Angular Deformities of the Lower Extremities
often present very dramatically and lead to a great deal of anxiety for
parents and families. Most are physiologically normal variants that
will resolve spontaneously. However, pathologic forms of deformity that
can result in serious disability and persistent deformity without
treatment must be differentiated from a benign condition. This
differentiation is not always apparent on the initial examination.
Recognizing the different patterns of deformity and how they evolve is
the key to understanding and treating angular deformities in children.
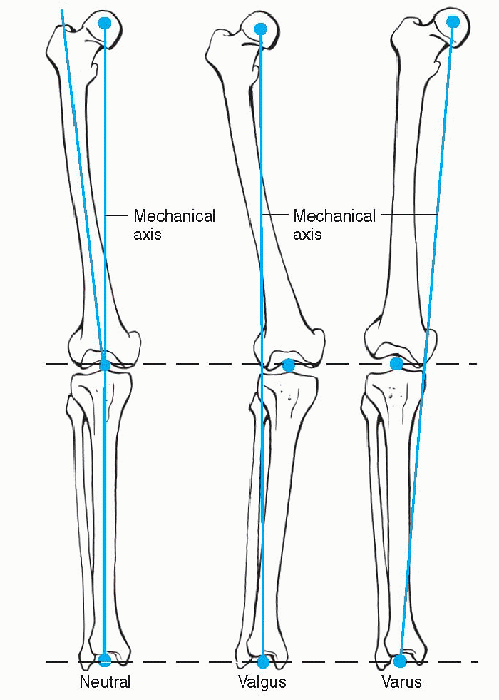
“bowlegs” or “knock-knees,” can present at varying stages of a child’s
development. The natural development of the coronal leg alignment or
femoral-tibial angle must be appreciated. At birth, the child has 10 to
15 degrees of varus at the knee. This bowleg appearance persists in
most children until 14 to 18 months, and sometimes up to 24 months of
age, when the femoral-tibial angle becomes neutral. The alignment
progresses to maximal valgus (knock-kneed) position by 3 or 4 years of
age and then gradually resolves into adult physiologic valgus (around 7
degrees) by the age of 8 years (Fig. 3-1).
deformity generally relies on measurements of the distance between the
child’s medial femoral condyles for varus deformity, and between the
medial maleoli for valgus deformity position. Although these numbers
can be recorded, they are a pseudo-quantification of the child’s gross
appearance; they can however be used for monitoring purposes.
A standing anteroposterior radiograph of both lower extremities is indicated for the following:
 |
|
Figure 3-1 Mechanical alignment of the lower extremity: normal (neutral), valgus, varus.
|
-
Trend not as expected
-
Unilateral involvement
-
Asymmetry
-
Pain
-
Generalized growth abnormality
can be determined from these films. A scanogram may also be indicated
in children over 3 years of age to evaluate concomitant leg length
discrepancy.
varum, for orthopedic evaluation. Differential diagnosis of an
ambulating toddler with excessive femoral-tibial varus alignment
includes the following:
-
Physiologic bowing
-
Infantile tibia vara, Blount’s disease
-
Metabolic disorders, rickets
-
Skeletal dysplasias, focal fibrocartilaginous dysplasia, chondrodysplasias
a benign variant of normal development, which usually resolves by 30 to
48 months of age. In some children, however, the varus alignment does
not correct and progresses as the proximal medial tibial physis
undergoes pathologic changes, failing to grow properly. This is known
as infantile tibia vara, or Blount’s disease. Less frequently, genu
varum is the result of metabolic disorders or skeletal dysplasias.
These last two categories of disorders can usually be screened based on
overall child growth (less than fifth percentile growth would suggest a
dysplasia), radiographic appearance (changes in physes elsewhere in the
body), or lab values (changes in calcium, phosphate, alkaline
phosphatase, vitamin D, or 1,25-dihydroxy vitamin D in rickets).
bowing is often difficult on initial presentation. Some experts
consider the two processes to be on a continuum. Blount’s disease
usually presents with an acute bowing at the proximal tibia whereas
smooth, evenly distributed bowing of the tibia is usually indicative of
physiologic genu varum. The pathologic genu varum may occur when the
compressive forces exerted by the deformity irreversibly injure the
medial aspect of the proximal tibial physis and metaphysis. In the case
of pathologic genu varum, there might be simultaneous changes in other
physes (ankle, femur, spine).
|
TABLE 3-1 LANGENSKIÖLD’S CLASSIFICATION OF BLOUNT’S DISEASE
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
tibia vara rely on identification of the physeal damage. They were
classically clarified and categorized by Langenskiöld, who published a
six-stage classification system for Blount’s disease based both on the
radiographic appearance of the proximal tibial physis and on patient
age (Table 3-1). Unfortunately, these criteria
are not useful for initial diagnosis, since most changes in the
proximal tibia are not evident until after 3 years of age. In addition,
interobserver
reliability
is poor (50%) with this classification system and it is especially
difficult to distinguish between stages II and IV, which might affect
the ultimate outcome of treatment of Blount’s disease.
