Examination of the Muscle Stretch Reflexes
– Neurologic Examination > Reflex Examination > Chapter 37 –
Examination of the Muscle Stretch Reflexes
localize neurologic pathology to the central or the peripheral nervous
system by looking for evidence of upper motor neuron or lower motor
neuron (or peripheral sensory nerve) dysfunction.
and ankles should be examined in all patients as part of a routine
neurologic examination. Testing for clonus in the ankles should be
performed when hyperreflexia is seen in the lower extremities.
the muscles that sense muscle stretch (lengthening). Tapping a tendon
with a reflex hammer causes a sudden muscle stretch that activates the
muscle spindles. The muscle spindles send a sensory impulse to the
spinal cord, which then synapses with motor neurons at that level of
the spinal cord to initiate reflex contraction of the same muscle that
was stretched. For example, tapping the left quadriceps tendon at the
knee stretches the left quadriceps muscle (and its muscle spindles),
initiating reflex contraction of the left quadriceps muscle, which is
observed clinically as extension of the knee. The corticospinal
tract—the upper motor neuron—has an inhibitory influence on the muscle
stretch reflexes in the spinal cord.
-
A reflex hammer.
-
Any kind of reflex hammer will do, but
reflexes are easier to obtain with a heavier hammer than the typical
lightweight, tomahawk-style reflex hammer. Many neurologists prefer the
Queen Square type of hammer, which consists of a rubber-rimmed disc on
the end of a stick. Others, including the author, prefer a
Tromner-style hammer, which is more “hammer-like” than the Queen Square
hammer or the tomahawk. All reflex hammers are fairly inexpensive; go
to a medical bookstore and pick out a hammer that you’ll actually carry
around and that works well for you.
-
It is easiest to test the reflexes with
the patient sitting on the side of a bed or an examining table;
however, the muscle stretch reflexes can also be tested with the
patient lying in bed. -
Test the upper extremity reflexes before
testing the lower extremity reflexes. It’s also best to check the same
reflex on each side before proceeding to the next muscle. In other
words, start by testing the right biceps jerk, then test the left
biceps jerk, then test the right triceps jerk, the left triceps jerk,
and so forth. -
Figures 37-1, 37-2, 37-3 and 37-4
illustrate and describe how to examine the major muscle stretch
reflexes in the upper and lower extremities. Hold each limb in the
optimal position for reflex testing for that muscle, as indicated in
the figures. It’s important to have the patient’s limb as relaxed as
possible (simply asking the patient to relax the muscle often helps). -
Grade the reflex on a scale of 0 to 4, with 0 meaning the reflex is unobtainable and 4 meaning it is severely hyperreflexic. Table 37-1
summarizes the definition of the grading scale used for muscle stretch
reflex testing. It is standard to report the grade as the number with a
plus sign after it. The plus has no real meaning, but it is standard to
write it that way. If you want, you can write the number without the
plus, because there is no distinction between a 2, for example, and a
2+. Unlike muscle strength grading, a minus signs tends not to be used,
so think of the reflex choices as only five grades (from 0 to 4), and
choose the one grade that seems to fit best. Some clinicians prefer one
more choice, however, between 0 and 1, called trace, meaning that there may be a suggestion of a slight reflex present, enough not to call it areflexic.
 |
|
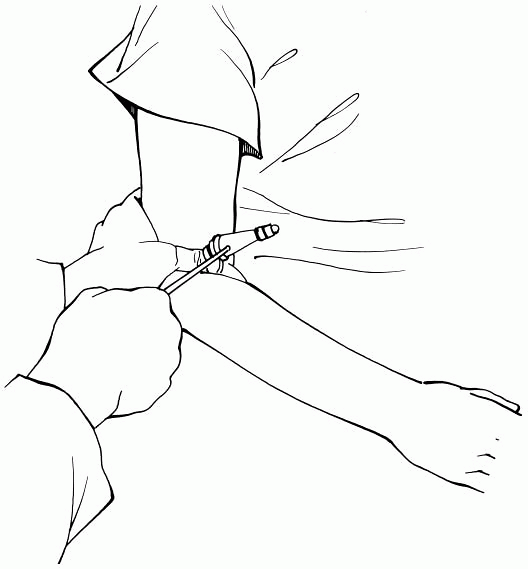
Figure 37-1
Testing the biceps reflex. Hold the patient’s arm so that it is passively flexed and that your thumb is resting on the biceps tendon. Tap on your thumb with the reflex hammer. |
 |
|
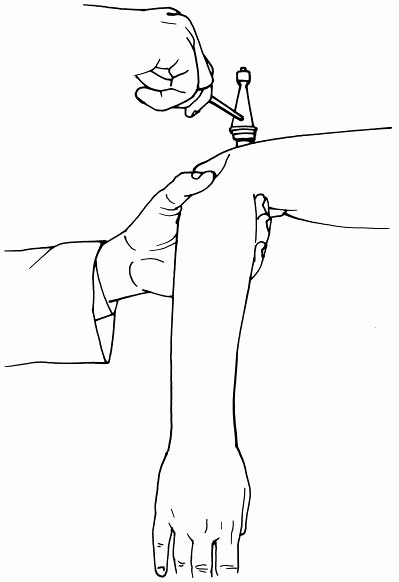
Figure 37-2
Testing the triceps reflex. Hold the patient’s arm so that the upper arm is abducted at the shoulder and the arm is passively dangling at the elbow. Tap on the triceps tendon with the reflex hammer. |
it may be because the patient’s muscle was not relaxed and the patient
is inadvertently suppressing the reflex. In this situation, it is
useful to try to distract the patient from the reflex task; this may
bring out the reflex if it is really intact and is called reinforcement of the reflex.
