The Surgical Management of Intraarticular Fractures of the Distal Humerus
well-deserved reputation of being very difficult to manage, with a poor
prognosis. Nonetheless, techniques that afford rigid fixation have
improved the overall results of the management of this difficult
fracture.
designed for stable fixation have improved that most intraarticular
fractures of the distal humerus are best treated by open reduction and
internal fixation. Operative reduction affords the opportunity to
accurately reduce the disrupted trochlea and restore its congruous
relationship to the olecranon, thereby ensuring the intrinsic stability
of the humeral/ulnar relationship (1,2,3,4,5,6,7,8,10).
Even the more complex distal humeral fractures such as those associated
with comminution, open fractures, or ipsilateral fractures of the limb
are now equally effectively treated by surgical means.
distal humerus can prove treacherous as the fragile articulations are
supported by a meager amount of subchondral bone and virtually no soft
tissue. When faced with such a fracture in the elderly, the ability of
the bone to support stable fixation with screws and plates proves to be
problematic. In such cases, the surgeon must determine his or her
ability to provide stable fixation or consider alternative treatment
such as total elbow arthroplasty.
carefully considered preoperatively. Because of the complex
architecture of the distal humerus, routine radiographs will often fail
to provide the true extent of the intraarticular fracture. An
anteroposterior (AP)
radiograph
obtained with traction on the forearm once anesthesia has been induced
will reveal a more accurate representation of the fracture anatomy.
Although standard CT scanning or MRI evaluations are of questionable
value, the three-dimensional CT reconstructions have added
substantially to the preoperative understanding of some comminuted
distal intraarticular fractures (Fig. 4-1).
Severe comminution of the supracondylar columns should alert the
surgeon to the availability of a bone graft and, in the elderly
patient, the possible need for total elbow arthroplasty.
 |
|
Figure 4-1. A low comminuted distal humerus fracture is accurately depicted in a three-dimensional CT reconstruction.
|
cases general endotracheal anesthesia is preferred. The patient is
placed in the lateral position with the involved limb supported over
bolsters, keeping it off the chest wall (Fig. 4-2).
A prone position with the arm over the side of the table is an
effective means of helping to release the fracture. Either position
permits ready access to the iliac crest for autogenous bone graft. A
sterile pneumatic arm tourniquet offers the possibility of a wider
sterile field and the ability to reapply the tourniquet as needed.
approach, particularly for comminuted fractures. Through a straight,
longitudinal skin incision (Fig. 4-3), the osteotomy is made in a shallow V or chevron fashion in the center of the olecranon sulcus (Fig. 4-4).
This area has in fact the smallest zone of articular cartilage in the
olecranon. The location will be best identified by elevation of the
anconeus muscle off the olecranon to directly visualize the articular
surface. A sponge is placed from lateral to medial and used as a
countertraction, as the osteotomy is created with a thin-bladed
oscillating saw (Fig. 4-5) and completed with a thin-bladed osteotome.
 |
|
Figure 4-2. The patient is placed in the lateral position. A sterile pneumatic tourniquet is preferred.
|
 |
|
Figure 4-3. A straight longitudinal skin incision is used.
|
 |
|
Figure 4-4. A: The olecranon osteotomy is marked out in the shape of a shallow V or chevron. (Abbreviation: CET, common extensor tendon.) B: The anconeus muscle is elevated off the lateral aspect to permit a sponge to be placed as countertraction.
|
 |
|
Figure 4-5. A,B: A thin-bladed oscillating saw is used to start the osteotomy.
|
should be exposed. The fascia over the flexor carpi ulnaris is
longitudinally split over 6 cm to enhance the nerve’s mobility. In
doing this there is less chance for the nerve to become surrounded by
fibrosis in the cubital tunnel.
proximally, leaving a margin of triceps tendon on either side to suture
upon completion of the surgery (Fig. 4-6). The
exact nature of the intraarticular fracture pattern may reveal itself
only at this juncture. The fracture hematoma should be cautiously
removed using a small dental pick or pulsed lavage, as the articular
fragments may lack soft tissue or bony attachments.
