Disorders of Speech and Language
– Mental Status Examination and Higher Cortical Functions > Chapter
6 – Disorders of Speech and Language
is the production of vocal sounds without word formation; it is
entirely a function of the larynx. Howls of rage, the squeals of little
girls, and singing a note with the mouth open are phonation. A
vocalization is the sound made by the vibration of the vocal folds,
modified by workings of the vocal tract. Speech consists of words,
articulate vocal sounds that symbolize and communicate ideas.
Articulation is the enunciation of words and phrases; it is a function
of organs and muscles innervated by the brainstem. Language is a
mechanism for expressing thoughts and ideas: by speech (auditory
symbols), by writing (graphic symbols), or by gestures and pantomime
(motor symbols). Language may be regarded as any means of expressing or
communicating feeling or thought using a system of symbols. Grammar (or
syntax) is the set of rules for organizing the symbols to enhance their
meaning.
and speech are uniquely human attributes. Linguistic communication
requires not only the motor acts necessary for execution, but also the
reception and interpretation of these acts when they are carried out by
others, along with the retention, recall, and visualization of the
symbols. Speech is as dependent upon the interpretation of the auditory
and visual images, and the association of these images with the motor
centers that control expression, as upon the motor elements of
expression.
often encountered are dysarthria and aphasia. The essential difference
is that aphasia is a disorder of language and dysarthria is a disorder
of the motor production or articulation of speech. The common
vernacular phrase “slurred speech,” could be due to either. Aphasia
usually affects other language functions such as reading and writing.
Dysarthria is defective articulation of sounds or words of neurologic
origin. In dysarthria, language functions are normal and the patient
speaks with proper syntax, but pronunciation is faulty because of a
breakdown in performing the coordinated muscular movements necessary
for speech production. A good general rule is that no matter how
garbled the speech, if the patient is speaking in correct sentences,
using grammar and vocabulary commensurate with their dialect and
education, they have dysarthria and not aphasia. In dysarthria there
are often other accompanying bulbar abnormalities, such as dysphagia,
and a brainstem lesion is usually a prominent clinical consideration.
Dysarthria is a problem with articulation of speech, aphasia is a
problem with language function. The implications of these two
conditions are quite different. Disturbed language function is always
due to brain disease, but dysfunction limited to the speech mechanisms
may occur with many conditions, neurologic and nonneurologic.
vocal cords. Properly articulated speech requires coordination between
the respiratory muscles and the muscles of the larynx, pharynx, soft
palate, tongue, and lips. All these components are referred to as the
vocal (oral) tract. Respiratory movements determine the strength and
rhythm of the voice. Variations in pitch are produced by alterations in
the tension and length of the vocal cords and the rate and character of
the vibrations transmitted to the column of air that passes between
them. Modifications in sound are produced by changes in the size and
shape of the glottis, pharynx, and mouth, and by changes in the
position of the tongue, soft palate, and lips. The oropharynx,
nasopharynx, and mouth act as resonating chambers and further influence
the timbre and character of the voice. Speech may be possible in the
absence of vocal cords, and whispered speech may be possible in
inspiration as well as expiration. An electrolarynx produces
electromechanical vibrations in the oral tract that are then
articulated into speech. Whispered sounds are also entirely
articulatory.
Several cranial nerves are involved in speech production, and an
adequate appraisal of speech requires evaluating the function of each.
The trigeminal nerves control the muscles of mastication and open and
close the mouth. The facial nerves control the muscles of facial
expression, especially the branches to the orbicularis oris and other
smaller muscles about the mouth that control lip movement. The vagus
nerves and glossopharyngeal nerves control the soft palate, pharynx,
and larynx, and the hypoglossal nerves control tongue movements. The
upper cervical nerves, which communicate with the lower cranial nerves
and in part supply the infrahyoid and suprahyoid muscles, the cervical
sympathetic nerves that contribute to the pharyngeal plexus, and the
phrenic and intercostal nerves also contribute to normal speech.
that the vocal cords are approximated. Voiceless sounds are made with
the glottis open. Either type of sound may be modulated by adjusting
the size and shape of the vocal cavities. Vowels are largely of
laryngeal origin, but are modified by the resonance of the vocal
cavities. Certain vowel sounds such as i, a, and y are modified by the
soft palate. Consonants may be either voiced or voiceless; they are
enunciated by constriction or closure at one or more points along the
vocal tract. A fricative is a sound articulated through a not quite
closed glottis that creates turbulence in the airflow causing a
frictional rustling of the breath, e.g., f, soft s.
related to the place of articulation, e.g., labiodental, interdental,
alveolar, palatal, alveopalatal, velar, and uvular. From an anatomic
and neurologic viewpoint it is more important to recognize how various
sounds are produced. Articulated labials (b, p, m, and w) are formed
principally by the lips. Modified labials (o and u, and to a lesser
extent i, e, and a) are altered by lip contraction. Labiodentals (f and
v) are formed by placing the teeth against the lower lip. Linguals are
sounds formed with tongue action. T, d, l, r, and n are tongue-point,
or alveolar, sounds, formed by touching the tip of the tongue to the
upper alveolar ridge. S, z, sh, zh, ch, and j are dentals, or
tongue-blade sounds. To hear distorted linguals, place the tip of your
tongue against the back of your bottom teeth, hold it there and say
“top dog,” “go jump,” and “train.” To hear distorted labials, hold your
upper lip between the thumb and forefinger of one hand and your bottom
lip similarly with the other and say “my baby.” Gutturals (velars, or
tongue-back sounds such as k, g, and ng) are articulated between the
back of the tongue and the soft palate. Palatals (German ch and g, and
the French gn) are formed when the dorsum of the tongue approximates
the hard palate.
neuromuscular control of the vocal tract. Normal development of the
tongue, larynx, and soft palate, and adequate hearing are essential to
proper pronunciation. The cultural and emotional background of the
individual are also important
in
appraising speech. No two individuals possess the same speech patterns.
