Hand Fractures Fracture-Dislocations
Authors: Doyle, James R.
Title: Hand and Wrist, 1st Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > Section III – Emergency Department > 9 – Hand Fractures Fracture-Dislocations
9
Hand Fractures Fracture-Dislocations
This chapter will discuss the general principles of
treating fractures of the phalanges and metacarpals and of treating
fracture-dislocations in the hand. Fractures of the hand are relatively
common, and are second in incidence to lacerations of the hand.
treating fractures of the phalanges and metacarpals and of treating
fracture-dislocations in the hand. Fractures of the hand are relatively
common, and are second in incidence to lacerations of the hand.
Treatment goals include restoring the bony anatomy, and
leaving it with acceptable alignment, length, and rotation.
Dislocations and ligament injuries in the hand are presented in Chapter 10.
leaving it with acceptable alignment, length, and rotation.
Dislocations and ligament injuries in the hand are presented in Chapter 10.
General Principles
Although restoration of the original anatomic
configuration is the goal of treatment, it should not be obtained at
the risk of soft-tissue scarring and joint stiffness, or at the risk of
altering the blood supply to the bone. This may result in non-union.
configuration is the goal of treatment, it should not be obtained at
the risk of soft-tissue scarring and joint stiffness, or at the risk of
altering the blood supply to the bone. This may result in non-union.
Fractures in the hand are considered to be stable or unstable.
Stable fractures may require minimal immobilization, whereas unstable
fractures may require special immobilization techniques and or internal
fixation. Unstable fractures of the metacarpal diaphysis most often
angulate with the apex dorsal whereas fractures of the midaspect of the
proximal phalanx angulate with the apex volar. The action of the wrist
extensors that insert proximally extend the proximal portion of the
metacarpal, and the interosseous muscles and the long-finger flexors
flex the distal segment. Unstable fractures of the proximal phalanx are
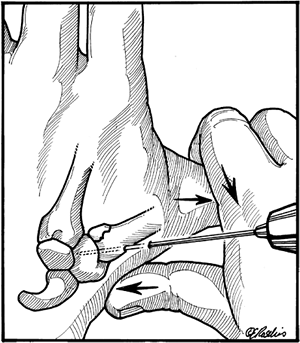
deformed by the extensor mechanism and the intrinsic muscles (Figure 9-1).
Stable fractures may require minimal immobilization, whereas unstable
fractures may require special immobilization techniques and or internal
fixation. Unstable fractures of the metacarpal diaphysis most often
angulate with the apex dorsal whereas fractures of the midaspect of the
proximal phalanx angulate with the apex volar. The action of the wrist
extensors that insert proximally extend the proximal portion of the
metacarpal, and the interosseous muscles and the long-finger flexors
flex the distal segment. Unstable fractures of the proximal phalanx are
deformed by the extensor mechanism and the intrinsic muscles (Figure 9-1).
The classic fracture deformities described above are not
representative of all fracture deformities that may be seen, but they
do serve to introduce the concept that unstable fractures angulate and
deform.
representative of all fracture deformities that may be seen, but they
do serve to introduce the concept that unstable fractures angulate and
deform.
Diagnosis
Patient History
-
The history of injury
with a hand fracture is usually straightforward, but fractures
associated with a laceration over the metacarpophalangeal (MCP) or
proximal interphalangeal (PIP) joints should raise the question of a
human bite wound that requires a different treatment approach. -
To treat a human bite wound, refer to the section of Chapter 5 that deals with human bite wounds.
Physical Examination
-
Physical signs of fracture include swelling, tenderness, ecchymosis, skin abrasions, and deformity—including malrotation.
-
Fractures may be associated with
collateral ligament injuries, tendon avulsion, and nerve or vascular
injury. These structures should be evaluated by physical examination.
Radiologic Examination
-
Posterior-anterior, lateral, and oblique x-ray views are obtained, along with accurate lateral profile views of the phalanges.
-
Comparison views of the uninjured hand or digit are obtained as needed.
Treatment
Closed Treatment
-
Closed treatment and external forms of immobilization are best used in stable rather than unstable fractures.
-
Stability is defined in this context as the maintenance of reduction following manipulation and external immobilization.
This concept is amplified by noting that a transverse fracture is intrinsically more stable than an oblique fracture.
Techniques of Closed Reduction
-
The following comments about closed
reduction are most appropriately applied to stable fractures of the
diaphysis of the middle and proximal phalanges, and the diaphysis
P.129of the metacarpals. They apply to fractures that are stable (usually transverse fractures) and reducible.
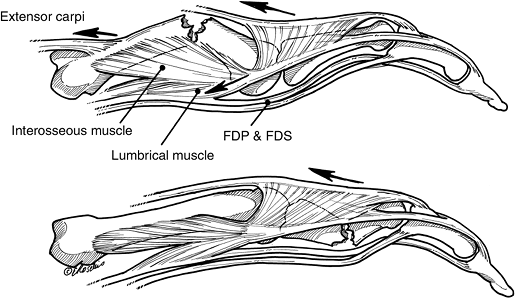 Figure 9-1 Classic fracture deformity in unstable fractures of the metacarpals and phalanges (see text for details).
Figure 9-1 Classic fracture deformity in unstable fractures of the metacarpals and phalanges (see text for details). -
Specific fractures of a more problematic
nature that require operative intervention or special techniques will
be discussed later.
Proximal and Middle Phalanges
-
Anesthesia prior to fracture reduction in the hand may be achieved by appropriate nerve blocks. Refer to Chapter 8.
