Anatomy of the Brachial Plexus
II – Single-Injection Peripheral Blocks > A – Upper Extremity > 6
– Anatomy of the Brachial Plexus
likelihood of success when performing peripheral nerve blocks. However,
it is important to recognize that variations are frequent, and that
“normal anatomy” is only found in 50% to 70% of cases.
to T1 (the posterior roots give innervation for skin and muscle of the
paravertebral area). Brachial plexus innervates the scapular belt and
the upper limb. It has a triangular shape with the base applied against
the cervical spine and the vertex in the axilla. The anterior rami
supply the superior (C5-6), middle (C7), and inferior (C8-T1) trunks.
At the level of the superior border of the first rib, each trunk
divides into an anterior and posterior division. The three posterior
divisions join to form the posterior cord. At the level of coracoid
process, the anterosuperior and middle divisions form the lateral cord
and the anteroinferior division becomes the medial cord. The axillary
and radial nerves originate from the posterior cord. The
musculocutaneous nerve quickly separates from the main brachial plexus
as it passes underneath the clavicle and becomes a single nerve as the
plexus transitions from divisions to cords. In the vertex of the
axilla, the lateral cord and part of the medial cord join to form the
median nerve; the medial cutaneous nerve of the arm and the forearm and
finally the ulnar nerve originate from the remainder of the medial
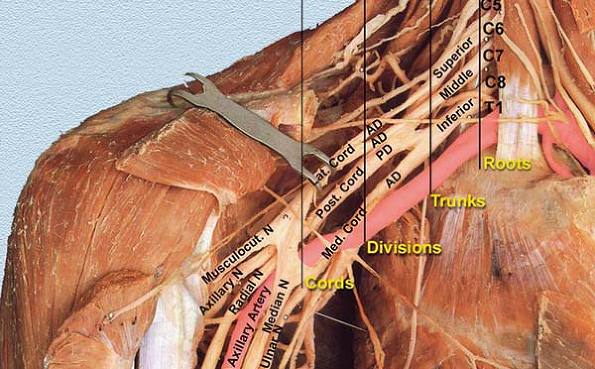
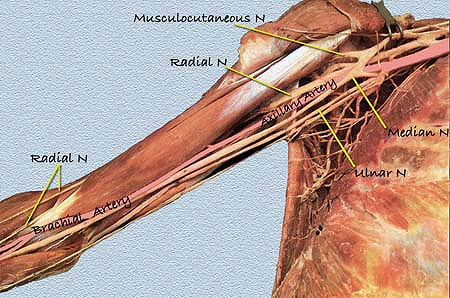
cord. See Figure 6-1 for the classical two
dimensional picture of the brachial plexus highly recommended to review
the anatomy in a fresh tissue cadaver whenever possible. In Figures 6-2 and 6-3
minimal alteration of the anatomy in these fresh tissue dissections
demonstrate the brachial plexus and the surrounding anatomy in situ.
complexity of the brachial plexus. During organogenesis, between the
4th and the 8th week of development, the brachial plexus has a cone
shape in the bud limb. The cutaneous innervation is distributed at the
periphery of the trunk wall. As the bud limb grows, dermatoma stretches
out. The cone then divides longitudinally into two independent plans,
anterior and posterior, with the appearance of three cords. The
posterior cord (posterior plane) provides innervation to the extensor
and supinator muscles while the anterior plane, more complex and
variable, provides the medial and lateral cords that innervate the
flexor and pronator muscles. Generally there is no anastomosis between
the anterior and posterior cords. The presence of the subclavian artery
explains why there are two anterior cords. Thus, in some species
without the subclavian
artery
(birds) only one anterior cord is found. Embryogenesis also explains
the frequency of variations and anastomosis between the nerves
originating from the anterior cords.
 |
|
Figure 6-1. Brachial plexus anatomy.
|
to the brachial plexus. This contribution allows one to differentiate a
“prefixed” plexus with a C4 predominant contribution versus a
“postfixed” plexus with a T2 predominant contribution. In humans, the
brachial plexus is predominantly “prefixed.” This differentiation may
explain the superior extension toward C4 that frequently occurs after
an interscalene block (prefixed).
are more relevant than others when performing brachial plexus blocks.