This is true not only for pitch and timbre, but also for the quality,
duration, and intensity of tones and sounds, and for the ability to
pronounce certain words and syllables. Normal variations in enunciation
and articulation result from regional variations in speech patterns
(“accents”) evident in the pronunciation of vowels and many of the
consonants. Education and training are important factors. The
uneducated, illiterate, and mentally deficient may mispronounce letters
and syllables despite normal powers of articulation. Some individuals
are never able to make certain sounds. Those who learned another
language before English may never master the pronunciation of certain
English sounds. Adult native English speakers may never be able to
accurately pronounce some of the guttural and palatal sounds that are
part of some languages.
patient’s spontaneous speech in normal conversation, usually during
taking of the history. The accuracy of pronunciation, rate of speech,
resonance, and prosody (variations in pitch, rhythm, and stress of
pronunciation) are noted. Abnormalities of articulation include
tremulousness, stuttering, slurring or sliding of letters or words,
scanning, explosiveness, and difficulties with specific sound
formations. Some difficult to enunciate phrases have been traditionally
used to test articulation. These require the pronunciation of labials,
linguals, and, to a lesser extent, velars. The nonsense phrase
“puhtuhkuh” or “pataka” tests all three: labials (puh/pa), linguals
(tuh/ta), and velars (kuh/ka). Traditional phrases have been selected
to test primarily the labials and linguals, such letters as l, r, b, p,
t, and d. As the patient repeats these phrases, various aspects of the
dysarthria may become more evident. These phrases are time-honored,
perhaps above their actual value, and are to a certain extent
colloquial. Nonetheless, they are often useful. Pronouncing r’s
requires a facile tongue, and many of the test phrases are loaded with
this letter. The best test words and phrases have the significant
consonants and vowels placed in the initial, middle, and final
positions. Commonly used words and phrases include: third riding
artillery brigade, Methodist Episcopal, West Register Street, liquid
electricity, truly rural, voluntary retribution, baby hippopotamus, and
irretrievable ball. Phrases such as “my baby ate a cupcake on the
train” contain all the pertinent elements.
and over as rapidly as possible. Normally the syllable can be
pronounced accurately at a rate of 5-7 Hz. Similarly for “tuh” and
“kuh.” Listen for abnormally slow or rapid repetition, regularity and
evenness, uniform loudness, or tremulousness.
might occur in myasthenia gravis, may be brought out by having the
patient count to 100 at about one number per second, enunciating each
number clearly. Listen for the voice to become hoarse, hypernasal,
slurred, or breathy. Disturbances of laryngeal function and of speech
rhythm may be elicited by having the patient attempt prolonged
phonation, such as by singing and holding a high “a” or “e” or “ah”
sound. Assess loudness, pitch, quality (hoarseness, breathiness),
steadiness, nasality, and duration. The voice may break, waver, or
flutter excessively, particularly when there is cerebellar dysfunction.
Note whether the pitch of the voice is appropriate for the patient’s
age and sex.
normal cough indicates that vocal cord innervation is intact. Dysphonia
with a normal cough suggests laryngeal disease or a nonorganic speech
disturbance. The glottal coup (glottic click, coup de glotte) is the
sharp sound at the beginning of a cough. The intensity of the glottic
click reflects the power of vocal cord adduction. The glottic click may
also be elicited by asking the patient to say “oh-oh,” or make a sharp,
forceful grunting sound. A cough without a glottal coup (bovine cough)
suggests vocal cord palsy.
resonance depends on an adequate seal between the oropharynx and
nasopharynx (velopharyngeal competence). When palatal weakness causes
an inadequate seal on pronouncing sounds that require high oral
pressure, the voice has a “nasal” quality. An audible nasal emission is
nasal air escape that causes a snorting sound.
Hypernasality
is more noticeable when the head is tipped forward; it is less evident
when the patient lies with his head back, because the weakened soft
palate falls back by its own weight and closes off the nasopharynx.
Velopharyngeal incompetence is common in patients with cleft palate.
Laryngeal disorders may alter the volume, quality, or pitch of the
voice (dysphonia). Laryngitis causes dysphonia. Aphonia is complete
voice loss. A central or peripheral disturbance of the innervation of
the articulatory muscles may cause dysarthria. Lesions may involve the
peripheral nerves, brainstem nuclei, or the central corticobulbar,
extrapyramidal, or cerebellar pathways. Anarthria is a total inability
to articulate because of a defect in the control of the peripheral
speech musculature.
subserve language function may cause aphasia, an abnormality of
language, even though the articulation mechanisms may be intact. Mutism
is a total inability to speak; usually the patient appears to make no
attempt to speak or make sounds. Mutism is usually of psychogenic
origin if present in an apparently otherwise normal patient, but may
occur with lesions of the cerebrum, brainstem, and cerebellum
(especially in children).
|
TABLE 6.1 Differential Diagnosis of Abnormal Speech in the Absence of Obvious Oral Abnormality
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
different pathologic conditions. Disturbances in the respiratory rhythm
interfere with speech, and respiratory muscle weakness causes a feeble
voice with abnormalities in regularity and rhythm. Laryngeal disease
may cause severe speech impairment, but whispered speech may still be
possible. In children, articulation disturbances may be developmental
and are often temporary. Structural abnormalities of the vocal tract,
such as congenital craniofacial defects (cleft palate, cleft lip),
ankyloglossia (abnormal shortness of the frenulum of the tongue;
“tongue-tie”), adenoidal hypertrophy, vocal cord edema or nodules,
nasal obstruction, or perforated nasal septum may cause abnormalities
in sound production. The importance of the teeth in articulation is
apparent in the speech of edentulous patients.
primary muscle diseases affecting the tongue, larynx, and pharynx;
neuromuscular junction disorders; lower motor neuron disease involving
either the cranial nerve nuclei or the peripheral nerves that supply
the muscles of articulation; cerebellar dysfunction, basal ganglia
disease, or disturbances of the upper motor neuron control of
vocalization. Lesions of the hypoglossal nerve or nucleus, or local
disorders of the tongue such as ankyloglossia, may cause impairment of
all enunciation, but with special difficulty pronouncing lingual
sounds. The speech is lisping in character and is clumsy and
indistinct. Paralysis of the laryngeal musculature causes hoarseness,
and the patient may not be able to speak above a whisper; there is
particular difficulty pronouncing vowels. Similar changes occur in
laryngitis and in tumors of the larynx. With unilateral laryngeal
muscle weakness, such as in recurrent laryngeal nerve lesions, the
voice is usually low-pitched and hoarse, but occasionally severe
unilateral vocal cord weakness may be present without much effect on
speech because the normal vocal cord is able to adduct across the
midline and approximate the abnormal cord. Hoarseness due to slight
vocal cord weakness may be brought out by having the patient talk with
the head turned to one side. With paralysis of the cricothyroid, the
voice is hoarse and deep and fatigues quickly. In bilateral abductor
paralysis, speech is moderately affected, but in bilateral total
paralysis it is lost.
detectable impairment of articulation. Weakness of the soft palate
results in nasal speech, caused by inability to seal off the nasal from
the oral cavity. Voice sounds have an added abnormal resonance. There
is special difficulty with the velar sounds, but labials and linguals
are also affected, as much of the air necessary for their production
escapes through the nose. The speech resembles that of a patient with a
cleft palate. Characteristically, b becomes m, d becomes n, and k
becomes ng. Amyotrophic lateral sclerosis and myasthenia gravis are
common causes of this type of speech difficulty.
