Motor Strength and Power
indicate the capacity of muscles to exert force and expend energy.
Decreased strength is weakness, or paresis; absence of muscle
contraction is paralysis, or plegia. Weakness may cause loss of the
speed, rapidity, or agility of movement and a decrease in the range, or
amplitude, of movement before there is loss of power to formal strength
testing. Other manifestations of impaired motor function include
fatigability, variation in strength on repeated tests, diminished range
and rate of movement, loss of coordination, irregularity and clumsiness
of motion, tremulousness, loss of associated movements, and lack of
ability to carry out skilled acts.
or resisting movement is the major criterion in the evaluation of
strength, observation and palpation of either the contraction of the
muscle belly or its movement of its tendon may be helpful adjuncts. The
contraction of an extremely weak muscle may sometimes be felt when it
cannot be seen. In nonorganic weakness, contraction of the apparently
weak muscle may be felt when the patient is asked to carry out
movements with synergistic muscles, or the antagonists may be felt to
contract when the patient is asked to contract the weak muscle.
Weakness may be masked when attempts to contract individual weak
muscles are accompanied by activation of other muscles to compensate
for the loss of power. In these substitution, or “trick,” movements,
the patient exploits a strong muscle with similar function to
compensate for the loss of action of a weak muscle. Careful observation
for alterations in normal movement patterns and substitution movements
may indicate loss of function. Endurance is the ability to perform the
same act repeatedly.
or active, muscle contraction rather than reflex contraction. Strength
may be classified as kinetic—the force exerted in changing position—and
static—the force exerted in resisting movement from a fixed position.
Strength may be tested in two ways. The patient may place a joint in a
certain position, and then hold it there as the examiner tries to move
it. Alternately the patient may try to move a joint or contract a
muscle against the fixed resistance of the examiner. In most disease
processes, both are equally affected, and the two methods can be used
interchangeably. Some patients may comprehend and cooperate better with
the first method, but having the patient initiate movement may better
detect mild weakness. There is disagreement about how the examiner
should apply force. Some authorities recommend a slow application of
resistance in which the patient and examiner match effort; others
contend that a rapid movement by the examiner will better detect mild
weakness. With very weak muscles, strength may have to be judged
without resistance or only against the resistance offered by gravity.
make assessment more difficult, such as fatigue, systemic illness, and
failure to understand or cooperate with testing. Other conditions may
result in a false or distorted impression of weakness, such as
extrapyramidal disease, ataxia, impairment of the range of motion due
to pain, spasm, joint ankylosis, or contractures, and psychiatric
conditions such as hysteria and malingering. Motor impersistence is the
inability to sustain voluntary motor acts that have been initiated on
verbal command. The patient is unable to sustain an activity, such as
keeping the eyes closed or the hand raised. It may be a form of
apraxia, and has been said to occur most often with left hemisphere
lesions. Passive movements are often helpful to distinguish loss of
range of motion due to contractures from other reasons such as
weakness, pain, and muscle spasm. With contracture, a muscle cannot be
stretched to its normal limits without considerable resistance and the
production of pain. Contractures are particularly common in the calf
muscles, drawing the foot downward (“tight heel cords”). In evaluating
contractures and deformities, it is important to differentiate between
those of neurogenic origin and those due to orthopedic disease,
congenital abnormalities, habitual postures, occupational factors, or
other factors that cause mechanical difficulty with movement.
examiner comparing the patient’s power to a belief of what normal
should be), or it may be assessed in comparison to the patient’s other
muscles. The comparison is most often to a homologous muscle on the
other side, as in comparing the two biceps muscles. But proximal
strength should be commensurate with distal strength in the same
patient. A patient with polymyositis may have weakness of the deltoids
on both sides, so one deltoid cannot be judged against the other. But
the deltoids may be obviously weaker than the wrist extensors, so there
is a proximal to distal gradient of increasing strength that is clearly
abnormal. The muscles on the dominant side are usually slightly
stronger.
individual muscles is tested and graded quantitatively using some
scale. Strength is most commonly graded using the 5-level MRC (Medical
Research Council) scale, which was developed in Britain in World War II
to evaluate patients with peripheral nerve injuries (Table 18.1).
The MRC scale has been widely applied to the evaluation of strength in
general. However, because of the original purpose the scale is heavily
weighted toward the evaluation of very weak muscles. So the most
commonly used strength grading scale has significant limitations when
dealing with many patients.
muscle power, affecting examiners as well as patients, dependent in
part upon size, gender, body build, age, and activity level. A large,
young, powerful physician examining a small, old, sick patient may
overcall weakness. Conversely, a small, relatively weak physician
examining a large, powerful patient may miss significant weakness
because of strength mismatch. As a general principle, reliable strength
testing should attempt to break a given muscle. By varying the length
of lever and the shortening of the muscle permitted, the examiner may
give or take mechanical advantage as necessary to compensate for
strength mismatch. Many patients
of
different ages, sizes, and strength levels must be examined in this
fashion in order to develop an appreciation of the expected strength of
a muscle for a given set of circumstances.
|
TABLE 18.1 The Medical Research Council Scale of Muscle Strength
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
pattern may help greatly in lesion localization and differential
diagnosis. Identification of the process causing weakness is further
aided by accompanying signs, such as reflex alterations and sensory
loss. Table 18.2 reviews the features of upper motor neuron vs. lower motor neuron weakness. Table 18.3 summarizes some common patterns of weakness and their localization.
follow the distribution of some structure in the peripheral nervous
system, such as a peripheral nerve or spinal root. It may affect one
side of the body in a “hemi” distribution. A hemi distribution may
affect the arm, leg, and face equally on one side of the body, or one
or more areas may be more involved than others. The corticospinal tract
(CST) preferentially innervates certain muscle groups, and these are
often selectively impaired. When weakness is nonfocal, it may be
generalized, predominantly proximal, or predominantly distal.
Identification of the process causing weakness is further aided by
accompanying signs, such as reflex alterations and sensory loss.
involves both sides of the body, more or less symmetrically. When a
patient has truly generalized weakness, bulbar motor functions—such as
facial movements, speech, chewing, and swallowing—are involved as well.
Weakness of both arms and both legs with normal bulbar function is
quadriparesis or tetraparesis. Weakness of both legs is paraparesis.
When weakness affects all four extremities, the likely causes include
spinal cord disease, peripheral neuropathy, a neuromuscular junction
disorder, or a myopathy.
|
TABLE 18.2 Features of Upper Motor Neuron vs. Lower Motor Neuron Weakness
|
|||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||
|
TABLE 18.3 Common Patterns of Weakness with Lesions at Different Locations in the Neuraxis
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
is incomplete, more severe involvement of those muscles preferentially
innervated by the CST can frequently be discerned. Reflexes are usually
increased (though in the acute stages they may be decreased or absent);
there is usually some alteration of sensation; sometimes a discrete
spinal “level”; superficial reflexes disappear; and there may be bowel
and bladder dysfunction. Generalized peripheral nerve disease tends to
predominantly involve distal muscles, although there are exceptions.
There is no preferential involvement of CST innervated muscles;
reflexes are usually decreased; sensory loss is frequently present; and
bowel and bladder function are not disturbed. With a neuromuscular
junction disorder, the weakness is likely to be worse proximally;
sensation is spared; reflexes are normal; and there is usually
involvement of bulbar muscles, especially with ptosis and
ophthalmoplegia. When the problem is a primary muscle disorder,
weakness is usually more severe proximally; reflexes are normal;
sensation is normal; and with only a few exceptions, bulbar function is
spared except for occasional dysphagia. These are generalizations. Some
neuropathies may cause proximal weakness, and some myopathies may
affect distal muscles; not all patients with a neuromuscular
transmission disorder have bulbar involvement.
lateral sclerosis (ALS) characteristically involves both the upper and
lower motor neurons. It produces a clinical picture of weakness and
wasting due to involvement of the lower motor neurons in the anterior
horn of the spinal cord, combined with weakness and hyperreflexia due
to involvement of the upper motor neurons in the cerebral cortex that
give rise to the corticospinal tract. There is upper motor neuron
weakness (cerebral cortex pathology) superimposed on lower motor neuron
weakness (spinal cord pathology).
hemiparesis. This may range in severity from very mild, manifest only
as pronator drift and impairment of fine motor control, to total
paralysis. Monoparesis is weakness limited to one extremity, such as
the leg contralateral to an anterior cerebral artery stroke. Diplegia
is weakness of like parts on the two sides of the body; the term
spastic diplegia refers to weakness of both legs that occurs in
cerebral palsy; and facial diplegia is weakness of both sides of the
face. Spastic weakness of one arm and the opposite leg is referred to
as cruciate or crossed paralysis, or hemiplegia alternans.
Reflexes—typically increased unless the process is acute—and
accompanying sensory loss help identify such focal weakness as central
in origin.
peripheral nerve, plexus, or root lesion. A mononeuropathy, such as a
radial nerve palsy, or a spinal root lesion, such as from a herniated
disc, causes weakness limited to the distribution of the involved nerve
or root. A plexopathy may cause weakness of the entire limb, or
weakness only in the distribution of certain plexus components. With
such lower motor neuron pathology, reflexes are typically decreased and
there is often accompanying sensory loss. Localization of focal
weakness due to root, plexus, and peripheral nerve pathology requires
intimate familiarity with peripheral neuroanatomy.
level of the lesion are at risk. When multiple muscles of an extremity
are weak in a non-CST distribution, localization depends on recognizing
the common innervating structure: root, plexus component, or peripheral
nerve.
typically decreased, and there is often accompanying sensory loss.
