Arthrocentesis
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Arthrocentesis
Arthrocentesis
Michelle Cameron MD
Timothy S. Johnson MD
Description
Aspiration of synovial joints is performed for diagnostic or therapeutic purposes.
Etiology
-
Causes of joint effusions:
-
Infection
-
Crystalline arthropathies
-
Hemophilia
-
Autoimmune arthropathies
-
Trauma
-
PVNS
-
Signs and Symptoms
-
Synovial joints (Table 1) are aspirated for myriad reasons, the most common of which include:
-
To rule out infection
-
To diagnose arthropathies
-
To relieve pain
-
-
Joints with enough fluid to perform arthrocentesis generally have a palpable effusion.
-
Infectious, autoimmune, and crystalline
arthropathies often are warm to the touch and may display overlying
erythema or cellulitis.
Physical Exam
-
An effusion usually is palpable.
-
The patient with infectious and crystalline arthropathies or trauma may have difficulty with ROM of the affected joint.
-
There may be outward signs of trauma or inflammation such as abrasions, erythema, or cellulitis.
|
Table 1 Best Locations for Aspirating Joint Effusions
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
Table 2 Joint Fluid Analysis
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Tests
Imaging
Radiographs often are helpful to rule out trauma and to evaluate degenerative changes within the joint.
Pathological Findings (Table 2)
-
Crystalline arthropathies show crystals when specimens are examined with polarized light:
-
Gout: Monosodium urate crystals appear
sharp (needle-like) by normal light microscopy and are brightly
birefringent on compensated polarized microscopy. -
The calcium pyrophosphate crystals of pseudogout have blunt ends and are not birefringent.
-
-
Aspirates from septic arthritis often
have cell counts >100,000 with >80–90% polymorphonuclear cells,
and they may have organisms present on Gram staining. -
Crystalline and inflammatory arthropathies also can have high white cell counts in the 50,000/mm3 range.
Differential Diagnosis
-
Septic arthritis
-
Gout
-
Pseudogout
-
Autoimmune disorders, such as rheumatoid arthritis or systemic lupus erythematosus
-
Trauma
-
Hemophilia
General Measures
-
Patients with traumatic effusions should
be treated appropriately for their underlying traumatic injury, but
arthrocentesis of the affected joint often makes these patients more
comfortable. -
Patients with septic arthritis require joint irrigation and débridement; the type of débridement depends on the joint involved.
-
Appropriate antibiotics also should be administered after all cultures are obtained.
-
Patients with inflammatory and
crystalline arthropathies generally respond well to anti-inflammatory
medications and should be referred to a rheumatologist for evaluation.
P.31
Surgery
-
Sterile skin preparation is required before aspiration.
-
Injection of local anesthetic with a
small-gauge needle into the skin may lessen the pain of aspiration
(especially if more than 1 attempt is necessary). -
The needle gauge should be large enough to withdraw the viscous joint fluid (usually 18 gauge or larger) (Fig. 1).
Complications
-
Risk of iatrogenic infection:
-
Care should be taken, especially when aspirating a potentially infected joint.
-
If cellulitis is present, care should be
taken to aspirate through uninvolved skin to avoid infecting a
previously aseptic joint.
-
-
Aspiration may be predisposing in as many as 23% of all cases of septic arthritis (1,2).
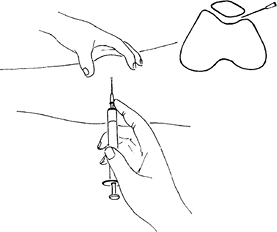 Fig. 1. Arthrocentesis of the knee is most easily done from the lateral side, under the patella.
Fig. 1. Arthrocentesis of the knee is most easily done from the lateral side, under the patella.
References
1. Esterhai JL, Jr, Gelb I. Adult septic arthritis. Orthop Clin North Am 1991;22:503–514.
2. Tsumura
H, Ikeda S, Torisu T. Debridement and continuous irrigation for the
treatment of pyogenic arthritis caused by the use of intra-articular
injection in the osteoarthritic knee: indications and outcomes. J Orthop Surg (Hong Kong) 2005;13:52–57.
H, Ikeda S, Torisu T. Debridement and continuous irrigation for the
treatment of pyogenic arthritis caused by the use of intra-articular
injection in the osteoarthritic knee: indications and outcomes. J Orthop Surg (Hong Kong) 2005;13:52–57.
Additional Reading
Park AL, Diabach JA. Infectious arthritis. In: Canale ST, ed. Campbell’s Operative Orthopaedics, 10th ed. St. Louis: Mosby, 2003:685–711.
FAQ
Q: What is the appearance of the joint aspirate under light microscopy in the setting of gout?
A: Sharp, needle-like crystals.
Q: A joint aspirate with a white blood cell count >100,000 per high-powered field is consistent with which type of arthritis?
A: Septic arthritis.