Several maneuvers are helpful to do this: One method of distraction is
simply to ask the patient to “bite down” at the time you test the
reflex; another maneuver is to ask the patient to make a tight fist
with the opposite hand while you test the upper extremity reflex on the
other side.
-
Instruct the patient to curl the fingers of each hand and lock the fingers together in front of him or her.
-
Ask the patient to pull the arms tight (still locked at the fingers) at the count of three.
-
Say “1, 2, 3, pull!” and tap on the lower extremity reflex with the hammer while the patient pulls the arms tight.
these maneuvers but is difficult to obtain without the maneuver, it
should be graded according to the grade with the maneuver, because the
true reflex was brought out by the distraction. This can be reported,
for example, as, “The biceps jerk was 2+ with reinforcement.”
 |
|
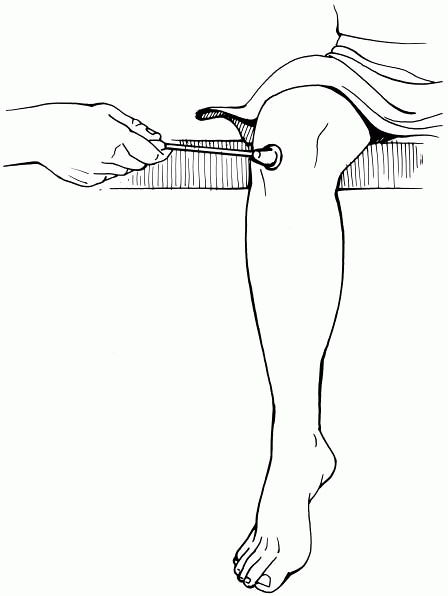
Figure 37-3
Testing the knee jerk. With the patient sitting and the legs dangling, tap on the quadriceps tendon (if the patient is lying in bed, lift the patient’s thigh up slightly with your hand under the posterior thigh so that the leg is slightly passively flexed at the knee and relaxed, then tap on the patellar tendon). |
 |
|
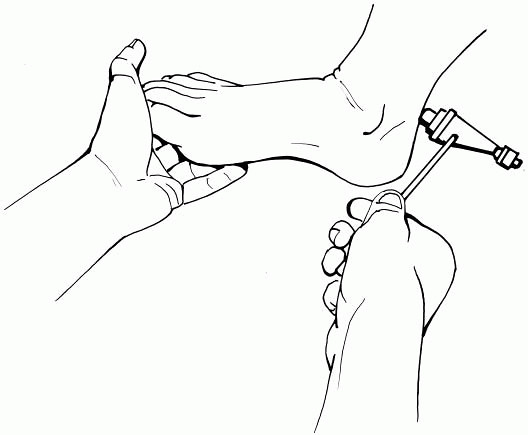
Figure 37-4
Testing the ankle jerk. Push the patient’s foot slightly upward so that it is passively slightly dorsiflexed at the ankle, and then tap on the Achilles tendon. |
|
TABLE 37-1 Grading of the Muscle Stretch Reflexesa
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||
-
Hold the patient’s posterior calf with one hand while you hold your other hand on the sole of the patient’s foot.
-
Keeping the patient’s leg stationary, abruptly (but not painfully) push the sole of the patient’s foot upward.
