Staying Out of Trouble with a Limping Child
|
|
|
TABLE 11-1 Essential Questions When Evaluating a Limp1
|
||||||
|---|---|---|---|---|---|---|
|
important reasons for a child to visit an orthopaedist. The etiology of
abnormal gait in a child can range from the most simple and benign
(transient synovitis or a splinter in the foot) to the most serious
(first presentation of a life-threatening malignancy). To stay out of
trouble, always take the parents’ concern seriously. If a patient’s mom
says there is a limp, you should find it or prove her wrong.
physical exam. Obtaining the best possible history is your first
priority, as it can narrow the long list of possibilities very quickly,
sometimes to the one single cause. Nail down the details regarding how
long the limp has been there and the circumstances surrounding its
first recognition (Table 11-1).
to miss something subtle like a balance problem or a limp that can only
be seen with running. Get the child out into the hallway, dressed in
shorts so you can see the whole lower limb. Do not hesitate to have the
child walk down the hallway many times. The child can even run if there
is room. If you are having trouble seeing the limp, sometimes it helps
to close your eyes and listen for an irregular cadence. As the child
becomes tired, or forgets the doctor is watching, the limp may become
more obvious. Look at one aspect of gait for each lap down the hall,
letting your eye work bottom to top: foot, ankle, knee, pelvis, torso.
(including the bottom of the feet). Look for subtle signs of muscle
atrophy, swelling, or discoloration. When faced with the typically
frustrating scenario of a limping toddler with normal radiographs and
no helpful details in the history, search for the point of maximum
tenderness (PMT). The PMT can sometimes be a little confusing. Thigh or
knee pain (rubbing) is a clue to think of hip pathology. Remember, a
toddler’s fracture does not have to be in the tibia; it can be in the
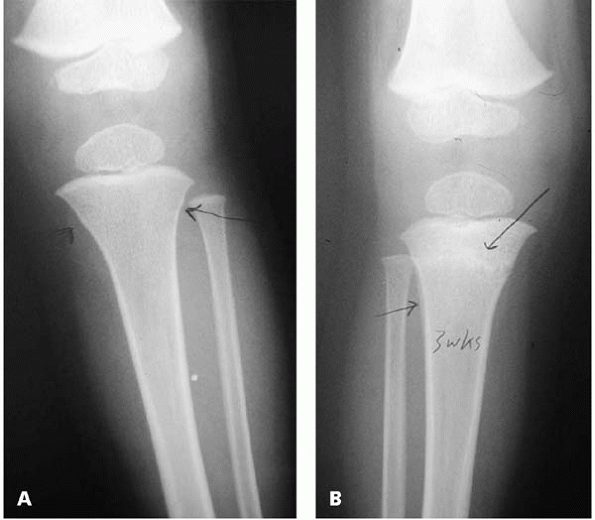
calcaneus or elsewhere (Fig. 11-1).
Unless an obvious source reveals itself quickly (e.g., toddler
fracture), range every joint (and that includes spine
flexion/extension) (Fig. 11-2).
 |
|
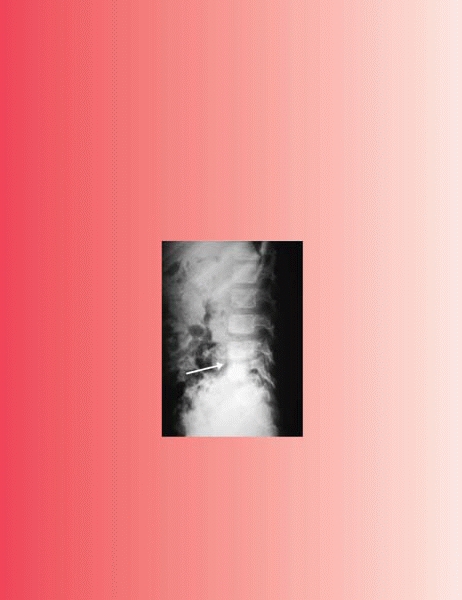
▪ FIGURE 11-1
A “toddler’s fracture” does not always have to be in the tibia. Children who jump down stairs or off playground equipment may sustain a fracture of the calcaneus that can be very difficult to see on initial radiographs. This calcaneus “toddler’s fracture” (arrow) revealed itself after 6 weeks in a short leg cast. |
the differential anatomically, from bottom to top: the ones on the top
are often more serious (spinal cord tumor), more easily overlooked
(discitis), and are more difficult to localize on a physical exam since
the structures are not as superficial (iliacus abscess).