labials and labiodentals. Dysarthria is noticeable only in peripheral
facial palsy; the facial weakness in the central type of facial palsy
is usually too mild to interfere with articulation. Bell palsy
occasionally causes marked dysarthria because of inability to close the
mouth, purse the lips, and distend the cheeks. Similar articulatory
defects are found in myopathies involving the labial muscles (e.g.,
facioscapulohumeral or oculopharyngeal dystrophy), in cleft lip, and
with wounds of the lips. There is little impairment of articulation in
trigeminal nerve lesions unless the involvement is bilateral; in such
cases there are usually other characteristics of bulbar speech. Trismus
may affect speech because the patient is unable to open the mouth
normally.
articulation may occur in cranial neuropathies. Lesions of the ninth
and eleventh nerves usually do not affect articulation. A unilateral
lesion of CN X causes hypernasality. Lesions involving the vagus
bilaterally distal to the origin of the superior laryngeal nerve may
leave the vocal cords paralyzed in adduction, resulting in a weak voice
with stridor. With more proximal lesions, there is no stridor but the
voice and cough are weak.
junction disorders, often interfere with speech. In myasthenia gravis
(MG), prolonged speaking, such as counting, may cause progressive
weakness of the voice with a decrease in volume and at times the
development of a bulbar or nasal quality, which may even proceed to
anarthria. As the voice fatigues, the speech of a patient with
bulbar
myasthenia may be reduced to an incoherent whisper. An occasional
myasthenic patient must hold the jaw closed with the hand in order to
enunciate.
weakness of the tongue, pharynx, larynx, soft palate, and, to a lesser
extent, the facial muscles, lips, and muscles of mastication. Both
articulation and phonation may be affected; speech is slow and hesitant
with failure of correct enunciation, and all sounds and syllables may
be indistinct. The patient talks as though his mouth were full of
mashed potatoes. Supranuclear lesions involving the corticobulbar
pathways may also cause dysarthria. Unilateral cortical lesions do not
usually affect speech unless they are in the dominant hemisphere and
cause aphasia. Occasionally some dysarthria accompanies aphasia.
Rarely, lesions in the cortical motor areas for articulation may cause
severe dysarthria without aphasia. Both dysarthria and dysprosody, or a
defect in rhythm, melody, and pitch, have been described with localized
frontal lobe lesions; these may be due to an apraxia of speech.
corona radiata, internal capsule, cerebral peduncles, pons, or upper
medulla may cause pseudobulbar palsy with spastic dysarthria. The
muscles which govern articulation are both weak and spastic. Phonation
is typically strained-strangled, and articulation and diadochokinesis
are slow.
Athetotic grimaces of the face and tongue may interfere with speech.
Irregular spasmodic contractions of the diaphragm and other respiratory
muscles, together with spasms of the tongue and pharynx, may give the
speech a curious jerky and groaning character. In addition, there may
be a pseudobulbar element with slurred, indistinct, spastic speech.
When chorea is present, the violent movements of the face, tongue, and
respiratory muscles may make the speech jerky, irregular, and hesitant.
The patient may be unable to maintain phonation and occasionally there
is loss of the ability to speak.
rapid, and soft (hypophonic). There may sometimes be bradylalia, with
feeble, slow, slurred speech because of muscular rigidity and
immobility of the lips and tongue. There is dysprosody and the speech
lacks inflections, accents, and modulation. The patient speaks in a
monotone, and the words are slurred and run into one another. The voice
becomes increasingly weak as the patient talks, and he may become
unable to speak above a whisper; as the speech becomes more indistinct
it may become inaudible or practically disappear. Words may be chopped
off. There may be sudden blocks and hesitations, or speech may stop
abruptly. There may be pathologic repetition of syllables, words, or
phrases (palilalia). Like the parkinsonian gait, the speech may show
festination, with a tendency to hurry toward the end of sentences or
long words.
and pitch. There may be associated tremor of the extremities or head,
or other signs of neurologic dysfunction. Voice tremor may further
complicate the other speech disturbances of parkinsonism. Voice tremor
occurs commonly in essential tremor, a frequently familial syndrome
which most often affects the hands. Fine voice tremors are
characteristic of essential tremor; coarse tremors are more
commensurate with cerebellar disease. Voice tremor is a common
manifestation of anxiety. Lip and chin tremors, when severe, may
interfere with speech. In habit spasms, Tourette syndrome, and
obsessive-compulsive states, there may be articulatory tics causing
grunts, groans, or barking sounds. In Tourette syndrome, palilalia may
also occur.
coordination (scanning speech, ataxic dysarthria, or speech asynergy).
There is a lack of smooth coordination of the tongue, lips, pharynx,
and diaphragm. Ataxic speech is slow, slurred, irregular, labored, and
jerky. Words are pronounced with irregular force and speed, with
involuntary variations in loudness and pitch lending an explosive
quality. There are unintentional pauses causing words and syllables to
be erratically broken, with excessive separation of syllables and
skipped sounds in words producing a disconnected, disjointed,
faltering, staccato articulation (scanning speech). The speech pattern
is reminiscent of a person who is sobbing or breathing hard from
exertion. The unusual spacing of sounds with perceptible pauses
between
words and irregular accenting of syllables may cause a jerky, sing-song
cadence that resembles the reading of poetry. Ataxic speech is
particularly characteristic of multiple sclerosis. It may be
accompanied by grimaces and irregular respirations. Ataxia of the voice
and scanning speech may be more apparent when the patient repeats a
fairly long sentence.
a striking abnormality of voice production. In adductor dysphonia,
irregular involuntary spasms of the vocal muscles causes erratic
adduction of the cords. As the patient strains to speak through the
narrowed vocal tract, the voice takes on a high pitched, choked quality
that varies markedly during the course of a sentence. It is most marked
in stressed vowels.
abnormalities or specific dysfunction of the articulatory apparatus, as
seen in individuals with hearing defects, delayed physical development,
mental retardation, and psychogenic disturbances.
articulation. Speech, but not language, disorders may occur on a
nonorganic basis. Nonorganic voice disorders can take many different
forms and can be caused by a variety of factors. The most common
nonorganic voice disorders are dysphonia and aphonia. Onset is often
abrupt, perhaps in association with emotional trauma; there may be
periods of remission, and the condition may suddenly disappear. The
speech defect may vary in type from time to time. It is often bizarre,
and does not correspond to any organic pattern. The patient may fail to
articulate and speak only by whispering. Speech may be lost but the
patient is able to sing, whistle, and cough. There may be associated
dysphagia and globus hystericus. In anxiety and agitation the speech
may be broken, tremulous, high-pitched, uneven, and breathless.
