Extra-Articular Injuries of the Knee
the patella and the physes of the distal femur and proximal tibia.
Great force generally is required to disrupt these structures in
children and adolescents. This leads to increased risks of associated
injuries and growth arrest. Neurovascular structures are also at
increased risk because of close proximity to the distal femur and
proximal tibia. Growth disturbances may have severe consequences due to
rapid growth around the knee. Accurate reduction is critical for proper
knee function. Therefore, careful assessment and anatomic alignment
with stable fixation are generally recommended for extra-articular
injuries of the knee. Parents should be advised that x-ray follow-up is
essential for early detection and treatment of growth disturbances from
these injuries.
and/or shortening; this has been reported in 35% to 50% of patients regardless of anatomic reduction.3,44,53,71,89,154,159
The prognosis is better for very young children and nondisplaced
fractures, but complications are frequent and may occur with any distal
femoral physeal injury. Careful assessment, anatomic reduction, and
secure immobilization or fixation are recommended for most injuries.
Follow-up for many months is recommended for early detection of growth
disturbances.
termed “wagon-wheel injury” or “cartwheel injury” because it occurred
when boys attempted to jump onto a moving wagon and the leg became
entrapped between the spokes of the moving wheel. This often led to
amputation because of associated neurovascular trauma.70 Today, most distal femoral fracture separations are the result of motor vehicle or sports-related trauma (Table 23-1).3
Underlying conditions such as neuromuscular disorders, joint
contractures, difficult deliveries, or nutritional deficiencies may
predispose some children to separation of the distal femoral epiphysis.4,5,7,94,121
The principles of management for pathologic fractures may vary from
those for fractures in otherwise healthy children because severe trauma
is generally necessary to separate the distal femoral epiphysis in
healthy children. This is especially true between the ages of 2 to 11
years. Less force is required for physeal disruption in infants and
adolescents.133 Child abuse should
be suspected in infants and toddlers when a small peripheral
metaphyseal fragment of bone, also called a “corner fracture,” is
identified in association with a nondisplaced distal femoral epiphyseal
fracture (Fig 23-1).87
In the adolescent age group, valgus and torsional injury during sports
are a common cause of distal femoral epiphyseal separation (Fig 23-2).
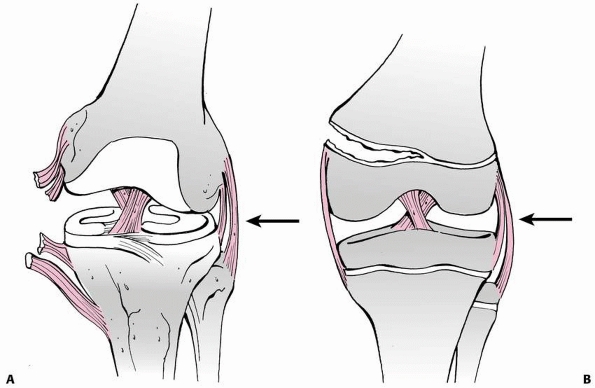
stress across the knee joint. In skeletally mature individuals, this
mechanism of injury can cause ligamentous disruption because ligaments
commonly fail before bone fails when a bending stress is applied across
the knee joint (Fig. 23-3A). However, loading
to failure across the immature knee is more likely to lead to physeal
failure due to tensile stresses that are transmitted through the
ligaments to the adjacent physis (Fig. 23-3B).45
Bending creates tension on one side of the physis and compression on
the opposite side. This leads to disruption of the periosteum and
perichondrial ring on the tension side, followed by a fracture plane
that begins in the hypertrophic zone and proceeds in an irregular
manner through the physis.21
Salter-Harris type I fractures generally extend through the
hypertrophic zone and the zone of provisional calcification without
traversing the germinal layers. Salter-Harris type II fractures exit
through the
metaphysis with a spike of metaphyseal bone attached to the epiphysis on the compression side (Thurstan-Holland fragment) (Fig. 23-4A).
Salter-Harris type III and IV fractures cross the entire physis
vertically and enter the joint through the articular cartilage. Bright
et al.21 demonstrated that male and
prepubescent animals are less resistant to epiphyseal separation when
various loads are applied, and that the growth plate is also weakest in
torsion. Direction of force determines direction of displacement of the
distal fragment. When the knee is hyperextended, the distal fragment is
displaced anteriorly. Pure compression force also can cause distal
femoral physeal damage (Salter-Harris type V). Premature growth arrest
has been reported after pure compression injuries and also in
association with nonphyseal fractures of the femoral and tibial shafts.10,66,107,142
Salter-Harris type III fractures of the distal medial femoral condyle
result from the same mechanism of injury that produces medial
collateral and cruciate ligament disruption in skeletally mature
patients. The pull of the medial collateral ligament (MCL) results in
condylar separation instead of MCL disruption. Salter-Harris type III
fractures of the medial femoral condyle are frequently associated with
cruciate ligament injuries.22,98,130,162
This pattern of fracture occurs near skeletal maturity when the central
portion of the distal femoral physis begins to close before the medial
and lateral physis. Thus the mechanism of this injury is similar to
that of the juvenile Tillaux fracture in the adolescent ankle.98
|
TABLE 23-1 Mechanism of Injury in Clinical Reviews of Separation of the Distal Femoral Epiphysis
|
||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||
 |
|
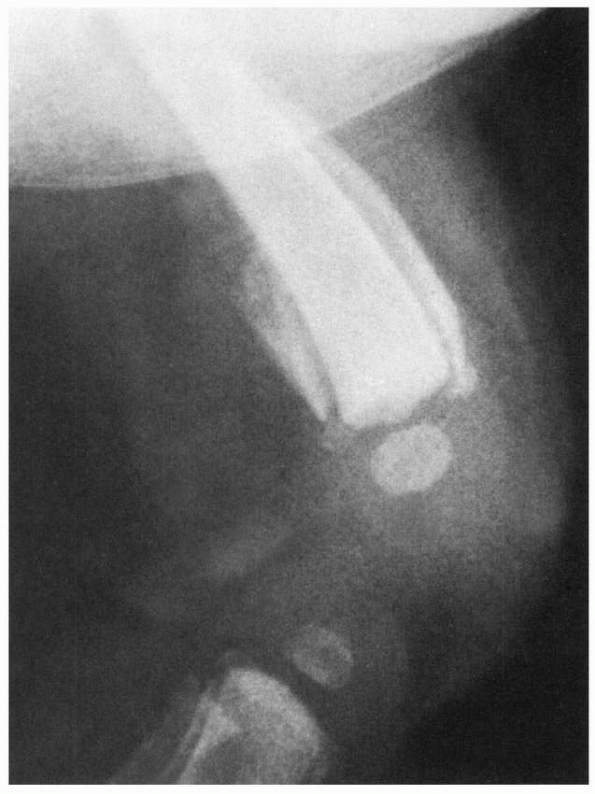
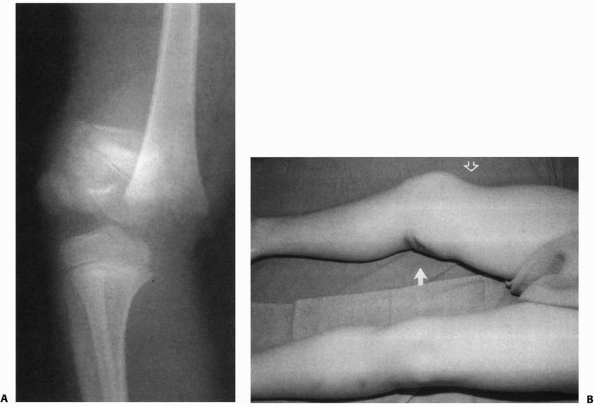
FIGURE 23-1
Lateral radiograph of a swollen knee in a 3-month-old girl who reportedly fell out of her crib 8 days earlier. Subperiosteal ossification along the distal femoral shaft indicates separation of the distal femoral epiphysis. Note evidence of fracture-separation of the proximal tibial epiphysis as well. Final diagnosis: abused child. |
 |
|
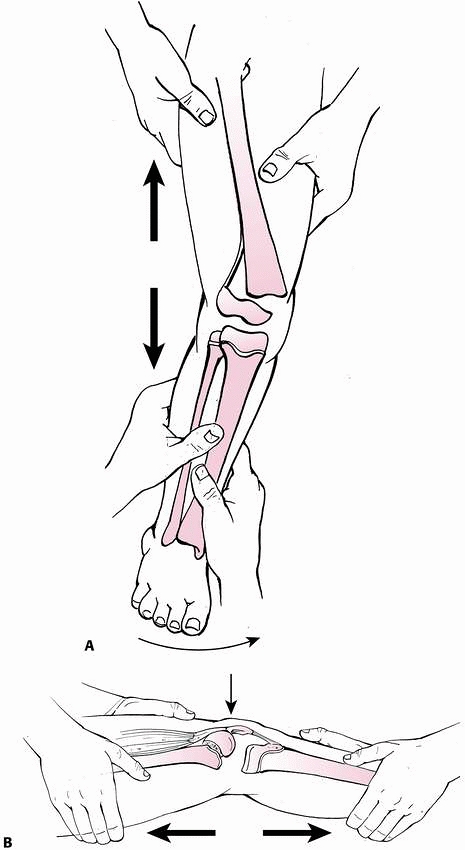
FIGURE 23-2 Valgus and torsional stress across the knee may cause a ligament injury or physeal separation.
|
 |
|
FIGURE 23-3 A. In a skeletally mature patient with closed physis, tensile failure usually occurs across the ligament. B.
In a skeletally immature patient with open physis, failure usually occurs across the physis. (Reprinted with permission from Skaggs DL, Flynn JF. Trauma about the knee, tibia, and foot. In Skaggs DL, Flynn JF, eds. Staying out of Trouble in Pediatric Orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 2006.) |
 |
|
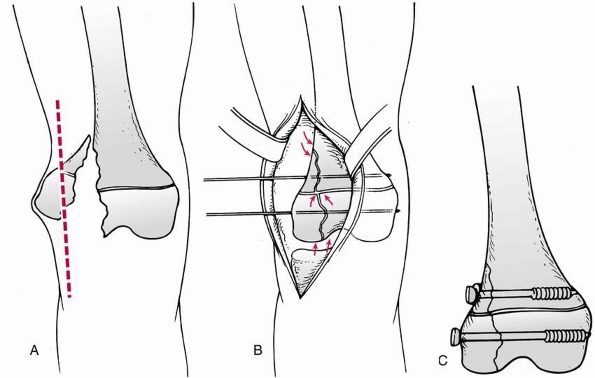
FIGURE 23-4 A.
In a Salter-Harris type II fracture, the side where the fracture occurred through the physis fails in tension, with disruption of the periosteum. The side of the fracture with the Thurstan-Holland fragment failed in compression, with the periosteum usually intact. The intact periosteum can be used for fracture reduction. B. With fracture reduction, the periosteum may become interposed within the fracture site, preventing an anatomic reduction |
separation is usually obvious, but minor degrees of displacement may
require careful examination and x-ray interpretation. The patient is in
pain and cannot walk or bear weight on the injured limb immediately
after sustaining a displaced separation of the distal femoral
epiphysis. Most often, these injuries result from significant force
causing visible malalignment of the limb, swelling, and/or ecchymosis
that make the diagnosis of a fracture obvious (Fig. 23-5).
Abrasion or laceration of the overlying soft tissues may be a clue to
the mechanism of injury or to an open fracture. More swelling and
prominence may be noted on the side that opened in tension. On this
side, the periosteum is usually ruptured and the metaphyseal fragment
may buttonhole through the quadriceps muscle. On the opposite side, in
the direction of displacement, the periosteum is usually intact and may
help guide reduction. If a fracture is suspected, it is better to
obtain x-rays before any manipulation. When muscle spasm can be
relaxed, instability just above the knee joint may be felt. Fracture
crepitus sometimes may be absent if the periosteum is interposed
between the metaphysis and the epiphysis. Whenever epiphyseal
separation is suspected, careful neurovascular examination of the lower
leg and foot should be performed, including pulses, color, temperature,
and motor and sensory status. The extremity may become cyanotic if
venous return is impaired. The use of Doppler ultrasound may be helpful
in evaluating circulation distal to the injury. Compartmental pressure
recordings should be obtained if there are clinical findings of
compartment syndrome. Extravasation of blood into the soft tissues of
the distal thigh and popliteal fossa produces ecchymosis that may
become more apparent within 72 hours after injury.
 |
|
FIGURE 23-5 A.
Completely displaced Salter-Harris type II fracture of the distal femur in a 6-year-old girl whose foot was on the back of the driver’s headrest when the automobile in which she was riding was involved in an accident. B. Ecchymosis in the popliteal fossa and anterior displacement of the distal femur are evident. Clinical examination revealed absence of peroneal nerve function and a cold, pulseless foot. |
is able to bear some weight on the limb and it may be possible to
localize tenderness to the level of the physis rather than the joint
line where ligament disruptions are more frequent. Abnormal laxity may
be perceived on clinical examination but can be the result of physeal
instability rather than a ligamentous tear. In an adolescent or child
with a knee injury and swelling, occult physeal instability should be
suspected. Stress x-rays or magnetic resonance imaging (MRI) may be
indicated when doubt exists.98,147,162
MRI may be tolerated better by patients and provides the advantage of
evaluating possible ligament injuries. Ultrasonography may be used as a
diagnostic tool in infants and toddlers.68
concomitant injury to knee ligaments that may be present at the time of
initial management of the epiphyseal separation. Bertin and Goble15
found that six of 16 patients seen in follow-up for distal femoral
physeal fractures had ligamentous instability. A review of 151 children
with distal femoral physeal fractures found symptomatic knee
ligamentous laxity in 12 patients (8%).44 Salter-Harris type III fractures of the medial femoral condyle are frequently associated with cruciate ligament injuries.22,98,130,162
For this reason, an MRI, instead of stress x-rays, may provide more
information about Salter-Harris type III fractures to help diagnose
ligamentous injury. Early diagnosis of injury to the ligaments or
menisci can facilitate early management.15
In general, fracture stabilization is the first step with ligament
reconstruction or meniscal repair done after physeal healing. If there
is no meniscal injury, a rehabilitation program is indicated initially.
If there is a reparable meniscal tear, cruciate reconstruction can be
done at the time of meniscal repair depending on the patient’s age and
activity level.
 |
|
FIGURE 23-5 (continued)
The fracture was irreducible by closed methods and required open reduction, internal fixation, and repair of a popliteal artery laceration. C,D. Incomplete reduction Salter-Harris type II fracture in a 6-year-old girl with 25 degrees of posterior angulation and abundant callus formation. E,F. Four years later, remodeling has occurred and no growth disturbance is noted. Results such as this cannot be relied upon, and early anatomic reduction is recommended. |
Intimal tear and thrombosis in the popliteal artery may be caused by
trauma from the distal end of the metaphysis when the epiphysis is
displaced anteriorly during a hyperextension injury.11,44,140
In patients with known vascular injury, vascular repair should be
carried out immediately after fracture stabilization. If vascular
impingement occurs but is relieved by prompt reduction of the displaced
epiphysis, the patient should still be closely observed for the classic
signs of vascular impairment or compartment syndrome. Arteriography and
vascular consultation should be considered when perfusion is less than
normal. If there is an associated fracture of the pelvis or femoral
shaft, arteriography may be necessary to localize the vascular injury.
Vascular impairment may develop slowly from increasing compartmental
pressure. If the patient has inordinate persistent pain or a cool and
pale foot, a femoral arteriogram and compartment pressure measurement
should be considered even when peripheral pulses are present.
 |
|
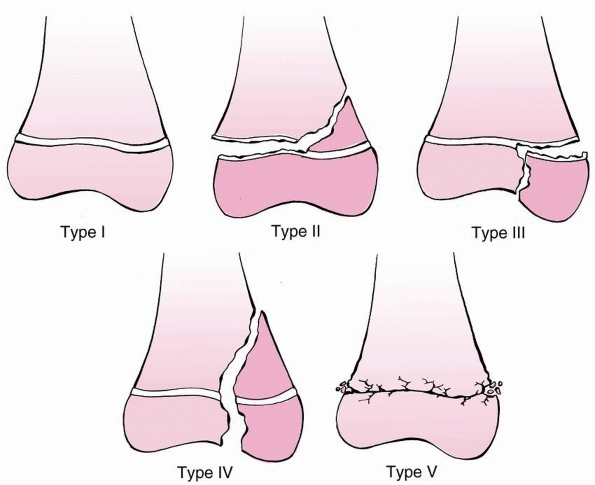
FIGURE 23-6 The Salter-Harris classification of fractures involving the distal femoral physis.
|
is unclear whether vascular repair or fracture stabilization should be
carried out first.20,26,153
Most distal femoral epiphyseal separations can be stabilized rapidly
with screw or pin fixation before vascular repair. Ischemia time may be
increased when prolonged fracture stabilization is performed first, but
vascular repair is at risk for avulsion when it is done before
manipulations necessary for fracture stabilization.
It may be stretched by anterior or medial displacement of the epiphysis
with resulting neurapraxia. Spontaneous recovery can be expected
following reduction and fixation of the fracture.44,149
The exception to this is a transected nerve in association with an open
injury, which can be treated with repair or grafting. Persistent
neurologic deficit after 6 months warrants electromyographic
examination. If the conduction time is prolonged and fibrillation or
denervation is present in distal muscles, exploration and microneural
reanastomosis or resection of any neuroma may be indicated.
classified according to the pattern of fracture, the direction and
magnitude of displacement, and the age of the patient. The
Salter-Harris classification140 is
useful for description and treatment planning. Classification by
direction and degree of displacement may help plan the reduction and
predict the risk of complications.3,71 Classification by age may help identify the mechanism of injury and the implications for growth disturbance.
growth disturbance.3,36,44,89,133
Salter-Harris type I and II fractures in other areas of the body
usually have a low risk of growth arrest, even minimally displaced
Salter-Harris type I and II fractures of the distal femur should be
followed closely for physeal injury. Growth disturbance is uncommon in
patients younger than 2 years of age,133 but these fractures in older children lead to growth arrest in 40% to 50% of patients.71,133
the distal femoral physis, without fracture through the adjacent
epiphysis or metaphysis (Fig. 23-7). It occurs
in infants as a birth injury or abuse and in adolescents, often as a
nondisplaced separation. This type of fracture may go undetected.
Sometimes, the diagnosis is made only in retrospect, when subperiosteal
new bone formation occurs along the adjacent metaphysis. When
displacement is present before the age of 2 years, it is usually in the
sagittal plane.
 |
|
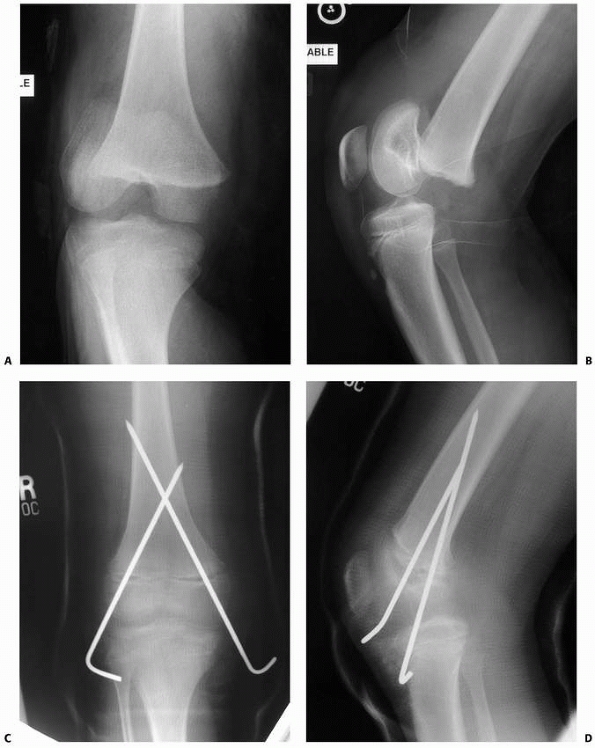
FIGURE 23-7 A. Salter-Harris type I fracture of the distal femur in an 8-year-old. B. Lateral view shows hyperextension. C. Fixation following closed reduction under general anesthesia. Note that pins are widely separated at the fracture site. D. Lateral view of fixation.
|
This pattern is characterized by an oblique extension of the fracture
across one corner of the adjacent metaphysis. The metaphyseal
corner
that remains attached to the epiphysis is called the Thurston-Holland
fragment. Displacement is usually toward the side of the metaphyseal
fragment.
 |
|
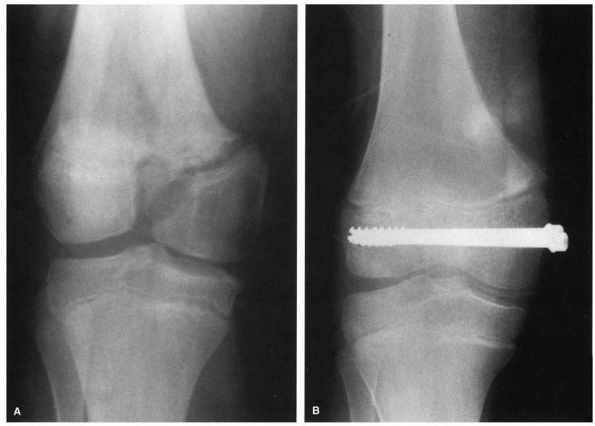
FIGURE 23-8 A. Salter-Harris type II fracture in a 12-year-old boy. B. Lateral view. C. AP view after closed reduction and fixation. Note that screws function in compression with threads across fracture line. D. Lateral view. E.
