Congenital Deformity
embryologic vertebral development that can lead to severe malalignment
of the trunk, depending on the type and location of defect in the
spine. These deformities can be more difficult to treat than idiopathic
curves owing to the frequency of associated medical problems, their
presence in extremely young patients, and increased curve rigidity. The
most likely times of increasing deformity match the phases of normally
rapid spinal growth (first 2 to 3 years and during adolescence).
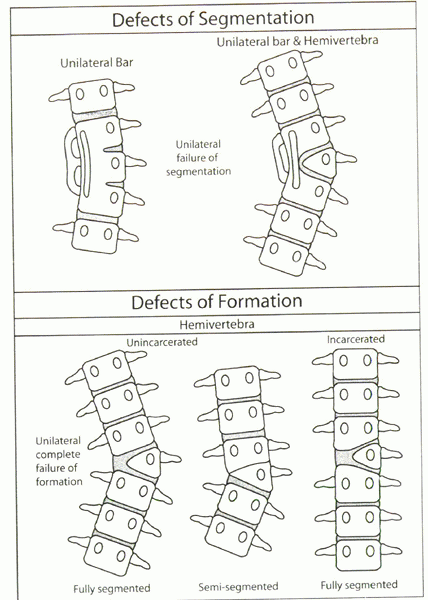
two basic types of malformations based on the development of the
vertebral elements:
-
Defects of formation
-
Defects of segmentation
mixture of deformities at different levels in the spine. This chapter
focuses on congenital scoliosis and kyphosis.
caused by developmental vertebral anomalies that produce deviations in
spinal alignment. These deficiencies occur in the first trimester of
intrauterine development and commonly are associated with cardiac and
urologic abnormalities that develop during the same period. The
vertebral anomalies are present at birth, but the clinical deformity
may not become evident until later as the child grows, classifying it
as congenital scoliosis. This condition should not be confused with
infantile idiopathic scoliosis, in which the scoliosis also develops
early in life, yet all the vertebral elements are normal in shape. The
etiology is unknown in humans; however, in animal studies, congenital
scoliosis has occurred after exposure to toxic elements during the
fetal period.
true incidence in the population is unknown because only some patients
progress to warrant an investigation and a subsequent radiograph.
Wynne-Davies analyzed the families of 337 patients with congenital
spinal anomalies. She showed that isolated hemivertebrae or similar
localized defects were sporadic events that carried no risk to
subsequent siblings. In patients with multiple anomalies, however,
there is a 5% to 10% risk that siblings also will be affected. The
Minneapolis group found 1% of patients with congenital spinal deformity
had a relative with the problem.
-
Failures of vertebral formation (type I)
-
Failures of segmentation between the vertebrae (type II)
-
Types I and II combined (type III or mixed)
right side of the body or involve the anterior or posterior elements,
resulting in scoliosis or kyphosis/lordosis. Combined defects are
common, so coronal and sagittal planes need to be evaluated.
formation (type I). These triangular-shaped vertebrae form only on one
side of the spine and can be subclassified as follows:
-
Vertebrae that have disc and growth potential on the superior and inferior ends of the vertebra—fully segmented
-
Vertebrae that have disc and growth potential on either the superior or the inferior end only—semisegmented
-
Vertebrae that are fused to the vertebrae above and below—nonsegmented
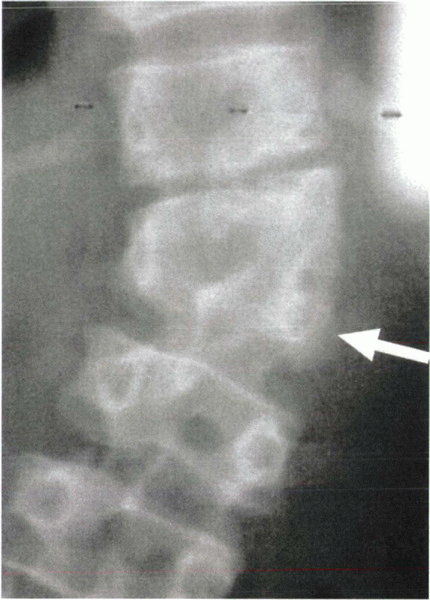
progressive scoliosis with the risk and rate of progression greatest
for the fully segmented hemivertebrae and least for the nonsegmented
hemivertebrae. Hemivertebrae are said to be incarcerated when they lie within the confines of the curve and vertebral column or unincarcerated when they extend laterally beyond the contour of the adjacent vertebrae (Fig. 19-2).