Stuttering and stammering are common.
resulting deficit reflects the area involved, e.g., hemiparesis with
conditions affecting the posterior frontal lobe, or visual field
defects with conditions affecting the occipital lobe. When disease
affects association cortex or areas of the brain which subserve high
level integrative function, a variety of abnormalities of “higher
cortical function” may result. Aphasia refers to a disorder of
language, including various combinations of impairment in the ability
to spontaneously produce, understand, and repeat speech, as well as
defects in the ability to read and write. A deficit affecting only
speech is usually dysarthria, due to cerebellar disease or weakness or
spasticity of the speech producing musculature.
previously intact language abilities due to brain damage. A more
comprehensive definition considers it a defect in (dysphasia) or loss
of (aphasia) the power of expression by speech, writing, or gestures or
a defect in or loss of the ability to comprehend spoken or written
language or to interpret gestures, due to brain damage. Aphasia implies
that the language disorder is not due to paralysis or disability of the
organs of speech or of muscles governing other forms of expression. The
term dysphasia is not helpful and easily confused with dysphagia, and
has fallen into disuse.
comprehension. The first is the level of “arrival,” a function of the
primary cortical reception areas; at this level language symbols are
perceived, seen, or heard, without further differentiation of the
impulses. The second level is that of “knowing,” or gnostic function,
concerned with the recognition of impulses, formulation of engrams for
recall of stimuli, and revisualization. The third level, the one of
greatest importance in aphasia, has to do with recognition of symbols
in the form of words, or the higher elaboration and association of
learned symbols as a function of language. There are also three levels
of motor speech function. In aphasia, the most elementary of these is
least frequently affected, and the most
complex
most often involved. Most primitive is the emotional level; the patient
may respond to a painful stimulus with an “ouch,” even though other
language functions are entirely absent. Emotional language may be
preserved when all other language functions are lost. Next is the
automatic level, that concerned with casual, automatic speech; the
patient may be able to answer questions with words such as “yes” and
“no,” count, or recite the days of the week, even though other elements
of speech are severely impaired. The highest level is propositional,
volitional, symbolic, or intellectualized language, which is most
easily disrupted and most difficult to repair. Language requires the
use of symbols (sounds, marks, gestures) for communication.
Propositional language is the communication of thoughts, ideas,
feelings, and judgments using words, syntax, semantics, and rules of
conversation. A normal individual is able to understand complex
sentences and make statements that require thought and concentration.
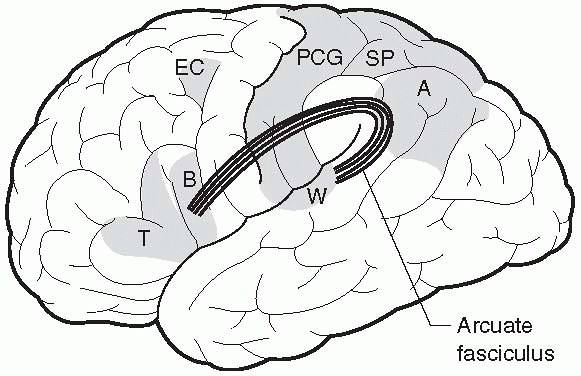
The language areas form a C shaped mass of tissue around the lips of
the Sylvian fissure extending from Broca area to Wernicke area. The
central sulcus intersects the Sylvian fissure near its posterior ramus.
The posterior inferior frontal (PIF) language areas lie in front of the
central sulcus in the frontal lobe and are referred to as anterior or
prerolandic. The posterior superior temporal (PST) areas lie posterior
to the central sulcus and are referred to as posterior or postrolandic.
The anterior speech areas subserve the motor, or expressive, aspects
and the posterior areas the sensory, or perceptive, aspects of
language. Broca speech area lies in the inferior frontal gyrus. It is
essentially the motor association cortex, the executive area for
language function, that lies just anterior to the primary motor areas
for the lips, tongue, and face. The region of the left precentral gyrus
of the insula, a cortical area beneath the frontal and temporal lobes,
seems to be important in the motor planning of speech. Wernicke speech
area lies in the superior temporal gyrus. It is essentially the sensory
association cortex that lies just posterior to the primary auditory
cortex. The arcuate fasciculus is a deep white matter tract that arches
from Wernicke area around the posterior end of the Sylvian fissure and
through the subcortical white matter of the insula to Broca area. Other
tracts in the subcortical white matter of the insula provide additional
connections between the PIF and PST areas. The angular gyrus is part of
the inferior parietal lobule; it caps the posterior ramus of the
Sylvian fissure and lies between Wernicke area and the visual cortex.
The angular gyrus is important for reading
and
similar nonverbal language functions. The supramarginal gyrus also lies
between the visual cortex and the posterior perisylvian language areas
and is involved with visual language functions.
 |
|
FIGURE 6.1
• Centers important in language. A, Angular gyrus; B, Broca area; EC, Exner writing center; SP, Superior parietal lobule, which with the PCG (postcentral gyrus) is important in tactile recognition; T, Pars triangularis;W, Wernicke area. |
during the taking of the history. Obvious deficits require exploration,
but there may be language deficits that are not readily apparent during
history taking, such as the inability to repeat that is the essential
characteristic of conduction aphasia, so some degree of formal
assessment is usually prudent. In evaluating aphasia it is important to
know about the patient’s handedness (and sometimes the familial
tendencies toward handedness), cultural background, native language and
other languages spoken, vocabulary, educational level, intellectual
capacity, and vocation.
left cerebral hemisphere is dominant for language in 99% of right
handers, and 60% to 70% of left handers. Of the remaining left handers,
about half are right hemisphere dominant and about half have mixed
dominance. Since clinical abnormalities of higher cortical function,
especially language, are heavily influenced by dominance, determination
of the patient’s handedness and dominance status is paramount. Cerebral
dominance and handedness are at least in part hereditary. In right
handed patients, aphasia will be due to a left hemisphere lesion in 99%
of the cases; the other 1% are “crossed aphasics.” In left handers the
situation is much more variable.
that are typically tested in the clinical arena: spontaneous
(conversational) speech, auditory comprehension, naming, reading,
writing, and the ability to repeat. It is often useful to assess these
components individually before trying to synthesize the findings into a
diagnostic entity.
