT image demonstrates well-defined erosions and soft tissue mass around the first metatarsal phalangeal joint.
|
P.838
 |
|
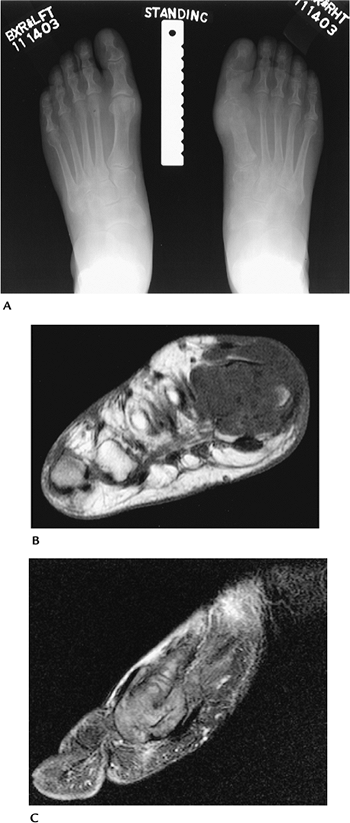
FIGURE 13-28 Gout. (A)
Standing radiographs of the feet demonstrate bone destruction involving the distal first metatarsal and proximal phalanx on the right. (B) Axial T1- and sagittal post-contrast (C) fat-suppressed T1-weighted images demonstrate advanced bone and soft tissue changes of gout. |
P.839
Suggested Reading
Pascual E. The diagnosis of gout and CPPD crystal arthropathy. Br J Rheumatol 1996;35:306–308.
Yuh JS, Chung C, Recht M, et al. MR imaging of tophaceous gout. AJR Am J Roentgenol 1997;168:523–527.
P.840
Hemochromatosis
Key Facts
-
Hemochromatosis is an inherited disorder
resulting in systemic iron deposition. It also may occur with
cirrhosis, multiple transfusions, or excessive iron intake. -
The disorder is most common in men aged more than 40 years.
-
The arthropathy resembles degenerative joint disease and calcium pyrophosphate deposition disease (CPPD).
-
Distribution: hands and wrists most common, followed by knees and hips
-
Imaging features:
-
Bilateral asymmetric arthropathy
-
Osteopenia
-
Chondrocalcinosis
-
Subchondral cysts
-
Joint space narrowing
-
Osteophyte formation
-
Subchondral sclerosis
-
P.841
 |
|
FIGURE 13-29
Hemochromatosis. Radiograph of the hand showing degenerative changes in the hand and wrist, with narrowing in the metacarpophalangeal joints, especially the second and third. |
Suggested Reading
Hirsh JH, Lillen C, Troupin RH. Arthropathy of hemochromatosis. Radiology 1976;118:591–596.
P.842
Calcium Pyrophosphate Deposition Disease
Key Facts
-
CPPD is the most common crystal arthropathy.
-
The condition affects 5% of the population, generally the middle-aged or elderly.
-
CPPD crystals are deposited in hyaline and fibrocartilage. Patients may have no symptoms or may present with severe pain.
-
Distribution: knee, pubic symphysis, and wrist most common, but may involve any joint
-
Imaging features:
-
Bilateral asymmetric arthropathy
-
Chondrocalcinosis
-
Joint space loss
-
Normal bone density
-
Multiple subchondral cysts
-
 |
|
FIGURE 13-30 CPPD. Standing radiographs of the knee showing meniscal calcifications and degenerative joint disease.
|
Suggested Reading
Adamson
TC III, Resnick CS, Gierra J Jr, et al. Hand and wrist arthropathies of
hemochromatosis and calcium pyrophosphate deposition disease. Distinct
radiologic features. Radiology 1983;147:377–381.
TC III, Resnick CS, Gierra J Jr, et al. Hand and wrist arthropathies of
hemochromatosis and calcium pyrophosphate deposition disease. Distinct
radiologic features. Radiology 1983;147:377–381.
