Fractures of the Midfoot and Forefoot
-
Injuries to the midfoot are relatively rare.
-
The midfoot is the section of the foot distal to Chopart joint line and proximal to Lisfranc joint line (Fig. 41.1).
-
Five bones comprise the midfoot: the navicular, cuboid, and the medial, middle, and lateral cuneiforms.
-
The midtarsal joint consists of the
calcaneocuboid and talonavicular joints, which act in concert with the
subtalar joint during inversion and eversion of the foot. -
The cuboid acts as a linkage across the three naviculocuneiform joints, allowing only minimal motion.
-
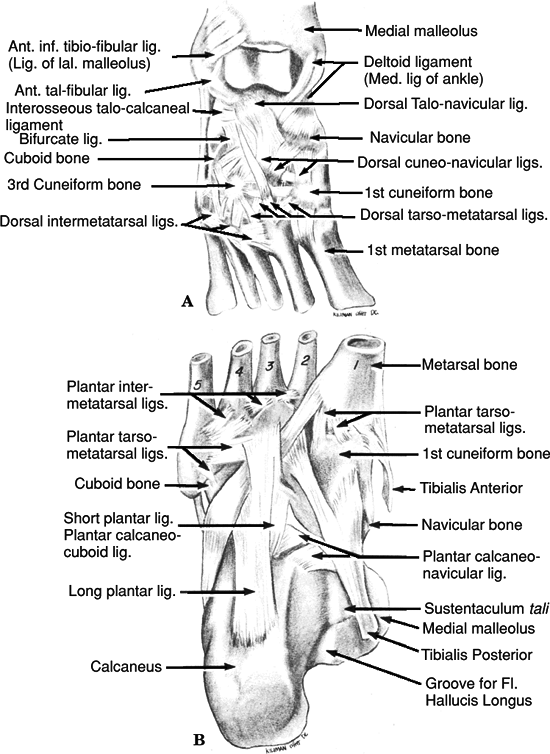
Ligamentous attachments include the
plantar calcaneonavicular (spring) ligament, bifurcate ligament, dorsal
talonavicular ligament, dorsal calcaneocuboid ligament, dorsal
cuboidonavicular ligament, and long plantar ligament (Fig. 41.2).
-
High-energy trauma: This is most common
and may result from direct impact from a motor vehicle accident or a
combination of axial loading and torsion, such as during impact from a
fall or jump from a height. -
Low-energy injuries: This may result in a sprain during athletic or dance activities.
-
Patient presentation is variable, ranging
from a limp with swelling and tenderness on the dorsum of the midfoot
to nonambulatory status with significant pain, gross swelling,
ecchymosis, and variable deformity. -
Stress maneuvers consist of forefoot
abduction, adduction, flexion, and extension and may result in
reproduction of pain and instability. -
A careful neurovascular examination
should be performed. In cases of extreme pain and swelling, serial
examinations may be warranted to evaluate the possibility of foot
compartment syndrome.
-
Anteroposterior (AP), lateral, and oblique radiographs of the foot should be obtained.
-
Stress views or weight-bearing x-rays may help to delineate subtle injuries.
-
Computed tomography (CT) may be helpful in characterizing fracture-dislocation injuries with articular comminution.
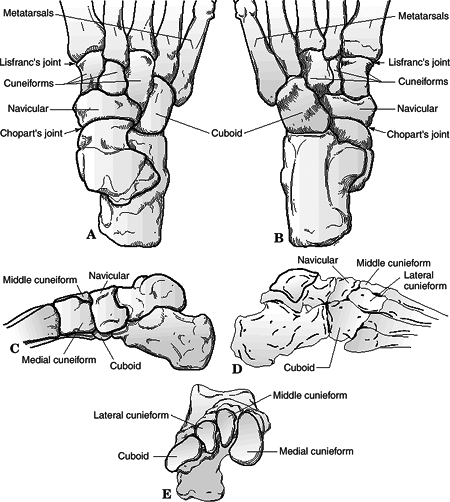 Figure
Figure
41.1. Bony anatomy of the midfoot. (A) Dorsal view. (B) Plantar view.
(C) Medial view. (D) Lateral view. (E) Coronal view.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Magnetic resonance imaging (MRI) may be used to evaluate ligamentous injury.
-
Inversion injury occurs with adduction of the midfoot on the hindfoot.
-
Flake fractures of the dorsal margin of
the talus or navicular and of the lateral margin of the calcaneus or
the cuboid may indicate a sprain. -
In more severe injuries, the midfoot may
be completely dislocated, or there may be an isolated talonavicular
dislocation. A medial swivel dislocation is one in which the
talonavicular joint is dislocated, the subtalar joint is subluxed, and
the calcaneocuboid joint is intact.
 |
|
Figure
41.2. Ligamentous structure of the midfoot. (A) The dorsal view shows extensive overlap of the interosseous ligaments. (B) The plantar ligaments are thicker than their dorsal counterparts and are dynamically reinforced by the tibialis anterior, tibialis posterior, and peroneus longus tendons. Note the extensive attachments of the tibialis posterior throughout the midfoot bones. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Force is transmitted through the
metatarsal heads proximally along the rays with resultant compression
of the midfoot between the metatarsals and the talus with the foot
plantar flexed. -
Longitudinal forces pass between the cuneiforms and fracture the navicular typically in a vertical pattern.
-
“Nutcracker fracture”: This is the
characteristic fracture of the cuboid as the forefoot driven laterally,
crushing the cuboid between the calcaneus and the fourth and fifth
metatarsal bases. -
Most commonly, this is an avulsion fracture of the navicular with a comminuted compression fracture of the cuboid.