Anterior horn cell disease often begins with focal weakness that may
simulate mononeuropathy, but it evolves into a more widespread pattern
as the disease progresses, culminating in generalized weakness. Except
for extraocular muscle involvement in myasthenia gravis, it is rare for
a myopathy or neuromuscular junction disorder to cause focal weakness.
whether it is organic or nonorganic, i.e., due to a psychiatric
disorder. This distinction is not always easy. Patients with nonorganic
weakness are commonly thought to have neurologic disease, but just as
often patients with real weakness are dismissed
as
uncooperative, hysterical, or malingering. Coaching is often helpful in
improving poor effort, but some patients, in spite of all, will give
only erratic and variable effort.
from nonorganic weakness. Patients with bona fide organic muscle
weakness will yield smoothly as the examiner defeats the weak muscle.
The patient gives uniform resistance throughout the movement. If the
examiner decreases his resistance, the patient will begin to win the
battle. If the examiner drops the resistance level, the patient with
nonorganic weakness will not continue to push or pull. Instead, the
patient will also stop resisting so that no matter how little force the
examiner applies, there is an absence of follow-through and the patient
never overcomes the examiner. When there is nonorganic weakness,
resistance is erratic and often collapses abruptly. The muscular
contractions are poorly sustained and may give way suddenly, rather
than gradually, as the patient resists the force exerted by the
examiner. Some patients will give up entirely and allow the muscle or
limb to flop; others will provide variable resistance throughout the
range of motion with alternating moments of effort and no effort. This
pattern of variable strength is referred to as “ratchety,” “give way,”
or “catch and give.” It is characteristic of nonorganic weakness. In
nonorganic weakness, functional testing may fail to confirm weakness
suspected during strength testing. For example, there may be apparent
foot dorsiflexion weakness, yet the patient is able to stand on the
heel without difficulty. The patient with nonorganic weakness may be
calm and indifferent while demonstrating the lack of strength, showing
little sign of alarm at the presence of complete paralysis, and smile
cheerfully during the examination. If the examiner raises and drops an
extremity, a limb with psychogenic paralysis may drop slowly to avoid
injury, while an extremity with real weakness would drop rapidly,
especially if the paralysis is flaccid.
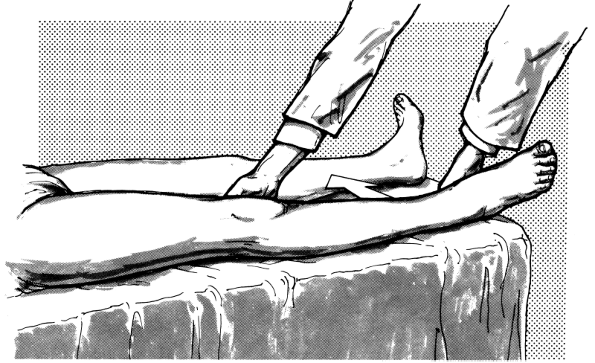
evaluating suspected nonorganic leg weakness. When a normal supine
patient flexes the hip to lift one leg, there is a downward movement of
the other leg. The extension counter-movement of the opposite leg is a
normal associated movement. An extension movement of one leg normally
accompanies flexion of the other leg, as in walking. In organic leg
weakness, the downward pressure of the contralateral heel occurs when
the patient tries to raise the weak leg, and the examiner can feel the
extension pressure by placing a hand beneath the heel that remains on
the bed. In nonorganic leg weakness, there is no downward pressure of
the contralateral heel, but the extension movement of the “paralyzed”
leg may be felt as the good leg is raised (Hoover sign).
positioning and avoidance of unwanted movements. Testing may be done in
various positions depending on the muscle to be tested and its power.
Testing in the seated position suffices under most circumstances. It is
important to fix the proximal portion of a limb when the movements of
the distal portion are being tested. For instance, when testing forearm
pronation strength, the patient must not be allowed to internally
rotate the shoulder to compensate for lack of pronation power. When
evaluating very weak muscles, gravity must be eliminated to detect
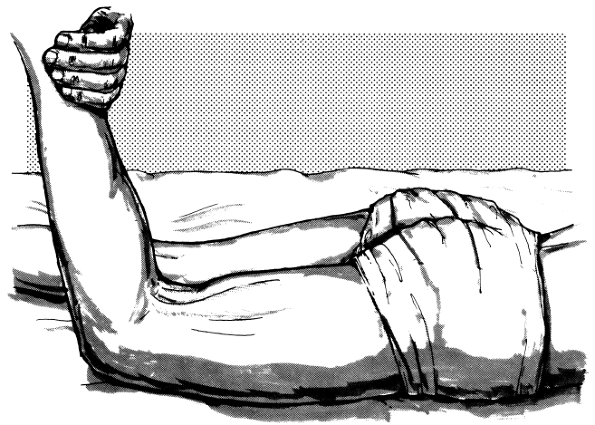
residual power. A very weak biceps muscle (MRC grade 2/5), even when it
cannot succeed against gravity, may be able to flex the elbow if the
arm is raised to shoulder height so that the forearm can be moved
horizontally. The wrist and finger drop of radial nerve palsy creates
such a mechanical disadvantage for contraction that the patient may
appear to have weakness of grip and finger abduction, but these
functions are intact when the wrist and fingers are passively extended.
learning muscle examination techniques. There is some difference
regarding the exact innervation of individual muscles among different
reference sources, and occasionally there is variable or anomalous
innervation. Table 18.4 through Table 18.7
give the most generally accepted spinal cord segment and peripheral nerve innervation of the more important muscles. Table 18.8 and Table 18.9 give the innervation by root.
|
TABLE 18.4 Innervation of Muscles Responsible for Movements of the Head and Neck
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(retraction), rotation (turning), and lateral bending (tilting,
abduction). Many different muscle groups contribute to the various neck
movements. Except for the sternocleidomastoid (SCM) and trapezius it is
not possible to examine them individually, and the assessment is made
of movement (e.g., neck flexion) rather than particular muscles. The
SCM is a flexor and rotator of the head and neck; the trapezius
retracts the neck and
draws
it to one side. Other muscles contribute to neck flexion, especially
the prevertebral group. Many muscles contribute to neck extension,
including the trapezius and the paravertebral muscles. Many of these
muscles when contracting unilaterally rotate the spine. The
paravertebral musculature is a massive, complex amalgam of individual
muscle groups that primarily serve to extend and rotate the neck and
trunk.
|
TABLE 18.5 Innervation of Muscles Responsible for Movements of the Shoulder Girdle and Upper Extremity
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
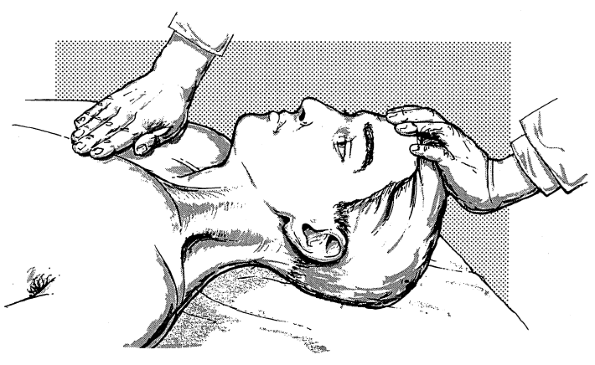
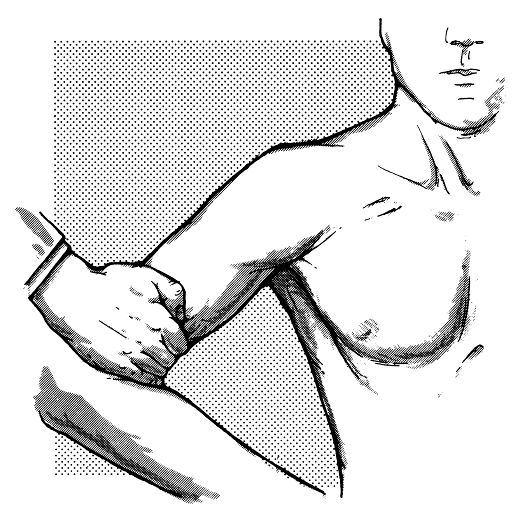
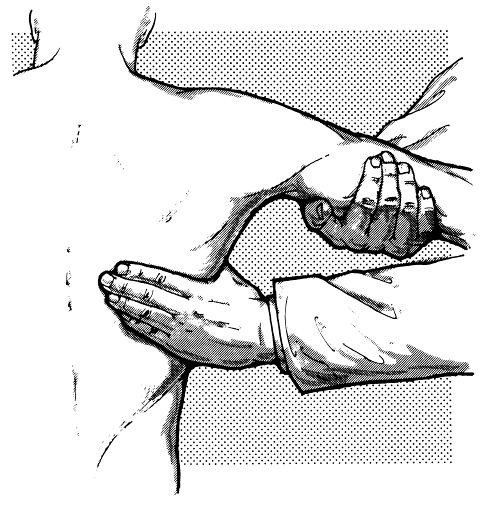
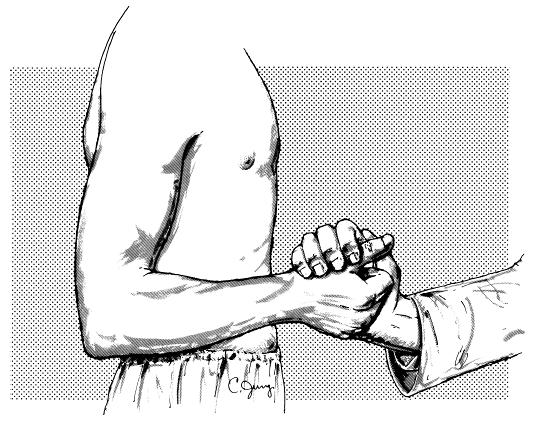
place the chin on the chest as the examiner applies extension force to
the forehead (Figure 18.1). Extensors are tested by having the patient extend against the examiner’s resistance applied to the occiput (Figure 18.2).