 |
|
▪ FIGURE 11-2 Discitis presenting as a limp. A:
This 6-year-old boy presented with a “limp” that was really an abnormal gait resulting from his efforts to decrease motion in his lumbar spine. He walked with a very straight back and a slight crouch. B: Lateral radiograph of the lumbosacral spine shows decreased disc height at L4-5 consistent with discitis (arrow). |
understand the normal variations of gait in the very young. New walkers
have a wide base gait, poor balance, and a tendency to toe walk, but
none of these are “limps” (except maybe in the worried mind of a new
parent). There are five unique limps, or abnormal gaits, in children:
antalgic, Trendelenburg, spastic, muscle weakness, and short limb gait.
An antalgic limp does not have to come from the leg. It can come from
the spine, pelvis, or sacroiliac joint. Sometimes you need to watch a
longer stretch of walking or get the child to run in order to
appreciate a subtler Trendelenburg gait. In a spastic gait, spasticity
will affect the whole limb, so watch for the effects on multiple joints
one at a time—floor to spine. Look for signs of contracture (equinus,
crouch gait due to hamstring contracture), or decreased motion and its
effects (decreased knee motion is due to rectus spasticity, causing toe
dragging). If suspicious of spasticity, always get the child to run.
You may pick up subtle upper extremity posturing that clinches the
diagnosis (see Fig. 2-2). A muscle weakness
gait is seen in conditions such as Duchenne muscular dystrophy (DMD).
To the uninitiated, this may not look like a limp, just a “funny walk.”
It will be hard for the parent to describe, and it will come on
gradually. You might see a lurch.
Remember that most kids with hemiplegia have a short limb on the
affected side. Do not mistakenly blame LLD when it’s the hemiplegia
that’s causing the limp.
|
TABLE 11-21 Gait Types and Associated Causes
|
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Make the pace and intensity of your workup (lots of tests immediately
vs. watch and revisit) appropriate for the conditions on your
differential diagnosis. Sometimes doing too much testing causes as much
trouble as doing too little: for instance, you find some unrelated red
herring on MRI that someone wants to biopsy and there is really nothing
there, or you put a toddler under general anesthesia for an MRI that’s
not really needed. Good plain radiographs are always the starting
point; they are quick, widely available, sensitive, and specific for
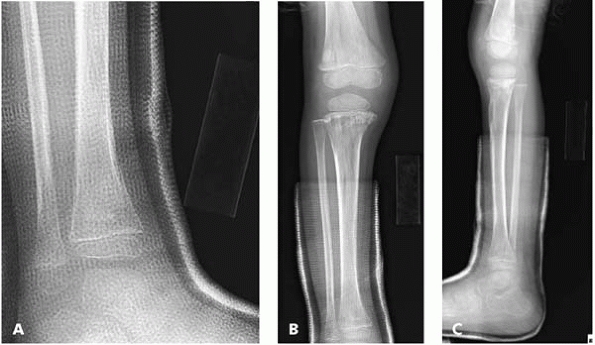
many things on the differential diagnosis (Fig. 11-3).