-
Following suitable anesthesia, longitudinal traction is performed, followed by correction of the deformity.
-
This axial traction may be aided by the
use of finger traps, and the entire procedure is performed most
comfortably for the patient and surgeon by having the patient lay
supine with the elbow flexed to 90 degrees. -
In digital fractures, the potentially deforming forces of the intrinsics are relaxed by flexion of the MCP joints.
-
Wrist extension facilitates flexion of the MCP joints and longitudinal traction of the finger or fingers.
-
After reduction, stability of the reduction is determined along with rotational alignment.
-
Rotational alignment is evaluated by
“sighting” down the plane of the finger nails (from distal to proximal)
to note the relative tilt of the nail plate of the injured finger in
comparison to the adjacent fingers and using the uninjured hand for
comparison as needed. -
Rotation may also be checked by noting absence of “crossing over” of the digit during flexion, and by noting its normal parallel alignment with the adjacent fingers.
-
Post reduction radiographs are made in sufficient number and detail to verify and document the reduction.
-
Depending on the digits fractured, a radial or ulnar gutter splint is used to immobilize the injured digits.
-
The so-called intrinsic plus position is utilized with the wrist in extension, the MCP joints in 90 degrees of flexion, and the PIP joints in extension.
-
Ninety degrees of flexion at the MCP
joints may not always be achieved. It has been noted that 60 degrees of
flexion of the MCP joint may be adequate. -
This position results in relaxation of
the potential deforming force of the intrinsic muscles, and avoids
contracture of the collateral ligaments of the MCP and PIP joints. -
An alternative to the radial or ulnar
gutter splint is to immobilize the wrist and hand in extension, and
place the reduced digit on an outrigger splint with the MCP joint
flexed to 90 degrees and the PIP joint in extension. -
This method allows visual evaluation of the alignment; this may be confirmed as indicated by radiograph (Figure 9-2).
-
Protected motion of the fractured digit
may begin at 3 to 4 weeks after reduction, with continued splinting as
needed and based on the experience of the surgeon. -
In selected patients, some minimally
displaced, stable, and suitably aligned fractures of the proximal and
middle phalanges may be treated by strapping the injured digit to an
adjacent finger and allowing early protected motion. -
Appropriate x-ray views should be
obtained 1 week or less after reduction, and weekly or biweekly
thereafter based on the fracture and the experience of the surgeon.
P.130
Metacarpal Fractures
-
The same comments about patient positioning and anesthesia apply as noted for phalangeal fractures.
-
The wrist is extended, and longitudinal
traction achieved by grasping the flexed proximal phalanx as a lever
for distal traction and aligning and rotating the distal segment of the
metacarpal. -
A “cobra” splint or cast may be used to
immobilize these fractures with the wrist in extension and the MCP
joints flexed 80 to 90 degrees (Figure 9-3). -
The PIP joints are left free for flexion;
if malrotation is a potential problem, the injured digit may be taped
to an adjacent uninjured digit. -
Splinting may be performed for 3 to 4 weeks based upon the nature of the fracture and the experience of the surgeon.
 |
|
Figure 9-2
Artist’s depiction of a Bohler-type outrigger splint used for postreduction immobilization of fractures of the proximal and middle phalanges. |
Early Motion in Hand Fractures
-
Fractures that are secondary to
high-energy trauma, such as crush injuries or those associated with
joint injuries, are more likely to develop residual stiffness and loss
of function. -
Early mobilization and measures to reduce
edema (elevation of the injured part) may be useful adjuncts to avoid
this complication.-
Think of edema and swelling as internal glue that is associated with stiffness.
-
-
True elevation of the hand requires it to
be 30 cm or higher than the level of the heart. This is best achieved
by lying down and elevating the hand on some form of support. -
Maintaining the hand in an arm sling (although better than letting the hand hang at the side) is not elevation.
 Figure 9-3
Figure 9-3
An example of a “cobra cast” used to immobilize a fracture of the
metacarpal. The carefully padded cast is molded to the contours of the
hand and the position of the wrist and MCP joints neutralize the
deforming force of the interosseous muscles. -
Early motion is believed to lessen
harmful adhesions of the soft tissues, including the extensor and
flexor tendon systems and joint capsules. -
Early motion along with proper joint positioning may lessen these complications.
-
Some surgeons have noted that
immobilization of fingers beyond 4 weeks will lead to long-term
stiffness due to tendon adhesions and joint contracture.-
Thus, fractures treated with closed
reduction and splinting are usually mobilized after 3 to 4 weeks, even
in the absence of osseous union by radiograph.
-
-
Stability of the fracture at this stage is due to fibrous union that most often proceeds to osseous union.
-
In general, only splint the joints that are absolutely needed, in order to allow early motion of uninjured joints.
-
The PIP joint does not need to be immobilized in fractures of the distal phalanx or distal interphalangeal (DIP) joint.
Open Treatment
-
The indication for closed versus open
reduction may depend on many factors, including the special needs of
the patient and the experience and preferences of the surgeon. -
Fractures with articular step-off, open
fractures (especially in those with bone loss and significant
soft-tissue injury), fractures with significant shortening or bone
loss, and fractures that fail closed reduction are indications for
surgical treatment. -
Other surgical indications include
multiple fractures, fractures that are intrinsically unstable,
fractures with rotational malalignment as seen in spiral and oblique
fractures, and fractures associated with joint subluxation or
dislocation. -
Internal fixation should be achieved with
minimal soft-tissue disruption in order to limit scarring and
disruption of the blood supply of the fractured bone. -
Ideally, the fixation should be rigid enough to allow immediate active motion.