Of the various types of hemivertebrae, the fully segmented
unincarcerated hemivertebra has the greatest potential for progression
with growth. Rib deficiencies tend to match the vertebral deficiencies,
and a mismatch of the number of ribs (right versus left) should lead to
suspicion for congenital anomalies. The term hemimetameric shift
defines two hemivertebrae that are present on opposite sides of the
spine and separated by at least one normal vertebra. In this case,
global balance of the spine in the coronal plane often is maintained.
 |
|
Figure 19-1
Diagrammatic representation of classification system of congenital scoliosis. (Modified from McMaster MJ. Congenital scoliosis. In: Weinstein SL, ed. The pediatric spine: principles and practice, 2nd ed. Lippincott Williams and Wilkins, Philadelphia, 2001, Chapter 7, p. 163.) |
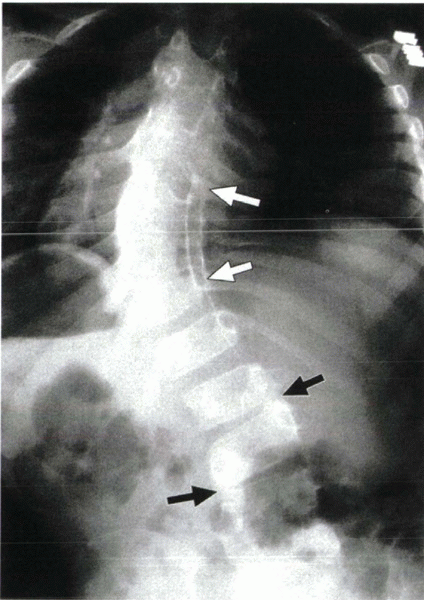
both sides of the spine, causing a bar of bone bridging the disc
spaces, the pedicles, or the facet joints. These anomalies inhibit
longitudinal growth and result in little deformity if they occur
circumferentially around the spine (block vertebra). A unilateral
unsegmented bar causes a growth tether that generally results in marked
scoliosis (Fig. 19-3). Unilateral unsegmented
bars are seen most commonly in the thoracic spine. Radiographically a
failure of segmentation often is seen best as conjoined pedicles or
ribs, or both.
The radiographs of a mixed congenital malformation may be difficult to
interpret fully. A newborn or infant radiograph (if available) is often
the most useful for identifying the malformations.
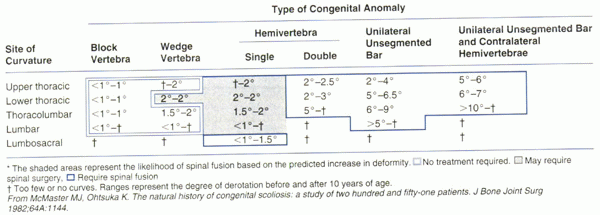
scoliosis developing a progressive deformity is difficult to know.
There are features, however, of the malformation that allow educated
predictions. McMaster and Ohtsuka studied the natural history of 251
patients followed past age 10 without treatment. Three fourths of the
patients’ curves progressed substantially, and this progression seems
related to curve location and type of anomaly. The annual rates of
curve progression for each of the congenital anomalies are presented in
Table 19-1.