Six months after injury, this plain radiograph and clinical picture was suspicious of increased valgus. Note that the radiograph is not centered on the distal physis, and thus the physis is difficult to visualize. |
portion of the epiphysis, with a vertical fracture line extending from
the physis down to or through the articular surface of the epiphysis (Fig. 23-9).
Salter-Harris type III injuries of the distal femur usually involve the
medial condyle. These injuries are produced by valgus stress during
sports activity and may have an associated injury to the cruciate
ligaments.22,125 Nondisplaced fractures may only be detectable with a stress x-ray or MRI.98 McKissick et al.98
noted that the Salter-Harris type III fracture pattern may be related
to the sequence of closure of the distal femoral physis, similar to a
juvenile Tillaux fracture of the distal tibia.98
of the condyle similar to the “Hoffa fracture” of the posterior condyle seen in adults.85,110 This fracture is very difficult to diagnose with standard x-rays.138
 |
|
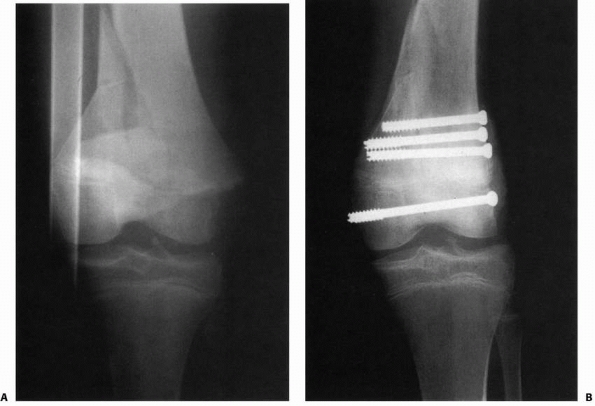
FIGURE 23-9 A.
Salter-Harris type III fracture-separation of the distal femur. Note the vertical fracture line extending from the physis distally into the intercondylar notch with displacement. B. After reduction and fixation with two compression screws extending transversely across the epiphyseal fragments. Note closure and healing of the vertical fracture line in the epiphysis, with restoration of the articular surface. |
uncommon. The fracture line extends vertically through the metaphyseal
cortex, across the physis, and exits through the articular surface of
the epiphysis (Fig. 23-10). Even slight
displacement of a Salter-Harris type IV fracture may produce a bony
bridge from the displaced epiphysis to the metaphysis. Therefore,
anatomic reduction and internal fixation are essential for type IV
fractures.
 |
|
FIGURE 23-10 A. Comminuted Salter-Harris type IV fracture of the distal femur in a 14-year-old boy involved in a motor vehicle accident. B. Six months after open reduction and internal fixation with cannulated screws in the metaphysis and epiphysis
|
crushed without displacement. This injury is rare and often diagnosed
retrospectively when growth disturbance is observed following an injury
to the knee.148 When a type V injury
is suspected, an MRI may identify bone contusion on both sides of the
growth plate, suggesting compression damage of the growth plate.142
not fit into the original Salter-Harris classification. A type VI
injury has been proposed and is occasionally identified following
femoral epiphyseal trauma.113,131
A type VI injury is an avulsion of the periphery of the physis with a
fragment of metaphyseal and epiphyseal bone attached. This small
fragment, including a portion of the perichondrium and underlying bone,
may be torn off when the proximal attachment of the collateral ligament
is avulsed.
Anterior displacement of the epiphysis results from hyperextension of
the knee and has an increased risk of neurovascular damage,36,149 but direction
of displacement does not correlate with other complications such as
angular deformity, growth disturbance, or loss of motion. In contrast, severity of displacement does predict final outcome and complications.3,71,159
Amount of displacement has been evaluated by several different methods,
but displacement of more than one third of bone width correlates with
higherenergy trauma and more frequent complications.3,71,89,159
Metaphyseal comminution which may indicate higher-energy trauma has
also been correlated with an increased risk of complications.71
Distal femoral epiphyseal fractures in children aged 2 to 11 years are
caused by more severe trauma and have the worst prognosis.44,133
In adolescents, low-energy sports injuries are the most frequent cause
of epiphyseal separation. Because adolescents have little growth,
remaining severe growth retardation is uncommon. Separations of the
distal femoral epiphysis before the age of 2 years generally have
satisfactory outcomes,95,133,159 possibly because epiphyseal undulations and the central peak are not as prominent in infants as in older children (Fig. 23-11A).111
In juveniles and adolescents, the fracture may pass through the central
prominence and lead to central growth arrest due to interference with
vascularity in this region or due to the fracture plane exiting and
re-entering the central physis (Fig.23-11B).111,133,151
 |
|
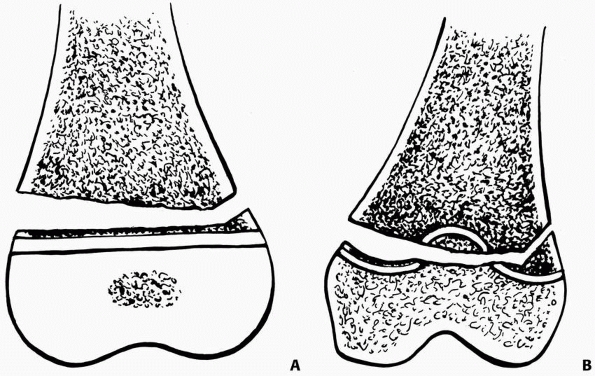
FIGURE 23-11 A. Distal femoral physeal separation prior to the age of 2 years may not disrupt growth because the physis is flat. B.
After the age of 2 years, a central ridge and four quadrants of undulation develop in the distal femur. Fractures in this age group are more likely to cross multiple planes of bone and cartilage. |
diagnosed by widening, displacement of the epiphysis, or adjacent bony
disruption; however, a nondisplaced Salter-Harris type I or III
fracture without separation can be easily overlooked.7,138,162 Oblique views of the distal femur may reveal an occult fracture through the epiphysis or metaphysis (Table 23-2).
It has been suggested that stress views should be considered if
multiple plain films are negative in a patient with an effusion or
tenderness localized to the physis;147
however, when a fracture is not visible on standard x-rays,
immobilization in a cast may be preferable because stress x-rays may be
painful or further disrupt alignment. Also, there is no urgent reason
to repair ligamentous injuries, so 2 weeks of immobilization will
usually define the injury as accurately as stress radiographs.151
Another option for early diagnosis of occult injury is MRI, which
should be diagnostic for fracture and/or associated soft tissue
injuries.98 A computed tomography
(CT) scan may be preferable for evaluating fractures with metaphyseal
comminution or determining fracture geometry for fixation purposes.
most distal femoral epiphyseal fractures. The magnitude and direction
of displacement along with the fracture pattern are used to guide
treatment. Medial or lateral displacement or a vertical epiphyseal
fracture line is best seen on an anteroposterior (AP) view. This view
allows differentiation of Salter-Harris types III and IV injuries from
other types. Minor degrees of displacement may be difficult to measure
on plain films unless the x-ray projection is precisely in line with
the plane of fracture. Even small amounts of displacement are
significant.71,89 Anterior or posterior displacement of the epiphysis is best appreciated on the
lateral projection. The anteriorly displaced epiphysis is usually
tilted so that the distal articular surface faces anteriorly
(hyperextension). The posteriorly displaced epiphysis is rotated so
that the distal articular surface faces the popliteal fossa. Separation
of the distal femoral epiphysis in an infant is difficult to see on
initial x-rays unless there is displacement because only the center of
the epiphysis is ossified at birth. This ossification center should be
in line with the axis of the femoral shaft on both AP and lateral
views. Comparison views of the opposite knee may be helpful.
Ultrasonography, arthrography, or MRI of the knee may help to identify
a separation of the relatively unossified femoral epiphysis.69,173
|
TABLE 23-2 Imaging Studies in the Evaluation of Distal Femoral Physeal Fractures
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
adolescent knee injuries. In a review of MRI scans of 315 adolescents
with traumatic knee injuries, physeal injuries of the distal femur were
diagnosed in seven patients and of the proximal tibia in two patients.
Plain films available on eight patients showed signs of fracture in
seven patients, but the fracture was clearly delineated in only one
patient.32 For evaluation of the
physis with MRI, fat-suppressed three-dimensional spoiled
gradient-recalled echo sequences reportedly provide the best
information.41
to ossify and is present at birth. From birth to skeletal maturity, the
distal femoral physis contributes 70% of the growth of the femur and
37% of the growth of the lower extremity. The annual rate of growth is
approximately three eighths of an inch or 9 to 10 mm. The growth ceases
at a mean skeletal age of 14 years in girls and 16 years in boys.2,172
An intercondylar groove develops along with medial and lateral sulci.
This divides the physis into four quadrants of concave configuration
that match the four convex surfaces of the distal femoral metaphysis.
This complex geometry may help resist shear and torsional forces and
also the large cross-sectional area of the distal femoral physis
contributes to stability. The perichondral ring and ligamentous
structures provide additional resistance to disruption of the physis,
but these structures become thinner during the adolescent growth period.30,103
Thus, substantial force is required to disrupt the distal femoral
physis in juveniles, but less force may produce separation in infants
and adolescents. When fractures do occur in the distal femur, the
irregular configuration of the physis may predispose to crack lines
that extend through multiple regions of the physis regardless of
fracture type (see Fig. 23-11).133
During reduction of displaced fractures, epiphyseal ridges may grind
against the metaphyseal projections and damage germinal cells. Gentle,
anatomic reduction is recommended, but reduction under general
anesthesia does not correlate with reduced risk of growth disturbance.159 Salter-Harris type I fractures generally extend through the hypertrophic
zone and the zone of provisional calcification without traversing the
germinal layers. Salter-Harris type II fractures exit through the
metaphysis with a spike of metaphyseal bone attached to the epiphysis
on the compression side (Thurston-Holland fragment) (see Fig. 23-4A).
In any type of epiphyseal fracture, a flap of torn periosteum may
become interposed between the fragments and prevent reduction (see Fig. 23-4B). Salter-Harris types III and IV fractures cross the entire physis vertically and enter the joint through articular cartilage.
condyle, the metaphysis of the distal femur widens sharply to the
adductor tubercle. In contrast, the metaphysis flares minimally on the
lateral side to produce the lateral epicondyle. The mechanical axis of
the femur is formed by a line between the centers of the hip and knee
joints (Fig. 23-12). A line tangential to the
distal surfaces of the two condyles (the joint line) is in
approximately 3 degrees of valgus relative to the mechanical axis. The
longitudinal axis of the diaphysis of the femur inclines medially in a
distal direction at an angle of 6 degrees relative to the mechanical
axis and an angle of 9 degrees relative to the distal articular plane.67
 |
|
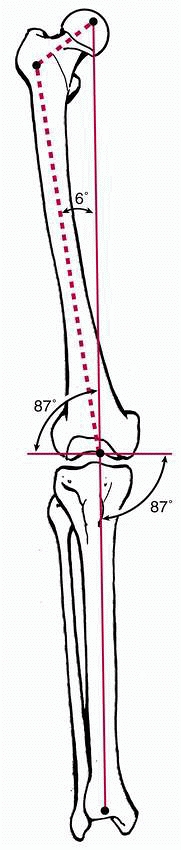
FIGURE 23-12
The mechanical and anatomic axis of the lower extremity. Note that the knee joint is in a mean of 3 degrees of valgus. The femoral shaft intersects the transverse plane of the distal femoral articular surface at an angle of 87 degrees. |
epiphysis is covered by cartilage for articulation with the proximal
tibia and patella. The anterior or patellar surface has a shallow
midline concavity to accommodate the longitudinal ridge on the
undersurface of the patella. The distal or tibial surface of each
condyle extends on either side of the intercondylar notch far around
onto the posterior surface. Here, the articular cartilage nearly
reaches the posterior margin of the physis.
Anteriorly and posteriorly, the synovial membrane and joint capsule of
the knee attach to the femoral epiphysis close to the distal femoral
physis. Anteriorly, the suprapatellar pouch balloons proximally over
the anterior surface of the metaphysis. On the medial and lateral
surfaces of the epiphysis, the proximal attachment of the synovium and
capsule is below the physis and separated from the physis by the
insertions of the collateral ligaments. The strong posterior capsule
and all major supporting ligaments of the knee are attached to the
epiphysis of the femur distal to the physis. Both cruciate ligaments
originate in the upward-sloping roof of the intercondylar notch distal
to the physis. Compression and tension forces can be transmitted across
the extended knee to the epiphysis of the femur by taut ligaments.
originate from the distal femur, proximal to the joint capsule. Thus,
fractures due to forces transmitted through the muscles and tendons do
not seem to be as much of a factor as forces transmitted through the
ligaments and capsule.
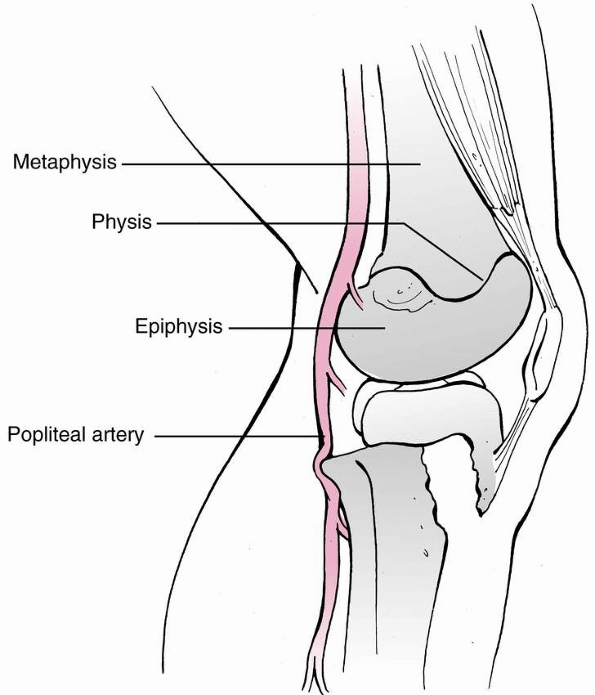
surface of the distal femur by only a thin layer of fat. Directly
proximal to the femoral condyles, the superior geniculate arteries pass
medially and laterally to lie between the femoral metaphysis and the
overlying muscles. As the popliteal artery continues distally, it lies
on the posterior capsule of the knee joint between the femoral
condyles. At this level, the middle geniculate artery branches
anteriorly to enter the posterior aspect of the distal femoral
epiphysis. The popliteal artery and its branches are vulnerable to
injury from the distal femoral metaphysis at the time of hyperextension
injury.
nerves proximal to the popliteal space. The peroneal nerve descends
posteriorly between the biceps femoris muscle and the lateral head of
the gastrocnemius muscle to a point just distal to the head of the
fibula. Thus, there is interposed muscle protecting the nerve from the
potentially sharp edges of a physeal fracture. The nerve is subject to
stretch if the distal femoral epiphysis is tilted into varus or rotated
medially.
from a rich anastomosis of vessels. It is unlikely that the distal
femoral epiphysis would be completely shorn of its blood supply unless
an articular fragment is extruded or completely stripped of its
soft
tissue attachments. Clinically, osteonecrosis of the epiphysis is not a
commonly recognized sequela of distal femoral epiphyseal fractures.
fractures is growth disturbance with angular deformity and/or limb
length discrepancy.3,36,44,89
Ligamentous instability and loss of knee motion are also frequently
reported long-term sequelae. Completely nondisplaced fractures can be
managed with cast immobilization, but close follow-up is recommended to
detect and treat any displacement (Table 23-3).3,71
Closed reduction can be attempted for Salter-Harris types I and II
fractures, but subsequent displacement is frequent when patients are
immobilized in long-leg casts without internal fixation.44,53,159 Anything less than anatomic reduction increases the risk of growth disturbance.44,51,89,133 Fracture remodeling is unpredictable when small degrees of malalignment are accepted in patients older than 2 years of age.133
For these reasons, anatomic reduction, stable fixation, and careful
follow-up are the basis of treatment of physeal fractures of the distal
femur.
of the distal femoral epiphysis are uncommon. Outcomes with cast
immobilization are usually satisfactory,89,159 but displacement can occur even with cast immobilization.3,44
A well-molded long-leg cast is applied with the knee in approximately
15 degrees to 20 degrees of flexion with the intact periosteal hinge
tightened. Thus, if the metaphyseal fragment of a nondisplaced
Salter-Harris type II separation is on the lateral side of the
metaphysis, the cast is applied with three-point molding into slight
varus. Alternative methods of immobilization include a posterior
splint, cylinder cast from proximal thigh to ankle, and a single hip
spica cast. The more secure form of immobilization or internal fixation
should be considered if the patient is obese or potentially unreliable.
|
TABLE 23-3 Methods of Treatment for Distal Femoral Physeal Fractures
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
types III and IV fractures are managed by open reduction and stable
fixation, which are discussed later in this section. Closed reduction
can be attempted up to 10 days after injury for Salter-Harris types I
and II fractures, but these fractures are inherently unstable when
immobilized without restricting motion of the hip. Anatomic reduction
is recommended, with less than a 2-mm gap following reduction.44,71 Redisplacement in long-leg casts has been reported in 30% to 70% of patients treated without internal fixation.44,53,133,159
Minor degrees of displacement may increase the risk of angular
deformity or growth disturbance. Gentle reduction has been recommended
by some authors.133,159
General anesthesia often is helpful to decrease associated muscle spasm
and diminish the risk of further injury to the physis, but Thomson et
al.159 observed that while reduction
under general anesthesia was more likely to be associated with anatomic
alignment it did not reduce the risk of premature physeal arrest. One
cause of failure of reduction is interposed periosteum which may become
entrapped in the fracture (see Fig. 23-4B). Although the alignment may be acceptable, the interposed periosteum, increases the risk of premature growth arrest.126
Joint aspiration may precede manipulation. The periosteum is usually
intact in the direction of displacement of the distal fragment, which
is on the side of the metaphyseal fragment in a Salter-Harris type II
fracture. The first principle for reduction is to avoid harm to the
physis. The maneuver should be 90% traction and 10% leverage. The first
maneuver increases the deformity slightly while traction is applied.
The proximal edge of the displaced epiphysis can then be aligned with
the edge of the metaphysis on the same side as the periosteal tether.
Reduction is then completed by correcting angular deformity and
closing
the fracture gap without sliding the distal fragment over the corner of
the femoral metaphysis. The sequence of events is to pull, tip, and
close the separation. Multiple attempts at closed manipulation are not
warranted and may increase the risk of growth disturbance.
 |
|
FIGURE 23-13 Closed reduction and stabilization of a Salter-Harris type I or II fracture. A.
With medial or lateral displacement, traction is applied longitudinally along the axis of the deformity to bring the fragments back to length. B. For anterior displacement, the reduction can be done with the patient prone or supine. Length is gained first, then a flexion moment is added. |
leg is grasped with the knee in extension and the hip in slight
flexion. The thigh is held by an assistant as moderate longitudinal
traction is exerted by a handhold on the leg above the ankle. If the
displacement of the epiphysis is medial, varus is increased gently and
cautiously to avoid stretching the peroneal nerve. With one hand
holding traction on the leg, the palm of the other hand is placed
against the concave surface of the angulated distal femur. The
epiphysis is pushed toward the metaphysis as the leg is realigned with
the thigh. Once reduction is obtained, longitudinal traction is
released.
epiphysis can be reduced with the patient either supine or prone. With
the patient supine, the hip is flexed approximately 60 degrees and the
thigh is held by an assistant. Longitudinal traction is applied with
the knee in partial flexion. Posterior pressure on the epiphysis is
exerted manually. With continuing traction on the leg, the knee is
flexed 45 to 90 degrees. Prone reduction requires fewer assistants. If
the reduction is done with the patient prone, traction is applied to
the limb, an assistant pushes down on the posterior aspect of the
proximal femur, and the knee is flexed approximately 110 degrees. This
sequence is similar to that for reduction of a supracondylar humeral
fracture. After reduction of an anteriorly displaced epiphysis, it is
important to check the pulses in the foot and ankle. Maintaining
reduction in a cast may be problematic following reduction of this type
of fracture. Immobilization of a swollen knee in flexion of more than
90 degrees may compromise the popliteal vessels and interfere with
circulation to the leg, and regaining extension of the knee may be
difficult after prolonged immobilization in flexion.55
In addition, judgment of frontal plane alignment is difficult in the
flexed knee. For this reason, casting in mild knee flexion of 20 to 30
degrees may be preferable.
displacement of the distal femoral epiphysis, the patient is placed
supine and the surgeon grasps the leg and exerts downward longitudinal
traction while the knee is held partly flexed. Longitudinal traction is
continued as the leg is brought up to extend the knee. An assistant
pulls up directly under the distal femoral epiphysis with one hand and
pushes down on the distal metaphysis of the femur with the other. Such
flexion type injuries can be immobilized in extension.36
is recommended 5 to 7 days after immobilization to detect any
subsequent displacement. Union is normally rapid because the distal
femoral physis is a metabolically active area of bone formation.
