Gunshot and Wartime Injuries
One – General Principles: Basics > Principles of Treatment > 11 –
Gunshot and Wartime Injuries
workload for some urban trauma centers in the United States and are
also common in war-torn regions throughout the world. The purpose of
this chapter is to review the epidemiology, pathophysiology, and
treatment of gunshot wounds and war injuries. This chapter is intended
not only to help those who evaluate gunshot wounds as a major part of
their practice but also orthopaedic surgeons who occasionally see
patients with such injuries.
settings differ. Firearms seen in nonmilitary settings include
handguns, rifles, and shotguns.7,35,83,84,141 Conventional military weapons can be divided into the categories of small arms and explosive munitions. Small arms consist of pistols, rifles, and machine guns. Explosive munitions
consist of artillery, grenades, bombs, mortars, and land mines. Armored
vehicle crew casualties represent a special subgroup of injuries seen
in those who work and fight in and around armored vehicles.
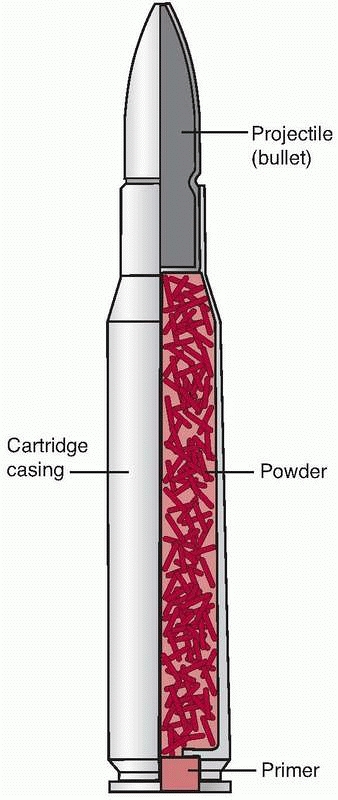
barrel to a target. The bullet is usually contained in a cartridge
consisting of powder, a primer, and a cartridge case all in one unit (Fig. 11-1).
Handguns and rifles are classified by the diameter (size) of the barrel
(9 mm, 0.45 inch, 7.62 mm). Handguns used by the military are the same
as used those by civilian police
and
others in regard to size, shape, and caliber. They are usually
semiautomatic, which means a bullet is fired every time the trigger is
pulled and as long as there is ammunition in the weapon’s magazine.7,35,83
 |
|
FIGURE 11-1
Schematic drawing of a cartridge. An entire cartridge is made up of the cartridge case, the bullet, a primer, and powder. When struck, the primer initiates powder burning, generating the pressure to propel the bullet in flight. |
nonmilitary injuries. A handgun is intended to be fired over a short
range and is small. Two types of handguns are most commonly seen:
pistols and revolvers (Fig. 11-2A). A pistol has a magazine that contains cartridges, which are fed (or cycled) into the barrel every time the trigger is pulled (Fig. 11-2B).
Revolvers contain cylinders with chambers that contain cartridges. The
cylinder rotates so that a cartridge is aligned to the barrel when the
trigger is pulled.83,141
 |
|
FIGURE 11-2 Types of handgun. A.
A 9-mm Browing P-35 pistol used in several countries as the military handgun. It is also available to the nonmilitary market. This firearm was first produced in the 1930s. B. Revolver; the cylinder rotates to align with the barrel for each cartridge. |
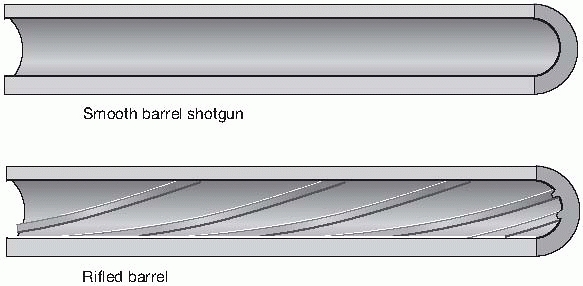
strike a target farther away from the shooter than can a handgun or
shotgun (Fig. 11-3). In general, the barrel is
longer and has rifling to impart a spin on the bullet, lending
gyroscopic stability in air. Rifling consists of spiral grooves that
line the barrel, engaging the bullet and causing it to spin on the
longitudinal axis. The bullets fired from rifles are more aerodynamic
in shape than those fired from pistols, leading to more accurate bullet
flight. Bullets for nonmilitary rifles may have an open tip or “soft
nose” to allow for expansion of the bullet when striking the target.
Military bullets have complete metal jacketing to limit deformation or
fragmentation, which decreases wound damage. Machine guns are intended
to fire in the full automatic mode; this occurs when repeated shots are
fired as long as the trigger is held down, as opposed to the
semiautomatic fire described earlier. Machine guns generally weigh more
than rifles and are installed onto vehicles and aircraft.130
and have the ability to fire in both fully automatic and semiautomatic
modes. In an effort to reduce recoil, cartridges used in these weapons
are not the full-powered rifle cartridges seen in civilian hunting
rifles or in military weapons of the first half of the twentieth
century.141 For example, the
standard Soviet infantry rifle for World Wars I and II was the Mosin
Nagant M 91/30, which fired a 7.62-mm, 150-grain bullet at
approximately 2800 feet per second (fps). After World War II, the
replacement rifle (AK-47) fired a 7.62-mm, 120-grain bullet at 2340
fps. The AK-47 also has the ability to be fired in the fully automatic
and semiautomatic modes.
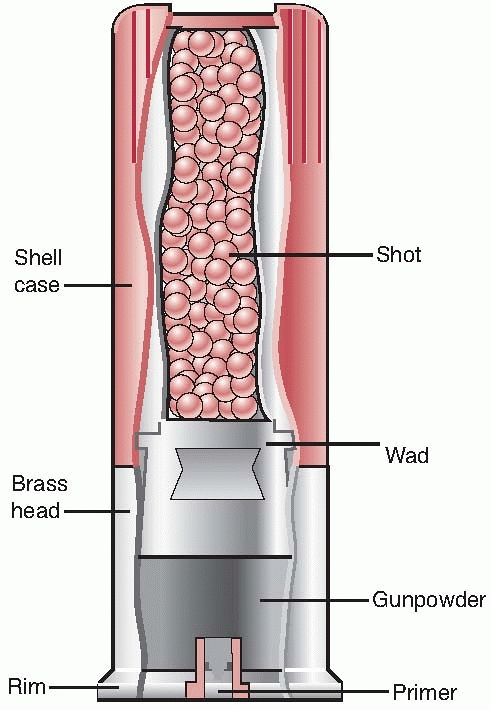
pellets are often contained in a cup or wad that keeps them together and pushes the shot out of the barrel (Fig. 11-5). The pellets begin to spread the farther they move from the barrel.84
The spread of the pellet shot over a given distance is dependent on the
size of the shot, the length of the barrel, and the degree of “choke”
on the barrel. Choke is a constriction at the end of the barrel that
will cause less spread of the shot over a given distance. A standard
measure of choke is the amount of pellets that are put into a circle at
40 yards. A full choke should put 70% of its pellets into the circle,
whereas an “improved cylinder” choke should put 50%. When within a few
feet of the barrel, the spread of the shot is negligible.
 |
|
FIGURE 11-3 M-16 series military rifles (from top to bottom): M16A1, M-16A2, M-4A1, and M-16A4.
|
 |
|
FIGURE 11-4
Barrel types: smoothbore (shotgun) and rifled. The smoothbore barrel is commonly used for shotguns, whereas a rifled barrel is used in both rifles and handguns. |
They are the most common agents for wounding soldiers on a battlefield,
starting during the World War I (1914-1918), when artillery became more
common on the battlefield, and continuing to be the most common injury
mechanism through today. Table 11-1 describes
the relative proportion of different types of weapons that generated
casualties on the battlefield from various wars during the 20th century.
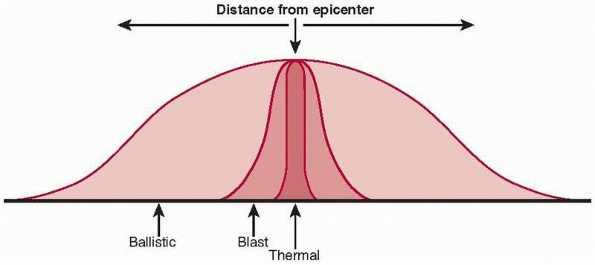
around the explosive device. Blast injuries occur because of a transient blast overpressure caused by the exploding munitions. Thermal injuries
are caused by a transient increase in local temperature as a result of
the explosion. Blast and thermal injuries occur relatively close to the
exploding munitions, whereas ballistic injuries also can occur farther
from the device.12,34,120
The distances from the munitions that the various effects may be seen
(ballistic, blast, thermal) will vary with the type of device and the
environment. An explosion in a confined space, for example, will
increase the effects of blast overpressure. Someone who is wounded
closer to the exploding munitions may have combined ballistic, thermal,
and blast effects compared with someone farther away. A typical mortar
shell, when detonated in an open area, might have thermal effects
within a few feet of detonation. The blast or pressure wave may cause
ear injury within 30 feet. Fragments, however, can still cause injury
at greater than 100 yards from detonation.
 |
|
FIGURE 11-5
Shotgun shell. A shotgun shell consists of the primer, powder, wad, and shot. All of this is contained in the shell casing. When powder burning is initiated by the primer, the wadding propels the shot down the barrel and into free flight. |
|
TABLE 11-1 Casualty Generation by Weapon
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
in a range of up to several miles. The projectiles may be antivehicle,
contain white phosphorus, or be explosive filled. The diameter of U.S.
military artillery cannon barrels ranges in size from 105 mm to 8
inches. The explosive-filled projectiles are most often used against
infantry soldiers. When detonated, they produce fragments of varying
shape and size, which cause wounds. The fragments produced depend on
the casing of the artillery round. Modern artillery casings break up to
produce more uniform fragments over a given area. The fragments may
range from a few milligrams to several grams in weight. After
detonation, fragments may initially travel at several thousand meters
per second. This initial velocity rapidly decreases because of the
irregular shape of the fragments.8,12,34,120
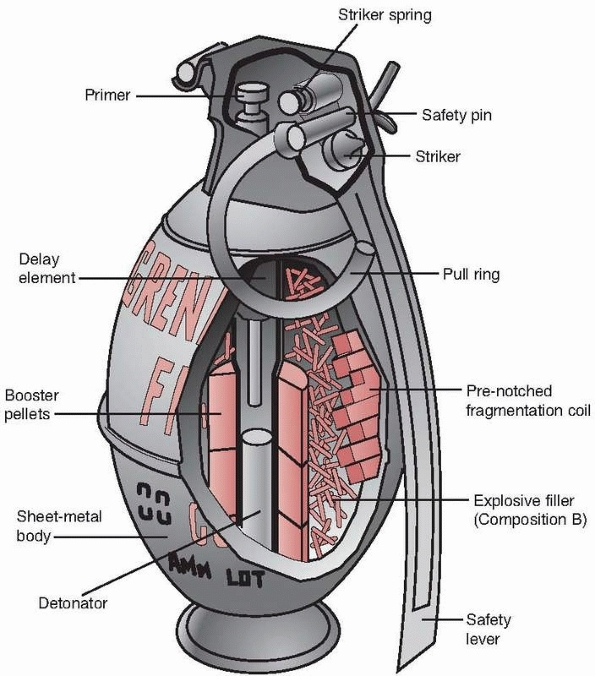
Grenades may produce smoke for signaling or be designed to disable or
destroy tanks or to injure soldiers. As with artillery shells, the type
of fragments produced is dependent on the composition of the container.
Most modern grenades have a notched or prefragmented casing that
produces fragments of a uniform size when detonated.8,12,34,120
arc to produce indirect fire. Projectiles fired from mortars may
produce smoke, white phosphorus, or explosive fragments. These weapons
are smaller and are more limited in range compared with the cannon. As
with the other weapons described earlier, fragments produced by the
explosive shells vary with the composition of the shell’s casing.8,9
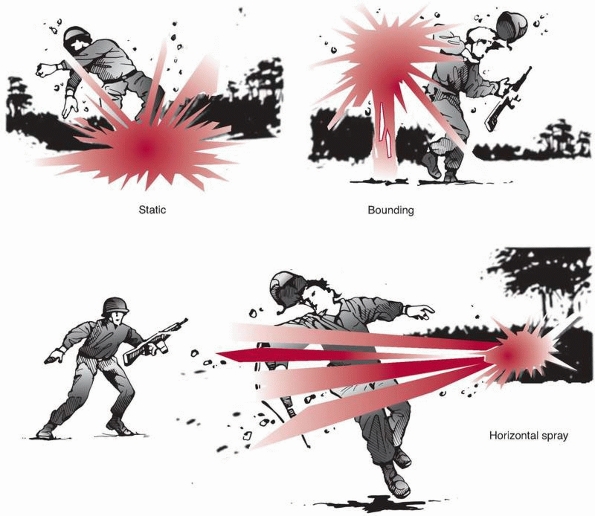
land mines are intended to destroy or disable vehicles, such as tanks.
Antipersonnel land mines are classified by the U.S. Army as static,
bounding, or horizontal spray (Fig. 11-8).