spontaneous utterances may include the lower level functions of
emotional and automatic speech. Emotional speech is spontaneous speech
prompted by a high emotional charge. Some patients with aphasia,
primarily non-fluent aphasia, even when severe, may swear and curse
eloquently when angry, often to the shock and surprise of friends and
family. Automatic speech refers to the recitation of simple overlearned
items from early childhood, or to a specific retained speech fragment
which an aphasic patient is still capable of saying even in the
presence of severe non-fluency. Even when unable to produce
propositional speech, an aphasic patient may be able to automatically
count, say the days of the week or months of the year, repeat the
alphabet, say his name, or recite nursery rhymes. Some aphasic patients
are able to sing simple overlearned songs, such as Happy Birthday, even
when they are unable to speak. A retained fragment that an aphasic
patient repeats over and over has been referred to as a monophasia
(recurring utterance, verbal stereotypy, verbal automatism,
verbigeration). In monophasia, the individual’s vocabulary is limited
to a single word, phrase, or sentence, such as “do-do-do” or “Oh, God.”
Verbal automatisms occur most often in global aphasia. The recurrent
utterance may be a real word or a neologism. Sometimes the monophasia
is an outrageous expletive that bursts from an otherwise dignified and
respectable patient under socially awkward circumstances.
substitutes a wrong word or sound for the intended word or sound.
Paraphasic errors are common in aphasic patients. In a phonemic
(phonologic, literal) paraphasia, there is the addition, deletion, or
substitution of a phoneme but the word is recognizable and may be
clearly pronounced. Substitution of the wrong phoneme would cause the
patient to say “blotch” instead of watch, or “thumbness” instead of
numbness. Technically, a literal paraphasia is a single letter
substitution. Phonemic paraphasia is the preferable term since a single
letter substitution also changes the phoneme and the brain thinks in
phonemes, not letters. Illiterate patients commit phonemic paraphasias
despite their ignorance of letters. In a semantic (verbal) paraphasia,
the patient substitutes the wrong word. A semantic paraphasia would
cause the
patient
to say “ring” instead of watch. Paraphasias are similar to the
malapropisms, spoonerisms, and sniglets everyone occasionally utters,
but aphasic patients make them more often and may not recognize them as
wrong. A neologism is a novel utterance, a non-word made up on the
spot. The patient might call a watch a “woshap.” Phonemic paraphasias
are more typical of anterior, and semantic paraphasias more typical of
posterior, perisylvian lesions.
word and sentence formation, fluency, cadence, rhythm, prosody,
omission or transposition of syllables or words, misuse of words,
circumlocutions, repetition, perseveration, paraphasias, jargon, and
the use of neologisms. Aphasic patients may use unusual synonyms or
circumlocutions in order to avoid the use of a word that cannot be
recalled. There may be omissions of words, hesitations and
inappropriate pauses, perseveration, difficulty understanding the
implication of words, verbal automatisms, agrammatism, jargon or
gibberish. When the patient is having difficulty with fluency, it is
difficult to evaluate propositional spontaneous speech. Fluency refers
to the volume of speech output. Normal speech is 100 to 115 words per
minute. Speech output is often as low as 10 to 15 words per minute,
sometimes less, in patients with nonfluent aphasia. If the maximum
sentence length is <7 words, the patient is nonfluent. Patients are
usually aware of nonfluency and frustrated by it. Their speech may tend
toward the laconic, answering questions but trying to speak no more
than necessary. Patience and open ended questions are the best
approaches in persuading the patient to converse. Patients unable to
express themselves through speech may use pantomime or gesture, shaking
or nodding the head, shrugging the shoulders, or demonstrating visible
emotional reactions. In severe aphasia the patient may be unable to
utter a single word.
and to everyday questions and comments give information about his
ability to understand speech. Comprehension may be tested by having the
patient follow verbal commands (“show me your teeth,” “stick out your
tongue,” “close your eyes,” or “point to the ceiling”). Comprehension
can be judged reasonably intact if the patient follows a complicated,
multi-step command, but failure to follow a command, even a simple one,
does not necessarily prove that comprehension is impaired. A patient
may not comply because of apraxia. A patient with a left hemisphere
lesion may even have apraxia for functions of their non-paretic left
hand. They may be unable to salute, wave goodbye, or perform other
simple functions on command using the left hand because of involvement
of fibers that transmit information from the language areas on the left
to the motor areas on the right (sympathetic apraxia). When the patient
does not follow simple commands, establish whether he can say or shake
his head “yes” and “no.” Then ask ridiculous, simple questions, such as
“are you from the planet Jupiter,” “did you have nails for breakfast,”
“are you riding in a taxicab,” or “are you a man (or a woman).” The
answers to the ridiculously simple questions should be known. The
responses may be nonverbal. An elderly woman who laughs when asked “are
you pregnant” has understood the question. More complex yes-no
questions might include “is a mother older than her daughter,” “do you
have dinner before breakfast,” “can you fly in a car,” “did the sun
come up this morning,” or “do you have feet on the ends of your legs.”
Since the chance of a correct response is 50%, it is important to ask
enough questions to exclude lucky answers. The patient may have more
difficulty with polysyllabic words and long sentences than with simple
words and short sentences. Compound sentences and double or complex
commands may be used to see if comprehension is more than superficial.
The aphasia examination begins to overlap with the mental status
examination with commands such as “place one coin on the table, give me
the second, and keep the third in your hand” or “here is a piece of
paper; tear it in four parts and place one on the table, give one to
me, and keep two for yourself.” Both comprehension and retention are
evaluated by telling a short story and then asking questions about it.
Patients with impaired comprehension have particular difficulty with
passive constructions (“the lion was killed by the tiger, which animal
is dead?” or “the boy was slapped by the girl, who got hit?”) and
possessives (is my wife’s brother a man or a woman?).
Patients
who are unable to comprehend spoken or written language may understand
pantomime, gestures, and symbols. They may imitate the examiner in
placing a finger to the nose or putting out the tongue. Imitation,
however, is a lower level function than comprehension.
orientation, especially with posterior lesions. Right-left confusion is
part of Gerstmann syndrome. Testing right-left orientation might
include such commands as “show me your right thumb” or “touch your
right ear with your left thumb.” It is important to determine baseline
function before concluding a patient has right-left confusion.
aphasia examination. Naming is a delicate function, and most aphasic
patients have some difficulty with it. However, naming defects are
nonspecific. In anomic aphasia, an inability to name is an isolated
defect, but more often misnaming occurs as part of some other aphasic,
or even non-aphasic, syndrome. In confrontation naming, the patient is
asked to name simple objects such as a key, pencil, coin, watch, parts
of the body (nose, ear, chin, fingernail, knuckle), or to name colors.
