Cervical Blocks
Editors: Chelly, Jacques E.
Title: Peripheral Nerve Blocks: A Color Atlas, 3rd Edition
Copyright ©2009 Lippincott Williams & Wilkins
> Table of Contents > Section
II – Single-Injection Peripheral Blocks > C – Miscellaneous Blocks
> 16 – Cervical Blocks
II – Single-Injection Peripheral Blocks > C – Miscellaneous Blocks
> 16 – Cervical Blocks
16
Cervical Blocks
Laurence Marr
General Comments
The regional approach to anesthesia for carotid
endarterectomy offers several advantages over general anesthesia. With
the patient awake, it offers an instant monitor of adequate blood flow
from the contralateral side when the carotid artery is clamped.
Additionally, hemodynamics are better preserved, compared with
emergence from general anesthesia and extubation.
endarterectomy offers several advantages over general anesthesia. With
the patient awake, it offers an instant monitor of adequate blood flow
from the contralateral side when the carotid artery is clamped.
Additionally, hemodynamics are better preserved, compared with
emergence from general anesthesia and extubation.
Cervical plexus block is an easy block to do in most
patients, but there is a learning curve. As with most regional
techniques, they are not always perfect, and it is important to have a
plan to manage the failed blocks.
patients, but there is a learning curve. As with most regional
techniques, they are not always perfect, and it is important to have a
plan to manage the failed blocks.
There are several points of note when doing regional
anesthesia for carotid endarterectomy. First, it is important to choose
patients who understand what is expected and explain the procedure well
to them. They need to know they will be awake with little sedation,
which means they will know they are being worked on and that they will
feel touch, pressure, and temperature, but should be free from pain and
discomfort for most of the procedure. Do not be afraid to change to a
general anesthetic if when you begin the block the patient seems unduly
uncomfortable with this approach. Second, it helps if the surgeon can
complete the procedure in less than one and a half hours. Most of these
patients are elderly and have arthritis, and will get uncomfortable if
lying on a hard operating table for extended periods. Third, it is
important that the surgeon be prepared to supplement the block with
additional local anesthetic. There are two areas where this may be
necessary. First, there are areas of overlap of unanesthetized
dermatomes coming from the contralateral side, and because the incision
comes close to the midline, it may be necessary to add additional
local. Also, structures inside the carotid sheath receive innervation
from the cranial nerves IX and X. If painful for the patient when the
carotid sheath is entered, this can be eliminated by topical
administration of local anesthetic to the area. If bradycardia becomes
a problem with traction on the carotid sinus, then local anesthetic to
that area can help. At the completion of the procedure and in the
recovery room, it is important to control the blood pressure, as
improved blood supply to the affected side can produce some mild
cerebral edema and confusion if the blood pressure is too high.
anesthesia for carotid endarterectomy. First, it is important to choose
patients who understand what is expected and explain the procedure well
to them. They need to know they will be awake with little sedation,
which means they will know they are being worked on and that they will
feel touch, pressure, and temperature, but should be free from pain and
discomfort for most of the procedure. Do not be afraid to change to a
general anesthetic if when you begin the block the patient seems unduly
uncomfortable with this approach. Second, it helps if the surgeon can
complete the procedure in less than one and a half hours. Most of these
patients are elderly and have arthritis, and will get uncomfortable if
lying on a hard operating table for extended periods. Third, it is
important that the surgeon be prepared to supplement the block with
additional local anesthetic. There are two areas where this may be
necessary. First, there are areas of overlap of unanesthetized
dermatomes coming from the contralateral side, and because the incision
comes close to the midline, it may be necessary to add additional
local. Also, structures inside the carotid sheath receive innervation
from the cranial nerves IX and X. If painful for the patient when the
carotid sheath is entered, this can be eliminated by topical
administration of local anesthetic to the area. If bradycardia becomes
a problem with traction on the carotid sinus, then local anesthetic to
that area can help. At the completion of the procedure and in the
recovery room, it is important to control the blood pressure, as
improved blood supply to the affected side can produce some mild
cerebral edema and confusion if the blood pressure is too high.