Another category, unconventional or improvised devices, will be handled
separately in this section. Currently, there is much concern about land
mines throughout
the
world because of vast land-mined tracts that remain in Asia, Africa,
and the Balkans. Estimates vary, but between about 70 to 100 million
land mines remain in place, which, until removed, will continue to be a
hazard to those living or working in the area (Fig. 11-9).1,7,8,12,34,112,120
 |
|
FIGURE 11-6
Mechanisms of injury explosive munition. The three mechanisms of injury are ballistic, blast, and thermal. The ballistic effects take place much farther away from the explosion compared with blast or thermal effects. |
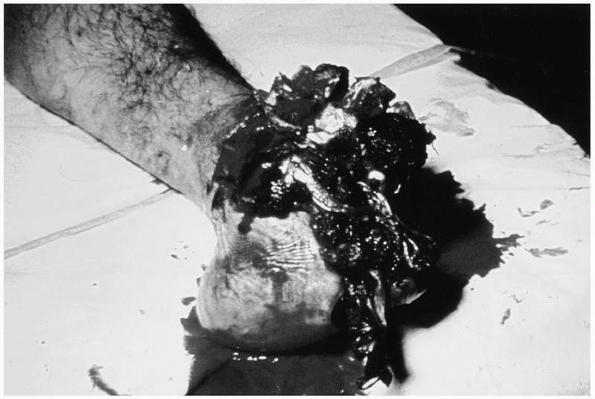
that are laid on top of the ground or buried in soil and are detonated
when someone steps on the device. They are the most common type of land
mine seen throughout the world. They contain a small amount of
explosive (100-200 g) and produce a characteristic pattern of injury112 (Fig. 11-10).
Russian surgeons obtained considerable experience with land mines
during their war in Afghanistan (1979-1988), which prompted them to
conduct both laboratory and clinical investigations on the mechanism of
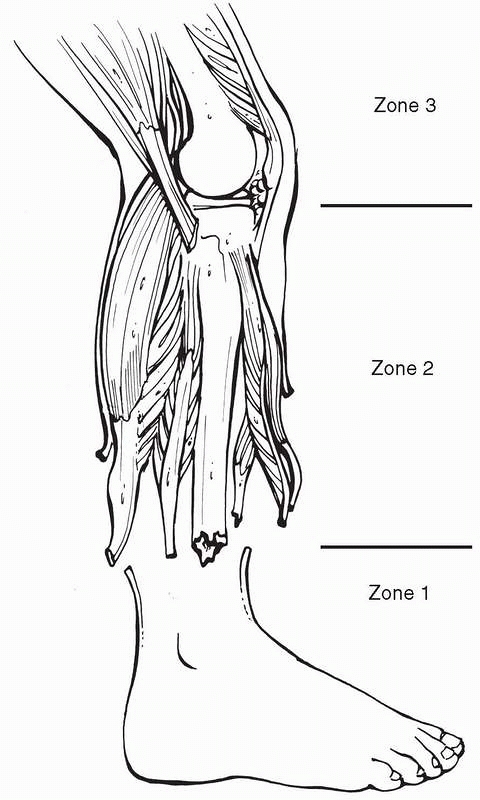
injury. Injuries produced by static land mines are primarily to the
lower extremity (Fig. 11-11). There are three areas of injury—there is an area of mangling or avulsion (traumatic amputation), which occurs at the midfoot or distal tibia. There is a second area in which the soft tissues are separated
from bone along fascial planes in the leg (brisant). This area is a
tidewater area in terms of tissue survival; the tissue is compromised,
but it may heal. The area extends from below the knee to the level of
“avulsion” injury of the foot or lower leg. Third, more proximally,
injuries may occur from fragments or debris
propelled from the land mine but not necessarily from direct effects of
the blast itself. The degree of injury is dependent on the size and
shape of the individual’s limb, the type of footwear and clothing worn,
the amount and type of soil overlying the land mine, and the size of
the land mine.1,112
 |
|
FIGURE 11-7
Grenade. This cutaway illustrates the casing, which is composed of notched wire, producing fragments when detonated. The powder is stored in the casing and is ignited by the detonator. |
 |
|
FIGURE 11-8
Antipersonnel land mines. This illustrates the types of manufactured antipersonnel land mines seen throughout the world. A static mine is tripped when a person steps on the mine. A bounding mine, when tripped, propels an explosive device to about waist high and then detonates. The horizontal spray mine directs multiple small fragments in one direction when tripped. |
 |
|
FIGURE 11-9
Small static land mine. Note the small size of this land mine compared with a hand. These are usually made of minimal metal components to avoid detection. |
mines that, when tripped, propel a small grenadelike device to about 1
to 2 m in height. The device then explodes, producing multiple small
fragment wounds similar in nature to those produced by grenades.112
are mines that, when tripped, fire fragments in one direction. These
land mines may be used to protect a perimeter or during an ambush. The
U.S. Army’s Claymore mine is an example of this type of mine. It fires
about 700 steel balls that weigh 10 grains each in one direction. The
weapons produce multiple fragment wounds to exposed personnel nearby (Fig. 11-12).112
ordnance, such as a grenade or mortar shell, to detonate when a person
steps on the device, a person pulls a tripwire, or the device is
triggered remotely by radio or control wires. These devices may be made
out of locally available materials as well. They vary in construction
from smaller antipersonnel devices to large explosive devices with
several kilograms of explosive to disable or destroy vehicles (Fig. 11-13).
 |
|
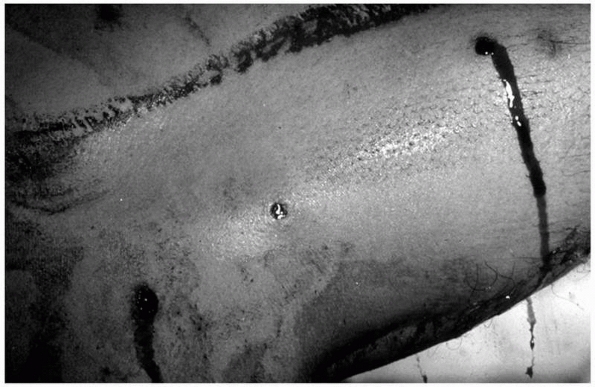
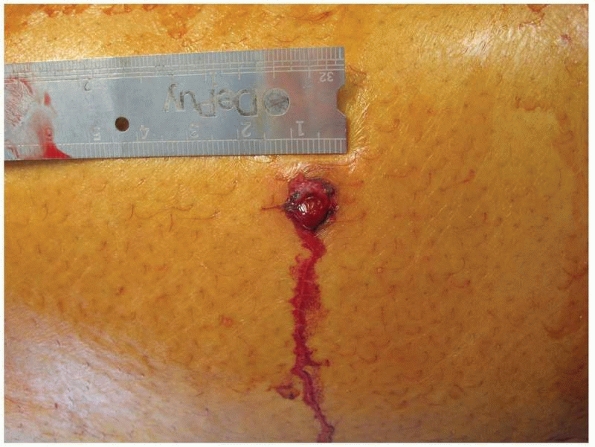
FIGURE 11-10
This photograph is of a foot injured by a small planted land mine. The mine was under the forefoot and the patient had footwear. |
 |
|
FIGURE 11-11
Small static land mine injury. This illustrates the three areas of injury sustained from a small static land mine. First, there is an area of avulsion or amputation; second, there is an area of soft tissue stripping where tissue may or may not survive. Third, proximal to this area, there may be fragment wounds from debris or the land mine, or injury from the fast translation of being propelled upward from the land mine itself. |
 |
|
FIGURE 11-12
Claymore mine injury. This photograph illustrates multiple small fragment wounds of a thigh from a patient injured by a Claymore mine. |
Afghanistan and Iraq conflicts are improvised explosive devices. One of
the larger antipersonnel mines used against civilians is the suicide bomber.
This is a term given to an individual who carries a large explosive
charge and detonates it in location of a crowd or building to achieve
maximum casualties. One of the more common constructs for such a bomb
is in the form of a vest containing explosive along with material for
fragments. The fragments increase the wounding potential of the device
and consist of items such as ball bearings or nails. Large antivehicle
land mines have made transportation and troop movements difficult.1,8,34
aircraft. They may consist of one large explosive device or may carry
submunitions that are distributed more uniformly over a target area.
Cluster bombs are an example of the latter device.9,12,120
Injuries to crewmembers occur both in and around vehicles. Those
injured outside of the vehicle have injuries similar to infantrymen.
Two types of weapons are used to perforate the armored vehicle’s
envelope to cause injury to the crewmen (antitank land mines may be
considered a third type).
 |
|
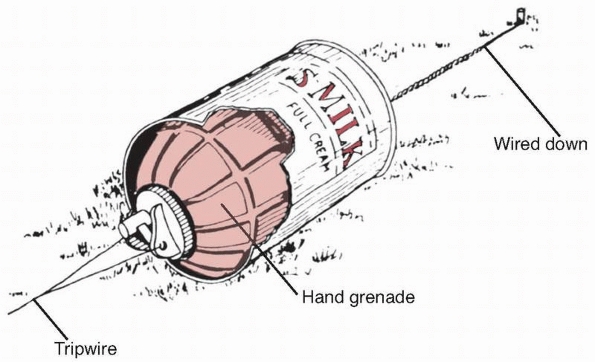
FIGURE 11-13
Improvised explosive device (IED). This illustrates an IED (“booby trap”) made from a grenade that is inserted into a can. When the wire is tripped, the grenade explodes. This drawing is taken from a World War II British Commando manual. IEDs are the most common type of land mine or booby trap seen in the Vietnam, Iraq, and Afghanistan conflicts. |
 |
|
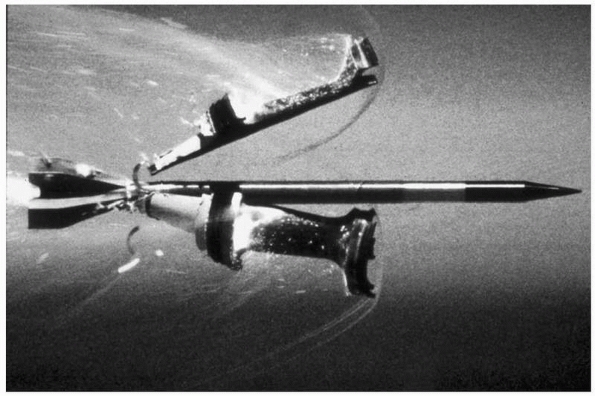
FIGURE 11-14
Kinetic energy armor piercing round. This illustration shows the dense metal penetrator shaped like an arrow and the “petals” of the sabot surrounding the penetrator falling away. |
This consists of a hard piece of metal, such as tungsten or depleted
uranium, that is fired out of a cannon at a high velocity. The
projectiles used today are long and narrow and cause a high
concentration of pressure over a very small cross-sectional area to
defeat the armor plate. If the round penetrates to the crew
compartment, injuries may be caused by the penetrating round itself,
debris knocked off from the inside of the vehicle itself, or armor
debris. Because the penetrating rounds are large, injuries to
individuals tend to be catastrophic.35
 |
|
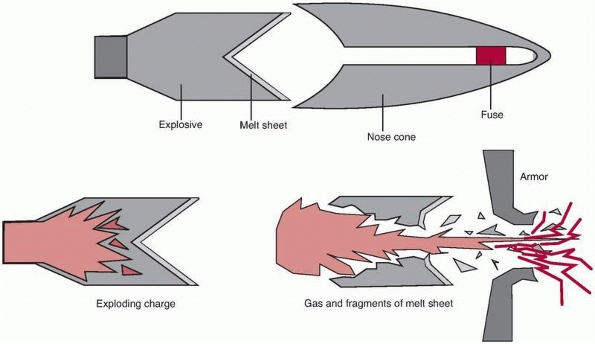
FIGURE 11-15
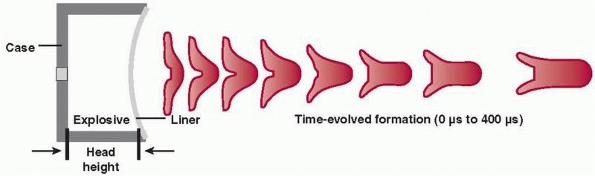
Shaped charge or high-explosive, antitank (HEAT) round. Explosive is packed around a reverse cone-shaped metal liner called a melt sheet. When detonated, it generates a jet of high temperature and pressure that defeats armor through plastic or elastic deformation. |
They consist of an explosive-filled warhead that is packed around a
reverse cone-shaped piece of metal (copper or aluminum). When
detonated, the liner collapses and a jet is produced, which travels at
up to 10,000 feet per second. The jet produces an area of high
temperature and pressure over a very small cross-sectional area. When
the jet penetrates the armor, it produces two areas of under armor
debris. First, there is the jet of the shaped charge. The jet produces
catastrophic wounds when it directly hits one of the crewmen. Second,
there is an area of under armor debris called spall,
which is material knocked off from the inside face of the armored plate
itself. Many of today’s armored vehicles have liners that do not allow
spall debris to form.35,112
This device has a shallow concavity for the liner and forms a “slug”
rather than a fully developed jet to penetrate vehicles. The “slug” is
less affected by intermediate targets, such as dirt and debris, than
the jet of the shaped charge. Although it is considered to be a new
innovation, this technology has been present since at least the 1930s.2
reported estimates of gunshot injuries in the United States for 1993
through 1998. The authors estimated that during this period, there were
approximately 180,533 fatal gunshot wounds and about 411,000 nonfatal
gunshot wounds for the 6-year period. There was a decline in the annual
nonfatal
rate
by 40% (from 40.5 to 24 per 100,000 population) and in the fatal rate
by 21.1% (from 15.4 to 12.1 per 100,000 population). This decline
corresponded with the overall decrease in violent crime of 21%. The
stated cause for injury was assault in 57%, self-inflicted in 20%,
unintentional for 13%, and unknown for 10%. During the study period,
the average number of self-inflicted fatalities exceeded those from
assault (18,227 versus 15,371 per year).56
 |
|
FIGURE 11-16
Explosively formed projectile (EFP). A modification of the shaped charge, the liner has a shallow concavity that propels a “slug” at high velocity. The slug is less likely to be disturbed by intermediate targets or debris compared with the jet of the shaped charge. Antivehicle land mines based on this principal are being used against U.S. and Allied Forces in the Iraqi Conflict. |
in violent crime from 566.4 to 473.5 per 100,000 population (16.5%) and
in murder from 6.3 to 5.7 per 100,000 population (9.5%).48 Deaths caused by firearms in the United States also decreased from 35,957 (13.5 per 100,000) to 29,569 (10.5 per 100,000).26
found that males were seven times more likely to receive a firearm
injury than were females. Black men aged 20 to 24 years had the highest
annual firearm-related injury rate for both fatal and nonfatal groups
(166.7 and 690 per 100,000 population, respectively). This compared
unfavorably to the firearm injury rate of 13.4 per 100,000 (fatal) and
30.1 per 100,000 (nonfatal) for the entire population. These
demographics also explain why the concentration of patients with
gunshot wounds is higher in trauma centers for cities with a higher
black population, such as Detroit, Los Angeles, Philadelphia, Chicago,
and New Orleans.26,48,61
reported on orthopaedic patients treated for gunshot wounds in New
Orleans at an inner-city Level I trauma center. They found that
patients with gunshot wounds represented 24% of all admissions and 26%
of all orthopaedic trauma surgical cases. The most common locations for
nonfatal gunshot wounds are in the extremities (Table 11-2). Gotsch et al.56
reported that extremity wounds represented 46% of nonfatal wounds
caused by assault and 71.8% of unintentional wounds. A series from
Cordoba, Argentina, found that 63% of gunshot victims had injuries to
the upper or lower extremities.14 A
review of records at Henry Ford Hospital in Detroit, MI, from 2001
through 2006 found that 42.4% of all patients admitted with a diagnosis
of gunshot wounds had extremity wounds. This figure increases to 50.2%
if pelvic and spine injuries are included.