They include:
-
The long thoracic nerve that directly originates from the C5 to C7 roots.
It supplies the serratus anterior muscle. The nerve runs posterior to
the brachial plexus. Therefore, when performing an interscalene block,
the stimulation of the serratus anterior muscle suggests that the
needle should be redirected anteriorly. -
The dorsal scapular nerve supplies the levator scapulae and rhomboid minor and the superior part of the rhomboid major muscles.
It is one of the first nerves to leave the plexus. The stimulation of
this nerve produces an elevation of the scapulae (interscalene
approach). The injection of local anesthetic solution following its
stimulation produces a block of the deep cervical plexus, which may be
of interest in the case of a carotid surgery. -
The suprascapular nerve supplies both the supraspinatus and the infraspinatus muscles and sends branches to the shoulder joints.
It originates at the level of the interscalene groove. Moreover, like
the long thoracic nerve, the suprascapular nerve runs posterior to the
brachial plexus. Its stimulation, which produces a posterior
contraction of the rotator cuff (shoulder ascension), indicates that
the needle needs to be redirected anteriorly. Diffusion of local
anesthetic toward this nerve after a supraclavicular approach is
inconsistent. -
The subclavius nerve
supplies the subclavius muscle and anastomoses with the phrenic nerve,
a nerve that also originates from C5. This explains in part why,
even with limited extension to the cervical plexus or limited volume of
local anesthetic, a blockade of the phrenic nerve with an interscalene
block results in a reversible diaphragmatic paralysis.
 |
|
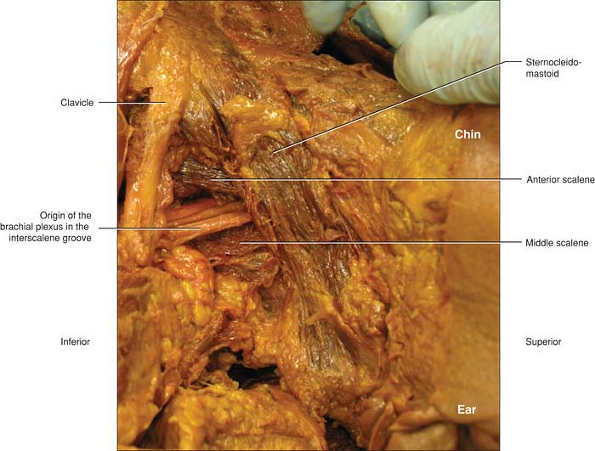
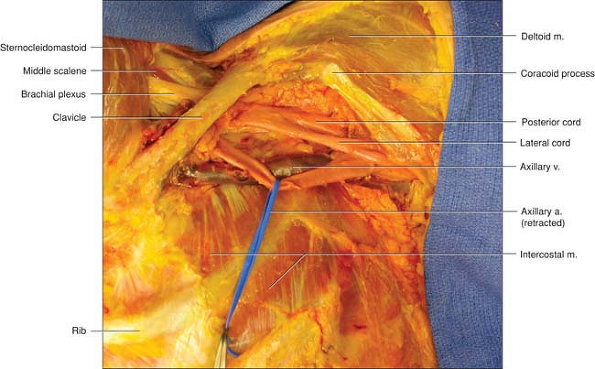
Figure 6-2.
A very limited dissection demonstrating how the brachial plexus lies in the neck as transverse from its origin of individual roots from the cervical spine to somewhat join into divisions and group into cords. The divisions travel in a similar plane at this level and are organized in a parallel fashion to each other. The plexus is framed by the sternocleidomastoid at the superior edge of the triangle until it gives way to the anterior border of the anterior scalene. At times the anterior scalene is not prominent as in this specimen. The inferior border is the clavicle. The triangle is completed by the posterior border in the middle scalene muscle. |
the lateral and medial cords. It runs first laterally to the axillary
artery and progressively crosses over the brachial artery to become
medial to the brachial artery at the inferior third of the arm. It does
not give any branch until the inferior part of the arm, although in
one-third of cases it provides an anastomosis to the musculocutaneous
nerve. Around the elbow several branches originate from the median
nerve (articular to the elbow, muscular to pronator teres muscle).