When lost for the name of an object, the patient may describe it or
tell its use. The patient may be able to name an object, such as a
watch, but be unable to identify the component parts, such as the band
or buckle. Some caution is necessary, as there are age, cultural, and
even gender influences at work. When unable to retrieve a name, an
aphasic patient may be able to select the correct name from a list.
Another naming test is to have the patient point to something named by
the examiner, e.g., the telephone, the window.
is word list generation. The patient is asked to name as many items as
possible in a certain category in one minute. Animals are a common
category for testing spontaneous naming. The patient may name any type
of animals (farm, zoo, etc.), but groups should not be suggested ahead
of time since there may be an inability to shift groups. It is wise to
check more than one item category; other useful categories include
tools, foods, countries, and modes of transportation. Spontaneous
naming ability also depends on age and educational level. Normal
patients should name a minimum of 12 items in a category; some
adjustment may be necessary for poorly educated and older patients.
Another measure of spontaneous naming is to ask the patient to list all
the words they can think of that begin with a certain letter. The
“F-A-S” test is popular. The patient thinks of words beginning with one
of these letters, excluding proper nouns or morphological variants. For
FAS, a person of average education should produce 12 or more words per
letter in 1 minute, or 36 words with all three letters in three
minutes. Standardization and reference values for testing naming are
imperfect. Language competence depends on education, dialect,
experience, and other factors. Often the reference population does not
include less well educated people, nor every dialect. Poor word list
generation may also occur with dementia, depression, parkinsonism, and
prefrontal lesions. Responsive naming is also useful, and uses audition
rather than vision. The patient may be asked for nouns (“where do
teachers work”), verbs (“what do you do with a cup”) or adjectives
(“how does sugar taste”).
paradoxically preserved in certain aphasic syndromes. Most often the
inability to repeat is proportional to the defect in comprehension or
fluency, and repetition is a good screening test for aphasia. The
patient is asked to repeat words or phrases back to the examiner. A
patient’s repetition span, the number of words he can repeat, is
usually two more than his digit span. Simple repetition tasks might
include counting, avoiding numbers that might be repeated by automatic
speech, or single words. More complex tasks include polysyllabic words,
such as “catastrophe,” phrases, such as “if he were here, I would go
away,” or tongue twisters such as “Popocatepetl” (po-poh-cah-teh-petl,
a volcano in Mexico). The stock phrases used to test for dysarthria
work for this purpose as well. A popular phrase for testing repetition
in aphasia is “no ifs, ands, or buts.” Omitting the s’s may not be an
error in some
dialects
of English. A better repetition test is “they heard him speak on the
radio last night” (modified from the Boston Diagnostic Aphasia
Examination). Patients with impaired repetition may omit words, change
the word order, or commit paraphasic errors. Repetition is preserved in
anomic, transcortical, and some cases of subcortical aphasia.
also be assessed. It may be disturbed in conjunction with abnormalities
of spoken language, or separately. Patients who are aphasic in speech
are also aphasic in writing, but writing may be preserved in patients
with dysarthria or verbal apraxia. In all aphasias, reading and writing
are typically worse than understanding and speaking, probably because
they are secondarily acquired skills. The patient may be asked to write
spontaneously or to dictation. A spontaneous writing sample might
include a few words, a sentence, or a paragraph. The writing sample
usually reveals the same sorts of naming difficulties and paraphasias
evident in the patient’s speech. Patients may be able to write
elementary, overlearned things such as name, address, days of the week,
and months of the year, but be unable to write more complex material.
There may be a difference in the patient’s ability to print and to
write in cursive.
symbols can be tested by having him read. Written language is perceived
by the visual system and the information conveyed to the perisylvian
language centers. Dysfunction of the language centers or interruption
of the connections with the visual system may cause an inability to
read (alexia). Reading difficulty due to acquired alexia is unrelated
to the developmental (congenital) dyslexia seen most often in
school-age boys that may cause severe reading disability. Patients may
have alexia without any accompanying inability to comprehend speech—the
syndrome of pure word blindness. Alexia may occur with or without a
hemianopia. Alexia may occur with or without accompanying agraphia.
Most patients with alexia also have difficulty with writing (alexia
with agraphia). Some patients have alexia without agraphia, a
disconnection syndrome. Judging reading ability by having the patient
follow a written command such as “close your eyes” involves a praxis
element and should be interpreted with caution. For patients unable to
read aloud, use questions that can be answered by “yes” or “no,” or by
gestures. It is also important to determine whether the patient is able
to read his own writing. Reading aloud is a different task from reading
comprehension, and may be preserved despite impaired reading
comprehension.
disorders vary in severity, even with a lesion in the same location,
and are frequently mixed in type. There have been many attempts at
classification from anatomic, physiologic, and psychological points of
view. None is entirely satisfactory. A strictly anatomic classification
does not apply in all instances, for a small lesion may cause severe
impairment of both fluency and comprehension, while an extensive lesion
sometimes causes an isolated defect. Lesions similar in size and
location on imaging studies may be associated with different aphasic
syndromes even in persons with identical cerebral dominance for speech,
and lesions in different locations and of variable size may produce
similar aphasic syndromes. Nevertheless, some general relationships
exist between anatomic sites and the type of aphasia.
expressive and receptive types. In expressive aphasia, the patient has
difficulty with speech output and struggles to talk (nonfluent); in
receptive aphasia the primary difficulty is with understanding
language, while speech output is unaffected (fluent). A major problem
with the expressive-receptive classification of aphasia is that all
aphasic patients have difficulty expressing themselves. This causes
difficulty, particularly for trainees and non-neurologists. There is a
tendency to classify almost all aphasias as expressive,
even
when they are flagrantly receptive. It requires some clinical
experience to recognize that a patient may be having difficulty
expressing himself linguistically because of a defect in the reception
(comprehension) of spoken language.
|
TABLE 6.2 The Major Aphasia Syndromes
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
and popularized by Benson, Geschwind, and others at the Boston Aphasia
Research Center. It divides aphasias into fluent and nonfluent
varieties (Tables 6.2 and 6.3).
