The Spinal Accessory Nerve
nerve, cranial nerve XI (CN XI), is actually two nerves that run
together in a common bundle for a short distance. The smaller cranial
portion is a special visceral efferent accessory to the vagus. The
cranial root exits through the jugular foramen separately from the
spinal portion then blends with the vagus. It is distributed
principally with the recurrent laryngeal nerve. The major part of CN XI
is the spinal portion. The fibers of the spinal root arise from motor
cells in the SA nuclei in the ventral horn from C2 to C5, or even C6.
Its axons emerge as a series of rootlets laterally between the anterior
and posterior roots. These unite into a single trunk which ascends
between the denticulate ligaments and the posterior roots. The nerve
enters the skull through the foramen magnum, ascends the clivus for a
short distance, then curves laterally. The spinal root joins the
cranial root for a short distance, probably receiving one or two
filaments from it. It exits through the jugular foramen in company with
CNs IX and X.
lower portion of the precentral gyrus. Fibers from the lateral
corticospinal tract in the cervical spinal cord communicate with the SA
nucleus. There is some controversy, but the bulk of current evidence
indicates that both the sternocleidomastoid (SCM) and trapezius receive
bilateral supranuclear innervation, but the input to the SCM motor
neuron pool is predominantly ipsilateral and that to the trapezius
motor neuron pool is predominantly contralateral. The SCM turns the
head to the opposite side, and its supranuclear innervation is
ipsilateral; therefore the right cerebral hemisphere turns the head to
the left.
distinguished from those of CN X, and examination is limited to
evaluation of the functions of the spinal portion. One SCM acts to turn
the head to the opposite side or to tilt it to the same side. Acting
together, the SCMs thrust the head forward and flex the neck. The
muscles should be inspected and palpated to determine their tone and
volume. The contours are distinct even at rest. With a nuclear or
infranuclear lesion there may be atrophy or fasciculations.
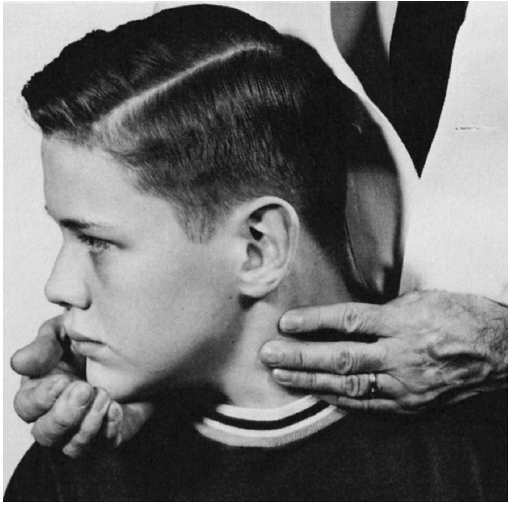
fully to one side and hold it there, then try to turn the head back to
midline, avoiding any tilting or leaning motion. The muscle usually
stands out well, and its contraction can be seen and felt (Figure 15.1).
Unilateral SCM paresis causes little change in the resting position of
the head. Even with complete paralysis, other cervical muscles can
perform some degree of rotation and flexion; only occasionally is there
a noticeable head turn.
 |
|
FIGURE 15.1
• Examination of the sternocleidomastoid muscle. When the patient turns his head to the right against resistance, the contracting muscle can be seen and palpated. |
there is diminished but not absent neck rotation, and the head may
droop or even fall backward or forward, depending upon whether the SCMs
or the trapezei are more involved. The two SCM muscles can be examined
simultaneously by having the patient flex his neck while the examiner
exerts pressure on the forehead, or by having the patient turn the head
from side to side. Flexion of the head against resistance may cause
deviation of the head toward the paralyzed side. With unilateral
paralysis, the involved muscle is flat and does not contract or become
tense when attempting to turn the head contralaterally or to flex the
neck against resistance. Weakness of both SCMs causes difficulty in
anteroflexion of the neck, and the head may assume an extended position.