About 2 or 3 cm below the elbow, the median nerve provides the
interosseous nerve, which innervates the anterior aspect of the flexor
digitorum profundus and anterior aspect of the carpal joint, with
frequent anastomosis with the posterior interosseous nerve. In the
forearm the median nerve runs between the flexor digitorum
superficialis and flexor digitorum profundus muscles. At the distal
third of the forearm the median nerve runs between the tendons of the
flexor carpi radialis and palmaris longus muscle. It is of interest to
note that the palmaris longus muscle is absent in 15% of the
population. Several centimeters above the wrist crease the median nerve
provides a sensory
palmar
branch. Finally, the median nerve enters the hand through the carpal
tunnel under the flexor retinaculum and divides into small muscular
branches innervating a part of the thenar muscles and branches
contributing to the palmar digital nerve.
 |
|
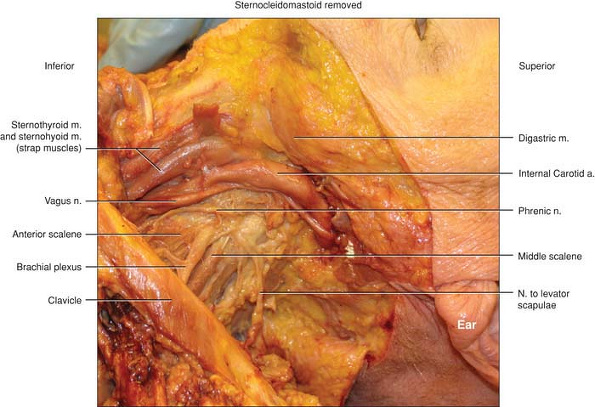
Figure 6-3.
The brachial plexus and its surrounding structures. In this dissection the sternocleidomastoid and the internal jugular vein have been reflected away so that the surrounding structures could be better visualized. The close proximity to the phrenic can be appreciated as well as the relatively close internal carotid artery and vagus nerve. Of note in this specimen is an example of how small in diameter the phrenic nerve can be and how close. At the upper end of the origin of the brachial plexus they are almost side by side. This is often demonstrated during performance of an interscalene block with just a very small change in needle direction causing a phrenic nerve stimulation of the diaphragm or the desired twitch of stimulation of the brachial plexus. |
axilla from the medial cord. Initially the ulnar nerve runs medial to
the axillary artery and progressively posterior, reaching the elbow
between the medial humeral epicondyle and the olecranon. It leaves its
first collateral branch at the elbow for the joint. Below the elbow,
branches originate to the flexor carpi ulnaris and part of flexor
digitorum profundus muscles. Along the forearm the ulnar nerve runs
posterior to the flexor carpi ulnaris and posterior and medial to the
ulnar artery. Several centimeters before the wrist crease the ulnar
nerve leaves two branches: a palmar branch and a dorsal branch for the
palmar and dorsal aspect of the hand. The ulnar nerve enters the hand
running under the flexor retinaculum and divides into superficial
branches to the palmar digital nerves and deep motor branches that
innervate the hypothenar, interosseous, and parts of the lumbrical and
thenar muscles.
cord. It leaves the vascular/nervous space high in the axilla,
diffusing in the direction of the coracobrachialis muscle,
which
it perforates. In the arm, it runs in the groove between the biceps and
brachialis muscles. It supplies these two muscles and the
coracobrachialis muscle. Several variations of the course and
distribution of the musculocutaneous nerve may be observed. In 20% of
cases, instead of piercing the coracobrachialis muscle it lies against
the median nerve for a variable distance along the arm before supplying
the three muscles. It pierces the deep fascia just before the elbow and
divides in two branches that run on each side of the cephalic vein and
become the lateral cutaneous nerve of the forearm. It supplies the skin
of the lateral border of the forearm up to the wrist. In some cases it
can extend until the thenar region.
 |
|
Figure 6-4. Terminal branches (anterior plan).
|
are both formed in the medial cord. The medial cutaneous nerve of the
arm quickly leaves the plexus in the axilla and dives in the direction
of the armpit where it joins the intercostobrachial nerve (Hyrtl
anastomosis). It supplies the skin of the medial border of the arm. The
cutaneous nerve of the forearm arises from the medial cord and runs
with the ulnar nerve until the elbow. In the upper part of the arm it
leaves some branches (one or two) for the anterior and internal part of
the arm. It pierces the deep fascia just before the elbow and divides
in two branches on each side of the basilic vein. It supplies the skin
of the medial aspect of the forearm until the wrist.
