Tibia Fibula Shaft
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > IV – Lower Extremity Fractures and Dislocations > 37 – Tibia Fibula Shaft
37
Tibia Fibula Shaft
EPIDEMIOLOGY
-
Fractures of the tibia and fibula shaft are the most common long bone fractures.
-
In an average population, there are about 26 tibial diaphyseal fractures per 100,000 population per year.
-
Men are more commonly affected than
women, with the male incidence being about 41 per 100,000 per year and
the female incidence about 12 per 100,000 per year. -
The average age of a patient sustaining a
tibia shaft fracture is 37 years, with men having an average age of 31
years and women 54 years.
ANATOMY
-
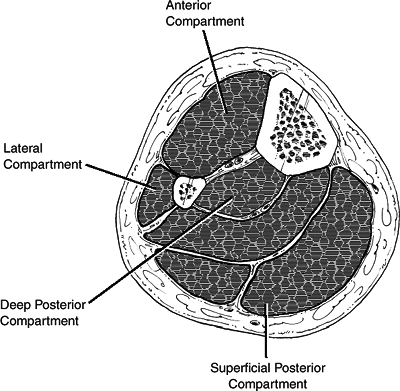
The tibia is a long tubular bone with a
triangular cross section. It has a subcutaneous anteromedial border and
is bounded by four tight fascial compartments (anterior, lateral,
posterior, and deep posterior) (Figs. 37.1 and 37.2). -
Blood supply
-
The nutrient artery arises from the
posterior tibial artery, entering the posterolateral cortex distal to
the origination of the soleus muscle. Once the vessel enters the
intramedullary (IM) canal, it gives off three ascending branches and
one descending branch. These give rise to the endosteal vascular tree,
which anastomose with periosteal vessels arising from the anterior
tibial artery. -
The anterior tibial artery is particularly vulnerable to injury as it passes through a hiatus in the interosseus membrane.
-
The peroneal artery has an anterior
communicating branch to the dorsalis pedis artery. It may therefore be
occluded despite an intact dorsalis pedis pulse. -
The distal third is supplied by
periosteal anastomoses around the ankle with branches entering the
tibia through ligamentous attachments. -
There may be a watershed area at the junction of the middle and distal thirds (controversial).
-
If the nutrient artery is disrupted,
there is reversal of flow through the cortex, and the periosteal blood
supply becomes more important. This emphasizes the importance of
preserving periosteal attachments during fixation.
-
-
The fibula is responsible for 6% to 17% of a weight-bearing load.
-
The common peroneal nerve courses around
the neck of the fibula, which is nearly subcutaneous in this region; it
is therefore especially vulnerable to direct blows or traction injuries
at this level.
MECHANISM OF INJURY
-
Direct
-
High-energy: motor vehicle accidentP.389
-
Transverse, comminuted, displaced fractures commonly occur.
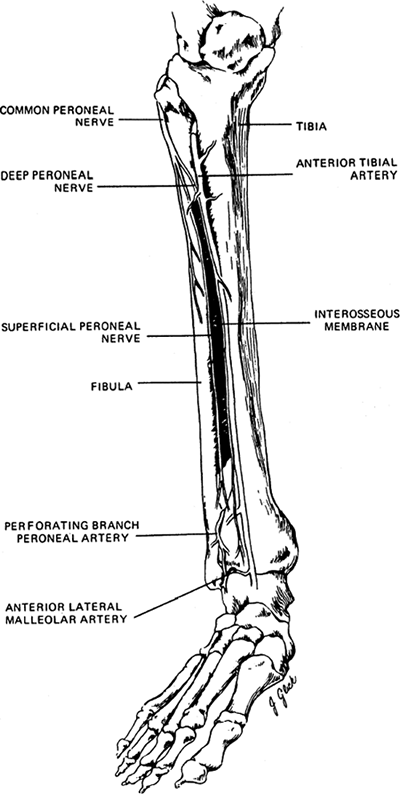 Figure 37.1. The anatomy of the tibial and fibular shaft.(From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 2. Philadelphia: Lippincott-Raven, 1996:2124.)
Figure 37.1. The anatomy of the tibial and fibular shaft.(From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 2. Philadelphia: Lippincott-Raven, 1996:2124.) -
The incidence of soft tissue injury is high.
-
-
Penetrating: gunshot
-
The injury pattern is variable.
-
Low-velocity missiles (handguns) do not
pose the problems from bone or soft tissue damage that high-energy
(motor vehicle accident) or high-velocity (shotguns, assault weapons)
mechanisms cause.
-
-
Bending: three- or four-point (ski boot injuries)
-
Short oblique or transverse fractures occur, with a possible butterfly fragment.
-
Crush injury occurs.