(<1 degree per year), whereas hemivertebrae with a contralateral
unsegmented bar progress the most (>10 degrees per year). Deformities of the
thoracic spine are in general at greater risk for progression than deformities in the lumbar spine.
 |
|
Figure 19-2 Radiograph showing a semisegmented hemivertebra (arrow).
|
 |
|
Figure 19-3 Radiograph shows a typical bar with fused pedicles (white arrows). Black arrows show narrowing of the disc spaces, also suggesting bar formation.
|
history, developmental milestones, family history, and complete review
of systems. Of patients with congenital spinal malformations, 33% have
genitourinary abnormalities, 25% have Klippel-Feil syndrome (cervical
vertebral fusion), 15% have intraspinal anomalies (diastematomyelia,
tethered cord), and 10% have congenital heart disease. Given the
frequency of these associated lesions, the history and exam should
include these areas.
shape and neurologic function. The effect of the spinal malformation on
the trunk may be visible as a shift of the head or trunk off midline, a
rotational prominence of the ribs, or a sagittal plane deformity such
as kyphosis. Specific findings that suggest an intraspinal lesion
include skin lesions on the back (e.g., hairy patches, dimples, masses,
nevi, lipomas) and lower extremity abnormalities (e.g., clubfoot,
vertical talus, cavovarus foot, thigh or calf atrophy, reflex
asymmetry, leg-length discrepancy).
sequential frontal and lateral radiographs, upright if the child is
mature enough to sit or stand. Congenital scoliosis must be followed
closely during the times of rapid spinal growth using serial
radiographs. The interval of observation (6 months to 2 years) varies
by the age of patient and type of deformity, with more frequent
radiographs for children age 0 to 3 years and 9 to 14 years and
children with lesions most likely to progress. Interobserver
variability in Cobb measurement of congenital scoliosis may be 10
degrees. Measuring the compensatory curve, if present, provides another
means to assess curve progression.
system should be screened with a renal ultrasound. Magnetic resonance
imaging of the entire spine and brain should be obtained to rule out
malformations, such as a tethered cord or diastematomyelia, if anything
in the history or physical exam suggests an abnormality or the patient
is to undergo surgical treatment of the deformity. A preoperative
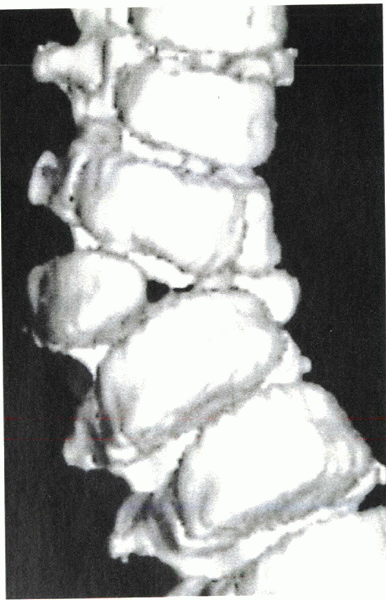
three-dimensional computed tomography (CT) scan can be helpful to
visualize the bone elements of the spine, and multiplanar reformatted
images have proved useful in identifying anomalies not seen on standard
CT (Fig. 19-4).
effective in preventing progression of congenital scoliosis.
Occasionally, it may be helpful in rebalancing the trunk or in reducing
a compensatory curve. Exercises, spinal manipulation,
electrical stimulation, special diets, and shoe lifts are not effective in preventing progression.
 |
progressive congenital scoliosis. Because operative reduction of the
curve magnitude in congenital scoliosis is more complex (with greater
risk) and less effective than in idiopathic scoliosis, early
intervention is suggested when progression is appreciated. Surgical
intervention in some cases may come at a relatively young age (1 to 3
years).
 |
|
Figure 19-4
Three-dimensional CT scan shows an unincarcerated fully segmented hemivertebra. (From Newton PO, Wenger DR, Lovell. Idiopathic and congenital scoliosis. In: Winter’s pediatric orthopaedics, 5th ed. Lippincott Williams and Wilkins, Philadelphia, 2001, p. 732.) |
-
Posterior fusion (with or without instrumentation)
-
Combined anterior and posterior fusion
-
Convex hemiepiphysiodesis (anterior or posterior hemiarthrodesis)
-
Hemivertebra excision
progression. The surgeon, patient, and parents must understand that, by
design, surgical treatment halts the growth of the spine. This
knowledge generates concern about shortening; however, continued growth
without surgery would not lead to increased height, but instead would
result in worsening spinal alignment. It also has been shown that these
children are small for their age and remain short, even if they do not
require surgery. Ultimate standing height is maximized by allowing the
unaffected segments of the spine to grow normally. Because the ultimate
goal is to halt progression, in situ fusion commonly is performed. If
instrumentation is used to add stability, the corrective force must be
applied with extreme caution, if at all, because neurologic risk seems
to be higher in these patients. Even with limited correction, however,
the internal support decreases the need for postoperative external
immobilization in many cases.