It runs deeply against the capsule of the shoulder joint, and it curves
posteriorly along the surgical neck of the humerus through a
quadrangular space formed laterally and medially by the humerus and the
triceps brachii muscle and superior and inferior by the teres minor and
major muscles. Then it divides into anterior and posterior branches. It
supplies the skin of the inferior half of the shoulder and the lateral
aspect of the arm. It also supplies the teres minor and deltoid muscles
and gives branches to the shoulder joint.
in the axilla. It runs initially posterior to the axillary artery and
progressively in a spiral course around the humerus in a specific
sulcus
to run laterally and then anteriorly at the elbow. It supplies the
triceps brachii muscle through a branch leaving at various levels in
the axilla. Frequently it leaves a spindly branch to the brachialis
muscle. At the third distal part of the arm it leaves branches for the
brachioradialis and extensor carpi radialis longus muscles. It supplies
skin of the posterior aspect of the arm and the forearm and the lateral
border of the elbow. Around the elbow, it gives articular branches to
the joint. The cutaneous branch for the forearm leaves the trunk at the
inferior part of the radial sulcus. At various levels around the elbow,
the radial nerve divides into sensory (superficial) and motor (deep)
terminal branches. The superficial branch runs along the lateral border
of the forearm and pierces the fascia at the lower third. At this level
it is in close relation to the cephalic vein. It supplies the lateral
part of skin of the dorsal aspect of the hand. The deep branch
(posterior interosseous muscle) winds posteroinferiorly around the neck
of the radius and runs between the superficial and deep planes of the
extensor muscles. It supplies all extensor and supinator muscles and
the dorsal face of the carpal joint.
nerves. Anastomoses are frequent with many variations, and some are
more important than others. In approximately one-third of cases an
anastomosis exists between the musculocutaneous and the median nerve.
In most cases it is a lateromedial anastomosis that follows the course
of the musculocutaneous nerve, but sometimes it is a mediolateral
anastomosis that follows the course of the median nerve. Consequently,
if during an axillary or humeral block it is difficult to locate the
musculocutaneous nerve, the clinician should determine if the
musculocutaneous nerve is not already blocked by an injection of local
anesthetic following the identification of the median nerve.
anastomosis between median and ulnar nerves occurs frequently (20%). In
general, it is median fibers that are found in the deep branch of the
ulnar nerve, which could explain why when one uses a nerve stimulator
it is sometimes difficult to differentiate between these two nerves. In
cases of doubt, one can search for a response of the flexor carpi
ulnaris muscle (always supplied by the ulnar nerve) or a response of
the flexor carpi radialis muscle (always supplied by the median nerve).
to recognize the difference between skin, muscle, and bone innervation.
Such knowledge is essential to predict the extension of the motor and
sensory block and determine the most appropriate approach for a given
surgery (especially if a distal block is chosen). It also explains the
motor response associated with the stimulation of a given nerve.
shoulder, while the axillary nerve innervates the lower half; however,
overlapping with intercostal nerves for the anterior aspect of the
shoulder and with dorsal ramus of C3 to T3 roots for the posterior
aspect of the shoulder is possible. This explains why, even with a
successful interscalene block, cutaneous anesthesia could be
insufficient to provide adequate anesthesia for the insertion of a
posterior trocar or deltopectoral groove incision.
not produce a sensory block of the posterior aspect of the forearm
because this territory is supplied by the posterior
cutaneous
nerve, a branch of the radial nerve that originates in the middle of
the arm. In general, at the level of the elbow and thereafter, none of
the three nerves (median, ulnar, and radial) have branches to supply
the shin of the forearm.