Oblique radiographs (especially of the foot) are valuable for seeing
subtle abnormalities that might cause a limp. To stay out of trouble,
keep in mind that plain radiographs may reveal no sign of early
osteomyelitis. It can take 10 or more days for signs of infection to
produce radiographic changes of the bone. Instead, the best early
radiographic finding may be soft-tissue swelling. Comparison views may
be helpful in seeing such subtle signs. When dealing with a limping
toddler in whom symptoms cannot be localized, consider plain
radiographs of the entire lower extremity—hip to feet. Tech99 bone scan can be a valuable tool when localization by history and physical with plain radiographs have
failed. Bone scan has been shown to be better than plain films and labs as a screening test for infection in toddlers.4 Keep in mind that a cold on bone scan may indicate a particularly bad case of the osteomyelitis.5
Likewise, leukemia, which presents as musculoskeletal pain 25% of the
time, may result in an increase, decrease, or no change in tech99 uptake4 (Fig. 11-4).
 |
|
▪ FIGURE 11-3
A subtle toddler’s fracture. Although toddler’s fractures are typically a nondisplaced spiral fracture of the tibial shaft, stay out of trouble by imaging the entire bone—or even the entire limb. Good quality plain radiographs showing most of the lower limb will allow you to identify even very subtle changes suggesting a fracture. A: A very subtle cortical irregularity is seen in the proximal tibia. The child was placed in a long leg cast. B: Three weeks after injury, radio-dense metaphyseal bone and periosteal new bone is evident laterally in this healing fracture. |
 |
|
▪ FIGURE 11-4
Leukemia presenting as a limping child. This 3-year-old presented for a second opinion regarding persistent limping after an “ankle fracture” diagnosed at an outside hospital. A: An AP view of the ankle showed no clear sign of a fracture, but did show an irregular appearance to the bone. Fortunately, the treating pediatric orthopaedist sent the child back for a full-length AP and lateral of the tibia. AP (B) and lateral (C) of the entire tibia and distal femur show marked irregularities of the metaphyseal bone at the knee consistent with a systemic process. A rapid and aggressive workup quickly revealed that this child had leukemia. (Case courtesy of R. Davidson, MD.) |
for a hip effusion in a child. Ultrasound can guide a successful
aspiration, which has been shown to decrease the time to OR for septic
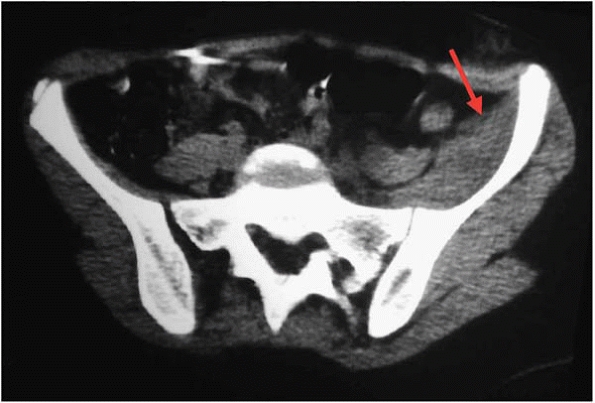
hips by 50%.6 A CT scan can be valuable to diagnose a pelvic cause of a limp (Fig. 11-5).
Although MRI should not be the first test chosen for the limping child,
it is the best way to see processes in the bone marrow, joint, or
cartilage. MRI can be valuable for finding malignancies and stress
fractures once you have localized the area to examine. MRI may be
particularly valuable in identifying the cause of a limp that
originates in the pelvis and spine, as a physical exam is limited in
these areas.
 |
|
▪ FIGURE 11-5
This child’s mysterious limp, thought to be coming from his hip joint, was diagnosed as an abscess of the iliacus muscle, seen on this CT scan cut (arrow). |
|
TABLE 11-31 Differential Diagnosis of Antalgic Gait: Age Factor
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
presents with an acute, nontraumatic limp, especially if there are any
constitutional symptoms, night pain, etc. White blood cell count (WBC)
is the least helpful, as it is neither sensitive nor specific. WBC
differential is helpful when leukemia is a consideration. Erythrocyte
sedimentation rate (ESR) is too slow to rise to be helpful in the early
phase of an acute process. If it is elevated >50 in a limping child,
there is a high likelihood of an infection; if it is >100,
osteomyelitis is likely. C-reactive protein (CRP) rises within 6 hours
of onset of an acute process, and is a better measure than ESR.7
Joint aspiration can be the most important test for septic arthritis
evaluation. Because there is considerable overlap of WBC aspirates for
different conditions, there is no magic number to definitively diagnose
septic arthritis. Between 50,000/mL and 80,000/mL is often used as a
range above which the concern for septic arthritis becomes high.8,9 The WBC differential, gram stain, and clinical picture are more important than the total WBC in the fluid (Table 11-3).