Neck rotation is accomplished by the contralateral SCM and ipsilateral
splenius capitus and trapezius; examination of the SCM and trapezius
muscles is discussed in Chapter 15. Neck
flexor strength may be tested with the patient sitting or supine, neck
extension sitting or prone. Examination of the neck muscles must be
done carefully in any patient at risk for cervical spine disease.
|
TABLE 18.6 Innervation of Muscles Responsible for Movements of the Thorax and Abdomen
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
TABLE 18.7 Innervation of Muscles Responsible for Movements of the Lower Extremities
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
TABLE 18.8 Major Upper-Extremity Muscles Innervated by Different Roots
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||
|
TABLE 18.9 Major Lower-Extremity Muscles Innervated by Different Roots
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
 |
|
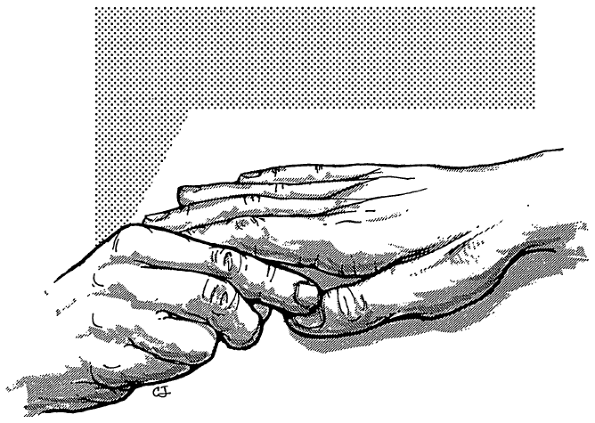
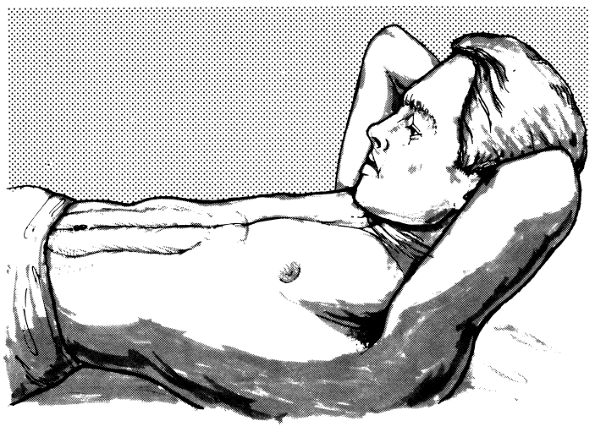
FIGURE 18.1
• Examination of flexion of the neck. The patient attempts to flex his neck against resistance; the sternocleidomastoid, platysma and other flexor muscles can be seen and palpated. |
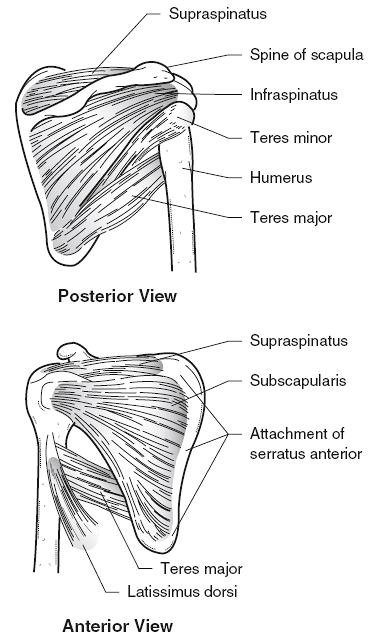
sternoclavicular, acromioclavicular, and glenohumeral joints. Because
the scapula is firmly connected to the clavicle at the
acromioclavicular joint, the two bones tend to move as a unit with the
motion taking place primarily at the sternoclavicular joint. Movements
of the scapula are elevation, depression, retraction (movement away
from the chest wall), protraction (movement toward the chest wall), and
rotation. The ventral surface of the scapula is a
concavity
known as the subscapular fossa that is filled mostly with the
subscapularis muscle. The serratus anterior lies between the
subscapularis and the chest wall and inserts into a thin rim of the
scapula along the vertebral border and slightly expanded triangular
areas at the superior and inferior angles (Figure 18.3).
The serratus runs obliquely from its origination from the upper eight
ribs along the lateral chest wall to its attachment to the scapula. The
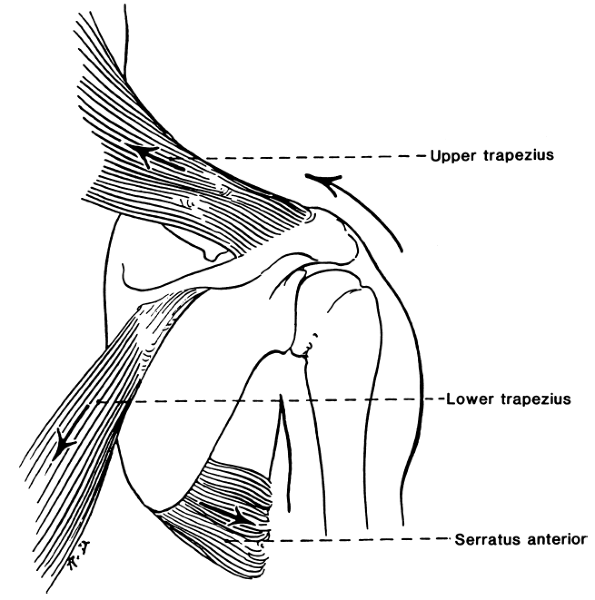
trapezius is a diamond-shaped muscle that attaches widely to the
shoulder girdle. The superior fibers insert along the posterior border
of the clavicle and scapular spine, the middle and lower fibers along
the scapular spine. The upper and middle fibers insert laterally along
the scapular spine, the lower fibers more medially (Figure 18.4).
The rhomboids (major and minor) arise from the spinous process of the
upper thoracic vertebrae, and insert along the medial border of the
scapula. The levator scapula originates from the upper cervical
vertebra and drops diagonally to insert along the upper medial border
of the scapula.
 |
|
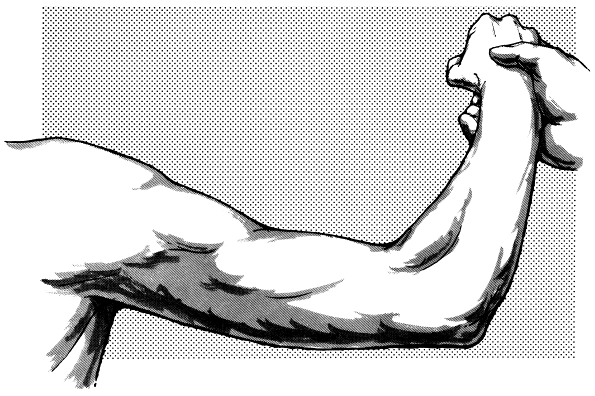
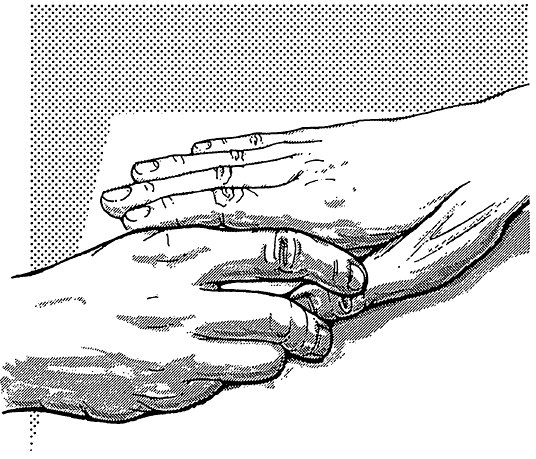
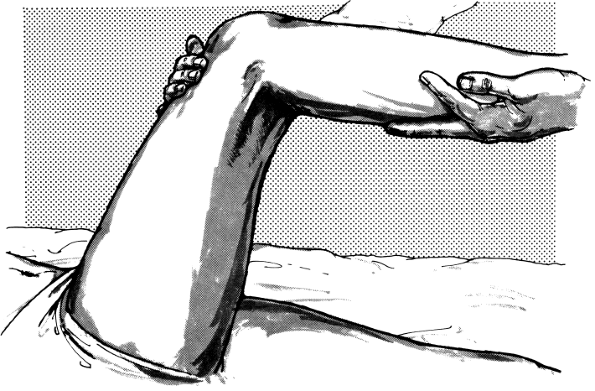
FIGURE 18.2
• Examination of extension of the neck. The patient attempts to extend his neck. The patient attempts to extend his neck against resistance; contraction of the trapezius and other extensor muscles can be seen and felt, and strength of movement can be judged. |
 |
|
FIGURE 18.3 • The muscles of the scapula.
|
levator scapula, elevate the scapula and the point of the shoulder, and
rotate the scapula upward. The middle fibers rotate the scapula upward
and assist the rhomboids in retraction. The lower fibers rotate and
depress the scapula, and draw it toward the midline. The rhomboids act
primarily to retract the scapula, bracing the shoulder backward. The
levator scapulae acts with the trapezius to elevate the scapula. The
serratus anterior, assisted by the pectoralis minor, protracts the
scapula, pulling it anteriorly. It is critical in all functions that
involve reaching or pushing forward. The expanded insertion at the
inferior angle helps to pull the inferior scapular angle forward around
the chest wall. It also, along with the trapezius, rotates the scapula
and raises the point of the shoulder to abduct the arm above
horizontal. It helps to fix the scapula while other muscles abduct or
flex the arm.
is carried out by the upper trapezius and levator scapulae muscles,
assisted by the sternocleidomastoid. The levator scapula is innervated
by
direct branches from C3 and C4 with a contribution from C5 via the
dorsal scapular nerve. The levator scapulae draws the scapula upward
and rotates it so that the inferior angle approaches the spinal column.