-
In more severe trauma, the talonavicular
joint subluxes laterally, and the lateral column of the foot collapses
because of comminution of the calcaneocuboid joint.
-
Forces directed at the plantar region may
result in sprains to the midtarsal region with avulsion fractures of
the dorsal lip of the navicular, talus, or anterior process of the
calcaneus.
-
Sprains: Nonrigid dressings are used with protected weight bearing for 4 to 6 weeks; prognosis is excellent.
-
Nondisplaced fractures may be treated with a short leg cast or boot with initial non–weight bearing for 6 weeks.
-
High-energy mechanisms resulting in
displaced fracture patterns often require open reduction and internal
fixation (ORIF; e.g., with Kirschner wires or lag screws) and/or
external fixation. -
Prognosis is often poor, depending on the degree of articular incongruity.
-
Bone grafting of the cuboid may be necessary in lateral stress injuries.
-
Severe crush injuries with extensive comminution may require arthrodesis to restore the longitudinal arch of the foot.
-
Posttraumatic osteoarthritis may occur as
a result of residual articular incongruity or chondral injury at the
time of trauma. If severe and debilitating, it may require arthrodesis
for adequate relief of symptoms.
-
Isolated fractures of the navicular are
rare and should be diagnosed only after ruling out concomitant injuries
to the midtarsal joint complex.
-
The navicular is the keystone of the medial longitudinal arch of the foot.
-
It is wider on its dorsal and medial aspect than on its plantar and lateral aspect.
-
The medial prominence known as the
navicular tuberosity provides the attachment point for the posterior
tibialis on its medial inferior surface. -
Proximally, the articular surface is
concave and articulates with the talus. This joint enjoys a significant
arc of motion and transmits the motion of the subtalar joint to the
forefoot. It is the point from which forefoot inversion and eversion
are initiated. -
The distal articular surface of the
navicular has three separate broad facets that articulate with each of
the three cuneiforms. These joints provide little motion; they mainly
dissipate loading stresses. -
Laterally, the navicular rests on the dorsal medial aspect of the cuboid with a variable articular surface.
-
Thick ligaments on its plantar and dorsal
aspect support the navicular cuneiform joints. The spring ligament and
superficial deltoid provide strong support to the plantar and medial
aspects of the talonavicular joint. -
Anatomic variants to be aware of when
viewing the navicular involve the shape of the tuberosity and the
presence of an accessory navicular (os tibiale externum). They are
present up to 15% of the time and bilateral 70% to 90%.
-
Direct blow, although uncommon, can cause avulsions to the periphery or crush injury in the dorsal plantar plane.
-
More often, indirect forces of axial
loading either directly along the long axis of the foot or obliquely
cause navicular injury. -
Injury may result from a fall from a
height or a motor vehicle accident. Fractures may occur in running and
jumping athletes, with increased risk in patients with a cavus foot or
calcaneal navicular coalition.
-
Patients typically present with a painful foot and dorsomedial swelling and tenderness.
-
Physical examination should include
assessment of the ipsilateral ankle and foot, with careful palpation of
all bony structures to rule out associated injuries.
-
AP, lateral, medial oblique and lateral
oblique views should be obtained to ascertain the extent of injury to
the navicular as well as to detect associated injuries. -
If possible, the initial films should be weight bearing to detect ligamentous instability.
-
Medial and lateral oblique x-rays of the
midfoot will aid in assessing the lateral pole of the navicular as well
as the medial tuberosity. -
CT may be obtained to better characterize the fracture.
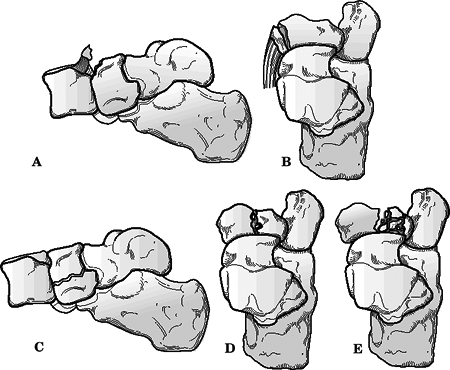 Figure
Figure
41.3. The present popular classification of navicular fractures is
composed of three basic types with a subclassification for body
fractures suggested by Sangeorzan. (A) Avulsion-type fracture can
involve either the talonavicular or naviculocuneiform ligaments. (B)
Tuberosity fractures are usually traction-type injuries with disruption
of the tibialis posterior insertion without joint surface disruption.
(C) A Type I body fracture splits the navicular into dorsal and plantar
segments. (D) A Type II body fracture cleaves into medial and lateral
segments. The location of the split usually follows either of the two
intercuneiform joint lines. Stress fractures are usually included in
this group. (E) A Type III body fracture is distinguished by
comminution of the fragments and significant displacement of the medial
and lateral poles.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
MRI or technetium scan may be obtained if a fracture is suspected but not apparent by plain radiography.
-
The most commonly used classification of
navicular fractures is composed of three basic types with a
subclassification for body fractures (Sangeorzan) (Fig. 41.3).-
Avulsion-type fracture can involve either the talonavicular or naviculocuneiform ligaments.
-
Tuberosity fractures are usually traction
type injuries with disruption of the tibialis posterior insertion
without joint surface disruption. -
Type I body fracture splits the navicular into dorsal and plantar segments.
-
Type II body fractures cleave into medial
and lateral segments. The location of the split usually follows either
of the two intercuneiform joint lines. Stress fractures can usually be
included in this group. -
Type III body fractures are distinguished
by comminution of the fragments and significant displacement of the
medial and lateral poles.