-
Maintain upward pressure on the patient’s
foot, so that it stays forcefully (again, not painfully) dorsiflexed
for a few seconds and observe the response.
the biceps, triceps, quadriceps (the patellar reflex or knee jerk), and
the Achilles reflex (ankle jerk). These reflexes should be 1+, 2+, or
3+ and be reasonably symmetric on both sides. If ankle clonus is
tested, there should be no more than a couple of beats of clonus seen.
however. It is normal for some elderly patients to have diminished
ankle jerks, even in the absence of symptoms of a polyneuropathy.
Although variable, younger patients tend to have brisker reflexes than
older patients, and reflexes are often brisker with anxiety. Last,
triceps reflexes are sometimes harder to obtain than the other reflexes
described.
-
Hyperreflexia of the muscle stretch
reflexes is potentially abnormal. Because the corticospinal tract (the
upper motor neuron) normally has an inhibitory influence on the
reflexes, hyperreflexia—especially extreme hyperreflexia—of the muscle
stretch reflexes suggests dysfunction of the corticospinal tract (in
the brain, brainstem, or spinal cord) anywhere above the segment of the
spinal cord that serves that reflex. Table 36-1 summarizes the lesion localizations suggested by different patterns of hyperreflexia. -
Although very hyperactive reflexes, such
as sustained clonus (see following section, Clonus), are usually
clearly pathologic, the normal patient-to-patient variation in reflexes
makes it important to interpret reflexes only
P.125
within
the context of the clinical situation and not to overinterpret isolated
reflex findings. The likelihood of significance of a reflex finding is
greater when it was anticipated by the clinical history and the rest of
the examination. For example, in the clinical setting of bilateral
upper and lower extremity weakness and numbness due to a probable
cervical spinal cord process (myelopathy), the finding of 3+
hyperreflexia would support that clinical localization. On the other
hand, in a patient without motor or sensory symptoms, the finding of
the same diffusely brisk reflexes would likely be a clinically
nonsignificant finding and normal for that patient.
|
TABLE 37-2 Spinal Root Levels Tested by the Muscle Stretch Reflexes
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
continuous rhythmic plantar flexion of the foot while the examiner
holds the foot in a position to force dorsiflexion. Sustained clonus is
simply extreme hyperreflexia, with the same implications as the finding
of hyperreflexia described previously (see Hyperreflexia).
Clonus can occur elsewhere, but it most commonly occurs at the ankle;
it rarely can be seen when the patellar reflex is tested in patients
who are markedly hyperreflexic at the knee.
-
Hyporeflexia of the muscle stretch
reflexes is potentially abnormal, and absence of a muscle stretch
reflex (areflexia) is usually abnormal. Decreased or absent muscle
stretch reflexes suggest lower motor neuron or sensory nerve
dysfunction at the level of the reflex tested, affecting the reflex
arc. Table 36-1 summarizes the localizations
suggested by different patterns of hyporeflexia. In general, diffuse or
distal hyporeflexia or areflexia is most suggestive of a
polyneuropathy, and solitary hyporeflexia or areflexia is most commonly
seen due to individual nerve root dysfunction (radiculopathy). -
In the clinical setting of a suspected cervical or lumbar radiculopathy (see Chapter 47,
Examination of the Patient with a Radiculopathy), the finding of a
diminished or absent muscle stretch reflex is a particularly helpful
sign in localization of the nerve root dysfunction. Table 37-2
summarizes the spinal root levels involved in producing the reflex arc
for the four major muscle stretch reflexes. Hyporeflexia or areflexia
of one of these reflexes in the clinical context of a probable
radiculopathy in that extremity would suggest dysfunction of the nerve
root involved in that reflex. For example, a patient with pain
radiating down the posterior left leg who has an absent left ankle jerk
(but all other reflexes are present) most likely has a left S1
radiculopathy.
-
Testing reflexes in all your patients
undergoing a neurologic examination will give you the best feel of the
normal variation of reflexes and help you decide what “normal,”
“hypoactive,” or “hyperactive” is—although the clinical situation is
always most important in deciding whether a reflex is pathologically
brisk or diminished. -
The brachioradialis reflex is another C5,
C6 reflex (similar to the biceps reflex). This can be tested by tapping
on the insertion of the brachioradialis tendon on the dorsal lateral
radius a couple of centimeters proximal to the wrist. Although usually
obtainable, this reflex isn’t as readily elicited as the other upper
extremity reflexes, and for most clinical situations, it rarely adds
much to the examination that wasn’t already discovered by the biceps
reflex. -
The muscle stretch reflexes are also commonly referred to as deep tendon reflexes.
This terminology is not neuroanatomically accurate because the reflex
tested is initiated by muscle stretch and not from the Golgi tendon
organs; however, many clinical neurologists, including, admittedly,
this author, still use the term. Use whatever terminology you like.