If speech output is high and articulation facile, the aphasia is
referred to as fluent; if speech output is sparse and effortful the
aphasia is classified as nonfluent. Nonfluency occurs when a lesion
involves the anterior speech areas in the region of Broca area in the
frontal lobe. When these areas are relatively spared fluency is
preserved. Broca is a type of nonfluent aphasia. When the posterior
speech areas in the region of Wernicke area in the temporal lobe are
involved, auditory comprehension is impaired. When this area is spared,
comprehension is relatively preserved. The most common fluent aphasia
is Wernicke. In global or total aphasia there is both nonfluency and
impaired comprehension; the lesion may involve both anterior and
posterior speech areas. Other types of aphasia include conduction,
anomic, and transcortical. Difficulty arises because not all patients
can be satisfactorily placed into one of these categories. The clinical
features of aphasia evolve over time. For example, global aphasia can
occur with a purely anterior lesion, but usually evolves into a Broca.
If seen acutely, about 60% to 80% of aphasic patients fit into the
anterior-nonfluent/posterior-fluent classification.
decreased amount of linguistic output: few words, short sentences, and
poor grammar. Any degree of nonfluency is possible, as long as fluency
is impaired compared to comprehension. In severe Broca aphasia the
speech consists of nouns and substantive verbs produced with great
effort. Patients are aware of and frustrated by their difficulty
speaking. There is a tendency to leave out nonessential words such as
adjectives, adverbs, and functor words (articles, pronouns,
conjunctions,
and
prepositions that serve primarily to provide sentence structure rather
than convey meaning). Such parsimonious use of language is sometimes
referred to as telegraphic speech. The patient knows what he wishes to
say, but is unable to say it, or to say it correctly. The ability to
comprehend speech is relatively unimpaired. Because of the severe
nonfluency, patients are unable to repeat what they hear and unable to
read aloud. The patient can identify objects but not name them.
Although the patient is nonfluent for propositional speech, there may
be preservation of emotional and automatic speech, and the patient may
be able to sing. Occasionally speech is reduced to monophasia or
recurrent utterances. The patient is aphasic in writing as in speech,
even when using the non-paretic, usually left, hand. Preservation of
writing suggests verbal apraxia (see below). Patients with Broca
aphasia classically have a contralateral hemiparesis or faciobrachial
paresis, but no visual field deficit.
|
TABLE
6.3 Organization of Common Aphasia Syndromes (According to Whether Spontaneous Speech Is Fluent or Nonfluent and Whether Auditory Comprehension and Repetition Are Good or Poor) |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|
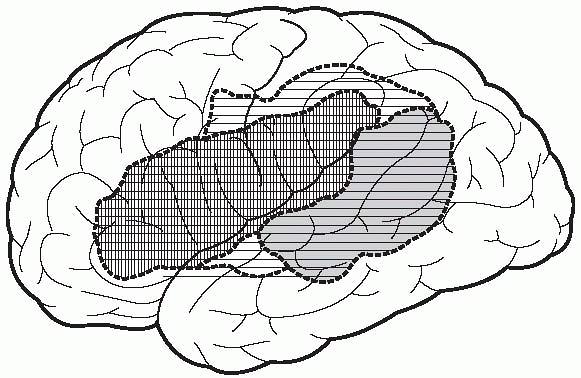
FIGURE 6.2
• The extent of the lesion classically causing global aphasia is indicated by the dashed outer line, the lesion causing Broca aphasia by the crosshatched lines, and the lesion causing Wernicke aphasia by the horizontal lined area. |
control speech but not language. The patient may have difficulty with
speech, but comprehension is perfect and writing is not affected.
Emotional and automatic speech functions are preserved. The problem is
essentially an isolated apraxia for speech, which may or may not be
accompanied by other evidence of buccofacial apraxia. The lesion is
these cases may be confined to Broca area, while in the more typical
case of Broca aphasia the lesion is usually more extensive. This
condition has been called apraxia of speech (AOS; verbal apraxia,
cortical dysarthria, acquired apraxia of speech, Broca area aphasia,
mini-Broca, or baby-Broca). Patients with AOS appear to have forgotten
how to make the sounds of speech. There is speech sound distortion as
their articulatory muscles grope for the right position. There is
defective control but no weakness of the vocal tract. Prosody may be
impaired and speech may have a stuttering quality. The speech pattern
may change so that the patient sounds as though he has developed a
foreign accent.
which involves the auditory association cortex and the angular and
supramarginal gyri (Fig. 6.2). Patients are
unable to understand speech (word deafness). They are relatively
fluent, with a normal or even increased word output (logorrhea), but
there is loss of the ability to comprehend the significance of spoken
words or recall their meaning. Speech production is effortless; phrase
and sentence length and prosody are normal. Although speech is
abundant, it is devoid of meaningful content. The patient can still
hear and can recognize voices, but not the words they utter. Paraphasic
errors are frequent, resulting in incorrect or unintelligible words,
unconventional and gibberish sounds, and senseless combinations. The
speech abounds in neologisms. There is an inability to use proper
syntax, so that sentence structure is defective (paragrammatism). The
resultant misuse of words and defective syntax is termed agrammatism.
There may be circumlocution and an excess of small filler words. Speech
may be fluent but the patient cannot understand his own speech; he is
not aware of, and does not correct, his errors in speaking. The
frequent paraphasias and neologisms, combined with agrammatism, along
with the high word output, may lead to completely unintelligible
speech, termed jargon aphasia or word salad. Hughlings-Jackson
described this type of aphasia as “plentiful words wrongly used.”
Naming and repetition deficits arise from poor comprehension. Patients
with Wernicke aphasia often have a visual field deficit but no
hemiparesis. When due to vascular disease, the ischemia is usually in
the distribution of the inferior division of the MCA.
entire perisylvian language center or separate lesions have destroyed
both the PIF and PST regions (Fig. 6.2).
Grossly nonfluent speech is combined with a severe comprehension
deficit and inability to name or repeat. Typically there is both a
hemiplegia and a visual field cut. Global aphasia is usually due to
internal carotid or proximal MCA occlusion. In some patients,
comprehension improves, leaving a deficit resembling Broca aphasia.
 |
|
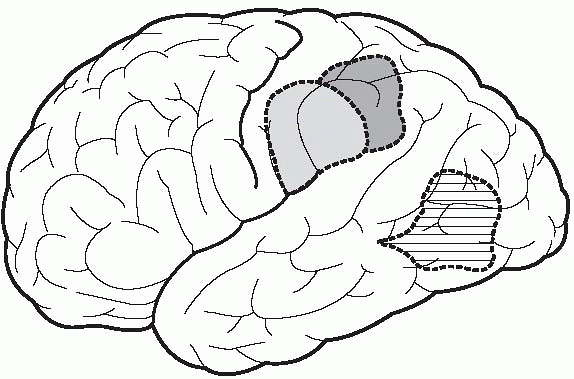
FIGURE 6.3
• The lesion classically causing conduction aphasia is indicated by the lightly shaded area, the lesion causing anomic aphasia by horizontal lines, and the lesion causing the angular gyrus syndrome by the darkly shaded area. |
the conduction of impulses between Wernicke and Broca areas. The
characteristic deficit is poor repetition with preservation of other
language functions. The patient is fluent and comprehension is
unaffected; naming is variable. The lesion most often lies in the deep
white matter in the region of the supramarginal gyrus and involves the
arcuate fasciculus and other fiber tracts that run from the posterior
to the anterior language areas (Fig. 6.3). The
etiology is most often an embolic occlusion of a terminal branch of the
MCA. Because it disconnects the anterior from the posterior perisylvian
language areas, conduction aphasia represents one of the disconnection
syndromes.
