Examination of Eye Movements
– Neurologic Examination > Cranial Nerve Examination > Chapter 14
– Examination of Eye Movements
to look for evidence of dysfunction of the third or sixth cranial
nerves, the extraocular muscles, or the brainstem. Another purpose of
the eye movement examination is to assess the function of the central
nervous system pathways that control voluntary conjugate gaze of the
eyes.
of the six extraocular muscles that attach to the globe. Innervation to
these extraocular muscles comes from three cranial nerves: the
oculomotor (third) nerve, the abducens (sixth) nerve, and the trochlear
(fourth) nerve. Table 14-1 summarizes the cranial nerve innervation to the extraocular muscles and the principal action of each muscle.
that arise in the cerebral hemispheres and descend into the brainstem,
ultimately controlling conjugate gaze through their action on the
cranial nerve nuclei in the brainstem. Horizontal gaze (the most
clinically important pathway to know about) is initiated by impulses
from the “frontal eye field” of each cerebral hemisphere that project
to the contralateral pons.
-
Stand in front of the patient, holding
your index finger approximately 1 ft or more away from the patient,
holding the finger up vertically, midline between the patient’s eyes. -
Ask the patient to follow your finger
with his or her eyes while keeping his or her head still. It sometimes
helps to hold the patient’s head still by gently resting your other
hand on the patient’s head or under the patient’s chin. -
Smoothly move your finger across to your right to observe the patient’s horizontal eye movements toward the left.
-
Then smoothly move your finger across to your left to observe the patient’s horizontal eye movements toward the right.P.47TABLE 14-1 Summary of the Innervation and Principal Actions of the Extraocular Muscles
Cranial Nerve
Origin of
Cranial NerveExtraocular
Muscles InnervatedPrincipal Action
of MuscleIII (Oculomotor)
Midbrain
Superior rectus
Inferior rectus
Medial rectus
Inferior oblique
Moves eye up
Moves eye down
Moves eye medially
Moves eye up (best when eye is in adducted position)
IV (Trochlear)
Midbrain
Superior oblique
Moves eye down (best when eye is in adducted position)
VI (Abducens)
Pons
Lateral rectus
Moves eye laterally
-
Move your finger back to the midline so that the patient’s eyes follow back to the midline.
-
Change the orientation of your index finger so that it is now horizontal.
-
While your finger remains in the midline
(between the patient’s eyes), move your finger smoothly up to assess
the patient’s vertical upward eye movements. -
Finally, move your finger smoothly down to assess the patient’s vertical downward eye movements.
directions of gaze tested, and both eyes should move together in
parallel (i.e., conjugately) in all directions.
action of one of the eye muscles suggests dysfunction of that muscle or
of the nerve that supplies it. The abnormality can potentially be
anywhere within the pathway from the cranial nerve nucleus in the
brainstem to the cranial nerve to the neuromuscular junction to the
muscle itself. Use the rest of the history and examination (see Chapter 49,
Examination of the Patient with Visual Symptoms) to determine where
along the pathway the problem most likely arises. There are, however,
patterns of findings on the eye movement examination suggestive of
particular cranial nerve lesions.
-
Incomplete abduction of an eye suggests a lesion of the ipsilateral sixth (abducens) cranial nerve (Fig. 14-1), although dysfunction of the lateral rectus muscle itself could also cause this finding.
-
Incomplete adduction, upward movement,
and downward movement of an eye suggest a lesion of the ipsilateral
third (oculomotor) cranial nerve. When a third nerve palsy is severe,
the affected eye deviates laterally and downward (see Fig. 10-1) because of the unopposed actions of the muscles innervated by the sixth and the fourth nerves. -
Oculomotor (third) nerve palsies can be categorized as either pupillary involving or pupillary sparing, depending on whether the pupillary constriction
P.48
fibers are affected. Oculomotor nerve palsies due to compression of the
nerve (such as from an aneurysm or mass lesions) tend to involve the
pupil because the pupillary constricting fibers are susceptible as they
lie on the outer surface of the nerve; therefore, the pupil may be
dilated and unreactive to light (see Fig. 10-1).