both ways. The choice depends on the type of curve, magnitude,
location, age of the patient, and experience of the surgeon.
involves placement of bone graft (autograft or allograft or both) along
the lamina, facets, and transverse processes of the vertebrae to be
fused. A brace or cast is worn for 4 to 6 months postoperatively.
Instrumentation provides children older than about 3 years the
potential for added stability, although postoperative immobilization
due to limited fixation in an immature spine is recommended.
in which substantial anterior vertebral growth is expected (Risser 0
and open triradiate cartilage) and often are combined with a posterior
fusion. The advantages of the anterior approach include halting
anterior spinal growth (which may lead to the additional “crankshaft
deformity”) and increasing the flexibility of the spine in cases in
which correction is planned. There seems to be an increased risk of
spinal cord injury owing to disruption of the blood supply to the cord
from dividing segmental vessels during anterior surgery in patients
with congenital deformity (particularly kyphosis). Monitoring of the
spinal cord with sensory and motor potentials is recommended. An
anterior and posterior combined fusion is used most commonly for young
patients with highly progressive deformities (e.g., fully segmented
hemivertebrae or hemivertebrae with a contralateral bar). Block
vertebrae, semisegmented hemivertebrae, and wedge vertebrae are less
likely to require anterior procedures because of their limited growth
potential.
performing a fusion only on the convex side of the curve, usually
anteriorly and posteriorly. The goal of this procedure is to create a
bone tether (convex fusion mass) that would allow subsequent growth on
the concave side, ultimately reducing the deformity. One level above
and one level below a hemivertebra often are included in the
hemiarthrodesis to encourage correction. This technique is best
reserved for failures of formation with less than 50 degrees of
deformity in patients younger than 5 years old.
correction and is coupled with stabilization by arthrodesis. This
procedure is technically demanding with greater neurologic risk but has
been shown to be safe and effective in experienced hands. It is safest
below the level of the conus (tip of the cord) and has the most
pronounced effect on truncal imbalance when performed in the lower
lumbar region. The procedure may be performed as simultaneous or staged
anterior and posterior procedures and via an isolated posterior
exposure. Spinal cord monitoring and a Stagnara wake-up test are
required to ensure neurologic function after the realignment. Care must
be taken not to compress neural elements when the gap created by the
bone excision is closed. Instrumentation appropriate to the size of the
patient is used, often with a body cast as well.
deformity show that localized fusion is effective in preventing
progression of the deformity. The complication rates are low because
the spine is not manipulated, and instrumentation is not used. The
cosmetic improvement in trunk shape is limited, but this remains the
gold standard for most congenital spinal deformities.
experienced hands and depends on the location of the defect. Correction
rates on average of 60% to 70% can be achieved. A successful outcome
depends on careful exposure and protection of the neural elements
combined with secure internal fixation.
mixed. In many cases, the hemiarthrodesis functions as an in situ
fusion limiting progression but not achieving correction. The greatest
chance for true correction by modifying growth exists for the youngest
patients with smaller deformities (patients <5 years old with a
hemivertebra and <50 degrees of curvature).
is necessary. If associated medical conditions are identified
preoperatively, most postoperative complications can be avoided.
Neurovascular checks are vital to identify any neurologic deficit.
Because of the immature nature of the patients, it often is necessary
to use casts and braces while the fusion is maturing. In patients
younger than 3 years old, the cast may need to include an arm or leg,
or both. The length of time necessary for immobilization usually is 3
to 4 months.
deformities but have a higher likelihood of developing neurologic
impairment. Congenital kyphosis is a deformity in which there is an
abnormal posterior convex angulation of a segment of the spine caused
by anomalous vertebrae.