with preservation of other language functions. The patients are fluent,
have good comprehension, and are able to repeat. Anomic aphasia is the
most common but least specific type of aphasia. Anomia occurs with
every type of aphasia. Patients with any aphasia type as it develops or
recovers may pass through a stage in which anomia is the primary
finding, and it may be the most persistent deficit. Only when anomia
occurs as an isolated deficit throughout the course of the illness is
the designation anomic aphasia appropriate. When anomic aphasia is
accompanied by all four elements of Gerstmann syndrome, the lesion
virtually always lies in the dominant angular gyrus (Fig. 6.3).
perisylvian language area is preserved but disconnected from the rest
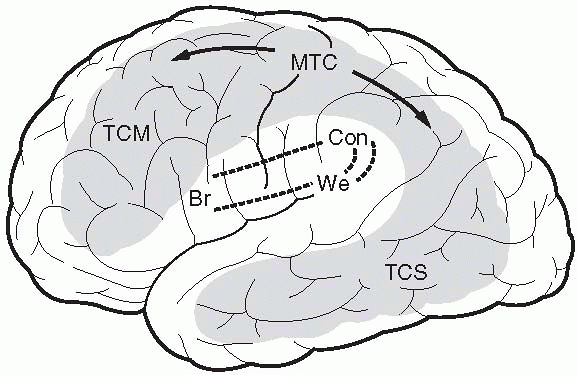
of the brain (Fig. 6.4). The usual etiology is
a watershed (border zone) infarction. Because the PIF and PST areas and
the connecting arcuate fasciculus are intact, the patients are aphasic
but have a paradoxical preservation of the ability to repeat.
Repetition can be so well preserved that the patients display
echolalia, repeating everything they hear. When the condition is severe
and the entire perisylvian language complex is separated from the rest
of the brain, the patients are not fluent in spontaneous speech and are
unable to comprehend. This syndrome has been termed isolation of the
speech area, or mixed transcortical aphasia. When the lesion is
primarily anterior the syndrome resembles Broca aphasia with nonfluency
in spontaneous speech but intact comprehension. Repetition is better
then spontaneous speech. This is the syndrome of transcortical motor
aphasia (anterior isolation syndrome). The supplementary motor area and
dorsolateral
prefrontal
cortex, which are responsible for the planning and initiation of
speech, are isolated from the PIF region. In transcortical sensory
aphasia (posterior isolation syndrome) there is greater involvement of
the posterior language areas. The PST region is isolated from the
surrounding parietal, occipital, and temporal cortex that store word
associations. The patients are fluent, but have difficulty with
comprehension; repetition is better than spontaneous speech. The
transcortical aphasias are more common than is often appreciated.
 |
|
FIGURE 6.4
• Areas typically involved in transcortical aphasias; these correspond to the watershed zones between major arterial distributions. Br, Broca;We, Wernicke; Con, conduction; TCM, transcortical motor; TCS, transcortical sensory; MTC, mixed transcortical. (From Benson DF, Geschwind N. The aphasias and related disturbances. In: Joynt RJ, ed. Clinical Neurology. Philadelphia: J.B. Lippincott, 1990;1-34.) |
arise not from damage to the perisylvian language areas, but from
lesions, usually vascular, involving the thalamus, caudate, putamen, or
internal capsule of the language dominant hemisphere. The speech
disorder is difficult to categorize in the Broca-Wernicke scheme and
may most reasonably be a transcortical aphasia.
hemisphere remains a matter of debate. Non-right-handers, particularly,
are thought to have some speech function in the nondominant hemisphere.
Some of the recovery from aphasia and the persistence of emotional and
automatic speech suggest some language function may be present in the
minor hemisphere. Lesions of the nondominant hemisphere cause speech
disturbances that affect the nonlinguistic elements of language. There
is loss or impairment of the rhythm and emotional elements of language.
Prosody refers to the melodic aspects of speech; the modulation of
pitch, volume, intonation, and inflection that conveys nuances of
meaning and emotional content. Hyperprosody is exaggeration,
hypoprosody a decrease, and aprosody an absence of the prosodic
component of speech. Dysprosody, typically hypoprosody or aprosody, may
occur with right hemisphere lesions. Patients lose the ability to
convey emotion in speech or to detect the emotion expressed by others.
visual perception. With a lesion involving the visual association
cortex, visual perception is intact but there may be impairment of the
ability to recognize and interpret visual stimuli. The region of the
angular gyrus and the adjacent cortex in the dominant hemisphere (Fig. 6.1) is important for the recognition and interpretation of symbols
in the form of letters and words. Connections between the visual cortex
and the dominant angular gyrus are vital for visual recognition of
language symbols. Geschwind said the angular gyrus, “turns written
language into spoken language and vice versa.” Loss of the ability to
read in the absence of actual loss of vision is alexia (word
blindness). A lesion of the angular gyrus, or its connections to the
visual cortex, causes alexia. There is loss of the ability to
recognize, interpret, and recall the meaning of visual language
symbols. Printed words have no meaning, although the patient may talk
without difficulty and understand what is said to him.
incoordination, or other neurologic dysfunction of the arm or hand is
called agraphia. Milder involvement may be referred to as dysgraphia.
There are three types of agraphia: aphasic, constructional, and
apractic. Agraphia is seen in all types of aphasia except pure word
blindness and pure word mutism. Although agraphia typically accompanies
aphasia, it may occur as an isolated finding and as part of other
syndromes in which the patient is not aphasic. Agraphia without alexia
is a feature of Gerstmann syndrome. Agraphia may be manifested as
contraction of words, omission of letters or syllables, transposition
of words, or mirror writing. Having the patient write spontaneously
will usually bring out all the errors present in speech as well as
spelling and letter formation errors. Patients with constructional
apraxia may also have difficulty writing. The visuospatial deficit
interferes with the proper alignment and orientation of the text.
Apractic agraphia is due to inability to properly use the writing hand
in the absence of other deficits.