 |
|
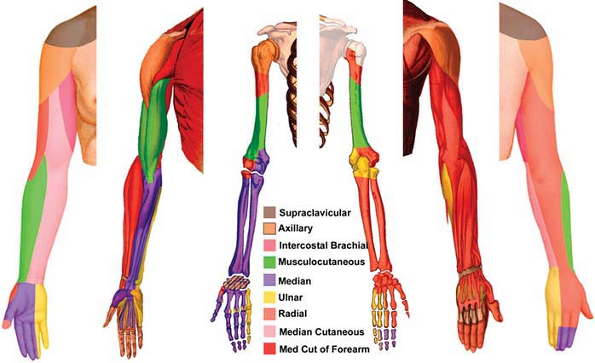
Figure 6-5. Upper limb innervation.
|
by palmar branches of the ulnar and median nerves. These branches, as
the dorsal branch of the ulnar nerve, originate several centimeters
above the wrist crease. This explains why median and ulnar blocks at
the wrist need to be performed at the distal third of the forearm (5 to
6 cm above the wrist crease). In addition to the palmar aspect of the
second, third, and fourth fingers, the palmar digital branches of the
median and ulnar nerves supply the two-thirds dorsal part of these
fingers. Consequently, a block of the common palmar branch provides
anesthesia to 75% of the finger with a single injection. In contrast,
the palmar aspect of the second, third, and fourth fingers depends on
the palmar digital branch of the median nerve. Consequently, a block of
the common palmar branch provides anesthesia to 75% of the palm with a
single injection.
the radial superficialis nerve. At the level of the hand there is also
a considerable overlap in zones of distribution of the different
nerves. This must be taken into account when the intensity of each
block is being tested. The median nerve contains the most important
contingent of sensitive fibers for the hand.
are supplied by the brachial plexus. This explains why it is difficult
to obtain a complete muscle relaxation of the shoulder even with an
efficient brachial plexus block. This could be of importance for some
types of surgery, like shoulder arthroplasty, even if anesthesia is
sufficient with an interscalene block.
anterior group (biceps, brachial, and coracobrachialis muscles) all
supplied by the musculocutaneous nerve and a posterior group (triceps
muscle) supplied by the radial nerve.
an anterior and medial group in charge of flexion and pronation
movement supplied by the median and the ulnar nerve;
a
lateral group for supination supplied by the deep radial nerve; and a
posterior group for extension that is also supplied by the radial nerve.
nerve except for a part of the thenar muscles and the first and second
lumbrical muscles, which are supplied by the median nerve.
The figures derived from the book published by Déjerine in 1926 are in
agreement with the concept that the innervation of the joint is
generally supplied by the same nerves that supply the muscles
mobilizing the joint (Hilton’s law).
suprascapular, subscapular, and pectoral lateral nerves. All these
nerves originate from the C5-6 roots and are effectively blocked by an
interscalene approach.
(a branch of the median nerve) with frequent ulnar anastomosis and by
the posterior interosseous nerve (a branch of the radial nerve).
innervation are based on superficial distribution, it is important to
realize that the muscular and bone innervation is not strictly
superimposed. The only location in which a single nerve innervates all
structures is the medial aspect of the hand and the fifth finger (ulnar
nerve). For example, in the case of an exploration of a first
interdigit wound, it is necessary to block the median and radial nerves
to provide adequate anesthesia of the anterior and posterior aspect of
the skin, and to block the ulnar nerve to provide anesthesia of the
interosseous muscles.
delineates two triangles: one superior, the omotrapezius triangle with
the trapezius muscle; and one inferior, the omoclavicular triangle with
the clavicle. Roughly, we can consider that we find the trunk of the
brachial plexus in the superior triangle and the cords in the inferior
triangle.
and fascia surrounds all the brachial plexus and vessels. In the
supraclavicular area this space is limited anteriorly by the anterior
scalene muscle and posteriorly by the middle scalene. Anteriorly the
superficial cervical fascia lies between the trapezius and the
sternocleidomastoid muscles, and posteriorly the profound cervical
aponeurosis is formed by the fusion of the pretracheal and prevertebral
fasciae.
superior brachial plexus, composed of the superior (C5-6) and middle
(C7) trunk, and the inferior plexus, deeply localized behind the
subclavian vessels and lying on the pleural space. In some cases the
C5-6 root is not found in the interscalene groove but runs in front of
the anterior scalene muscle. Moreover, Hovelacque described a frequent
muscular lamina tight between the scalene muscles, which separates the
first two roots of the plexus from the others. These considerations
explain in part why it is difficult to obtain a complete brachial
plexus anesthesia after an interscalene block. They also explain that:
-
When the needle is positioned too medially, there is an increased risk of vertebral artery puncture or perimedullar puncture.