P.163
Contraindications (absolute and relative)
-
Patient refusal
-
Patients that are confused and cannot cooperate
-
Patients with an uncontrollable cough
-
Patients that cannot lie flat
-
Patients with a high bifurcation of the common carotid requiring excessive retraction for surgical exposure
Anatomic Considerations
Anesthesia for carotid endarterectomy can be adequately
supplied by blocking cervical nerves 2, 3 and 4. These nerves supply
the area from behind the head down to the clavicle. Also, there is some
overlap of dermatomes from the contralateral side. In addition, the
third division of the trigeminal nerve supplies sensation down to the
superior surface of the mandible. Lastly, the structures within the
carotid sheath are supplied by cranial nerves IX and X.
supplied by blocking cervical nerves 2, 3 and 4. These nerves supply
the area from behind the head down to the clavicle. Also, there is some
overlap of dermatomes from the contralateral side. In addition, the
third division of the trigeminal nerve supplies sensation down to the
superior surface of the mandible. Lastly, the structures within the
carotid sheath are supplied by cranial nerves IX and X.
The roots of the cervical nerves emerge superior to the
transverse process of each cervical vertebra. The superficial plexus
emerge form the border of the posterior border of the
sternocleidomastoid muscle, the majority arising from the midpoint.
transverse process of each cervical vertebra. The superficial plexus
emerge form the border of the posterior border of the
sternocleidomastoid muscle, the majority arising from the midpoint.
Supplies
-
Mayo stand and sterile cover
-
Three sterile towels
-
Prep solution
-
Cup for local anesthetic
-
Package of 4 × 4 sterile sponges
-
Three 5-cc syringes
-
One 10-cc syringe
-
Three 22-gauge × 1.5-in needles
-
One 25-gauge or smaller needle
-
One short extension tubing
-
One 20-cc vial of lidocaine 1.5% with 1/400,000 epi
-
One 20-cc vial of lidocaine 1% plain
Sedation
It is important not to oversedate the patient. The
patient must be awake enough to follow commands, indicating adequate
cerebral blood flow. A combination of benzodiazepines and narcotics can
be titrated to a desired effect. In the elderly benzodiazepines may
result in restlessness and confusion.
patient must be awake enough to follow commands, indicating adequate
cerebral blood flow. A combination of benzodiazepines and narcotics can
be titrated to a desired effect. In the elderly benzodiazepines may
result in restlessness and confusion.
Technique
Step 1
The patient is placed on the table with the head slightly extended and turned to the contralateral side.
P.164
 |
|
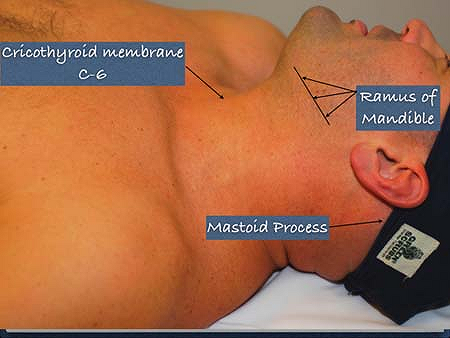
Figure 16-1. Anatomic landmarks.
|
 |
|
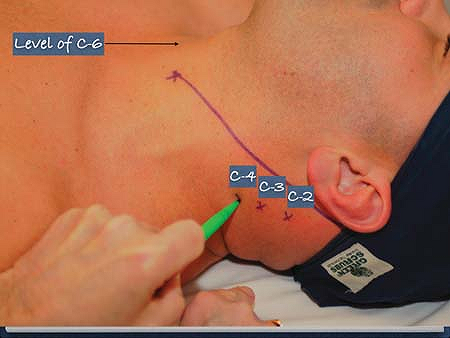
Figure 16-2. Location of C-2, C-3, and C-4.
|
A line is drawn from the mastoid process, to a point
located two fingerbreadths lateral to the midline of the cricothyroid
membrane (a point representing the transverse process of C-6) (Fig. 16-1).
located two fingerbreadths lateral to the midline of the cricothyroid
membrane (a point representing the transverse process of C-6) (Fig. 16-1).
Step 2
To locate C-2, a point is marked two fingerbreadths
caudal to the mastoid process along a line approximately 30° to the
previous line. C-3 and C-4 are located one fingerbreadth respectively
along that line as shown in Figure 16-2.
caudal to the mastoid process along a line approximately 30° to the
previous line. C-3 and C-4 are located one fingerbreadth respectively
along that line as shown in Figure 16-2.
Step 3
The neck is prepped and draped.