Partial weight-bearing on crutches with touchdown gait can be started 2
to 3 weeks after injury. Cast immobilization is continued for
approximately 4 weeks in most cases, and this can be followed by a
removable knee immobilizer and gentle range-of-motion exercises. Full
weight-bearing is generally permitted 6 weeks after initial injury.
X-ray and clinical follow-ups at 6 and 12 months after injury are
recommended to detect early growth disturbances. Even nondisplaced
fractures should be followed until normal resumption of growth can be
determined.
Salter-Harris types I and II epiphyseal fractures of the distal femur
can be reduced by closed manipulation and stabilized with percutaneous
pins or screws under fluoroscopic control. Internal fixation maintains
anatomic reduction better than cast immobilization
and is recommended by most of the more recent authors on this subject.3,44,53,133,157,159,179
A basic principle is that fixation devices should avoid crossing the
physis if adequate fixation can be achieved without doing so.3
In Salter-Harris type I fractures as well as type II fractures with
small metaphyseal fragments, crossing the physis is necessary but
fracture stabilization is important to avoid loss of reduction during
the postoperative period. When traversing the physis is unavoidable,
smooth pins are recommended. Although it may not be possible to tell
with complete certainty whether a subsequent growth disturbance arose
from the injury or pins crossing the physis, clinical experience
suggests smooth pins crossing a physis are unlikely to cause a growth
disturbance. Studies in the rabbit model have determined that drill
holes of 2 to 2.5 mm (3% to 5% of physeal area) do not cause growth
disturbance.73,93
Thus, it is unlikely that a 3 to 3.5 mm (one eighth of an inch) smooth
pin would contribute to growth disturbance following fixation of a
distal femoral epiphyseal fracture. Pins should be widely separated at
the fracture site (see Fig. 23-7C), which is
generally easiest to achieve by inserting the pins at a high angle so
they cross proximal to the physis. Pins can be inserted from each
condyle across the fracture and into the femoral metaphysis, or both
pins can be inserted laterally with one entering the lateral femoral
shaft and proceeding distally and medially. The other pin then enters
the distal femoral epiphysis and proceeds proximally and medially to
engage the opposite cortex. The pins can be cut off under the skin
before application of a long-leg cast or left percutaneous. Infection
is frequent if pins in this region are left out through the skin for
longer than 4 weeks, and intra-articular pins may lead to a septic
knee. If the metaphyseal fragment is large enough, cannulated screws
can be directed transversely across the metaphysis after reduction (Fig. 23-14; see also Fig. 23-8C).
Stability should be gently tested because the metaphyseal spike may not
be firmly attached to the epiphysis in high-energy injuries with
comminution. After stabilization with pins or screws, the lower
extremity is immobilized in a long-leg cast. Postoperative management
is similar to that after closed reduction without fixation. Pins are
generally removed 2 to 3 weeks after fracture, with continued cast
immobilization for a total of 4 weeks.
 |
|
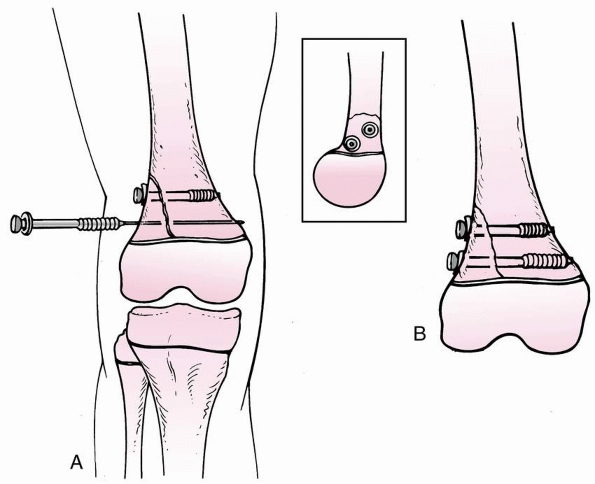
FIGURE 23-14 Screw fixation following closed oropen reduction of Salter-Harris type II fracture with a large metaphyseal fragment. A.
When using cannulated screws, place both guidewires before screw placement to avoid rotation of the fragment while drilling or inserting screw. Screw threads should be past the fracture site to enable compression. Washers help increase compression. Screws may be placed anterior and posterir to each other, which is particularly helpful when trying to fit multiple screws in a small metaphyseal fragment. B. This form of fixation is locally “rigid,” but must be protected with long-leg immobilization or long lever arm. |
require open reduction to obtain anatomic alignment, although
arthroscopic-assisted reduction and percutaneous fixation of a
Salter-Harris type IV fracture have been described.83
is indicated for irreducible Salter-Harris types I and II fractures and
for most displaced Salter-Harris types III and IV fractures. Open
reduction is also appropriate for open fractures or when associated
injuries mandate it (i.e., vascular or ligament injury). A tourniquet
around the proximal thigh can be used for temporary hemostasis if it is
placed proximally enough to avoid binding the thigh muscles under the
inflated tourniquet. How much of a “fracture gap” of a type II fracture
is acceptable is open to debate. Interposed periosteum may contribute
to growth arrest125,126 and has been identified as a possible cause of growth arrest in distal tibial physeal fractures.8 Anatomic reduction is recommended, with less than 2-mm gap following reduction.44,71
fracture displacement because the apex of deformity is the most likely
location of any obstacles to reduction. For a Salter-Harris type II
separation in the coronal plane, a longitudinal incision over the
distal femoral metaphyseal fragment gives direct exposure of any
obstacles to reduction and avoids disruption of the periosteal hinge.
If the displacement is anterior, exposure is best obtained with a
standard medial approach at the anterior border of the sartorius
because this can be extended to expose the popliteal artery if
necessary. After exposure of the fracture, irrigation and removal of
clotted blood permit better inspection of the separation. Interposed
muscle or a flap of periosteum may be identified and removed between
the epiphysis and metaphysis. Special care is taken to avoid any
additional damage to the physis. Once the muscle and periosteal flap
are removed, reduction is carried out primarily with traction and
gentle realignment. To avoid damage to the physis, instruments should
not be placed in the physeal interval. Fixation should be performed as
described previously. After closure of the wound, a long-leg or hip
spica cast is applied.
with internal fixation is almost always necessary for displaced
Salter-Harris types III and IV fractures of the distal femur. Precise
reduction and rigid internal fixation restored articular congruity and
can reduce the risk of growth arrest.51 An anteromedial or anterolateral longitudinal incision is used (Fig. 23-15).
For severely comminuted fractures, an anterior approach may be chosen
with a future total knee replacement in mind. The anterior physeal and
articular margins of the fracture are exposed. Reduction is checked by
noting the apposition of the articular surfaces, the physeal line
anteriorly, and the fracture configuration (see Fig. 23-15). Final reduction can be confirmed with fluoroscopy. The gastrocnemius has been reported as an obstacle
to reduction in a Salter-Harris type III fracture of the medial femoral epiphysis.1
Provisional stabilization is obtained with Kirschner wires (K-wires).
When reduction is accomplished, screws are directed transversely across
the epiphysis in Salter-Harris type III separations or across the
metaphysis and epiphysis in Salter-Harris type IV injuries (see Figs. 23-10, 23-14, and 23-15)
If crossing the physis with fixation is unavoidable, smooth pins should
be used. A coronal plane fracture, or Hoffa fracture, usually involves
the lateral condyle and is approached through an anterolateral incision
except for the unusual medial condyle coronal plane fracture, which the
approach is anteromedial.110
Fixation is generally a lag screw inserted from anterior to posterior.
It may be possible to use an extra-articular starting point.138
Otherwise, the screw can be placed perpendicularly through the
articular surface with the screw head or headless screw slightly buried
beneath the articular surface. Alternatively, Jarit et al.74
demonstrated in cadavers that posterior to anterior stabilization is
more stable, but a small posterolateral exposure is required for screw
insertion. After reduction and fixation, the knee joint is thoroughly
irrigated and inspected for other fractures and ligament disruption.
The limb is immobilized in a long-leg cast in addition to the internal
fixation. Postoperative management is as described on page 873.
 |
|
FIGURE 23-15 Open reduction of displaced lateral Salter-Harris type IV fracture of the distal femur. A.
A longitudinal skin incision, cheating anteriorly if fracture severity raises concern of needing total knee replacement in future. B. Alignment of joint and physis are used to judge reduction. Guidewires for cannulated screws placed above and below physis, parallel to physis. C. Screws inserted in compression with washer on metaphyseal fragment. Washer is optional in epiphyseal fragment if later prominence is of more concern than need for additional compression. |
growth disturbance in a rabbit distal femoral fracture model has been
reported with equivocal results.149
Although nonsteroidal anti-inflammatory medications have been shown to
inhibit callus formation, recommendations for this treatment to prevent
growth arrest are premature.
identified with preoperative imaging or at the time of surgery, it can
be repaired at the time of open reduction. Otherwise, internal fixation
is used to allow early mobilization and rehabilitation of both the
physeal separation and the ligamentous injury. As noted previously, a
rehabilitation program is initiated following union of the fracture
when there is a cruciate ligament tear without meniscal injury. If
there is a repairable meniscal tear and a cruciate ligament tear, then
cruciate ligament reconstruction can be done at the time of meniscal
repair depending on the patient’s age and activity level (see Chapter 24).
S-shaped incision or medial approach is used to follow the course of
the femoral artery. The medial incision is usually preferred because it
provides adequate exposure of the fracture and the artery. Care should
be taken during the incision because the vessel may be superficial
beneath the skin, particularly in an anteriorly displaced fracture. The
hamstring tendons may be “bowstrung” around the femoral metaphysis. The
artery may be in spasm, occluded by intimal tear, or disrupted. After
the vascular structures are identified, the fracture is reduced and
stabilized rapidly before vascular repair, except as noted earlier on
page 847.
soft-tissue injuries or staged surgeries are planned, external fixation
may be indicated. Spanning external fixation may also be indicated in
combination with limited internal fixation for severely comminuted
fractures or other special circumstances. Because of the risks of
secondary knee joint infection and loss of motion, external fixation is
not indicated for most distal femoral physeal fractures.161
stop all remaining growth while the plate is in place. Standard screw
fixation of the plate to bone may crush the perichondral ring and
contribute to growth arrest; however, more modern periarticular locking
compression plates may allow fixation with the plate slightly elevated
from the physis and bone. Also, unicortical fixation is sufficient in
some fracture segments. These plates may eventually provide a method of
temporary fixation of some epiphyseal fractures to reduce damage to the
physis. After bone union, the plates need to be removed so that growth
can resume in a manner similar to temporary staples for guided growth.
At the time of this writing, this option is reserved for adolescents
near the end of growth and children with severe injuries in which severe growth disturbance is believed to be inevitable.
of the patient is useful information for advising parents about the
types and severity of potential complications, but management is
primarily based on the fracture pattern and amount of displacement. The
amount of displacement guides treatment only to the extent that the
fracture is nondisplaced or displaced more than 2 mm. Only nondisplaced
fractures are managed closed with cast immobilization. Special imaging
studies are indicated whenever doubt exists about minor displacement
and for assessment of unusual fracture patterns. MRI is recommended for
type III fractures before surgery. Increasing amounts of displacement
indicate more severe trauma and greater potential for complications,
but the treatment of all displaced fractures is reduction and surgical
stabilization, regardless of the amount of displacement.
that types III and IV fractures almost always require open reduction,
and there is a higher frequency of ligamentous injury associated with
type III fractures. Types I and II fractures can usually be managed
with closed reduction and percutaneous fixation as the primary
treatment. The possibility of child abuse in infants or presence of
compartment syndrome, coronal plane fractures of the condyle, ligament
damage, and neurologic injury should be kept in mind. The need for
follow-up for at least a year should be emphasized to parents at the
time of the initial encounter. The opportunity for early intervention
for growth disturbance is frequently missed because parents believe
their asymptomatic child has fully recovered.
 |
|
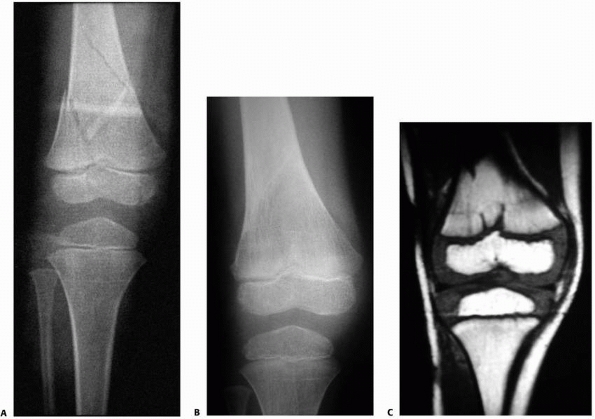
FIGURE 23-16 Five-year-old boy hit by car with fracture of the distal femur. A. AP radiograph of minimally displaced Salter-Harris type IV fracture of the distal femur. B.
AP radiograph of healed fracture. From this view, it is difficult to determine if injury to the physis has occurred, though a central growth arrest was suspected. C. MRI shows a central growth plate injury probably did occur, although this did not result in formation of a bony bar or growth arrest. (Courtesy of Robert Kay, MD, Los Angeles, CA.) |
We believe that even 1 or 2 mm of displacement is cause for concern
about increased risk for growth arrest and also for further
displacement in the cast. A long-leg cast is applied for fractures with
no more than 2 mm or less displacement and less than 3 degrees of
angulation. The cast is applied as closely towards the groin as
possible with firm triangular molding of the shape of the proximal
thigh to aid rotational control. Clinical and x-ray follow-up is
strongly recommended 5 to 7 days after initial treatment to assess
maintenance of reduction. Limited weight-bearing is recommended for 6
weeks, but the cast is removed at 4 weeks. A knee immobilizer is then
provided for 2 more
weeks
along with gentle range-of-motion exercises to reduce the risk of loss
of knee motion. X-ray follow-up is continued until resumption of normal
growth is documented.
displacement is more than 2 mm or angulation is more than 3 degrees. In
all age groups, these fractures are reduced under general anesthesia
and stabilized with percutaneous crossed pins or metaphyseal screws. If
the displacement is anterior, we perform the reduction with the patient
supine. Otherwise, reductions are performed as described earlier in
this chapter. Open reduction is done when anatomic reduction better
than the above criteria cannot be achieved by closed manipulation. For
Salter-Harris type I fractures, smooth 2.0-to 3.2-mm pins are used in a
crossed configuration. Pins are bent to prevent migration, and the skin
is protected by sterile quarter-inch thick felt (see Fig. 23-7C).
We attempt to maximally separate the pins at the fracture site for
stability. Pin insertion sites should avoid the synovial cavity of the
knee. One pin can be inserted from the lateral thigh proximal to the
fracture, across the physis medially, and into the epiphysis. Pins are
removed in 2 to 3 weeks to reduce the risk of pin track infection, but
cast immobilization is continued for 4 weeks after injury.
metaphyseal fragment, one or two cannulated cancellous screws are
placed across the metaphyseal spike and into the femur proximal to the
physis (see Figs. 23-8 and 23-14).
At least two guidewires are placed before drilling and tapping to
prevent rotation of the fragment. Different sized screws, such as a
6.5-mm or 7.3-mm screw in the base of the metaphyseal fragment and a
4.5-mm screw in the smaller upper portion, can be used (see Fig. 23-8E).
for some of these fractures. Also, there may be additional fracture
planes that are difficult to detect with standard x-rays. When
possible, an MRI is recommended preoperatively for types III fractures.
An MRI or CT scan is also useful for Salter-Harris type IV fractures
when there is concern about amount of displacement or fracture pattern.
reduction for all displaced type III and IV fractures to reduce the
risk of growth disturbance and to restore anatomic congruity of the
articular surface of the knee. Anecdotally, we have noted that
significant joint incongruity can be present even with apparently
anatomic fluoroscopic films intraoperatively. X-rays should be
scrutinized for rotational deformity of individual fragments. For a
truly nondisplaced type III fracture, percutaneous screw fixation is
adequate. Medial condylar type III fractures are more common than
lateral condylar fractures, but an anteromedial or anterolateral
approach is used based on the location of the fracture. The fracture
line, the physis, and the joint surface are observed to confirm
anatomic reduction. Cannulated screws are then inserted with either an
open technique or percutaneously with the aid of image intensification.
Insertion through articular cartilage is rarely necessary, but large
osteochondral fragments can be fixed with headless screws countersunk
below the articular surface in the unusual instance where
extra-articular fixation is not possible. Every effort is made to
achieve rigid fixation to allow early motion approximately 4 weeks
after injury. A long-leg fiberglass cast is placed with the knee in 10
to 30 degrees of flexion.
after initial treatment to detect any subsequent redisplacement.
Partial weight-bearing is allowed 2 weeks after injury. Cast
immobilization is continued for approximately 4 weeks in most cases,
and this is followed by a removable knee immobilizer and gentle
range-of-motion exercises for 2 more weeks. Full weight-bearing is
generally permitted 6 weeks after initial injury. When smooth pins have
been used, these are removed 2 to 3 weeks postoperatively to reduce the
risk of infection, but cast immobilization is continued until
approximately 4 weeks postoperatively. Cannulated screws can be removed
as early as 3 to 4 months after injury if MRI is necessary to evaluate
potential growth arrest. A full-length standing x-ray of both lower
extremities is recommended in the early postoperative period to
document limb lengths and alignment. A scanogram may also be obtained,
but we prefer a full-length standing x-ray.139
Repeat full-length x-rays are recommended 6 and 12 months after injury,
regardless of fracture type or initial displacement. Early detection of
complete or partial growth arrest is essential because any growth
disturbance is rapidly progressive and should be treated as soon as it
is detected.
-
When the knee is swollen in infants and
children, distal femoral epiphyseal separation associated with
difficult deliveries, child abuse, myelodysplasia, or other pathologic
conditions should be suspected. -
Minimally displaced fractures of the distal femoral epiphysis are at risk for further displacement.
-
A significantly painful knee examination
with normal x-rays warrants stress x-rays or MRI to detect obscure
distal femoral or proximal tibial epiphyseal fractures.-
Stable fixation with pins or cannulated screws is recommended for all fractures that require reduction.
-
When a cast is used, it should be
extended as far proximally as possible and molded at the proximal thigh
into a triangular shape to provide a small amount of rotational support. -
Repeat x-rays are obtained 5 to 7 days after injury and treatment.
-
-
Growth disturbance is frequent and troublesome, especially between the ages of 2 and 12 years.
-
Reduction is 90% traction and 10% leverage.
-
Multiple closed reduction attempts should be avoided.
-
Follow-up with full-length x-rays of both legs at 3, 6, and 12 months after injury is essential.
-
-
Associated ligamentous injuries may be present.
-
Joint stability should be checked following union.
-
MRI should be considered, especially for type III injuries.
-
-
Stiffness is not uncommon.
-
The cast is removed at 4 weeks and a knee immobilizer is applied for most cases.
-
Gentle range of motion is begun early, but forceful manipulation must be avoided because of the risk of added injury (Table 23-4).
-
|
TABLE 23-4 Distal Femoral Physeal Fractures: Pitfalls and Prevention
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
patients immobilized in a long-leg cast following reduction of
displaced fractures without internal fixation.44,53,133,159 Eid et al.44
reported that a hip spica cast reduced the risk of redisplacement, but
loss of reduction still occurred in 10% of their patients treated in a
spica cast. Late reductions may be problematic whether performed for
redisplacement or for initial treatment. Rang and Wenger131
advised that multiple attempts at closed reduction, or reductions more
than 7 to 10 days after fracture, may do more damage to the physis. An
experimental study in rats did not demonstrated increased risk of
growth disturbance associated with physeal fractures reduced at the
human equivalent of 7 days after injury; however, attempts at reduction
at the equivalent of 10 days resulted in diaphyseal fracture rather
than reduction of the epiphysis.42 Based on this study and opinions of others, it seems reasonable to attempt closed reduction
before fixation up to 10 days following initial distal femoral epiphyseal separation.64,131
After 10 days, open reduction may be required to re-establish
alignment. When fractures are treated more than 10 days after initial
injury, it may be better to observe Salter-Harris types I and II
fractures for possible remodeling or to perform later osteotomies
rather than perform open reduction. For displaced Salter-Harris types
III and IV fractures that are treated late, open reduction is
recommended as soon as possible to restore articular congruity.102
|
TABLE 23-5 Complications of Fractures of the Distal Femoral Epiphysis
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
epiphyseal fracture is growth disturbance with angular deformity or
shortening. This has been reported in 35% to 50% of patients regardless
of anatomic reduction.3,44,53,71,89,154,159
Salter-Harris types I and II fractures in other areas of the body
usually have a low risk of growth arrest, but even minimally displaced
fractures in the distal femur should be followed closely for growth
arrest (see Fig. 23-16) Growth disturbance is uncommon in patients younger than 2 years of age due to the flat shape of the physis in this age group.133
In juveniles, more energy is required to disrupt the physis and the
complex shape of the physis may predispose to fracture lines that
extend through multiple regions of the physis regardless of fracture
type.133 In adolescents, less force
is required to disrupt the physis, but the consequences of growth
arrest are not as severe as in patients between the ages of 2 and 12
years.
months after distal femoral epiphyseal fracture. The distal femur grows
approximately 1 cm a year and growth should resume within this time
frame. Full-length standing x-rays of both lower extremities are
recommended as soon as possible following the initial injury. These are
repeated approximately 6 months later to identify early angular
deformity or increasing length discrepancy. Bilateral AP and lateral
femoral x-ryas 6 months after injury should demonstrate growth arrest
lines (Park-Harris lines) that can be examined for symmetry and
alignment. Growth arrest lines develop when there is a temporary
slowing of growth during periods of malnutrition, trauma, chemotherapy,
or alcohol consumption.52,61,112,120
The normal longitudinal orientation of the zone of provisional
calcification becomes dense and interconnected, forming a transverse
line in the metaphysis. After growth resumes, this dense layer moves
away from the physis and is visible on x-rays as a radiodense line of
bone in the metaphysis.112 If the
line is growing symmetrically away from the physis, then normal growth
has resumed. Failure of a Park-Harris line to appear is evidence of
premature growth arrest when a line is visible in the uninjured distal
femoral metaphysis. An oblique Park-Harris line that converges toward
the physis indicates asymmetrical growth caused by a bone bridge across
the physis that is preventing growth of one side of the physis. When
there is doubt about premature physeal closure, screw removal is
recommended before an MRI study. Growth disturbance can be detected by
MRI as early as 2 months after injury.41
Fat-suppressed three-dimensional spoiled gradient-recalled echo
sequence MRI technique has been described as the best method for
diagnosis and follow-up of premature physeal arrest.41
angulation can reduce the need for osteotomy if diagnosis is made
before a clinically significant deformity develops. After deformity has
developed, an osteotomy is generally required whether bar excision is
performed or not. The risk of significant angular disturbance is
greatest in patients with significant growth remaining. When asymmetric
growth follows a type II separation, the portion of the physis
protected by the Thurston-Holland fragment is usually spared. The
localized area of growth inhibition occurs in that portion of the
physis not protected by the metaphyseal fragment. Therefore, if the
metaphyseal spike is medial, deformity is more likely to be valgus due
to lateral growth arrest.
than 50% of the total area of the physis and at least 2 years of growth
remains, excision of the bony bridge has been recommended.80,123 Although Langenskiöld82 reported normal resumption of growth in 80% of patients, others have reported normal growth in only 25% to 50% of patients.16,23,62,174
Therefore, bilateral epiphysiodesis should be considered when there is
less than 3 to 4 cm of growth remaining and deformity is minor.