-
If this is not possible, protected motion
should begin as soon as possible based upon the nature of the fracture
and the surgeon’s experience. -
Surgical intervention may be associated with stiffness unless early mobilization is used.
-
Minimum surgical dissection will favor recovery of motion.
-
Many fractures that require reduction and fixation can be treated with percutaneous fixation techniques.
-
Phalangeal fractures treated with plates
and screws (most likely because of wider surgical dissection) have a
higher incidence of stiffness. -
Percutaneous fixation can be performed with Kirschner wires.
-
Screws may be placed in selected cases through limited incisions.
-
Oblique fractures are prone to rotational
malalignment, and stabilization is achieved by compression screws or
0.045-inch Kirschner wires placed perpendicular to the fracture line. -
The fixation devices are positioned to avoid compromise to the tendons, so that early motion is not compromised.
-
Figure 9-4 demonstrates an unstable spiral-oblique fracture of the proximal phalanx fixed with two miniscrews.
-
The fracture was exposed through a
longitudinal incision in the extensor tendon, which gave excellent
exposure; this stable construct allowed protected motion early. -
The aftercare and supervised rehabilitation program is very important to achieve maximum recovery and function.
-
Dynamic external fixation methods have
been developed for treatment of difficult articular fractures,
especially about the PIP joint. -
These methods are technically challenging but may be used based on the surgeon’s experience and preference.
-
Operating room fluoroscopy units are useful aids in reduction and placement of fixation devices.
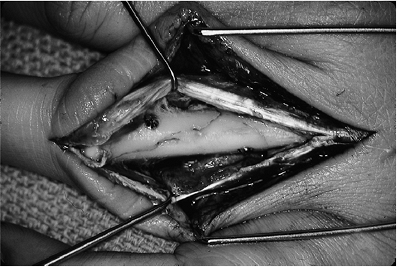
![]() Figure 9-4
Figure 9-4
An unstable, spiral-oblique fracture of the proximal phalanx exposed
through an extensor tendon splitting approach and fixed with two mini
screws. -
Arthroscopic evaluation of joint surfaces
has allowed some surgeons to more accurately reduce and fix certain
intra-articular fractures.
P.131
Some Caveats about Kirschner Wires
-
Kirschner wires should be placed with understanding that they will be removed at some point in the future.
-
They may be cut off beneath the skin, or left protruding from the skin for ease of removal.
-
Infection may be avoided by keeping the exit sites of the K-wires clean and dry.
-
Inappropriately placed K-wires may damage vital structures such as nerve, blood vessel, or tendon.
-
They should be placed so that soft-tissue gliding may occur during rehabilitation, without any impingement or compromise to the soft tissues.
-
K-wires that cross joints may break, and their broken ends may erode and damage articular cartilage.
-
When broken in this manner they are difficult to remove without causing additional joint damage.
-
-
Transarticular K-wires should be protected with a splint or cast until their timely removal.
-
Making a right-angle bend on the exposed
end of the K-wire and cutting it off about 2 to 3 mm beyond the bend
may prevent excessive migration. In some instances, this facilitates
removal. -
Threaded K-wires are prone to “wrap-up” adjacent soft tissues; for that reason, smooth wires are preferred.
Specific Fractures Phalanges Metacarpals
Distal Phalanx
Fractures of the Tuft
-
Fractures of the distal phalanx are the most common hand fracture.
-
Tuft fractures are usually due to a crush
injury, and are often associated with a subungual hematoma and
sometimes a nail bed laceration. -
Initial treatment consists of drainage of the subungual hematoma, if present.
-
In patients with a disrupted nail and
significant laceration or disruption of the nail bed, consider
repairing the underlying nail bed with fine absorbable sutures. -
If a suitable nail plate is present, it may be replaced as a biologic stent.
-
Splinting of the DIP joint for 2 to 3
weeks may protect the soft-tissue injury and give symptomatic relief
for the fracture. Nonunion of one or more fracture fragments is common,
and requires no particular treatment.
Fractures of the Shaft
-
Fractures of the diaphysis may be transverse or longitudinal.P.132
 Figure 9-5 Clinical and x-ray appearance of a displaced fracture of the proximal metaphysis of the distal phalanx with K-wire fixation. A. Note the displaced fingernail. B. Radiographs showing displacement of the fracture. C. Longitudinal K-wire fixation.
Figure 9-5 Clinical and x-ray appearance of a displaced fracture of the proximal metaphysis of the distal phalanx with K-wire fixation. A. Note the displaced fingernail. B. Radiographs showing displacement of the fracture. C. Longitudinal K-wire fixation. -
Most are minimally displaced and respond
well to 2 to 3 weeks of DIP joint splinting. Fractures from high-energy
injuries may damage the germinal matrix.
Fractures of the Proximal Metaphysis
-
These injuries often displace the
proximal nail from its bed, and the nail should be anatomically reduced
and held in place with sutures. A transfracture K-wire may be used to
stabilize the fracture, and is often more advantageous in maintaining
the reduction (Figure 9-5).
Fractures of the Base of the Distal Phalanx
-
Three types of these fractures exist. See Table 9-1.