Depression of the scapula is carried out primarily by the lower
trapezius, pectoralis minor, and subclavius muscles.
 |
|
FIGURE 18.4 • Upward rotators of the scapula. (Reprinted with permission from Weibers DO, Dale AJD, Kokmen E, Swanson JW, eds. Mayo Clinic Examinations in Neurology, 7th ed. St. Louis: Mosby, 1998.)
|
the rhomboids and the middle trapezius. The rhomboids also draw the
scapulae together, as in standing at attention. The rhomboids are
innervated by a twig directly from the C5 nerve root, and not via the
brachial plexus. Examination of the rhomboids is important in the
differentiation of C5 radiculopathy from upper trunk brachial
plexopathy. In protraction of the scapula, the scapula moves forward as
in throwing a punch. This movement is carried out primarily by the
serratus anterior (long thoracic nerve, C5-C7). The serratus keeps the
vertebral border of the scapula applied to the thorax and pulls the
scapula forward and laterally. Rotation of the scapula is accomplished
by the trapezius, serratus anterior, pectorals, rhomboids, and
latissimus dorsi. Normal scapular rotation is essential to efficient
shoulder abduction.
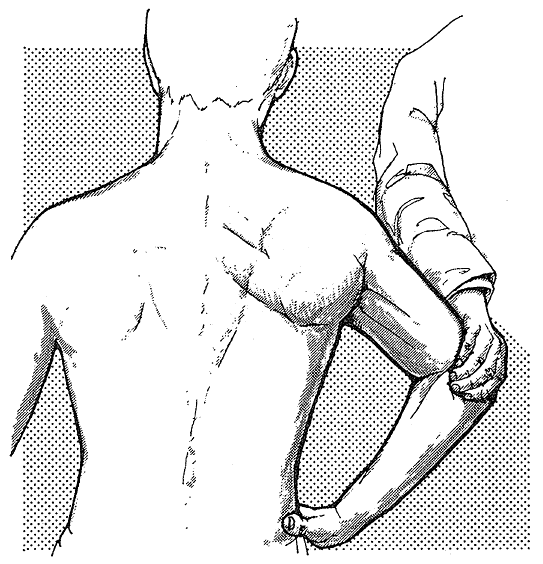
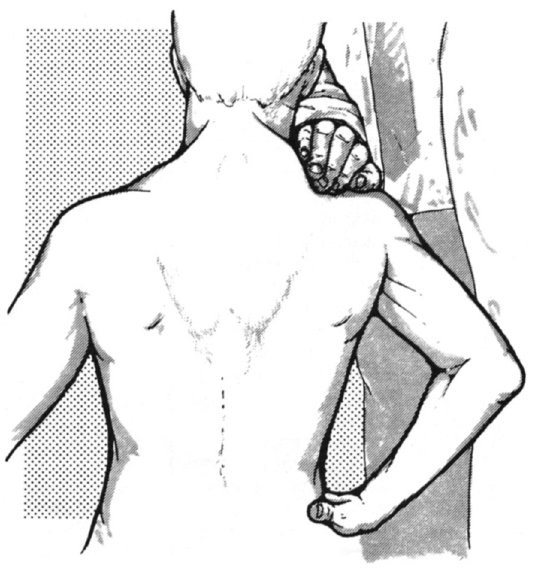
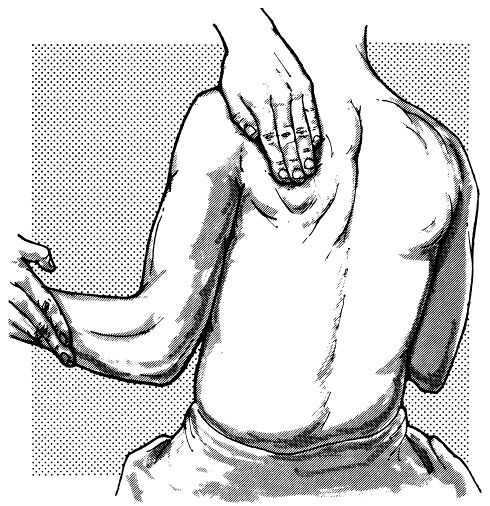
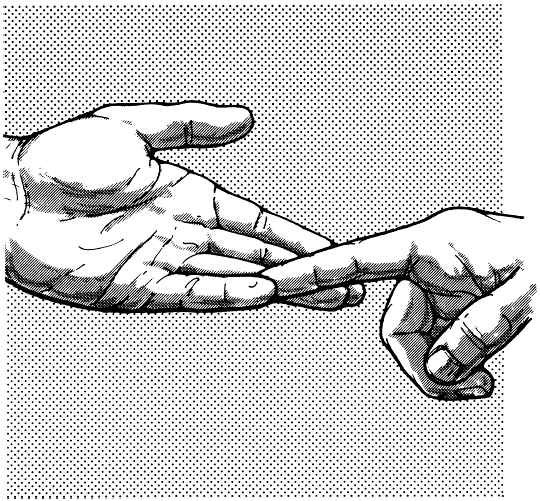
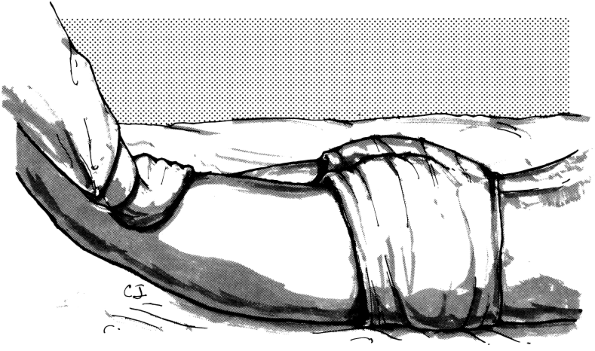
hand on hip, retract the shoulder, against the examiner’s attempt to
push the elbow forward (Figure 18.5). If the
patient braces the shoulders backward as if standing at attention, the
bulge of the rhomboids can be seen and palpated along the medial border
of the scapula. Another test of rhomboid function is to have the
patient place the back of the hand against the small of the back and to
push backward with the palm against the examiner’s resistance. The
rhomboid major contracts vigorously as a downward rotator of the
scapula. Lifting the hand off the small of the back is also used to
test the subscapularis.
 |
|
FIGURE 18.5
• Examination of the rhomboids. With hand on hip, the patient retracts the shoulder against the examiner’s effort to push the elbow forward; the contracting muscles can be seen and palpated. |
separately. One test of the upper fibers is to have the patient shrug
the shoulders against resistance (Figure 15.3).
A better test is resisting the patient’s attempt to touch the occiput
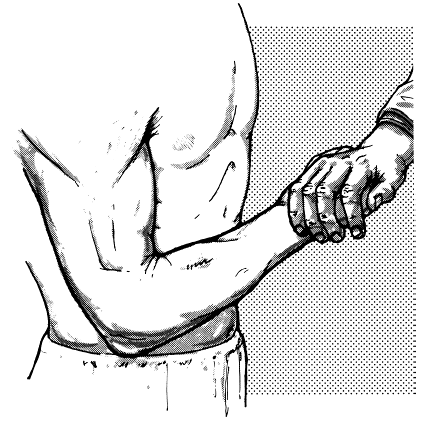
to the acromion. The middle fibers may be tested by having the patient
retract the scapula against resistance (Figure 18.6),
or having the patient hold the arm horizontally abducted, palm up, and
attempting to push the elbow forward. The serratus anterior can be
tested by having the patient make movements that involve forward
reaching or pushing, and observing for evidence of scapular winging
(see next section). The classical test is to have the patient push
against a wall, comparing how well the scapulae remain against the
chest wall on the two sides (Figure 18.7).
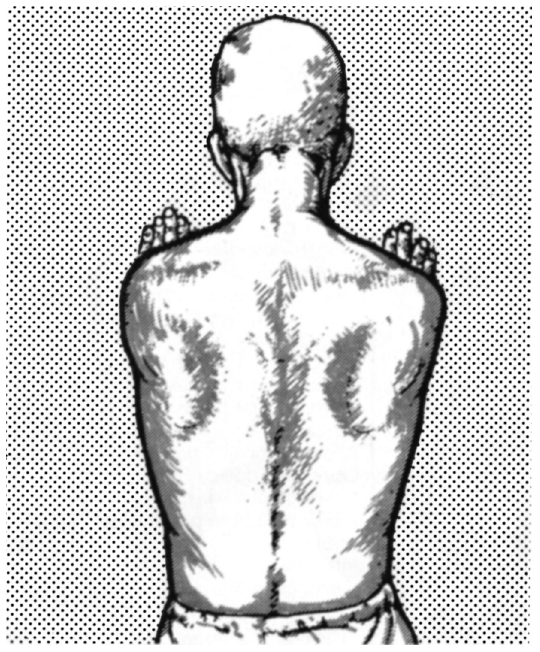
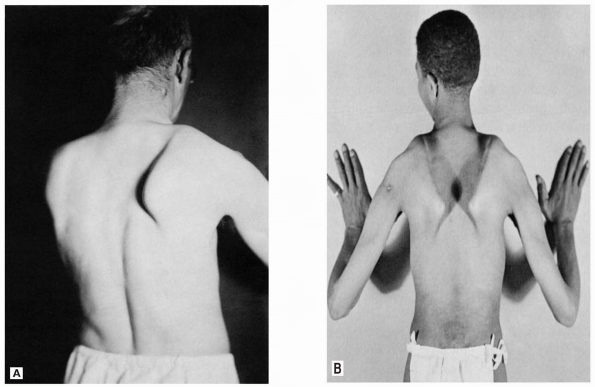
to the chest wall when the arms are raised. However, with weakness of
either the serratus anterior or the trapezius, the vertebral border or
the entire scapula protrudes posteriorly, away from the thoracic wall.
This causes the deformity
known as “winging” (Figure 18.8).
The trapezius is a rotator and retractor of the scapula and functions
primarily during abduction of the arm to the side in the coronal plane
of the body. When the trapezius is weak, scapular winging is more
apparent on attempted abduction of the arm than on forward elevation.