 |
|
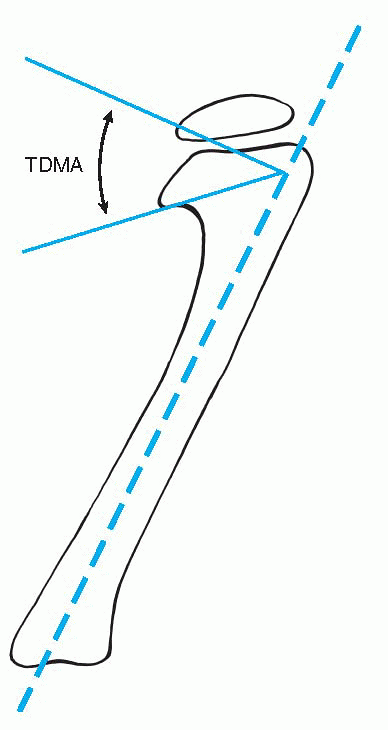
Figure 3-2
Tibial metaphyseal-diaphyseal angle (TDMA) of Levine and Drennan. The angle lies between a line drawn through the most distal point on the medial and lateral breaks of the tibial metaphysic and perpendicular to the long axis of the tibia. |
differentiate physiologic and pathologic tibia vara prior to the
development of changes in the physis as described by Langenskiöld. The
tibial metaphyseal-diaphyseal angle (TDMA) was originally described
with a threshold at 11 degrees, beyond which infantile tibia vara was
suspected (Fig. 3-2). More recently
investigators, raising the threshold to 16 degrees, have modified the
criteria for the TDMA. The “gray zone” of TDMA between 10 and 16
degrees warrants special attention as pathologic genu varum might
develop. When in doubt, magnetic resonance imaging is a useful tool to
identify pathologic changes in the proximal tibial physis.
patient age and proximal tibial physeal changes. Brace treatment may be
recommended for children under 3 years of age with a TDMA measured at
least 16 degrees or presenting with Langenskiold stage I or II. It
should continue for no longer than 1 year and should be discontinued if
deformity persists to age 4 years or progresses to stage III. Bracing
may be accomplished with one of a variety of various orthoses that
exert valgus movement on the proximal tibia. Traditionally, a
knee-ankle-foot orthosis (KAFO) is used. There are conflicting reports
on whether nighttime or daytime brace wear is sufficiently effective.
The more a brace is worn (as close to 24 hours a day as feasible), the
more effective it should be. However, it remains controversial, as its
efficacy has not been proved.
early. Practically, the definitive diagnosis of Blount’s disease is
made around 3 years of age, when Langenskiöld changes become evident. A
corrective valgus osteotomy is indicated for children who present at
age 4 years or older, with Langenskiöld stage III or higher even at a
younger age, or who have not benefited from bracing. There are numerous
potential complications with this procedure:
-
Recurrence of deformity:
-
□ Especially when done in older children
-
□ Inadequate correction: one should overcorrect infantile tibia vara to slight valgus alignment
-
□ Failure to laterally displace the distal segment
-
-
Compartment syndrome: prophylactic fasciotomy should be done
-
Peroneal nerve palsy: fibular osteotomy
should be done at a more distal site, in the diaphysis, to avoid injury
to common peroneal nerve -
Growth disturbance, which progresses to
recurvatum deformity of proximal tibia: reason the osteotomy is
performed distal to the tibial tubercle.
medial epiphyseal deformity, and in children approaching maturity
require more complex surgical intervention. An osseous bar excision
with or without interposition of fat or bony cement and elevation of
the medial epiphysis to resolve the contour of the joint surface might
be combined with lateral physeal stapling to reverse the pathologic
changes of the proximal tibia.
morbidly obese boys approaching skeletal maturity without previous
history of fracture or infection. A recent onset of deformity without
previous bowing should raise suspicions about adolescent Blount’s
disease. The workup of these children should include a long cassette
radiograph with patella centered over the femur to avoid rotational
error. The etiology of adolescent Blount’s disease is thought to be
varus deformity forced by the large thighs of these obese children
generating increased force across the medial aspect of the proximal
tibial physis. Unlike infantile Blount’s disease, however, the more
mature physis is stunted but not as profoundly deformed. The physis
will show widening on radiographs; however, the epiphysis will not be
as collapsed as in the infantile form.
adolescent Blount’s disease. Since most are far above the ninety-fifth
percentile for weight at their age, proper instrumentation must be used
and operative beds must be provided for these “large adult”-sized
patients being treated in a pediatric hospital. Many experts also
recommend sleep studies to evaluate for sleep apnea, which is present
to some degree in most of these patients. Furthermore, a slipped
capital femoral epiphysis should always be considered in this population.
operative. There is no role for bracing in this condition. Good results
have been reported with a number of approaches:
-
Osteotomy and internal fixation: usually closing wedge through proximal medial tibia, with avoiding overcorrection in adolescent Blount’s.