Type I
-
The extensor mechanism is attached to the
basal epiphysis, and closed reduction of the fracture results in
correction of the deformity. -
Continuous external splinting of the
distal joint in full extension for 3 to 4 weeks results in union of the
fracture and correction of the deformity.
Type II
-
This fracture is not to be confused with
the more common small bone fragment associated with a tendon avulsion
and mallet-finger deformity that is treated as a soft-tissue injury. -
Operative treatment has been recommended for fracture fragments involving more than one-third of the articular surface.Table 9-1 Types of Fractures of the Base of the Distal Phalanx
Type Description I. Transepiphyseal fracture as seen in children. II. Hyperflexion injury
that usually results in a fracture of the articular surface that
involves 20–50% of the articular surface (the so-called mallet
fracture).III. Hyperextension injury
with fracture of the articular surface that usually involves >50% of
the articular surface and is sometimes associated with late volar
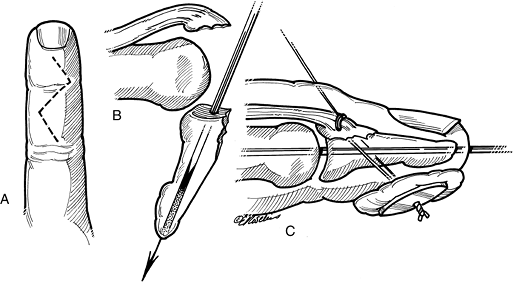
subluxation of the distal phalanx.P.133![]() Figure 9-6 Artist’s depiction of a method to reduce and fix a mallet fracture. A. A zigzag dorsal incision is used to expose the fracture. B. A 0.035-inch, double-ended K-wire is drilled longitudinally through the distal phalanx. C.
Figure 9-6 Artist’s depiction of a method to reduce and fix a mallet fracture. A. A zigzag dorsal incision is used to expose the fracture. B. A 0.035-inch, double-ended K-wire is drilled longitudinally through the distal phalanx. C.
The joint is reduced, the K-wire is driven proximally across the joint,
and the fracture fragment is reduced. If the fracture fragment cannot
be maintained in position, a loop of 4-0 wire is passed through the
fragment and distal phalanx and is tied over a padded button.
Intraoperative radiographs are made to determine anatomic reduction.
The transarticular K-wire is protected with a splint for 6 weeks. The
pullout wire may be removed in 3 or 4 weeks. -
An accurate reduction is advocated to prevent joint deformity with secondary arthritis and stiffness.
-
This fracture may be treated as depicted in Figure 9-6.
-
The reader should note that this is a technically challenging operation, and not all surgeons recommend its use.
-
Many surgeons advise closed splinting for this injury.
-
Operative repair of a mallet fracture is a technically difficult operation.
-
Attempted fixation of the fracture
fragment by K-wire or wire loop may result in comminution of the
fragment and loss of attachment of the extensor mechanism.
Type III
-
Figure 9-7 shows a radiograph of a type III hyperextension injury.
-
Treatment for this fracture is the same as for type II fractures.
-
Both type I and II injuries have been
treated successfully by closed means, and the reader is advised to note
the following caveats regarding this fracture.
Caveats
-
Wehbe and Schneider recommended
nonoperative treatment by extension splinting of all mallet fractures,
including the hyperextension type with subluxation of the distal phalanx. Figure 9-7 Lateral x-ray view of a type III mallet finger fracture (see text for details).
Figure 9-7 Lateral x-ray view of a type III mallet finger fracture (see text for details). -
They believe that restoring joint
congruity does not influence the end result, because remodeling of the
articular surface is reported to lead to a near-normal painless joint
in spite of persistent joint subluxation. -
A further caveat about hyperextension mallet fractures with volar subluxation is that splinting of the deformity in hyperextension at the DIP joint should be avoided to prevent volar subluxation of the distal phalanx.
Middle Phalanx
Nondisplaced and Extra-Articular Fractures
-
Most nondisplaced extra-articular fractures can be treated with buddy taping for 3 to 4 weeks.
-
Spiral fractures or others with potential
for instability may be splinted for 3 to 4 weeks, with timely follow-up
including radiographs. -
If displacement occurs, the fractures should be treated as noted for unstable displaced fractures (see discussion that follows).
Displaced and Articular Fractures
-
Displaced fractures should be considered
to be intrinsically unstable, and even when anatomically reduced they
may redisplace. This is especially true in oblique or comminuted
fractures.
Dorsal Fracture Subluxation of the PIP Joint
-
This fracture involves the volar aspect
of the articular surface of the base of the middle phalanx, and is one
of the most disabling injuries to the finger. -
Diagnosis and treatment are often delayed.
-
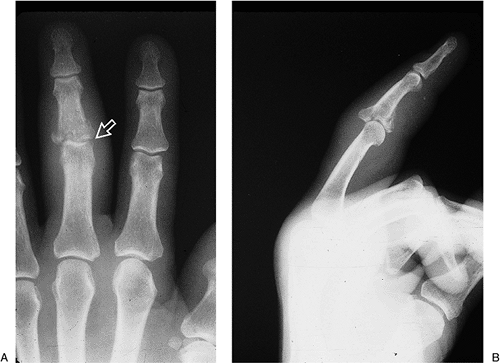
Figure 9-8 demonstrates the x-ray appearance of such an injury.
-
These comminuted and unstable fractures may be treated by some form of dynamic traction that maintains reduction and allows simultaneous movement of the injured joint.
-
Another treatment option is that of dorsal block splinting, in which the PIP joint is reduced and held in the degree
P.134of flexion that results in and maintains a concentric reduction.