Hemiepiphysiodesis alone is not an option for correcting deformity when
a bone bridge already exists on one side of the physis. However,
ipsilateral hemiepiphysiodesis combined with contralateral total
epiphysiodesis can maintain the current status of length and alignment
when growth arrests are diagnosed early in adolescent patients. We
recommend bar excision without osteotomy in an attempt to restore
growth when angular deformity is 5 to 20 degrees, there are more than 2
years of growth remaining, and the area of bar is less than 33% of the
area of the physis. Osteotomy at the time of physeal resection is
recommended when angular deformity exceeds 20 degrees.80,123
For bone bridges larger than 33% of the area of the physis or when
angulation is more than 20 degrees, we recommend osteotomy with
bilateral epiphysiodesis or ipsilateral lengthening depending on the
extent of growth remaining and current amount of discrepancy.
Descriptions of techniques for bar excision, epiphysiodesis, osteotomy,
or lengthening are beyond the scope of this text and are well-described
in other textbooks or periodicals.
Thus, when the patient is within 2 years of skeletal maturity at the
time of injury, the shortening probably will be insignificant. Serial
scanograms for calculation and timing of epiphysiodesis are not helpful
following posttraumatic distal femoral growth arrest. When complete
distal femoral arrest is diagnosed, the only method to prevent
progressive discrepancy is immediate epiphysiodesis of the
contralateral distal femur. Thus, the only decision following diagnosis
is whether to close the opposite physis, allow the discrepancy to
increase within physiological limits, or plan for limb lengthening.
femoral epiphysis may be caused by intra-articular adhesions, capsular
contracture, or muscular contracture. This should be treated with
active and active-assistive range-of-motion exercises. Following
prolonged
immobilization and osteoporosis, periarticular fractures from
overzealous manipulation for knee contracture has been reported.30
Drop-out casts and dynamic braces may be of benefit for persistent
stiffness. For patients with stiff knees in whom conservative treatment
has failed, surgical release of contractures and adhesions, followed by
continuous passive motion, may regain significant motion.146
presented a cogent argument against the use of stress views to
differentiate between a collateral ligament injury and a physeal
fracture of the distal femur. He reported that this test may have been
needed in the past, when the treatment of a collateral ligament injury
was operative and the treatment of a nondisplaced physeal fracture was
immobilization. Stanitski152 argued
that, because the current initial treatment of both a collateral
ligament injury and a nondisplaced femoral fracture is immobilization,
the need for an immediate diagnosis and stress views is no longer valid.
There is no clear answer at the current time. Some prefer an MRI for
diagnosis of obscure injuries because of comfort to the patient along
with the potential to diagnose associated ligamentous or chondral
injuries and bone contusions.98,151
An MRI should always be considered for evaluation of type III fractures
of the medial condyle because the mechanism of injury is similar to the
“triad” injury associated with anterior cruciate ligament and meniscal
disruption.98 Also, MRI is preferred for evaluation of partial or complete growth arrest.41
A CT scan is preferred to assess fracture patterns for surgical
fixation, especially when there is metaphyseal comminution and
intra-articular involvement.
For this reason, separation of the proximal tibial epiphysis requires
significant force. The collateral ligaments provide some protection
from epiphyseal disruption. On the lateral side, the fibula also
provides a buttress for the proximal tibial epiphysis. Anteriorly, the
tibial tubercle projects distally from the epiphysis and overhangs the
adjacent metaphysis. This provides some stability for anterior and
posterior translational forces. Avulsion injuries of the tibial
tuberosity are discussed in the next section. These are very rare prior
to adolescence. Perhaps the most critical feature of fractures of the
proximal tibial epiphysis is the proximity and tethering of the
popliteal artery to the posterior tibia. This increases the risk for
associated vascular injury. Treatment consists of careful observation
and management of associated injuries along with anatomic reduction and
stable fixation of displaced fractures.
sports activities, or other traumatic events such as lawn mower
accidents. Child abuse has been reported to cause a Salter-Harris type
II fracture.158 Separations of this epiphysis can also occur during passive manipulation of the lower limbs in infants with arthrogryposis.39
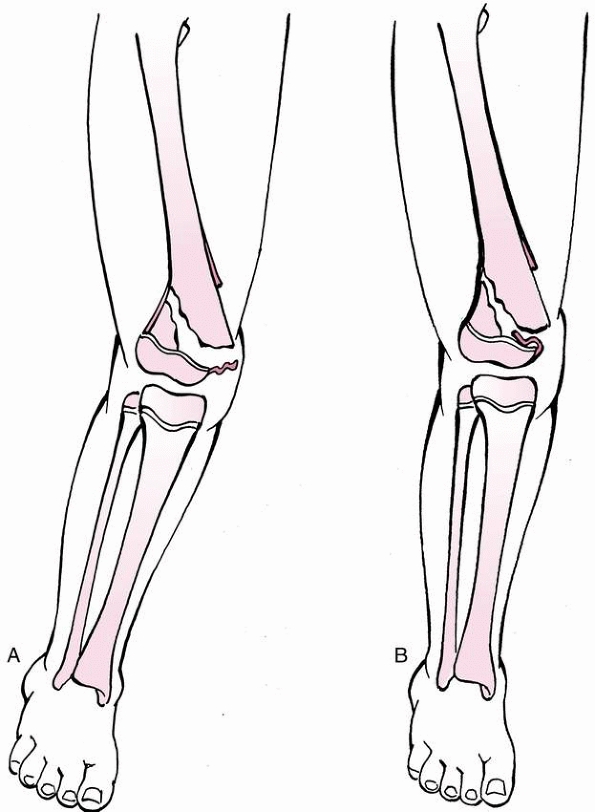
Hyperextension force is a common mechanism, with the metaphyseal
fragment displacing posteriorly. Valgus stress can open the physis
medially with the fibula acting as a lateral resistance force.176
Rarely, a flexion force can cause a Salter-Harris type II or III
fracture. This flexion fracture pattern has a mechanism similar to that
of tibial tuberosity avulsion injuries.
epiphysis usually presents with pain, knee swelling, and a
hemarthrosis. Limb deformity may or may not be present. Extension is
limited because of hamstring spasm. Pain is present over the proximal
tibial physis distal to the joint line. When the proximal metaphysis of
the tibia is displaced posteriorly, a concavity is seen clinically and
can be palpated anteriorly at the level of the tibial tubercle. If the
metaphysis is displaced medially, a valgus deformity is present. There
may be tenderness or angulation of the proximal fibula as well. When
the proximal end of the metaphysis protrudes under the subcutaneous
tissues on the medial aspect of the knee, a tear of the distal end of
the MCL should be suspected. Vascular status should be carefully
evaluated, including distal pulses and warmth and color of extremity
should be noted. Compartments should be assessed by palpation and by
assessment of sensation plus passive and active ankle and toe motion,
especially active dorsiflexion.
associated hemarthrosis may be identified as an increased distance
between the patella and distal femur on a lateral view. Small fracture
lines may be seen extending proximally through the epiphysis or
distally through the metaphysis. A tiny bony fragment at the periphery
of the metaphysis may be the only clue to the diagnosis. Other fracture
lines may be visible only on oblique views. Differentiating a proximal
tibial physeal fracture from a ligament injury should be attempted at
time of presentation, and stress views may be warranted. However, the
same concerns regarding stress films are present with proximal tibial
epiphyseal fractures as with distal femoral epiphyseal fractures. MRI
is a safe, accurate, and more comfortable method for diagnosis of
obscure fractures or ligamentous injuries.151
CT scans may be helpful to determine treatment for Salter-Harris types
III and IV injuries because it provides better identification of the
fracture pattern, articular incongruity, and metaphyseal comminution.
separation of the proximal tibial epiphysis and may be unrecognized.
One series reported concomitant avulsion of the tibial eminence in 40%
of patients with types III and IV fractures.128
The popliteal artery is tethered by its major branches near the
posterior surface of the proximal tibial epiphysis. The posterior
tibial branch passes under the arching fibers of the soleus. The
anterior tibial artery travels anteriorly over an aperture above the
proximal border of the interosseous membrane. A hyperextension injury
that results in posterior displacement of the proximal tibial
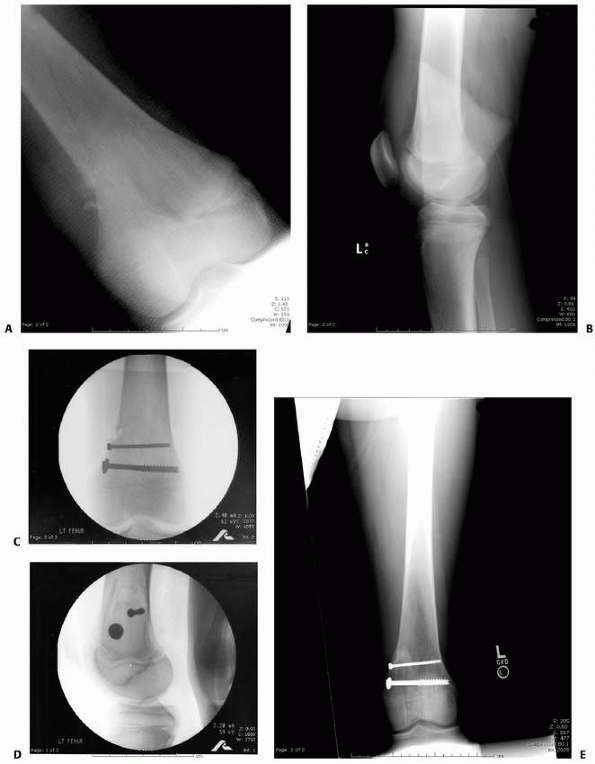
metaphysis may stretch and tear the tethered popliteal artery (Figs. 23-17 and 23-18).
usually resolves following reduction, but motor function, pulses,
warmth, and color should be checked frequently during the initial 48 to
72 hours. It is important to remember that even a fracture that appears
minimally displaced at presentation in an emergency department may have
had significant displacement at the time of injury, particularly in
motor vehicle accidents (see Fig. 23-18).160
Careful attention to evaluating and monitoring the arterial status is
particularly warranted for proximal tibial physeal fractures. Arterial
insufficiency may result from either a tear in the popliteal artery at
the time of epiphyseal separation or from a compartment syndrome. Delay
in recognition results in delay of treatment, which is potentially
catastrophic. Arteriography for isolated injuries but may be helpful
when vascularity is questionable. Fracture fixation is generally
recommended before vascular repair, as discussed for distal femoral
epiphyseal fractures. The extended medial approach usually provides the
best approach for fracture and vessel management, but the posterior
approach provides easier access to the popliteal space and can be used
with percutaneous fixation of the fracture. The lateral approach is
rarely used for vascular access except for localized injuries to the
bifurcation of the popliteal artery.
 |
|
FIGURE 23-17
Posterior displacement of the epiphysis following fracture-separation at the time of injury can cause arterial injury. In addition, a posteriorly displaced fragment can cause persistent arterial occlusion by direct pressure. (Reprinted with permission from Skaggs DL, Flynn JF. Trauma about the knee, tibia, and foot. In Skaggs DL, Flynn JF, eds. Staying out of Trouble in Pediatric Orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 2006.) |
separation of the proximal tibial epiphysis usually recovers
spontaneously with time. Therefore, observation is recommended unless
there is an open wound with possible sharp trauma to the nerve.
described by Salter-Harris type along with direction and amount of
displacement (Table 23-6). A specific
classification for these fractures has not been proposed. Most
separations of the proximal tibial epiphysis are Salter-Harris types I
and II injuries. The frequency of Salter-Harris type III injuries may
be skewed by the inclusion of displaced avulsion fractures of the
tibial tubercle. The incidence of Salter-Harris type IV injuries
depends on whether certain open injuries to the knee are included
(i.e., lawnmower injuries).25 Fifty
percent of Salter-Harris type I separations of the proximal tibia are
nondisplaced. When these fractures are displaced, the metaphysis is
usually medial or posterior relative to the epiphysis.
displacement and the fibula prevents lateral displacement of the
metaphysis. There may be an associated fracture of the proximal
diaphysis of the fibula or a separation of the proximal fibular
epiphysis. Two thirds of Salter-Harris type II fracture-separations of
the proximal tibial are displaced. Displacement of the tibial
metaphysis usually is medial (Fig. 23-19), and
the associated metaphyseal fracture usually is lateral, resulting in
valgus deformity. The proximal fibula may also be fractured.
Salter-Harris type III separations have a vertical fracture line
through the proximal epiphysis into the articular surface to the
physis. There is some controversy about whether intra-articular tibial
tubercle avulsion fractures should be included as a type III proximal
tibial physeal fracture.144
Generally, this fracture is not included in series of tibial epiphyseal
fractures. When the fracture line of a tibial tubercle avulsion
fracture is visible on the AP view, we consider it a proximal tibial
epiphyseal fracture. If, on the other hand, the fracture line is
visible only on the lateral film, then we consider it as a tibial
tubercle fracture (see Fig. 23-26). When
avulsion fractures of the tibial tubercle are excluded from
Salter-Harris type III injuries, the most common fracture involves the
lateral epiphysis, and this is frequently accompanied by a tear of the
ligament. This lateral fragment usually requires internal fixation, and
the ligament may need surgical repair. Triplane and coronal split
fractures of the proximal tibial epiphysis have also been described.
These occur through a partially closed physis during the normal
sequence of physeal closure.34,63,122
lateral tibial plateau. Salter-Harris type V injuries are rare but have
been reported in the proximal tibia.79
Usually, the diagnosis of a type V injury is made in retrospect when
progressive angulation or leg-length discrepancy is noted. Another type
of proximal
tibial epiphyseal fracture is of an avulsion of lateral tibial condyle. Sferopoulos et al.143
described seven patients with either a fracture of Gerdy’s tubercle or
a Segond fracture. All were sustained during a sporting event, and all
were treated nonoperatively in a cylinder cast for 6 weeks. All of the
patients returned to sports between 3 and 4 months after injury. Of
note, two patients also had a concomitant and ipsilateral fractures of
the anterior intercondylar eminence.
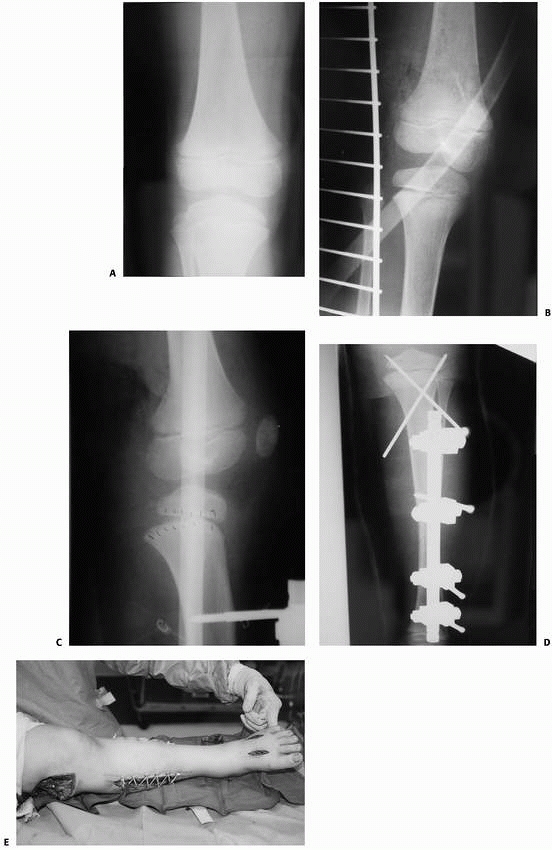 |
|
FIGURE 23-18 Child on back of bicycle struck by car sustained ipsilateral proximal femoral and tibial shaft fracture. A,B. Proximal tibial physeal fracture on initial radiographs were not appreciated. C.
Following external fixation of the tibial diaphyseal fracture, a Salter-Harris type I fracture of the proximal tibial physeal is evident. D. Closed reduction and K-wire fixation were used to treat the proximal tibial physeal fracture. E. Compartment syndrome occurred, which is associated with proximal physeal fractures of the tibia. In this case, the contribution of concomitant injuries to the compartment syndrome is difficult to discern. (A and E reprinted with permission from Skaggs DL, Flynn JF. Trauma about the knee, tibia, and foot. In Skaggs DL, Flynn JF, eds. Staying out of Trouble in Pediatric Orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 2006.) |
|
TABLE 23-6 Classifications and Implications of Proximal Tibial Physeal Fractures
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
technique. The classic hyperextension type has an apexposterior
angulation and results from forced hyperextension. Varus and valgus
types result from abduction or adduction forces. A flexion type injury
may separate the entire proximal tibial epiphysis in a manner similar
to avulsion of the tibial tubercle except that the epiphysis stays
intact as it separates from the metaphysis.72,137
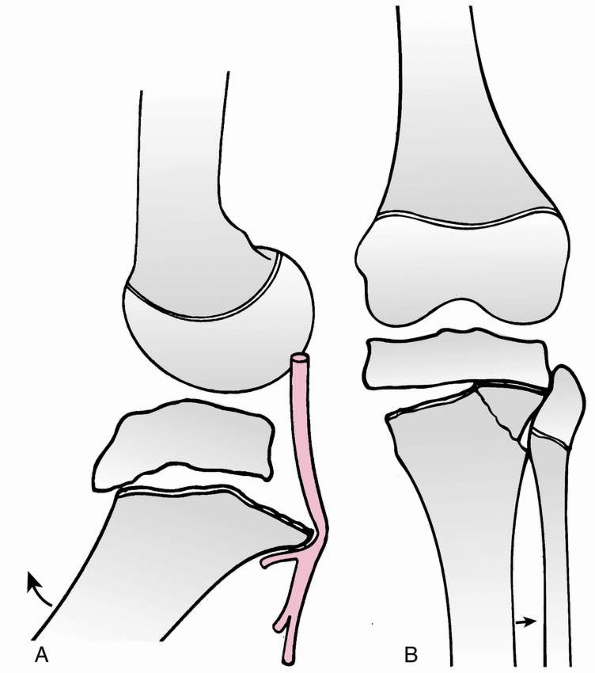 |
|
FIGURE 23-19 A.
Salter-Harris type II separation of the proximal tibial metaphysis, with medial displacement of the proximal tibial metaphysis and complete fracture of the upper third of the fibula. B. After reduction and percutaneous fixation with a 4.5-mm cannulated screw. |
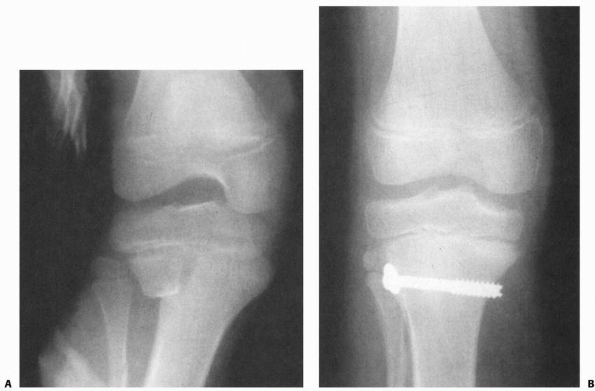 |
|
FIGURE 23-20 Classification of proximal tibial physeal fractures by direction of displacement. A. Type I: hyperextension type usually caused by direct force. Risk of vascular damage exists. B.