Step 4
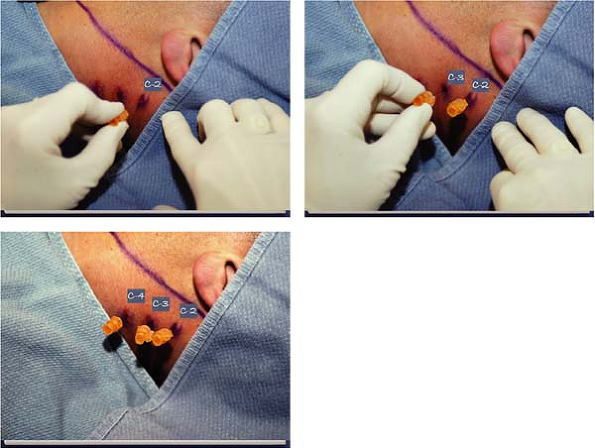
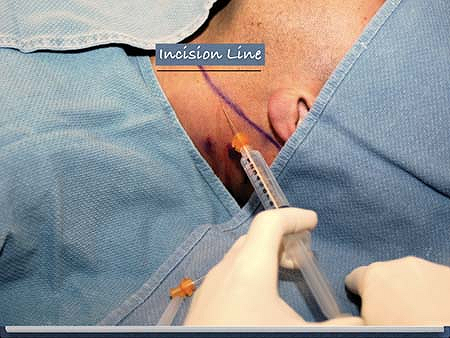
A skin wheal is raised at C-2, C-3, and C-4, with lidocaine 1%, (Figs. 16-3 through 16-5) followed by subcutaneous injections at the same levels.
Step 5
A 22-gauge needle is inserted at C-2, C-3, and C-4,
(slightly anterior and cephalad), deep to the transverse process of the
respective levels and then pulled back 1 to 2 mm.
(slightly anterior and cephalad), deep to the transverse process of the
respective levels and then pulled back 1 to 2 mm.
Step 6
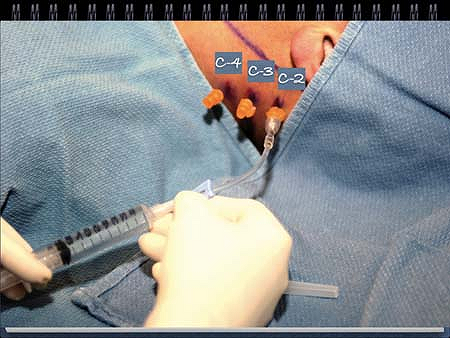
Next, C-2, C-3, and C-4 are blocked by attaching a
syringe with a short extension and after negative aspiration, injecting
6 cc of lidocaine 1.5% with 1/400,000 of epinephrine at each level (Fig. 16-6).
syringe with a short extension and after negative aspiration, injecting
6 cc of lidocaine 1.5% with 1/400,000 of epinephrine at each level (Fig. 16-6).
Step 7
Next, the superficial portion of the block is carried out by injecting subcutaneously along the incision line (Fig. 16-7).
It is also necessary to inject along the inferior border of the
mandible to include that sensation supplied by the V-3 portion of the
trigeminal nerve.
It is also necessary to inject along the inferior border of the
mandible to include that sensation supplied by the V-3 portion of the
trigeminal nerve.
P.165
 |
|
Figures 16-3 through 16-5.
A needle is inserted at C-2, C-3, and C-4 deep to the transverse process of the respective levels and then pulled back 1 to 2 mm. |
 |
|
Figure 16-6.
C-2, C-3, and C-4 are blocked by attaching a syringe with a short extension and after negative aspiration, injecting 6 cc of lidocaine 1.5% with 1/400,000 of epinephrine at each level. |
 |
|
Figure 16-7. The superficial portion of the block is carried out by injecting subcutaneously along the incision line.
|
P.166
-
Patient selection is important.
Cooperation is mandatory and therefore sedation is kept to a minimum
and titrated to effect. Benzodiazepines in the elderly may have the
opposite effect. -
Oxygen by nasal cannula is often better tolerated than by face mask. Monitoring as for any other major procedure is mandatory.