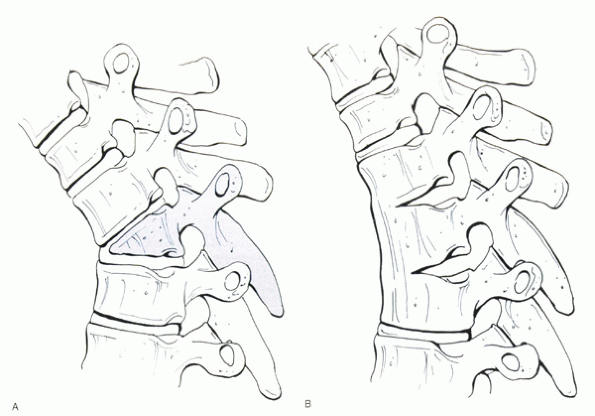
with failures of formation (type I), failures of segmentation (type
II), and mixed deformities (type III) (Fig. 19-5).
kyphosis and the highest likelihood of paraplegia, especially when
located between T4 and T9 (vascular watershed area). It is the second
most common cause of paraplegia after the infectious spinal
deformities. Type I deformities can result in kyphosis and scoliosis if
the greatest absence of vertebral body is anterolateral. Defects of
segmentation (type II) occur most often in the lower thoracic spine and
thoracolumbar junction. They are less progressive and rarely cause
paraplegia. Surgery is required (in situ fusion or correction by
osteotomy) if there is a significant deformity or if progression
occurs. Mixed (type III) deformities often progress rapidly and require surgery.
 |
|
Figure 19-5 Diagrammatic representation of classification system of congenital kyphosis. (A) Defect of formation. (B) Defect of segmentation.
|
and III defects. The severity of kyphosis and likelihood of progression
are related directly to the amount of vertebral body missing.
Conservative treatment is ineffective, and early surgical treatment is
suggested. The surgical approach is based on the age of the patient,
type of vertebral anomaly, size of the deformity, and presence or
absence of spinal cord compression.
treated by posterior in situ fusion; however, in deformities larger
than this, a combined anterior-posterior fusion is recommended.
Anterior “strutting” within the concavity is biomechanically superior
to a posterior fusion mass under tension.
or bladder dysfunction, hyperreflexia), the patient should undergo
anterior decompression, not laminectomy alone. An anterior approach is
the method of choice for decompressing the spinal cord by removing the
posterior remnant of the vertebral body. Preoperative halo traction is
contraindicated because this stretches the spinal cord even tighter
over the apical bone.
degrees are excellent. The kyphosis in patients with continued anterior
growth may improve over time, especially in younger patients. The
results of posterior fusion alone, with or without instrumentation, are
poor in stabilizing a deformity greater than 50 degrees. The most
successful results in patients with curves greater than 50 degrees
occur in those treated with anterior disc excision, strut grafting, and
arthrodesis combined with a posterior arthrodesis. Correction obtained
in published series is roughly 30%.
because of a frequent reduction in the cross-sectional area of the
canal and stretching of the spinal cord induced by reduction. The
results for improvement of preoperative neurologic deficits vary from
complete recovery to no recovery at all, depending on the chronicity of
the deficit and severity of the compression.
There are frequently associated malformations of the cardiac, urologic,
and neurologic structures. Progression of a deformity is an indication
for surgical stabilization, most often by in situ arthrodesis.
DM, Marrero G, King J, et al. Avoiding paraplegia during anterior
spinal surgery: the role of somatosensory evoked potential monitoring
with temporary occlusion of segmental spinal arteries. Spine
1991;16:S365-S370.
DM, Ruderman RJ, Conrad RW, et al. Congenital scoliosis and urinary
tract abnormalities: are intravenous pyelograms necessary? J Pediatr
Orthop 1987;7:441-443.
CJ, Moore DP, Fogarty EE, et al. Long-term results from in situ fusion
for congenital vertebral deformity. Spine 2002;27: 619-628.
AG, MacEwen GD, Bose WJ. Transpedicular convex anterior
hemiepiphysiodesis and posterior arthrodesis for progressive congenital
scoliosis. Spine 1992;17:S291-S294.