![]() Figure 9-8 X-ray appearance of a comminuted and displaced fracture subluxation of the base of the middle phalanx.
Figure 9-8 X-ray appearance of a comminuted and displaced fracture subluxation of the base of the middle phalanx. -
Active flexion of the joint is performed and the dorsal blocking splint gradually extended over a 4 to 5 week period.
-
When seen late, these injuries may be salvaged by a volar plate arthroplasty.
-
An example of a similar injury in the
proximal phalanx of the thumb demonstrates the use of balanced dynamic
traction to treat such an injury (Figure 9-9).-
This method requires careful monitoring and balancing of the forces involved.
-
-
Some surgeons may elect to treat this
injury by a thumb spica cast or splint, and others may choose an open
reduction and fixation with K-wires, plates and/or screws. -
These first two examples are contrasted to an unstable fracture-dislocation of the PIP joint with a relative large and non-comminuted fragment that can be reduced and fixed.
-
Such an anatomic reduction is stable and with early protected motion, an excellent outcome may be anticipated (Figure 9-10).
Proximal Phalanx
Peri-Articular Fractures
At the PIP Joint
-
Fractures that involve the articular
surface of the proximal phalanx at the PIP joint are intrinsically
unstable. If they are not reduced and internally stabilized, deformity
and arthrosis will result. -
Figure 9-11 demonstrates a neglected oblique fracture of the proximal phalanx that healed with an articular offset and subsequent deformity. A realignment osteotomy corrected the deformity.
At the MCP Joint
-
Fractures of the articular surface of the
proximal phalanx at the MCP joint are best treated by internal fixation
followed by protected early motion. Figure 9-12 demonstrates such a case.
Diaphyseal Fractures of the Proximal Phalanx
-
Injuries at this level are prone to
angulate with the apex volar due to the action of the intrinsic muscles
and extensor mechanism. -
Treatment by closed means, or internal
fixation with K-wires or screws, is based on the anticipated stability
of the fracture and the preferences of the surgeon. -
Reduction of phalangeal fractures is
performed by flexing the MCP joint to relax the intrinsic muscles,
followed by axial traction, digital pressure, and accentuation of the
deformity to disengage the fracture fragments as needed.
Metacarpal
Fractures of the Neck
-
These injuries are relatively common, and most often involve the little finger metacarpal.
-
They often occur from punching various things with a tightly clenched fist, and the eponym boxer’s fracture is often used to describe these injuries.P.135
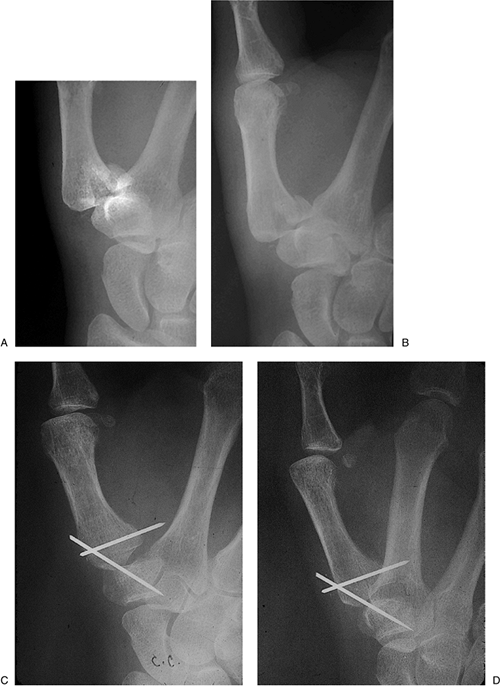
 Figure 9-9 A dynamic traction method for treatment of a comminuted and displaced fracture of the proximal phalanx of the thumb. A, B. Pretreatment x-ray appearance; note the comminution and volar subluxation of the proximal phalanx. C.
Figure 9-9 A dynamic traction method for treatment of a comminuted and displaced fracture of the proximal phalanx of the thumb. A, B. Pretreatment x-ray appearance; note the comminution and volar subluxation of the proximal phalanx. C.
The traction device in place demonstrating a “dorsal lifting” K-wire in
the base of the proximal phalanx, and a longitudinal traction K-wire in
the distal phalanx. Traction was achieved by rubber bands between the
outrigger device and the K-wires. The device was left in place for 6
weeks. (D–E) The x-ray appearance of the fracture at 3 months.P.136![]() Figure 9-10 A noncomminuted but unstable volar lip fracture-dislocation of the base of the proximal phalanx that is amenable to fixation.
Figure 9-10 A noncomminuted but unstable volar lip fracture-dislocation of the base of the proximal phalanx that is amenable to fixation. -
Some surgeons consider all of these fractures as stable and impacted ones that are not easily reduced.
-
Patients do not always present in a
timely fashion, and if seen even after 7 to 10 days, these fractures
may be impossible to move even under appropriate anesthesia and
vigorous manipulation. -
The most controversial aspect of these injuries is determining which require treatment.
-
The basis of treatment for surgeons who
treat these more aggressively is determined by the degree of angulation
of the fracture as noted on a radiograph. The published acceptable
ranges of deformity vary with the finger involved.-
The little finger appears to tolerate a
flexion deformity at the metacarpal neck better than the other fingers
due to its hypermobility. -
Thirty degrees of flexion seems to have no appreciable effect on function in biomechanical studies.