reported a ratio of 1:1.2:1 for deaths:hospital admissions and
transfers:emergency department treatment and discharge, respectively.
A prospective study on battle casualties was conducted during the
Bougainville campaign in the Solomon Islands during World War II to
assess patient injuries based on the weapon and tactical circumstances.120
The patients were then followed through their initial surgical care to
look at outcome. A second study was performed during the Vietnam
Conflict to assess 7964 casualties during an 18-month period during the
conflict. The patients in this study (Wound Data and Munitions
Effectiveness Team [WDMET]) were evaluated in terms of the tactical
situation, the weapons used, the injuries produced, and patient outcome.9
injured is relatively constant, probably because wounds produced on the
battlefield tend to be a random event (Table 11-3).
Between 60% and 70% of wounded patients admitted to a medical treatment
facility have wounds to the extremities, and about 21% of those
admitted have fractures. Use of body armor to protect soldiers and
airmen was studied in World War II and the Korean
Conflict and was found to reduce thoracic and abdominal wounds.13,73
|
TABLE 11-2 Anatomic Distribution of Gunshot Wounds
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
TABLE 11-3 Percentage Anatomic Distribution of Wounds (Living Wounded U.S. Soldiers)
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
from World War I, the Bougainville campaign in World War II, and the
Vietnam Conflict is shown in Table 11-1.9,92,111
The proportion of injuries caused by bullets has been relatively
constant from conflict to conflict. Recently, fragment-producing
explosive munitions have accounted for an increasing proportion of
casualties seen from the battlefield. This trend is expected to
continue.
From both the Bougainville and WDMET data, the lethality of a bullet
wound is about 0.33. Fragments from grenades, mortars, and artillery
range from 0.05 to 0.10. Death from tripping a land mine is also about
33%.9,120
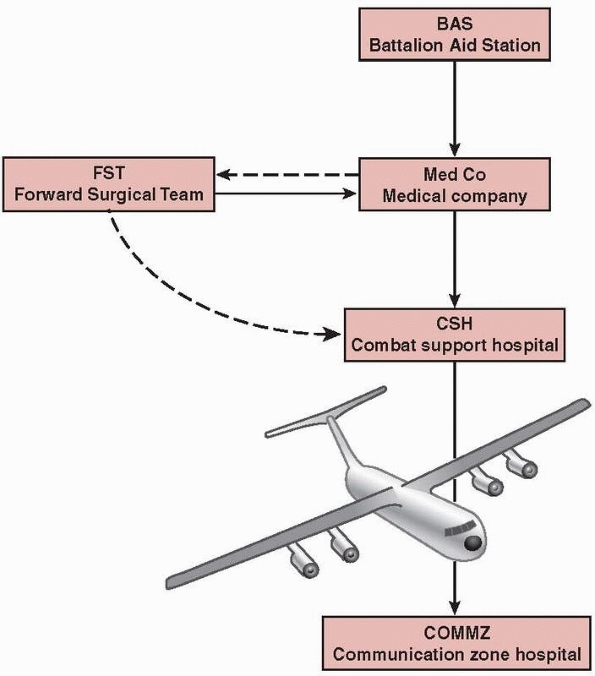
All major armies throughout the world have made some provisions to care
for wounded soldiers. The U.S. military (Army, Navy, and Air Force)
have similar echelons of care to treat wounded solders.97,98
battlefield consists of self-care or buddy care. The first step may be
to take cover from hostile fire. Treatment for extremity wounds
consists of stopping the bleeding, applying a dressing, and splinting.
the patient and adjusts the dressings and splint. The medic also has
the capability of providing pain relief, administering antibiotics, and
arranging for further evacuation.
|
TABLE 11-4 Lethality by Weapon
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
contact for a wounded soldier. Here, the patient is further evaluated,
splints and dressings are adjusted, and the patient is triaged. If the
casualty load is light, patients are treated as they arrive. If the
casualty load is heavy, patients must be triaged to allocate the
resources of evacuation and surgical care. Ideally, the triage takes
place along the entire evacuation chain. If a patient’s condition
worsens, his or her priority may increase.97,98
care in the evacuation scheme. This facility has the capability of
providing blood transfusions and has limited radiographic capability.
This unit is the first level of care with any bed holding capability.
Adjacent to the medical company may be the forward surgical team (FST)
that provides the first possible surgical support on the battlefield.
The purpose of this unit is to provide surgical care of
nontransportable patients, who are those patients whose outcome would
be compromised by being evacuated farther for surgical care. Examples
of patients who should have surgery at the FST are those with
penetrating abdominal wounds who are in shock and those with major
traumatic amputations. Because of the mission to treat emergent
patients, the FST is staffed with one orthopaedic surgeon and three
general surgeons. Having an orthopaedic surgeon is important to make
decisions concerning amputations as well as caring for those with
multiple injuries. Often those with multiple injuries have major
extremity wounds. Because the FST has no bed holding capability, it
must be colocated with a medical company to complete its mission. Goals
of surgery are to stabilize the patients and prepare them for
evacuation. Similar units for the U.S. Navy are the Surgical Company to
support the U.S. Marines and the MFST for the U.S. Air Force. While all
three are not exactly the same because of the need to meet
service-specific requirements, they all function at the same level of
care.97,98
next echelon of care on the battlefield. The entire unit when assembled
has 296 beds and includes intensive care unit capability, six operating
rooms, and laboratory capability, and it is staffed by three
orthopaedic surgeons in addition to general surgeons, internists, and
emergency physicians. This hospital is presently deployed as a modular
unit in a 40-bed slice with two operating rooms. There are three
general surgeons and one orthopaedic surgeon assigned to the hospital
in this configuration. This facility is the first surgical echelon for
the majority of battlefield patients, including those with orthopaedic
injuries. Goals of care at this hospital are to stabilize the patients
and to prepare them for evacuation out of the combat zone. Examples of
care for patients arriving at the CSH include the treatment of soft
tissues,
fracture stabilization via casting or external fixator application, and
treatment of a partial or complete amputation. The CSH is ideally
located near an airfield. The equivalent U.S. Navy hospital is the
Fleet Hospital, and for the U.S. Air Force, the Expeditionary Medical
Support (EMEDS) Hospital, which is a modular system.97,98
 |
|
FIGURE 11-17
U.S. military medical evacuation. This shows the present scheme of evacuation for wounded soldiers used by the U.S. Army. Surgical care by orthopaedic surgeons takes place at the forward surgical team (FST), combat support hospital (CSH), or communication zone hospitals. |
(FST or CSH) directly from the battlefield depending on the severity of
the injury and if the tactical situation permits. In more stationary
situations, such as during the Vietnam Conflict, this occurs more
frequently.90,91
During the Vietnam Conflict, the U.S. military controlled the airspace
and did not have much geographic movement of hospitals or troops, such
as occurred during World War II. Because of this, overflight of
facilities in the evacuation chain occurred to bring patients promptly
to a facility that could provide more care.
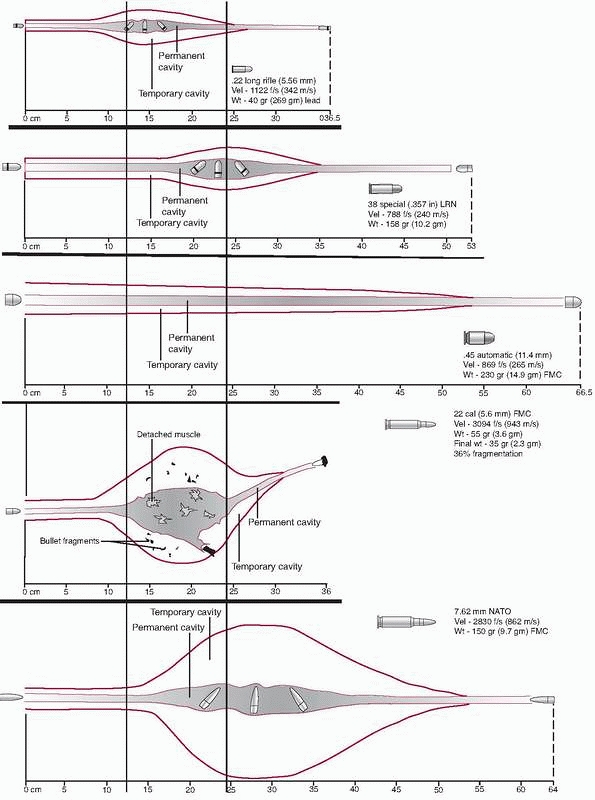
Three observable phenomena occur when a bullet strikes tissue. First,
tissue is crushed by the projectile as it passes through, leading to a
localized area of cell necrosis that is proportional to the size of the
projectile. This area of the projectile’s path is called the permanent
track or permanent cavity (Fig. 11-18).
The stretch results from a lateral displacement of tissue that occurs
after the passage of the projectile. There is a transient increase in
pressure of 4 to 6 atmospheres (atm) for a few milliseconds’ duration.
This transient lateral displacement of tissue, such as skeletal muscle,
vessels, and nerves, macroscopically appears as blunt trauma. Inelastic
tissue, such as bone, may fracture in this area.
pressure wave that travels at the speed of sound preceding the bullet
in tissue. This pressure wave is of very short duration, a few
microseconds, but it may generate pressures up to 100 atm in magnitude.43,67,68 The shock wave has not been shown to cause tissue injury.
When a projectile strikes skin and creates a permanent cavity, it
produces a small amount of necrosis that is proportional to the size of
the projectile. The temporary cavity splits the skin, which produces a
larger opening of tissue. Grundfest et al.57
used cadaver skin to test threshold velocities for penetration. The
skin was stretched over a frame during testing, thus altering the
behavior seen in vivo. The authors used steel ball bearings from 1/16
inch to 1/4 inch in size as well as 11/64-inch lead spheres fired from
an air rifle. They found that increasing the size of the projectile
also required increasing the velocity needed to perforate the skin.
porcine animal model. These investigators used a solid nondeforming
5.56-mm bullet and fired it into the thighs of the animals. The authors
found larger exit wounds compared with the entrance wounds as a result
of splits in the skin caused by the larger temporary cavity produced as
the bullet yawed in tissue. The larger wound allowed for better
exposure of the wound path and freer drainage of wounds. Also, the
authors found skin vasospasm, which produces blanching, soon after
wounding. This area did not revascularize for several hours. If the
loss of blood supply is a criterion for excision, the transitory nature
of the blanching shows that viable tissue would be sacrificed in this
area if evaluated soon after wounding.
 |
|
FIGURE 11-18
Projectile tissue interaction. Three areas can be measured in the projectile tissue interaction: the sonic wave, the temporary cavity, and the permanent track. The temporary cavity is caused by a transient lateral displacement of tissue (stretch), whereas the permanent track is made by passage of the projectile, crushing tissue. The sonic wave, although measurable, has not been shown to cause tissue injury. |
found that projectile shape was important in determining the appearance
of a skin wound. The authors fired a solid nondeforming bullet point
first and then base first, noting the different appearance of the skin
wound in each case. The bullets were fired at over 5000 fps. For the
projectile going base first, large skin splits were produced by an
early temporary cavity. No such effect was seen with the bullets going
point first through the skin.