P.449 -
-
Excessive flexion or eversion of midfoot
results in a dorsal lip avulsion of the navicular by the talonavicular
capsule and the anterior fibers of the deltoid ligament. -
Symptomatic, small, nonarticular
fragments may be excised. Large fragments (>25% articular surface)
may be reattached with a lag screw.
TUBEROSITY FRACTURES (20% TO 25%)
-
Forced eversion injury causes avulsion of the tuberosity by the posterior tibial tendon insertion or deltoid ligament.
-
This is often part of the “nutcracker fracture,” so concomitant midtarsal injury must be excluded.
-
One must rule out the presence of an accessory navicular, which is bilateral in 70% to 90% of cases.
-
If symptomatic, small fragments can be
excised and the posterior tibial tendon reattached; larger fragments
require ORIF with lag screw fixation, especially if posterior tibial
tendon function is compromised.
-
These occur primarily in young athletes.
-
They frequently require bone scan or MRI for diagnosis.
-
The fracture line is usually sagittally oriented in the middle third and may be complete or incomplete.
-
Owing to increased incidence of
persistent problems with pain and healing, screw fixation with
autologous bone grafting should be used with comminuted fractures.
satisfactory outcome are maintenance or restoration of the medial
column length and articular congruity of the talonavicular joint.
-
Nondisplaced fractures of the navicular should be treated in a short leg cast or boot with non–weight bearing for 6 to 8 weeks.
-
Repeat radiographs should be done at 10
to 14 days after the initial injury to confirm the absence of bony or
soft tissue instability. If instability appears or other injuries
become apparent, appropriate surgical intervention should be considered.
-
Surgical indications
-
Any unstable injury or fracture resulting in loss of position or articular congruity should be treated surgically.
-
Because the joint is concave, a 2-mm
separation in any plane is considered incongruent. Most authors agree
these injuries need to be managed aggressively with surgery. -
Cortical avulsion fractures found to
involve a significant portion of the dorsal anterior surface should be
considered for operative treatment.
-
-
Surgical management
-
Individual fragments are stabilized using small or minifragment screws.
-
Bone graft should be considered for crushed areas requiring elevation.
-
If anatomic restoration of 60% or more of
the talonavicular surface can be achieved, an effort should be made to
salvage the joint. -
If more than 40% of the articular surface cannot be reconstructed, an acute talonavicular fusion should be considered.
-
-
Postoperative management
-
Cast or brace immobilization with non–weight bearing is recommended for 12 weeks.
-
-
These include nonunion, arthritic
degeneration, late instability, loss of normal foot alignment through
bony resorption or collapse, and osteonecrosis. -
Osteonecrosis: The risk is increased with
significantly displaced, markedly comminuted fractures. It may result
in collapse of the navicular, with need for bone grafting and internal
fixation. -
Posttraumatic osteoarthritis may occur as a result of articular incongruity, chondral damage, or free osteochondral fragments.
-
Isolated dislocation or subluxation of the navicular is rare.
-
The mechanism is hyperplantar flexion of the forefoot with subsequent axial loading.
-
Open reduction is usually necessary to restore both navicular position and articular congruity.
-
Injury to the cuboid can occur as an
isolated entity but is usually seen in association with injuries to the
talonavicular joint or other midfoot structures or in conjunction with
Lisfranc injuries.
-
The cuboid is part of the lateral support column of the foot.
-
The cuboid articulates with the calcaneus
proximally, the navicular and lateral cuneiform medially, and the
lateral two metatarsals distally. -
Its plantar aspect forms a portion of the
roof of the peroneal groove through which the peroneus longus tendon
runs; scarring and irregularity of the peroneal groove caused by cuboid
fracture may compromise function of peroneus longus tendon.
-
Direct: This is uncommon; trauma to the dorsolateral aspect of the foot may result in fractures of the cuboid.
-
Indirect: This accounts for most cuboid fractures.
-
“Nutcracker injury”: Torsional stress or
forefoot abduction may result in impaction of the cuboid between the
calcaneus and the lateral metatarsals. -
Extreme plantar flexion may cause
isolated sprain or dislocation of calcaneocuboid joint in high-velocity
trauma, dance injuries, or patients with Ehlers-Danlos syndrome.
-
-
Stress fractures may occur in athletic individuals.
-
Patients typically present with pain, swelling, and tenderness to palpation at the dorsolateral aspect of the foot.
-
Palpation of all bony structures of the foot should be performed to rule out associated injuries.
-
Pain on the lateral aspect of the foot
may be confused with symptoms of peroneal tendonitis in cases of stress
fractures of the cuboid.
-
AP, lateral, and oblique views of the foot should be obtained.
-
Multiple medial oblique radiographic
views may be needed to see the articular outlines of both the
calcaneocuboid and cuboid metatarsal joints. -
As with other potential midfoot problems,
weight-bearing or stress views should be obtained to rule out
interosseus instability of surrounding structures. -
A small medial or dorsal avulsion fracture of the navicular is considered a sign of possible cuboid injury.
-
CT scan may be necessary to assess the extent of injury and instability.
-
MRI or bone scan may be used for diagnosing a stress fracture.
-
Isolated fractures of the cuboid with no
evidence of loss of osseous length or interosseus instability can be
treated in a cast or removable boot. -
Non–weight bearing for 4 to 6 weeks is recommended.
-
ORIF is indicated if there is more than 2 mm of joint surface disruption or any evidence of longitudinal compression.