-
Some authors will allow up to 50 degrees of angulation, while others allow up to 70 degrees.
-
-
It has been argued that laborers and athletes that grip bats or racquets may be candidates for more aggressive management.
-
Treatment of these fractures is based on
the surgeon’s experience and the perceived needs of the patient. Most
single-bone fractures are treated by closed reduction and some level of
immobilization. -
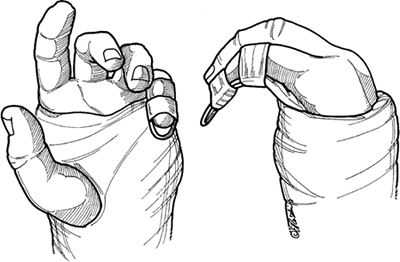
Figure 9-13 demonstrates a useful technique for reduction.
-
It is performed by using the cup or
proximal articular surface of the proximal phalanx as a “pusher” to
reduce the volar flexed aspect of the head and neck of the metacarpal.
-
-
Multiple displaced fractures may indicate more aggressive treatment.
-
In single bone fractures, two parallel
percutaneous pins that pass through the reduced distal aspect of the
fracture into the adjacent metacarpal keep the fracture in alignment,
are minimally invasive, and are easily removed. -
Figure 9-14 shows a patient with significant displacement of fractures of the neck of the metacarpals of the little and ring fingers.
-
Some surgeons would suggest that open reduction and internal fixation is indicated.
-
Closed reduction would no doubt be difficult, if not impossible.
-
Fractures of the Diaphysis
-
Although the ring and little fingers may
tolerate up to 40 degrees of angulation of a fractured metacarpal shaft
due to carpometacarpal (CMC) motion at the hamate articulation, this
amount of angulation leaves a prominent bump on the back of the
hand—which most patients find unacceptable. -
Angulation beyond acceptable tolerances
requires reduction and some form of fixation or immobilization based
upon the patient’s needs and the surgeon’s preferences. -
Current thinking about the acceptable
amount of shortening in metacarpal fractures is said to have decreased
from 1 cm to less than 5 mm. -
Extensor lag associated with shortening
of the metacarpal may be accommodated by MCP hyperextension in the
absence of musculotendinous shortening. -
Although some shortening is acceptable, rotation is not.P.137
 Figure 9-11 A neglected oblique fracture of the articular surface of the neck of the proximal phalanx. A, B. Note the clinical and x-ray deformity. C. Realignment was obtained by osteotomy.
Figure 9-11 A neglected oblique fracture of the articular surface of the neck of the proximal phalanx. A, B. Note the clinical and x-ray deformity. C. Realignment was obtained by osteotomy. -
Figure 9-15 demonstrates the clinical appearance of a malrotated index finger following an open reduction and internal fixation.
-
Caveat: It does not take much rotation or malalignment at the fracture site to yield a malrotated finger.
-
Treatment of metacarpal shaft fractures may vary from a closed reduction, a well-applied cobra cast (see Figure 9-3),
and a careful follow-up including radiographs, to various forms of
fixation, including K-wires, screws, screws and plates, and external
fixation devices. -
Minimum profile plates may be used in certain cases. Figure 9-16 shows such a plate in place.
-
Soft-tissue dissection should be kept to
a minimum, and although such techniques allow early protected motion,
they should be used in carefully selected patients. -
Compression screws placed at right angles to oblique fractures may also be used.
![]() Figure 9-12 An unstable fracture at the base of the proximal phalanx. A. Note the displaced and slightly comminuted fracture at the base of the proximal phalanx. B.
Figure 9-12 An unstable fracture at the base of the proximal phalanx. A. Note the displaced and slightly comminuted fracture at the base of the proximal phalanx. B.
A single K-wire was used to fix the fragment to the phalanx, and a
longitudinal K-wire was used to stabilize the joint. The longitudinal
K-wire was removed at 3 weeks, and protected motion was started by
strapping the middle finger to the index finger. -
K-wires may be used in selected cases, either in crossed or parallel configuration.
-
Bi-cortical passage of the K-wires promotes better fixation and prevent rotation.
-
Stabilization of metacarpal fractures
with external fixators, as well as transversely oriented K-wires from
an intact metacarpal to one with a fracture or bone loss defect, may be
especially useful when severe soft-tissue injuries are present.
P.138
 |
|
Figure 9-13 Closed reduction technique for boxer’s fracture.
|
Fracture of the Finger Metacarpal Base
-
Injuries to the finger metacarpal base most often involve the ring and little fingers.
-
They are often associated with fractures of the adjacent carpal bones.
-
These fractures may be missed on routine radiographs, and the diagnosis may be aided by an oblique supination view.
-
Open reduction and internal fixation is required to restore the normal alignment of the articular surfaces of the CMC joints.
-
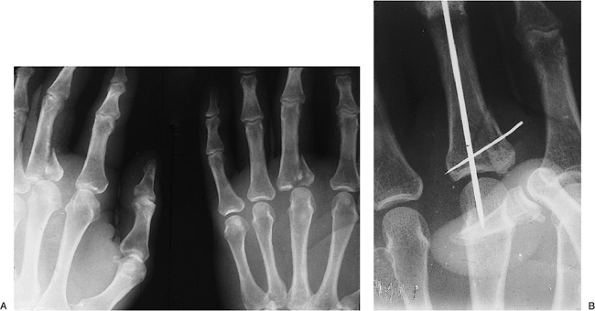
Figure 9-17 shows such an injury to the base of the little finger metacarpal and an associated fracture of the ring finger metacarpal.