Type II: varus or valgus type. Vascular injury is uncommon. Reduction may be inhibited by interposition of pes anserinus or periosteum. |
normally present at birth. It lies in the center of the cartilaginous
anlage, somewhat closer to the metaphysis than to the articular
surface. Occasionally, the ossification center is double. The secondary
center in the tubercle appears between the ages of 9 and 14 years. The
proximal epiphyseal ossification center unites with the tubercle and is
almost completely ossified by age 15.
proximal tibiofibular joint by a thin layer of joint capsule.
Hemorrhage from an epiphyseal separation may extend into the adjacent
tibiofibular joint cavity and through it into the knee joint itself.
The physis closes from central to anteromedially followed by
posteromedial closure.72,116
epiphyseal disruption. The superficial portion of the MCL extends
distal to the physis inserting into the medial metaphysis of the tibia.
The lateral collateral ligament inserts on the proximal pole of the
fibula. The patellar ligament attaches to the secondary ossification
center of the tibial tuberosity that forms the anterior extension of
the physis. This attachment can lead to avulsion injuries of the
anterior epiphysis, but these are uncommon until adolescence when the
quadriceps becomes stronger and the physis weaker. Also, some fibers
extend distal to the physis into the anterior aspect of the upper
tibial diaphysis. The synovium and the capsule of the knee joint insert
into the proximal tibial epiphysis proximal to the physis. There is a
defect in the capsule where the popliteus tendon runs over the
posterolateral corner of the tibia. The capsular ligament anchors the
menisci to the tibial epiphysis medially and laterally.
the posterior aspect of the proximal tibia. Firm connective tissue
septa hold the vessel against the knee capsule. The popliteus muscle
intervenes between the artery and bone (Fig. 23-21).
The lateral inferior geniculate artery runs across the surface of the
popliteus muscle, anterior to the lateral head of the gastrocnemius,
and turns forward underneath the lateral collateral ligament. The
medial inferior geniculate artery passes along the proximal border of
the popliteus muscle, anterior to the medial head of the gastrocnemius,
and extends anterior along the medial aspect of the proximal tibia. The
popliteal artery divides into the anterior tibial and posterior tibial
branches beneath the arch of the soleus muscle.
supply from an anastomosis between the geniculate arteries. The lateral
tibial condyle derives its blood supply anteriorly from the anterior
tibial recurrent artery and posteriorly from branches of the inferior
lateral geniculate artery.35,60 Hannouche et.al.60
suggested that the standard anterolateral approach to the lateral
tibial condyle with submeniscal arthrotomy may damage the epiphyseal
vascularity.
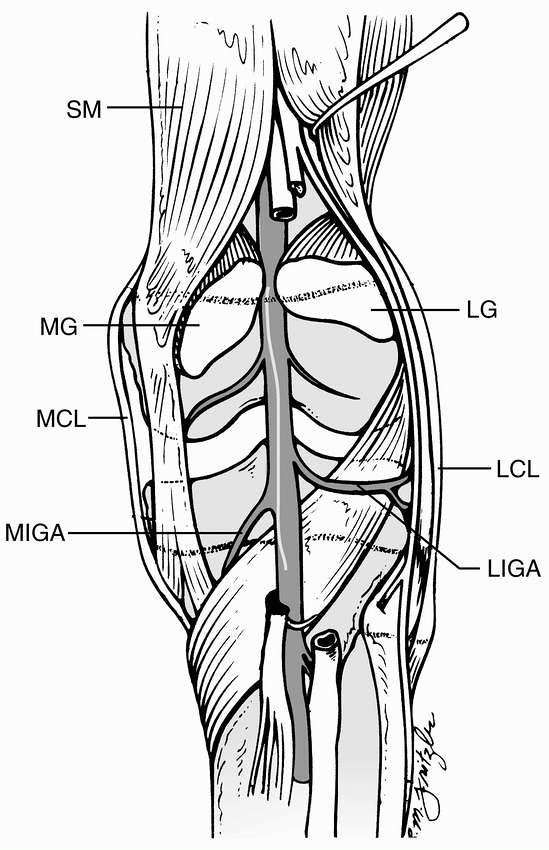 |
|
FIGURE 23-21
Posterior anatomy of the right popliteal region. Note that the popliteal vessels are protected from bone (especially the tibia) only by the popliteus muscle. The vessels are tethered by the geniculate branches and by the trifurcation of the popliteal artery into the peroneal, posterior tibial, and anterior tibial arteries. Note that the anterior tibial artery passes anteriorly between the proximal tibia and fibula, thus causing the popliteal artery to press against a posteriorly displaced tibial metaphysis. ATA, anterior tibial artery; LCL, lateral collateral ligament; LG, lateral gastrocnemius head; LIGA, lateral inferior geniculate artery; MCL, medial collateral ligament; MG, medial gastrocnemius head; MIGA, medial inferior geniculate artery; SM, semimembranosus. |
Traction is important during reduction to minimize the risk of damage
to the physis. Hyperextension fractures are reduced with traction in
combination with gentle flexion. A fracture with valgus angulation can
usually be reduced by adducting the leg into varus with the knee
extended. This should be done with gentle manipulation to decrease the
risk of injury to the peroneal nerve. After reduction, a long-leg cast
with varus molding is applied with the knee in slight flexion.
surprisingly unstable. Reducible but unstable types I and II fractures
can be stabilized with smooth pins inserted percutaneously.
Salter-Harris type II fractures with a large metaphyseal spike can be
stabilized with compression screws that fix the spike to the metaphysis
without crossing the physis (see Fig. 23-19).
|
TABLE 23-7 Methods of Treatment for Proximal Tibial Epiphyseal Fractures
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
reduced require open reduction for removal of soft tissue
interposition. The pes anserinus and periosteum have been reported as
obstructions to reduction of Salter-Harris type II fractures.31,158,176
Operative fixation of a Salter-Harris type I or II hyperextension
injury is recommended to facilitate wound management when vascular
repair is necessary. Pin or screw fixation in an expeditious manner is
generally recommended before vascular repair.
types III and IV injuries. An anterior incision is used to allow
inspection of the articular surface. Anatomic reduction is performed,
using the joint surface as a guide. A pin can be inserted in the
displaced fragment as a joystick to assist reduction if needed. Smooth
pins or screws are then inserted horizontally across the epiphysis in
type III fractures. Metaphyseal and epiphyseal screws parallel to the
physis are recommended for Salter-Harris type IV fractures to avoid
physeal damage and allow growth to resume. A torn meniscus should be
repaired if possible.
sterile precautions. Injection of 2 to 5 cc of 0.5% bupivacaine can
help relieve pain and allow better examination. Conscious sedation or
general anesthesia can be used for additional pain relief and muscle
relaxation. Patients with a nondisplaced (2 mm or less) proximal tibial
epiphyseal fracture are placed in a long-leg cast with the knee flexed
20 to 30 degrees. One-half-inch thick foam is placed along the
popliteal fossa and calf and/or the cast is bivalved to permit
swelling. In most instances, the child is admitted to the hospital for
observation and gentle elevation because of the high incidence of
vascular injury and the possibility of developing a compartment
syndrome. AP and lateral x-rays are repeated 1 week after the injury to
confirm maintenance of reduction. The cast is removed 4 to 6 weeks
after injury if the fracture is radiographically and clinically healed.
Return to normal activities is generally permitted in 3 to 6 weeks
following cast removal.
injury, we check for signs of neurologic or circulatory impairment. If
there are signs of poor circulation, the child is brought urgently to
the operating room for reduction under general anesthesia. When this is
not possible, a closed reduction can be done in the emergency
department with conscious sedation. For all closed reductions of
physeal fractures, the principle of 90% traction and 10% leverage is
used. The patient is positioned supine. The hip and knee are flexed to
45 degrees while an assistant provides countertraction by stabilizing
the thigh. The surgeon grasps the proximal leg and applies traction
while displacing the metaphysis anteriorly. Further flexion of the knee
is rarely necessary, but may aid initial reduction. Reduction is
confirmed with fluoroscopy or standard x-rays. When the reduction is
stable through a gentle range of knee motion, a bivalved cast is
applied. If the reduction is not stable, percutaneous smooth pin
fixation is used to avoid excessive knee flexion. With or without
internal fixation, a long-leg cast is applied with the knee in 20 to 30
degrees of flexion. The child is admitted for observation and
elevation. For an abduction injury with valgus angulation, the
reduction is done with the knee in full extension, followed by
immobilization in almost full extension with varus molding.
diameter Kirschner wires is used for Salter-Harris types I and II
fractures. These are inserted in a crossing manner through the tibial
metaphysis and across the physis to stabilize the epiphysis (Fig. 23-22).
The leg is immobilized in a bivalved cast with the knee in 20-30
degrees of flexion. Three weeks after fixation, the pins are removed,
but cast immobilization is continued for up to 3 more weeks. Return to
normal activities is generally permitted in 4 to 8 weeks following cast
removal.
when reduction is incomplete. Most Salter-Harris types III and IV
fractures should be stabilized with smooth Kirschner wires or with
cannulated screws. We prefer cannulated screws inserted parallel to the
physis. After internal fixation, the knee is carefully stressed into
valgus to verify if the MCL is intact. Similarly, a gentle Lachman test
is performed to ensure anterior cruciate ligament/tibial spine
integrity. An MCL injury should heal with immobilization of the
fracture but, an anterior cruciate ligament/tibial spine injury may
require reconstruction and/or fixation (see Chapter 24).
is removed. Non-weight-bearing is recommended during early healing of
Salter-Harris types III and IV injuries to reduce the risk of
displacement.
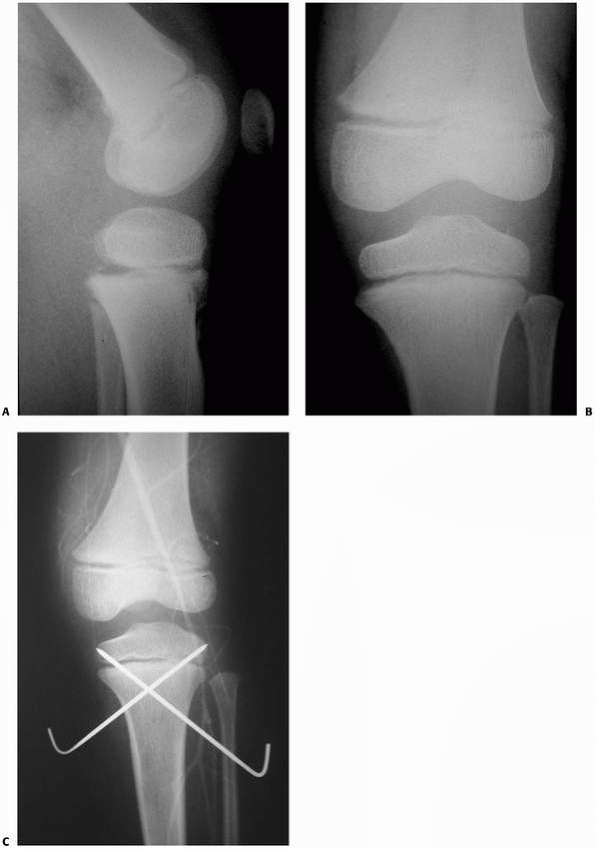 |
|
FIGURE 23-22 A. Lateral radiograph demonstrating minimal posterior displacement of a Salter-Harris type I fracture of the proximal tibia. B. No significant displacement is noted on the AP radiograph. C. Although angiogram demonstrates good flow past the fracture site, a compartment syndrome developed. (A
reprinted with permission from Skaggs DL, Flynn JF. Trauma about the knee, tibia, and foot. In Skaggs DL, Flynn JF, eds. Staying out of Trouble in Pediatric Orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 2006.) |
-
X-rays should be scrutinized for nondisplaced proximal tibial fractures especially for
-
children with knee pain following trauma.
-
patients with polytrauma.58,143
-
-
Observation in the hospital is
recommended for all fractures of the proximal tibia because of the risk
of vascular injury or development of compartment syndrome. -
All casts should be bivalved or nonconstricting splints should be used for early immobilization.
-
Unrecognized or late presentation of arterial injury.
-
Even minimally displaced fractures may have arterial injury from displacement at time of injury.
-
-
Compartment syndrome.
-
Nondisplaced fractures can be misdiagnosed as medial collateral ligament injuries.169 Stress x-rays or MRI can help make the correct diagnosis.
-
Proximal tibial growth disturbance can occur following diaphyseal fractures.66,107
-
This may be due to unrecognized trauma or generalized response to injury.
-
Recurvatum is the most common deformity
and must be carefully assessed on lateral x-rays with comparison to the
contralateral side. Osteotomy may be necessary for correction.119
-
-
Intra-articular pin placement can lead to a septic joint.
-
An unrecognized anterior cruciate ligament/tibial spine avulsion can cause late instability.
unstable, regardless of the Salter-Harris type. It is wise to obtain
x-rays 1 week after injury to verify alignment. At that point, it is
still possible to remanipulate if necessary. This complication can
usually be avoided by using screw or smooth pin fixation following
fracture reduction.
|
TABLE 23-8 Complications of Proximal Tibial Physeal Fractures*
|
|||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||
physeal fractures because of mechanical blockage of the vascular
structures by a displaced fracture, damage to the popliteal artery, or
collateral damage to soft tissues at time of a large force injury. It
is important to remember in this injury that even a small posterior
displacement of the metaphysis may obstruct popliteal blood flow as the
artery is tethered anteriorly against the metaphysis by the anterior
tibial artery (see Fig. 23-17) Burkhart and Peterson25
reported a 12-year-old hurdler who sustained a closed Salter-Harris
type III injury that was treated with closed reduction and a long leg
cast. Increased pressure in both the anterior and posterior muscle
compartments caused narrowing of the terminal branches of the popliteal
artery, although arteriography showed that the popliteal artery itself
remained patent. Fasciotomies and a sympathectomy failed to save the
leg.
injuries to the proximal tibial epiphysis may cause shortening or
angulation from subsequent growth inhibition. This inhibition can occur
after all types of proximal tibial epiphyseal injuries. Anatomic
reduction with internal fixation reduces the risk of growth disturbance.140
The amount of angulation depends on the proximity of the area of growth
arrest to the periphery of the physis and the years left for growth
after injury. When partial or complete growth arrest is diagnosed, the
only methods to prevent progressive deformity are excision of an
epiphyseal bar or bilateral epiphysiodesis. Hemiepiphysiodesis will not
correct angular deformity when that deformity is caused by a bone
bridge. Early recognition and treatment of growth disturbance following
fracture may prevent the need for osteotomy. The proximal tibial physis
grows approximately 6 mm per year and growth ceases at approximately
age 14 in girls and 16 in boys.2,172
If complete growth arrest follows an epiphyseal separation at this
level and the patient is within 3 years of the end of growth, an
equalization procedure may be unnecessary. If more years of growth
remain, immediate epiphysiodesis of the opposite extremity may be
considered, or leg lengthening at a later stage may be indicated
depending on the expected final leg length discrepancy.
instability and two additional patients had asymptomatic anterior
laxity. In the same series, degenerative changes were noted on x-rays
in two patients with varus deformity. Bertin and Goble15
reported eight cases of ligamentous laxity in 13 patients with proximal
tibial physeal fractures. Most other series do not report late
instability or degenerative changes, but this may be underreported for
type III and IV fractures.
uncommon injury accounting for less than 1% of all epiphyseal injuries
and approximately 3% of all proximal tibial fractures in adults and
children.18,96,124 This injury is most commonly sustained by adolescents during sports activity.
occur in adolescents during jumping activities such as basketball, when
jumping is resisted, or during eccentric loading while landing.18,28,29,59,104,116 Tibial tuberosity fractures are reported almost exclusively in males.18,28,29,59,104,116
Avulsion of the tibial tubercle occurs when the patellar ligament
traction exceeds the combined strength of the physis and the supporting
soft tissues. During adolescence, quadriceps strength increases and
physeal stability decreases.21,91
There are two mechanisms of injury: violent contraction of the
quadriceps muscle against a fixed tibia, as occurs in resisted jumping,
and acute passive flexion of the knee against the contracted
quadriceps. A study of two adolescent gymnasts with tibial tuberosity
fractures found extension strength of the contralateral and injured
knee was greater than nonathletic controls and their gymnastic peers.
The authors hypothesized that the greater-than-usual strength of the
quadriceps was able to overcome the strength of the tibial tuberosity
or the physis.91
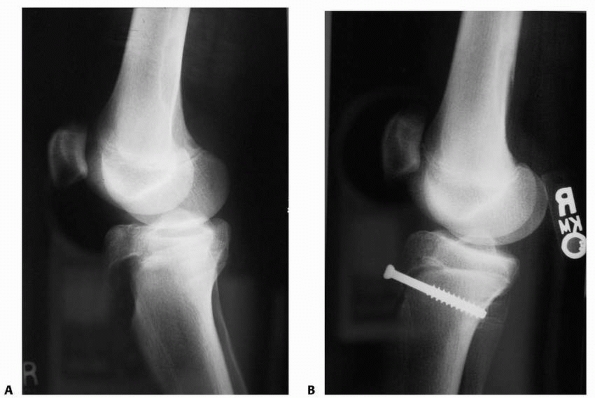 |
|
FIGURE 23-23 Type III tibial fracture with intra-articular extension. A. Lateral view demonstrates fracture and patella alta. B.
Fracture was treated with open reduction and internal fixation with one 7.3-mm cannulated screw. Alternatively, multiple smaller screws could have been used. |
aspect of the proximal tibia. Joint effusion and tense hemarthrosis may
be present. A freely movable triangular fragment of bone may be
palpated subcutaneously between the proximal tibia and the femoral
condyles. This fragment may have rotated so that the distal end
projects forward, tenting the overlying skin. The bed from which the
fragment was avulsed may be identified by a palpable defect on the
anterior aspect of the proximal tibia.
severity of displacement of the tibial tubercle and may be as much as
10 cm. With a type I avulsion, the patient may be able to partially
extend the knee actively through the remaining soft tissue attachments.
Active extension is very impaired or impossible with types II and type
III injuries.
adolescents in whom the secondary ossification of the tibial tubercle
has developed. The best x-ray view to demonstrate displacement is a
lateral projection with the tibia rotated slightly internally because
the tubercle lies just lateral to the midline of the tibia. In this
projection, the size and degree of displacement of the fragment can be
identified more clearly. Two nondisplaced fragments may represent
normal ossification of the tibial tubercle since two or more secondary
ossification centers can be present as the tibial tubercle matures. A
smooth, horizontal nondisplaced radiolucent line through the tubercle
should not be confused with an epiphyseal fracture. Patella alta is
absent in normal knees and can indicate a displaced tibial tuberosity
avulsion fracture or distal pole patella sleeve fracture. The patella
will displace proximally the same distance as the tibial tuberosity is
displaced (Fig. 23-23). Patella alta17,165
may also help diagnose sleeve avulsion fractures of the tibial
tubercle, or patellar tendon ruptures, which have also been reported in
children.38,106
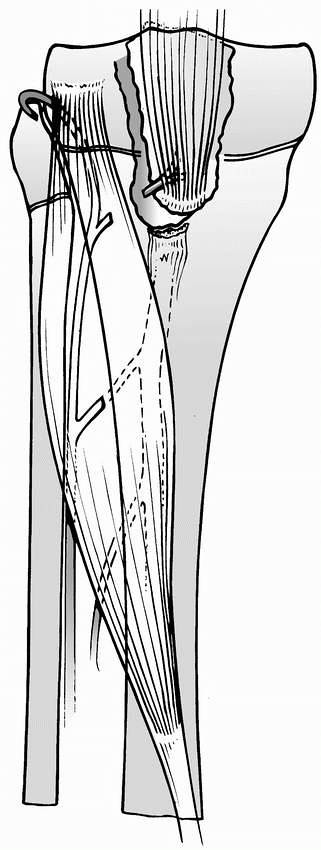 |
|
FIGURE 23-24
Probable mechanism of development of compartment syndrome after tibial tubercle avulsion. The anterior tibial recurrent artery, and possibly its branches, is torn and retracts into the anterior compartment musculature. |
predisposed to development of compartment syndrome. The anterior tibial
recurrent artery near the base of the tibial tubercle may be avulsed
and bleed into the anterior compartment of the leg (Fig. 23-24).118 Severe pain greater than expected from this injury alone should raise suspicion of impending compartment syndrome.
include patellar ligament and quadriceps tendon avulsions, collateral
and cruciate ligament tears, meniscal damage, and a lateral plateau rim
fracture.18,99,104,117 Avulsion of the anterior tibialis muscle has also been reported.76,175
differentiated from Osgood-Schlatter disease by anatomic pathology and
clinical presentation. Osgood-Schlatter disease is a chronic traction
injury of the anterior ossicle of the tuberosity with no involvement of
the physis (Fig. 23-25). Ogden and Southwick116
observed new bone formation anterior to the secondary ossification
center in Osgood-Schlatter disease and concluded that the weak link in
Osgood-Schlatter disease is the attachment of the tendon to the
anterior surface of the tibial tubercle. In contrast, tibial tubercle
avulsions fail through the underlying physis, which is the posterior
surface of the tibial tubercle. A prospective study of Osgood-Schlatter
lesions evaluated with serial MRI, CT, and bone scans showed that the
most striking feature was soft tissue inflammation, not bony avulsion.135
An ossicle was seen anterior to the tibial tubercle in only one third
of the patients. There are clear differences in presentation as well.