Trapezius winging may be made more conspicuous by having the patient
bend
forward
at the waist so the upper body is parallel to the ground, then raise
the arms to the sides, as if beginning a swan dive. This requires
strong action by the trapezius to retract the scapula and accentuates
the posterior displacement of the shoulder girdle.
 |
|
FIGURE 18.6
• Examination of the trapezius. On retraction of the shoulder against resistance, the middle fibers of the muscle can be seen and palpated. |
 |
|
FIGURE 18.7
• Examination of the serratus anterior. The patient pushes against a wall with his arms extended horizontally in front of him; normally, the medial border of the scapula remains close to the thoracic wall. |
 |
|
FIGURE 18.8 • “Winging” of the scapula. A. Unilateral winging secondary to paralysis of the right serratus anterior. B. Bilateral winging in a patient with muscular dystrophy.
|
scapula and functions during forward arm elevation. When the serratus
is weak, the inferior angle is shifted medially and the entire
vertebral border rides up from the chest wall. Serratus anterior
weakness causes winging that is more obvious when trying to elevate the
arm in front, in the sagittal plane of the body; it is less obvious
when the arms are abducted to the sides. This difference aids in
differentiating serratus anterior winging (as from a long thoracic
nerve palsy) from the flaring of the scapula that occurs with trapezius
weakness (as from a spinal accessory nerve palsy). Serratus winging may
be accentuated by having the patient protract the scapula against
resistance (Figure 18.7). Scapular winging is also discussed in Chapter 15.
abduction, adduction, external and internal rotation, flexion,
extension, and elevation of the arm. These movements are best
appreciated as taking place in the plane of the body of the scapula
rather than in the body as a whole.
region. The deltoid has three portions: anterior, middle, and
posterior. The middle deltoid and supraspinatus muscles abduct the
shoulder. With deltoid contraction, the arm is abducted (raised
laterally) to the horizontal plane. Further abduction, or elevation
above the horizontal plane, is carried out by the associated action of
the trapezius and the serratus anterior, which rotate the scapula and
tilt the angle of the glenoid fossa upward.
noting the ability of the patient to abduct the arm through the range
up to 90 degrees against resistance (Figure 18.9),
or to hold the arm in abduction to the horizontal level, either
laterally or forward (the elbow may be either flexed or extended), and
resist the examiner’s attempt to push it down. Testing both sides
simultaneously helps the patient maintain balance and also helps in the
comparison of strength on the two sides. The supraspinatus helps abduct
the shoulder through the first 15 degrees. The muscle belly lies in the
supraspinous fossa of the scapula; its contraction can be palpated and
sometimes seen when the arm is abducted less than 15 degrees against
resistance (Figure 18.10). The supraspinatus, along with the infraspinatus, teres minor, and subscapularis, form the rotator cuff.
major and latissimus dorsi. On attempts to adduct the horizontally
abducted arm against resistance, the contraction of the sternocostal
and
clavicular portions of the pectoralis can be seen and felt (Figure 18.11).
The muscle can also be tested by having the patient move the
horizontally abducted arm forward, or try to press the hands together
with the arms in front, or try to internally rotate the forearms with
the elbows at the side and flexed, in a position as if holding a book.
The latissimus dorsi adducts, extends, and medially rotates the
shoulder and may be tested in various ways (Figure 18.12). The muscle belly can also be felt when the patient coughs or pushes the arm downward and backward.
 |
|
FIGURE 18.9
• Examination of the deltoid. The patient attempts to abduct his arm against resistance; the contracting deltoid can be seen and palpated. |
 |
|
FIGURE 18.10 • Examination of the supraspinatus. Contraction of the muscle fibers can be felt during early stages of abduction of the arm.
|
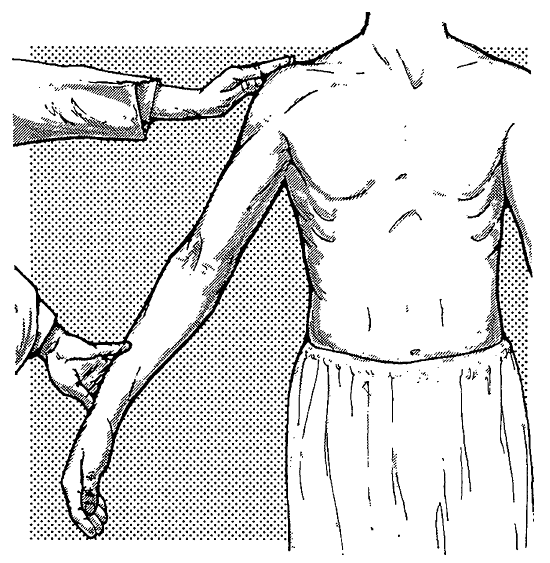
principally by the infraspinatus and teres minor muscles. To test these
muscles, the patient attempts to externally rotate the shoulder by
turning the forearm laterally and backward against resistance while the
elbow is flexed at an angle of 90 degrees and held at the side (Figure 18.13).
Internal rotation at the shoulder results primarily from contraction of
the subscapularis, the chief internal rotator, and teres major muscles;
other muscles also
contribute.
Internal rotation is tested by having the patient move the forearm
medially against resistance with the elbow flexed and at the side—the
opposite motion from external rotation. Internal rotation can also be
tested by having the patient lift the back of the hand off the small of
the back against resistance, as is done when testing the rhomboids.
 |
|
FIGURE 18.11
• Examination of the pectoralis major. Contraction of the muscle can be seen and felt during attempts to adduct the arm against resistance. |
 |
|
FIGURE 18.12
• Examination of the latissimus dorsi. On adduction of the horizontally and laterally abducted arm against resistance, the contracting muscle fibers can be seen and palpated. |
extension of the forearm at the elbow joint and pronation and
supination at the radioulnar joint.
ones are the biceps brachii, brachialis, and brachioradialis. Which
muscle is the prime mover depends on the position of the forearm. The
biceps is an elbow flexor and also a strong supinator of the forearm.
Its supination power is greatest
when
the forearm is flexed and pronated. Its flexion power is greatest when
the forearm is supinated. The brachialis flexes the elbow regardless of
forearm position. The brachioradialis acts as an elbow flexor when the
forearm is held midway between pronation and supination (thumb up). The
brachioradialis acts as a supinator when the forearm is extended and
pronated, but as a pronator when the forearm is flexed and supinated.
 |
|
FIGURE 18.13
• Examination of the external rotators of the arm. On external rotation of the arm while the elbow is flexed and kept close to the body, the contracting infraspinatus muscle can be seen and palpated. |
 |
|
FIGURE 18.14
• Examination of the biceps brachii. On attempts to flex the forearm against resistance, the contracting biceps muscle can be seen and palpated. |
patient attempt to flex the elbow against resistance. The biceps
contraction can be seen and felt, but the brachialis is buried (Figure 18.14). The brachioradialis is tested by attempts to flex the semi-pronated forearm (Figure 18.15).
When the biceps muscle is weak, the patient may employ trick movements
by putting the forearm into midpronation and bringing in the
brachioradialis, or pulling the elbow backwards. The latter resembles
the movement bartenders make when drawing a draft beer and has been
called the “bartender’s sign.”
test it, place the elbow in a position midway between flexion and
extension and have the patient attempt to either extend the elbow or to
hold
position against the examiner’s resistance (Figure 18.16).
The triceps muscle is less powerful when the elbow is fully flexed, and
slight weakness may be more easily detected with testing in this
position.
 |
|
FIGURE 18.15
• Examination of the brachioradialis. On flexion of the semipronated forearm (thumb up) against resistance, the contracting muscle can be seen and palpated. |
 |
|
FIGURE 18.16
• Extension of the forearm. On attempts to extend the partially flexed forearm against resistance, contraction of the triceps can be seen and palpated. |
supinator muscle, assisted by stronger muscles for movements requiring
power. The biceps muscle is the most powerful forearm supinator.
Although the supinator is less powerful, it acts through all degrees of
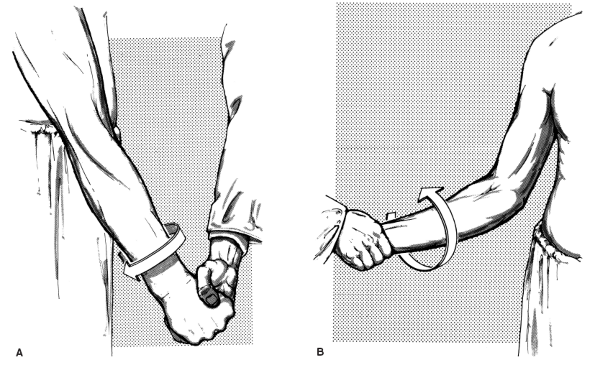
flexion and supination. Supination is tested by having the patient
supinate against the examiner’s resistance. With the forearm in
extension, the brachioradialis also participates; with the forearm in
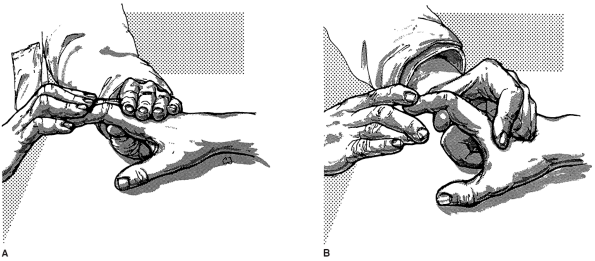
flexion, the biceps also participates (Figure 18.17).
 |
|
FIGURE 18.17 • Supination of the forearm. A. On attempts to supinate the extended forearm against resistance, the contracting brachioradialis can be seen and palpated. B. On attempts to supinate the flexed forearm against resistance, the contracting biceps can be seen and palpated.
|
 |
|
FIGURE 18.18
• Pronation of the forearm. On pronation of the forearm against resistance, contraction of the pronator teres can be seen and palpated. |
quadratus (PQ), which is assisted by the much stronger pronator teres
(PT) for movements requiring power. To test the PT and PQ, the patient
attempts to pronate against resistance (Figure 18.18).
To isolate the action of the PQ, pronation should be tested with the
elbow extended, when the PT is maximally lengthened and exerts its
weakest pull. Flexion of the elbow would signal that the patient is
trying to bring the PT into play.