-
The proximity of the inferior cervical node explains the frequent Horner syndrome.P.52
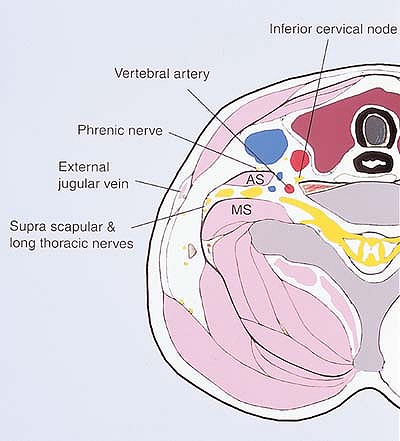
![]() Figure 6-6. Topographic anatomy.
Figure 6-6. Topographic anatomy. -
It is important to recognize the presence
of the phrenic nerve anteriorly and the supra-scapular and long
thoracic nerves posteriorly to the brachial plexus. Their stimulation
provides critical information about how to reorient the needle. -
The external jugular vein is anterior to
the brachial plexus and prolongs the line perpendicular to the middle
of the clavicle. Its localization is helpful when the interscalene
groove is difficult to feel, especially in obese patients.
knowledge of the general disposition of the trunk fibers provides
helpful information in the understanding of nerve stimulation for the
interscalene approach. The superior trunk could be separated in two
contingents, one superior with fiber for musculocutaneous and axillary
nerves and one inferior for radial and median nerves. The middle trunk
contains fibers mainly for the radial and to a lesser degree for the
musculocutaneous and median nerves. Consequently, the stimulation of
the superior trunk (C5-6) produces a contraction of either the biceps
brachii or the deltoid muscles while the stimulation of the
brachioradialis or triceps brachii muscles can be related to either a
stimulation of the posterior part of the superior trunk or a
stimulation of the middle trunk. A finger flexion suggests a
stimulation of the inferior trunk with a needle close to the pleura.
trunks and cords occurs corresponding to the cleavage between
innervation of flexors (anterior plan) and extensor muscles (posterior
plan). The main interest of this region is the closeness of the
brachial plexus nerves, which suggest extensive diffusion with a single
injection. But this zone corresponding to the supraclavicular fossa is
considered quite dangerous by anatomists and surgeons because of the
close relations between nerves, vessels, and pleural space. Several
collaterals of the subclavian artery (transversa colli and the
suprascapular or the cervical superficialis arteries) cross or
interlace the brachial plexus. Consequently, independently of a direct
vascular injection
of
local anesthetic, a vascular puncture can lead to the development of a
profound hematoma with an increasing risk of secondary neurologic
compressions or fibrosis.
 |
|
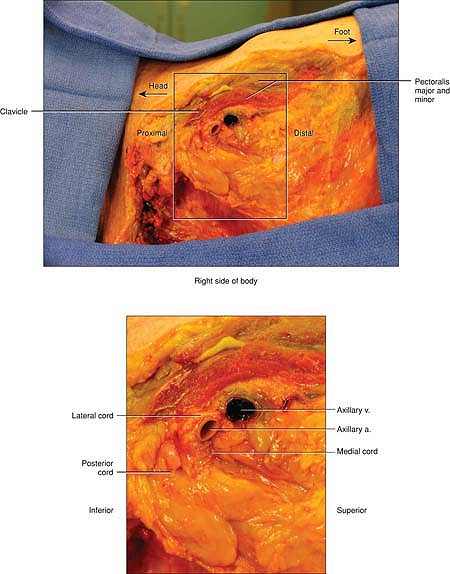
Figure 6-7.
