Trigger Finger
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Trigger Finger
Trigger Finger
Dawn M. LaPorte MD
Chris Hutchins MD
Description
-
A “trigger finger” is a manifestation of
stenosing tenosynovitis that results in painful catching of the
involved flexor tendon as the patient flexes and extends the digit. -
As the affected digit is slowly flexed, it snaps or triggers into a flexed position.
-
Once the digit triggers, extension is difficult and, occasionally, must be obtained manually.
Pregnancy Considerations
-
Incidence in pregnant females may be higher than that in the general population.
-
Treat with corticosteroid injection for temporary triggering relief because it likely will resolve or not recur.
Epidemiology
-
Affected digits:
-
In the adult, all digits, but most commonly, the thumb, ring, and middle fingers
-
In the child, primarily the thumb
-
-
Children (congenital type) and middle-aged patients predominate.
-
The adult variety of trigger finger is more common in females than in males.
Incidence
The lifetime incidence in nondiabetic adults >30
years old is reported to be 2.2% and that in adults with
insulin-dependent diabetes mellitus is up to 10% (1).
years old is reported to be 2.2% and that in adults with
insulin-dependent diabetes mellitus is up to 10% (1).
Risk Factors
-
Rheumatoid arthritis
-
Increased age
-
Diabetes mellitus
Etiology
-
A nodule usually develops on the flexor tendon, most likely in response to abrasion of the tendon in the tendon sheath.
-
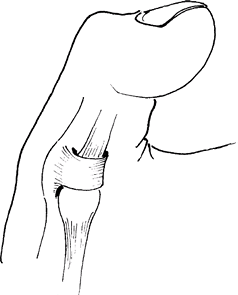
The nodule then impinges on one of the
rings of fibrous tissue encircling the flexor tendon sheath known as
the A1 pulley; the result is “triggering” when the digit is extended (Fig. 1). -
This problem is self-perpetuating because the irritation from triggering prevents a decrease in the swelling.
-
In the pediatric population (<2 years
old), a congenital narrowing of the tendon sheath or a nodular
thickening in the tendon (Notta node) may be present, resulting in
congenital trigger digit, most commonly the thumb.
Associated Conditions
-
In congenital trigger digit, an association with trisomy 13 exists.
-
In the adult patient, other disorders related to tenosynovitis, such as de Quervain tenosynovitis and CTS, may be present.
-
Systemic disorders that cause connective
tissue abnormalities, such as diabetes, gout, and rheumatoid arthritis,
also may be present.
Signs and Symptoms
-
Sign: A nodule in the palm of the hand, just distal to the distal palmar crease
-
Symptom: Painful locking or snapping of the digit into a flexed position with flexion
Physical Exam
-
By gently palpating the flexor tendon
sheath of the affected digit in the region of the distal palmar crease
and then having the patient flex the digit, the offending nodule and/or
triggering sometimes may be palpated. -
In children <2 years old, 30% have bilateral involvement (2–4).
Tests
Lab
No serum laboratory tests aid in this diagnosis.
Imaging
Imaging studies usually are not necessary because trigger finger is a clinical diagnosis.
 |
|
Fig. 1. In trigger finger, a nodule in the tendon sheath prevents it from sliding under the pulley. The finger does not extend.
|
Differential Diagnosis
-
Tendon rupture
-
Contracted (ankylosed) joints
-
Congenital clasped thumb
-
Absent extensor
-
Tumor of tendon sheath
-
Loose body in the MCP joint
General Measures
-
Triggering may unlock with rest.
-
In children:
-
<6 months old: 30% resolve spontaneously (2).
-
6–30 months old: Only 12% resolve spontaneously (2).
-
Many require surgical intervention, which
is recommended before 4 years of age to prevent permanent contracture
of the IP joint (5)
-
-
In adults: Corticosteroid injection is 1st line of treatment.
-
When nonoperative therapy fails, surgical incision of the A1 pulley has a 98% cure rate.
-
No restrictions are placed on activity after injection.