![]() Figure 37.2. The four compartments of the leg.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 37.2. The four compartments of the leg.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Highly comminuted or segmental patterns are associated with extensive soft tissue compromise.
-
Must rule out compartment syndrome and open fractures.
P.390 -
-
Fibula shaft fractures: These typically result from direct trauma to the lateral aspect of the leg.
-
-
Indirect
-
Torsional mechanisms
-
Twisting with the foot fixed and falls from low heights are causes.
-
These spiral, nondisplaced fractures have minimal comminution associated with little soft tissue damage.
-
-
Stress fractures
-
In military recruits, these injuries most
commonly occur at the metaphyseal/diaphyseal junction, with sclerosis
being most marked at the posteromedial cortex. -
In ballet dancers, these fractures most
commonly occur in the middle third; they are insidious in onset and are
overuse injuries. -
Radiographic findings may be delayed several weeks.
-
-
CLINICAL EVALUATION
-
Evaluate neurovascular status. Dorsalis
pedis and posterior tibial artery pulses must be evaluated and
documented, especially in open fractures in which vascular flaps may be
necessary. Common peroneal and tibial nerve integrity must be
documented. -
Assess soft tissue injury. Fracture blisters may contraindicate early open reduction.
-
Monitor for compartment syndrome. Pain
out of proportion to the injury is the most reliable sign of
compartment syndrome. Compartment pressure measurements that have been
used as an indication for four-compartment fasciotomy have been (1)
pressures higher than 30 mm Hg and (2) pressure within 30 mm Hg of
diastolic pressure. Deep posterior compartment pressures may be
elevated in the presence of a soft superficial posterior compartment. -
Tibial fractures are associated with a high incidence of knee ligament injuries.
-
About 5% of all tibial fractures are bifocal, with two separate fractures of the tibia.
P.391
RADIOGRAPHIC EVALUATION
-
Radiographic evaluation must include the
entire tibia (anteroposterior [AP] and lateral views) with
visualization of the ankle and knee joints. -
Oblique views may be helpful to further characterize the fracture pattern.
-
Postreduction radiographs should include the knee and ankle for alignment and preoperative planning.
-
A surgeon should look for the following features on the AP and lateral radiographs:
-
The location and morphology of the fracture should be determined.
-
The presence of secondary fracture lines: These may displace during operative treatment.
-
The presence of comminution: This signifies a higher-energy injury.
-
The distance that bone fragments have
traveled from their normal location: Widely displaced fragments suggest
that the soft tissue attachments have been damaged and the fragments
may be avascular. -
Osseous defects: These may suggest missing bone.
-
Fracture lines may extend proximally to the knee or distally to the ankle.
-
The state of the bone: Is there evidence of osteopenia, metastases, or a previous fracture?
-
Osteoarthritis or the presence of a knee arthroplasty: Either may change the treatment method selected by the surgeon.
-
Gas in the tissues: These are usually
secondary to open fracture but may also signify the presence of gas
gangrene, necrotizing fasciitis, or other anaerobic infections.
-
-
Computed tomography and magnetic resonance imaging (MRI) usually are not necessary.
-
Technetium bone scanning and MRI scanning
may be useful in diagnosing stress fractures before these injuries
become obvious on plain radiographs. -
Angiography is indicated if an arterial injury is suspected.
CLASSIFICATION
Poor sensitivity, reproducibility, and interobserver reliability have been reported for most classification schemes.
P.392
Descriptive
-
Open versus closed
-
Anatomic location: proximal, middle, or distal third
-
Fragment number and position: comminution, butterfly fragments
-
Configuration: transverse, spiral, oblique
-
Angulation: varus/valgus, anterior/posterior
-
Shortening
-
Displacement: percentage of cortical contact
-
Rotation
-
Associated injuries
OTA Classification of Tibial Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
Gustilo and Anderson Classification of Open Fractures
| Grade I: | Clean skin opening of <1 cm, usually from inside to outside; minimal muscle contusion; simple transverse or short oblique fractures |
| Grade II: | Laceration >1 cm long, with extensive soft tissue damage; minimal to moderate crushing component; simple transverse or short oblique fractures with minimal comminution |
| Grade III: | Extensive soft tissue damage, including muscles, skin, and neurovascular structures; often a high-energy injury with a severe crushing component |
| IIIA: | Extensive soft tissue laceration, adequate bone coverage; segmental fractures, gunshot injuries, minimal periosteal stripping |
| IIIB: | Extensive soft tissue injury with periosteal stripping and bone exposure requiring soft tissue flap closure; usually associated with massive contamination |
| IIIC: | Vascular injury requiring repair |
Tscherne Classification of Closed Fractures
-
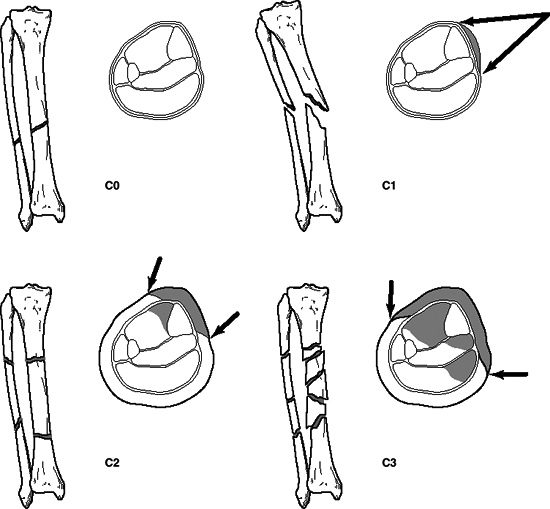
This classifies soft tissue injury in closed fractures and takes into account indirect versus direct injury mechanisms (Fig. 37.3).