-
Treatment was by open reduction and
K-wire fixation of the CMC dislocation, with parallel K-wires across
the ring finger metacarpal fracture.
-
Thumb Metacarpal
Fractures of the Diaphysis
-
Fractures of the diaphysis are relatively uncommon, and fractures about the thumb metacarpal usually involve the base.
-
The thumb has significant CMC motion, and
dorsal angulation of fractures of the diaphysis of the metacarpal may
be better tolerated than angulatory deformity in the fingers
(especially the index and middle).P.139![]() Figure 9-14 A–C. X-ray appearance in three views of severely displaced boxer’s fractures of the ring and little finger metacarpals.
Figure 9-14 A–C. X-ray appearance in three views of severely displaced boxer’s fractures of the ring and little finger metacarpals.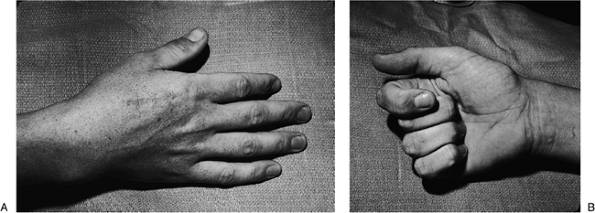 Figure 9-15 Malrotation deformity of an internally fixed index metacarpal fracture. A. Note the scar over the dorsal aspect of the index finger, and the subtle supination deformity seen in the index fingernail. B. The deformity is most pronounced during flexion. A corrective derotational osteotomy was performed.P.140
Figure 9-15 Malrotation deformity of an internally fixed index metacarpal fracture. A. Note the scar over the dorsal aspect of the index finger, and the subtle supination deformity seen in the index fingernail. B. The deformity is most pronounced during flexion. A corrective derotational osteotomy was performed.P.140![]() Figure 9-16 Intraoperative view of a miniplate and screws for treatment of a metacarpal fracture.
Figure 9-16 Intraoperative view of a miniplate and screws for treatment of a metacarpal fracture. Figure 9-17 CMC joint dislocation of the little finger and fracture of the ring finger metacarpal. A, B.
Figure 9-17 CMC joint dislocation of the little finger and fracture of the ring finger metacarpal. A, B.
X-ray appearance of the injury. Note the CMC dorsal dislocation of the
little finger metacarpal and fracture of the ring finger metacarpal.
Note also that the oblique view is more revealing than the AP view. C, D. Postoperative appearance showing anatomic reduction and fixation with K-wires. Note the bent ends of the K-wires (see text). -
Although dorsal angulation of some degree
may be functionally acceptable (some surgeons accept up to 30 degrees),
it may not always be acceptable from the patient’s perspective. -
Both closed and operative methods may be used for reduction and fixation of diaphyseal fractures, as previously described.
-
The most suitable position for
immobilization of the thumb is abduction and extension of the CMC
joint, with minimal flexion of the MCP joint and extension of the IP
joint. -
This position may be demonstrated on your
own hand by noting the posture of the thumb when it lightly touches the
tip of the semi-flexed index finger.
P.141
Fractures of the Base
-
Extra-articular
fractures of the base of the thumb metacarpal are treated like
fractures of the diaphysis, and most can be managed by closed means. -
It is the intra-articular fractures—classified as Bennett’s or Rolando’s fractures—that are most problematic and challenging for the surgeon.
Bennett’s Fracture
Pertinent Anatomy and Pathomechanics
-
The volar projection of the base of the
thumb metacarpal is firmly held to the adjacent trapezium by the
superficial anterior oblique ligament (SOAL) and the deep anterior
oblique ligament (DOAL).-
The latter is also known as the “beak ligament.”
-
-
These ligaments firmly hold the volar
projection of the thumb metacarpal in place, and in the presence of
axial loading, a fracture occurs rather than a dislocation of the CMC
joint. -
The resultant fracture is oblique and is
displaced by the proximal and dorsal pull of the abductor pollicis
longus (APL) tendon that inserts on the dorsal base of the thumb
metacarpal. -
In addition, the adductor pollicis (AP) places a radially deforming force on the metacarpal.
Diagnosis
-
This injury is most accurately diagnosed by a true lateral radiograph of the CMC joint.
-
A true lateral is obtained by placing the
radial border of the thumb flat on the x-ray plate with the wrist and
forearm pronated 15 to 35 degrees. -
Placing the wrist and hand in this
position naturally extends the wrist and hand. This position is
maintained with a foam wedge placed under the ulnar border of the hand. -
The x-ray beam is centered over the CMC joint and directed at a 15-degree angle from distal to proximal.
Treatment
-
An anatomical reduction and maintenance of that reduction is required.
-
This is an unstable fracture, and it is highly unlikely that a closed reduction can be maintained by a cast or a splint.
![]() Figure 9-18 Technique for percutaneous fixation of a Bennett’s fracture of the thumb (see text for details).