-
Severe comminution and residual articular
displacement may necessitate calcaneocuboid arthrodesis for proper foot
alignment and to minimize late complications.
-
Osteonecrosis: This may complicate severely displaced fractures or those with significant comminution.
-
Posttraumatic osteoarthritis: This may result from articular incongruity, chondral damage, or free osteochondral fragments.
-
Nonunion: This may occur with significant
displacement and inadequate immobilization or fixation. If severely
symptomatic, it may necessitate ORIF with bone grafting.
-
These usually occur in conjunction with tarsometatarsal injuries.
-
The usual mechanism is indirect axial loading of the bone.
-
Localized tenderness over the cuneiform
region, pain in the midfoot with weight bearing, or discomfort with
motion through the tarsometatarsal joints can signify injury to these
bones. -
AP, lateral, and oblique views should be obtained. These should be weight bearing if possible.
-
Coronal and longitudinal CT scan of the midfoot can be used to better define the extent of the injury.
-
These are generally considered rare.
-
Approximately 20% of Lisfranc injuries may be initially overlooked (especially in polytraumatized patients).
-
In the AP plane, the base of the second
metatarsal is recessed between the medial and lateral cuneiforms. This
limits translation of the metatarsals in the frontal plane. -
In the coronal plane, the middle three
metatarsal bases are trapezoidal, forming a transverse arch that
prevents plantar displacement of the metatarsal bases. The second
metatarsal base is the keystone in the transverse arch of the foot. -
There is only slight motion across the
tarsometatarsal joints, with 10 to 20 degrees of dorsal plantar motion
at the fifth metatarsocuboid joint and progressively less motion
medially except for the first metatarsocuneiform (20 degrees of plantar
flexion from neutral). -
The ligamentous support begins with the strong ligaments linking the bases of the second through fifth metatarsals. The most
P.453
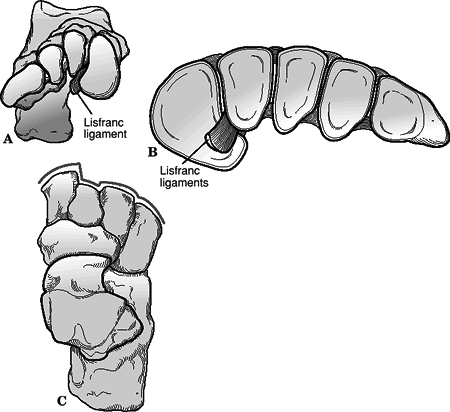
important ligament is Lisfranc ligament, which attaches the medial cuneiform to the base of the second metatarsal.![]() Figure
Figure
41.4. The anatomy of the tarsometatarsal joints. (A) Proximal view of
the cuneiform and cuboid articular surfaces. (B) Distal view of the
corresponding articular surfaces of the metatarsals. (C) Schematic
representation of the contour of the tarsometatarsal joint line. Note
the keying in place of the base of the second metatarsal.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Ligamentous, bony, and soft tissue
support provides for intrinsic stability across the plantar aspect of
Lisfranc joint; conversely, the dorsal aspect of this articulation is
not reinforced by structures of similar strength. -
There is no ligamentous connection between the base of the first and second metatarsals.
-
The dorsalis pedis artery dives between
the first and second metatarsals at Lisfranc joint and may be damaged
during injury or reduction.
-
Twisting: Forceful abduction of the
forefoot on the tarsus results in fracture of the base of the second
metatarsal and shear or crush fracture of the cuboid. Historically,
this was seen in equestrian accidents when a rider fell from a horse
with a foot
P.454
engaged in a stirrup. It is commonly seen today in motor vehicle accidents. -
Axial loading of a fixed foot may be seen
with (1) extrinsic axial compression applied to the heel such as a
heavy object striking the heel of a kneeling patient or (2) extreme
ankle equinus with axial loading of the body weight, such as a missed
step off a curb or landing from a jump during a dance maneuver. -
Crushing mechanisms are common in
industrial-type injuries to Lisfranc joint, often with sagittal plane
displacement, soft tissue compromise, and compartment syndrome.
-
Patients present with variable foot deformity, pain, swelling, and tenderness on the dorsum of the foot.
-
Diagnosis requires a high degree of clinical suspicion.
-
Twenty percent are misdiagnosed.
-
Forty percent have no treatment in the first week.
-
-
Be wary of the diagnosis of “midfoot sprain.”
-
A careful neurovascular examination is
essential, because dislocation of Lisfranc joint may be associated with
impingement on or partial or complete laceration of the dorsalis pedis
artery. In addition, dramatic swelling of the foot is common with
high-energy mechanisms; compartment syndrome of the foot must be ruled
out on the basis of serial neurovascular examination or compartment
pressure monitoring if necessary. -
Stress testing may be performed by gentle
passive forefoot abduction and pronation, with the hindfoot firmly
stabilized in the examiner’s other hand. Alternatively, pain can
typically be reproduced by gentle supination and pronation of the
forefoot.
-
The medial border of the second metatarsal should be colinear with the medial border of the middle cuneiform on the AP view (Fig. 41.5).
-
The medial border of the fourth metatarsal should be colinear with the medial border of the cuboid on the oblique view (Fig. 41.6).
-
Dorsal displacement of the metatarsals on the lateral view is indicative of ligamentous compromise.
-
Flake fractures around the base of the second metatarsal are indicative of disruption of Lisfranc joint.
-
Weight-bearing radiographs provide a stress film of the joint complex.
-
If clinically indicated,
physician-directed stress views should be obtained. The forefoot is
held in abduction for the AP view and in plantar flexion for the
lateral view. -
A CT scan can be used to assess the plantar osseous structures as well as the amount of intraarticular comminution.