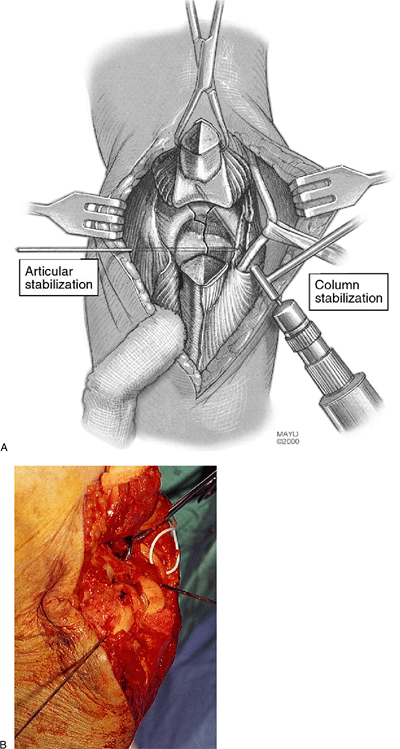
reduce the articular fragments onto the bony columns of the distal
humerus, initially holding the reduction with provisional Kirschner
wire fixation (Fig. 4-7).
trochlea may be found to be present in both the sagittal and coronal
planes (Fig. 4-8). In these cases, the Herbert screws have been of particular use, as the threads can be buried under the articular surface (Fig. 4-9).
An alternative to the Herbert screw is the fine-threaded Kirschner
wires. If a defect exists in the subchondral bone, one should plan to
support the articular fragment with autogenous cancellous bone graft.
 |
|
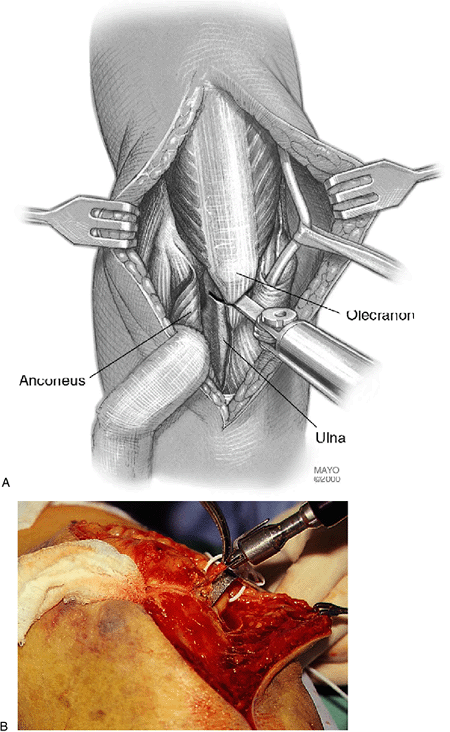
Figure 4-6. A,B:
The osteotomized proximal olecranon fragment is elevated proximally. Note the ulnar nerve has been isolated and mobilized and protected with the rubber loop. |
 |
|
Figure 4-7. A,B: The fracture is reduced and provisionally secured with Kirschner wires.
|
 |
|
Figure 4-8. Intraarticular fractures of the trochlea occurring in the coronal plane are especially difficult to secure.
|
 |
|
Figure 4-9. Reduced and fixed fracture in the AP (A) and lateral (B) projection. The Herbert screw may be used for articular fragments.
|
begins with interfragmentary screw fixation of the sagittal fracture of
the trochlea. One or two 3.5-mm cortical or 4.0-mm cancellous screws
will be sufficient to provide a firm hold of the fragments. In those
cases in which comminution is present in the sagittal plane, these
screws should not be placed as interfragmentary screws; rather, they
should be placed without “overdrilling” the near cortex to prevent
overcompressing the fragments, which will tend to narrow the trochlea,
thus threatening the intrinsic stability of the trochlea/olecranon
relationship (Fig. 4-10). With certain fracture
patterns the surgeon may find that the articular reconstruction may be
facilitated by securing one of the articular components directly to one
of the bony columns of the distal humerus. This would be followed by
restoration of the remaining articular element to this stable skeletal
and articular unit.
 |
|
Figure 4-10. When intraarticular comminution exists, a full-threaded, not a lag, screw is best placed without compressing the fragments.
|
either the tip or the head of the screws in the cubital tunnel. In such
cases, the ulnar nerve is best further mobilized by releasing the
distal part of the medial intermuscular septum to allow the nerve to
sit more freely in the subcutaneous tissues.