P.843
Wilson Disease
Key Facts
-
Wilson disease is a rare liver disease resulting in copper deposition in bones, joints, and other tissues.
-
Copper interferes with normal osteogenesis, resulting in osteomalacia.
-
Up to 50% of patients develop arthropathy.
-
Distribution: hands, wrists, feet, shoulders, hips, elbow, knees
-
Imaging features:
-
Bone fragmentation
-
Marked irregularity of articular and subchondral bone
-
Osseous loose bodies
-
Resembles osteoarthritis
-
 |
|
FIGURE 13-31
Wilson disease. Advanced joint destruction with loose bodies, fragmentation, and chronic rotator cuff tear in the right shoulder. |
Suggested Reading
Menerey KA, Eides W, Brewer GJ, et al. Arthropathy of Wilson disease. Clinical and pathologic features. J Rheumatol 1988;15:331–337.
P.844
Ochronosis
Key Facts
-
Ochronosis is a metabolic disease caused
by lack of homogentisic acid oxidase. Homogentisic acid (a dark
pigment) is deposited in joints, resulting in cartilage degeneration. -
Patients typically present after age 40 years.
-
Distribution: Spine—may resemble
ankylosing spondylitis. Peripheral joints (knee, hip, shoulder)—similar
to CPPD or osteoarthritis. -
Imaging features:
-
Bilateral asymmetric arthropathy
-
Osteopenia
-
Disc degeneration and calcification
-
Subchondral sclerosis
-
Lack of significant osteophytes
-
Loose bodies
-
 |
|
FIGURE 13-32 Ochronosis. AP (A) and lateral (B) radiographs of the thoracic spine showing diffuse disc space narrowing and disc calcification.
|
Suggested Reading
Brower AC. Arthritis in black and white, 2nd ed. Philadelphia: WB Saunders; 1997:367–378.
P.845
Neurotrophic Arthropathy
Key Facts
-
Neurotrophic arthropathy results from repetitive trauma to joint without sensory nerve supply.
-
Relaxation of supporting structures
results in malalignment of osseous structure fragmentation and, in most
cases, subchondral sclerosis. -
Diabetic neuropathy is the most common
cause. Multiple sclerosis, syphilis, syringomyelia, meningomyeloceles,
and congenital insensitivity to pain also may cause neurotrophic
arthropathy. -
Distribution: lower extremity, especially foot and ankle
-
Imaging features:
Atrophic: Bone resorption and demineralization Hypertrophic: Most common Articular and osseous fragmentation Bone sclerosis Osteophyte formation Subluxation
 |
|
FIGURE 13-33 Neurotrophic arthropathy. AP radiograph of the ankle showing joint deformity, bone formation, and loose bodies.
|
P.846
 |
|
FIGURE 13-34
Diabetic patient with neurotrophic arthropathy. AP radiograph of the foot showing joint subluxations with tarsometatarsal fragmentation. |
Suggested Reading
Sequeira W. The neuropathic joint. Clin Exp Rheumatol 1994;12:325–337.
P.847
Synovial Chondromatosis/Osteochondromatosis
Key Facts
-
Primary synovial chondromatosis or
osteochondromatosis is a condition of unknown cause. Synovial
chondromas or osteochondromas form resulting from synovial metaplasia.
There are three phases:-
Phase 1: active synovial metaplasia with no loose bodies
-
Phase 2: transitional phase with metaplasia and loose bodies
-
Phase 3: no active metaplasia, but loose bodies
-
-
In older patients (>50 years of age)
the condition is twice as common in males as females. However, the
condition is also common in younger females (aged 20–30 years) and most
often involves the hip. -
The condition involves the hip in 50% of
cases, but may also involve the knee, elbow, wrist, hand, shoulder, and
temporomandibular joint. -
Radiographs may be normal unless the
loose bodies are calcified or ossified. Conventional, CT, and MR
arthrography are more useful to confirm the diagnosis. -
Secondary degenerative arthritis follows this condition.