| Grade 0: | Injury from indirect forces with negligible soft tissue damage |
| Grade I: | Closed fracture caused by low-moderate energy mechanisms, with superficial abrasions or contusions of soft tissues overlying the fracture |
| Grade II: | Closed fracture with significant muscle contusion, with possible deep, contaminated skin abrasions associated with moderate to severe energy mechanisms and skeletal injury; high risk for compartment syndrome |
| Grade III: | Extensive crushing of soft tissues, with subcutaneous degloving or avulsion, with arterial disruption or established compartment syndrome |
P.393
TREATMENT
 |
|
Figure 37.3. The Tscherne classification of closed fractures: C0, simple fracture configuration with little or no soft tissue injury; C1, superficial abrasion, mild to moderately severe fracture configuration; C2, deep contamination with local skin or muscle contusion, moderately severe fracture configuration; C3, extensive contusion or crushing of skin or destruction of muscle, severe fracture.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
Nonoperative
Fracture reduction followed by application of a long leg
cast with progressive weight bearing can be used for isolated, closed,
low-energy fractures with minimal displacement and comminution.
cast with progressive weight bearing can be used for isolated, closed,
low-energy fractures with minimal displacement and comminution.
-
Cast with the knee in 0 to 5 degrees of
flexion to allow for weight bearing with crutches as soon as tolerated
by patient, with advancement to full weight bearing by the second to
fourth week. -
After 4 to 6 weeks, the long leg cast may be exchanged for a patella-bearing cast or fracture brace.
-
Union rates as high as 97% are reported, although with delayed weight bearing related to delayed union or nonunion.
Acceptable Fracture Reduction
-
Less than 5 degrees of varus/valgus angulation is recommended.
-
Less than 10 degrees of anterior/posterior angulation is recommended (<5 degrees preferred).
-
Less than 10 degrees of rotational deformity is recommended, with external rotation better tolerated than internal rotation.
-
Less than 1 cm of shortening; 5 mm of distraction may delay healing 8 to 12 months.
-
More than 50% cortical contact is recommended.
-
Roughly, the anterior superior iliac spine, center of the patella, and base of the second proximal phalanx should be colinear.
P.394
Time to Union
-
The average time is 16±4 weeks: This is highly variable, depending on fracture pattern and soft tissue injury.
-
Delayed union is defined as >20 weeks.
-
Nonunion: This occurs when clinical and
radiographic signs demonstrate that the potential for union is lost,
including sclerotic ends at the fracture site and a persistent gap
unchanged for several weeks. Nonunion has also been defined as lack of
healing 9 months after fracture.
Tibia Stress Fracture
-
Treatment consists of cessation of the offending activity.
-
A short leg cast may be necessary, with partial-weight-bearing ambulation.
Fibula Shaft Fracture
-
Treatment consists of weight bearing as tolerated.
-
Although not required for healing, a short period of immobilization may be used to minimize pain.
-
Nonunion is uncommon because of the extensive muscular attachments.
Operative Treatment
Intramedullary (IM) Nailing
-
IM nailing carries the advantages of
preservation of periosteal blood supply and limited soft tissue damage.
In addition, it carries the biomechanical advantages of being able to
control alignment, translation, and rotation. It is therefore
recommended for most fracture patterns. -
Locked versus unlocked nail
-
Locked nail: This provides rotational
control; it is effective in preventing shortening in comminuted
fractures and those with significant bone loss. Interlocking screws can
be removed at a later time to dynamize the fracture site, if needed,
for healing. -
Nonlocked nail: This allows impaction at
the fracture site with weight bearing, but it is difficult to control
rotation. Nonlocked nails are rarely used.