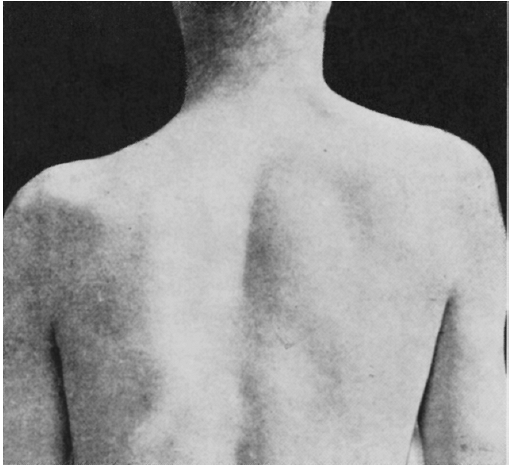
with depression or drooping of the shoulder contour and flattening of
the trapezius ridge (Figure 15.2). Severe
trapezius weakness causes sagging of the shoulder, and the resting
position of the scapula shifts downward. The upper portion of the
scapula tends to fall laterally, while the inferior angle moves inward.
This scapular rotation and displacement are more obvious with arm
abduction.
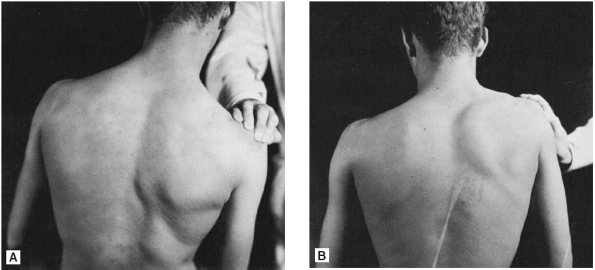
However, much of shoulder shrugging is due to the action of the levator
scapulae. A better test of the upper trapezius is resisting the
patient’s attempt to approximate the occiput to the acromion. The
movement may be observed and the contraction seen and palpated. To
examine the middle and lower trapezius, place the patient’s abducted
arm horizontally, palm up, and attempt to push the elbow forward.
Muscle power should be compared on the two sides. In unilateral
weakness of the trapezius these movements are impaired.
stabilize the scapula and create a platform for movements of the
humerus. The serratus anterior protracts the scapula, moving it forward
as in a boxing jab. The trapezius is a synergist to the main mover, the
rhomboids, in retracting the scapula. The trapezius and serratus
anterior act in concert to rotate the scapula when the arm is
abducting. The trapezius brings the glenoid fossa progressively more
cephalad so that the abduction motion is unrestricted. In addition,
contraction of the upper trapezius adds the final few degrees
of
abduction, after the glenohumeral and acromioclavicular ranges of
motion are exhausted, so that the arm can be brought directly overhead.
 |
|
FIGURE 15.2
• Paralysis of the left trapezius muscle. There is a depression in the shoulder contour with downward and lateral displacement of the scapula. |
scapulohumeral rhythm and impairs arm abduction. Impairment of upper
trapezius function causes weakness of abduction beyond 90 degrees.
Weakness of the middle trapezius muscle causes winging of the scapula.
The winging due to trapezius weakness is more apparent on lateral
abduction in contrast to the winging seen with serratus anterior
weakness, which is greatest with the arm held in front. In fact, with
winging due to trapezius weakness, the jutting of the inferior angle
lessens when the arm is raised anteriorly; in winging due to serratus
anterior weakness, it worsens. Scapular winging is discussed further in
Chapter 18. When the trapezius is weak, the arm
hangs lower on the affected side, and the fingertips touch the thigh at
a lower level than on the normal side. Placing the palms together with
the arms extended anteriorly and slightly below horizontal shows the
fingers on the affected side extending beyond those of the normal side.