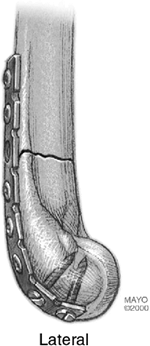
humeral bony columns is preferentially accomplished with strategically
placed plates. Mechanical strength will be enhanced by placing the
plates and respective screws as close to 90 degrees to each other as
possible. For most T or Y fractures that split the bony columns of the
distal humerus well proximal to the olecranon fossa, the plates can be
applied to the medial ridge of the medial column and along the
posterior aspect of the lateral column. The topographical anatomy of
the distal humerus is most amenable to this, as the articular cartilage
of the capitellum does not extend onto the posterior part of the distal
humerus (Fig. 4-11).
in the very distal part of the bony columns below the level of the
medial epicondyle. In such cases a plate applied along the ridge of the
medial bony column would be ineffective in supporting the articular
fragments. In these cases, several options exist for the surgeon. Using
3.5-mm reconstruction plates, the plate can be contoured to bend around
and “cradle” the medial epicondyle (Fig. 4-12).
The very distal screws can be directed into the medial epicondyle and
angulated from each other to afford an “interlocking” relationship
between the screws. An alternative to this is to direct the distal
screw proximally to secure fixation into the lateral column (Fig. 4-13).
This would require elevation of the origin of the brachioradialis and
wrist extensor muscles, which can be sutured back into place. This
placement provides an opportunity to gain a further hold on the
trochlea fragments through a screw placed transversely from the most
distal screw hole into the trochlea (Fig. 4-15). Defects beneath the plate should be reconstructed with autogenous iliac crest graft.
of motion in order to visually control the stability of the internal
fixation. If motion of the fracture fragments is observed,
it would be best to revise or alter the fixation at this point using the alternative plate application described earlier.
 |
|
Figure 4-11.
The plate on the lateral bony column can extend distally, as the articular cartilage of the capitellum does not extend posteriorly. |
 |
|
Figure 4-12.
With complex “low” fractures, a plate can be constructed to bend around the medial epicondyle with screws directed into the medial epicondyle from different directions providing an “interlock” between the screws. |
 |
|
Figure 4-13.
An alternative with the contoured plate bent around the medial epicondyle is to pass a screw through the plate and into the lateral column. |
 |
|
Figure 4-14. A,B:
Another option is to place three plates with one along the lateral column, one posterior on the lateral column, and one bent around the medial epicondyle. |
 |
|
Figure 4-15. A transverse screw is placed through the lateral plate and across the trochlear fracture fragments.
|
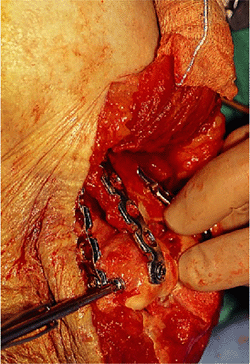
My preference for internal fixation continues to be tension band wires
with two obliquely placed Kirschner wires providing rotational control (Fig. 4-16).
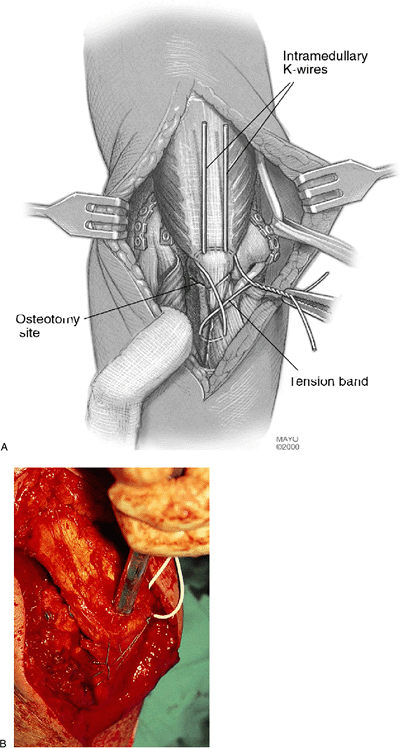
Care is taken to bend the proximal ends of the Kirschner wires and seat
them onto the proximal olecranon both to prevent proximal migration and
to avoid the prominence of the wire interfering with full elbow motion (Fig. 4-17).