Frontal dissection of the brachial plexus demonstrating its course from the interscalene area to the beginning of the axilla. The pectoralis major and minor have been removed. The plexus exits the interscalene region, passes under the clavicle, and surrounds the artery. The axillary artery has been retracted by the blue band to show the posterior cord of the plexus or it would not have been seen at all. The medial cord is too deep to be shown in this frontal view. The vein is quite inferior and if it is punctured by the needle, the needle should be removed and reentered 1 to 2 cm superiorly. Note in this section the boundaries of the lung as seen by the edges of the intercostal muscles and why it is possible to enter the lung with both the vertical infraclavicular block and the coracoid infraclavicular block. |
on the direct approach of the supraclavicular fossa and instead select
a more lateral approach, in search of a stimulation of the lateral cord.
pectoral muscle, posteriorly by the latissimus dorsi muscle, laterally
by the biceps brachii and coracobrachialis muscles, medially by the
thorax and anterior serratus muscle, and superiorly by the scapula,
clavicle, and the first rib. In this area the three cords divide into
the terminal branches of the brachial plexus at the level of the
scapulohumeral joint and posteriorly to the inferior border of the
pectoralis minor muscle. At this level, the plexus is in close
proximity to vessels and especially the axillary artery: In the upper
part of the axilla behind the clavicle, the artery is anterior to the
plexus and progressively becomes central as it runs along the axilla.
As with the suprascapular region, the entire plexus is located in a
common diffusion space between the clavipectoral fascia in front, the
subscapular teres major latissimus dorsi posteriorly, the
coracobrachialis laterally, and the anterior serratus medially. It is
necessary to distinguish the upper part of the axillary region
corresponding to the infraclavicular region and the lower part
corresponding to the axillary hollow.
brachial plexus originate. As for the supraclavicular region, we can
roughly define an anterior plan centered by the median nerve with the
musculocutaneous nerve laterally and the ulnar and medial antebrachial
cutaneous nerves medially. A posterior plane can be made with the
radial and axillary nerves. After their differentiation, the
musculocutaneous and axillary nerves quickly leave the common diffusion
space, which explains why there is an increased risk of block failure
if an injection of local anesthetic is made following the stimulation
of either the musculocutaneous or axillary nerve. In contrast, a
stimulation of the median nerve produces more consistent results.
to note the close proximity of the nerves and vessels (axillary
vessels, thoracoacromial artery, and cephalic vein) in this region
where hemostasis with a simple compression could be difficult.
central axis of the nerves and vessel bundle. Although Partridge and
Retzl have shown variation of localization of the nerves around the
artery, we can consider that the median nerve is lateral, the ulnar
nerve is medial and anterior, and the radial nerve is medial and
posterior to the axillary artery. At this level, the diffusion space is
divided into secondary sheaths. This concept is very old: In 1855
Marcellin Duval described a common sheath for vessels and nerves
partitioned by septa. Lassale and Ang demonstrated the existence of a
common space between the median and ulnar nerves and the axillary
vessels but without the radial, axillary, and musculocutaneous nerves.
The presence of these septa was confirmed by Thompson and Rorie, who
compared clinical, radiologic, and anatomic data. Even though some
subsequent studies have limited the value of these findings, they
explain why it is difficult to obtain more than 80% of a complete block
with a single injection.
and nerves, vascular puncture in this area is easy to control with
external compression.
including nerves and vessels, except between the brachial artery and
the median nerve (in some rare cases the ulnar nerve is included in
this space). Therefore, a high humeral block requires each nerve to be
blocked individually. Although the distribution of the nerves around
the brachial artery is comparable, a greater distance separates each
nerve. To perform a high humeral block, the needle must be introduced
at the proximal third of the arm (and not more distal) to avoid
crossing the radial nerve on the lateral aspect of the humerus and it
becoming inaccessible to the needle. This explains why the term
“humeral or brachial canal block” is preferred to the term “midhumeral
block” that was initially proposed. When stimulating the radial nerve,
a contraction of the triceps brachii must not be accepted as the end
point but rather an extension of the thumb. This response corresponds
to a stimulation of the muscular branch, which at this level is at some
distance from the radial nerve.
distal third of the arm. It is possible to distinguish the superficial
nerves, which supply the skin of the forearm, and the deep nerves that
supply muscles of the forearm and the skin and the muscles of the hand.
are near the elbow. The lateral antebrachial cutaneous nerve (terminal
branch of the musculocutaneous nerve) has two branches: one anterior
and one posterior on each side of the cephalic vein. The medial
antebrachial
cutaneous
nerve also has two branches, which are satellites of the basilic vein.