Figure 9-18 Technique for percutaneous fixation of a Bennett’s fracture of the thumb (see text for details). -
Some surgeons, however, recommend closed
reduction and casting provided a stable reduction can be maintained and
provided there is less than 1 mm displacement or articular step-off. -
Maintenance of the reduction is best
achieved by some form of fixation, either by closed percutaneous
pinning or by open reduction and fixation.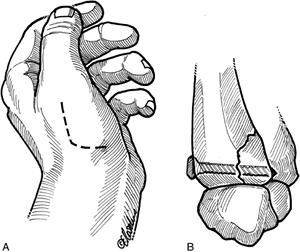 Figure 9-19 Technique for screw fixation of Bennett’s fracture. A. The incision. B. Reduction and screw fixation.P.142
Figure 9-19 Technique for screw fixation of Bennett’s fracture. A. The incision. B. Reduction and screw fixation.P.142![]() Figure 9-20 X-ray appearance of Bennett’s fracture with K-wire fixation. A, B. Prereduction appearance. C, D.
Figure 9-20 X-ray appearance of Bennett’s fracture with K-wire fixation. A, B. Prereduction appearance. C, D.
Note the anatomic reduction and K-wire fixation of the fracture
fragment, and a second transarticular K-wire across the CMC joint. Question
to the reader: What would you have done differently in terms of the cut
off ends of the K-wires? Answer: A 90-degree bend prior to cutting off
the K-wires would have prevented migration of the ends of the pins
beneath the dorsal cortex of the metacarpal and made pin removal at 6
weeks a less complex procedure. -
Some surgeons base their decision for closed versus open methods based on the size of the volar lip (articular) fragment.
-
If the fragment is less than 15% to 20% of the articular surface, closed reduction and percutaneous pinning is elected.
-
If the articular fragment is greater than 25% to 30%, open reduction is performed.
-
Management of this fracture by percutaneous fixation
is performed by longitudinal traction on the thumb, simultaneous
pressure over the dorsal aspect of the base of the thumb metacarpal,
and pronation of the thumb followed by insertion of a transarticular
K-wire across the dorsal base of the metacarpal into the trapezium (Figure 9-18).-
This construct is protected by a secure
cast or splint, the pin is removed at 5 weeks, and motion starts based
on the clinical and x-ray findings.
-
-
Open reduction is performed through a J-shaped incision that reflects the base of the thenar muscles away from the CMC joint.
-
This approach allows a profile view of the fracture and CMC joint.
-
The fracture fragment is reduced
anatomically and fixed to the main body of the metacarpal by one or two
K-wires or screws, based on the surgeon’s choice and experience. -
This construct is protected with a cast or splint, and motion is started based on the nature and stability of the fixation (Figure 9-19).
-
Figure 9-20 demonstrates the x-ray appearance of a Bennett’s fracture and its reduction and fixation with K-wires.
-
P.143
Rolando’s Fracture
-
This fracture was originally described as a fracture of the base of the thumb metacarpal with a Y- or T-shaped intra-articular component.
-
The term has now come to include any comminuted intra-articular fracture of the base of the thumb metacarpal.
Treatment
-
In those fractures that meet Rolando’s
original description, treatment is by open reduction and internal
fixation with K-wires, plates, and screws. -
In those more comminuted fractures, treatment techniques have included skeletal traction and mini-external fixators.
-
The goals of treatment for these
comminuted fractures is to maintain thumb length and as much congruity
of the articular surface as possible.
Suggested Reading
Doyle JR, Botte MJ. Surgical anatomy of the hand and upper extremity. Philadelphia: Lippincott Williams & Wilkins, 2002.
Eaton
RG, Malerich MW. Volar plate arthroplasty of the proximal
interphalangeal joint: a review of thirty years experience. J Hand Surg
1980;5:260–268.
RG, Malerich MW. Volar plate arthroplasty of the proximal
interphalangeal joint: a review of thirty years experience. J Hand Surg
1980;5:260–268.
Glickel
SZ, Barron OA, Eaton RG. Dislocations and ligament injuries in the
digits. In: Green DP, Hotchkiss RN, Pederson WC, eds. Green’s operative
hand surgery. 4th Ed. New York: Churchill Livingstone, 1999:772–808.
SZ, Barron OA, Eaton RG. Dislocations and ligament injuries in the
digits. In: Green DP, Hotchkiss RN, Pederson WC, eds. Green’s operative
hand surgery. 4th Ed. New York: Churchill Livingstone, 1999:772–808.
Gutow
AP, Slade JF, Mahoney JD. Phalangeal injuries. In Trumble T, ed. Hand
surgery update 3, hand, elbow and shoulder. Rosemont, IL: American
Society for Surgery of the Hand, 2003:1–27.
AP, Slade JF, Mahoney JD. Phalangeal injuries. In Trumble T, ed. Hand
surgery update 3, hand, elbow and shoulder. Rosemont, IL: American
Society for Surgery of the Hand, 2003:1–27.
Markiewitz
AD. Metacarpal fractures. In Trumble T, ed. Hand surgery update 3,
hand, elbow and shoulder. Rosemont, IL: Amer. Soc Surg Hand, 2003:29–35.
AD. Metacarpal fractures. In Trumble T, ed. Hand surgery update 3,
hand, elbow and shoulder. Rosemont, IL: Amer. Soc Surg Hand, 2003:29–35.
Stern
PJ: Fractures of the metacarpals and phalanges. In: Green DP, Hotchkiss
RN, Pederson WC, eds. Green’s operative hand surgery. 4th Ed. New York:
Churchill Livingstone, 1999:711–771.
PJ: Fractures of the metacarpals and phalanges. In: Green DP, Hotchkiss
RN, Pederson WC, eds. Green’s operative hand surgery. 4th Ed. New York:
Churchill Livingstone, 1999:711–771.
Wehbe MA, Schneider LH. Mallet fractures. J Bone Joint Surg 1984; 66A:658–669.