At the completion of the fixation the elbow is again put through a
range of motion to test the security of the internal fixation.
 |
|
Figure 4-16. A,B: The olecranon osteotomy is secured with oblique Kirschner wires and a tension band wire.
|
 |
|
Figure 4-17. A,B:
Attention should be paid to tapping the bent ends of the Kirschner wires into the proximal olecranon to diminish local discomfort. |
secured. Over a large suction drain the wound is closed in layers. A
bulky dressing using Dacron batting is applied and a resting splint of
plaster is applied to the elbow in full extension. A resting splint for
nighttime use only with the elbow in extension helps to lessen the
problem with flexion contracture.
to the operative approach to the distal humerus: inadequate exposure,
ulnar nerve mobilization, unrecognized articular comminution, fractures
of the bony columns just above the articular surfaces, and stable plate
fixation.
specific aspects of the exposure and procedure: extensile exposure
through olecranon osteotomy, wide mobilization of the ulnar nerve,
careful identification and provisional fixation of the articular
fragments, custom placement of plates distal on the posterior aspect of
the lateral bony column and bent around the medial epicondyle, direct
screws into the cortical bone of the bony columns, and careful fixation
of the olecranon osteotomy. Adherence to these concepts makes the
difference between a successful and an unsuccessful procedure.
elderly patient who is not active might be better treated with a
primary total elbow arthroplasty (9) (see Chapter 18).
day. The patient is instructed to lie supine and forward-flex the
involved shoulder to bring the elbow overhead. With the uninjured arm
supporting the involved forearm, gravity is used to assist elbow
flexion. A similar approach is used for elbow extension exercises, but
in this case the patient sits upright and gently assists the forearm
into extension (Fig. 4-18).
are continued throughout the first 3 to 4 weeks. A splint is applied
only for the first few weeks and only during sleep with the elbow
extended. Radiographs should be obtained frequently to assess the
stability of the internal fixation. It is imperative that the surgeon
monitor the patient and coordinate the rehabilitation process. A
trained physical therapist can be helpful to similarly serve as a
monitor, but passive activities and resisted exercises are to be
avoided.
progressing satisfactorily, the patient may begin light resisted
exercises to restore muscle tone and strength.
 |
|
Figure 4-18.
Postoperatively, active motion is begun by the patient under the guidance of a physical therapist. Gravity is used to assist elbow flexion and extension. |
greatest influence on outcome. However, the ability to apply the
principles of rigid fixation and early motion also will influence the
final result. Most activities of daily living can be performed with a
range of motion from 30 to 130 degrees. Loss of full extension is more
easily compensated for than is loss of flexion. Typically, pronation
and supination are unaffected by this fracture. With current techniques
approximately 80% can attain an adequate arc of flexion even after
severe fractures (1,2,3,4,5,6,7,8).
fracture union. This reality influences the editor (BFM) to favor
replacement in the older patient with severe comminution. Muscle
strengthening and endurance form the basis of a supervised exercise
program. Typically, lack of full extension exists, and I often treat
this with dynamic and/or static types of splints. Once fracture union
has been assured, passive therapy modalities can be initiated.
results from a lack of secure fixation of the implants at the time of
surgery. Clinically, fixation instability is heralded by pain and
limited motion, and ultimately is confirmed by radiographic
documentation of implant loosening or breakage. If suspected within the
initial 6 weeks, consideration for reoperation or referral to an
individual or center with extensive experience is appropriate. Cast
immobilization is appealing to many but all too often results in an
extremely limited range of motion.
approach to these fractures becomes more widely accepted. Management is
difficult and includes rigid fixation with two or even three plates,
decompression of the ulnar nerve, and release of the anterior capsule.
When this occurs in the older patient, the disability may be profound.