-
Treatment consists of synovectomy and/or removal of loose bodies.
 |
|
FIGURE 13-35 Synovial chondromatosis. AP (A) and lateral (B)
radiographs of the knee showing multiple periarticular calcifications. Note the lack of significant degenerative changes at this stage. |
P.848
 |
|
FIGURE 13-36 Noncalcified synovial chondromatosis. Arthrogram image shows multiple filling defects. The joint space is normal.
|
Suggested Reading
Milgram JW. Synovial chondromatosis. A histopathologic study of 30 cases. J Bone Joint Surg 1977;59A:792–801.
Peh WCG, Shek TWH, Davies AM, et al. Osteochondroma and secondary synovial osteochondromatosis. Skel Radiol 1999;28:169–174.
P.849
Pigmented Villonodular Synovitis
Key Facts
-
Pigmented villonodular synovitis (PVNS)
is a relatively uncommon disorder characterized by synovial
proliferation with hemosiderin deposition in synovial tissues. -
The condition may involve joints, bursae, or tendon sheaths.
-
There are diffuse forms (80% involve the knee) and localized forms such as giant cell tumor of the tendon sheath.
-
The condition is diagnosed most commonly in the second through fifth decades.
-
PVNS is typically monoarticular involving
the knee followed by the hip, ankle, shoulder, elbow, temporomandibular
joint, and spine. -
Radiographic findings are evident in 80%
of cases. Findings include swelling, joint effusion (often denser than
a simple effusion), and cystic or erosive changes in bone. -
MR features are characteristic with areas
of low signal intensity on T1- and T2-weighted sequences resulting from
hemosiderin deposition. -
Treatment consists of synovectomy.
Recurrence rates are 25% to 50%. Postoperative baseline MR examinations
are recommended for more optimal detection of residual PVNS or
recurrence.
 |
|
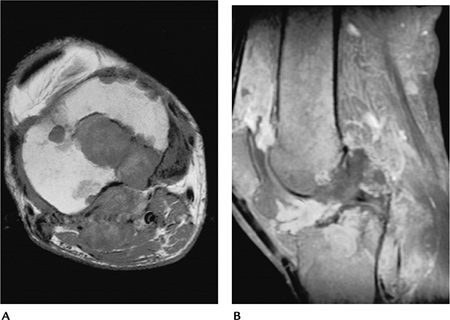
FIGURE 13-37 PVNS. Sagittal T1- (A) and T2- (B)
weighted images of the knee demonstrate lobulated soft tissue masses in the knee with areas of low signal intensity on both sequences resulting from hemosiderin deposition. |
Suggested Reading
Jelinek JS, Kransdorf MJ, Utz JA, et al. Imaging of pigmented villonodular synovitis with emphasis on MR imaging. AJR Am J Roentgenol 1989;152:337–342.
P.850
Amyloid Arthropathy
Key Facts
-
Amyloid arthropathy is attributed to
long-term dialysis using cuprophane dialysis membranes.
B2-microglobulin is deposited in the form of amyloidosis. -
Clinically the condition is unusual in
patients on dialysis less than 5 years, but occurs in 80% of patients
on dialysis for more than 10 years. Patients present with pain and
swelling in the involved joints. -
Radiographs demonstrate large cystic lesions in bone with lobulated soft tissue swelling. Pathologic fractures may occur.
-
On MR images the interosseous lesions
demonstrate signal intensity between muscle and fibrous tissue
regardless of the pulse sequence. Distention of the joint and bursa is
common. Rarely large lytic bone lesions (amyloidoma) may be evident
resembling neoplasms.
 |
|
FIGURE 13-38 Amyloid arthropathy. (A) Axial T1- and (B) sagittal T2-weighted images demonstrate low signal intensity (muscle density) deposits in the tibia (A) and in the anterior and posterior joint (B) with joint and bursal distention.
|
Suggested Reading
Cobby MJ, Adler RS, Swarz R, et al. Dialysis-related amyloid arthropathy: MR findings in four patients. AJR Am J Roentgenol 1991;157:1023–1027.