-
Fractures of the cuneiforms, cuboid, and/or metatarsals are common.
-
The second metatarsal is the most frequent associated fracture.
 |
|
Figure 41.5. Anteroposterior view of the tarsometatarsal joint. Normal joint alignment on weight bearing.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
clinician in defining the extent and pattern of injury, although they
are of little prognostic value.
| Homolateral: | All five metatarsals displaced in the same direction |
| Isolated: | One or two metatarsals displaced from the others |
| Divergent: | Displacement of the metatarsals in both the sagittal and coronal planes |
 |
|
Figure 41.6. Medial oblique view of the tarsometatarsal joint. Normal joint alignment on weight bearing.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Injuries that present with painful weight
bearing, pain with metatarsal motion, and tenderness to palpation but
fail to exhibit any instability should be considered a sprain. -
Patients with nondisplaced ligamentous
injuries with or without small plantar avulsion fractures of the
metatarsal or tarsal bones should be placed in a well-molded short leg
cast or removable boot. -
Initially, the patient is kept non–weight bearing with crutches and is permitted to bear weight as comfort allows.
-
Repeat x-rays are necessary once swelling decreases, to detect osseous displacement.
-
This should be considered when displacement of the tarsometatarsal joint is >2 mm.
-
The best results are obtained through anatomic reduction and stable fixation.
-
The most common approach is using two
longitudinal incisions. The first is centered over the first/second
intermetatarsal space allowing identification of the neurovascular
bundle and access
P.457P.458
to the medial two tarsometatarsal joints. A second longitudinal incision is made over the fourth metatarsal.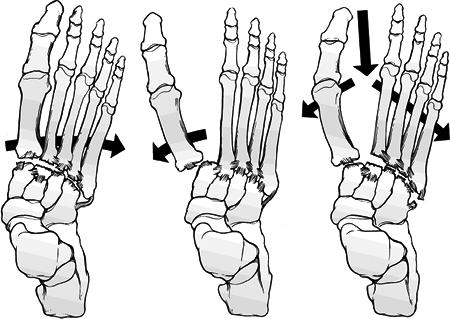 Figure
Figure
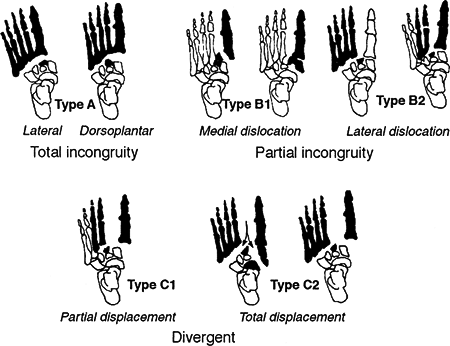
41.7. The common classification devised by Quenu and Kuss. Further
subdivisions are used to identify the direction of dislocation in the
homolateral pattern (medial or lateral) and the partial disruption
(first or lesser).(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)![]() Figure 41.8. Myerson classification of Lisfranc fracture-dislocations.(From Myerson
Figure 41.8. Myerson classification of Lisfranc fracture-dislocations.(From Myerson
MS, Fisher RT, Burgess AR, et al. Fracture-dislocations of the
tarsometatarsal joints: end results correlated with pathology and
treatment. Foot Ankle 1986;6:225–242.) -
The key to reduction is correction of the
fracture-dislocation of the second metatarsal base. Clinical results
suggest that accuracy and maintenance of reduction are of utmost
importance and correlate directly with the overall outcome. -
Once reduction is accomplished, screw fixation is advocated for the medial column.
-
The lateral metatarsals frequently reduce with the medial column, and Kirschner wire fixation is acceptable.
-
If intercuneiform instability exists, one should use an intercuneiform screw.
-
Stiffness from ORIF is not of significant concern because of the already limited motion of the tarsometatarsal joints.
-
The foot is immobilized in a non–weight-bearing cast or boot for 6 to 8 weeks.
-
Progressive weight bearing is then permitted as comfort allows.
-
Advancement out of cast immobilization is done once pain-free, full weight bearing is achieved.
-
Lateral column stabilization can be removed at 6 to 12 weeks.
-
Medial fixation should not be removed for 4 to 6 months.
-
Some advocate leaving screws indefinitely unless symptomatic.
-
Posttraumatic arthritis
-
Present in most, but may not be symptomatic
-
Related to initial injury and adequacy of reduction
-
Treated with arthrodesis for the medial column
-
Possibly treated with interpositional arthroplasty for the lateral column
-
-
Compartment syndrome
-
Infection
-
Complex mediated regional pain syndrome (RSD)
-
Neurovascular injury
-
Hardware failure
-
The forefoot serves two purposes during gait.
-
As a unit, it provides a broad plantar
surface for load sharing. Weight-bearing studies show that the two
sesamoids and the four lesser metatarsal heads share an equal amount of
the forefoot load in normal gait. -
The forefoot is mobile in the sagittal
plane. This enables the forefoot to alter the position of the
individual metatarsal heads to accommodate uneven ground.
-
-
This is a common injury; however, the
true incidence of metatarsal shaft fractures is unknown, owing to the
variety of physicians treating such injuries.
-
Displaced fractures of the metatarsals result in the disruption of the major weight-bearing complex of the forefoot.
-
Disruptions produce an alteration in the
normal distribution of weight in the forefoot and lead to problems of
metatarsalgia and transfer lesions (intractable plantar keratoses).
-
Direct: This most commonly occurs when a heavy object is dropped on the forefoot.