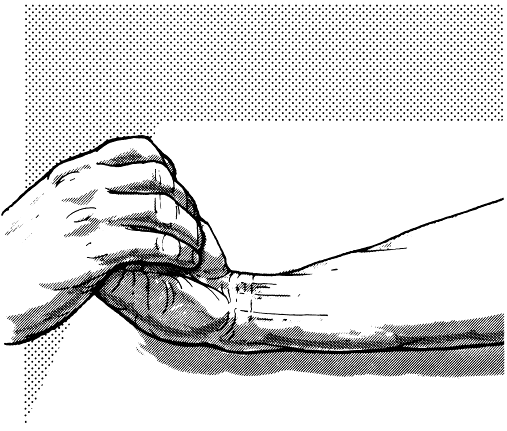
extension. Flexion of the wrist is carried out primarily by the flexor
carpi radialis (FCR) and flexor carpi ulnaris (FCU) muscles. Wrist
flexion is tested by having the patient resist the examiner’s attempts
to extend the wrist (Figure 18.19). Both the FCR and FCU are superficial; their contraction can be seen and felt. The FCR can be
tested individually by having the patient flex the wrist toward the
radial side against resistance directed toward the thumb. Function of
the FCU can be tested by having the patient flex the wrist toward the
ulnar side while the examiner presses on the hypothenar region.
 |
|
FIGURE 18.19
• Flexion at the wrist. On flexion of the hand at the wrist against resistance, the tendon of the flexor carpi radialis can be seen and palpated on the radial side of the wrist, and that of the flexor carpi ulnaris on the ulnar side; the tendon of the palmaris longus can also be seen and palpated. |
 |
|
FIGURE 18.20
• Extension at the wrist. On attempts to extend the hand at the wrist against resistance, the bellies of the extensors carpi radialis longus, carpi ulnaris, and digitorum communis can be seen and palpated. |
primarily by the extensor carpi radialis longus (ECRL), extensor carpi
radialis brevis, and extensor carpi ulnaris. To test the wrist
extensors, the forearm is held in pronation with the wrist partially
extended. The patient then resists the examiner’s attempts to pull the
wrist into flexion (Figure 18.20).
extrinsics and intrinsics. The extrinsic muscles originate in the
forearm and insert on hand structures; the intrinsics originate and
insert within the hand. Possible movements include flexion, extension,
adduction, abduction, and opposition.
superficialis (FDS) and the flexor digitorum profundus (FDP). The FDS
tendons pass through the carpal tunnel and then diverge to insert on
the palmar surfaces of the middle phalanges. The FDS primarily flexes
the proximal interphalangeal (PIP) joints of the four fingers. The
tendons of the FDP pass through the carpal tunnel, and then pierce the
tendons of the FDS and insert on bases of the distal phalanges. The
main action of the FDP is flexion of the distal interphalangeal (DIP)
joints.
abducts the proximal phalanx of the little finger. Two other muscles
acting on the little finger are the abductor digiti minimi (ADM) and
the opponens digiti minimi. The palmaris brevis wrinkles the skin over
the hypothenar eminence and deepens the hollow of the hand. The
palmaris brevis sign is wrinkling of the skin over the hypothenar
eminence with small finger abduction in the face of weakness of the
ulnar hand intrinsics; it proves the lesion involves the deep palmar
branch.
the distal phalanges of the individual fingers against resistance while
the middle phalanges are fixed (Figure 18.21). The FDS is tested by having the patient flex the fingers at the PIP joints while the proximal phalanges are fixed (Figure 18.22).
The patient should try to relax the distal phalanges to eliminate any
action of the FDP on the PIP joint. The interossei and lumbricales flex
the MCP joints and extend the interphalangeal (IP) joints.
Weakness
of these intrinsic hand muscles causes loss of MCP joint flexion and
loss of PIP joint extension, together with loss of adduction and
abduction of the fingers. The hand assumes a position of rest in which
the MCP joints are held in extension and the PIP and DIP joints are
flexed (claw hand). Ulnar neuropathy is the most common cause of claw
hand (ulnar griffe). Ulnar clawing primarily affects the ring and small
fingers because both lumbrical and interosseous function are lost.
 |
|
FIGURE 18.21
• Examination of the flexor digitorum profundus. The patient resists attempts to extend the distal phalanges while the middle phalanges are fixed. |
digitorum communis (EDC), extensor indicis proprius (EIP, aka extensor
indicis), and the extensor digiti minimi (EDM). The tendons insert on
the dorsal extensor expansions of the first phalanges of the fingers.
The primary action of the EDC is extension of the MCP joints, but it
can exert some force to extend each joint it crosses. The EIP extends
the index finger; the EDM extends the little finger. The interossei and
lumbricals also extend the PIP and DIP joints of the fingers.
 |
|
FIGURE 18.22
• Examination of the flexor digitorum superficialis. The patient resists attempts to straighten the fingers at the first interphalangeal joint. |
 |
|
FIGURE 18.23
• Examination of the extensor digitorum communis. With hand outstretched and interphalangeal joints held in extension, the patient resists the examiner’s attempt to flex the fingers at the metacarpophalangeal joints. |
resists attempts to push the fingers down at the MCP joints with the
forearm pronated and the wrist stabilized (Figure 18.23).
The extensor function of the lumbricales and interossei is tested by
having the patient try to extend the PIP and DIP joints against
resistance while the MCP joints are hyperextended and fixed (Figure 18.24).
difference in some of the motions is subtle (e.g., flexion vs.
adduction), but the muscle involved and the clinical significance may
be marked. Two sets of muscles control thumb motion: those in the
forearm (extrinsic thumb muscles), and those that make up the thenar
eminence (intrinsic thumb muscles).
elaborate muscle control compared to the other digits. Because the
classical anatomical terms describing directions of movement are not
easily applied to the thumb, additional directions are designated:
palmar, dorsal, ulnar, and radial.
carpometacarpal (CMC) joint can move in many directions. In palmar
abduction, the thumb moves upward at right angles to the plane of the
palm; in
radial
abduction, the thumb moves away in the plane of the palm. Ulnar and
palmar adduction are movements that touch the first and second
metacarpals together. Opposition (anteposition) is the motion of
circumduction of the thumb with extended MCP and IP joints; this turns
the thumb into semipronation and touches the palmar surface of the tip
of the thumb to the palmar surface of the tip of the small finger.
 |
|
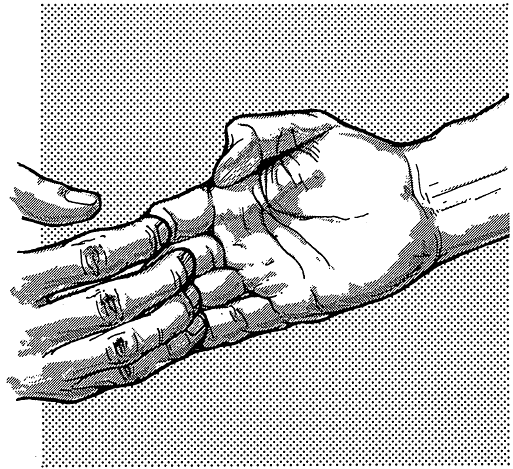
FIGURE 18.24 • A and B.
Extension of the middle and distal phalanges. The patient attempts to extend the fingers against resistance while the metacarpophalangeal joints are fixed. |
 |
|
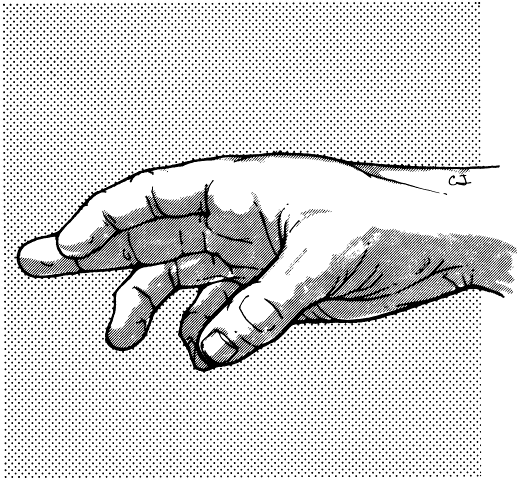
FIGURE 18.25
• Examination of the flexor pollicis longus. The patient resists attempts to extend the distal phalanx of the thumb while the proximal phalanx is fixed. |
are the abductor pollicis longus (APL), extensor pollicis longus (EPL),
extensor pollicis brevis (EPB), and flexor pollicis longus (FPL). The
APL abducts the thumb and extends it to a slight degree. The EPL
extends the terminal phalanx; the EPB extends the proximal phalanx. The
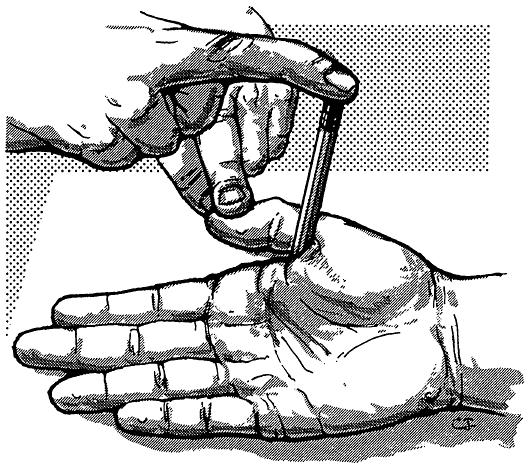
FPL flexes the distal phalanx of the thumb. To test the FPL, the
patient flexes the distal phalanx of the thumb while the proximal
phalanx is flexed and immobilized (Figure 18.25). The EPL is tested by having the patient extend the thumb at the IP joint while the proximal phalanx is immobilized (Figure 18.26). The EPB is tested by having the patient extend the thumb at the MCP joint while the metacarpal bone is immobilized (Figure 18.27).
abductor pollicis brevis (APB), opponens pollicis (OP), and flexor
pollicis brevis (FPB). The APL and APB muscles produce palmar
abduction. The OP pronates the thumb, turning the volar thumb surface
down, to touch the tip of
the
thumb to the small finger. The FPB flexes the MCP joint of the thumb.