Special Therapy
Physical Therapy
None is needed.
Medication
First Line
-
In adults, treatment commences with
injection of the tendon sheath (but not the tendon) with lidocaine and
cortisone in the region of the A1 pulley.-
A single injection results in a 44–93% success rate (6–8).
-
The use of >3 injections has a 77–88% success rate (6–8).
-
Surgery
-
A small transverse or oblique incision is
made in the region of the A1 pulley (just distal to the distal
transverse palmar crease) and overlying the affected flexor tendon. -
The A1 pulley is incised.
-
After surgical release, the hand is bandaged for several days.
-
Activity is resumed gradually.
P.473
Prognosis
The prognosis is good.
Complications
-
Errant injections may result in damage to the tendon or digital nerves and vasculature, but these complications are rare.
-
Surgical risks include digital nerve laceration, tendon rupture, infection, and reflex sympathetic dystrophy.
Patient Monitoring
None is necessary after surgical release.
References
1. Stahl S, Kanter Y, Karnielli E. Outcome of trigger finger treatment in diabetes. J Diabet Complications 1997;11:287–290.
2. Dinham
JM, Meggitt BF. Trigger thumbs in children. A review of the natural
history and indications for treatment in 105 patients. J Bone Joint Surg 1974;56B:153–155.
JM, Meggitt BF. Trigger thumbs in children. A review of the natural
history and indications for treatment in 105 patients. J Bone Joint Surg 1974;56B:153–155.
3. Ger E, Kupcha P, Ger D. The management of trigger thumb in children. J Hand Surg 1991;16A:944–947.
4. Wood VE, Sicilia M. Congenital trigger digit. Clin Orthop Relat Res 1992;285:205–209.
5. Wolfe
SW. Tenosynovitis. In: Green DP, Hotchkiss RN, Pederson WC, et al, eds.
Green’s Operative Hand Surgery, 5th ed. Philadelphia: Elsevier
Churchill Livingstone, 2005:2137–2159.
SW. Tenosynovitis. In: Green DP, Hotchkiss RN, Pederson WC, et al, eds.
Green’s Operative Hand Surgery, 5th ed. Philadelphia: Elsevier
Churchill Livingstone, 2005:2137–2159.
6. Freiberg A, Mulholland RS, Levine R. Nonoperative treatment of trigger fingers and thumbs. J Hand Surg 1989;14A:553–558.
7. Griggs SM, Weiss APC, Lane LB, et al. Treatment of trigger finger in patients with diabetes mellitus. J Hand Surg 1995;20A:787–789.
8. Rhoades
CE, Gelberman RH, Manjarris JF. Stenosing tenosynovitis of the fingers
and thumb. Results of a prospective trial of steroid injection and
splinting. Clin Orthop Relat Res 1984;190: 236–238.
CE, Gelberman RH, Manjarris JF. Stenosing tenosynovitis of the fingers
and thumb. Results of a prospective trial of steroid injection and
splinting. Clin Orthop Relat Res 1984;190: 236–238.
Additional Reading
Lister G. Inflammation. In: The Hand: Diagnosis and Treatment,3rd ed. New York: Churchill Livingstone; 1993:323–353.
Codes
ICD9-CM
-
727.03 Trigger finger, acquired
-
756.89 Congenital
Patient Teaching
Patients are advised to have surgical release for recurrent symptoms.
FAQ
Q: What is the initial treatment for a trigger digit?
A: Most trigger digits in adults can be treated successfully with corticosteroid injection.
Q: Is trigger digit associated with any medical comorbidities, and does this affect prognosis?
A:
“Secondary” trigger digit can be associated with diabetes mellitus,
gout, renal disease, rheumatoid arthritis, and other rheumatic
diseases. It is associated with a worse prognosis after nonoperative or
operative management.
“Secondary” trigger digit can be associated with diabetes mellitus,
gout, renal disease, rheumatoid arthritis, and other rheumatic
diseases. It is associated with a worse prognosis after nonoperative or
operative management.