Muscle that is touched by the projectile in the permanent tract has a
microscopic rim of tissue that is actually necrotic. This tissue, if
the blood supply to the muscle remains intact, can heal over time
without surgical intervention. The area of cell death sloughs and, as
long as the wound can drain, will heal up spontaneously.
causing the temporary cavity. The stretched area of temporary cavity
may split along fascial planes. This area appears grossly as bruised or
contused tissue. Bruised skeletal muscle ordinarily heals uneventfully.
Microscopically, there are disrupted skeletal muscle fibers and
capillaries. After a period, there is leukocyte infiltration followed
by inflammation and healing.36,42,48,69,103
formed; thus, the region stretched by the temporary cavity is
perforated in multiple places. Tissue weakened by these tiny
perforations is often split by the temporary cavity stretch, and pieces
between perforations are detached. This often greatly increases the
size of the permanent cavity.48
body when it is fired, the high-pressure gas that pushes the projectile
out of the barrel will pass into the tissues through the hole formed by
the projectile—often causing greatly increased tissue displacement and
disruption.
Fractures may occur via two mechanisms, either when the projectile
strikes bone or, rarely, indirectly by the temporary cavity. Direct
fractures (Fig. 11-19) occur when a projectile
strikes the bone. Because of the density and relative inelastic
behavior of bone, fracture line propagation may occur well beyond the
area crushed by the projectile itself, leading to bone comminution and
the production of secondary missiles from the bone itself. Because the
secondary missiles of bone disrupt tissue before it is stretched by the
temporary cavity, this has the effect of increasing comminution around
the bullet path, and might even cause increased soft tissue disruption,
reminiscent of the previously mentioned synergism between bullet
fragmentation and temporary cavity stretch.
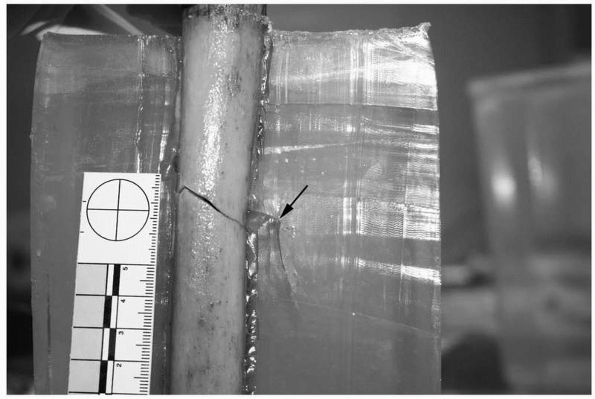
may occur when a projectile passes close to the bone in soft tissue and
a strain occurs to such a degree as to cause a fracture. Indirect
fractures are almost always simple. Clinically, indirect fractures to
bone are rare compared with those formed when bone is struck directly
by the projectile.28,67,68,69,70 Figure 11-20
illustrates the shot path 8 mm from the edge of the diaphyseal bone in
ordnance gelatin, showing how indirect fractures appear. The bullet
path is perpendicular to the page, going away from the reader.
 |
|
FIGURE 11-19
Direct fracture. Cortical bone is very dense, so when a projectile strikes, fracture lines propagate away from the bullet’s path, causing comminution. The temporary cavity may cause further displacement. |
fired through fluorescein-soaked gauze placed on the surface of the
skin to determine the amount of fracture site contamination that
occurred with each shot. The authors found massive fluorescein
contamination with the direct fractures; however, only 3 of 14 bones
with indirect fractures had medullary fluorescein contamination.
Periosteal contamination was less with indirect fractures compared with
the direct fractures.
 |
|
FIGURE 11-20 Indirect fracture. A fracture may occur without the bullet striking the bone. This illustrates a bullet path (arrow) adjacent to the bone. A simple fracture occurred from the effects of the temporary cavity.
|
proposed a classification of incomplete fractures because of gunshot
wounds, describing “drill hole” and “divot” fractures. The “drill hole”
fractures are seen with bullet perforation of both cortices yet minimal
comminution surrounding the bullet tract. They occur in metaphyseal
bone. The “divot” fracture was described as an eccentric perforation of
a diaphyseal long bone. More extensive injury may be present than
apparent on plain radiographs, and the “divot” injury may be an occult
complete fracture of diaphyseal bone. Such fractures should be treated
as complete fractures unless other radiographic measures, such as a
computed tomography scan, show an incomplete fracture.
First, some authors have exaggerated the effects of velocity to include
it as being the sole criterion for increased injury or as a means to
classify gunshot wounds. Velocity is one of several factors involved
with the production of the wound. The introduction of the M-16 rifle
during the Vietnam Conflict was heralded as producing equivalent wounds
or causing equivalent “incapacitation” because of the weapon’s higher
muzzle velocity of an advertised 3200 fps. The M-193 bullet fired from
the M-16A1 rifle was 5.56 mm in diameter and weighed 3.6 g. This
compared with the 7.62-mm bullet fired at a velocity of 2700 fps
weighing 8 g. Later testing in the laboratory found that the increased
severity of wounds sometimes seen with the M-16A1 was the result of
bullet fragmentation, not the modest 10% increase in velocity. In fact,
the greatest increase in muzzle velocity for military rifles occurred
in the late nineteenth century when the armed services of several
nations, including the United States, changed to a full metal jacketed
bullet from a solid lead one. This resulted in an increase of muzzle
velocity from about 1000 fps to 2000 fps.39 The change in firearms, however, resulted in decreased wound severity because bullet deformation was limited by the jacketing.
is the idea that “kinetic energy” or “energy deposit” is directly
proportional to wound severity. Kinetic energy is the amount of
potential energy available for work. “Energy deposit” is a description
of how much energy is lost or “deposited” in tissue. While one can
measure the projectile’s velocity and weight as it enters and exits a
body or tissue medium, it does not describe how this potential energy
is used. The potential energy may be used for the crush or stretch, but
it may also be consumed in mechanics that may not cause any tissue
injury. Examples where energy may be consumed, but not cause tissue
damage, include the shock wave, bullet heating, and bullet deformation.
should include a thorough history and physical examination. The
extremity should be inspected for both entrance and exit wounds after
all clothing has been removed. The limb should also be inspected for
swelling, deformity or shortening, and ecchymosis. The limb should be
palpated for crepitus. Examination for distal pulses should be done to
assess vascular status. In an awake patient, assessment should also be
done to assess the patient’s motor and sensory status. If the patient
is not able to comply, this fact should be documented with a note to
recheck if the patient’s condition improves.
covering the path of the bullet. Standard long bone radiographs,
including both the joint above and below, should be done if included in
the bullet’s path. If a joint wound is suspected, standard views should
be taken of the joint.
Second, there is a wound that contains splits in the skin but has
negligible skin loss and can eventually be closed without resorting to
more extensive skin grafting or flap coverage (Fig. 11-22).
Third, there is a wound in which there is skin loss, which requires the
use of partial-thickness skin grafting or flap coverage (Fig. 11-23).
Likewise, successful treatment of simple fractures associated with
minimal soft tissue disruption have also been treated with local wound
care and fracture stabilization in a cast or splint.54,72,86,92,101,157
resulting from the temporary cavity, from a projectile that is
traveling sideways and presenting the long axis of the bullet to the
skin, or from bone becoming a secondary missile, causing a more
extensive wound. The splits produce an exit wound that will allow for
free drainage of the wound, preventing the formation of an abscess or a
hematoma.
 |
|
FIGURE 11-21 Simple perforating wound. This shows a simple wound caused by perforation of the bullet.
|
 |
|
FIGURE 11-22 Skin splits. Splits in the skin may be caused by bone fragments, debris, or the stretch of the temporary cavity.
|
from shotgun pellets, bullets, or bone fragmentation. Initial treatment
of the more extensive wounds should be done in the operating room.
Longitudinal incisions of the skin and underlying fascia to relieve
pressure, remove hematoma and debris, and expose the underlying muscle
should be done. Surgical removal of skin is rarely indicated for the
initial surgery, other than trimming irregular edges. As described
earlier, blanching may give a false impression of nonviable skin if
seen soon after injury and lead the surgeon to excise viable skin.
seen in wartime. Injuries range from single fragment wounds to multiple
fragment wounds with extensive soft tissue loss (Fig. 11-24).
Often, a person has multiple fragment wounds of the extremity skin,
subcutaneous fat, and skeletal muscle, yet without significant injury
to bone, vascular, or nerve structures.9,120 In certain controlled circumstances, small fragment wounds may be treated nonoperatively.17
closure [VAC] dressings) for the initial management of more extensive
wounds has been suggested to reduce the size of defect needing
coverage, promote local growth factors, and remove debris and nonviable
tissue from the wound. A randomized study comparing this method to
standard dressing changes is not available in the literature.91
 |
|
FIGURE 11-23
Skin defect. A skin defect may occur from secondary missiles created by bone fragments or by multiple fragments or projectiles. This case illustrates a shotgun wound from close range. |
 |
|
FIGURE 11-24
Multiple fragment wounds. This illustrates multiple small skin wounds that occur with many exploding munitions. They are often of the skin, subcutaneous fat, and skeletal muscle only. |
surgeon or a hand surgeon who is skilled in extremity soft tissue
coverage. Before soft tissue coverage, the wound should be stable.
all demonstrated that a relatively minimal margin of necrosis occurs in
skeletal muscle if the blood supply remains intact. Excision of tissue
has been recommended for skeletal muscle that would not survive, thus
acting as a bacteria medium. Recognition of how to identify tissue that
needs to be excised is imprecise, at best. Scully et al.135
evaluated 60 biopsy samples taken from the initial wound excision of 12
war wounds during the Korean Conflict. The surgery took place between 3
and 8 hours from the time of injury. The samples were graded by the
surgeon as to the presence of the four “C’s”: color, consistency,
contractility, and circulation (bleeding). The samples were then
evaluated by a pathologist who graded the degree of muscle fiber
damage. The authors found correlation of microscopic damage to
consistency, contractility, and bleeding. Color was not found to
correlate to the degree of soft tissue damage. Also, time was not found
to be a factor in determining tissue viability.
limb, there is a small rim of cell death that will heal uneventfully if
the wounds are allowed to drain.46,67,103
For wounds in which there is more extensive skeletal muscle injury, a
more formal exploration of the wound is warranted. The wound may be
enlarged through the use of longitudinal skin incisions as described
earlier. Macroscopic evaluation of skeletal muscle will determine what
tissue needs to be removed. A simple analogy for surgeons is, “muscle
that looks like hamburger should be excised, muscle that looks like
steak should stay.”
Wars by Larrey and Desault showed that incision, to allow for free
drainage of the wound and to relieve swelling (compartment pressure),
was the technique used by these surgeons for extremity wounds.
wound is designed to relieve the area of excessive tension, rid it of
dead tissue and massive hematoma and provide excellent drainage. Perhaps relief of tension is the most important contribution of wound debridement [authors’ emphasis].”64
inside a relatively closed space, such as the anterior compartment of
the leg, which is surrounded by fascia and bone. The swelling occurs
because of direct trauma, hemorrhage, or ischemia. A hematoma inside of
a compartment may lead to pressure and ischemia of muscle. The
diagnosis of compartment syndrome is primarily clinical.
Longitudinal incisions to release pressure within a compartment and to
expose tissue has been recommended by military surgeons at least since
the time of the Napoleonic Wars.44
gunshot wound may range from minimal to that involving the entire
compartment. Involvement of the entire compartment is rare, but it does
occur when patients have extensive soft tissue injury or vascular
injury causing ischemia. With the initial evaluation, patients with a
large hematoma, vascular injury, or excess swelling are candidates for
more formal operative treatment of the soft tissues.
those who sustain gunshot injury. Bullet wounds are contaminated
wounds. Bullets themselves, when fired, do not become “sterile” because
of the heating and friction encountered in the barrel. LaGarde89
created contaminated wounds by firing bullets contaminated with anthrax
into an animal model. The animals developed an anthrax infection.
Dziemian and Herget36 placed barium
sulfate dye on the surface of an ordnance gelatin block. After shooting
through the surface into the gelatin, the dye coated the entire path of
the projectile’s path, showing that surface material is brought into
the wound.
evaluated 420 wounded Israeli soldiers following the 1973 October War.