Avulsion of the tibial tubercle occurs acutely with a specific injury,
whereas the patient with an Osgood-Schlatter lesion usually presents
with a gradual onset of symptoms characteristic of an overuse injury.
An adolescent with a displaced acute avulsion of the tibial tubercle is
immediately unable to stand or walk; however, an adolescent with
Osgood-Schlatter disease often tries to continue athletic activities
despite discomfort. There are several reports of acute tibial tubercle
avulsions patients with pre-existing Osgood-Schlatter disease,33,104,109,116
which has led to speculation that Osgood-Schlatter disorder may
predispose children to tibial tuberosity avulsion, but convincing
scientific evidence is absent and both conditions are prevalent in
adolescent male athletes.
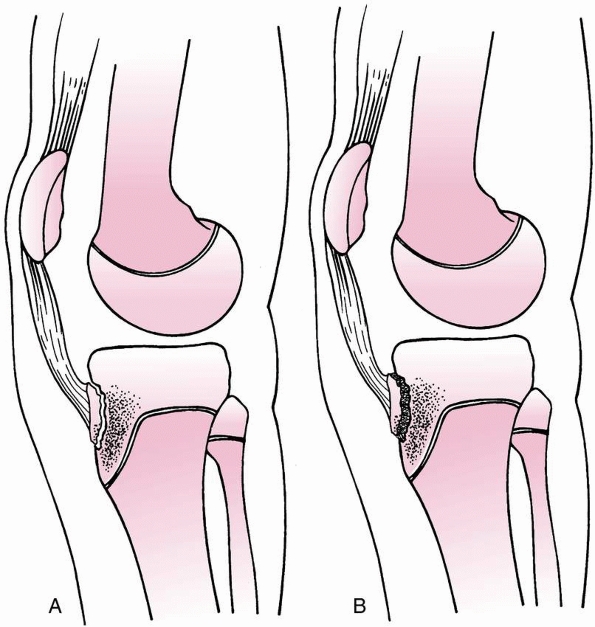 |
|
FIGURE 23-25 Development of Osgood-Schlatter lesion. A.
Avulsion of osteochondral fragment that includes anterior surface cartilage and a portion of the secondary ossification center of the tibial tubercle. This may be clearly differentiated from a tibial tuberosity fracture, which occurs along the apophysial cartilage. B. New bone fills in the gap between the avulsed osteochondral fragment and the tibial tubercle but does not disrupt the physis. |
fractures that extend into the joint with Salter-Harris type III
separations of the anterior tibial epiphysis. For example, Shelton and
Canale144 and Burkhart and Peterson25
included tubercle avulsions in their reviews of proximal tibial physeal
separations. because the mechanism of injury, associated injuries, and
treatment of tibial tubercle avulsions with intra-articular extension
are more similar to tibial avulsion fractures than proximal tibial
epiphyseal fractures, we consider this type of fracture a tibial
tuberosity fracture.
fracture in which the physeal separation occurs through the tibial
tuberosity and extends posteriorly into the horizontal tibial physis.
Sleeve avulsion fractures of the tibial tuberosity extending over the
anterior metaphyseal area of the tibia have been described in four
children, aged 10 to 15 years.24,38
These injuries are similar to patellar sleeve fractures in that initial
x-rays may show no more than small subchondral fragments of bone. Open
reduction and fixation were recommended. We follow Davidson and Letts’38
recommendation that sleeve avulsion injuries of the tibial tubercle can
be added to the Watson-Jones system as a type V. Fractures may be
comminuted or have multiple fracture lines not easily classifiable
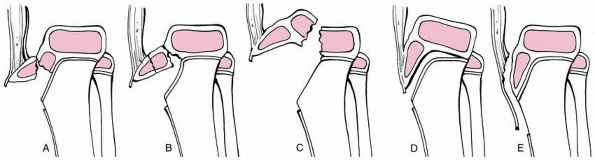 |
|
FIGURE 23-26 A.
Type I—the physeal separation occurs through the tubercle apophysis. The fracture of tubercle is distal to the junction of the ossification centers of the tibial tubercle and the proximal tibial epiphysis. B. Type II—the physeal separation occurs through the tubercle apophysis. The fracture extends anteriorly through the area bridging the ossification centers of the tibial tubercle and the proximal tibial epiphysis. C. Type III—the physeal separation occurs through the tubercle apophysis. The fracture propagates through the proximal tibial epiphysis into the knee joint under the anterior attachments of the menisci. D. Type IV—the physeal separation occurs through the tubercle apophysis and propagates posteriorly through the horizontal proximal tibial epiphysis. The fracture may exit posteriorly through the physis, as a Salter-Harris type I equivalent, or through the metaphyseal, as a Salter-Harris type II equivalent. E. Type V—avulsion of a large area of periosteal attachment of the patellar tendon associated with small subchondral fragments of bone. Not a true physeal fracture. |
prominence on the anterior aspect of the proximal tibia. It lies
approximately one to two fingerbreadths distal to the proximal
articular surface of the tibia and forward of the anterior rim of the
proximal articular surface.
the postnatal development of the tibial tubercle into four stages. The
cartilaginous stage occurs before the secondary ossification center
appears and persists in girls until approximately 9 years of age and in
boys until 10 years of age. The apophyseal stage, in which the
ossification center appears in the tongue of cartilage, occurs between
8 and 12 years in girls and between 9 and 14 years of age in boys. The
epiphyseal stage, in which the secondary ossification centers coalesce
to form a tongue of bone continuous with the proximal tibial epiphysis,
occurs in girls between 10 and 15 years and in boys between 11 and 17
years of age. In the final bony stage, the epiphyseal line is closed
between the fully ossified tuberosity and the tibial metaphysis.
pole of the patella and the tibial tubercle, is the terminal portion of
the powerful quadriceps muscle. During the apophyseal stage of
development of the tubercle, the patellar ligament inserts into an area
of cartilage proximal and anterior to the secondary ossification center
of the tubercle. The main attachment is in the proximal area of this
insertion zone between the secondary ossification centers of the
tubercle and the proximal tibial epiphysis. The fibrocartilaginous
tissue lying anterior to the secondary ossification center receives
only the distal part of the insertion. During the epiphyseal stage, the
patellar ligament inserts through fibrocartilage on the anterior aspect
of the downwardprojecting tongue of the proximal tibial epiphysis. The
inserting fibers merge distally into deep fascia after spanning the
physis. With traumatic avulsion of the tibial tubercle in this stage of
development, a broad flap of adjacent periosteum is attached to the
displaced fragment. In the final bony stage, the tendon fibers insert
directly into bone. After physiologic epiphysiodesis has occurred, the
tibial tubercle rarely is avulsed if the patient has normal bone.
insertion of the quadriceps muscle onto the leg beyond the knee joint,
it is reinforced by retinacular fibers radiating from the medial and
lateral margins of the patella obliquely down to the respective tibial
condyles. After traumatic avulsion of the tibial tuberosity, a limited
amount of active extension of the knee still is possible through the
retinacular extensions of the extensor mechanism. However, patella alta
and an extensor lag are present. The anatomic position of the tibial
tubercle is biomechanically important in terms of patellar tracking and
patellofemoral forces.
a plexus of arteries behind the patellar ligament at the level of the
attachment to the tibial tubercle.35 This vascular anastomosis arises from the anterior tibial recurrent artery and may be torn with this fracture.118,175
Several small branches extend down into the secondary ossification
center. A smaller part of the blood supply enters the superficial
surface of the tubercle from adjacent periosteal vessels.
type I fractures. Persistence of even a small gap between the distal
end of the tubercle and the adjacent metaphysis may indicate an
interposed flap of periosteum.29,59
Minimally displaced, small avulsion fragments have been treated
successfully with immobilization in a cylinder cast or long-leg cast.28,29,104,116
The leg is positioned with the knee extended, but even with a long-leg
cast, a straight leg raise can place tension on the fracture. Molding
above the proximal pole of the patella has been suggested to help
maintain reduction.
tubercle avulsions that are intra-articular or displaced more than 2 to
3 mm.18,28,59,109
Residual displacement may lead to extensor lag and quadriceps weakness.
It may also be difficult to maintain reduction following closed
reduction.
fractures, anatomic reduction with stable fixation is recommended by
several authors.28,29,104,116
facilitate any possible knee surgery in the future. The fracture bed is
carefully cleared of debris. A periosteal flap is frequently an
impediment to reduction.29,59
This is extracted and the fragment is reduced with the knee extended.
Screw fixation is used when the tuberosity fragment is large enough for
this type of fixation. The screw is inserted from anterior to posterior
but does not need to engage the posterior cortex when cancellous lag
screws are used. When there are 3 or more years of growth remaining or
when the fragment is too small for screw fixation, transfixing pins can
be used instead of screw fixation. Alternatively, a tension band can be
passed around the fragment or through the patellar ligament and fixed
through a drill hole across the anterior tibia distal to the attachment
of the tuberosity. Tension band wiring has also been reported as a
method to facilitate rapid rehabilitation in athletes.109
The wire is driven around the proximal pole of the patella or through a
drill hole in the distal pole and then looped distally through a
cannulated cortical screw that is inserted across the anterior tibia
distal to the patellar tendon insertion. This method may also be useful
when the fracture fragments are comminuted or too small for secure
fixation to the tibial metaphysis.
recommended fixation with small cancellous screws and heavy
nonabsorbable sutures to repair the torn retinaculum and periosteum.
Protection in a cast is recommended for 6 weeks because fixation
depends on soft-tissue stability.
10 degrees of flexion is recommended for a period of 4 to 6 weeks.
Shorter periods of immobilization are used in younger adolescents when
fixation is secure. For large fragments that are securely fixed with
two or more screws, a knee immobilizer can be substituted for cast
immobilization. Range of motion and quadriceps strengthening are
initiated 6 weeks following injury.
fractures that are displaced less than 2 mm and are stable enough for
the patient to actively fully extend the knee against gravity. A
long-leg cast is applied, and straight leg raising is discouraged.
Lateral x-rays are repeated at 1 week to verify anatomic alignment.
Postreduction treatment is as described after operative treatment.
recommended for all tibial tuberosity avulsion fractures that are
displaced or intra-articular (Fig. 23-27). Even
when closed reduction is successful, percutaneous surgical
stabilization is recommended. For open reduction, a longitudinal
incision just lateral to the tibial tubercle is preferred to minimize
the potential for scar discomfort over prominent bone. The gap between
the displaced fragment and its bed is cleared of any soft tissue
interposition. A tourniquet can be used high on the thigh, but may need
to be released if it is hindering reduction of a displaced fracture due
to constriction of the quadriceps muscle. If the reduced fragment is
large enough, we prefer to use cancellous screws in compression,
extending through the tubercle and parallel to the joint into the
metaphysis. Fixation across the posterior cortex is not essential,
because the cortex is quite thin at this level. If large screw heads
are a concern for later discomfort in thin patients or if bone
fragments are small and/or comminuted, multiple 4.5-mm screws are used (Fig. 23-28)
instead of a larger 6.5 or 7.3-mm screw. If the patient is more than 3
years from skeletal maturity, which is uncommon for this fracture,
smooth pins are used. Alternatively, a tension band technique can be
used to prevent fixation across the distal tibial physis. A number 1
braided polyester nonabsorbable suture (Ticron, Kendall Company,
Mansfield, MA, or Ethibond, Johnson & Johnson, Langhorne, PA) can
be used for this repair. The suture is passed through the distal
patellar ligament and looped through a cancellous screw that has been
inserted through a drill hole across the anterior tibial cortex.
Sutures are also used to repair the periosteum to add stability. During
an open reduction, the anterior compartment fascia is released when
there is early swelling of the anterior compartment. Following wound
closure, a long-leg or cylinder cast is applied in full knee extension
and the patient is observed in the hospital with elevation overnight.
articular surface is used as a guide to fracture reduction, and the
menisci should be inspected for tears.
-
Open reduction with internal fixation is recommended for almost all tibial tuberosity avulsion fractures.
-
There is an increased risk of compartment syndrome due to bleeding of the recurrent anterior tibial artery.
-
Recognition of sleeve avulsion fractures without bone may be difficult.
-
Use of a tourniquet may bind the quadriceps and hinder reduction of a displaced fracture.
-
Premature anterior physeal growth arrest may cause genu recurvatum that requires osteotomy for correction.119
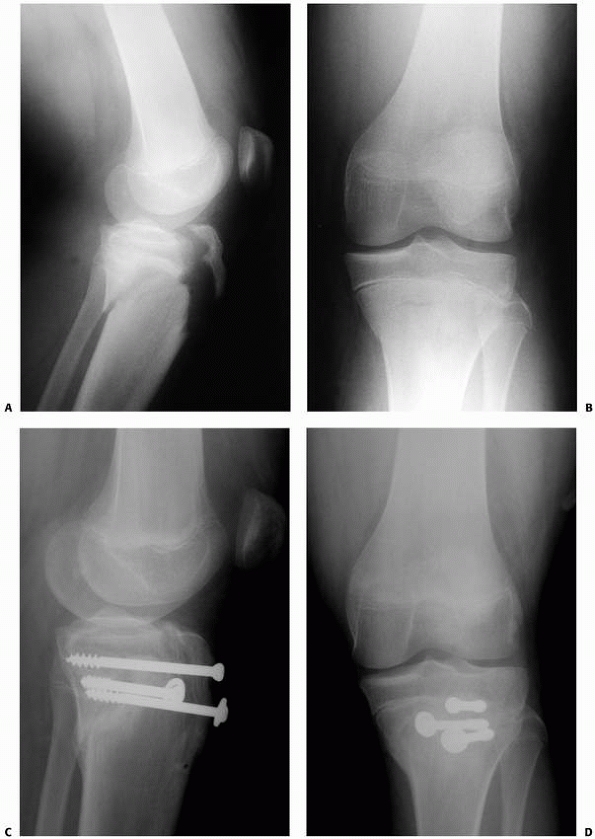 |
|
FIGURE 23-27 A.
Lateral radiograph demonstrating a complex tibial tuberosity fracture extending into the joint, as seen in a type III fracture, as well as posterior along the physis and out the epiphysis. B. AP radiograph. C. Lateral view 3 months after surgery. D. AP view 3 months after surgery. (Courtesy of Robert Kay, MD.) |
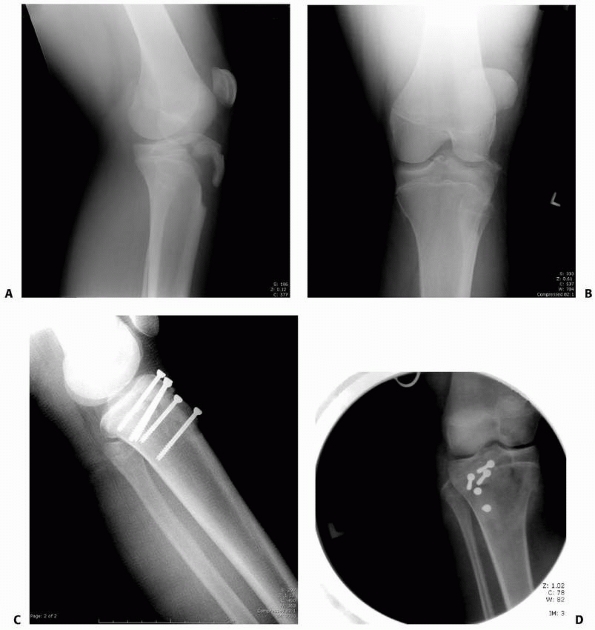 |
|
FIGURE 23-28
Type III tibial tuberosity avulsion in a 14-year-old girl sustained while landing after a jump in basketball. This is a very common mechanism of injury. A. Lateral view at injury. B. AP view at injury. C. Lateral view following open reduction and internal fixation with cannulated 4.5-mm screws. Note that screws are in compression with threads not crossing the fracture site. There is no significant growth left in this patient, so screw placement relative to the proximal tibial physis was not of concern. D. AP view of fixation. Note that screws are placed perpendicular to the plane of the fracture, which often leads to the screws directed laterally. |
with few complications after reduction and surgical stabilization of
displaced fractures and closed management of nondisplaced
extra-articular fractures (Table 23-9). When
fractures unite in anatomic position, many series report no
complications other than prominent screws. Most patients return to full
athletic activity without residual sequelae within 3 to 6 months.42,52,61,64,120,176
genu recurvatum in a growing child. However, this complication is rare
because most of these injuries occur near the end of growth. If this
complication occurs, we recommend a proximal tibial osteotomy as
described by Pappas et al.119
anterior tibial recurrent vessels, which fan out at the tubercle but retract into the anterior compartment when torn.118,175
Close monitoring is recommended for all patients with displaced tibial
tuberosity avulsion fractures. Prophylactic anterior compartment
fasciotomy should be considered at the time of open reduction when the
anterior compartment is already swollen.18
|
TABLE 23-9 Complications of Tibial Tubercle Avulsion Fracture
|
||||||
|---|---|---|---|---|---|---|
|
may be impossible without risking fracture of a tuberosity fragment.
Wiss et al.175 reported five of 15
patients with bursitis over prominent screw heads, four of whom had
6.5-mm screws. Overall, eight of the 15 patients underwent screw
removal. Fixation with small screws or use of a tension band may be an
alternative, but we recommend secure fixation even if prominent screws
may require secondary procedures for removal.
fractures in the postoperative period. Cast immobilization is
recommended to reduce this risk unless fixation is securely placed into
a large tuberosity fracture fragment. Wiss et al.175
reported one refracture in a child who returned to sports 4 weeks after
injury. In one patient, a transverse proximal tibial fracture occurred
7 months postoperatively at the level of the retained screws.18 Recovery of motion and strength is rarely problematic. Christie and Dvonch29
reported a patient with persistent loss of 25 degrees of knee flexion
19 months after a type III injury. Patella alta can be expected if a
displaced tibial tubercle is not reduced adequately. Thrombophlebitis
has also been reported.116
in adults, with estimates ranging from 1% to 6% of all patellar
fractures.92,132 Avulsion fractures of the patella are more common in children and may be difficult to diagnose.56,92
The sleeve fracture is unique to children and consists of a large
chondral fragment pulled from the ossification center with only a small
rim of bone attached (Fig. 23-29).47,65 In general, the treatment of patellar fractures in children is similar to treatment in adults.92,132
blow, sudden contraction of the extensor mechanism, or a combination of
these direct and indirect forces. The patella is primarily in tension
when the quadriceps contracts with the knee in extension. However,
flexion produces compression and three-point bending forces on the
patella with the distal femur acting as a fulcrum (Fig. 23-30). The bending moment increases with increasing knee flexion.27 Thus, a direct blow with the knee in flexion is the most common mechanism for patellar fracture.27
A typical history is that the patient fell with the knee flexed or the
knee was struck while it was in a flexed position with the quadriceps
under tension. Fractures of the patella may also occur without a direct
blow when the quadriceps forcefully contracts with the knee flexed.
This is a more likely mechanism during jumping or other sports
activities,27,37 and injury is most likely to produce a transverse, sleeve, or other avulsion fracture.27,56 Comminuted fractures are most often the result of a high-energy direct blow such as motor vehicle trauma.27,37
In a young child, the patella is more flexible and adapts to
three-point bending or compression forces without breaking. The
patellar ossification center appears between the ages of 3 to 6 years,114,115 and patellar fractures have rarely been reported in patients younger than 8 years of age.