-
Twisting: This occurs with body torque
when the toes are fixed, such as when a person catches the toes in a
narrow opening with continued ambulation. -
Avulsion: This occurs particularly at the base of the fifth metatarsal.
-
Stress fractures: These occur especially at the necks of the second and third metatarsals and the proximal fifth metatarsal.
-
Patients typically present with pain, swelling, and tenderness over the site of fracture.
-
Neurovascular evaluation is important, as well as assessment of soft tissue injury and ambulatory capacity.
-
In isolated injuries to the foot, weight-bearing films should be obtained in the AP and lateral planes.
-
The lateral radiographic view of the metatarsals is important for judging sagittal plane displacement of the metatarsal heads.
-
Oblique views can be helpful to detect minimally displaced fractures.
-
Except in the case of an isolated direct
blow, initial films should include the whole foot to rule out other
potential collateral injuries that may also require attention. -
MRI and technetium bone scan may aid in the diagnosis of an occult stress fracture.
-
This bone is larger and stronger than the lesser metatarsals and is less frequently injured.
-
The lack of interconnecting ligaments between the first and second metatarsal bones allows independent motion.
-
The first metatarsal head supports two sesamoid bones, which provide two of the six contact points of the forefoot.
-
Injuries usually relate to direct trauma (often open and/or comminuted).
-
Anatomic reduction and stable fixation are important.
-
If no evidence of instability can be seen
on stress films, and no other injury of the midfoot or metatarsals is
evident, isolated first metatarsal fractures can be adequately treated
with a short leg cast or removable boot with weight bearing as
tolerated for 4 to 6 weeks. -
Malunion, nonunion, and arthritic
degeneration of the tarsometatarsal and metatarsophalangeal (MTP)
joints are all possible complications of first metatarsal fractures.
Transfer metatarsalgia to the lesser toes can occur with shortening of
the metatarsal length.
-
The four lesser metatarsals provide only one contact point each on the plantar weight-bearing surface.
-
Significant ligamentous structures link each of the bones to their adjacent neighbors.
-
Fractures of the central metatarsals are
much more common than first metatarsal fractures and can be isolated or
part of a more significant injury pattern. -
Indirect twisting mechanisms may result
in a spiral pattern. One must be wary of Lisfranc injury with
involvement of base of second metatarsal. -
Most isolated individual central
metatarsal fractures can be treated closed with hard-soled shoes and
progressive weight bearing as tolerated. -
The surgical criterion most often
mentioned is any fracture displaying more than 10 degrees of deviation
in the dorsal plantar plane or 3 to 4 mm translation in any plane. -
Complications of treating central metatarsal fractures usually stem from incomplete restoration of plantar anatomy.
-
These usually result from direct trauma.
-
Fractures are separated roughly into two groups, proximal base fractures and distal spiral fractures.
-
Proximal fifth metatarsal fractures are further divided by the location of the fracture and the presence of prodromal symptoms (Fig. 41.9).
-
Zone 1: cancellous tuberosity (93%)
-
Insertion of the peroneal brevis and plantar fascia
-
Involvement of the metatarsocuboid joint
-
-
Zone 2: distal to the tuberosity (4%)
-
Zone 3: distal to the proximal ligaments (3%)
-
Extension to the diaphysis for 1.5 cm
-
Usually stress fractures
-
-
-
Zone 1 injury
-
This results from avulsion from lateral plantar aponeurosis.
-
Treatment is symptomatic, with a hard-soled shoe.
-
Healing is usually uneventful.
-
-
Zone 2 injuries are true Jones fractures.
-
They result from adduction or inversion of the forefoot.
-
The fracture is caused by tensile stress along the lateral border of the metatarsal.
-
Treatment is controversial: advocates recommend both weight bearing and non–weight bearing in a short leg cast as well as ORIF.
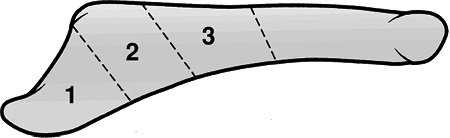 Figure
Figure
41.9. Three zones of proximal fifth metatarsal fracture. Zone 1:
avulsion fracture. Zone 2: fracture at the metaphyseal-diaphyseal
junction. Zone 3: proximal shaft stress fracture.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Union is frequently a concern.
P.461 -
-
Zone 3 injuries are now referred to as proximal diaphyseal stress fractures.
-
These are relatively rare and seen mainly in athletes.
-
They occur in the proximal 1.5 cm of the diaphyseal shaft of the metatarsal.
-
Patients usually present with prodromal symptoms before complete fracture.
-
This particular entity poses problems because of its tendency to nonunion.
-
Initial treatment is between casted
non–weight bearing for up to 3 months and surgical intervention with
grafting and internal compression.
-
-
The remainder of the fifth metatarsal fractures not resulting from a direct blow have been termed dancer’s fractures.
-
The usual pattern is a spiral, oblique fracture progressing from distal-lateral to proximal-medial.
-
The mechanism of injury is a rotational force being applied to the foot while axially loaded in a plantar flexed position.
-
Treatment is symptomatic, with a hard soled shoe.
-
-
Mobility of the MTP joints is essential
for forefoot comfort in normal gait; attempts should thus be made to
salvage any motion at this level.
-
Injuries to the first MTP joint are relatively common, especially in athletic activities or ballet.
-
The incidence in US football and soccer
has risen because of the use of artificial playing surfaces as well as
lighter, more flexible shoes that permit enhanced motion at the MTP
joint.