They found an overall infection rate of 22% for all wounded. Wounds
from explosive munitions have a higher rate of infection than those
from gunshot wounds alone. Eight of 20 (40%) soldiers with femur
fractures developed infection. In addition to femur fractures, the
authors found burns of greater than 25% body surface area and
penetrating abdominal wounds of the colon were risk factors.
further evaluated risk factors in war wounds after the 1982 War in
Lebanon. The authors compared 1 month of hospital admissions for
wounded Israeli soldiers during the 1973 and 1982 wars. They found the
overall infection rates were similar between the two groups (31.5% and
30.4%, respectively). Risk factors for fracture site infections were
found to be the presence of open drains, amputations, multisystem
injury, and a fractured femur.
compared 3471 wounded soldiers with 436 soldiers who had wounds “at
risk” for the development of gas gangrene (open fractures, more
extensive soft tissue injury, long delay to care, wounds to the buttock
or thigh). Those with wounds at risk were treated with penicillin,
whereas those without at-risk wounds were not. Infection developed in
28 of 3471 (5 with gas gangrene) untreated wounds and in 2 of 436 (0
with gas gangrene) penicillin-treated wounds.
divided 310 patients with open fractures (78 because of gunshot wounds)
into one of three treatment groups: no antibiotics, penicillin and
streptomycin, and cephalothin. Four of 78 wounds (5%) became infected,
one with osteomyelitis. The authors attributed the infection to
severity of injury in three of the patients who had shotgun wounds with
extensive soft tissue damage. A fourth infection occurred in the
no-antibiotic group.
compared the use of ceftriaxone and cefazolin for gunshot fractures
with minimal soft tissue disruption (<1-cm wound) that were treated
nonoperatively, with 50 patients in each group. Follow-up was 59%, and
the authors reported no infections based on the cultures taken in the
emergency department. They concluded that the 1-day ceftriaxone regimen
is more cost effective than the 3-day cefazolin regimen.
reported a prospective study at their institution of 186 patients with
218 gunshot fractures. All fractures were treated nonoperatively and
were considered to be “low velocity” based on the appearance of the
wound and history. Wounds larger than 1 cm associated with fractures
were excluded. The authors compared the use of oral antibiotics
(ciprofloxicillin 750 mg twice a day) to the use of intravenous
antibiotics (cephapirin sodium 2 g every 4 hours and gentamicin 80 mg
every 8 hours). There were two infections reported in each group. All
infections were associated with fractures of the distal tibia.
nonmilitary setting is low. None of these studies show the superiority
of any particular antibiotic regimen; rather, it is the presence of
antibiotics versus no antibiotics that helps reduce infection.
Infections from war wounds remain higher than those associated with
nonmilitary gunshot wounds alone.95,137,138
Patients with war wounds are usually injured by explosive munitions,
which are more debris and dirt ridden, as well as historically having
delayed care because of medical evacuation.
for nonmilitary gunshot wounds are dependent on injury severity.
Isolated perforating wounds of the soft tissue only without vascular
injury, or those patients with isolated simple fractures, may be
treated initially with a first-generation cephalosporin. This applies
to those who are treated as either inpatients or outpatients. Those
with more extensive injuries with soft tissue loss may benefit from the
addition of an aminoglycocide. For patients who are allergic to
penicillin, consider using clindamycin or vancomycin.
|
TABLE 11-5 Recommended Antibiotic Regimen
|
|||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||
morbidity compared with other gunshot wounds. Intra-articular injuries
may result in arthritis secondary to trauma as well as through the
degenerative effects of lead itself. While elevated serum lead levels
may be present with extra-articular gunshot wounds, the most common
reports are with intra-articular wounds.94,134
Retained intra-articular bullets not only cause lead synovitis and
arthritis but also can cause systemic lead poisoning. Animal studies
have demonstrated significant articular degeneration with implantation
of lead into rabbit knees compared with controls.15
Early changes (1-2 weeks) include synovial hyperplasia, mild
inflammation, and articular surface slit formation. Late changes (3-6
weeks) include giant cells and foreign particles (lead and bone
fragments) in the synovium, focal chondrocyte proliferation,
duplication of the tidemark, and chondrocyte columnar disorganization.15,66
Implantation of lead pellets into rabbit knees induces significantly
greater degeneration in the femoral and tibial articular surfaces,
medial and lateral meniscus, and synovium at 4, 6, 10, and 14 weeks.15,66,94,96,134
Nearly 95% of the lead storage in the body occurs in bone. The
half-life of lead in the blood stream is less than 2 months compared
with 20 to 30 years in the bone.94
handgun bullets, and it may be a potential source of lead poisoning.
Steel shot has replaced lead in many areas of the world in an attempt
to reduce the lead burden on wildlife. Bismuth shot is also being used
as a lead replacement in Canada. Modern shotguns therefore may be
firing steel rather than lead shot. Regardless of whether the
projectile is known to be lead, trauma from a bullet, pellet, or
fragment will still have adverse consequences for the joint. Because of
this, all intra-articular projectiles should be removed. Through
irrigation and debridement of the joint cavity is necessary to remove
all the foreign material, including fragments of skin and clothing.
the absence of fracture, should undergo surgery. Clothing and other
debris from the outside may be aspirated into the joint. Also,
cartilage damage is common despite the normal radiographic appearance
of the joint.148
fractures are present, the stabilization of the fractures is carried
out initially with spanning external fixation, followed by repeat
irrigation and debridement 48 to 72 hours later and definitive internal
fixation once adequate debridement has been achieved.
treating patients with intra-articular bullet injures of the shoulder,
elbow, hip, and knee. Advantages of this technique include better
visualization of the joint surface and the ability to more easily
repair osteochondral fragments, ligaments, or knee meniscus.
Disadvantages include increased operative and setup time as well as
potential compartment syndrome. Care must be taken with using this
technique to ensure the equipment is available and the surgeon is
familiar with its use.
of the shoulder region, including arterial, venous, and nerve injuries.
Vascular injury is present in 15% of these cases. The risk of vascular
injury in the shoulder is four times higher in patients with a major
fracture than in those without a major
fracture.157,160 Nerve injuries are the most important determinant of long-term function of the limb.
open surgical techniques for removal of the bullet and its fragments
from the shoulder joint and the subacromial space.5,30,111,119,145
In cases where the joint capsule is violated by the bullet and the
bullet has traversed the joint, clothing fragments, skin, and other
debris could be driven into the joint. In the absence of
intra-articular bullet fragments, irrigation and débridement of the
joint is warranted.
be stabilized with arthroscopic techniques. Small and nonviable
fragments should be removed.145
Unstable fractures and those involving the articular surface require
open reduction and internal fixation. Large osteochondral fragments can
be stabilized with bioabsorbable pins, headless screws such as Herbert
screws, Acutrak screws, or a combination of these devices (Fig. 11-25).
In the presence of intra-articular fracture displacement, comminution
and metaphyseal-diaphyseal dissociation, an open technique with a
deltopectoral approach is used to reconstruct the joint surface.
Fractures of the surgical neck and shaft can be addressed with internal
fixation using a locked plate and screws. Hemiarthroplasty is an option
in nonreconstructable fractures.
 |
|
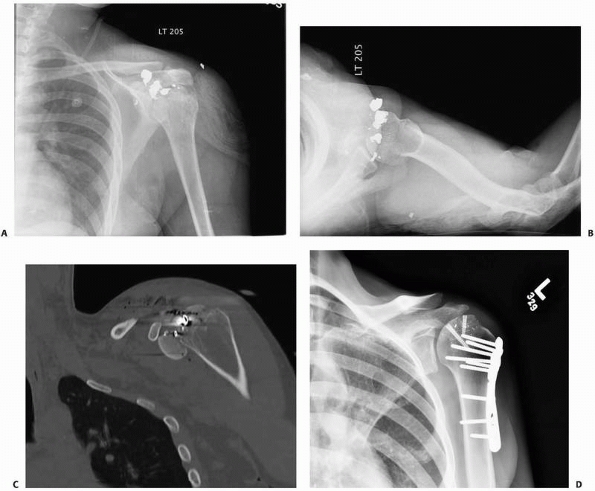
FIGURE 11-25 Preoperative anteroposterior (A) and lateral (B) radiographs and computed tomography scan (C) of the shoulder showing intra-articular injury. D. Postoperative radiograph showing reduction with plate and screws. Headless screws were used for the articular fragments.
|
In a series of 58 patients with penetrating injury to the brachial
plexus, there were 6 ulnar nerve injuries, 12 median nerve injuries, 2
radial nerve injuries, 5 musculocutaneous nerve injuries, 1 axillary
nerve injury, and 3 suprascapular nerve injuries. In the same cohort,
there were 13 C-5, 10 C-6, 10 C-7, 5 C-8, and 10 T-1 root injuries.
There were 8 lateral cord, 6 medial cord, and 10 posterior cord
injuries. The trunk injuries included seven upper trunk, three middle
trunk, and three lower trunk injuries. In this series, 24% of the
patients had vascular injuries when brachial plexus injury was present.
One or more elements of the plexus were repaired in 36 of the 58
patients in this series. There were 3 good (8%), 23 useful (64%), and 8
(22%) poor results.144 The main complications include stiffness, infection, and pain.
In rare cases of an isolated bullet or pellet in the elbow joint,
irrigation and débridement and bullet removal can be achieved with the
use of the arthroscope.80
elbow joint injury is open irrigation and débridement of the joint, and
removal of foreign material, bullet fragments, or small loose bone
fragments, if present. Initial stabilization of the elbow following a
fracture of the distal humerus, the proximal radius, or proximal ulna
can be done with a splint. With more comminuted fractures, use of
external fixation spanning the elbow can be utilized. After
stabilization, computed tomography (CT) will aid in assessment of the
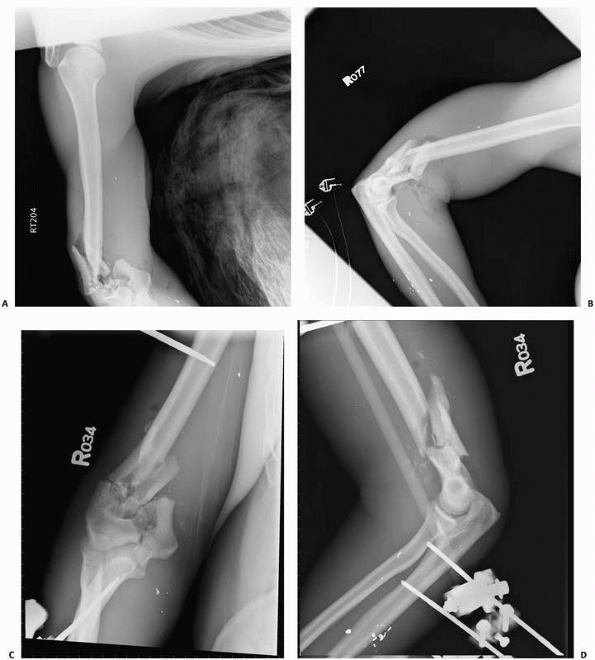
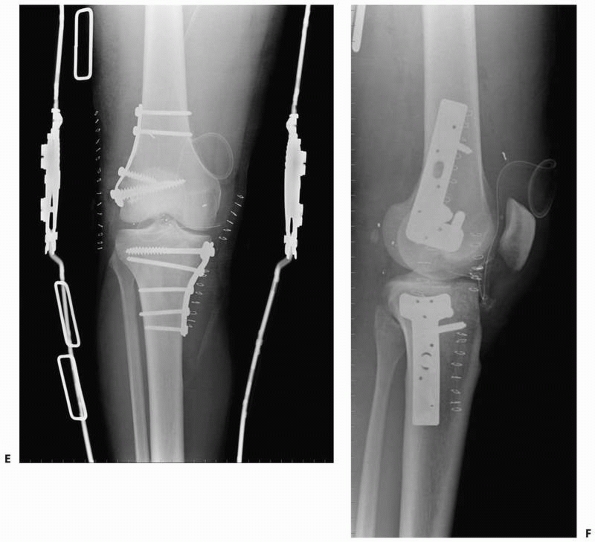
fracture and the elbow joint for definitive fracture fixation (Fig. 11-26A-D).
In unstable, open fracture-dislocations, urgent internal fixation of
the fractures may be necessary, alone or in addition to spanning
external fixation of the joint.18
various techniques, including internal fixation and/or hinged external
fixation (Fig. 11-26E-F). Salvage of a severely injured joint may be achieved with compression plate arthrodesis of the elbow102 or arthroplasty.31
Young and active patients are not good candidates for elbow
arthroplasty. In one study, intermediate-range follow-up of 8 to 12
years postarthroplasty showed a five of seven (71%) failure rate. In
the presence of an arthritic and painful elbow, this subgroup of
patients may be considered for arthrodesis.
In a cohort of 44 patients with elbow gunshot wounds at the author’s
institution, 4 died of other injuries and 6 were lost to follow-up. Of
the remaining 34 patients, 19 (56%) patients had nerve injuries. The
nerve injuries included 8 ulnar, 11 radial, and 2 median nerve
injuries. Two patients had combined injuries. Two nerves (one radial
and one ulnar) were repaired with partial return of function. Two
complete radial nerve injuries were treated with tendon transfers. Four
patients (12%) had brachial artery injury that required repair. Four
patients (12%) developed deep infections requiring irrigation and
débridement in the operating room. Three patients required secondary
bone grafting to achieve bony union of the fracture.