-
Lateral epiphysiodesis: if adequate
growth is remaining to slowly correct the varus (may be done by
stapling, which is potentially reversible). -
Gradual correction of deformity with
external fixator: numerous techniques have been designed to correct the
deformity in multiple planes if necessary.
proven successful, and an overall good final result should be expected.
Complications are not uncommon, however, and careful preoperative
planning is necessary with these procedures.
are 3 to 5 years of age, when the maximal valgus angulation of the
lower extremities occurs. However, if that deformity persists beyond 8
years of age and is outside 2 standard deviations of the norm, it is
defined as pathologic. As with other deformities, the level of
deformity needs to be evaluated on long cassette standing radiographs.
Most commonly, the deformity is in the distal femur, however, proximal
tibia and joint laxity should also be considered. Classification of the
degree of deformity can be made based on how far laterally the
mechanical axis of the extremity falls from the center of the knee.
individualized. As with most deformities the severity of deformity, the
functional and cosmetic ramifications, and the unilateral involvement
are considered. Possible treatment options include:
-
Hemi-epiphysiodesis: staple
epiphysiodesis either permanent or transient, depending on remaining
growth; less predictable but lower morbidity than osteotomy. -
Osteotomy: in the skeletally mature; most often a closing medial wedge osteotomy of the distal femur is performed.
sound alignment of the lower extremity with a horizontally positioned
tibial plateau and ankle joint.
severelooking deformity in a newborn, with a calcaneus positioned foot
and dorsiflexion contracture at the ankle. This is a benign condition.
The etiology is presumed to be an intrauterine packaging phenomenon,
without any associated abnormalities. The abnormal position of the foot
resolves with simple parental stretching and plantar foot stimulation.
Serial casting is rarely necessary. The tibia deformity resolves by 2
years of age in nearly all cases. Ultimately the affected limb will end
up with a smaller calf musculature and leg length discrepancy.
Typically, the discrepancy is between 3 and 8 cm. Contralateral
epiphysiodesis is the most common treatment. Investigators have
reported a correlation between the degree of initial angulation and the
eventual growth retardation.
disorder, affecting 1 in 140,000 to 190,000 newborns. Often there is no
fracture at the time of birth; however, the abnormal structure of the
bone usually leads to inevitable fracture. This deformity is closely
associated with neurofibromatosis. Approximately 5% of patients with
neurofibromatosis have the deformity, and over half of the children
with a congenital pseudoarthrosis are eventually diagnosed with
neurofibromatosis. An association with fibrous dysplasia is also
reported. Classification schemes for this entity are based on the
radiographic appearance of the bone at the pseudoarthrosis. The most
commonly cited is the Boyd classification (Table 3-2).
consistently been difficult. If fracture has not yet occurred, a total
contact orthosis is recommended to protect the extremity until
maturity. Once fractured, the pseudoarthrosis will generally not heal
without surgery. Surgical principles
for
this problem include excision of the fibrous tissue present at the
pseudoarthrosis and then obtaining rigid fixation. Surgical approaches
include the following:
|
TABLE 3-2 BOYD’S CLASSIFICATION OF NEUROFIBROMATOSIS
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Intramedullary fixation, initially crossing ankle and subtalar joint
-
Vascularized fibular transfer
-
Distraction osteogenesis, Ilizarov techniques.
site, particularly with intramedullary fixation, late complications are
common. Refracture, joint stiffness, and leg length discrepancies
severely limit the success of any surgical approach to this problem.
Trans-pseudoarthrosis, below knee or Syme amputation is not an uncommon
salvage procedure.
varying degrees of fibular hypoplasia. In the more severe forms,
complete absence of the fibula might present with an anteromedial bow
of a shortened tibia, a ball and socket ankle joint, tarsal coalitions,
and absence of one or more lateral rays of the foot. These patients
might present with structural anomalies of the upper extremities as
well. Proximal focal femoral deficiency (PFFD) frequently coexists with
fibular hypoplasia. Treatment depends on the severity of the fibular
hypoplasia. Treatment for limbs with absent fibula and more extensive
hypoplasia with unstable foot is most commonly treated with a modified
Syme amputation. Less involved limbs with fibular hypoplasia and a
stable plantigrade foot might benefit from simple treatment of the leg
length discrepancy and do fine.
DJ, Schoenecker PL, Sheridan JJ, et al. Use of an intramedullary rod
for the treatment of congenital pseudoarthrosis of the tibia. J Bone
Joint Surg 1992;4A:161-168.
MD, Schoenecker PL. Use of the metaphyseal-diaphyseal angle in the
evaluation of bowed legs. J Bone Joint Surg 1993;75A: 1602-1609.
AM, Drennan JC. Physiological bowing and tibia vara: the
metaphyseal-diaphyseal angle in the measurement of bowleg deformities.
J Bone Joint Surg 1982;64A:1158-1163.
SJ, Edwards PM, Tidwell MA. Langenskiold classification of tibia vara:
an assessment of interobserver variability. J Pediatr Orthop
1994;14:152-155.