-
The MTP joint is composed of a cam-shaped
metatarsal head and a matched concave articulation on the proximal
phalanx. These contours contribute little to the overall stability of
the joint. -
Ligamentous constraints includes dorsal
capsule reinforced by the extensor hallucis longus tendon, plantar
plate (capsular ligament) reinforced by the flexor hallucis longus
tendon, flexor hallucis brevis tendon, and medial and lateral
collateral ligaments. -
The plantar capsule is a thick,
weight-bearing structure with strong attachments to the base of the
proximal phalanx. There is a thinner, more flexible attachment to the
plantar aspect of the metatarsal head proximally. Imbedded in this
plantar structure are the two sesamoids.
-
“Turf toe”: This is a sprain of the first
MTP joint. It reflects hyperextension injury to the first MTP joint as
the ankle is in equinus causing temporary subluxation with stretching
on plantar capsule and plate. -
In ballet dancers, injury may occur as a
dancer “falls over” the maximally extended first MTP joint, injuring
the dorsal capsule. Forced abduction may result in lateral capsular
injury with possible avulsion from the base of the proximal phalanx. -
Dislocation of the first MTP joint is
usually the result of high-energy trauma, such as a motor vehicle
accident, in which forced hyperextension of the joint occurs with gross
disruption of the plantar capsule and plate.
-
Patients typically present with pain, swelling, and tenderness of the first MTP joint.
-
Pain may be reproduced with range of motion of the first MTP joint, especially at terminal dorsiflexion or plantar flexion.
-
Chronic injuries may present with decreased range of motion.
-
Most dislocations are dorsal with the
proximal phalanx cocked up and displaced dorsally and proximally,
producing a dorsal prominence and shortening of the toe.
-
AP, lateral, and oblique views of the
foot may demonstrate capsular avulsion or chronic degenerative changes
indicative of longstanding injury.
| Grade I: | Strain at the proximal attachment of the volar plate from the first metatarsal head |
| Grade II: | Avulsion of the volar plate from the metatarsal head |
| Grade III: | Impaction injury to the dorsal surface of the metatarsal head with or without an avulsion or chip fracture |
| Type I: | Volar plate avulsed off the first metatarsal head, proximal phalanx displaced dorsally; intersesamoid ligament remaining intact and lying over the dorsum of the metatarsal head |
| Type IIA: | Rupture of the intersesamoid ligament |
| Type IIB: | Longitudinal fracture of either sesamoid |
-
First MTP sprains
-
Rest, ice, compression, and elevation (RICE) and nonsteroidal antiinflammatory medication are used.
-
Protective taping with gradual return to
activity is recommended; the patient may temporarily wear a hard-soled
shoe with a rocker bottom for comfort. -
Pain usually subsides after 3 weeks of
treatment, but an additional 3 weeks are usually necessary to regain
strength and motion for return to competitive activity. -
Operative intervention is rarely
indicated except in cases of intraarticular fractures or significant
discrete instability. The presence of avulsion fragments and
significant valgus instability may need to be addressed by ORIF or
debridement and ligamentous repair. -
Displaced intraarticular fractures or osteochondral lesions should be fixed or debrided depending on their size.
-
-
Dislocations
-
Jahss Type I fracture: Closed reduction
may be initially attempted. However, if irreducible by closed means, it
will require open reduction. -
Jahss Type IIA, IIB fractures: These are
easily reduced by closed means (longitudinal traction with or without
hyperextension of the first MTP joint). -
After reduction, the patient should be
placed in a short leg walking cast with a toe extension for 3 to 4
weeks to allow capsular healing. -
Displaced avulsion fractures of the base
of the proximal phalanx should be fixed with either lag screws or a
tension band technique. Small osteochondral fractures may be excised;
larger fragments require reduction with Kirschner wires, compression
screws, or headless screws.
-
-
Hallux rigidus and degenerative arthritis complicate chronic injuries and may prevent return to competitive activity.
-
Posttraumatic osteoarthritis: This may
reflect chondral damage at the time of injury or may result from
abnormal resultant laxity with subsequent degenerative changes. -
Recurrent dislocation: Uncommon, although it may occur in patients with connective tissue disorders.
-
Stability of the MTP joints is conferred
by the articular congruity between the metatarsal head and the base of
the proximal phalanx, the plantar capsule, the transverse metatarsal
ligament, the flexor and extensor tendons, and the intervening
lumbrical muscles.
-
Dislocations are usually the result of low-energy “stubbing” injuries and are most commonly displaced dorsally.
-
Avulsion or chip fractures may occur by the same mechanism.
-
Comminuted intraarticular fractures may occur by direct trauma, usually from a heavy object dropped onto the dorsum of the foot.
-
Patients typically present with pain, swelling, tenderness, and variable deformity of the involved digit.
-
Dislocation of the MTP joint typically manifests as dorsal prominence of the base of the proximal phalanx.
-
Location
-
Angulation
-
Displacement
-
Comminution
-
Intraarticular involvement
-
Presence of fracture-dislocation
-
Simple dislocations or nondisplaced
fractures may be managed by gentle reduction with longitudinal traction
and buddy taping for 4 weeks, with a rigid shoe orthosis to limit MTP
joint motion, if necessary.
-
Intraarticular fractures of the
metatarsal head or the base of the proximal phalanx may be treated by
excision of a small fragment, by benign neglect of severely comminuted
fractures, or by ORIF with Kirschner wires or screw fixation for
fractures with a large fragment.
-
Posttraumatic arthritis: May result from articular incongruity or chondral damage at the time of injury.