The posterior antebrachial cutaneous nerve (a branch of the radial
nerve) is at the level of the posterior aspect of the elbow. All of
these nerves can be blocked by subcutaneous infiltration.
 |
|
Figure 6-8.
Sagittal section of the infraclavicular area. This dissection is a sagittal section of the right side demonstrating the relationship of the brachial plexus below the clavicle. The pectoralis major and minor are virtually the only muscles above the plexus. The lung is not visible and has not been violated. At the level of a vertical infraclavicular block, the lung would be visible. The axillary vein is prominently seen inferior to the plexus, which surrounds the axillary artery. The fascicles of the lateral cord (which contains one-half of the median nerve) is virtually laying on the artery. The posterior cord (which contains 100% of the radial nerve) is actually superior but is deeper than the artery from the surface of the skin. It is large and round in this specimen compared with the lateral cord, which is flattened and surrounds the upper surface of the artery. The medial cord (which contains the other part of the median nerve and the ulnar nerve) is just under the artery and is the deepest cord to the skin. |
median nerve lies between the medial border of the biceps brachii
tendon and the lateral border of the pronator teres muscle tendon. In
this region the nerve is located medially to the brachial artery, which
constitutes an easy landmark for a median block. The radial nerve lies
between the lateral border of the biceps brachii tendon and the medial
border of the brachioradialis biceps tendon. It has a mirror position
with the median nerve regarding the biceps brachii tendon, but is more
profound. Frequently, contraction of the pronator muscles for the
median nerve and contraction of the brachioradialis nerve for the
radial nerve are first observed with the nerve stimulator. These
responses must not be accepted as an end point, and the needle must be
moved more laterally for the median nerve and more medially for the
radial nerve. The ulnar nerve runs on the posterior aspect of the
elbow, very superficially, in the groove between the olecranon and the
medial epicondyle.
antebrachial cutaneous, and the posterior antebrachial cutaneous nerves
are the three superficial branches of the distal third of the forearm.
These three nerves supply the skin of the forearm until the wrist
crease with a frequent thenar extension for the lateral antebrachial
cutaneous nerve. These nerves can be blocked by subcutaneous
infiltration. Moreover, the superficial radial branch, which supplies
part of the dorsal face of the hand located on the lateral border of
the forearm, can be blocked at the level of the wrist crease.
medially and the flexor carpi radialis tendon laterally. Located 3 to 4
cm above the wrist, it gives a palmar branch for the hand.
Consequently, a median nerve block at the wrist must be performed at
least 5 cm above the crease. Since at this level the median nerve is
mainly composed of sensitive fibers with a small motor contingent, the
use of a nerve stimulator produces inconsistent motor results. Finally,
at this level the median nerve is surrounded by the flexor tendons,
which constitute a real space of diffusion for local anesthetics.
aspect of the carpal joint. It lies in front of the interosseous
membrane posterior to the median nerve and is separated from it by the
pronator quadratus muscle. It is unlikely that injection of local
anesthetic for a median nerve block at the wrist could extend to the
anterior interosseous nerve.
posterior to the flexor carpi ulnaris tendon and the ulnar artery.
Between 4 and 6 cm above the wrist crease it contains two branches, one
posterior for the dorsal face of the hand and one palmar branch.
Consequently, a block of the ulnar nerve should be performed more than
5 cm above the wrist crease. In contrast to the median nerve, however,
the ulnar nerve at this level is mainly motor and very easy to locate
with the nerve stimulator. Since its location under the flexor carpi
ulnaris is variable, a blind injection of local anesthetics would be
associated with a high failure rate.