Oculomotor nerve palsies due to ischemia to the nerve (such as when a
patient with diabetes or hypertension has infarction of the nerve due
to occlusion of its vascular supply) tend to spare the pupil;
therefore, the pupil will likely be symmetric in size compared to the
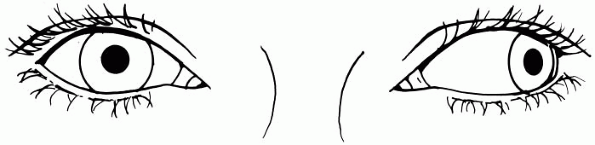
other side and reactive to light. Figure 14-1
Figure 14-1
Severe weakness of abduction of the left eye in a patient with a left
sixth nerve palsy. The patient is trying to follow the examiner’s
finger to the left.
-
Severe difficulty for both eyes to look
up—upgaze paresis—suggests a lesion of the centers that control
vertical gaze in the posterior (dorsal) midbrain/thalamic region, such
as from pineal lesions. This finding can be nonspecific, however,
especially because diminished upgaze is a common finding in normal
aging. -
Severe difficulty for both eyes to look
down—downgaze paresis—is an uncommon finding that is primarily
associated with the extrapyramidal disorder known as progressive supranuclear palsy (see Chapter 46, Examination of the Patient with a Movement Disorder). -
Horizontal gaze palsies—problems with
lateral conjugate gaze to one side—are usually associated with the more
prominent finding of bilateral sustained deviation of both eyes to the
other side (see Chapter 42, Examination of the Comatose Patient).
-
Nystagmus, a jerking movement of the
eyes, is another finding that can be seen while testing eye movements.
Nystagmus can be seen in vestibular disorders, such as from peripheral
(inner ear) or central (brainstem or cerebellar) vestibulopathies.
Nystagmus is described further in Chapter 44, Examination of the Dizzy Patient. -
Incomplete adduction of one eye on
attempted lateral gaze (with all other movements of that eye being
normal), often accompanied by nystagmus of the abducting eye, is called
an internuclear ophthalmoplegia (Fig. 14-2).
This finding suggests a lesion within the brainstem affecting the
medial longitudinal fasciculus, the nerve fiber pathway that connects
the sixth cranial nerve on one side of the brainstem to the third
cranial nerve on the other side. Internuclear ophthalmoplegias can
occur due to any lesion affecting this region of the brainstem, such as
from stroke or multiple sclerosis. The finding of a bilateral
internuclear ophthalmoplegia, however, is most commonly seen due to
multiple sclerosis.
 |
|
Figure 14-2
Incomplete adduction of the right eye while the patient is trying to look to the left, consistent with a right internuclear ophthalmoplegia. There is also nystagmus of the left (abducting) eye. This patient has a lesion of the right brainstem affecting the right medial longitudinal fasciculus. |
-
Complete paralysis of movement of an extraocular muscle is called an ophthalmoplegia, and milder weakness of an eye muscle is called an ophthal-moparesis.
-
It is usually only necessary to look for
abnormalities of the medial, lateral, superior, and inferior rectus
muscles and to ignore the superior and inferior oblique muscles as you
assess eye movements. Trying to assess the action of the oblique
muscles adds a level of complexity that is only rarely additionally
useful in routine neurologic assessment. -
Because it isn’t usually helpful to
assess for the action of the oblique muscles, you only need to
routinely assess vertical eye movements while the eyes are in the
center and not at the extremes of lateral gaze. Check the side-to-side
(horizontal) eye movements, then, when the eyes are back in the middle,
check the up and down (vertical) eye movements. You don’t need to check
the corners. -
If you do need to assess the action of
the oblique muscles (e.g., if a fourth nerve palsy is suspected
clinically), the superior oblique is best tested by having the eye look
down while adducted; the inferior oblique is best tested by having the
eye look up while adducted. Information about how to recognize the
symptoms and signs of a fourth nerve palsy can be found in Chapter 49, Examination of the Patient with Visual Symptoms. -
The eye movements described in this chapter are called pursuit eye movements;
these are the slow eye movements that are used to track moving objects,
like the movements of the examiner’s finger. Another type of eye
movement, saccadic eye movement, is the
more rapid movement of the eyes that occurs when quickly changing
direction of gaze. In routine neurologic assessment, you only need to
assess pursuit eye movements.