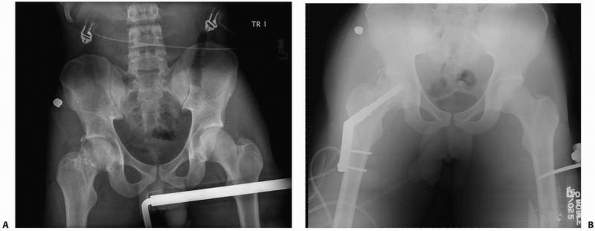
hip joint is about 2% of all extremity gunshot wounds and 4% of lower
extremity gunshot wounds. The prevalence of gunshot wounds to the hip
region (femoral neck, peritrochanteric region), with or without joint
involvement, with or without fractures is 9% of all extremity gunshot
wounds and 17% of lower extremity gunshot wounds.
step in management of these injuries. The trajectory of the bullet or
its fragments can traverse the abdomen, bowel, and/or bladder before
violating the hip joint. The projectile may enter the hip capsule
without causing a fracture of the acetabulum or the proximal femur, or
enter through the acetabulum. In absence of a fracture, the diagnosis
of hip joint violation can be difficult.
tomography scan findings. In the absence of fractures, or when
radiographs are inconclusive, a fluoroscopically assisted arthrogram is
the most sensitive test to detect joint violation.20,97
Documentation is important to determine the need for surgery to lavage
the joint. A negative arthrogram indicates no joint violation, possibly
allowing for nonoperative treatment.
high risk of infection and should be treated with emergent arthrotomy,
irrigation, and débridement. Bowel and bladder injuries should be
managed by general surgeons and urologists with either direct repair or
diverting colostomy and diversion procedures for the urinary tract
respectively.6,20,33
Hip arthroscopy requires special equipment and experience with the
technique. The use of a fracture table and fluoroscopy aid in
arthroscopy of the hip. Hip arthroscopy carries the risk of
intraabdominal fluid extravasation and abdominal compartment syndrome.6
In presence of acetabular fractures, extreme care must be taken to
measure the arthroscopy fluid inflow and outflow. If the inflow and
outflow are mismatched, fluid is likely extravasating into the pelvis
and abdomen and can cause cardiopulmonary arrest.
reduction and internal fixation. For acute fractures of the femoral
neck, use of standard techniques such as a compression screw and side
plate may be used for fractures with minimal comminution (Fig. 11-27). Comminuted fractures of the femoral neck may be treated by using fixed-angle devices such as a locking plate or blade plate.
surface of the femoral head or acetabulum are more difficult clinical
problems. Hip arthroplasty or arthrodesis in the acute setting is not
recommended.111,114
These procedures are reserved as elective salvage procedures. In the
presence of severe comminution when inadequate bone is available for
internal fixation, resection arthroplasty may be performed in the acute
setting. Complications of gunshot wounds to the hip include arthrosis,
infection, fistula formation,102,131 nonunion, malunion, and osteonecrosis.
femur and proximal tibia, are relatively frequent in all larger series
of gunshot wounds.† Perry et al.123
reported on 67 fractures to the knee: 37 sustained intra-articular
fractures and 27 sustained extra-articular fractures. There were 29
femoral, 29 tibial, and 9 patellar fractures. Twenty-three patients had
arteriograms for
suspected
vascular injury; of these, 6 arteriograms were positive. Five limbs
required vascular repair: one each of the common popliteal artery, a
branch of the common femoral artery, both the peroneal and posterior
tibial arteries, and the superficial femoral artery. Two patients had
common peroneal nerve injury. There were also two reported infections:
one superficial and one deep.
 |
|
FIGURE 11-26 Anteroposterior (A) and lateral (B) preoperative views of a distal humerus fracture that extends to the joint. C-F. An external fixator was applied and then converted to internal fixation after the swelling of the limb subsided. (continues)
|
 |
|
FIGURE 11-26 (Continued) The external fixator pins should be used outside the zone of injury.
|
absence of radiographic evidence of intra-articular debris, air, or
presence of fractures can be difficult. A saline arthrogram or dye
arthrogram can aid in diagnosis if the test is positive. However, these
tests have a low sensitivity of around 40% and a negative arthrogram
does not rule out an open joint injury.149
 |
|
FIGURE 11-27 Anteroposterior preoperative (A) and postoperative (B) radiographs of a femoral neck fracture sustained by an intra-articular bullet. Femoral neck fractures tend to be comminuted.
|
infection and stabilize the limb. In the presence of severely
comminuted and unstable fractures, spanning external fixation of the
joint is recommended. Delayed reconstruction of the joint may be
undertaken once the limb is stable. For larger fractures, an arthrotomy
should be used in treating major fractures with open reduction and
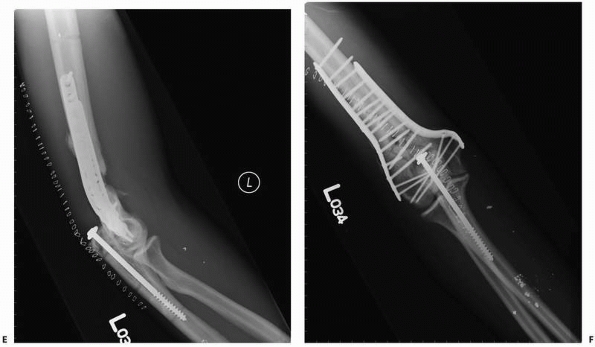
internal fixation (Fig. 11-28).
 |
|
FIGURE 11-28 Preoperative anteroposterior (A) and lateral (B) radiographs of a knee. C,D. Computed tomography scan shows the lateral femoral condyle fracture and proximal tibia fractures.
|
injuries, acute reconstruction of ligaments is not recommended. In
these cases, a delayed reconstruction after fracture healing and
rehabilitation may be undertaken. Meniscal tears and large
osteochondral fragments may be fixed acutely.
In a review of 33 gunshot wounds to the knee without radiographic
evidence of injury, arthroscopy showed 5 chondral injuries, 14 meniscal
injuries, and 5 knees with debris not seen on radiographs. Based on
these findings, diagnostic arthroscopy and arthroscopicassisted bullet
removal and irrigation and débridement are recommended for gunshot
wounds through the knee.
include fractures and nerve, vascular, and tendon injuries.159
Treatment is based on the personality of the fracture, ranging from
spanning external fixation and/or internal fixation for a low-velocity
injury. For patients with more severe soft tissue or bone injury,
arthrodesis or amputation should be considered. Arthroscopy is of
limited use because of the confined ankle space, good access through
incisions, and the prevalence of fracture necessitating open
debridement.
 |
|
FIGURE 11-28 (Continued) E,F. This patient was treated with open reduction and internal fixation of both fractures.
|
a significant clinical problem for orthopaedic surgeons in war or
peace. On the battlefield, caring for patients involves both
transportation and treatment. The evacuation of patients may involve
long distances, aircraft flight, and delayed definitive care. Initial
treatment of gunshot fractures in this setting involves temporary
stabilization with subsequent evacuation, followed by definitive
fixation once the patient arrives in a stable hospital environment.
Temporary stabilization involves the use of an external fixator to span
the fracture segment.
and cared for at the same institution without the complexity of patient
transportation through multiple echelons of care. Because of this,
immediate definitive stabilization for patients with isolated long bone
gunshot fractures has become a more common treatment method.
than lower extremity long bone fractures, with gunshot diaphyseal
humerus fractures generally being the third most common shaft fracture.
Complication such as nerve injuries59,117,136
are relatively common with patients who sustain gunshot wounds of the
humerus. There is an increased prevalence nerve injury associated with
the distal humerus compared with more proximal injuries.*
controversial. Reported methods of care include fracture brace,
external fixation, and internal fixation. There are no prospective
studies comparing the various methods of treatment for patients with
gunshot wounds.†
when there is minimal soft tissue injury and the fracture can be held
in alignment by this means. Proximal or very distal fractures are often
not amenable to this method of care.4,130,131
with more extensive injuries, such as with military wounds. Zinman et
al.161 reported on 26 Israeli war
casualties who had external fixation applied for treatment of open
humerus fractures. They applied monolateral external fixators to obtain
union in 15 patients
(57.7%).
Conversion to compression plates (five patients) or a cast (six
patients) was used for the other patients. Five delayed unions were
identified, four of which were treated with plating and bone grafting.
Fifteen patients had a total of 20 nerve injuries. One of the nerve
injuries was caused by a distal, lateral pin placement that injured the
radial nerve. There were four brachial and two radial artery repairs. A
total of 23 patients had 6.5 years of follow-up after injury. The
authors reported excellent results in 14 patients, good results in 4,
fair results in 3, and poor results in 2. All fractures did eventually
heal. They believed that external fixation was the best means for
stabilizing fracture and allowing access to wounds for wound care. For
the distal humerus, the authors recommended open pin placement if
lateral pins are to be used or placing the pins from a posterior
direction. They recommended this as a treatment for patients with
severe open injuries secondary to war wounds.
studied 37 patients who were treated at a Red Cross Hospital on the
Sudanese border. Patients were seen an average of 9.5 days after
injury, at which time 89% of the wounds were found to be infected.
Nerve palsy secondary to injury was present in eight patients in this
series. They were treated with external fixation, traction, and a
plaster of Paris splint. Twenty-three patients received a functional
brace with plaster of Paris and splint, and seven patients received
external fixation skeletal traction. Those treated with the splint had
an average time of immobilization of 35.8 days, and 90% obtained
adequate alignment. The authors also reported eight reoperations on
four patients. The seven patients treated with external fixation had
the frame applied for an average of 46.3 days, and 60% obtained
adequate angulation. The authors also reported a 71.5% nonunion rate
and 11 reoperations in five of the patients. Traction was used in seven
patients as well, with an average immobilization of 27.7 days, with
five patients obtaining union, and six reoperations on three of the
patients. Although the best results were obtained in patients who were
treated with splinting, the authors reported that those who had
external fixation and traction had the more severe injuries.
treated 89 humerus fractures with Ender nails, of which 22 were caused
by gunshot wounds (4 shotgun wounds). The authors reported good results
with these patients using this technique. We know of no reports using
Ender nails since this 1987 report. This technique has been overtaken
by conventional intramedullary nailing as for other trauma indications.
disruption, use of a functional brace following a coaptation splint
seems to yield acceptable results for both initial and definitive care.4,130,131
For patients with more extensive injuries, such as a shotgun blast at
close range, we recommend the use of a spanning external fixator to
provide initial stabilization for the patient.82,87,154,161
Use of the spanning external fixator is more common with distal
fractures. When both the limb and the patient have become stable,
planning for fracture stabilization and soft tissue coverage can be
done.
defects may be challenging. With extensive comminution and soft tissue
injury, use of a small pin fixator has been reported with good success.3,140 For skeletal defects, use of a cage with allograft3 or a fibular osteoseptocutaneous flap71 has been described.
There is a high reported rate of nerve injury associated with gunshot
wounds to this region, and a 10% rate of compartment syndrome.38,60,108
The goals of fracture care are to restore the length, alignment and bow
of the forearm. Care for diaphyseal forearm fractures depends on the
severity of the both the soft tissue and bone injury, just as with open
forearm fractures not associated with firearms.* Patients
with relatively stable fractures of the ulna and associated minimal
soft tissue trauma may be treated by application of a cast after
appropriate wound treatment. Displaced fractures should be treated with
open reduction and internal fixation when soft tissues permit.
If just the radius or ulna is involved, only splinting may be required.
Use of a soft tissue antibiotic-impregnated spacer may be used for
initial care of the void.53 A
second, staged procedure to reconstruct bone defects should then be
done once the limb is stable. Use of autologous bone graft has been
described to fill defects. Use of allograft and bioactive substances,
such as bone morphogenetic protein (BMP) or demineralized bone matrix,
has yet to be described.
Initial stabilization with this traction is commonly used today as a
temporary means of stabilization until more definitive care can be
provided.155
reported on 19 femur fractures that were intended to be treated with
external fixation to union. Six were converted to cast brace because of
pin track infection, and a further five femurs underwent open reduction
internal fixation (one for refracture). Fourteen of the femurs were
treated with bone grafting. The authors noted that further procedures
were not done until the limb was free of obvious infection. Average
time to union was 19 weeks.
The concept of using temporary external fixation as a bridge from
injury to definitive fracture stabilization has become a popular means
to initially stabilize a patient’s fracture.
fractures or malunion, nonunion, and infection associated with gunshot
wounds in the United States began after World War II.19,25
reviewed 26 patients who sustained fractures because of “low-velocity”
gunshot wounds and were treated with intramedullary nailing an average
of 9 days after injury. Nineteen of the patients were followed to
union, which occurred at an average of 4.5 months after injury. Two
patients had open nailing and the remaining 17 had closed nailing.
reviewed a series of 65 patients with gunshot femur fractures at Kings
County Hospital Center in Brooklyn, New York. The patients were treated
with reamed intramedullary nailing an average of 2 days (range, 0-14
days) after injury and were followed an average of 2 years after injury
(range, 9.5 months to 6 years). The authors found all fractures healed
an average of 18 weeks (range, 13-31 weeks). Two patients had
persistent drainage, which resolved with a course of oral antibiotics
at 2 and 3 weeks.
reviewed 38 of 55 patients with gunshot femur fractures treated with
intramedullary nailing who were followed an average of 2 years (range,
14-36 months). Average time to union was 8.6 weeks (range, 5-22 weeks).