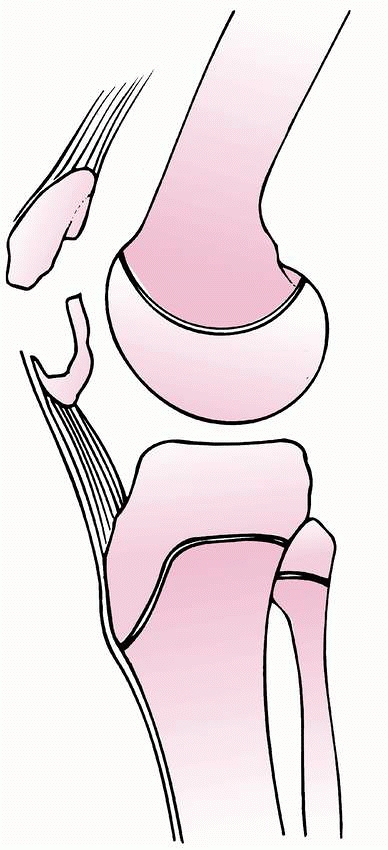 |
|
FIGURE 23-29
Sleeve fracture of the patella. A small segment of the distal pole of the patella is avulsed with a relatively large portion of the articular surface. |
avulsion of medial osteochondral fragments in association with acute
patellar dislocation.108 This injury and its treatment are discussed in Chapter 24. Stress fractures of the patella have also been reported in children, but are rare.48 Grogan et.al.56
cautioned that avulsion fractures of the inferior pole of the patella
may be confused with Sindig-Larsen-Johanssen lesion, but acute onset or
separation of the distal fragment is more likely to indicate fracture.
hemarthrosis. Active knee extension is impaired and may be painful, and
weight-bearing is often impossible. Palpation may reveal a high-riding
patella or a palpable defect in the extensor mechanism. If the distal
pole is avulsed, voluntary contraction of the quadriceps muscle draws
the patella upward, but the patellar ligament remains lax. With
marginal avulsion fractures, there may be little more than tenderness
and localized swelling over the lateral or medial margin of the
patella, and a straight-leg
raise
may be possible. An avulsion fragment adjacent to the medial margin of
the patella may indicate that an acute lateral dislocation of the
patella has occurred. The patella may have reduced spontaneously after
the injury. If dislocation has occurred, the apprehension test is
positive when the patient either resists passive manipulation by
contracting the quadriceps or may even grasp the examiner’s hand to
prevent further passive displacement. Pain at the lateral-superior
margin of the patella along with radiographic findings of a
nondisplaced fracture most likely represents a bipartite patella rather
than an acute fracture.54,115
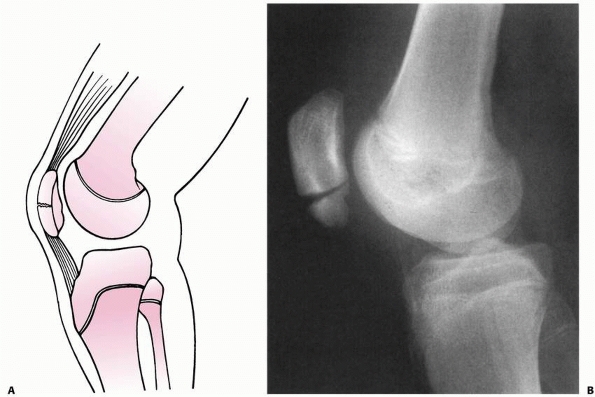 |
|
FIGURE 23-30 A.
Incomplete transverse fracture of the patella. The articular cartilage of the patella remains intact, but the fracture gaps anteriorly. B. Lateral radiograph shows incomplete transverse fracture of the patella. |
plan treatment for patellar fractures in children, but careful
attention should be paid to small flakes of bone that could represent
larger osteochondral avulsion fragments (see Fig. 23-29).9,81,170,171 When in doubt, MRI can help determine the nature and extent of injury.9
Transverse fractures are best seen on the lateral view. In a child, the
major fragments may tilt away from one another, with the maximal
separation anteriorly and minimal separation posteriorly.12
This may signify that the articular cartilage remains intact, even with
a complete fracture through the bony portion of the patella. The extent
of displacement may not be fully appreciated unless the knee is flexed
to 30 degrees when the x-ray is made.
noteworthy. A symptomatic, small, visible radiodensity on the inferior
pole of the patella may represent a Sindig-Larsen-Johanssen lesion.
Displacement is more likely to indicate an acute fracture.49,56
Fragmentation or elongation of the distal pole associated with patella
alta in a child with cerebral palsy indicates long-standing extensor
mechanism stress.
appreciated at first presentation to an emergency room. A barely
visible fleck of bone proximal to the patella may be the only x-ray
abnormality seen with a superior patellar sleeve fracture (Fig. 23-31). In an inferior patellar sleeve fracture, there may be patella alta in addition to a fleck of bone distal to the patella (Fig. 23-32).
on axial or skyline views. It is important to differentiate a medial
marginal fracture that traverses the entire thickness of the bone from
a medial tangential osteochondral fracture. CT scan may help
differentiate the two. An osteochondral fracture may include a
substantial amount of cartilage not visible on plain x-rays.
shows a crescent-shaped radiolucent line in the superolateral quadrant
of the patella and rounded margins of the accessory ossicle. If
symptoms are confusing, comparison x-rays of the opposite knee may be
helpful. A similar x-ray appearance of the contralateral patella
supports the diagnosis of bipartite patella.
associated with lateral dislocation of the patella. Comminuted
fractures are more likely to be caused by high-energy trauma with
associated fractures of the tibia, femur, or pelvis.
children is diagnosis of avulsion fractures with very small flakes of
bone
attached.
Signs and symptoms of acute traumatic injury to the knee in the
presence of a flake of bone on standard x-rays generally indicate an
avulsion injury of some type. A high-riding patella without evidence of
bony fragments suggests a sleeve fracture of the inferior patella or
tibial tubercle. A palpable defect along the extensor mechanism or
inability to actively extend the knee is consistent with a patellar
fracture. Developmental anomalies may also be confused with fractures
especially when bipartite patellae are symptomatic. Bipartite patellae
are generally tender near the proximal lateral pole, which is the most
common location of an extra ossification center. Also, bipartite
patella is generally nondisplaced and is not associated with
hemarthrosis or loss of active knee extension. Sindig-Larsen-Johanssen
lesions may also be confused with distal pole avulsion injuries, but
these are chronic repetitive injuries with point tenderness as the
principle clinical finding.49,100 Acute injuries are more likely to demonstrate swelling and slight displacement of fragments on x-rays. Rosenthal and Levine136
found fragmentation of the distal pole of the patella in seven patients
with spastic cerebral palsy involving the lower extremities. They
believed that the fragmentation represented stress fractures caused by
excessive tension in the muscle associated with a flexed-knee gait.
Three of the fragmented patellae healed after hamstring lengthening.
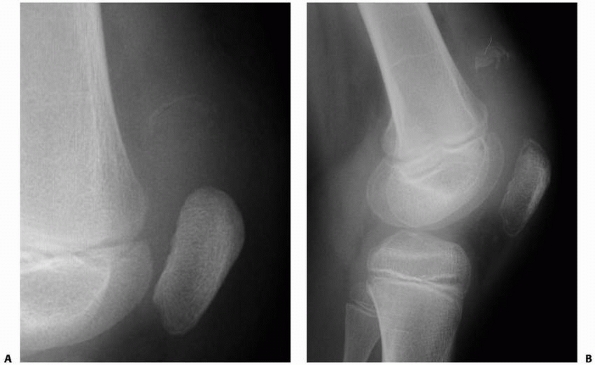 |
|
FIGURE 23-31 A.
Lateral view of a child’s knee with a superior patella sleeve fracture. The fracture was initially unrecognized at presentation. B. Two weeks later, ossification of the fracture is evident. Open reduction was necessary. |
morphology of the fracture pattern. Common categories of morphologic
classification are transverse, vertical, comminuted, osteochondral, and
sleeve.27 Grogan et al.56
classified avulsion fractures according to location of the avulsed
fragment into four categories: superior, inferior, medial, and lateral.
nondisplaced and displaced. Other classifications may help understand
the fracture mechanism and diagnostic challenges, but nondisplaced
fractures are treated nonoperatively regardless of fracture pattern,
and displaced fractures require accurate reduction and stable fixation
regardless of fracture pattern.
injury to some extent and may provide a more useful classification than
just description of the fracture morphology.27 The following classification is recommended for consideration as a combination of mechanism of injury and fracture pattern:
-
Comminuted Fractures are more likely to be caused by direct trauma.27 These are often nondisplaced, but direct trauma can produce damage to the articular contact area with poor outcomes.92
Direct impact with comminution is also more likely to be present with
open wounds or associated fractures of the femur tibia or pelvis.27,132 -
Transverse Fractures and Sleeve Fractures
are the result of a combination of tension and three-point bend. This
may occur during forceful contraction of the quadriceps with the knee
flexed or with a blow to the patella with the knee flexed during
quadriceps contraction. When the patella has a large ossification
center, a transverse fracture through bone is more likely to occur from
this mechanism; before the age of 13 years, sleeve fractures have been
reported as the most common fracture pattern.37,47,132
In this juvenile age group, the patella bends with transverse fracture
of the cartilage followed by avulsion of the cartilage from the ossific
nucleus. Thus, the outer shell is pulled off the ossification center
like
P.879the shell of a nut that is cracked transversely and pulled off the seed that remains inside the opposite half of the shell (see Figs. 23-29 and 23-32)
A small bone fragment from the ossification center remains attached to
the inside of the avulsed cartilage sleeve. The extent of injury is
often not appreciated on initial x-rays. Inferior pole avulsion is the
most common type.47,56,164,178 Superior pole avulsions are rare and more likely to be nondisplaced.56,164,178
Small traumatic fractures of the superior and inferior poles of the
patella should be distinguished from chronic repetitive stress injuries -
Medial Avulsion Fractures are associated with lateral dislocation of the patella and are discussed in Chapter 24. These are best seen on axial x-rays of the patella such as the Merchant
P.880view with the knee flexed 45 degrees and the x-ray beam angled distally
to intersect the knee at an angle of 30 degrees to the long axis of the
femur.101
Most medial avulsion fractures consist of small osteochondral
fragments, but large vertical sleeve fractures or vertical fractures of
the patella may also occur.56
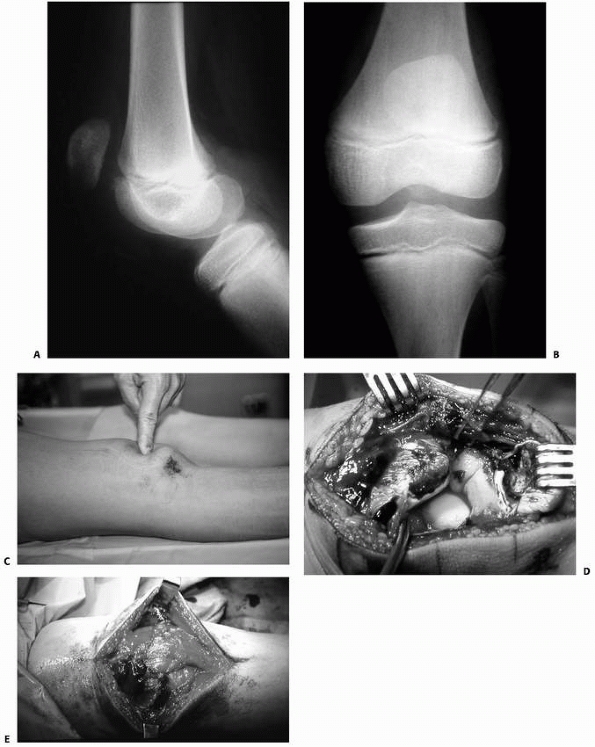 |
|
FIGURE 23-32 An inferior patella sleeve fracture. A. On lateral view, ossific fragment is difficult to appreciate. Patella alta may be noted. B. On AP view, ossific fragment can fortunately be seen within the joint space. C. On examination, defect is palpable in between the patella and patella tendon. D. Intraoperative exposure. E. Repair of transverse retinacular tears and patella sleeve fracture with sutures. (Courtesy of Robert Kay, MD.)
|
cartilage form. Ossification of the cartilaginous anlage begins between
3 and 6 years of age.114,115
Often, there is more than one central ossicle, and there may be as many
as six irregular centers. Gradually, the ossicles coalesce and
ossification proceeds peripherally until all cartilage except the
articular surface is replaced by bone. Until ossification is complete,
the edges of the enlarging ossific nucleus may appear irregular. The
pattern of bony development is similar in this respect to the growing
epiphysis of the distal femur (Fig. 23-33).
Ossification of the patella usually is complete by the beginning of the
second decade. Internal fixation of the patella at any age does not
retard growth because the patella enlarges by appositional growth
through intramembranous ossification without a discrete physis.
The overall incidence of bipartite patella in adolescents is reported
to be 2% to 15%, but that may include accessory ossification centers
instead of discrete bipartite patella in older adolescents.115
The true incidence of well-formed bipartite patella is probably much
lower than 2%. The most common location of the bipartite segment is the
superolateral pole of the patella.54,115
 |
|
FIGURE 23-33 Normal knee in a 6-year-old child. Note irregular ossification of the patella and the distal femoral condyle.
|
of the patella are uncommon. Although these variations in development
have been reported as isolated findings, they can also occur as part of
the hereditary symptom complex onycho-osteodysplasia or nail-patella
syndrome.6,19
noted differences between immature and mature specimens except for the
intraosseous arborization that occurs in the ossification center. An
anastomotic circle surrounds the patella with contributions from the
paired superior and inferior geniculate arteries, as well as the
anterior tibial recurrent artery. From the anastomotic ring, branches
converge centripetally toward the anterior surface of the patella and
enter through foramina in the middle third of this surface. Additional
blood supply to the patella enters the distal pole behind the patellar
ligament. Thus, virtually the entire blood supply to the patella comes
from the anterior surface or distal pole, with essentially no
penetration of vessels from the medial, proximal, or lateral margins of
the patella. Scapinelli141 noted
that these findings correlate with the fact that marginal fractures of
the patella are more likely to progress to nonunion. Also, injury to
blood vessels entering the anterior aspect of the patella may lead to
osteonecrosis of the proximal pole.141
Also, osteochondrosis and posttraumatic disturbance of ossification
have been reported that may indicate ischemia following trauma.105,127
fractures. Aspiration of a tense hemarthrosis may relieve pain. A
cylinder cast in extension is applied, and progressive weight-bearing
is permitted. Immobilization may be continued for 6 weeks.
fractures in children are essentially the same as for patellar
fractures in adults.37,92,132
Restoration of the extensor function and articular congruity is
essential. This requires accurate reduction and stabilization of
fracture fragments. Repair of torn retinaculum is also recommended,168 although percutaneous fixation with excellent outcomes has been reported in adults.90,156,163
An inability to actively extend the knee fully suggests major
disruption of the retinaculum and may be an indication for open repair.
nonabsorbable sutures through longitudinally drilled holes or
cannulated screws, the tension-band technique, and screws or pins
without tension band fixation. Choice of fixation is determined by the
fracture pattern. Displaced transverse fractures, including sleeve
fractures, are the most common type requiring internal fixation. An
experimental study by Weber et al.168 supported fixation by modified tension-band wiring. The method tested by Weber et al.168
consisted of a wire loop passed transversely behind the tips of two
longitudinal fixation wires and then tensioned as a longitudinal oval
over the anterior surface of the patella. The AO group popularized a
variation by crossing the tension band in a longitudinal
figure-of-eight on the anterior surface of the patella (Fig. 23-34) Carpenter et al.27 studied
several methods of fixation and determined that the strongest repair
was provided by two longitudinal cannulated screws with a tension band
wire passed through the central holes and twisted in a figure-of-eight
over the anterior surface of the patella. This forms a horizontal
figure-of-eight instead of a vertical figure-of-eight. In 2007, John et
al.75
tested different orientations of the figure-of-eight and determined
that the horizontal figure-of-eight with two twists of wire at adjacent
corners provided the greatest interfragmentary compression and
stability (Fig. 23-35). Braided wire or braided
polyester suture can also be used instead of stainless steel wire.
Absorbable suture has also been successfully used in a child.155 Fortunately, children heal rapidly
and tolerate immobilization, so the technique of wiring may not be as important in children as it is in adults.
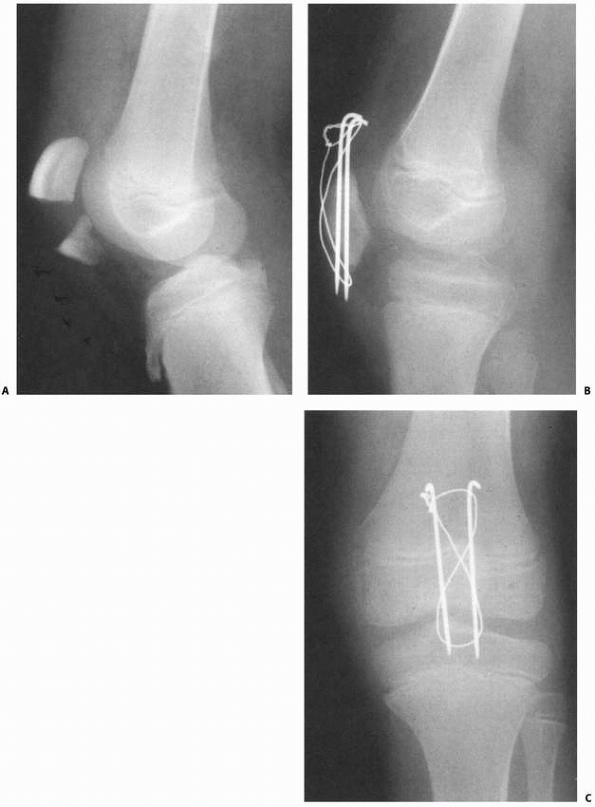 |
|
FIGURE 23-34 A. Displaced transverse fracture of the patella. B,C.
After open reduction and internal fixation with tension-band technique using figure-of-eight wire over parallel longitudinal pins. This case with steel wire was chosen to illustrate the technique. The authors prefer using heavy suture to possibly avoid the need for future hardware removal. |
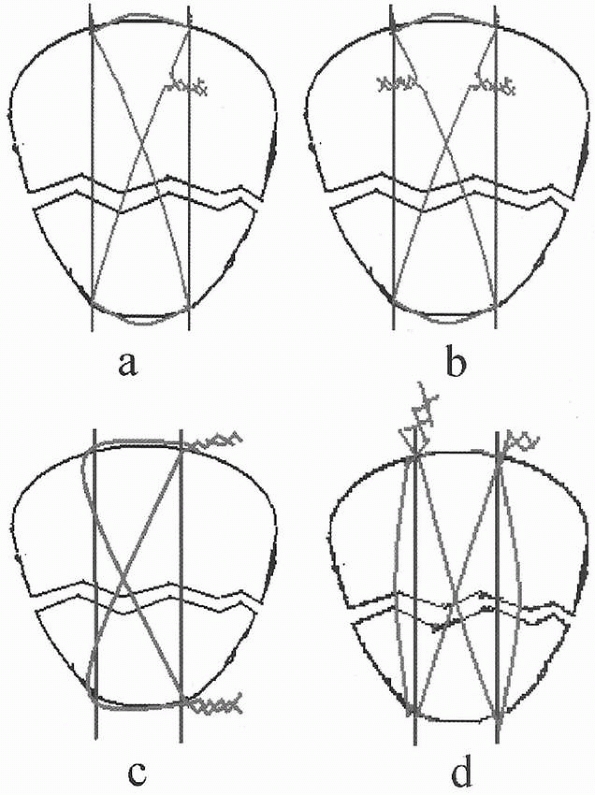 |
|
FIGURE 23-35
Four configurations of tension band loops. When stainless steel wire is used, configuration “D” provides greater interfragmentary compression and stability. A. Vertical figure-of-eight with one wire twist. B. Vertical figure-of-eight with two wire twists. C. Vertical figure-of-eight with two wire twists placed at adjacent corners. D. Horizontal figure-of-eight with two wire twists placed at adjacent corners. Method “D” can be achieved with two cannulated compression screws for added stability. (Reprinted with permission from John J, Wagner WW, and Kuiper JH. Tension-band wiring of transverse fractures of the patella. Intl Orthop 2007;31:703-707.) |
dislocation should be repaired to reduce the risk of recurrent
instability.56,134 The osteochondral fragment is either removed or repaired depending primarily on the size of the avulsed fragment.56,129
When larger than 1 cm, the fragment can usually be securely replaced
and fixed with pins, headless screws, sutures, or resorbable fixation
devices.13,56,97,129 Rorabeck and Bobechko134
advised repairing the extensor apparatus in children when osteochondral
fractures are associated with patellar dislocation. Repair was
successful with or without excision of the osteochondral fragment.134 A more detailed discussion of this injury can be found in Chapter 24.
stabilize. Comminution may produce fragments that are small or
detached. Cerclage wiring with small fragment fixation may allow
restoration of extensor function and articular congruity. Partial
patellectomy may be necessary, but total patellectomy should be avoided
if at all possible.27,37,92,132
Preservation of some of the articular surface is preferred to total
patellectomy. When partial patellectomy is necessary, the quadriceps
tendon or patellar tendon is pulled to the remnant of patella and
sutured as close as possible to the articular surface through drill
holes to minimize the step-off between the tendon and articular margin
of the patellar fragment. On the rare occasion when total patellectomy
is unavoidable, transverse closure is preferred to longitudinal closure
of the defect in the extensor mechanism.77
the patella. A long-leg cast is applied with the knee in slightly less
than full extension. Partial weight-bearing is allowed as soon as
symptoms permit, usually within the first several days.
fractures that are displaced more than 2 to 3 mm. Surgery for
transverse fractures including sleeve fractures is different from
surgery for comminuted fractures. For transverse fractures,
percutaneous fixation with arthroscopic control is an alternative, but
open reduction allows repair of any torn patellar retinaculum. We
prefer a longitudinal midline incision to facilitate possible future
surgery about the knee. Following irrigation and débridement of the
fracture, reduction is performed and evaluated. Visualization of the
articular surface should be possible through the retinacular tear. If
not, a small medial capsular incision can be made to expose the
articular surface of the patella. Then the fracture surfaces are
examined and a 2.0 or 2.5-mm Kirschner wire or guidewire is placed
through the fracture surface into the proximal or distal pole of the
patella. The wire is advanced until it is flush with the fracture
surface. Then provisional fixation is obtained with one or two bone
reduction forceps or towel clamps. The Kirschner wire or guidewire is
then advanced into the opposite fragment until it exits the pole of the
patella. The wires can be left in place for tension band wiring or
cannulated lag screws can be inserted over the guidewires. Two wires or
screws in a parallel longitudinal orientation are recommended. Final
fixation is achieved with a tension band looped around the protruding
tips of the wires proximally and distally. The loop crosses in the
middle of the patella to form a figure-of-eight. Recently, it has been
demonstrated that the horizontal configuration of the tension band wire
with two twist points provides stronger fixation and greater
compression at the fracture site (see Fig. 23-35).75
When screws are used, they should be stopped a few millimeters short of
the margin of the patella to avoid irritation or stress points on the
tension band. Lag screws with the tension band through the center holes
with two twist points is the strongest configuration for fixation of
transverse fractures.27,75
We have found that steel wire frequently causes irritation and requires
further surgery, where strong suture is less irritating and provides
sufficient fixation. In most children, due to rapid fracture healing,
we prefer internal fixation using the horizontal figure-of-eight
tension-band technique with a strong suture such as FiberWire braided
polyblend suture with Kevlar woven into it, size no. 2 (Arthrex,
Naples, FL) or size no. 2 braided polyester suture instead of wire.