old), do not be fooled by an immature gait. Fractures and infection
usually top the list of most common causes of abnormal gait in this
group. To stay out of trouble, you’ll want to move quickly to nail down
these diagnoses. For toe walkers, get the pregnancy and birth history
(was the child premature?). Idiopathic toe walking should be bilateral;
worry more when it’s unilateral. However, bilateral is not always
benign (DMD, diplegic cerebral palsy). Remember the Gower’s test in
boys.
scenario. Their gait is more mature and adult-like, so it is easier to
recognize a true, pathologic limp. In this age group, infection is less
likely to be the source of a limp compared to toddlers; injury (acute
and overuse) and hip disorders (Legg-Calvé-Perthes, transient
synovitis) become very common etiologies. The diagnosis of Duchenne
muscular dystrophy is often made at this age. One source of trouble is
dismissing symptoms as “growing pains.” Growing pains won’t make you
limp; instead, they are typically transient aching of the lower legs at
night that is variable, intermittent, and then resolves over time. More
worrisome symptoms associated with leg aches include frequent night
awakening, especially with pains referable to one side that cause limp
or other functional problems during the day. The school-age child is
old
enough
to provide a more useful description of the pain. A stress fracture of
a tarsal bone is a frequently overlooked diagnosis that can cause
limping (Fig. 11-6).
 |
|
▪ FIGURE 11-6 Bone scan was used to diagnose this metatarsal stress fracture (red arrow)
in an elite 13-year-old runner. Initial plain radiographs were normal. She did not want to see the doctor because of fear her running would be restricted. A persistent limp led to a bone scan and the diagnosis of stress fracture. |
accurate history and help you localize the cause of the symptoms.
Overuse and acute injury are important etiologies in this age group. In
order to stay out of trouble, realize that occasionally even a teenager
can’t help you with localization. You may not be able to localize the
problem until after completing a good exam, or maybe not until you’ve
done the correct diagnostic test. Examples of elusive diagnoses include
SCFE that masquerades as knee or thigh pain, sacroiliac problems that
seem to be the garden-variety low back pain, and stress fractures that
cause vague regional symptoms. Be careful when dealing with the teenage
group. Teens can be very manipulative of any situation. Secondary gain
rears its head in this age group. Teenagers can exaggerate symptoms to
avoid something (such as gym class) or they can minimize symptoms so
that they’ll be permitted to participate (such as their high school
basketball game).
-
If a patient’s mom says there is a limp, you should find it or prove her wrong.
-
Do not allow the
confines of the exam room to cause you to miss something subtle like a
balance problem or a limp that can only be seen with running. -
A toddler’s fracture does not have to be the tibia; it can be the calcaneus, or elsewhere.
-
Always perform a Gower’s test. This is easy to do, hard to remember to do.
-
Oblique radiographs (especially of the foot) are valuable for seeing subtle abnormalities that might cause a limp.
-
Leukemia, which presents as musculoskeletal pain 25% of the time, may result in increase, decrease, or no change on bone scan.
-
Idiopathic toe
walking should be bilateral; worry more when it’s unilateral. However,
bilateral is not always benign (DMD, diplegic cerebral palsy). -
Growing pains shouldn’t make a child limp.
MJ, McGuire KJ, McGowan KL, et al. Assessment of the test
characteristics of C-reactive protein for septic arthritis in children.
J Pediatr Orthop. 2003;23(3):373-377.