-
-
Reamed versus unreamed nail
-
Reamed nail: This is indicated for most
closed and open fractures. It allows excellent IM splinting of the
fracture and use of a larger-diameter, stronger nail. -
Unreamed nail: This is designed to
preserve the IM blood supply in open fractures where the periosteal
supply has been destroyed. It is currently reserved for higher-grade
open fractures; its disadvantage is that it is significantly weaker
than the larger reamed nail and has a higher risk of implant fatigue
failure.
P.395 -
Flexible Nails (Enders, Rush Rods)
-
Multiple curved IM pins exert a spring
force to resist angulation and rotation, with minimal damage to the
medullary circulation. -
These are rarely used in the United
States because of the predominance of unstable fracture patterns and
success with interlocking nails. -
They are recommended only in children or adolescents with open physes.
External Fixation
-
Primarily used to treat severe open
fractures, it can also be indicated in closed fractures complicated by
compartment syndrome, concomitant head injury, or burns. -
Its popularity in the United States has waned with the increased use of reamed nails for most open fractures.
-
Union rates: Up to 90%, with an average of 3.6 months to union.
-
The incidence of pin tract infections is 10% to 15%.
Plates and Screws
-
These are generally reserved for fractures extending into the metaphysis or epiphysis.
-
Reported success rates as high as 97%.
-
Complication rates of infection, wound breakdown, and malunion or nonunion increase with higher-energy injury patterns.
Proximal Tibia Fractures
-
These account for about 7% of all tibia diaphyseal fractures.
-
These fractures are notoriously difficult
to nail, because they frequently become malaligned, the commonest
deformities being valgus and apex anterior angulation. -
Nailing requires use of special techniques such as blocking screws.
-
Use of a percutaneously inserted plate has had recent popularity.
Distal Tibia Fractures
-
The risk for malalignment also exists with the use of an IM nail.
-
With IM nailing, fibula plating or use of blocking screws may help to prevent malalignment.
-
Use of a percutaneously inserted plate has had recent popularity.
P.396
Tibia Fracture with an Intact Fibula
-
If the tibia fracture is nondisplaced,
treatment consists of long leg casting with early weight bearing. Close
observation is indicated to recognize any varus tendency. -
Some authors recommend IM nailing even if tibia fracture is nondisplaced.
-
A potential risk of varus malunion exists, particularly in patients >20 years.
Fasciotomy
-
Evidence of compartment syndrome is an
indication for emergent fasciotomy of all four muscle compartments of
the leg (anterior, lateral, superficial, and deep posterior) through
one or multiple incision techniques. Following operative fracture
fixation, the fascial openings should not be reapproximated.
COMPLICATIONS
-
Malunion: This includes any deformity outside the acceptable range.
-
Nonunion: This associated with
high-velocity injuries, open fractures (especially Gustilo grade III),
infection, intact fibula, inadequate fixation, and initial fracture
displacement. -
Infection may occur.
-
Soft tissue loss: Delaying wound coverage
for greater than 7 to 10 days in open fractures has been associated
with higher rates of infection. Local rotational flaps or free flaps
may be needed for adequate coverage. -
Stiffness at the knee and/or ankle may occur.
-
Knee pain: This is the most common complication associated with IM tibial nailing.
-
Hardware breakage: Nail and locking screw
breakage rates depend on the size of the nail used and the type of
metal from which it is made. Larger reamed nails have larger cross
screws; the incidence of nail and screw breakage is greater with
unreamed nails that utilize smaller-diameter locking screws. -
Thermal necrosis of the tibial diaphysis
following reaming is an unusual, but serious, complication. Risk is
increased with use of dull reamers and reaming under tourniquet control. -
Reflex sympathetic dystrophy: This is
most common in patients unable to bear weight early and with prolonged
cast immobilization. It is characterized by initial pain and swelling
followed by atrophy of limb. Radiographic signs are spotty
demineralization of foot and distal tibia and equinovarus ankle. It is
treated by elastic compression stockings, weight bearing, sympathetic
blocks, and foot orthoses, accompanied by aggressive physical therapy. -
Compartment syndrome: Involvement of the
anterior compartment is most common. Highest pressures occur at the
time of open or closed reduction. It may require fasciotomy. Muscle
death occurs after 6 to 8 hours. Deep posterior compartment syndrome
may be missed because of uninvolved overlying superficial compartment,
and results in claw toes. -
Neurovascular injury: Vascular compromise
is uncommon except with high-velocity, markedly displaced, often open
fractures. It most commonly occurs as the anterior tibial artery
traverses the interosseous membrane of the proximal leg. It may require
saphenous vein interposition graft. The common peroneal nerve is
vulnerable to direct injuries to the proximal fibula as well as
fractures with significant varus angulation. Overzealous traction can
result in distraction injuries to the nerve, and inadequate cast
molding/padding may result in neurapraxia. -
Fat embolism may occur.
-
Claw toe deformity: This is associated with scarring of extensor tendons or ischemia of posterior compartment muscles.
P.397