The two trapezius muscles can be examined simultaneously by having the
patient extend his neck against resistance. Bilateral paralysis causes
weakness of neck extension. The patient cannot raise his chin, and the
head may tend to fall forward (dropped head syndrome).
 |
|
FIGURE 15.3 • Examination of the trapezius muscle. A. Examiner pressing shoulder down against patient’s resistance. B. Patient attempting to elevate shoulder against examiner’s resistance.
|
 |
|
FIGURE 15.4 • Two examples (A and B) of cervical dystonia (spasmodic torticollis).
|
 |
|
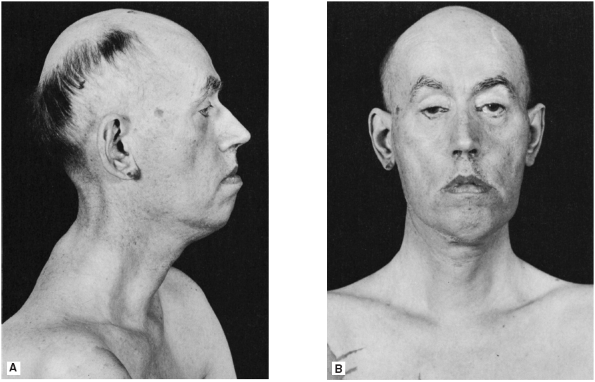
FIGURE 15.5 • A patient with myotonic dystrophy. There is atrophy of the sternocleidomastoid muscles.
|
by supranuclear, nuclear, or infranuclear lesions. Supranuclear
involvement usually causes at worst moderate loss of function since
innervation is partially bilateral. In hemiplegia there is usually no
head deviation, but testing may reveal slight, rarely marked, weakness
of the SCM, with difficulty turning the face toward the involved limbs.
There may be depression of the shoulder resulting from trapezius
weakness on the affected side. Abnormal involuntary movements of the
head and neck are seen in certain movement disorders. The SCM and
trapezius are frequently involved in cervical dystonia, a common focal
dystonia causing torticollis, anterocollis, or retrocollis (Figure 15.4).
With nuclear lesions of CN XI, such as in motor neuron disease, the
weakness is frequently accompanied by atrophy and fasciculations.
extra-medullary but within the skull, in the jugular foramen, or in the
neck—are the most common causes of impairment of function of the SA
nerve. Basal skull fractures, meningitis, extramedullary neoplasms
within the skull, or processes at or just distal to the foramen give
rise to a number of syndromes reflecting involvement of the lower
cranial nerves. Such conditions affect both the SCM and the trapezius.
very vulnerable, since it lies superficially, covered only by skin and
subcutaneous tissue. The nerve may be affected by severe cervical
adenopathy, neoplasms, trauma, or abscesses. These lesions are
generally distal to the SCM and affect only trapezius function. The
most common cause of SA neuropathy in the posterior triangle is trauma,
often iatrogenic. Surgical trauma may be unavoidable, as in radical
neck dissection, or inadvertent, as in lymph node biopsy. Traction
injury may occur when the shoulder is pulled down and the head turned
in the opposite direction. Carrying heavy loads on the shoulder may
cause SA injury due to local trauma or stretch.
often benign and self-limited, are likely comparable to similar focal
neuropathies, such as Bell palsy or long thoracic nerve palsy, or may
represent a restricted type of neuralgic amyotrophy. In these cases,
the onset is typically sudden with pain in the posterior triangle,
which resolves and is followed by SA palsy.
trapezius muscles include anterior horn cell disease, myasthenia
gravis, polymyositis, dermatomyositis, and facioscapulohumeral
dystrophy. Atrophy and weakness of both sternocleidomastoid muscles is
a prominent feature of myotonic dystrophy (Figure 15.5).
The “dropped head syndrome,” characterized by severe neck extensor
weakness and an inability to hold the head up, occurs in a variety of
neuromuscular disorders, especially polymyositis and myasthenia gravis.