-
Recurrent subluxation: Uncommon and may
be addressed by capsular imbrication, tendon transfer, cheilectomy, or
osteotomy, if symptomatic.
-
The incidence is highest with repetitive hyperextension at the MTP joints, such as in ballet dancers and runners.
-
The medial sesamoid is more frequently
fractured than the lateral owing to increased weight bearing on the
medial side of the foot.
-
The sesamoids are an integral part of the capsuloligamentous structure of the first MTP joint.
-
They function within the joint complex as
both shock absorbers and fulcrums in supporting the weight-bearing
function of the first toe. -
Their position on either side of the flexor hallucis longus forms a bony tunnel to protect the tendon.
-
Bipartite sesamoids are common (10% to 30% incidence in the general population) and must not be mistaken for acute fractures.
-
They are bilateral in 85% of cases.
-
They exhibit smooth, sclerotic, rounded borders.
-
They do not show callus formation after 2 to 3 weeks of immobilization.
-
-
Direct blows such as a fall from a height or a simple landing from a jump as in ballet can cause acute fracture.
-
Acute fractures can also occur with hyperpronation and axial loading seen with joint dislocations.
-
Repetitive loading from improper running usually gives rise to the more insidious stress fracture.
-
Patients typically present with pain well localized on the plantar aspect of the “ball” of the foot.
-
Local tenderness is present over the
injured sesamoid, with accentuation of symptoms with passive extension
or active flexion of the MTP joint.
-
AP, lateral, and oblique views of the forefoot are usually sufficient to demonstrate transverse fractures of the sesamoids.
-
Occasionally, a tangential view of the sesamoids is necessary to visualize a small osteochondral or avulsion fracture.
-
Technetium bone scanning or MRI may be used to identify stress fractures not apparent by plain radiography.
-
Transverse versus longitudinal
-
Displacement
-
Location: medial versus lateral
-
Nonoperative management should initially
be attempted, with soft padding combined with a short leg walking cast
for 4 weeks followed by a bunion last shoe with a metatarsal pad for 4
to 8 weeks. -
Sesamoidectomy is reserved for cases of
failed conservative treatment. The patient is maintained
postoperatively in a short leg walking cast for 3 to 4 weeks.
-
Sesamoid excision may result in problems
of hallux valgus (medial sesamoid excision) or transfer pain to the
remaining sesamoid owing to overload.
-
Phalangeal fractures are the most common injury to the forefoot.
-
The proximal phalanx of the fifth toe is the most often involved.
-
The first and fifth digits are in
especially vulnerable positions for injury because they form the medial
and lateral borders of the distal foot.
-
A direct blow such as a heavy object dropped onto the foot usually causes a transverse or comminuted fracture.
-
A stubbing injury is the result of axial
loading with secondary varus or valgus force resulting in a spiral or
oblique fracture pattern.
-
Patients typically present with pain, swelling, and variable deformity of the affected digit.
-
Tenderness can typically be elicited over the site of injury.
-
AP, lateral, and oblique views of the foot should be obtained.
-
If possible, isolation of the digit of
interest for the lateral radiograph may aid in visualization of the
injury. Alternatively, the use of small dental radiographs placed
between the toes has been described. -
Technetium bone scanning or MRI may aid
in the diagnosis of stress fracture when the injury is not apparent on
plain radiographs.
-
Location: proximal, middle, distal phalanx
-
Angulation
-
Displacement
-
Comminution
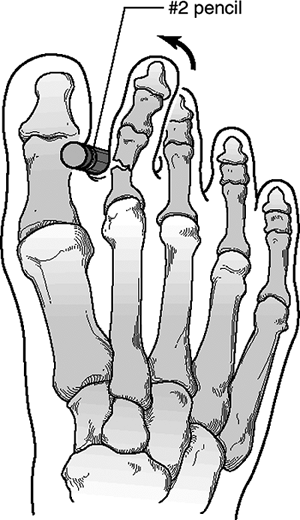
![]() Figure
Figure
41.10. A method of closed reduction for displaced proximal phalanx
fractures. A hard object, such as a pencil, is placed in the adjacent
web space and is used as a fulcrum for reduction.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Intraarticular involvement
-
Presence of fracture-dislocation
-
Nondisplaced fractures irrespective of
articular involvement can be treated with a stiff-soled shoe and
protected weight bearing with advancement as tolerated. -
Use of buddy taping between adjacent toes may provide pain relief and help to stabilize potentially unstable fracture patterns.
-
Fractures with clinical deformity require reduction. Closed reduction is usually adequate and stable (Fig. 41.10).
-
Operative reduction is reserved for those
rare fractures with gross instability or persistent intraarticular
discontinuity. This problem usually arises with an intraarticular
fracture of the proximal phalanx of the great toe or multiple fractures
of lesser toes. -
A grossly unstable fracture of the
proximal phalanx of the first toe should be reduced and stabilized with
percutaneous Kirschner wires or minifragment screws. -
Unstable intraarticular fractures of any
joint despite adequate reduction should be reduced and percutaneously
pinned in place to avoid late malalignment.
-
Nonunion: Uncommon.
-
Posttraumatic osteoarthritis: May
complicate fractures with intraarticular injury, with resultant
incongruity. It may be disabling if it involves the great toe.
-
Usually due to an axial load applied at the terminal end of the digit.
-
Most such injuries occur in the proximal joint, are dorsal in direction, and occur in exposed, unprotected toes.
-
Closed reduction under digital block and longitudinal traction comprise the treatment of choice for these injuries.
-
Once reduced, the interphalangeal joint
is usually stable and can be adequately treated with buddy taping and
progressive activity as tolerated.