-
Since it is possible to block the phrenic
nerve, only one side should be blocked at a time; patients with severe
COPD should be watched closely. -
Complications are rare, but significant
should they occur. The vertebral artery and subarachnoid space lie in
close proximity. Therefore, an intravascular or subarachnoid injection
is possible with CNS toxicity and either seizure activity, cardiac
instability, or a total spinal occurring. -
During clamping of the carotid artery, it
is important to communicate closely with the patient for signs of
altered or loss of consciousness. If this occurs, it will be necessary
to unclamp and place a shunt. -
Proper control of hemodynamics should
occur preoperatively, making intraoperative and postoperative
management of blood pressure easier. -
Postoperatively it is important to
control hypertension. Because of improved blood flow to the operative
side, excessive hypertension may produce mild cerebral edema and
confusion.
P.167
A. Cervical Plexus Block: Revisited One-Puncture Technique
Marco Barone
Pierre Diemunsch
The puncture site is located along the posterior border of the
sternocleidomastoid (SCM) muscle, midway between the mastoid and
clavicle (Fig. 16-8). An injection of local anesthetic, internally to the fascia superficialis, diffuses through the fascia prevertebralis, determining a superficial and deep cervical plexus block.
The needle is inserted perpendicular to the skin for all its length
(1.5 cm), avoiding muscular (SCM) or vascular (external jugular vein)
puncture, without looking for any paresthesia or any bony contact. The
volume of 10 to 15 mL of the chosen local anesthetic is injected over 5
min with multiple aspiration tests and maintenance of verbal contact
with the patient.
This block is systematically associated with the
subcutaneous infiltration (10–15 mL of local anesthetic) of the
incision line as previously drawn by the surgeon.
subcutaneous infiltration (10–15 mL of local anesthetic) of the
incision line as previously drawn by the surgeon.
-
A needle longer than 1.5 cm may be necessary for morbidly obese patients.
-
Transitory disturbance of phonation and
deglutition, phrenic paralysis, and sensitive or motor brachial block
are undesired but usual effects of local anesthetic diffusion.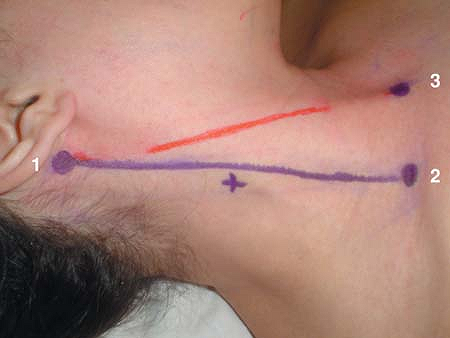 Figure 16-8. Surface landmarks. (1) mastoid; (2) clavicular insertion of the SCM muscle; (3) sternal insertion of the SCM muscle; cross, site of puncture. In red, the incision line.
Figure 16-8. Surface landmarks. (1) mastoid; (2) clavicular insertion of the SCM muscle; (3) sternal insertion of the SCM muscle; cross, site of puncture. In red, the incision line. -
Despite a relatively long onset time, long-acting local anesthetics offer the advantage of an excellent postoperative analgesia.
-
Additional local anesthetic can be administered topically during the surgery (e.g., before or during the adventitia dissection), as necessary.
-
The single-puncture technique offers the
advantage of reduced risk of complications that may result from the
successive injections used in multipuncture techniques.
P.168
Suggested Readings
Mehta
Y, Juneja R. Regional analgesia for carotid artery endarterectomy by
Winnie’s single-injection technique using a nerve detector. J Cardiothorac Vasc Anesth 1992;6:772–773.
Y, Juneja R. Regional analgesia for carotid artery endarterectomy by
Winnie’s single-injection technique using a nerve detector. J Cardiothorac Vasc Anesth 1992;6:772–773.
Pandit JJ, Dutta D, Morris JF. Spread of injectate with superficial cervical plexus block in humans: an anatomical study. Br J Anaesth 2003;91:733–735.
Sardanelli
F, Fausto A, D’Orta G, et al. Local distribution of a low dose of
anesthetic for cervical plexus block in carotid endarterectomy. Rivista di Neuroradiologia 2004;17:145.
F, Fausto A, D’Orta G, et al. Local distribution of a low dose of
anesthetic for cervical plexus block in carotid endarterectomy. Rivista di Neuroradiologia 2004;17:145.
Stoneham MD, Knighton JD. Regional anaesthesia for carotid endarterectomy. Br J Anaesth 1999;82:910–919.
Winnie AP, Ramamurthy S, Durrani Z, Radonjic R. Interscalene cervical plexus block: a single-injection technique. Anesth Analg 1975;54:370–375.