In this patient, Morrey has reported reliable salvage with joint
replacement arthroplasty (9).
patients and has been associated with a variety of methods of
techniques of internal fixation. This is in part the consequence of the
osteotomy having “smooth” fracture planes, thus being intrinsically
unstable. The use of a chevron-shaped osteotomy should minimize this
problem.
with open fractures, can prove catastrophic. If infection is suspected,
extensive wound debridement, lavage, and parenteral antibiotics are to
be instituted immediately. If the internal fixation is stable and the
infection is being actively managed, it is advisable to retain the
fixation, as fracture union can take place even in the face of active
infection.
prevented or minimized by mobilizing the nerve proximally and distally
at the time of surgery. If seen postoperatively and not responsive to
rest and corticosteroid injection, early exploration can offset the
profound disability that may be associated with a progressive motor
deficit associated with ongoing ulnar nerve ischemia.
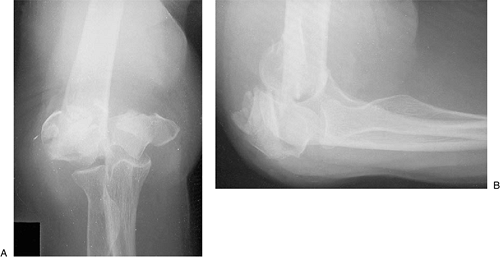
left nondominant upper extremity. Radiographs revealed a complex,
multifragmented intraarticular fracture of the distal humerus.
Anteroposterior and lateral radiographs reveal a low multifragmented
intraarticular
fracture of the distal humerus (Fig. 4-19).
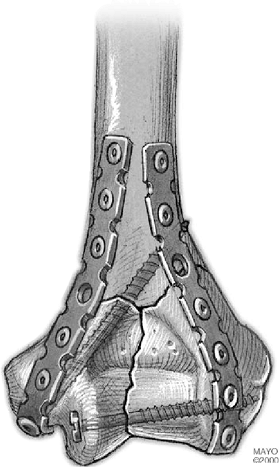
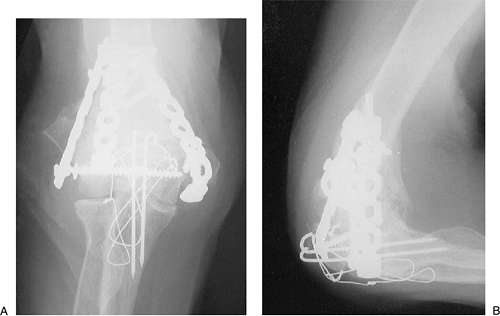
Through an olecranon osteotomy the articular surface was reduced and
secured back onto the bony columns of the distal humerus with three
strategically placed plates. Autogenous iliac crest bone graft was used
(Fig. 4-20). The comminuted extraarticular
fragments were secured under the plates with attention taken to
preserve soft-tissue attachments. Anteroposterior and lateral
radiographs demonstrate bony union along with maintenance of the
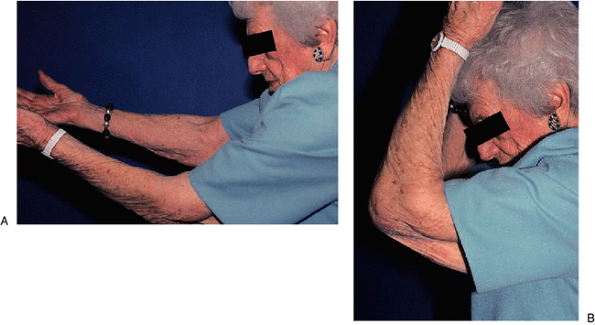
articular anatomy (Fig. 4-21). The patient was able to return to functional activities within 6 weeks following surgery (Fig. 4-22). She recovered 110 degrees of elbow flexion and lacked 40 degrees of elbow extension.
 |
|
Figure 4-19. Comminuted Y condylar fracture in elderly female seen on AP (A) and lateral projections (B).
|
 |
|
Figure 4-20. Three plates were employed to stabilize fracture distally. The comminution was treated by autogenous iliac bone graft.
|
 |
|
Figure 4-21. Near anatomic restoration is seen on the AP (A) and lateral projections (B).
|
 |
|
Figure 4-22. A useful arc of motion from 50 degrees (A) to 105 degrees (B) was obtained.
|