In testing the FPB the patient is asked to flex the MCP joint of the
thumb while keeping the IP joint extended.
 |
|
FIGURE 18.26
• Examination of the extensor pollicis longus. The patient attempts to resist passive flexion of the thumb at the interphalangeal joint; the tendon can be seen and palpated. |
 |
|
FIGURE 18.27
• Examination of the extensor pollicis brevis. The patient attempts to resist passive flexion of the thumb at the metacarpophalangeal joint; the tendon can be seen and palpated. |
the same plane as the palm (radial abduction), and at right angles to
the plane of the palm (palmar abduction). To test radial abduction, the
thumb is moved outward if the hand is horizontal, and upward if the
hand is vertical, against resistance. This movement is executed by the
APL and EPB (Figure 18.28). The APB is a thin
sheet of muscle lying just medial to the first metacarpal that performs
palmar abduction. To test palmar abduction the thumb is moved upward at
right angles to the palm, inside the radial margin of the hand, against
resistance. It is very easy for both patient and physician to confuse
abduction with extension. One trick is to place a pencil or similar
object between the thumb and the palm, or radial to the thumb,
perpendicular to the palm. The patient then raises the thumb to a point
vertically above its original position, keeping it parallel to the
pencil with the thumbnail at right angles to the palm (Figure 18.29).
In paralysis of abduction the thumb is adducted and rotated, thumbnail
parallel rather than perpendicular to the fingernails, falling into the
plane of the palm (simian or ape hand).
of the tip of the thumb should contact the palmar surface of the tip of
the little finger. When the OP is weak, the patient may be able to
oppose the thumb to the index or middle finger, but not the little
finger. In testing opposition of the little finger by the opponens
digiti minimi, the patient moves the extended little finger in front of
the other fingers and toward the thumb (Figure 18.31).
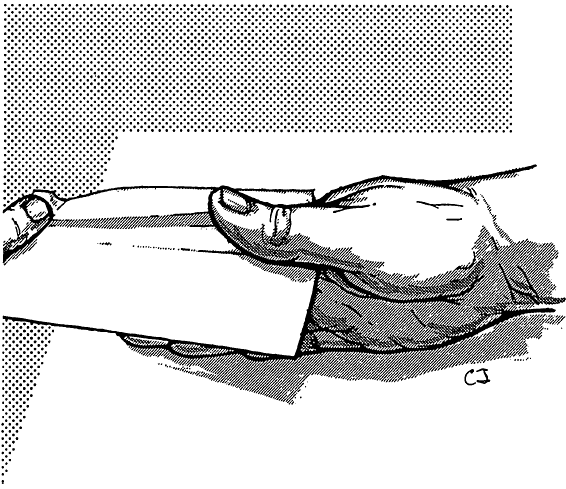
Opposition of the thumb and little finger may be tested in one
maneuver. When both are opposed their extended tips meet and form an
arch over the cupped palm (Figure 18.32). The
strength of the combined movement may be gauged by the patient’s
ability to hold onto a piece of paper held between finger and thumb as
the examiner tries to pull it free, or the examiner may attempt to pull
his finger between the touching tips of the thumb and little finger.
The flexors of the thumb and little finger and the short abductor of
the thumb probably enter into these movements.
 |
|
FIGURE 18.28
• Radial abduction of the thumb. The patient attempts to abduct the thumb in the same plane as that of the palm; the tendon of the abductor pollicis longus can be seen and palpated. |
 |
|
FIGURE 18.29
• Palmar abduction of the thumb. The patient attempts, against resistance, to bring the thumb to a point vertically above its original position. |
first metacarpal. Adduction of the thumb is also carried out in two
planes: in the plane of the palm (ulnar adduction), and in a plane at
right angles to the palm (palmar adduction). Ulnar adduction is
touching the ulnar aspect of the thumb to the radial aspect of the
second metacarpal and index finger, thumb in the same plane as the
palm, the thumbnail as nearly as possible parallel with the other
fingernails, as if to put the hand into salute position. In palmar
adduction, the ulnar aspect of the thumb touches the palmar aspect of
the second metacarpal and index finger so that the thumb and index
finger lie perpendicular to each other, with the thumbnail at right
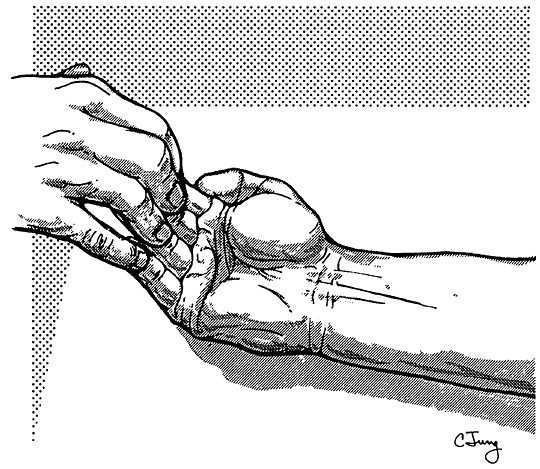
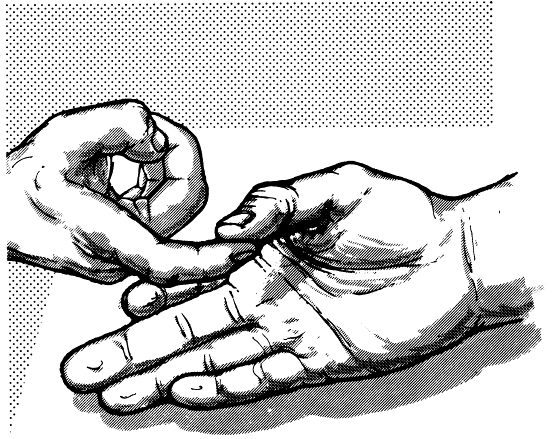
angles to the other fingernails (Figure 18.33). A commonly used test of adduction power in either
of these positions is to have the patient try to hold a piece of paper
tightly between thumb and hand as the examiner tries to extract it (Figure 18.34).
When thumb adduction is weak, the patient may make a substitution
movement, flexing the IP joint with the FPL and trying to secure the
paper with the tip of the thumb (Froment sign), a common finding in
ulnar neuropathy.
 |
|
FIGURE 18.30
• Examination of the opponens pollicis. The patient attempts, against resistance, to touch the tip of the little finger with the thumb. |
 |
|
FIGURE 18.31
• Examination of the opponens digiti minimi. The patient attempts to move the extended little finger in front of the other fingers and toward the thumb. |
 |
|
FIGURE 18.32 • Opposition of the thumb and little finger.
|
 |
|
FIGURE 18.33
• Palmar adduction of the thumb. The patient, against resistance, attempts to approximate the thumb to the palmar aspect of the index finger; the thumbnail is kept at a right angle to the nails of the other fingers. |
 |
|
FIGURE 18.34
• Ulnar adduction of the thumb. The patient attempts to grasp a piece of paper between the thumb and the radial border of the index finger while the thumbnail is parallel to the nails of the other fingers. |
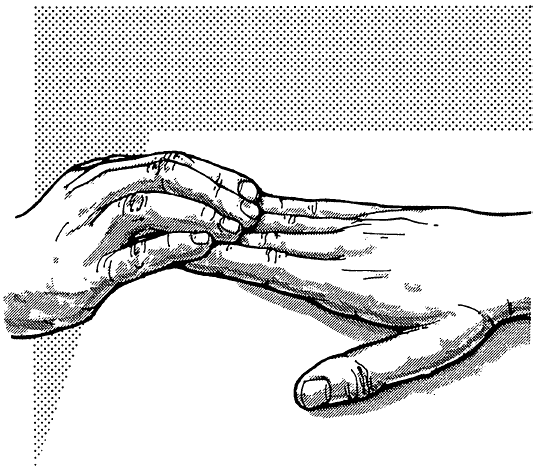
fingers tightly together; abduction spreads the fingers apart.
Adduction is a function of the volar interossei; abduction is a
function of the dorsal interossei. Abduction of the little finger is
done by the ADM. Adduction may be tested in several ways. With the
fingers abducted and extended, the patient may try to adduct the
fingers against resistance (Figure 18.35). The
patient may try to clutch a piece of paper between two fingers and
resist the examiner’s attempts to withdraw it. The examiner may
interdigitate his fingers between the patient’s and have the patient
squeeze as tightly as possible. The usual test of abduction is to have
the patient keep the fingers fully extended and spread apart and resist
the examiner’s attempt to bring them together (Figure 18.36).
 |
|
FIGURE 18.35 • Adduction of the fingers. The patient attempts to adduct the fingers against resistance.
|
 |
|
FIGURE 18.36 • Examination of the abduction of the fingers. The patient resists the examiner’s attempt to bring the fingers together.
|
and abdomen are often combined, and it is difficult to evaluate them
individually (Table 18.6). Except for the respiratory muscles, most of these muscles have scant neurologic significance.
external intercostals, and diaphragm. Muscles attached to the sternum,
clavicles, and scapulae act as accessory muscles of respiration. The
diaphragm is the principal muscle of respiration. During quiet
inspiration, intercostal contraction expands the anteroposterior and
transverse diameters of the thorax, and the vertical diameter is
increased by the descent of the diaphragm. In deep inspiration, the
accessory muscles are brought into action.
the costal margins and abdominal respiration, with alternate bulging
and retraction of the epigastrium as increased diaphragmatic
contraction compensates for the intercostal weakness (abdominal
breathing). The intercostal spaces may retract during inspiration, and
the ribs do not rise and separate. When bilateral paralysis of the
diaphragm is present, the excursion of the costal margins is increased
and the epigastrium does not bulge during inspiration. The moving
shadow caused by retraction of the lower intercostal spaces during
inspiration (Litten sign) is absent.
occur in neurologic patients. The abdominal muscles may be tested by
having the patient raise the head against resistance (Figure 18.37),
cough, or do a sit-up. If the abdominal muscles contract equally in all
four quadrants, the umbilicus will not move. If the lower abdominal
muscles are paralyzed, as in a T10 myelopathy, the upper abdominal
muscles will pull the umbilicus cephalad when the patient raises the
head or attempts a sit-up (Beevor sign).