Nicholas and McCoy113 reviewed 12
patients with 14 femur fractures treated with immediate (within 8
hours) intramedullary nailing. Three patients had vascular repairs and
two patients had sciatic nerve injuries. Average time to union was 5.5
months (range, 3-8 months). None of the patients had an infection.
performed a retrospective review of 77 patients who sustained gunshot
femur fractures, of which 56 had adequate records for follow-up. The
patients were initially treated with skeletal traction for 10 to 14
days, with intramedullary nailing done when the wound tracks healed. No
deep wound infections were reported. Average time to union was 23 weeks
(range, 14-40 weeks), and average follow-up was 16 months (range, 12-29
months). Five patients had limb length discrepancy of greater than 1
cm, and one patient had angulation of 15 degrees.
may be safely used for gunshot-induced diaphyseal femur fractures. This
procedure may be done immediately or on a delayed basis, depending on
the patient’s condition and the degree of soft tissue injury. More
proximal fractures, such as subtrochanteric fractures, may do best with
using reconstruction nails to obtain more proximal fracture
stabilization (Fig. 11-29).
caring for diaphyseal femur fractures, particularly those near the
knee. Initially, it was believed that an open fracture would be too
great of a risk for knee sepsis to permit using retrograde nails. Our
group recently reported on our series of 196 gunshot femur fractures,
of which 56 were treated with retrograde nailing (Fig. 11-30).
There was no increased infection rate associated with this method of
treatment, at either the fracture site or the knee joint. Therefore,
use of retrograde nailing for diaphyseal gunshot femur fractures
appears to be safe.
reported 5 of 56 patients requiring vascular repair in addition to the
treatment of the femur fracture. He also reported three associated
sciatic nerve injuries, one with return, one with partial return, and
one with no return to function. Two patients had peroneal nerve
palsies, one with return to function. Infection of patients is
infrequent in the nonmilitary setting with gunshot femur fractures.
Wiss et al.155 reported no deep infections with 56 patients at follow-up. Holloman and Horowitz75 reported no patients with infection after intramedullary nailing. Bergman et al.10 reported two patients with persistent drainage, and Nicolas and McCoy113 reported that none of their 14 patients with immediate nailing were infected.
femoral shaft fractures. We found the 3 of 102 patients treated for
diaphyseal gunshot wounds from 2001 through 2006 at Henry Ford Hospital
had the diagnosis of thigh compartment syndrome.
reported angulation deformity of 15 degrees for one of 56 patients,
rotational deformity reported in one patient, and five patients with a
leg length discrepancy of greater than 1 cm.
hospitals that treat nonmilitary gunshot wounds on a routine basis.
Intramedullary nailing allows for better alignment, less limb length
discrepancy, and earlier return to ambulation without an increased rate
of infection. The use of temporary external fixation to initially care
for patients with more extensive wounds or other severe injuries allows
for the patient to be stabilized before undergoing more extensive
surgery. Skeletal traction is an option for the short term
stabilization of a fracture before more definitive care.
Afghanistan conflicts has been with the staged management of care. For
U.S. or Allied soldiers, the fracture is stabilized with an external
fixator and the patient transported to a site of definitive care,
usually in the Continental United States. Once at a site of definitive
care, treatment of the bone by intramedullary nailing may be done if
the limb is free of infection and has good soft tissue coverage.
A variety of treatment methods have been reported for fracture care,
including the use of cast or fracture brace, external fixation, and
intramedullary nailing.
reported on the ambulatory treatment in a cast and then fracture brace
of 84 patients who sustained tibia fractures secondary to missile
injuries. All of the fractures in this series had some comminution.
Despite this, the authors reported less than 1 cm of shortening on 48
of 58 patients with isolated injury and an additional three patients
with 1 cm of shortening. Seven patients were reported to have
osteomyelitis, which prolonged the time to union. Brown and Urban22
reported on 63 fractures in 60 patients who were also injured by war
wounds and were treated in a similar manner. The fractures in this
series healed at an average of 19 weeks. Shortening averaged 9 mm,
ranging from 2 to 38 mm, compared with the contralateral limb.
Twenty-seven of the fractures had no shortening. Four of the 63
patients had persistent drainage. Sarmiento reported on 32 tibia
fractures caused by gunshot wounds treated with a fracture brace. The
average time to union was 17.5 weeks, with one nonunion.
conducted a retrospective review of 40 patients with 41 tibia fractures
caused by gunshot wounds. Thirty-five fractures were treated by casting
followed by fracture brace. An additional five fractures were treated
with external fixation because of injury severity, followed by
functional brace within the first 2 months. One patient had pins and
plaster. Those treated by casting healed at an average of 12 weeks,
whereas those treated by external fixation healed at an average of 21
weeks. Eight patients had persistent wound drainage, with two
undergoing a surgical procedure to care for the wound.
This
study was limited in that it reported follow-up of only 27% of the
total number of patients seen with this diagnosis at the institution.
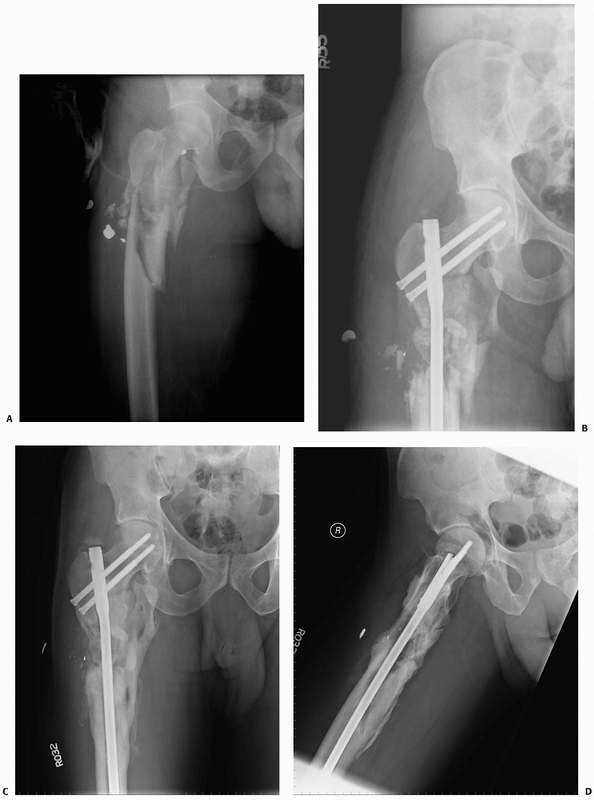 |
|
FIGURE 11-29 Anteroposterior preoperative (A) and postoperative (B-D)
views of a subtrochanteric fracture. The patient was treated with a reconstruction nail and had good callus formation in the zone of injury at 6 months. The periosteal sleeve, if left relatively undisturbed, will allow for bone formation. |
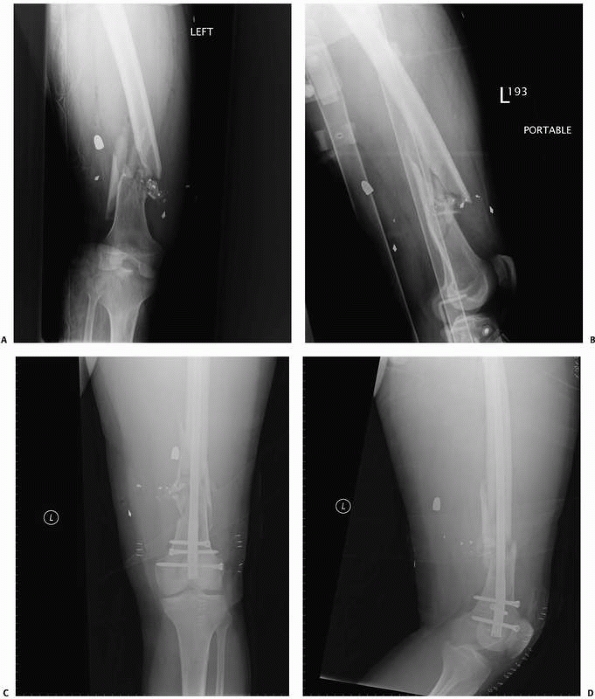 |
|
FIGURE 11-30 Preoperative (A,B) and postoperative (C,D) radiographs of a distal femur fracture. The patient was treated with an immediate retrograde intramedullary nail.
|
reported a retrospective review of 90 of 133 patients with tibia
fractures caused by gunshot wounds treated at Harbor/UCLA medical
Center. Fracture stabilization was a long leg cast for 58, external
fixation for 17, and unreamed intramedullary nailing for 15 patients.
The authors found that fractures classified as Winquist 0, 1, or 2
healed within 12 to 14 weeks and those with Winquist 3, 4, or 5 and
treated with intramedullary nailing healed at an average of 18 weeks;
those treated with external fixation averaged 27 weeks to union.
shaft depends on the amount of bone comminution and degree of soft
tissue injury. Patients with tibia shaft fractures having minimal
comminution, soft tissue injury, displacement, and angulation may be
successfully treated with local wound care in the emergency department
and application of a cast, followed by a functional brace. More
comminuted fractures are better cared for with intramedullary nailing.
If there is major soft tissue injury requiring a soft tissue transfer,
consideration should be given to external fixation until the soft
tissues are reconstructed, at which point the fixator may be removed
and an intramedullary nail is inserted.
gunshot wounds. The anatomic location of foot and ankle was 39 of 2277
(1.7%) of all gunshot injuries in 1505 patients seen at Henry Ford
Hospital between 2001 and 2006. Gunshot toe and metatarsal injuries
vary in the degree of both soft tissue and bone injury. Minimally
displaced fractures, particularly when an isolated injury, may be
treated without surgical stabilization. After treatment of the soft
tissues, a period of using a hardsoled postoperative shoe with dressing
changes allows for a good result.
with bone loss are candidates for surgical stabilization. Kirschner
wires or external fixation may be used for initial surgical
stabilization with these patients.16,152
metatarsal injuries and as a consequence require surgical
stabilization. For acute injuries with bone loss, external fixation to
span the area, followed by reconstruction of the bone with plates when
the limb is stable, is used. Talus and calcaneus fractures are less
likely to require surgical stabilization unless bone loss is present.
Treatment for isolated fractures should be dependent on the degree of
bone and soft tissue injury. With minimal soft tissue and bone
disruption, treatment of the soft tissues followed by casting gives the
best results. Infection is more common with foot injuries than other
anatomic regions. Boucree reported that 12 of 101 patients with gunshot
foot wounds had an infection; this is a higher incidence than reported
with other anatomic regions.16
reported that 250 of 1860 war casualties (13.4%) treated at the
authors’ facility in the former Republic of Yugoslavia had foot
injuries. Amputations were performed in 76 (26.5%) of the feet.
vehicles struck by a large mine. This “behind armor blunt trauma” is
similar to injuries seen with severe motor vehicle accidents and may be
treated with the same definitive care.112
war and peace. Caring for patients in war-torn regions of the world
remains challenging. Patients are often initially managed under austere
circumstances before and during transport for definitive care. Gunshot
injuries are a significant part of the health care problem for some
inner-city hospitals around the world. The orthopaedic surgeon should
be knowledgeable about the clinical course and outcome of patients with
gunshot wounds to provide the best care within the context of his or
her medical system.
(GlobalSecurity.org). Improvised explosive devices/booby traps.
Available at: http://www.globalsecurity.org/military/intro/ied.htm.
Accessed May 6, 2008.
N, Lehman R, Bodell L, et al. Surgical management of a long segmental
defect of the humerus using a cylindrical titanium mesh cage and
plates: a case report. J Orthop Trauma 2005;19:211-216.
GW, Marrero CE. Fracture brace for the treatment of humerus shaft
fractures caused by gunshot wounds. Orthop Clin North Am 1995;26:55-63.
A. Wounds of joints. In: Burkhalter WE, ed. Surgery in Vietnam,
Orthopaedic Surgery. Washington, DC: Center for Military History;
1994:107-130.
CS, DiFelice GS, Buly RL, et al. Cardiac arrest as a result of
intraabdominal extravasation of fluid during arthroscopic removal of a
loose body from the hip joint of a patient with an acetabular fracture.
J Orthop Trauma 1998;12:294-299.
RF, Zajtchuk R. Assessing the effectiveness of conventional weapons.
In: Zajtchuk R, ed. Conventional Warfare: Ballistic Blast and Burn
Injuries. Washington, DC: Office of the Surgeon General; 1991:53-82.
RF, Zajtchuk R. The weapons of conventional land warfare. In: Zajtchuk
R, ed. Conventional Warfare: Ballistic Blast and Burn Injuries.
Washington, DC: Office of the Surgeon General; 1991:1-52.
RF. Combat trauma overview. In: Anesthesia and Perioperative Care of
the Combat Casualty. Washington, DC: Office of the Surgeon General;
1995:1-42.
M, Tornetta P, Kerina M, et al. Femur fractures caused by gunshots:
treatment by immediate reamed intramedullary nailing. J Trauma
1993;34:783-785.
JC, Arima JK, Johnson DW. Enemy ordnance material. In: Beyer JC, ed.