When a vertical figure-of-eight is used, it is
important
to fit the transverse limbs underneath the wires and directly against
the superior and inferior poles of the patella without any interposed
soft tissue that may allow relaxation of tension in the postoperative
period. The retinaculum on both the medial and lateral sides is
repaired meticulously from outward in toward the margins of the patella.
used to gather all the fragments together. Small pins or small fragment
screws are used to approximate fragments that have soft-tissue
attachments. Devitalized or free, fragments may need to be discarded.
Every attempt should be made to avoid patellectomy, but partial
patellectomy may be necessary. When part of the patella remains, the
patellar tendon or quadriceps tendon is sutured to the remaining
portion of the patella with heavy no. 2 braided polyester sutures that
are attached to parallel drill holes placed in the bone as close as
possible to the articular surface of the remaining patella. A
figure-of-eight tension band can then be passed through the patellar
remnant and looped distally to the tibial tubercle or proximally into
the quadriceps tendon to protect the repair. This loop should not be
tightened so much that the remaining patella is displaced too far
distally or proximally.
with screws or sutures if large enough for fixation. Small fragments
are excised with repair of the retinaculum. This is described in more
detail in the next chapter.
recommended for children because stiffness is not as much of a concern
as it is in adults. Approximately 4 weeks after repair, gentle range of
motion is initiated. This is followed with strengthening exercises 6 to
8 weeks following injury and repair.
-
Late recognition of patellar sleeve
fractures is not uncommon—this diagnosis should be considered in any
patient who does not have full active extension of the knee. -
When repairing the retinaculum, all the
sutures are placed first without tying them. If the sutures are tied as
they are placed, it becomes increasingly difficult to visualize the
torn retinaculum and fracture. -
If closing the gap of the extensor mechanism is difficult:
-
The tourniquet, which may be tethering the quadriceps, can be released.
-
If the fracture is not acute, quadriceps
contraction may have occurred, in which case judicious musculotendinous
lengthening of the quadriceps complex may be needed.
-
wound complications. These may be due to the magnitude of the initial
trauma, technical deficiencies, or patient noncompliance. Repeat
fixation is recommended when secondary displacement is more than 3 to
4-mm of gap or more than 2 mm of step-off of the articular surface.
patellafemoral pain, and weakness. Fortunately, these are rare in
children when accurate reduction of the fracture is obtained and
maintained until union. Early gentle motion beginning 4 weeks after
surgery, with later strengthening exercises, can diminish the risk of
weakness or limited motion. Delayed diagnosis of sleeve fractures of
the patella is not uncommon.47,65,178
Repair with deébridement and approximation of the fracture fragments
has been reported as late as 2 months, although loss of knee flexion
may be a result.178 It is best to
avoid quadriceps lengthening at the time of repair even if knee
extension is required to approximate the fragments. Quadriceps
lengthening can be done at a later time if satisfactory flexion cannot
be achieved. Manipulation should be avoided because of the risk of
distal femoral physeal separation during manipulation under anesthesia.
E, Ansari A, Huang TL. Fracture of the distal medial femoral epiphysis
with subluxation of the knee joint. J Trauma 1980;20:339-341.
A, Warner WC Jr, Horn BD, et al. Predicting the outcome of physeal
fractures of the distal femur. J Pediatr Orthop 2007;27:703-708.
AJ, Johari AN. Epiphyseal separations after neonatal osteomyelitis and
septic arthritis. J Pediatr Orthop 2000;20:544-549.
EM, Kozlowski K. Small patella syndrome: a bone dysplasia to recognize
and differentiate from the nail-patella syndrome. Pediatr Radiol
1997;27:432-435.
A, Gaynor T, Mubarak SJ. Premature physeal closure following distal
tibia physeal fractures: a new radiographic predictor. J Pediatr Orthop
2003;23:733-739.
G, Kallieris D, Seeböck T, et al. Bioresorbable pins and screws in
paediatric traumatology. Eur J Pediatr Surg 1993;4:103-107.
JG. Surgical treatment of physeal bar resection. In: Eilert RE, ed.
Instructional Course Lectures. Rosemont: Amer Acad Orthop Surg;
1992:445-450.
EM, Van Bokhoven H, Van Thiensen MN, et al. The small patella syndrome:
description of five cases from three families and examination of
possible allelism with familial patella aplasia-hypoplasis syndrome. J
Med Genetics 2001;38:209-214.
M, Helland P, Myhre HO, et al. 11 femoral fractures with vascular
injury: good outcome with early vascular repair and internal fixation.
Acta Orthop Scand 1996;67: 161-164.
RW, Burstein AH, Elmore SM. Epiphyseal-plate cartilage. A biomechanical
and histological analysis of failure modes. J Bone Joint Surg Am
1974;56(4):688-703.
LA, Wroble RR. Salter-Harris type III fracture of the medial femoral
condyle associated with an anterior cruciate ligament tear. Report of
three cases and review of the literature. Am J Sports Med
1998;26(4):581-586.
NS, et al. Epiphyseolysis for partial growth plate arrest. Results
after four years or at maturity. J Bone Joint Surg Br 1989;71(1):13-16.
JD, Sanders RJ, Jansen BR. Ossification in the patellar tendon and
patella alta following sports injuries in children. Complications of
sleeve fractures after conservative treatment. Arch Orthop Trauma Surg
1993;112:157-158.
O, Subari M, Erdem K, et al. Treatment of vascular injuries associated
with limb fractures. Ann R Coll Surg Engl 2005;87:348-352.
SM, Batterman SC, Brighton CT. Shear strength of the human femoral
capital epiphyseal plate. J Bone Joint Surg Am 1976;58(1):94-103.
WA, Buschman WR, Rudolph CN. Irreducible fracture of the proximal
tibial physis in an adolescent. Orthop Rev 1989;18:891-893.
DA, Hinton RY. Bilateral tibial tubercle avulsion fractures associated
with Osgood-Schlatter’s disease. Am J Orthop 2008;37:92-93.
D, Letts M. Partial sleeve fractures of the tibia in children: an
unusual fracture pattern. J Pediatr Orthop 2002;22:36-40.
KA, Karunakar M, Phieffer L, et al. Early versus late reduction of a
physeal fracture in an animal model. J Pediatr Orthop 2002;22:208-211.
HB, Silva MJ, Sandell LJ, et al. Ligamentous versus physeal failure in
murine medial collateral ligament biomechanical testing. J Biomech
2005;38:703-706.
GT, Peterson HA, Berquist TH. Premature partial physeal arrest.
Diagnosis by magnetic resonance imaging in two cases. Clin Orthop Relat
Res 1991;272:242-247.
Mata S, Hidalgo Ovejero A, Martinez Grande M. Transverse stress
fracture of the patella in a child. J Pediatr Orthop 1999;8(3):208-211.
JS, McInernay VK, Avella DG, et al. Injuries to the inferior pole of
the patella in children. Orthop Rev 1990;7:643-649.
PH, Papaioannou T, Kenwright J. The influence on the spine of
leg-length discrepancy after femoral fracture. J Bone Joint Surg Br
1983;65(5):584-587.
LS, Volpon JB. Experimental physeal fracture-separations treated with
rigid internal fixation. J Bone Joint Surg Am 1993;75A:1756-1764.
E, Pérez-Ramírez A, Santolaria-Fernández F, et al. Association of
Harris lines and shorter stature with ethanol consumption during
growth. Alcohol 2007;41:511-515.
SP, Agarwal A. Concomitant double epiphyseal injuries of the tibia with
vascular compromise: a case report. J Orthop Sci 2004;9:526-528.
D, Duparc F, Beaufils P. The arterial vascularization of the lateral
tibial condyle: anatomy and surgical applications. Surg Radiol Anat
2006;28:38-40.
HA. The growth of the long bones in childhood with special reference to
certain bony striations of the metaphysis and to the role of vitamins.
Arch Int Med 1926;38: 785-806.
CC, Foster BK. Secondary tethers after physeal bar excision. a common
source of failure? Clin Orthop Relat Res 2002;405:242-249.
JP, Driessen MJ, Mulder H, et al. The triplane variant of the tibial
apophyseal fracture: a case report and review of the literature. J
Pediatr Orthop B 2003;12: 406-408.
JA. General principles for managing orthopedic injuries. In: Herring
JA, ed. Tachdjian’s Pediatric Orthopedics. Philadelphia: WB Saunders;
2002:2059-2086.
GR, Ackroyd CE. Sleeve fractures of the patella in children: a report
of three cases. J Bone Joint Surg Br 1979;61-B(2):165-168.
MT, Kasser JR. Physeal arrest about the knee associated with
non-physeal fractures in the lower extremity. J Bone Joint Surg Am
1989;71(5):698-703.
RW, Himeno S, Coventry MB, et al. Normal axial alignment of the lower
extremity and load-bearing distribution at the knee. Clin Orthop Relat
Res 1990;255:215-227.
U, Schlicht W, Outzen S, et al. Ultrasound in the diagnosis of
fractures in children. J Bone Joint Surg Br 2000;82:1170-113.
B, Raquillet C, Morel E, et al. Long-term prognosis of Salter-Harris
type 2 injuries of the distal femoral physis. J Pediatr Orthop B
2006;15:433-438.
PM, Wikstrom B, Hirsch G. The influence of transphyseal drilling and
tendon grafting on bone growth: an experimental study in the rabbit. J
Pediatr Orthop 1998; 18(2):149-154.
GJ, Kummer FJ, Gibber MJ, et al. A mechanical evaluation of two
fixation methods using cancellous screws for coronal fractures of the
lateral condyle of the distal femur (OTA type 33B). J Orthop Trauma
2006;20:273-276.
J, Wagner WW, Kuiper JH. Tension-band wiring of transverse fractures of
patella. The effect of site of wire twists and orientation of stainless
steel wire loop: a biomechanical investigation. Intl Orthop
2007;31:703-707.
K, Matsuda T, Mogami A, et al. Type III fracture of the tibial tubercle
with avulsion of the tibialis anterior muscle in the adolescent male
athlete. Injury 2004;35: 919-921.
YS, Jung YB, Ahn JH, et al. Arthroscopic assisted reduction and
internal fixation of lateral femoral epiphyseal injury in an adolescent
soccer player: report of one case. Knee Surg Sports Traumatol Arthrosc
2007;15:744-746.
SL, Pozo JL, Muirhead-Allwood WFG. Coronal fractures of the lateral
femoral condyle. J Bone Joint Surg Br 1989;71(1):118-120.
L, Bass R, Connolly JF. Stereological study of the developing distal
femoral growth plate. J Orthop Res 1989;7:868-875.
RT, Swinford A, Kuhns L. The use of helical computed tomographic scan
to assess bony physeal bridges. J Pediatr Orthop 1977;17:356-359.
SJ, Harvey JP Jr. Fractures of the distal femoral epiphyses. Factors
influencing prognosis: a review of thirty-four cases. J Bone Joint Surg
Am 1977;59(6):742-51.
D, Amato D, Arellano F, et al. Comparison of a technique using a new
percutaneous osteosynthesis device with conventional open surgery for
displaced patella fractures in a randomized controlled trial. J Orthop
Trauma 2006;20:529-535.
J, Grewal R. Avulsion of the tibial tuberosity: muscles too strong for
a growth plate. Clin J Sports Med 1997;7:129-133.
EA, Vainionpää S, Vihtonen K, et al. The effect of trauma to the lower
femoral epiphyseal plate. An experimental study in rabbits. J Bone
Joint Surg Br 1988;70(2): 187-191.
HH, Puppala G, Knuth A. Neonatal distal femoral physeal fracture
requiring closed reduction and pinning. J Perinatol 2005;25:216-219.
GV, Hui PW, Cheng JC. Translation of the radius as a predictor of
outcome in distal radial fractures of children. J Bone Joint Surg Br
1993;75(5):808-811.
DC, Rajmaira S. Distribution of physeal and nonphyseal fractures in
2,650 longbone fractures in children aged 0-16 years. J Pediatr
Orthop1990;10(6):713-716.
Y, Nakamura T, Suzuki R, et al. Biodegradable pin fixation of
osteochondral fragments of the knee. Clin Orthop Relat Res
1996;322:166-173.
RC, Gilley JS, DeLee JC. Salter-Harris Type III fractures of the medial
distal femoral physis—a fracture pattern related to the closure of the
growth plate: report of 3 cases and discussion of pathogenesis. Am J
Sports Med 2008;36:572-576.
RC, Lyne ED. Sinding-Larsen-Johansson disease. Its etiology and natural
history. J Bone Joint Surg Am 1978;60(8):1113-1116.
AC, Mercer RL, Jacobsen RH, et al. Roentgenographic analysis of
patellofemoral congruence. J Bone Joint Surg Am 1974;56(7):1391-1396.
RA, Calvo RD, Sterling JC, et al. Delayed treatment of a malreduced
distal femoral epiphyseal plate fracture. Med Sci Sports Exerc
1992;24:1311-1315.
E. Strength and morphology of growth cartilage under hormonal influence
of puberty. Reconstr Surg Traumatol 1978;10:3-104.
HH, Celebil L, Hapa O, et al. Bilateral patellar tendon rupture in a
child: a case report. Knee Surg Sports Traumatol Arthrosc
2005;13:677-682.
JA, González-López JL, López-Valverde S, et al. Premature physeal
closure after tibial diaphyseal fractures in adolescents. J Pediatr
Orthop 2000;20:193-196.
Y, Aalto K, Kallio PE. Acute patellar dislocation in children:
incidence and associated osteochondral fractures. J Pediatr Orthop
1994;14:513-515.
PA, Babis GC, Triantafillopolos IK, et al. Avulsion fractures of the
tibial tuberosity in adolescent athletes treated by internal fixation
and tension band wiring. Knee Surg Sports Traumatol Arthrosc
2004;12:271-276.
SE, Segina DN, Aflatoon K, et al. The association between
supracondylarintercondylar distal femoral fractures and coronal plane
fractures. J Bone Joint Surg Am 2005;87(3):564-569.
H, Turanli S, Baltaci G, et al. Avulsion of the tibial tuberosity with
a lateral plateau rim fracture. Knee Surg Sports Traumatol Arthrosc
2002;10:310-312.
JM, Goulet JA, Hensinger RN. Compartment syndrome complicating tibial
tubercle avulsion. Clin Orthop Relat Res 1993;295:201-204.
AM, Anas P, Toczylowski HM. Asymmetrical arrest of the proximal tibial
physis and genu recurvatum deformity. J Bone Joint Surg Am
1984;66(4):575-581.
SK, Lee FY, Behrens FF. Coronal split fracture of the proximal tibial
epiphysis through a partially closed physis: a new fracture pattern. J
Pediatr Orthop 2001;21: 451-455.
HA, Madhok R, Benson JT, et al. Physeal fractures: Part 1. Epidemiology
in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop 1994;14(4):
423-430.
M, Weber E, Stauffer UG. Interposition of periosteum in joint fractures
in adolescents; comparison of operative and conservative treatment
[article in German]. Z Kinderchir 1981;33:84-88.
LS, Meyer RA Jr, Gruber HE, et al. Effect of interposed periosteum in
an animal physeal fracture model. Clin Orthop Relat Res 2000;376:15-25.
H, Gul O, Boya H, et al. Osteochondrosis of the primary ossification
center of the patella (Kohler’s disease of the patella). Report of
three cases. Knee Surg Sports Traumatol Arthrosc 2002;10:141-143.
M, Velkes S, Levy O, et al. Suture fixation of osteochondral fractures
of the patella. J Bone Joint Surg Br 1995;77(1):154-155.
A, Kumar A, Shah SV. Salter-Harris type III fracture of the lateral
femoral condyle with a ruptured posterior cruciate ligament: an
uncommon injury pattern. Arch Orthop Trauma Surg 2007;127:29-31.
M, Wenger DR. The physis and skeletal injury. In: Wenger DR, Pring ME,
eds. Rang’s Children’s Fractures. Philadelphia: Lippincott Williams
& Wilkins; 2005: 11-25.
JM, Hendrix J. Incidence, mechanism of injury, and treatment of
fractures of the patella in children. J Trauma 1992;32:464-467.
EJ, Barrett IR, Shapiro F. Growth disturbances following distal femoral
physeal fracture-separations. J Bone Joint Surg Am 1983;65(7):885-893.
ZS, Kwelblum M, Cheung YY, et al. Osgood-Schlatter lesion: fracture or
tendinitis? Scintigraphic, CT, and MR Imaging features. Radiol
1992;185:853-858.
R, Levine DB. Fragmentation of the distal pole of the patella in
spastic cerebral palsy. J Bone Joint Surg Am 1977;59(7):934-939.
S, Henry P, Behrens F. Two cases of missed Salter-Harris III coronal
plane fracture of the lateral femoral condyle. Am J Orthop
2008;37:100-103.
S, Zhao C, McKeon JJ, et al. Computed radiographic measurement of
limb-length discrepancy. Full-length standing anteroposterior
radiograph compared with scanogram. J Bone Joint Surg Am
2006;88(10):2243-2251.
R. Blood supply of the human patella: its relation to ischaemic
necrosis after fracture. J Bone Joint Surg Br 1967;49(3):563-570.
NK, Rafailidis D, Traios S, et al. Avulsion fractures of the lateral
tibial condyle in children. Injury 2006;37:57-60.
WR, Canale ST. Fractures of the tibia through the proximal tibial
epiphyseal cartilage. J Bone Joint Surg Am 1979;61(2):167-173.
R, Lippiello L, Connolly JF. Uncertain effect of indomethacin on
physeal growth injury. Experiments in rabbits. Acta Orthop Scand
1988;59:46-49.
PT, Staheli LT. Periarticular fractures after manipulation for knee
contractures in children. J Pediatr Orthop 1995;15:288-291.
JF, Benfanti PL, McGuigan JJ, et al. Distal femoral physeal fractures
and peroneal palsy: outcome and review of the literature. Am J Orthop
2007;36:E43-45.
CL, Harvell JC, Fu F. Observations on acute knee hemarthrosis in
children and adolescents. J Pediatr Orthop 1993;13(4):506-510.
SW, Templeton PA, Oxborrow NJ. Internal fixation of a patella fracture
using an absorbable suture. J Orthop Trauma 2002;16:272-273.
RN, Demirors H, Tuncay CI, et al. Arthroscopic-assisted percutaneous
screw fixation of select patellar fractures. Arthroscopy
2002;18:156-162.
FP, Wells L. Popliteal artery transection complicating a non-displaced
proximal tibial epiphyseal fracture. Orthopedics 2007;30:876-7.
JS, Pavlov H, Morris VB. Salter-Harris type-III fracture of the medial
femoral condyle occurring in the adolescent athlete. J Bone Joint Surg
Am 1981;63(4):586-591.
A, Gunal I, Acar S, et al. Arthroscopic-assisted percutaneous
stabilization of patellar fractures. Clin Orthop Relat Res
2001;389:57-61.
JM, Gruber HE, Phieffer LS. Physeal Fractures, part I: histologic
features of bone, cartilage, and bar formation in a small animal model.
J Pediatr Orthop 2002; 22:703-709.
MJ, Janecki CJ, McLeod P, et al. Efficacy of various forms of fixation
of transverse fractures of the patella. J Bone Joint Surg Am
1980;62(2):215-220.
LM, Scholz S, Rusch M. Characteristic patterns and management of
intra-articular knee lesions in different pediatric age groups. J
Pediatr Orthop 2001;21:14-19.
LM, Scholz S, Rusch M, et al. Hemarthrosis after trauma to the
pediatric knee joint: what is the value of magnetic resonance imaging
in the diagnostic algorithm? J Pediatr Orthop 2001;21:338-342.
R, Menelaus M. A simple calculation for the timing of epiphysial
arrest: a further report. J Bone Joint Surg Br 1981;63B:117-119.
RV, Staheli LT. Partial physeal growth arrest: treatment by bridge
resection and fat interposition. J Pediatric Orthop 1990;10(6):769-776.
KB, Bradley JP, Ward WT. Pes anserinus interposition in a proximal
tibial physeal fracture. Clin Orthop Relat Res 1991;264:239-242.
M, Sukthankar A, Exner GU. Tripartite patella: late appearance of a
third ossification center in childhood. J Pediatr Orthop B
2006;15:75-76.