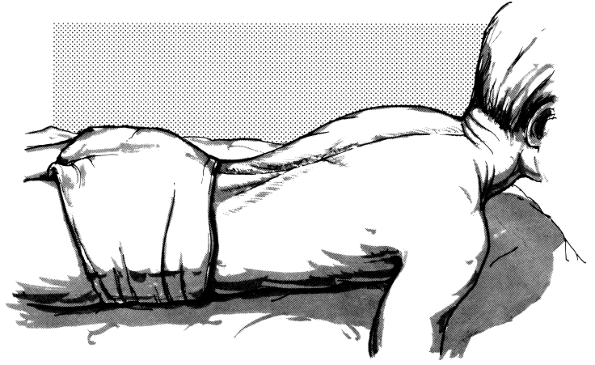
rotation, and lateral bending. The muscles that produce these movements
are examined en masse by examining the movements rather than individual
muscles. The extensors of the spine are tested by having the prone
patient raise the head and shoulders without the assistance of the
hands (Figure 18.38). The most common cause of
paraspinal weakness is primary muscle disease, particularly muscular
dystrophies, especially facioscapulohumeral dystrophy. The flexors of
the spine are tested by having the patient rise from recumbent to
seated, and then to a standing position without using the hands (Figure 18.39).
 |
|
FIGURE 18.37 • Examination of the abdominal muscles. The recumbent patient attempts to raise his head against resistance.
|
 |
|
FIGURE 18.38 • Examination of the extensors of the spine. The patient, lying prone, attempts to raise the head and upper part of the trunk.
|
 |
|
FIGURE 18.39
• Examination of the abdominal muscles and flexor muscles of the spine. The patient attempts to rise from a recumbent to a sitting position without the use of the hands. |
than those of the upper extremities, and there are fewer substitution
movements. Table 18.7 lists the pertinent muscles and their innervation.
extension, abduction, adduction, and internal and external rotation.
The principal hip flexor is the iliopsoas. The iliopsoas has two parts,
the psoas and the iliacus, which have the same function. The psoas
arises from both the transverse processes and the bodies of the lumbar
vertebra. The intervertebral foramina of L1-L4 lie between these two
points of origin, so that the roots that form the lumbar plexus exit
into the substance of the muscle and the plexus lies within it. This
anatomy accounts for the severe damage to the lumbosacral plexus that
commonly occurs with hemorrhage into the psoas muscle. The iliacus
portion arises in the iliac fossa.
help to maintain an erect posture by balancing the spine and pelvis
over the femurs, preventing a backward tilt. When the legs are fixed
they flex the trunk and pelvis forward, as in doing a sit-up. Hip
flexor strength is tested by having the patient flex the hip against
resistance (Figure 18.40). This may be done in the sitting or supine position.
gluteus maximus is important in climbing steps, jumping, and rising
from a chair. Hip extensor function is best tested with the patient
prone, raising the flexed knee up from the table against downward
pressure from the examiner (Figure 18.41).
Having the knee flexed minimizes any contribution from the hamstrings.
The gluteus maximus can also be tested with the patient lying on the
side and extending the hip, or seated and trying to press the raised
knee back down as the examiner holds it up, or by testing the ability
to stand upright from a stooped position. With hip girdle weakness,
particularly in the muscular dystrophies, there is marked weakness of
the hip extensors, and the patient arises from a stooped position by
using his hands to “climb up the legs” (Gowers maneuver, Figure 20.3).
gluteus minimus, and tensor fasciae latae (TFL). They also function as
internal rotators of the hip. The hip abductors may be tested
either
supine or sitting by having the patient attempt to hold the lower
extremities outward with ankles spread far apart, as the examiner tries
to force the ankles together (Figure 18.42).
The hip abductors are very important in walking. When the hip abductors
are weak there is an exaggerated pelvic swing during the stance phase
as the pelvis on the side of the swing leg drops downward
(Trendelenburg sign).
 |
|
FIGURE 18.40
• Examination of the flexors of the thigh. The patient attempts to flex the thigh against resistance; the knee is flexed and the leg rests on the examiner’s arm. |
 |
|
FIGURE 18.41
• Examination of the extensors of the thigh at the hip. The patient, lying prone with the leg flexed at the knee, attempts to extend the thigh against resistance; contraction of the gluteus maximus and other extensors can be seen and palpated. |
three adductors: longus, brevis, and magnus. The adductor magnus is the
longest and strongest hip adductor. The adductors can be tested with
the patient supine, sitting, or lying on one side. The patient attempts
to bring the legs together as the examiner tries to keep them apart (Figure 18.43).
As with the abductors, the adductors are so powerful it is helpful to
keep the patient’s knees extended to give the examiner the advantage of
a longer lever.
principally by the hip abductor muscles (glutei medius and minimus, and
TFL), with some contribution from the adductors. To test internal
rotation the patient lies supine with the hip and knee flexed, or prone
with the knee flexed. He then
attempts to move the foot laterally against resistance, thus rotating the hip medially (Figure 18.44).
Internal rotation can also be tested with the patient supine and the
leg extended, rotating the foot medially as if to touch the big toe to
the bed. Rotating the foot medially with the knee extended produces the
same hip motion as carrying the foot laterally with the knee flexed.
With a unilateral CST lesion (e.g., acute stroke), the internal
rotators are weak. When the patient lies supine, the involved leg lies
externally rotated compared to its fellow. This asymmetry of leg
position may be a clue to the presence of a hemiparesis in an obtunded
patient.
 |
|
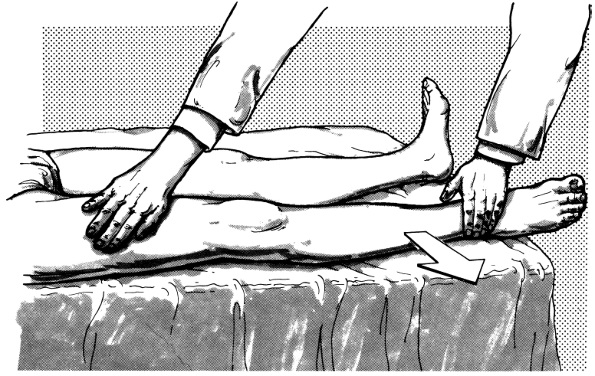
FIGURE 18.42
• Abduction of the thigh at the hip. The recumbent patient attempts to move the extended leg outward against resistance; contraction of the gluteus medius and tensor fasciae latae can be palpated. |
 |
|
FIGURE 18.43
• Examination of adduction of the thigh at the hip. The recumbent patient attempts to adduct the extended leg against resistance; contraction of the adductor muscles can be seen and palpated. |
is carried out primarily by the gluteus maximus. External rotation is
tested by maneuvers similar to those for testing internal rotation, but
the patient rotates the hip externally by attempting to carry the foot
medially against resistance with the knee flexed.
 |
|
FIGURE 18.44
• Examination of internal rotation of the thigh. The patient, lying prone with the leg flexed at the knee, attempts to carry the foot laterally against resistance, thus rotating the thigh medially. |
are flexion and extension. Flexion of the knee is carried out primarily
by the hamstring muscles (biceps femoris, semimembranosus,
semitendinosus). The hamstrings also act as powerful hip extensors. The
knee flexors may be tested with the patient prone (Figure 18.45),
supine, or sitting. With the knee in partial flexion the patient
resists the examiner’s attempts to straighten the knee. The knee
flexors are powerful and cannot normally be overcome. Another test is
to have the prone patient attempt to maintain both knees flexed at
about 45 degrees from horizontal with the feet slightly apart. When the
knee flexors are weak on one side, as in a CST lesion, the involved leg
will sink, gradually or rapidly (leg drift, leg sign of Barré).
Examination of knee flexion with the patient prone makes it easier to
see and palpate the muscle contractions and lessens the likelihood of
misinterpretation due to simultaneous action of the hip flexors. The
sartorius, the longest muscle in the body, has a complex set of
actions. It is an abductor, flexor, and lateral rotator of the hip, and
a flexor and medial rotator of the knee. The sartorius would be active
when trying to look at the bottom of one’s foot. The sartorius may be
examined by having the patient attempt to flex the knee against
resistance with the hip flexed and rotated laterally (Figure 18.46).
rectus femoris also crosses the hip, and serves as a hip flexor as well
as a knee extensor. The quadriceps may be tested when the patient,
sitting or supine, attempts to extend the knee against the examiner’s
resistance (Figure 18.47). The quadriceps is so
powerful it is nearly impossible to overcome in the normal adolescent
or adult except by taking extreme mechanical advantage. A sometimes
useful technique for testing knee extension is the “barkeeper’s hold” (Figure 18.48).
lean backward when trying to extend the knee, attempting to muster some
knee extension force by allowing the rectus femoris to contract across
the hip. The patient will have marked difficulty in rising from a
kneeling position and in climbing stairs; he can walk backward, but has
difficulty walking forward.
dorsiflexion, eversion, and inversion. Plantar flexion (flexion) of the
foot is carried out principally by the gastrocnemius and soleus
muscles.
Other
muscles cross posterior to the axis of rotation of the ankle, but
because of mechanical factors are not very effective plantarflexors.
The gastrocnemius also assists in flexing the knee. The gastrosoleus
raises the heel, as in walking, and inverts the foot.
 |
|
FIGURE 18.45 • Examination of flexion at the knee. The prone patient attempts to maintain flexion o
|