Wound Ballistics. Washington, DC: Office of the Surgeon General;
1962:1-90.
JC, Enos WF, Holmes RH. Personal protective armor. In: Beyer JC, ed.
Wound Ballistics. Washington, DC: Office of the Surgeon General;
1962:641-689.
A, Vigorita VJ, Meyerson RI, et al. Intra-articular histologic changes
secondary to local lead intoxication in rabbit knee joints. J Trauma
1995;38:688-671.
EA. Further evaluation of the use of intramedullary nailing in the
treatment of gunshot fractures of the extremities. J Bone Joint Surg Am
1957;39A:513-520.
EW, Brien WW, Long WT, et al. Concomitant injuries of the hip joint and
abdomen resulting from gunshot wounds. Orthopaedics 1992;15:1317-1319.
TD, et al. The impact of gunshot wounds on an orthopaedic surgical
service in an urban trauma center. J Orthop Trauma 1997;11:149-153.
A, Curran P. Necessity breeds invention: a study of outpatient
management of low-velocity gunshot wounds. Emerg Med J 2006;23:376-378.
CR, Turnispeed D. Experiences with intramedullary fixation of compound
femoral fractures in war wounds. J Bone Joint Surg Am 1953;35A:153-171.
for Disease Control and Prevention. WISQARS fatal injuries: mortality
reports. Available at:
http://webappa.cdc.gov/sasweb/ncipc/mortrate.html. Accessed January 18,
2008.
JR, Heley MB, Agel J, et al. Randomized prospective study of humeral
shaft fracture fixation: intramedullary nails versus plates. J Orthop
Trauma 2000;14: 162-166.
B, Komurcu M, Ozturk C, et al. Total elbow arthroplasty in patients who
have elbow fractures by gunshot injuries: 8- to 12-year-follow-up
study. Arch Orthop Trauma Surg 2008;128:17-24.
PJ, Hetz SP, Fackler ML. Weapons and weapons effects. In: Lounsbury DE,
ed. Emergency War Surgery Handbook. 4th Am. Ed. Washington, DC: Office
of the Surgeon General; 2004.
AJ, Mendelson JA, Lindsey D. Comparison of the wounding characteristics
of some commonly encountered bullets. J Trauma 1961;1:341-353.
JA, Pankovich AM, Egwele R. Extra-articular low-velocity gunshot
fractures of the radius and ulna. J Bone Joint Surg Am 1978;60A:335-341.
ML, Dougherty PJ. Theodor Kocher and the scientific foundation of wound
ballistics. Surg Gynecol Obstet 1991;172:153-160.
ML. Missile-caused wounds. In: Bowen TF, Bellamy RF, eds. Emergency War
Surgery. 2nd Am. Rev. Washington, DC: Office of the Surgeon General,
Department of the Army; 1988:13-34.
ML, Bellamy RF, Malinowski JA. A reconsideration of the wounding
mechanism of very high-velocity projectiles: importance of projectile
shape. J Trauma 1988;28: S63-S67.
ML, Breteau JPL, Courbil LJ, et al. Open wound drainage versus wound
excision in treating the modern assault rifle wound. Surgery 1989;105:
576-584.
LK, Brown RB, Nicholson JT, et al. Observations on the treatment of
battle wounds aboard a hospital ship. US Nav Med Bull 1943;41:299-305.
GM, DeSilva SP. Reconstruction of skeletal defects in the forearm after
trauma: treatment with cement spacer and delayed cancellous bone
grafting. J Trauma 1995;38:910-914.
A, Minkoff J, Price A, et al. A posterior arthroscopic approach to
bullet extraction from the hip. J Trauma 1987;27:1294-1300.
KE, Annest JL, Mercy JA, et al. Surveillance for fatal and nonfatal
firearm-related injuries: United States, 1993-1998. Morb Mortal Wkly
Rep MMWR 2001;50(SS02): 1-31.
H, Korr IM, McMillen JH, et al. Ballistics of the Penetration of Human
Skin by Small Spheres. Office of Scientific Research and Development;
July 6, 1945. Missile Casualty Report No. 11.
H. Penetration of Steel Spheres Into Bone. Interim report. Office of
Scientific Research and Development; July 20, 1945. Missile Casualty
Report No. 10.
Y, Chiou-Tan F. Radial nerve injuries from gunshot wounds and other
trauma: comparison of electrodiagnostic findings. Am J Phys Med Rehabil
2002;81:207-211.
OP. The management of penetrating wounds and suppurative arthritis of
the knee joint in the Mediterranean theater of operations. J Bone Joint
Surg 1946;28: 659-680.
OP. The indications for debridement of gunshot (bullet) wounds of the
extremities in civilian practice. J Trauma 1961;1:368-372.
KK, Weaver LD, Todd AO, et al. Efficacy of ceftriaxone versus cefazolin
in the prophylactic management of extra-articular cortical violation of
bone due to low-velocity gunshot wounds. Orthop Clin North Am
1995;26:9-17.
EN. Studies on wound ballistics. In: Andrus EC, Keefer CS, et al., eds.
Advances in Military Medicine, vol 1. Boston: Little, Brown, and Co;
1948:191-205.
EN, Korr IM, Oster G, et al. Secondary damage in wounding due to
pressure changes accompanying the passage of high-velocity missiles.
Surgery 1946;21: 218-239.
EN. McMillen JH, Butler EG, et al. Mechanism of Wounding. In: Beyer JC,
ed. Wound Ballistics. Washington, DC: Office of the Surgeon General;
1962:143-235.
C, Erdmann D, Levin LS. Treatment of segmental defects of the humerus
with an osteoseptocutaneous fibular transplant. J Bone Jt Surg
2002;84A:2216-2223.
MJ, Banks HH, Leach RB, et al. Extremity gunshot wound and gunshot
fracture in civilian practice. Clin Orthop Rel Res 1976;114:296-303.
CM, Coe GB, Beyer JC. Wound ballistics and body armor in Korea. In:
Beyer JC, ed. Wound Ballistics. Washington, DC: Office of the Surgeon
General; 1962:691-767.
J, Weir R, Dougherty P, et al. Gunshot wounds of femoral shafts in
urban populations: is emergent retrograde intramedullary nailing
appropriate? Presented at the Orthopaedic Trauma Association Annual
Meeting, Phoenix, AZ, October 2006.
MW, Horowitz M. Femoral fractures secondary- to low-velocity missiles:
treatment with delayed intramedullary fixation. J Orthop Trauma
1990;4:64-69.
DF, Harger JH, Buege LJ, et al. An experimental study in
bio-ballistics: femoral fractures produced by projectiles, II: shaft
impacts. J Biomech 1968;1:313-321.
TP, Patzakis MJ, Lee J, et al. Comparison of intravenous and oral
antibiotic therapy in the treatment of fractures caused by low-velocity
gunshots. J Bone Joint Surg Am 1996;78A:1167-1171.
M, Yanmiş I, Ateşalp AS, et al. Treatment results for open comminuted
distal humerus fractures with Ilizarov external fixator. Milit Med
2003;168:694-697.
BE, Rasmussen TE, Smith DL, et al. Experience with wound VAC and
delayed primary closure of contaminated soft tissue injuries in Iraq. J
Trauma 2006;61: 1207-1211.
MR, Brien WW, Gellman H, et al. Fractures of the forearm resulting from
low-velocity gunshot wounds. J Orthop Trauma 1992;6:32-35.
MA, Manton WI, Stewart RM, et al. Lead poisoning from retained bullets:
pathogenesis, diagnosis, and management. Ann Surg 1982;195: 305-313.
RB, Wetzler TF, Marshall JD, et al. The bacterial flora of battle
wounds at the time of primary debridement. Ann Surg 1955;141:369-374.
AG. The Medical Department of the United States in the World War.
Volume XV, Statistics. Washington, DC: Office of the Surgeon General;
1925:1019.
JA, Burkhalter WE, Ouellette EA, et al. Compression plate arthrodesis
of the elbow. J Bone Joint Surg Br 1992;74B:300-304.
NJ, Thiel B, Ninomiya JT. Retrieval of an intact, intra-articular
bullet by hip arthroscopy using the lateral approach. J Orthop Trauma
2002;16:51-53.
L, Yu-Yuan M, Rong-Xiang F, et al. The characteristics of the pressure
waves generated in the soft target by impact and its contribution to
indirect bone fractures. J Trauma 1988;28:S104-S109.
DM, Bumbasirevic MZ, Senohradski KK, et al. Pelvifemoral external
fixation for the treatment of open fractures caused by gunshot wounds.
Acad Orthop Belg 2002; 58:37-41.
S, Seery W, Borshuk S, et al. Septic arthritis secondary to
vesico-acetabular fistula: a case report. J Urol 1976;116:116-117.
EA, Gritsanov AI, Fomin NF, et al. Mine blast trauma. Experience from
the war in Afghanistan (Khlunovskaya GP, translator). Stockholm,
Sweden: Falths Tryckeri; 1995.
PJ, Turen Ch, Brumback RJ, et al. Conversion of external fixation to
intramedullary nailing for fractures of the shaft of the femur in
multiply injured patients. J. Bone Joint Surg Am 2000;82A:781-788.
F, Cuartas E. Arthroscopic removal of bullet fragments from the
subacromial space of the shoulder joint. Arthroscopy 2004;20:754-756.
AW, Hull HC, Sutherland FA, et al. Study on wound ballistics:
Bougainville campaign. In: Beyer JC, ed. Wound Ballistics. Washington,
DC: Office of the Surgeon General, Department of the Army; 1962:281-436.
SJ, Esformes I. The role of arthroscopy in management of low-velocity
gunshot wounds to the knee joint. Clin Orthop Rel Res 1984;185:207-213.
MJ, Harvey JP, Ivler D. The role of antibiotics in the management of
open fractures. J Bone Joint Surg Am 1974;56A:532-541.
W, Beske C, Stein V, et al. Arthroscopic removal of a projectile from
the intraarticular cavity of the knee joint. Arch Orthop Trauma Surg
2002;122:235-236.
ND, Zinman C, Besser MIB, et al. A philosophy of limb salvage in war:
use of the fixateur externe. Milit Med 1991;156:505-520.
SC, Fujisaki CK, Moore EE. Incomplete fractures associated with
penetrating trauma: etiology, appearance, and natural history. J Trauma
1988;28:106-109.
A, Zagorski JB, Zych GA, et al. Functional bracing for the treatment of
fractures of the humeral diaphysis. J Bone Joint Surg Am
2000;82A:478-486.
TM, Boswell SA, Scott JD, et al. External fixation as a bridge to
intramedullary nailing for patients with multiple injuries and with
femur fractures: damage control orthopaedics. J Trauma 2000;48:613-623.
SJA, Vuletin JC, Twersky J. Lead arthropathy: arthritis caused by
retained intraarticular bullets. Radiology 1985;156:299-302.
RE, Artiz CP, Sako Y. An evaluation of the surgeon’s criteria for
determining the viability of muscle during debridement. Arch Surg
1956;72:1031-1035.
YC, Harwood P, Grotz MR, et al. Radial nerve palsy associated with
fractures of the shaft of the humerus: a systematic review. J Bone
Joint Surg Br 2005;87B: 1647-1652.
E, Raz R, Stein H, et al. Risk factors for infection in fracture war
wounds (1973 and 1982 Wars, Israel). Milit Med 1991;156:520-527.
DL, Hale DM, Buggay D, et al. Use of a hybrid external fixator for a
severely comminuted juxta-articular fracture of the distal humerus. J
Orthop Trauma 1998;12: 449-442.
JS, Strauss E. Gunshot wounds to the upper extremity. Evaluation and
management of vascular injuries. Orthop Clin North Am 1995;26:29-36.
MA, Schmietd I, Tomlinson DP. Hip arthroscopy: a unique inferomedial
approach to bullet removal. Arthroscopy 2002;18:1-3.
P, Tiburzi D. Anterograde interlocked nailing of distal femoral
fractures after gunshot wounds. J Orthop Trauma 1994;8:220-227.
P III, Boes MT, Schepsis AA, et al. How effective is a saline
arthrogram for wounds around the knee? Clin Orthop 2008;466:432-435.
CH, Burgess AR, Vanco B. Skeletal stabilization for tibial fractures
associated with acute compartment syndrome. Clin Orthop
1995;315:163-168.
C, McLaughlin B, Law C, et al. Through-and-through gunshot wounds to
the foot: the “Fearless Fosdick” injury. Ann Plast Surg 2005;55:474-478.
LD, et al. Gunshot wound injuries: frequency and cost analysis in south
central Los Angeles. Orthop Clin North Am 1995;26:1-7.
TF, Radziejowski MJ. Gunshot fractures of the humeral shaft treated
with external fixation. J Orthop Trauma 1996;10:273-278.
DA, Brien WW, Becker V. Interlocking nailing for the treatment of
femoral fractures due to gunshot wounds. J Bone Joint Surg Am
1991;73A:598-606.
CO, Atesalp AS, Demiralp B, et al. High-velocity gunshot wounds of the
tibial plafond managed with Ilizarov external fixation. J Orthop Trauma
2003;17:421-429.
C, Norman D, Hamoud K, et al. External fixation for severe open
fractures of the humerus caused by missiles. J Orthop Trauma
1997;11:536-539.
